Introduction to SOS The SequentialOralSensory Approach to Feeding

- Slides: 17
Introduction to “SOS” The Sequential-Oral-Sensory Approach to Feeding Miranda Macaulay Community SLT
About “SOS” Developed by Dr Kay Toomey – Paediatric Psychologist, STAR centre, Denver Course also led by Dr Erin Ross SLT Programme to support “problem feeders” not picky eaters ie significant and persistent feeding difficulties. NB. “red flags” • Foods lost are not re-acquired • Extreme stress with new foods • Refuses entire categories of textures/food groups • Has a diet different from their family • * The SOS Approach to Feeding is a copyrighted program that requires therapists to attend specialized training conducted by Dr. Kay Toomey
Principles • Eating is the most complex sensory activity we do • Underlying reason for every behaviour • Systematic desensitization is best first approach to treatment • Using typical development as a guide • Specific skills need to be taught/best taught using food • Child in control: confidence and competence • Importance of postural stability 90: 90 We learn through experience and reinforcement
Learning about Food • Operant conditioning v classical conditioning • Need to introduce new foods over and over WITH positive reinforcement • Typical children take up to 10 times of being offered a food with positive reinforcement to accept the food • Children with eating & drinking difficulties will take longer The child needs to re-learn about food!

“Family meals” goals • • • Increase volume of preferred foods To learn mealtime routine and cues to eating Increase exposure to non-preferred foods Model good feeding behaviours Talk about food in positive way Model oral-motor movements Use “learning plate” if cannot tolerate food on plate Clear signals beginning/end of meal Limit mealtimes Family meals v therapy meals
“Family meals” goals contd. • • Prevent “food jags” by rotating menus, changing appearance of foods slightly Use plain placemat/plate Throw or blow food into bin at end of meal Allow to taste and spit out Offer easiest foods at most challenging time of day, hardest foods at best time Avoid rewarding food with food Praise any adaptive food behaviour and praise siblings’ eating
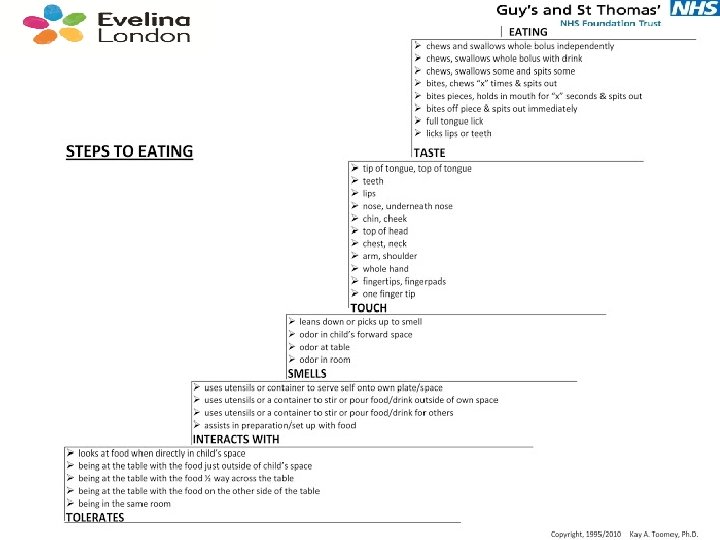
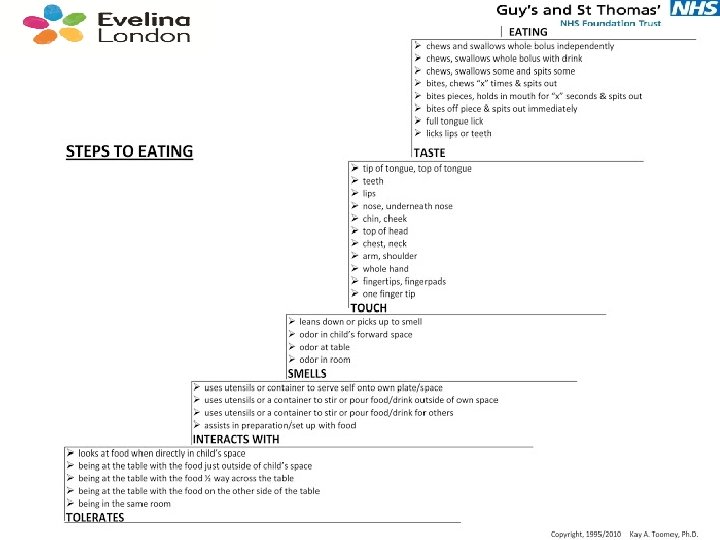
“Therapy meals” goals • Increase experience with wide number of foods • Movement up the “steps to eating” hierarchy • Teach new skills eg chewing using graded stimuli • Sensory preparation for optimum arousal • Each step paired with positive atmosphere (play/fun) • Peer reinforcement close to child’s level • Teaching about properties of food and making links between preferred and non-preferred foods • Child is in control
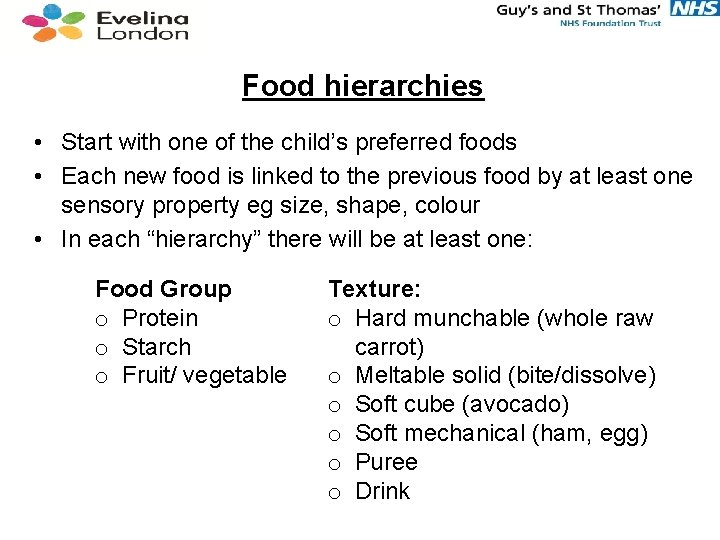
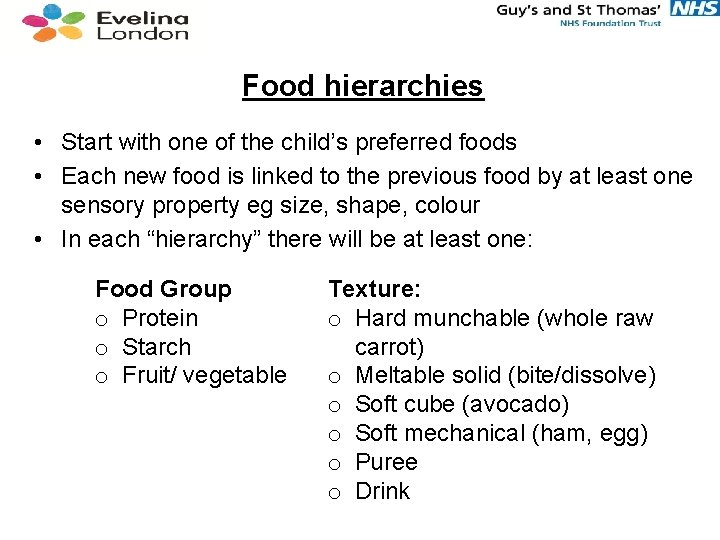
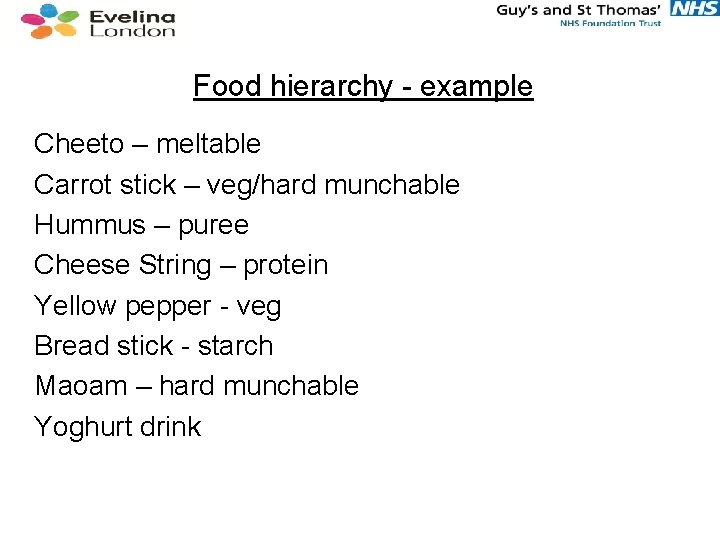
