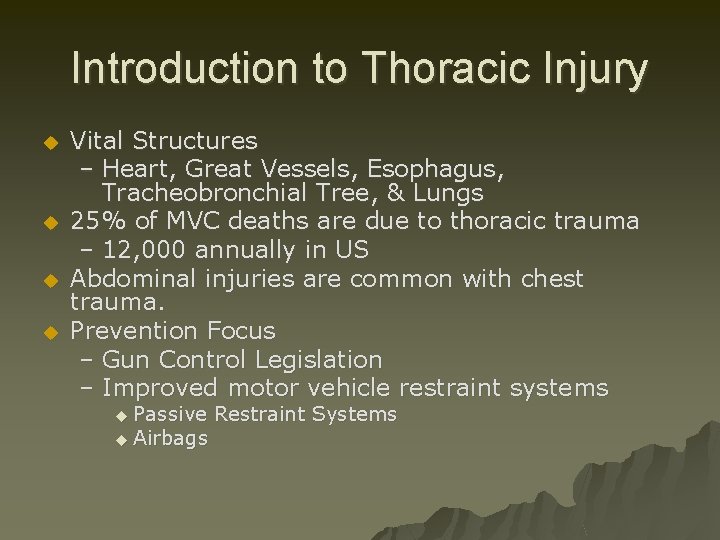
Introduction to Thoracic Injury u u Vital Structures





- Slides: 60
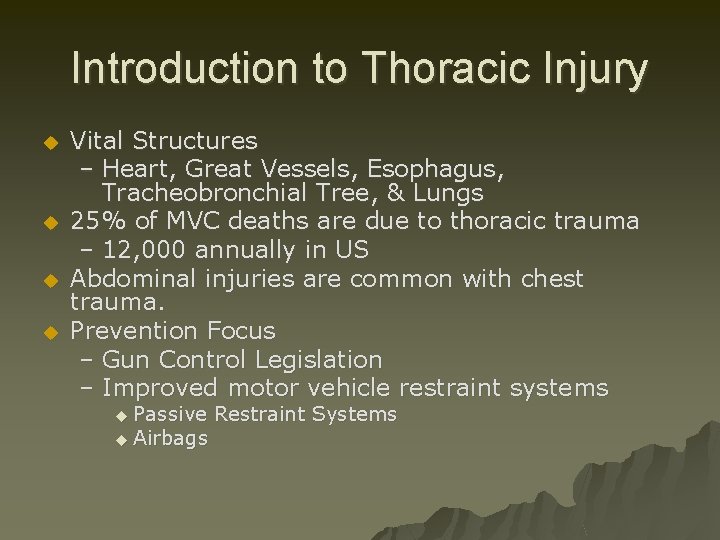
Introduction to Thoracic Injury u u Vital Structures – Heart, Great Vessels, Esophagus, Tracheobronchial Tree, & Lungs 25% of MVC deaths are due to thoracic trauma – 12, 000 annually in US Abdominal injuries are common with chest trauma. Prevention Focus – Gun Control Legislation – Improved motor vehicle restraint systems u Passive u Airbags Restraint Systems
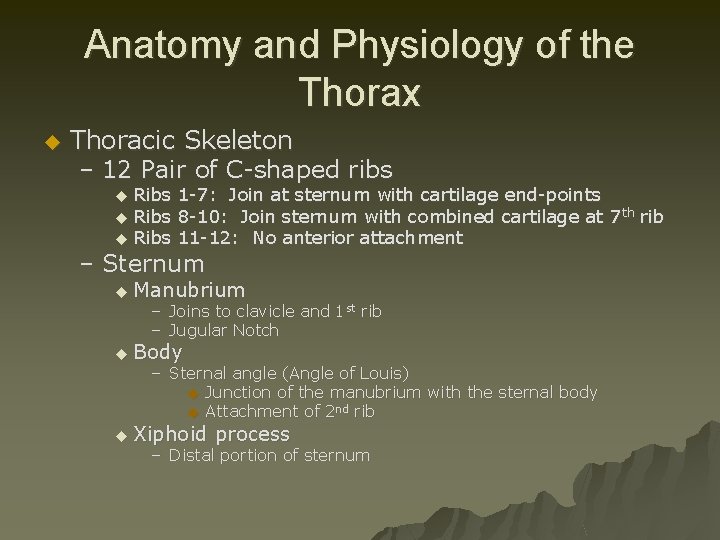
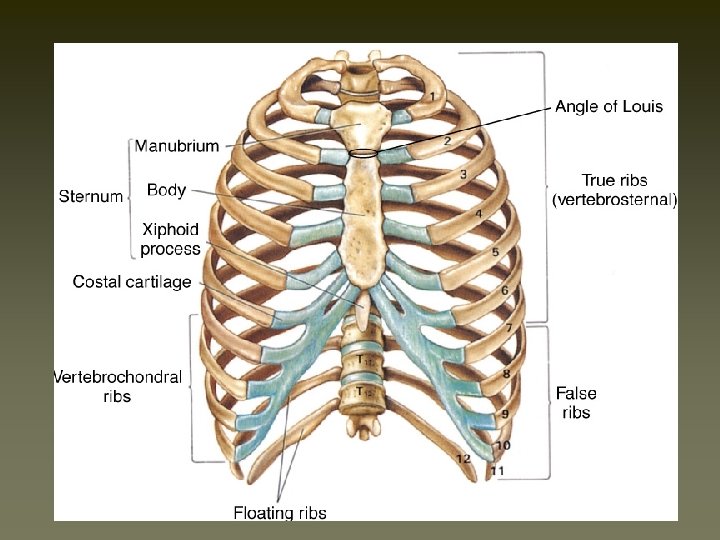
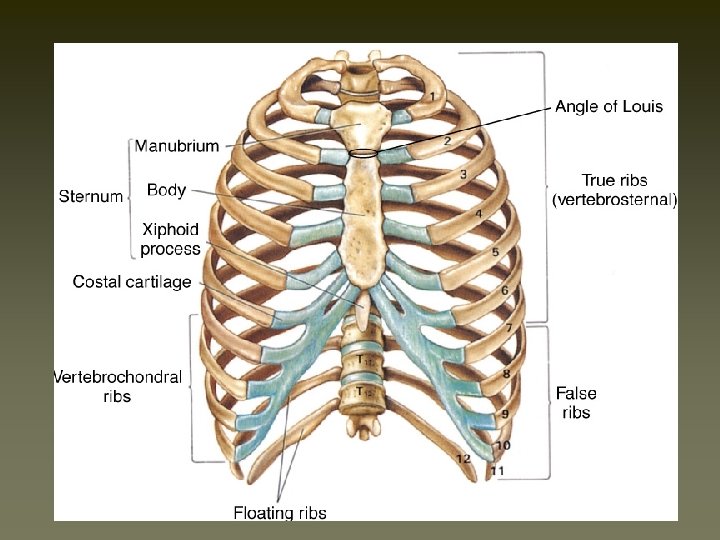
Anatomy and Physiology of the Thorax u Thoracic Skeleton – 12 Pair of C-shaped ribs Ribs 1 -7: Join at sternum with cartilage end-points u Ribs 8 -10: Join sternum with combined cartilage at 7 th rib u Ribs 11 -12: No anterior attachment u – Sternum u Manubrium – Joins to clavicle and 1 st rib – Jugular Notch u Body – Sternal angle (Angle of Louis) u Junction of the manubrium with the sternal body u Attachment of 2 nd rib u Xiphoid process – Distal portion of sternum
Anatomy and Physiology of the Thorax u Thoracic Skeleton – Topographical Thoracic Reference Lines Midclavicular line u Anterior axillary line u Mid-axillary line u Posterior axillary line u – Intercostal space u Artery, Vein and Nerve on inferior margin of each rib – Thoracic Inlet Superior opening of the thorax u Curvature of 1 st rib with associated structures u – Thoracic Outlet Inferior opening of the thorax u 12 th rib and associated structures & Xiphisternal joint u
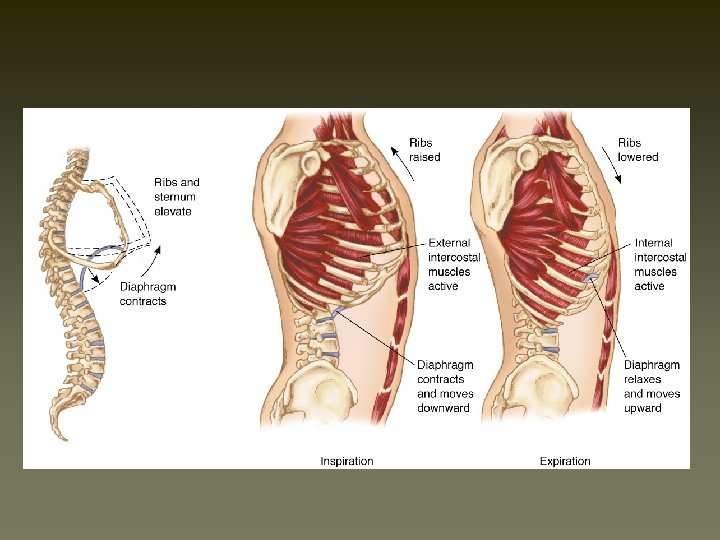
Anatomy and Physiology of the Thorax u Diaphragm – Muscular, dome-like structure – Separates abdomen from the thoracic cavity – Affixed to the lower border of the rib cage – Central and superior margin extends to the level of the 4 th rib anteriorly and 6 th rib posteriorly – Major muscle of respiration u Draws downward during inspiration u Moves upward during exhalation
Anatomy and Physiology of the Thorax u Associated Musculature – Shoulder girdle – Muscles of respiration u. Diaphragm u. Intercostal muscles – Contract to elevate the ribs and increase thoracic diameter – Increase depth of respiration u. Sternocleidomastoid – Raise upper rib and sternum
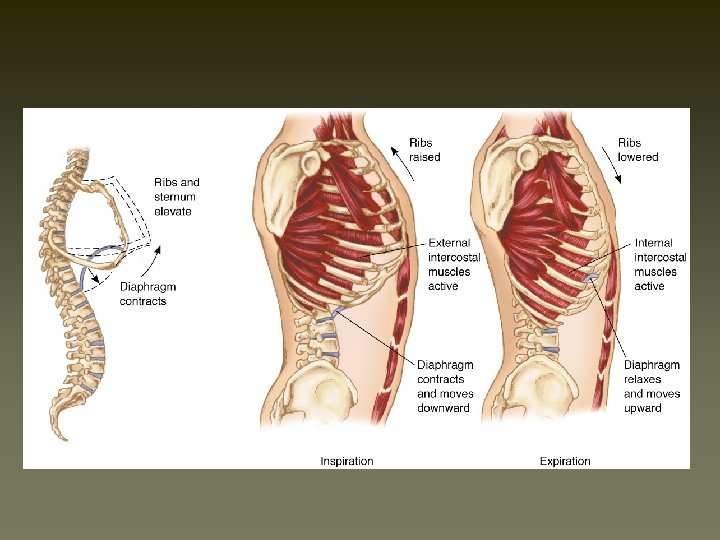
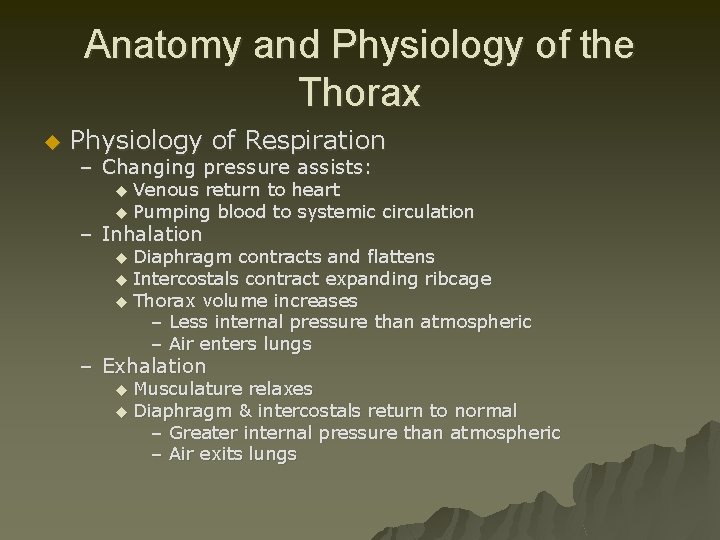
