INTRODUCTION TO Pathophysiology Mechanisms of Disease Diagnosis Treatment


- Slides: 26
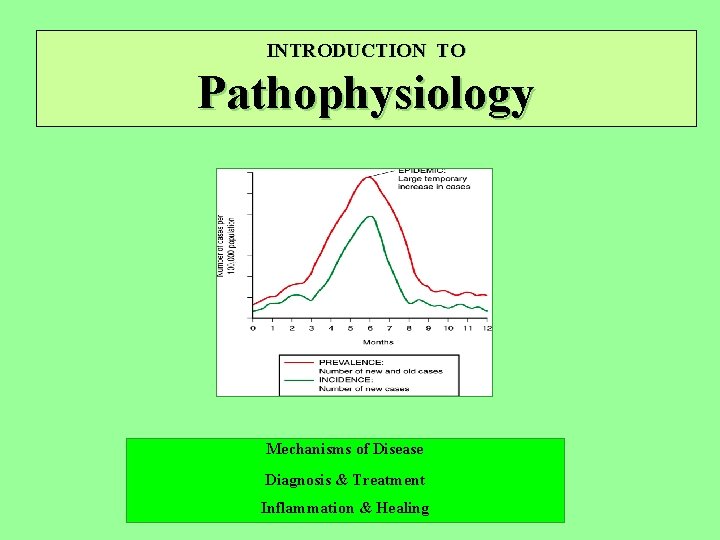
INTRODUCTION TO Pathophysiology Mechanisms of Disease Diagnosis & Treatment Inflammation & Healing
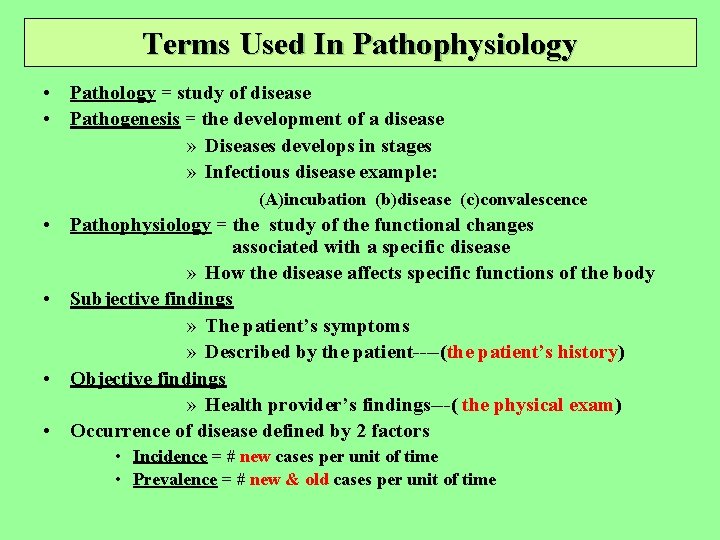
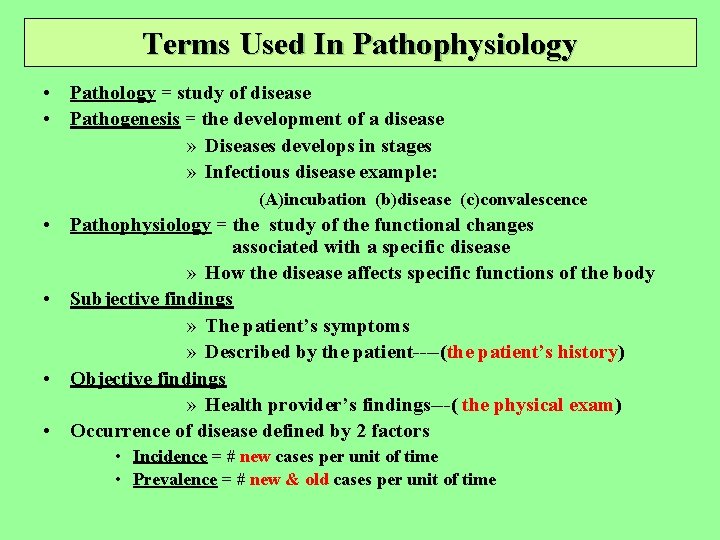
Terms Used In Pathophysiology • Pathology = study of disease • Pathogenesis = the development of a disease » Diseases develops in stages » Infectious disease example: (A)incubation (b)disease (c)convalescence • Pathophysiology = the study of the functional changes associated with a specific disease » How the disease affects specific functions of the body • Subjective findings » The patient’s symptoms » Described by the patient----(the patient’s history) • Objective findings » Health provider’s findings---( the physical exam) • Occurrence of disease defined by 2 factors • Incidence = # new cases per unit of time • Prevalence = # new & old cases per unit of time

• Disease terminology – – – – Etiology = cause of the disease Idiopathic = disease with unknown cause Iatrogenic = disease caused by human intervention Congenital diseases = diseases occurring at birth Syndrome = common cause of different signs & symptoms Remission = period when symptoms & signs of disease abates Exacerbation = period when symptoms & signs increase Endemic disease = disease native to local area