Food hierarchies • Start with one of the child’s preferred foods • Each new food is linked to the previous food by at least one sensory property eg size, shape, colour • In each “hierarchy” there will be at least one: Food Group o Protein o Starch o Fruit/ vegetable Texture: o Hard munchable (whole raw carrot) o Meltable solid (bite/dissolve) o Soft cube (avocado) o Soft mechanical (ham, egg) o Puree o Drink
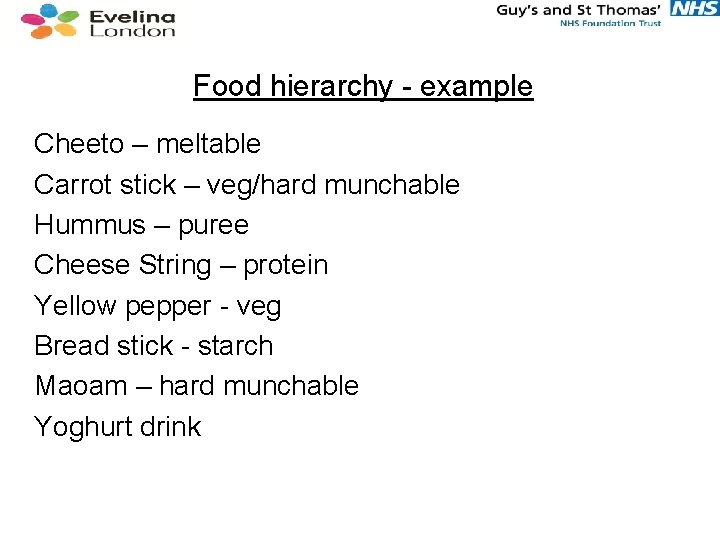
Food hierarchy - example Cheeto – meltable Carrot stick – veg/hard munchable Hummus – puree Cheese String – protein Yellow pepper - veg Bread stick - starch Maoam – hard munchable Yoghurt drink
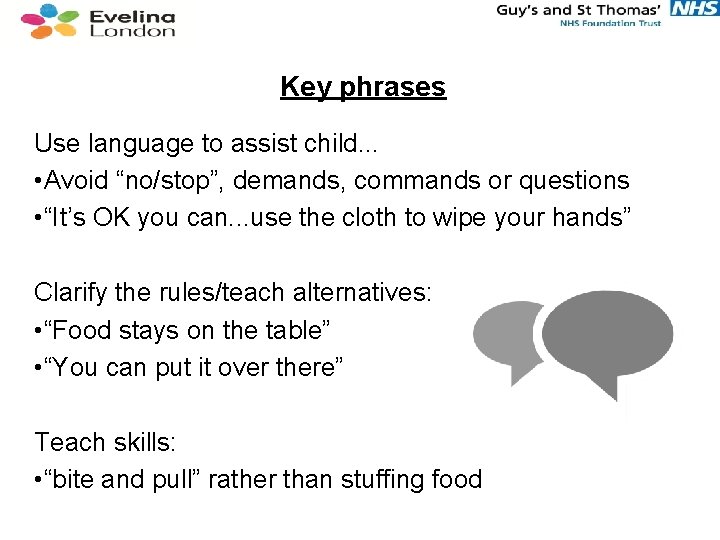
Key phrases Use language to assist child. . . • Avoid “no/stop”, demands, commands or questions • “It’s OK you can. . . use the cloth to wipe your hands” Clarify the rules/teach alternatives: • “Food stays on the table” • “You can put it over there” Teach skills: • “bite and pull” rather than stuffing food
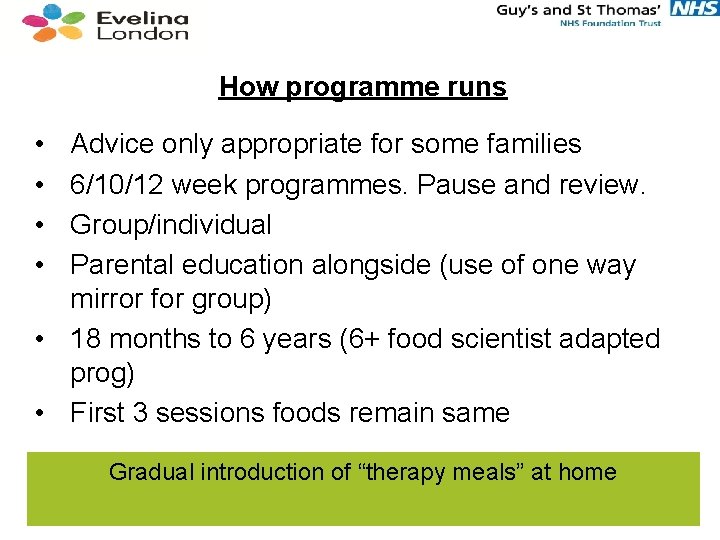
How programme runs • • Advice only appropriate for some families 6/10/12 week programmes. Pause and review. Group/individual Parental education alongside (use of one way mirror for group) • 18 months to 6 years (6+ food scientist adapted prog) • First 3 sessions foods remain same Gradual introduction of “therapy meals” at home
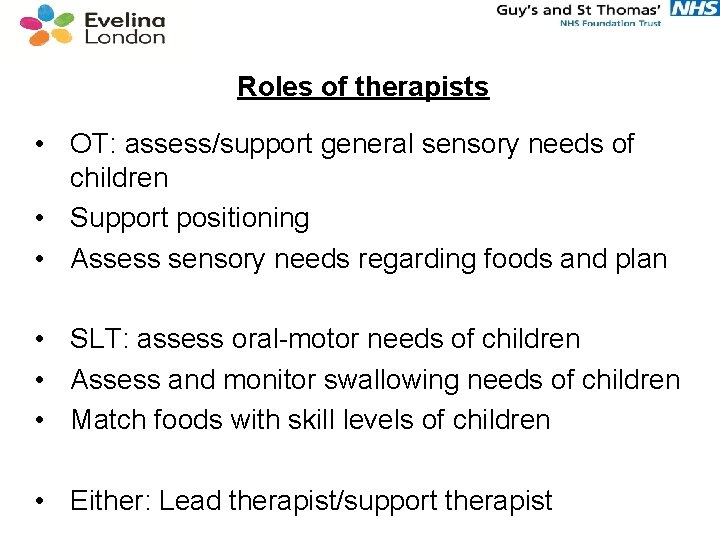