Anatomy and Physiology of the Thorax u Physiology of Respiration – Changing pressure assists: Venous return to heart u Pumping blood to systemic circulation u – Inhalation Diaphragm contracts and flattens u Intercostals contract expanding ribcage u Thorax volume increases – Less internal pressure than atmospheric – Air enters lungs u – Exhalation Musculature relaxes u Diaphragm & intercostals return to normal – Greater internal pressure than atmospheric – Air exits lungs u
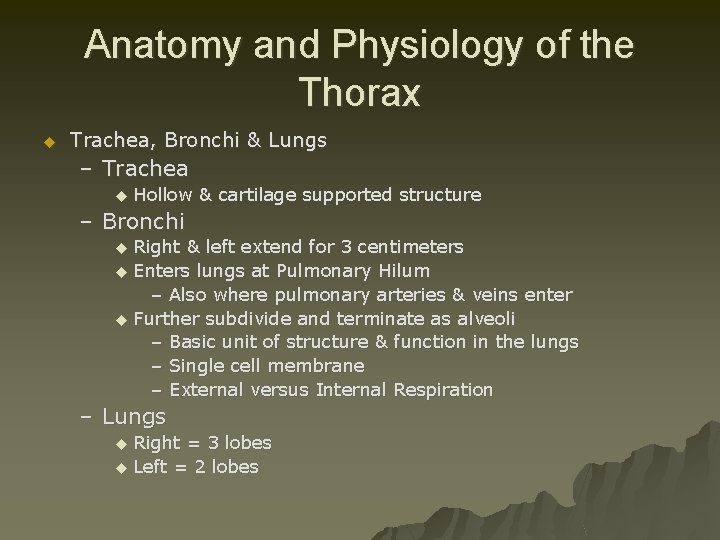
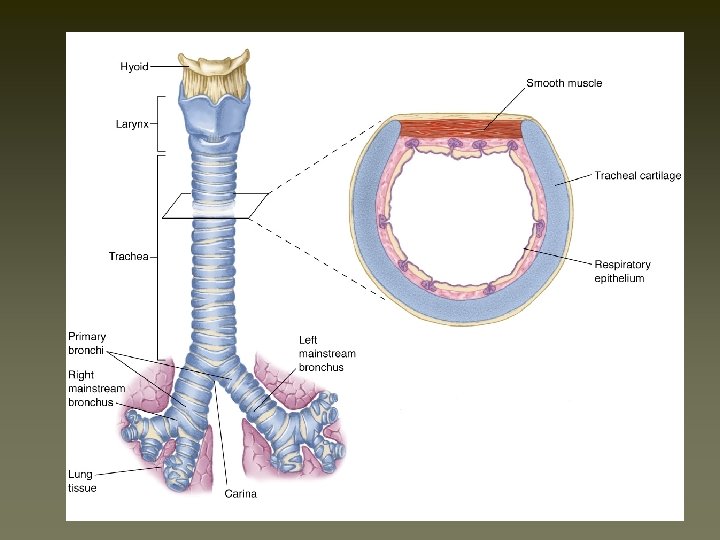
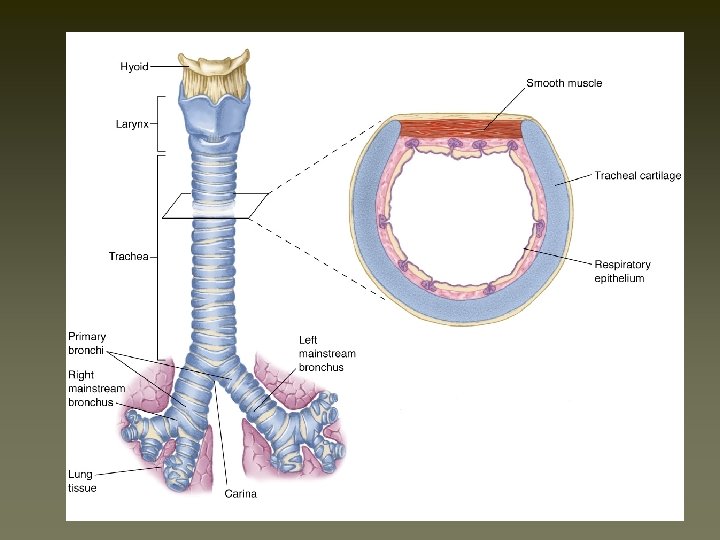
Anatomy and Physiology of the Thorax u Trachea, Bronchi & Lungs – Trachea u Hollow & cartilage supported structure – Bronchi Right & left extend for 3 centimeters u Enters lungs at Pulmonary Hilum – Also where pulmonary arteries & veins enter u Further subdivide and terminate as alveoli – Basic unit of structure & function in the lungs – Single cell membrane – External versus Internal Respiration u – Lungs Right = 3 lobes u Left = 2 lobes u
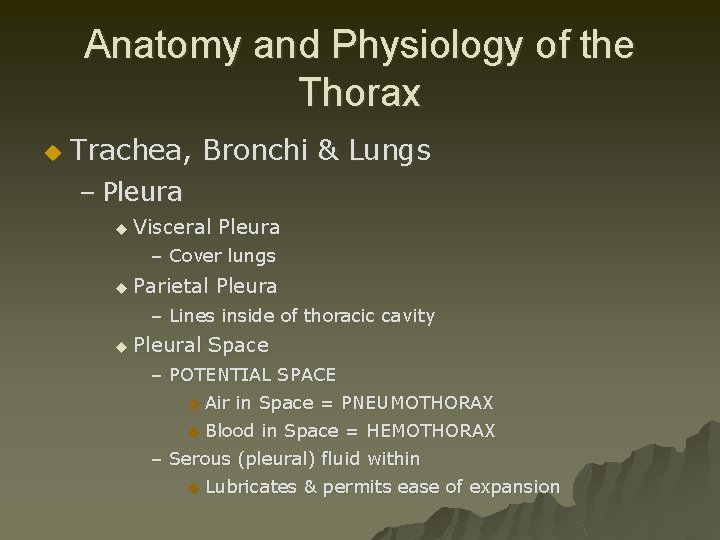
Anatomy and Physiology of the Thorax u Trachea, Bronchi & Lungs – Pleura u Visceral Pleura – Cover lungs u Parietal Pleura – Lines inside of thoracic cavity u Pleural Space – POTENTIAL SPACE u Air in Space = PNEUMOTHORAX u Blood in Space = HEMOTHORAX – Serous (pleural) fluid within u Lubricates & permits ease of expansion
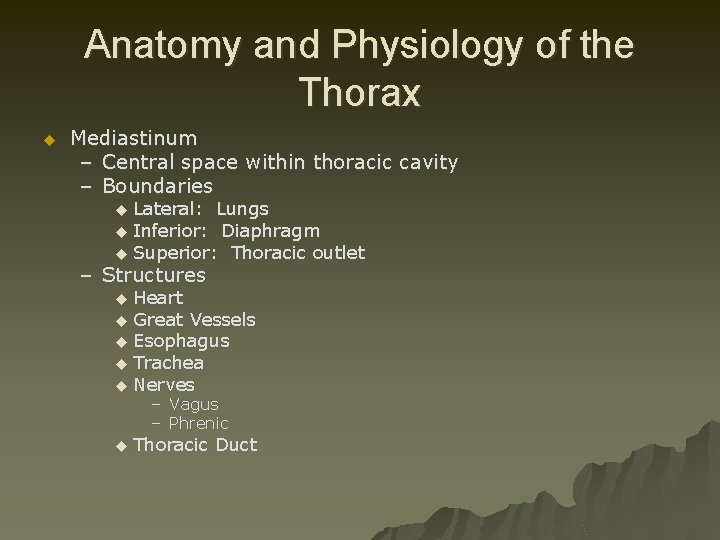
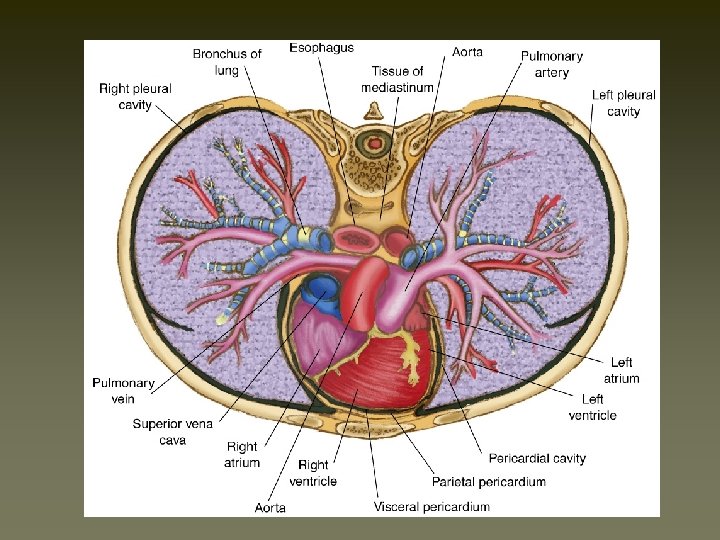
Anatomy and Physiology of the Thorax u Mediastinum – Central space within thoracic cavity – Boundaries Lateral: Lungs u Inferior: Diaphragm u Superior: Thoracic outlet u – Structures Heart u Great Vessels u Esophagus u Trachea u Nerves u – Vagus – Phrenic u Thoracic Duct
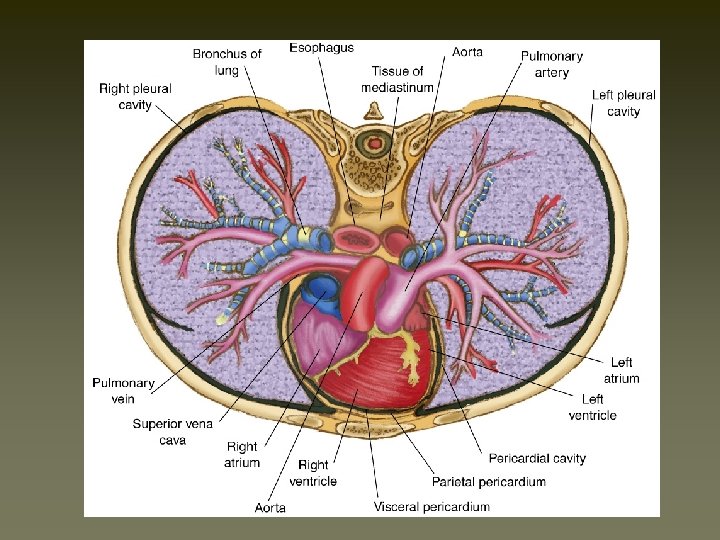
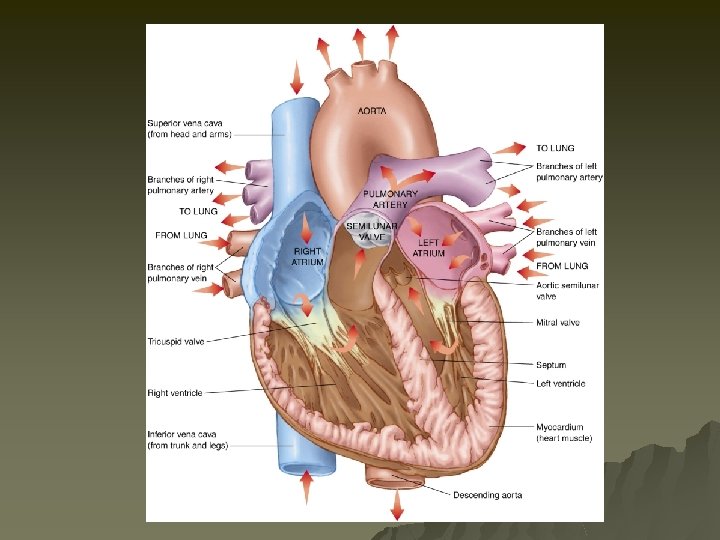
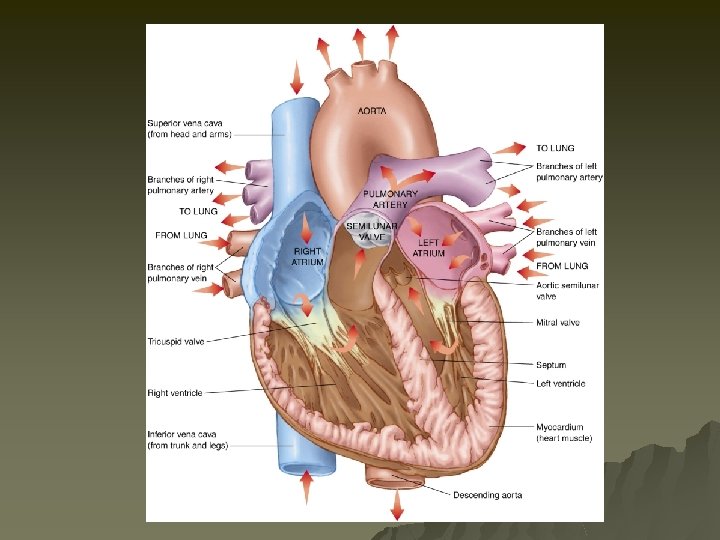
Anatomy and Physiology of the Thorax u Heart – Chambers – Valves – Vessels – External Vessels u Coronary u Arteries Contraction Cycle – Systole – Diastole u Filling of the coronary arteries occur
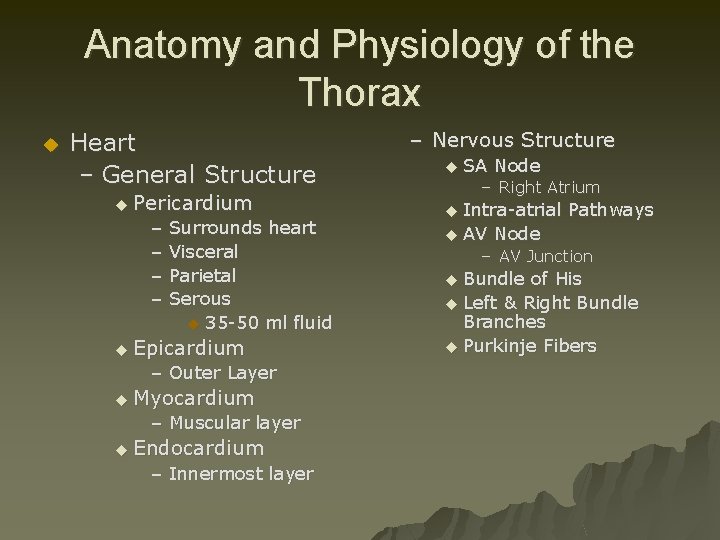
Anatomy and Physiology of the Thorax u Heart – General Structure u Pericardium – Surrounds heart – Visceral – Parietal – Serous u 35 -50 ml fluid u Epicardium – Outer Layer u Myocardium – Muscular layer u Endocardium – Innermost layer – Nervous Structure u SA Node – Right Atrium Intra-atrial Pathways u AV Node u – AV Junction Bundle of His u Left & Right Bundle Branches u Purkinje Fibers u
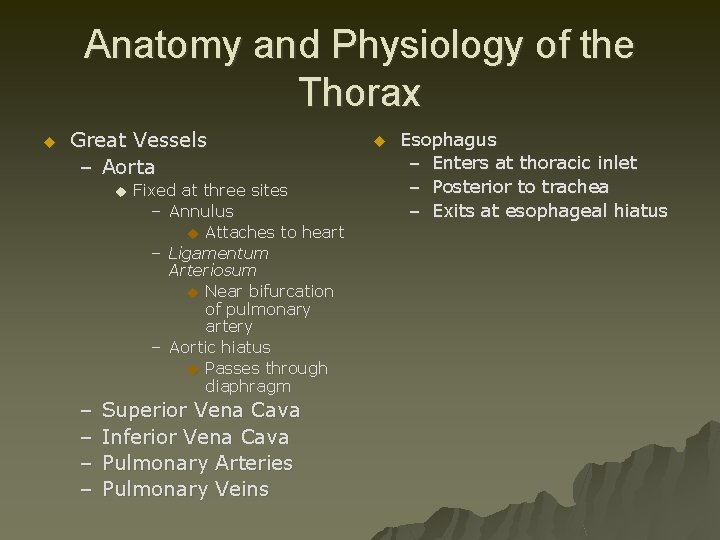