Epidemic = many people affected in a given area Pandemic = many people affected in large areas Incubation = latent period of the disease before develop signs & symptoms Prognosis = probability for recovery Morbidity = disease rates within a group Mortality = death rates within a group Epidemiology = how the disease occurs & spreads through an area
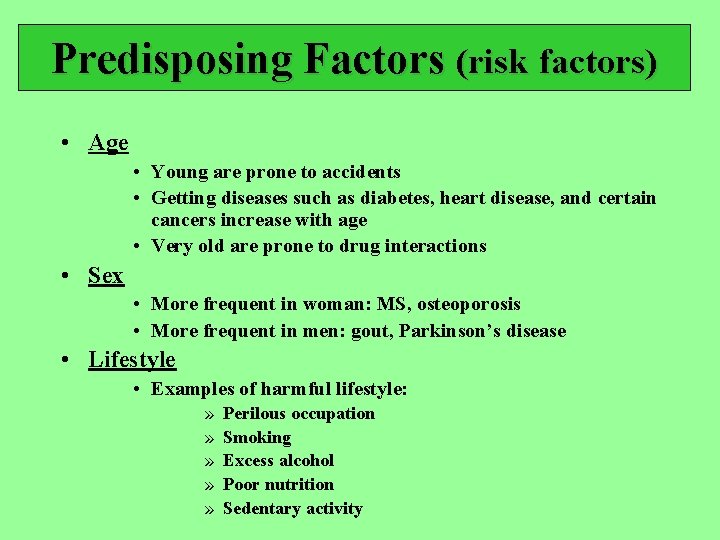
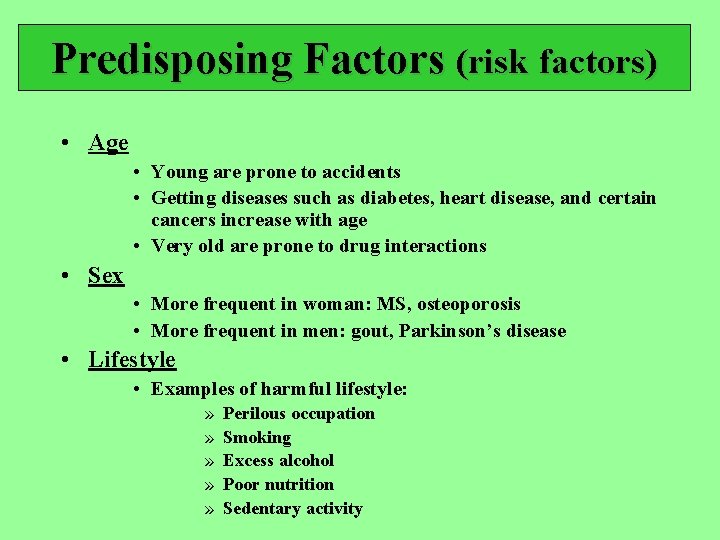
Predisposing Factors (risk factors) • Age • Young are prone to accidents • Getting diseases such as diabetes, heart disease, and certain cancers increase with age • Very old are prone to drug interactions • Sex • More frequent in woman: MS, osteoporosis • More frequent in men: gout, Parkinson’s disease • Lifestyle • Examples of harmful lifestyle: » » » Perilous occupation Smoking Excess alcohol Poor nutrition Sedentary activity
• Environment • • • Air pollution Water pollution Poor living conditions Excessive noise Chronic psychological stress • Heredity • Deals with genetic predisposition (inheritance) » Genetic predisposition + certain type of environment = mental retardation , lung cancer, etc. • Preventive health care • The best treatment of a disease is prevention !! • Deals with altering risk factors that can be changed