Roles of therapists • OT: assess/support general sensory needs of children • Support positioning • Assess sensory needs regarding foods and plan • SLT: assess oral-motor needs of children • Assess and monitor swallowing needs of children • Match foods with skill levels of children • Either: Lead therapist/support therapist
Structure of sessions • • • Sensory prep: obstacle course Transition to “food school” Separate from parent Blow bubbles (breathing/calming) Wash and dry hands/face Therapist models interaction with a food item Foods are offered 1 by 1 to child in plain bag (approx 10) If anxiety increases, therapist drops back to lower level Clean up at end and throw or blow food into bin
Outcome measures • Weights/heights pre/post • Food diaries • Steps to eating hierarchy Local outcome measures: • COPM (Canadian Occupational Performance Outcome Measure)
Evidence Toomey and Ross 2011 • Average weight gain 1 pound • Height gain approx 1 inch (normal growth factored out) • Average increase in calorie intake 100 calories/day Kim Boyd 2007 • N: 37 mix of aetiologies mean age 37 months • Increase in variety of different foods eaten from mean of 19 to 27 Peterson, Piazza & Volkert (2016) RCT ABA v SOS
Local context • • Children assessed in MDT Feeding Clinic Outreach visit to home or nursery Family mealtimes advice Identified children invited to 5 week block of SOS led by OT/SLT • Parent session at start/end