Anatomy and Physiology of the Thorax u Great Vessels – Aorta u – – Fixed at three sites – Annulus u Attaches to heart – Ligamentum Arteriosum u Near bifurcation of pulmonary artery – Aortic hiatus u Passes through diaphragm Superior Vena Cava Inferior Vena Cava Pulmonary Arteries Pulmonary Veins u Esophagus – Enters at thoracic inlet – Posterior to trachea – Exits at esophageal hiatus
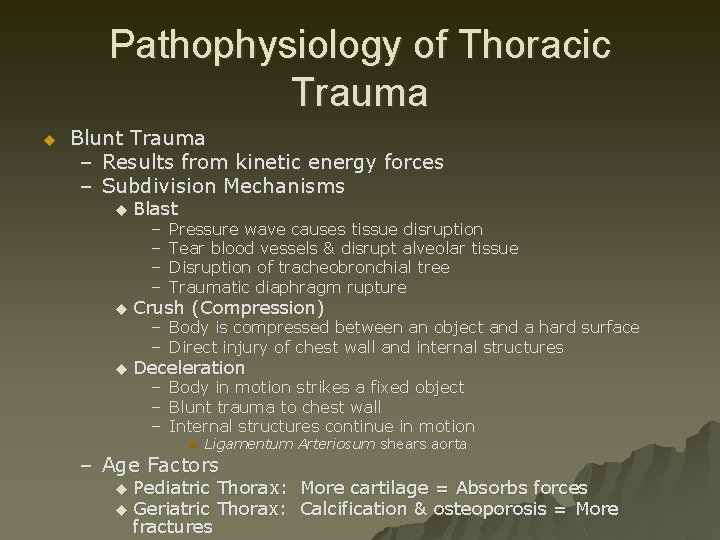
Pathophysiology of Thoracic Trauma u Blunt Trauma – Results from kinetic energy forces – Subdivision Mechanisms u Blast – – Pressure wave causes tissue disruption Tear blood vessels & disrupt alveolar tissue Disruption of tracheobronchial tree Traumatic diaphragm rupture u Crush (Compression) u Deceleration – Body is compressed between an object and a hard surface – Direct injury of chest wall and internal structures – – – Body in motion strikes a fixed object Blunt trauma to chest wall Internal structures continue in motion u Ligamentum Arteriosum shears aorta – Age Factors Pediatric Thorax: More cartilage = Absorbs forces u Geriatric Thorax: Calcification & osteoporosis = More fractures u
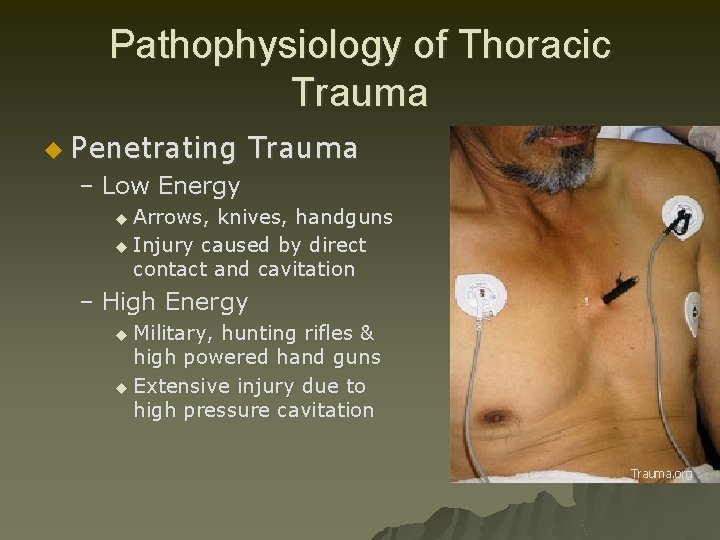
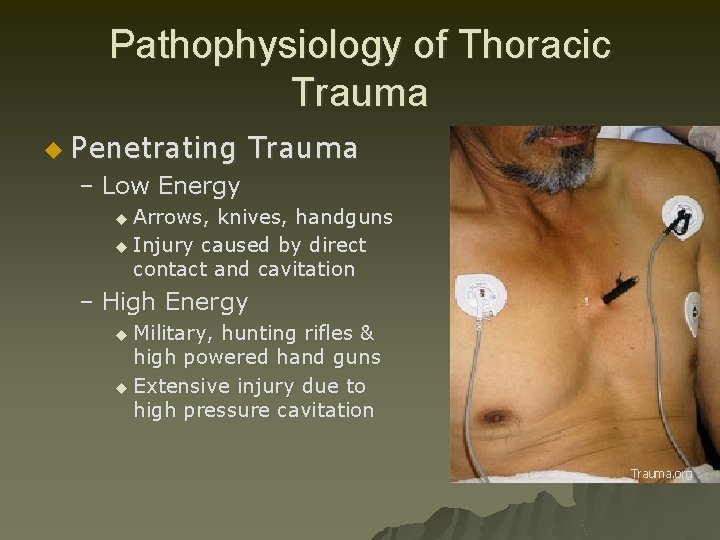
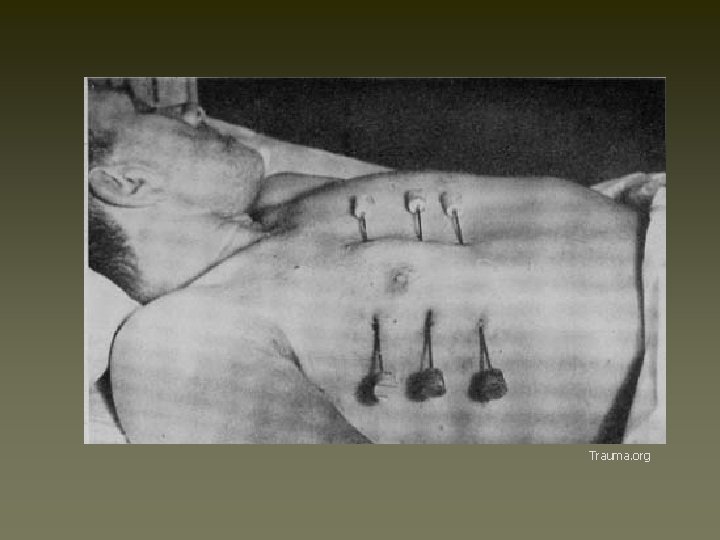
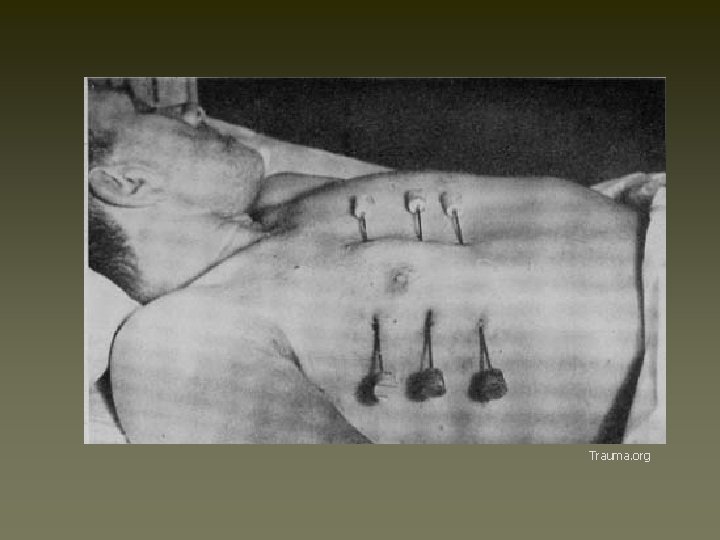
Pathophysiology of Thoracic Trauma u Penetrating Trauma – Low Energy u Arrows, knives, handguns u Injury caused by direct contact and cavitation – High Energy u Military, hunting rifles & high powered hand guns u Extensive injury due to high pressure cavitation Trauma. org
Pathophysiology of Thoracic Trauma u Penetrating Injuries (cont. ) – Shotgun u Injury severity based upon the distance between the victim and shotgun & caliber of shot u Type I: >7 meters from the weapon – Soft tissue injury u Type II: 3 -7 meters from weapon – Penetration into deep fascia and some internal organs u Type III: <3 meters from weapon – Massive tissue destruction

Trauma. org
Injuries Associated with Penetrating Thoracic Trauma u u u u Closed pneumothorax Open pneumothorax (including sucking chest wound) Tension pneumothorax Pneumomediastinum Hemothorax Hemopneumothorax Laceration of vascular structures u u u u Tracheobronchial tree lacerations Esophageal lacerations Penetrating cardiac injuries Pericardial tamponade Spinal cord injuries Diaphragm trauma Intra-abdominal penetration with associated organ injury