• Homeostasis & disease – Disease is the failure to maintain homeostatic conditions • Disease mechanisms – – – – Genetic = mutated or abnormal genes Pathogens (microscopic organisms) Loss of control mechanisms (e. G. Diabetes, immune problems) Degenerative changes (normal aging) Environmental hazards (trauma, chemicals) Nutritional factors Tumors (benign & malignant)
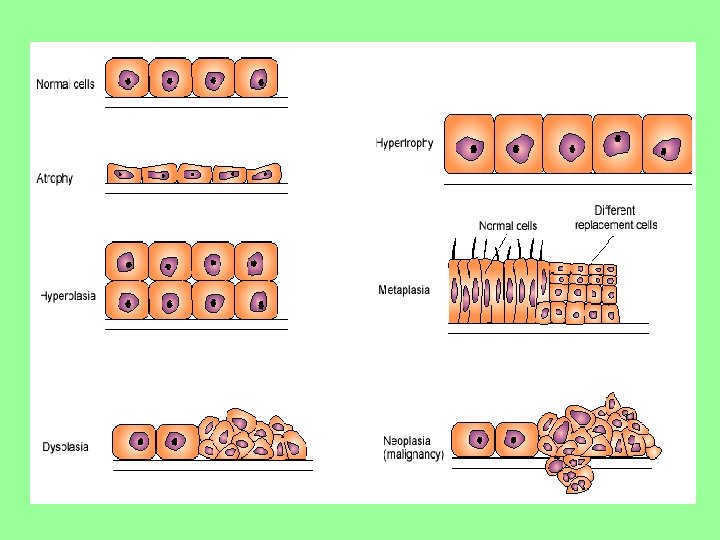
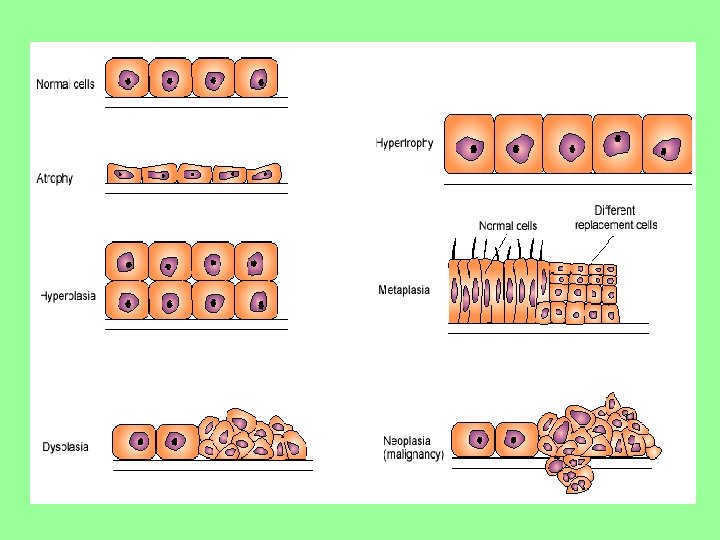
The Cell & Disease Changes in Growth • Changes in size of individual cell – Atrophy = decrease in cell size – Hypertrophy = increase in cell size • Changes in actual number of cells – Hyperplasia, Dysplasia, & Anaplasia = increase in rate of reproduction – Hyperplasia = increase in number of normal cells – Dysplasia = increase in number of atypical cells – Anaplasia = increase in number of frankly abnormal cells Change in Type of Cell • Change of one type of cell into another type (metamorphoses) – Metaplasia =change to different mature cell type
• Cell damage is the main reason to lose homeostasis – Deficiency of oxygen (hypoxia) = most common reason • Mechanism of progression: ischemia -to- necrosis -to- gangrene • Cell death – Once it occurs, lysis occurs with release of lysosomal enzymes • This causes inflammation • After inflammation, the dead cells(tissue) is either: • Replaced by scar tissue • Regenerated to resemble original tissue
