Introduction to the TPL Process New Business Billing
Introduction to the TPL Process New Business, Billing, Liens, Denials & Appeals
Our Job Mission: We assist hospitals in getting their invoices paid in full u We represent the hospital u You will be communicating with insurance companies, patients, medical professionals, government agencies and attorneys u You are a representative of the hospital and of Cardon Outreach
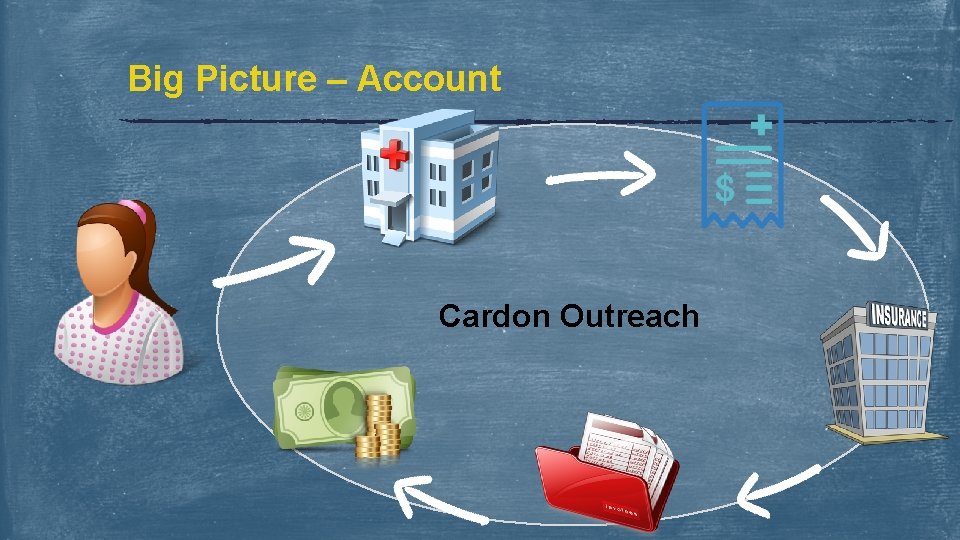
Big Picture – Account Cardon Outreach
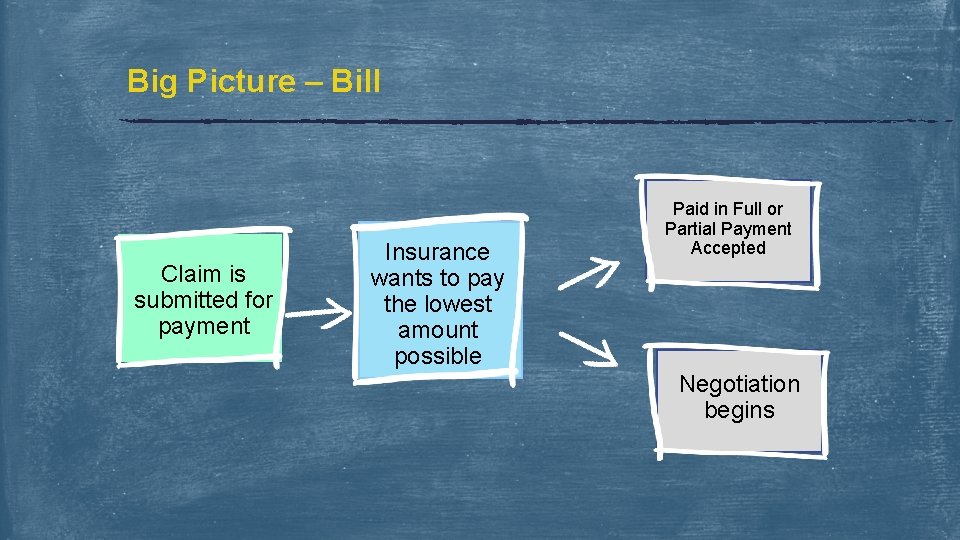
Big Picture – Bill Claim is submitted for payment Insurance wants to pay the lowest amount possible Paid in Full or Partial Payment Accepted Negotiation begins
Reason for Negotiation or an Appeal u Understanding payment u Assignment why the bill is being negotiated or pending of Benefits (NF 4) u No Fault Application (NF 2) u EUO – Examination Under Oath u Police Report u Medical Records u Duplicate Charges u Physician Bill u Fee Schedule - Hospital or State Specific u Timely Filing u Demand Packet from Attorney
Understanding: The Reasons for a Negotiation or an Appeal Assignment of Benefits (AOB, NF 4) - Assignment of benefits is a form the patient signs authorizing the hospital to receive pip funds as payment for his treatment. No Fault Application (PIP APP, NF 2) - A form that an injured person must complete and return to the PIP adjustor before any PIP payments can be issued. Contacting patients to force them to return a PIP App may be necessary to generate payment on some accounts. Examination Under Oath – EUO - The examination under oath is an important tool to help an insured prove his or her loss or to allow an insurer to cross-examine the proofs of loss to avoid potential fraud. Police Report - Proof of accident details Medical Records - A detailed report of a patient’s injuries at the time of treatment. Medrex are used by adjustors in conjunction with Medical Bill to determine that the treatment is related to the accident. Medical records can also verify any coding, including duplicate coding or necessary continuation of treatment.