Pathophysiology of Thoracic Trauma Chest Wall Injuries u Contusion – Most Common result of blunt injury – Signs & Symptoms u Erythema u Ecchymosis u DYSPNEA u PAIN on breathing u Limited breath sounds u HYPOVENTILATION – BIGGEST CONCERN = “HURTS TO BREATHE” u Crepitus u Paradoxical chest wall motion
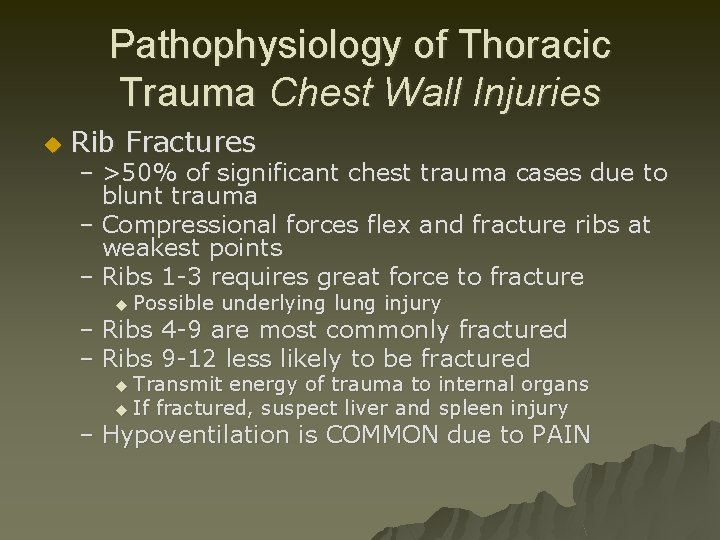
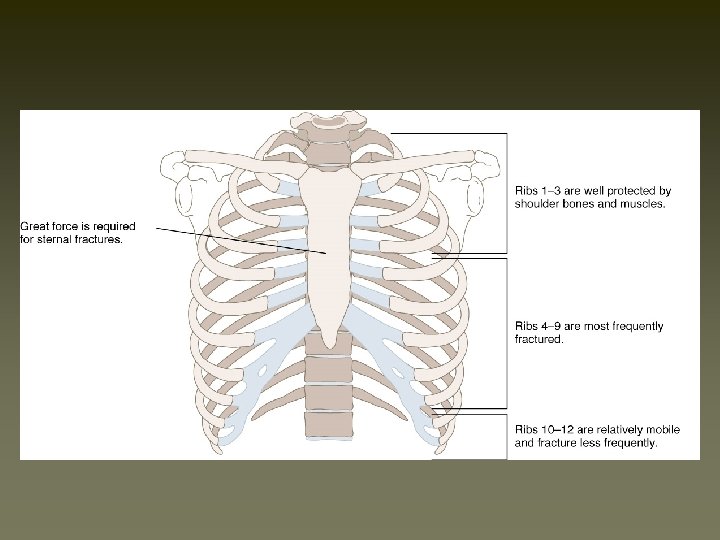
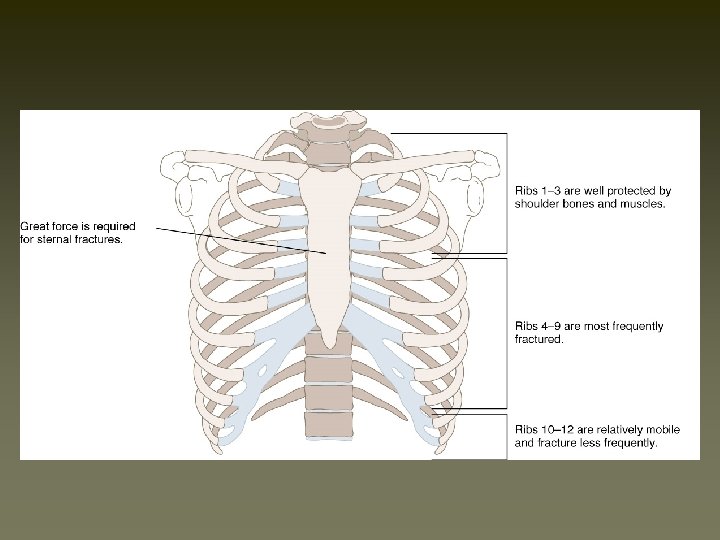
Pathophysiology of Thoracic Trauma Chest Wall Injuries u Rib Fractures – >50% of significant chest trauma cases due to blunt trauma – Compressional forces flex and fracture ribs at weakest points – Ribs 1 -3 requires great force to fracture u Possible underlying lung injury – Ribs 4 -9 are most commonly fractured – Ribs 9 -12 less likely to be fractured u Transmit energy of trauma to internal organs u If fractured, suspect liver and spleen injury – Hypoventilation is COMMON due to PAIN

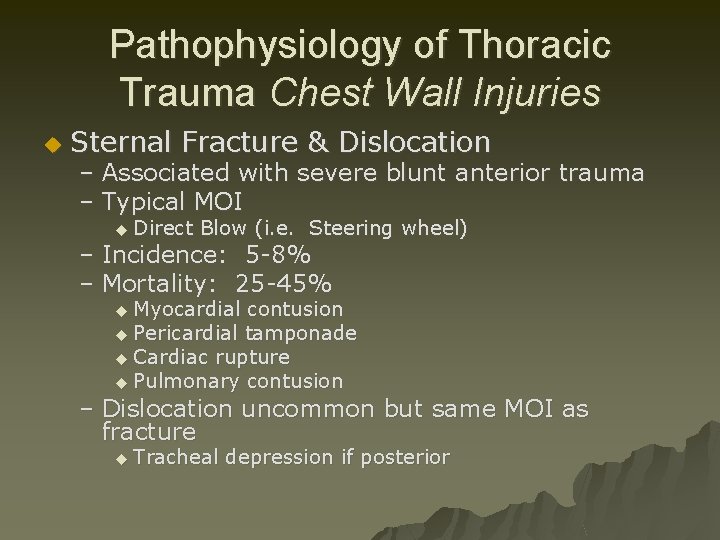
Pathophysiology of Thoracic Trauma Chest Wall Injuries u Sternal Fracture & Dislocation – Associated with severe blunt anterior trauma – Typical MOI u Direct Blow (i. e. Steering wheel) – Incidence: 5 -8% – Mortality: 25 -45% u Myocardial contusion u Pericardial tamponade u Cardiac rupture u Pulmonary contusion – Dislocation uncommon but same MOI as fracture u Tracheal depression if posterior
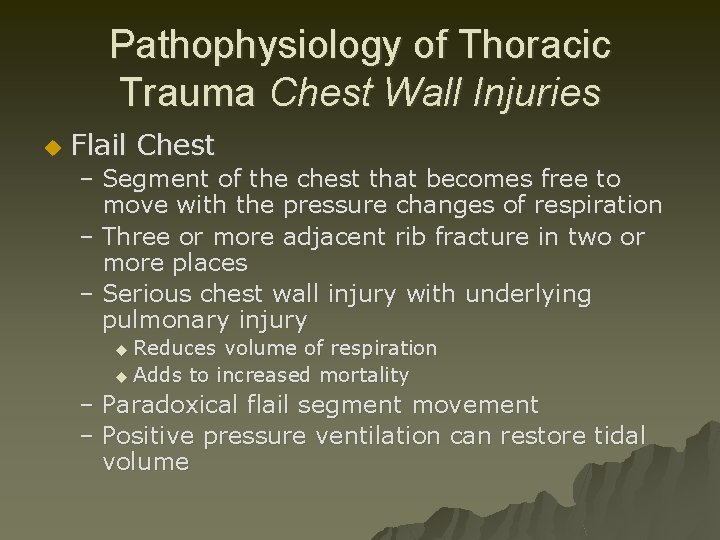
Pathophysiology of Thoracic Trauma Chest Wall Injuries u Flail Chest – Segment of the chest that becomes free to move with the pressure changes of respiration – Three or more adjacent rib fracture in two or more places – Serious chest wall injury with underlying pulmonary injury u Reduces volume of respiration u Adds to increased mortality – Paradoxical flail segment movement – Positive pressure ventilation can restore tidal volume
Pathophysiology of Thoracic Trauma Pulmonary Injuries u Simple Pneumothorax – AKA: Closed Pneumothorax u Progresses into Tension Pneumothorax – Occurs when lung tissue is disrupted and air leaks into the pleural space – Progressive Pathology Air accumulates in pleural space u Lung collapses u Alveoli collapse (atelectasis) u Reduced oxygen and carbon dioxide exchange u u Ventilation/Perfusion Mismatch – Increased ventilation but no alveolar perfusion – Reduced respiratory efficiency results in HYPOXIA – Typical MOI: “Paper Bag Syndrome”