Diagnosis & Treatment • “SOAP” protocol: “S” = subjective • “O” = objective “A” = assessment “P” = plan Subjective Findings = the patient’s symptoms • Obtained by taking a medical history – includes: » Chief complaint (cc) » present illness (PI) » past history (PH) ------- med/ surg/ allergies/ lifestyles » family history (FH) » review of systems (ROS) • Objective Findings = the patient’s physical manifestations • Obtained by doing a physical exam – – Begins with opening statement (WD/WN/WW) Then vita signs ------ T, P, BP, RR, Pain go from head to toes! Includes techniques of: » inspection » auscultation » palpation » percussion
• Assessment = arriving at a diagnosis – Differential diagnoses • Includes all possibilities – Lab • Basically a study of body fluids – Diagnostic tests • Imaging » X-ray, US, CAT, MRI, isotope scans • Endoscopies • Biopsies • Skin tests • Plan = all possible treatments with associated complications & prognoses • Includes a “Treatment Plan” – individualize – modalities available: » do nothing (primun nocere) » Talk (counseling) » Medication » Surgery • Includes a Prognosis
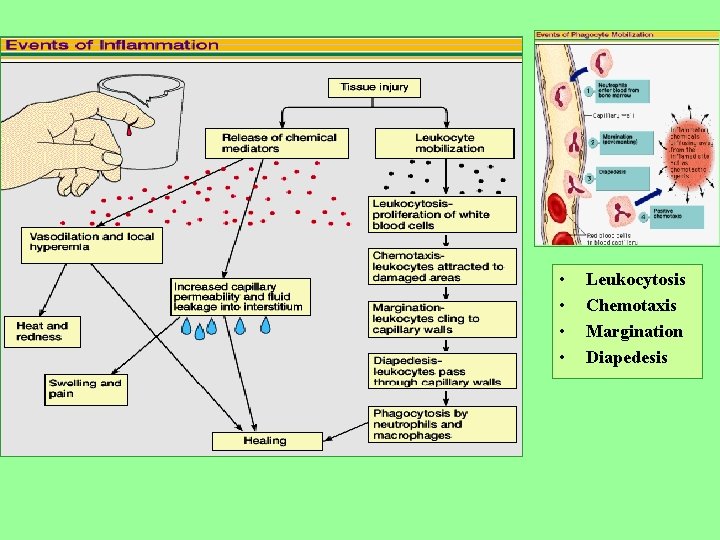
The Inflammatory Response • Key purposes = DEFENSE 1. 2. 3. • To hunt & kill invaders To limit their spread To prepare tissue for repair Key events 1. 2. 3. Increase of vascular permeability Recruitment (margination) & emigration (diapedesis) of WBC’s Phagocytosis