Understanding: The Reasons for a Negotiation or an Appeal Physician Bill - A lot of times the adjustor will request all related medical bills, this forces them to wait on the treating doctors bill to be received. Cardon does not handle the physician billing, so therefore we refer them back to the hospital to follow up with any outstanding physician bills. Fee Schedule - A list of maximum allowable charges for medical procedures or a list of charges established or agreed to by professionals within the field of medicine. Often also referred to as usual and customary rates (UCR), the fee schedule is often cited by insurance companies who short-pay on medical bills and liens. While insurance companies are allowed to pay according to the fee schedule, hospitals are not required to accept fee schedule payments as payment in full. Timely Filing - Patients and providers (Hospital & Cardon) must file claims within a qualifying time limit for payment to be considered. If both entities fail to do so, this may lead to a self pay or a hospital write off. Each State has a timely filing parameter, where medical bills and medical records must be submitted under a certain amount of days. Demand Packet - A packet of information that the attorney provides to the liability adjustor that includes his/her assessment as to what the case is worth. The demand will also include an offer from the attorney to settle the case should the adjustor agree to pay a determined sum of money. The adjustor can accept the demand move toward settlement or can counter-offer and continue negotiations.
Reasons for a Partial Payment or a Denial u Limits u Co Exhausted Pay u Deductible u Timely Filing u Fee Schedule - Hospital or State Specific u Visit Not Related to Liability Accident u Patient under the Influence u Patient being uncooperative
Understanding: Reasons for a Partial Payment or a Denial Limits Exhausted – The policy exhausted the funds available to pay out for the accident. For example, Utah’s PIP is $3, 000. 00 if the patient exceeds this amount then PIP is now exhausted and no other PIP funds are available. Co Pay - A payment made by a the patient or beneficiary in addition to that made by an insurer. Deductible - A specified amount of money that the insured (patient) must pay before an insurance company will pay a claim. Timely Filing - Patients and providers (Hospital & Cardon) must file claims within a qualifying time limit for payment to be considered. If both entities fail to do so, this may lead to a self pay or a hospital write off. Each State has a timely filing parameter, where medical bills and medical records must be submitted under a certain amount of days. Fee Schedules - A list of maximum allowable charges for medical procedures or a list of charges established or agreed to by professionals within the field of medicine. Often also referred to as usual and customary rates (UCR), the fee schedule is often cited by insurance companies who short-pay on medical bills and liens. While insurance companies are allowed to pay according to the fee schedule, hospitals are not required to accept fee schedule payments as payment in full.
Understanding: Reasons for a Partial Payment or a Denial Visit not Related – A bill will be denied if it is determined the injury was not a result of the liability accident. For example if a patient was treated for a pre existing condition as well as the injury they will not pay for the pre existing condition. Patient Under the Influence – Most insurance companies will not pay if the patient was under the influence or breaking the law at the time of the accident. In such cases, Cardon will return the account and let the hospital decide to either bill health or the patient. Patient Uncooperative – If the patient refuses to file a claim or refuses to work with the Hospital/Cardon, we have no choice but return the account as self pay. If the patient refuses to work with the insurance, they will deny the bill which will also result in a self pay bill. No Coverage Available – If the patient released the incorrect insurance information and the bill was submitted, the insurance may deny the bill due to no coverage being available.
How do you know? How do you know what is pending in regards to the bill? How do you know if the bill was denied? How do you know if it was paid in full?