Pathophysiology of Thoracic Trauma Pulmonary Injuries u Open Pneumothorax – Free passage of air between atmosphere and pleural space – Air replaces lung tissue – Mediastinum shifts to uninjured side – Air will be drawn through wound if wound is 2/3 diameter of the trachea or larger – Signs & Symptoms u Penetrating chest trauma u Sucking chest wound u Frothy blood at wound site u Severe Dyspnea u Hypovolemia
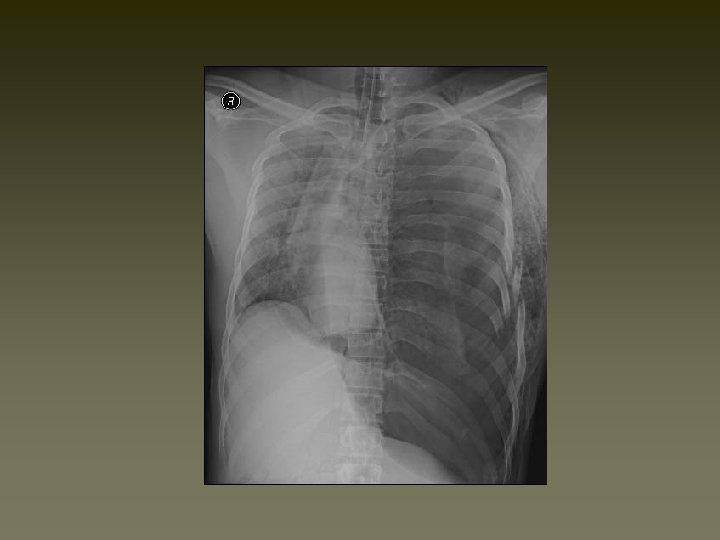
Pathophysiology of Thoracic Trauma Pulmonary Injuries u Tension Pneumothorax – Buildup of air under pressure in the thorax. – Excessive pressure reduces effectiveness of respiration – Air is unable to escape from inside the pleural space – Progression of Simple or Open Pneumothorax
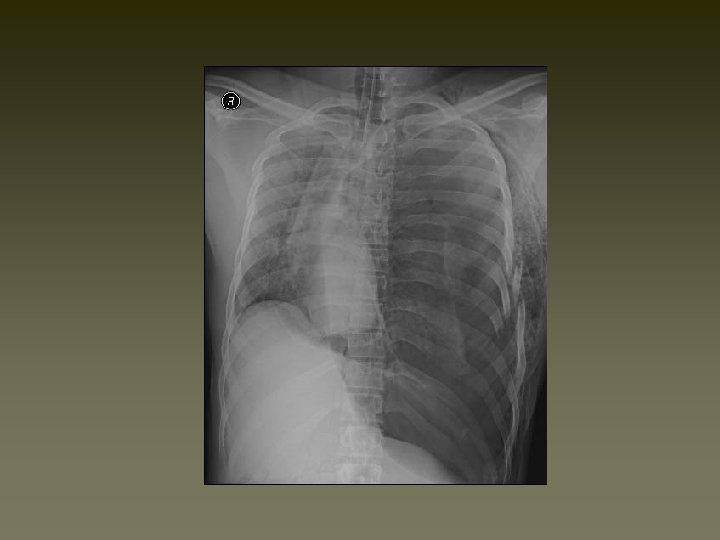
Pathophysiology of Thoracic Trauma Pulmonary Injuries Tension Pneumothorax Signs & Symptoms u u u Dyspnea – Tachypnea at first Progressive ventilation/perfusion mismatch – Atelectasis on uninjured side Hypoxemia Hyperinflation of injured side of chest Hyperresonance of injured side of chest u u u u Diminished then absent breath sounds on injured side Cyanosis Diaphoresis AMS JVD Hypotension Hypovolemia Tracheal Shifting – LATE SIGN
Pathophysiology of Thoracic Trauma Pulmonary Injuries u Hemothorax – Accumulation of blood in the pleural space – Serious hemorrhage may accumulate 1, 500 m. L of blood u Mortality rate of 75% u Each side of thorax may hold up to 3, 000 m. L – Blood loss in thorax causes a decrease in tidal volume u Ventilation/Perfusion Mismatch & Shock – Typically accompanies pneumothorax u Hemopneumothorax

Trauma. org

Pathophysiology of Thoracic Trauma Pulmonary Injuries u Blunt Hemothorax Signs & Symptoms or penetrating chest trauma u Shock – Dyspnea – Tachycardia – Tachypnea – Diaphoresis – Hypotension u Dull to percussion over injured side
Pathophysiology of Thoracic Trauma Pulmonary Injuries u Pulmonary Contusion – – Soft tissue contusion of the lung 30 -75% of patients with significant blunt chest trauma Frequently associated with rib fracture Typical MOI u Deceleration – Chest impact on steering wheel u Bullet Cavitation – High velocity ammunition – Microhemorrhage may account for 1 - 1 ½ L of blood loss in alveolar tissue u Progressive deterioration of ventilatory status – Hemoptysis typically present
Pathophysiology of Thoracic Trauma Cardiovascular Injuries u Myocardial Contusion – Occurs in 76% of patients with severe blunt chest trauma – Right Atrium and Ventricle is commonly injured – Injury may reduce strength of cardiac contractions u Reduced cardiac output – Electrical Disturbances due to irritability of damaged myocardial cells – Progressive Problems u Hematoma u Hemoperitoneum u Myocardial necrosis u Dysrhythmias u CHF & or Cardiogenic shock