The Inflammatory Response • Inflammatory response = normal body defense mechanism to tissue injury » Note: Inflammation is NOT infection • Cells of the inflammatory response when get tissue injury – Main groups; • Phagocytes --- “the eaters” – Macrophages --- become active as APC’s (antigen presenting cell) – Neutrophils --- “little eaters” – Monocytes --- become tissue macrophages • T- lymphocytes (helper-T) ---- produce cytokines which “ call to action” • Platelets ---- release PAF (platelet activating factor) which in turn begins call to action and release of chemical mediators • Mast cells --- release chemical mediators that begin inflammation
Chemical Mediators • The initial “macrophage (APC cell) – antigen complex” causes chemical mediators to be released: – Histamine • From basophils & mast cells • Cause vasodilation & increased permeability of vessels via release of nitric oxide – Prostaglandins • Made in mast cell membrane from fatty acid (arachidonic) • Cause pain & vasodilation – Leukotrienes • “bad” prostaglandins since cause symptoms of inflammation (pain & swelling) • Cause chemotaxis • Very important for causing allergies, asthma, & anaphylaxis
Chemical Mediators – Complement • Coats bacterial surface; enhances phagocytosis & lyses bacteria • Inactive plasma proteins become activated by initial An-Ab complex – Interferon • Proteins that are released by helper T’s & kill viruses – Bradykinins • From inactivated plasma protein • Cause similar effects like histamine • Cause pain • Induce WBC’s into area (chemotaxis