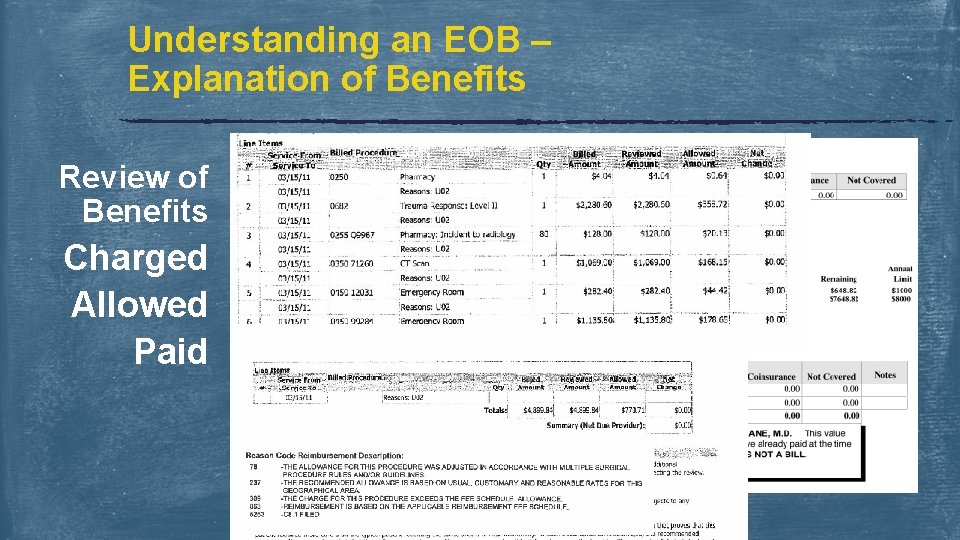
Understanding an EOB – Explanation of Benefits Review of Benefits Charged Allowed Paid
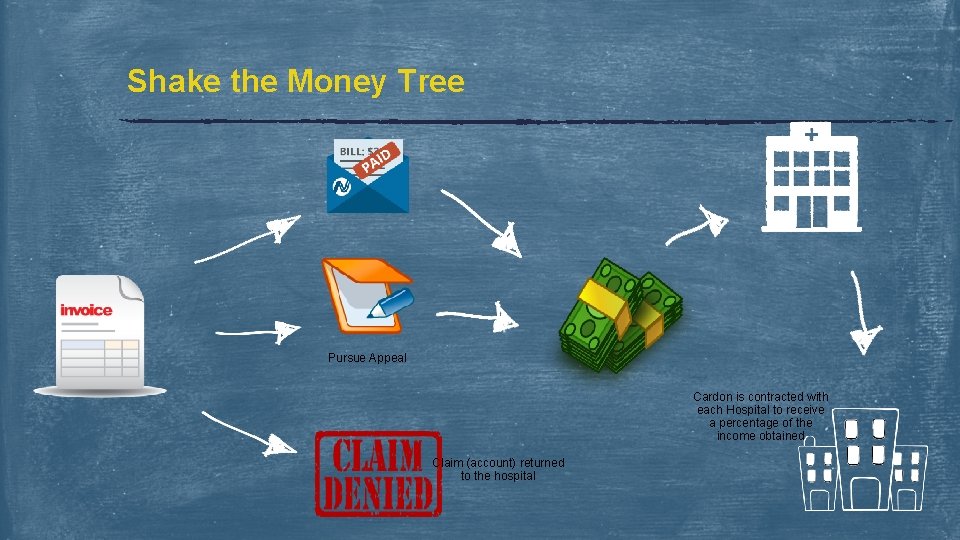
Shake the Money Tree Pursue Appeal Cardon is contracted with each Hospital to receive a percentage of the income obtained Claim (account) returned to the hospital
Don’t Forget about the most Important thing… HIPAA Protect PHI • • • Don’t share unnecessary information Don’t leave documents unattended Shred documents rather than throwing them away Keep Digital Information Secure • Don’t transmit PHI on unsecured devices • Don’t share log-ins • Remove PHI from hard drive once stored in MPower • • Follow Company Protocol Lock your computer when not in use Communications should be scanned into MPower
Additional Negotiating Tactics u If you do not understand the EOB or Denial, it is always best to call the adjustor u Don’t be afraid to ask questions and get clarification u Be sure you clearly understand the adjustor before discontinuing the phone call u Remember to escalate any issues to your supervisor u Always be respect and professional u Employees are always representing Cardon and the Hospital Please help me understand the following denial?
Documenting Your Work Notes for the account should be entered in MPower • Phone calls should be noted – who, when, outcome • Documentation received should be scanned into Mpower • Deadlines discussed and understood
Your Contribution to our Success Critical Thinking Review QA Deadlines Best course of action for success Evaluate $ eal Is app d? e justifi g issin No m rwork pape Language Accuracy Terminology Your accuracy & knowledge effects the process…
Goals & Expectations Urgency Attendance Competency Meet Expectations Accountability Accuracy
Questions ?
- Slides: 19