Pathophysiology of Thoracic Trauma Cardiovascular Injuries Myocardial Contusion Signs & Symptoms u Bruising of chest wall u Tachycardia and/or irregular rhythm u Retrosternal pain similar to MI u Associated injuries – Rib/Sternal fractures u Chest pain unrelieved by oxygen – May be relieved with rest – THIS IS TRAUMA-RELATED PAIN u Similar signs and symptoms of medical chest pain
Pathophysiology of Thoracic Trauma Cardiovascular Injuries u Pericardial Tamponade – Restriction to cardiac filling caused by blood or other fluid within the pericardium – Occurs in <2% of all serious chest trauma u However, very high mortality – Results from tear in the coronary artery or penetration of myocardium u Blood seeps into pericardium and is unable to escape u 200 -300 ml of blood can restrict effectiveness of cardiac contractions – Removing as little as 20 ml can provide relief
Pathophysiology of Thoracic Trauma Cardiovascular Injuries Pericardial Tamponade Signs & Symptoms u u u Dyspnea Possible cyanosis Beck’s Triad – JVD – Distant heart tones – Hypotension or narrowing pulse pressure u u Weak, thready pulse Shock u u Kussmaul’s sign – Decrease or absence of JVD during inspiration Pulsus Paradoxus – Drop in SBP >10 during inspiration – Due to increase in CO 2 during inspiration Electrical Alterans – P, QRS, & T amplitude changes in every other cardiac cycle PEA
Pathophysiology of Thoracic Trauma Cardiovascular Injuries u Myocardial Aneurysm or Rupture – Occurs almost exclusively with extreme blunt thoracic trauma – Secondary due to necrosis resulting from MI – Signs & Symptoms u Severe rib or sternal fracture u Possible signs and symptoms of cardiac tamponade u If affects valves only – Signs & symptoms of right or left heart failure u Absence of vital signs
Pathophysiology of Thoracic Trauma Cardiovascular Injuries u Traumatic Aneurysm or Aortic Rupture – Aorta most commonly injured in severe blunt or penetrating trauma u 85 -95% mortality – Typically patients will survive the initial injury insult u 30% mortality in 6 hrs u 50% mortality in 24 hrs u 70% mortality in 1 week – Injury may be confined to areas of aorta attachment – Signs & Symptoms u Rapid and deterioration of vitals u Pulse deficit between right and left upper or lower extremities