• Local effects of inflammation – 4 cardinal signs of inflammation • Redness (rubor) – from increased blood supply • Heat (calor) – from increased blood supply • Swelling (tumor) – from increased permeability & increased proteins in interstitial fluid • Pain (dolar) – from chemical mediators – Also get inflammatory exudate • Serous – from allergic reactions & burns • Purulent – from infections – May lead to abscess • Systemic effects of inflammation – – General malaise Fatigue Headache Fever • Caused by pyrogens (chemicals released from phagocytes) • Beneficial – Inhibits growth of pathogens – Enhances repair process via increased metabolic rate
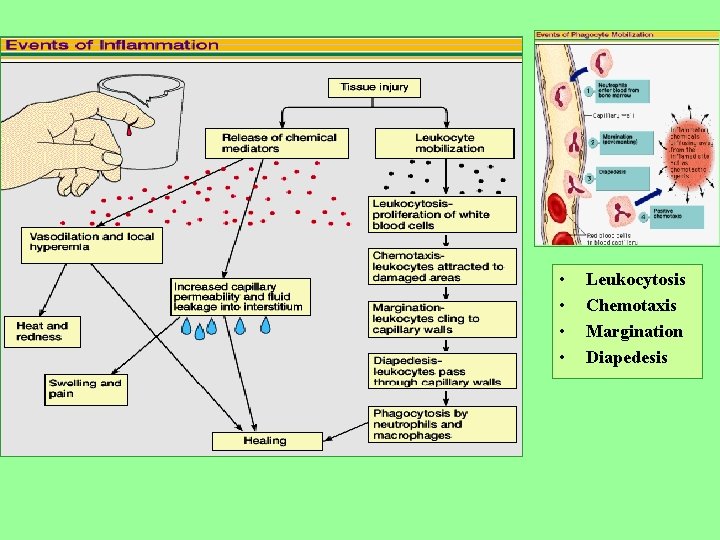
• • Leukocytosis Chemotaxis Margination Diapedesis
• Potential complications of inflammation • Infection • Ulceration – from chronic inflammation – May lead to: » perforation of viscera » excess scar formation • Skeletal muscle spasm • Local tissue reactive changes – Joints from decreased ROM become stiff – Lungs cannot exchange gases • Diagnostic tests for inflammation • • Leukocytosis Differential WBC count ESR Cell enzymes – may or may not be tissue specific – C-reactive protein