Pathophysiology of Thoracic Trauma Cardiovascular Injuries u Other Vascular Injuries – Rupture or laceration Superior Vena Cava u Inferior Vena Cava u General Thoracic Vasculature u – Blood Localizing in Mediastinum – Compression of: Great vessels u Myocardium u Esophagus u – General Signs & Symptoms Penetrating Trauma u Hypovolemia & Shock u Hemothorax or hemomediastinum u
Pathophysiology of Thoracic Trauma Other Thoracic Injuries u Traumatic Esophageal Rupture – Rare complication of blunt thoracic trauma – 30% mortality – Contents in esophagus/stomach may move into mediastinum u Serious Infection occurs u Chemical irritation u Damage to mediastinal structures u Air enters mediastinum – Subcutaneous emphysema and penetrating trauma present
Pathophysiology of Thoracic Trauma Other Thoracic Injuries u Tracheobronchial Injury – MOI Blunt trauma u Penetrating trauma u – 50% of patients with injury die within 1 hr of injury – Disruption can occur anywhere in tracheobronchial tree – Signs & Symptoms Dyspnea u Cyanosis u Hemoptysis u Massive subcutaneous emphysema u Suspect/Evaluate for other closed chest trauma u
Pathophysiology of Thoracic Trauma Other Thoracic Injuries u Traumatic Asphyxia – Results from severe compressive forces applied to the thorax – Causes backwards flow of blood from right side of heart into superior vena cava and the upper extremities – Signs & Symptoms u Head & Neck become engorged with blood – Skin becomes deep red, purple, or blue – NOT RESPIRATORY RELATED u JVD u Hypotension, Hypoxemia, Shock u Face and tongue swollen u Bulging eyes with conjunctival hemorrhage
Assessment of the Thoracic Trauma Patient u Scene Size-up u Initial Assessment u Rapid Trauma Assessment – Observe u JVD, SQ Emphysema, Expansion of chest – Question – Palpate – Auscultate – Percuss – Blunt Trauma Assessment – Penetrating Trauma Assessment u Ongoing Assessment
Management of the Chest Injury Patient General Management u Ensure ABC’s – – High flow O 2 via NRB Intubate if indicated Consider RSI Consider overdrive ventilation If tidal volume less than 6, 000 m. L u BVM at a rate of 12 -16 u – May be beneficial for chest contusion and rib fractures – Promotes oxygen perfusion of alveoli and prevents atelectasis u u Anticipate Myocardial Compromise Shock Management – Consider PASG u Only in blunt chest trauma with SP <60 mm Hg – Fluid Bolus: 20 m. L/kg – AUSCULTATE! AUSCULATE!

Management of the Chest Injury Patient u Rib Fractures – Consider analgesics for pain and to improve chest excursion u Versed u Morphine Sulfate – CONTRAINDICATION u Nitrous Oxide – May migrate into pleural or mediastinal space and worsen condition
Management of the Chest Injury Patient u u Sternoclavicular Dislocation – Supportive O 2 therapy – Evaluate for concomitant injury Flail Chest – Place patient on side of injury u ONLY if spinal injury is NOT suspected – Expose injury site – Dress with bulky bandage against flail segment u Stabilizes fracture site – High flow O 2 u Consider PPV or ET if decreasing respiratory status – DO NOT USE SANDBAGS TO STABILIZE FX
Trauma. org
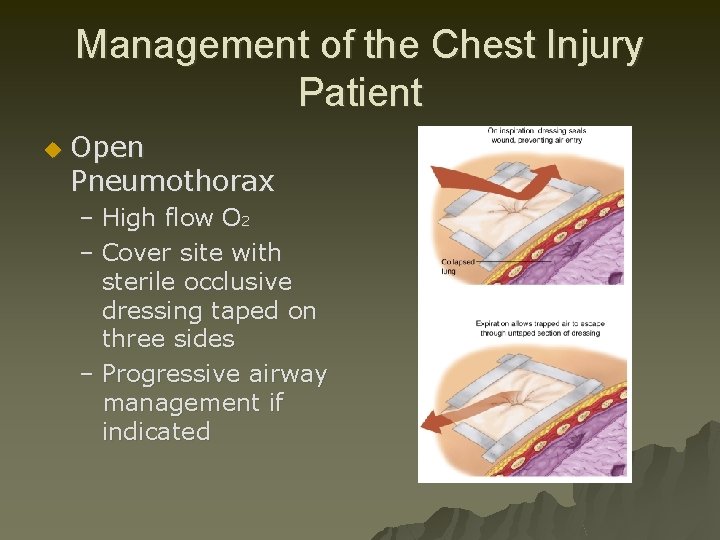
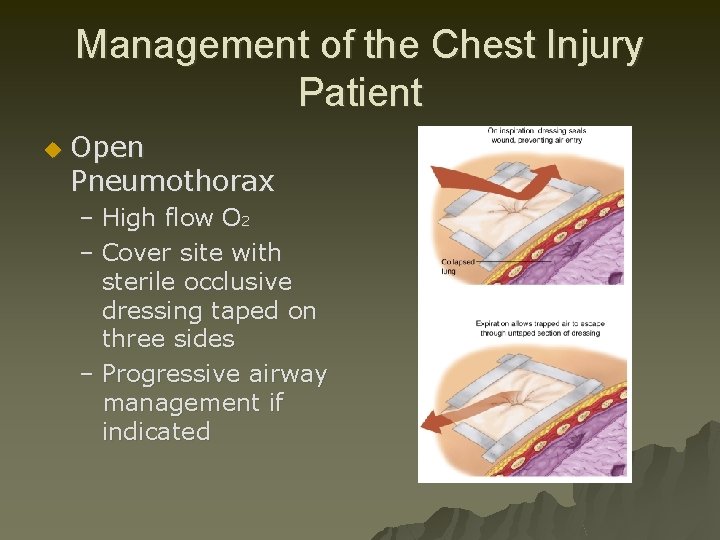
Management of the Chest Injury Patient u Open Pneumothorax – High flow O 2 – Cover site with sterile occlusive dressing taped on three sides – Progressive airway management if indicated
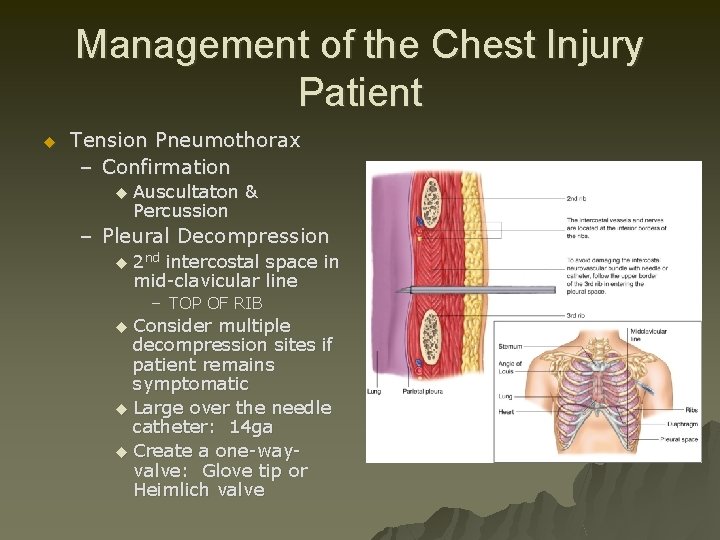
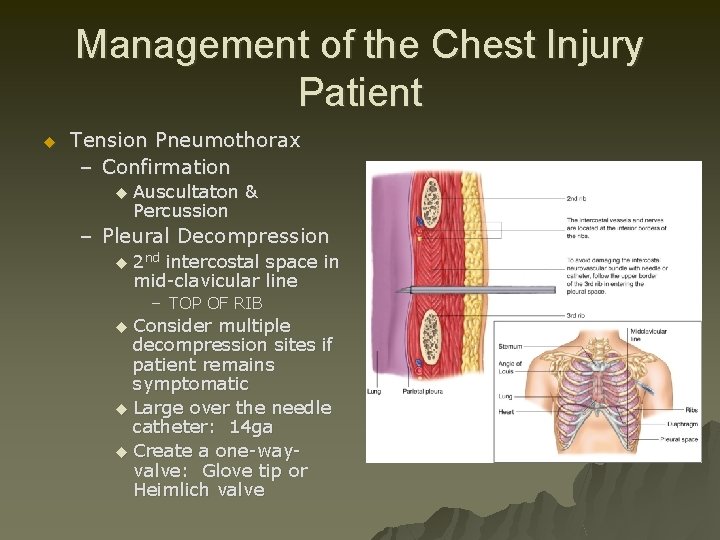
Management of the Chest Injury Patient u Tension Pneumothorax – Confirmation u Auscultaton & Percussion – Pleural Decompression u 2 nd intercostal space in mid-clavicular line – TOP OF RIB Consider multiple decompression sites if patient remains symptomatic u Large over the needle catheter: 14 ga u Create a one-wayvalve: Glove tip or Heimlich valve u
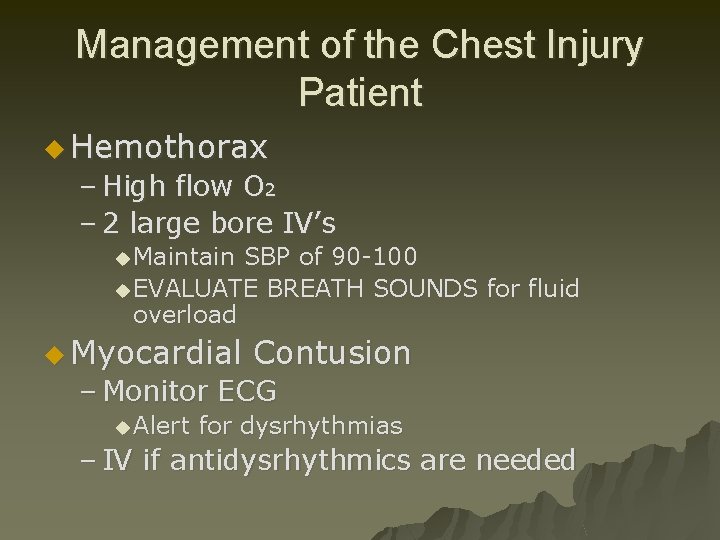
Management of the Chest Injury Patient u Hemothorax – High flow O 2 – 2 large bore IV’s u Maintain SBP of 90 -100 u EVALUATE BREATH SOUNDS for fluid overload u Myocardial Contusion – Monitor ECG u Alert for dysrhythmias – IV if antidysrhythmics are needed
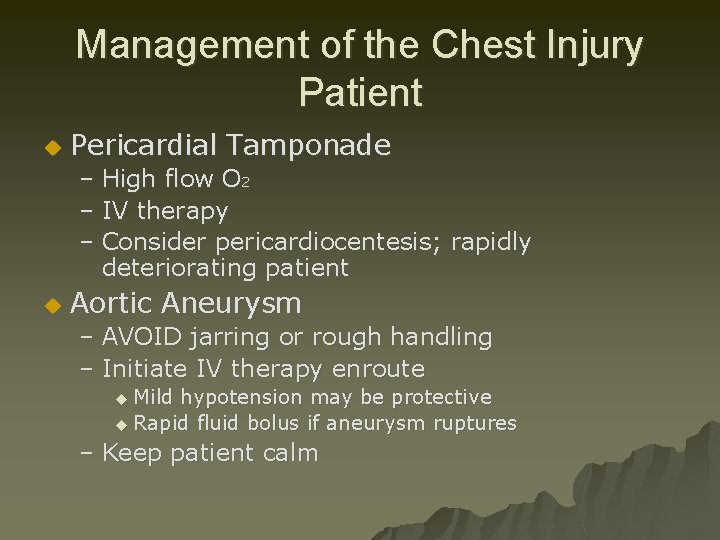
Management of the Chest Injury Patient u Pericardial Tamponade – High flow O 2 – IV therapy – Consider pericardiocentesis; rapidly deteriorating patient u Aortic Aneurysm – AVOID jarring or rough handling – Initiate IV therapy enroute u Mild hypotension may be protective u Rapid fluid bolus if aneurysm ruptures – Keep patient calm
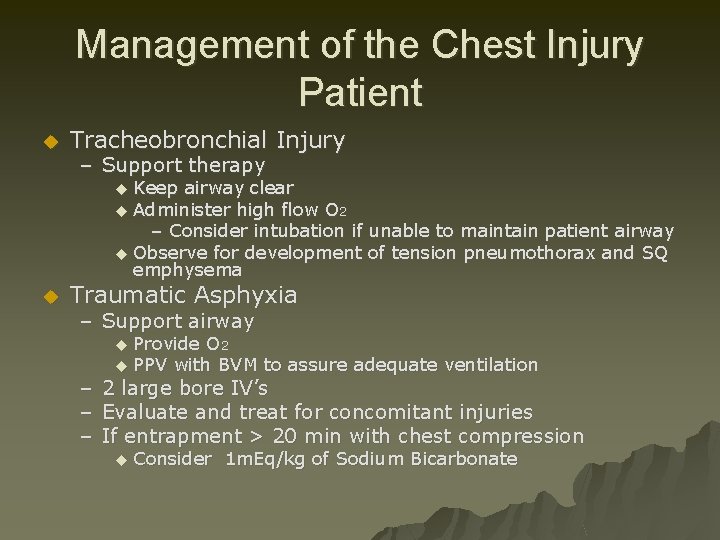
Management of the Chest Injury Patient u Tracheobronchial Injury – Support therapy Keep airway clear u Administer high flow O 2 – Consider intubation if unable to maintain patient airway u Observe for development of tension pneumothorax and SQ emphysema u u Traumatic Asphyxia – Support airway Provide O 2 u PPV with BVM to assure adequate ventilation u – 2 large bore IV’s – Evaluate and treat for concomitant injuries – If entrapment > 20 min with chest compression u Consider 1 m. Eq/kg of Sodium Bicarbonate