• Chronic Inflammation – The acute inflammatory reaction usually subsides within 48 – 72 hours as long as the cause is removed (e. g. touching a hot stove) – If the cause persists, you get chronic inflammation – Clinically: • Increase in connective tissue reaction to the chronicity – Get more fibroblasts & more collagen » Thus get more scar tissue » Can get granulomas (collection of chronically inflamed tissue) • Treatment of inflammation • • • Aspirin NSAID’s Glucocorticoids Heat & cold Physiotherapy if chronic » Prevents contractures
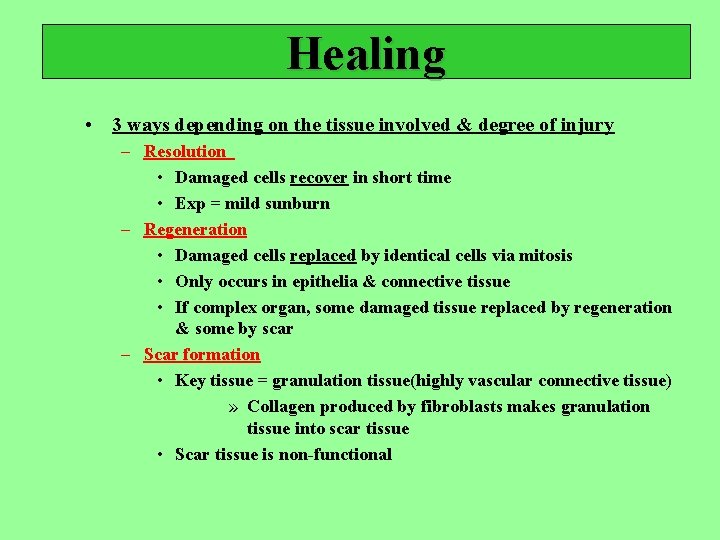
Healing • 3 ways depending on the tissue involved & degree of injury – Resolution • Damaged cells recover in short time • Exp = mild sunburn – Regeneration • Damaged cells replaced by identical cells via mitosis • Only occurs in epithelia & connective tissue • If complex organ, some damaged tissue replaced by regeneration & some by scar – Scar formation • Key tissue = granulation tissue(highly vascular connective tissue) » Collagen produced by fibroblasts makes granulation tissue into scar tissue • Scar tissue is non-functional
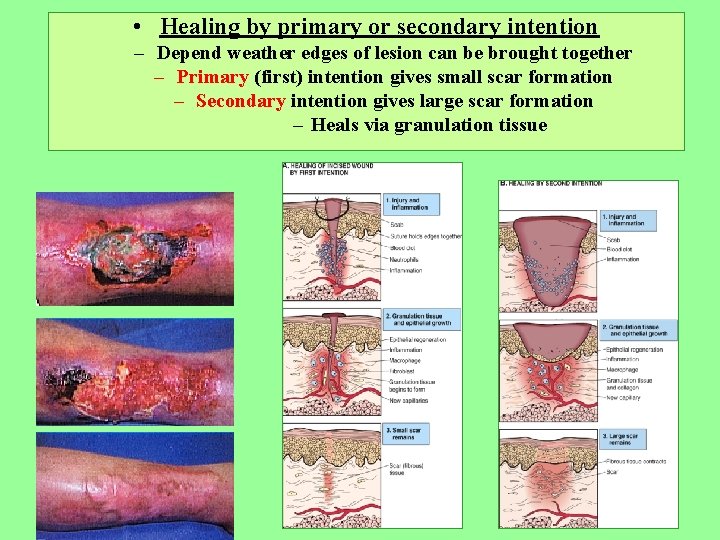
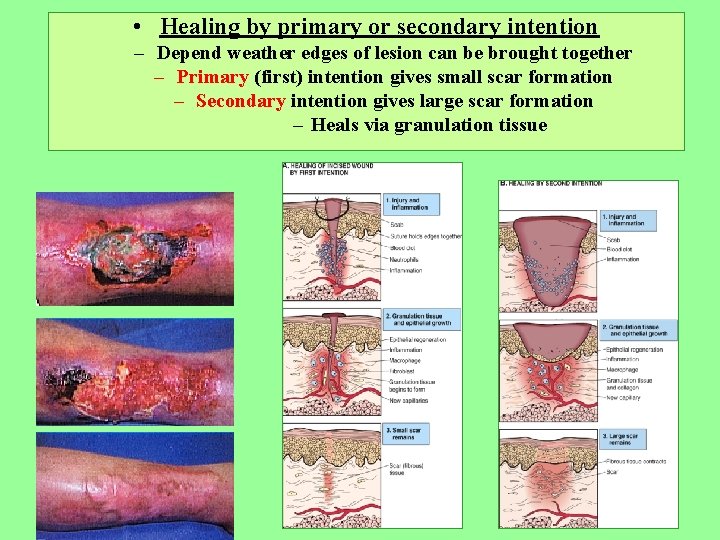
• Healing by primary or secondary intention – Depend weather edges of lesion can be brought together – Primary (first) intention gives small scar formation – Secondary intention gives large scar formation – Heals via granulation tissue
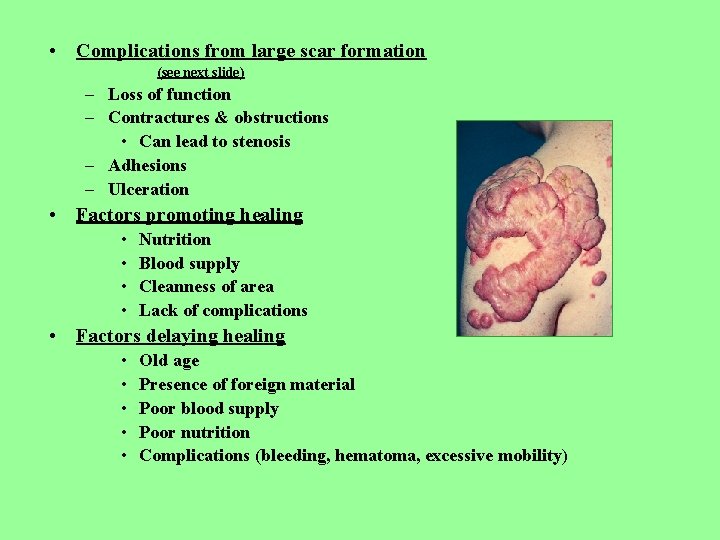
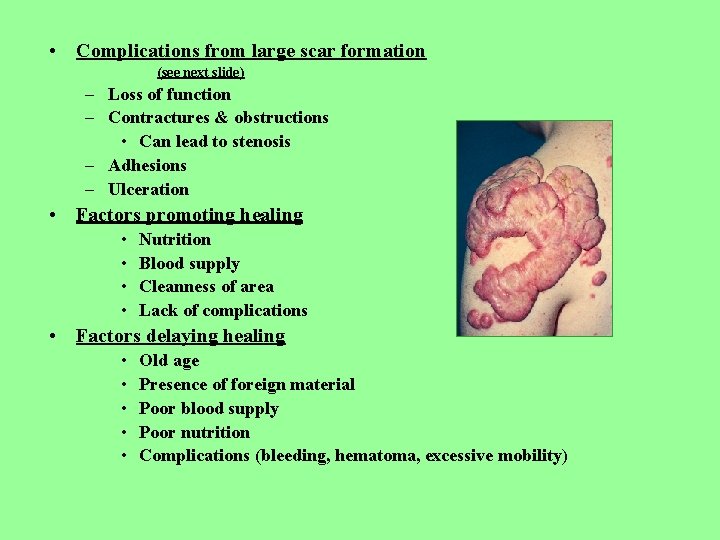
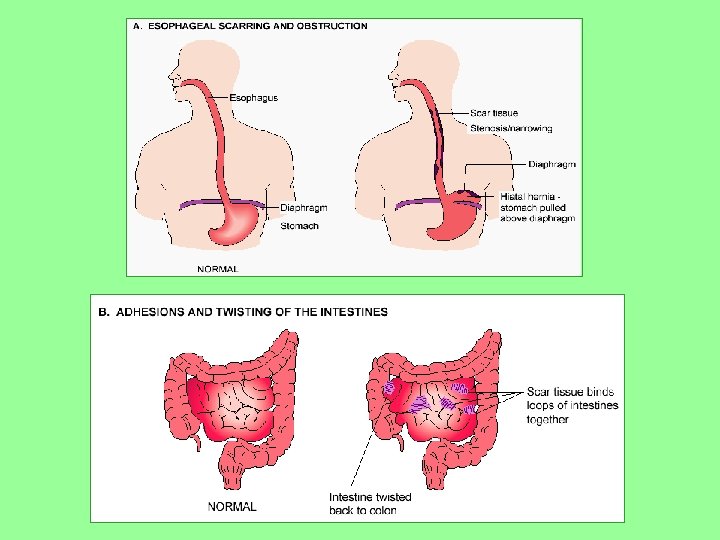
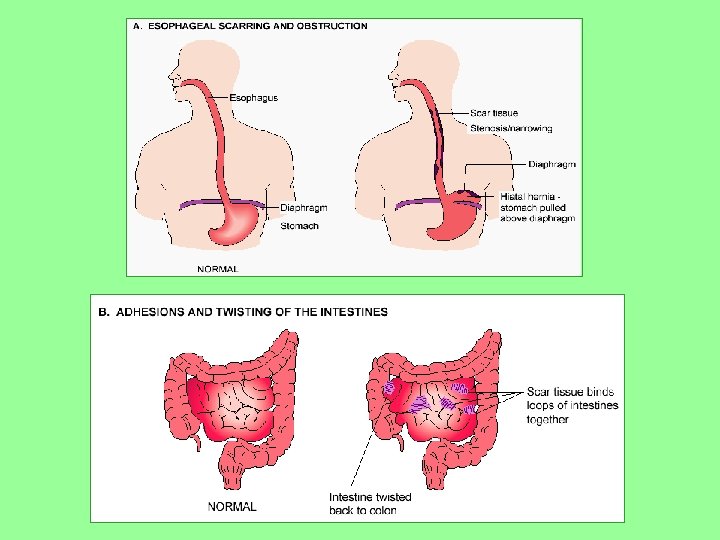
• Complications from large scar formation (see next slide) – Loss of function – Contractures & obstructions • Can lead to stenosis – Adhesions – Ulceration • Factors promoting healing • • Nutrition Blood supply Cleanness of area Lack of complications • Factors delaying healing • • • Old age Presence of foreign material Poor blood supply Poor nutrition Complications (bleeding, hematoma, excessive mobility)
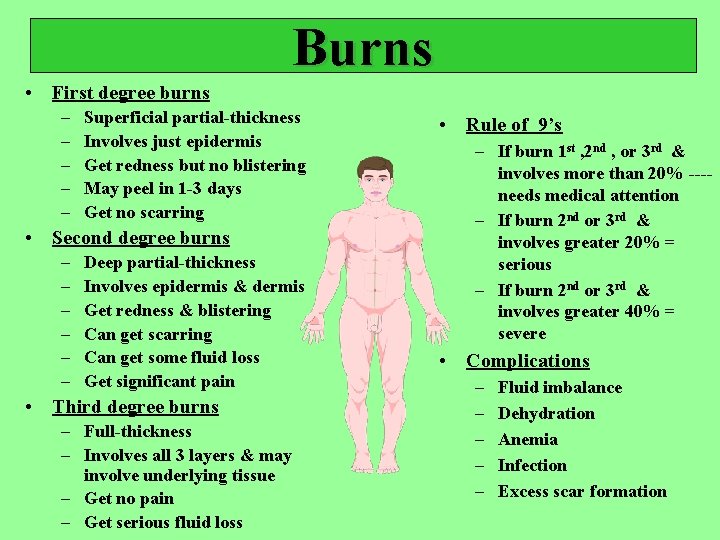
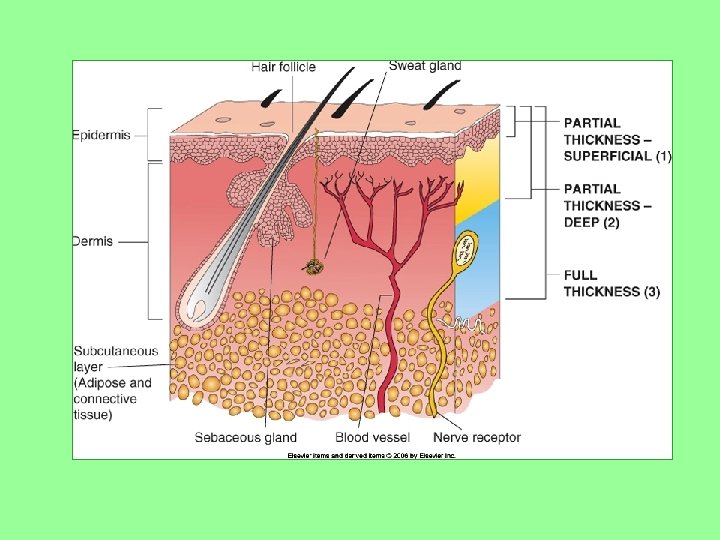
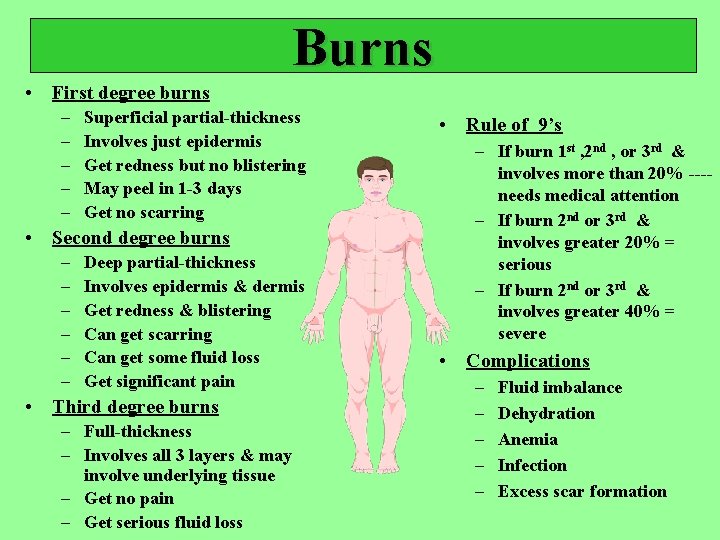
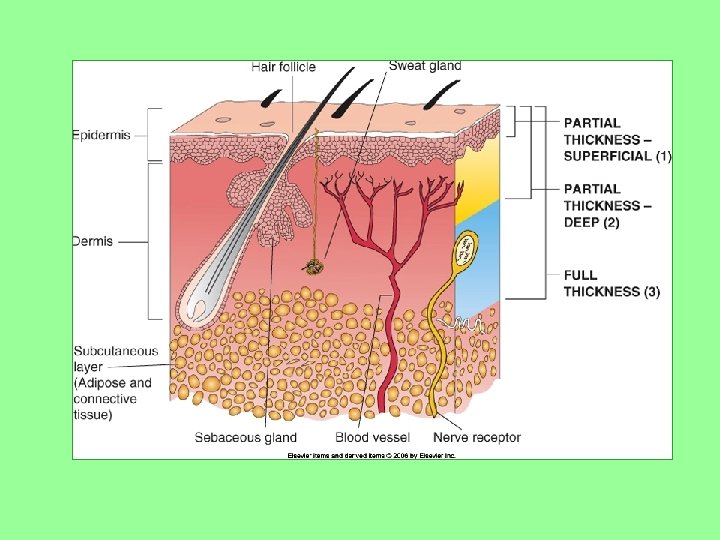
Burns • First degree burns – – – Superficial partial-thickness Involves just epidermis Get redness but no blistering May peel in 1 -3 days Get no scarring • Second degree burns – – – Deep partial-thickness Involves epidermis & dermis Get redness & blistering Can get scarring Can get some fluid loss Get significant pain • Third degree burns – Full-thickness – Involves all 3 layers & may involve underlying tissue – Get no pain – Get serious fluid loss • Rule of 9’s – If burn 1 st , 2 nd , or 3 rd & involves more than 20% ---needs medical attention – If burn 2 nd or 3 rd & involves greater 20% = serious – If burn 2 nd or 3 rd & involves greater 40% = severe • Complications – – – Fluid imbalance Dehydration Anemia Infection Excess scar formation