Introduction to mussels Human Anatomy Physiology I Dr















- Slides: 66
Introduction to mussels Human Anatomy & Physiology I Dr. Rivera
Functions of muscle tissue • Producing body movements • Stabilizing body positions • Storing and moving substances within the body • Generating heat (thermogenesis)

Prime function of muscles • Changing chemical energy into mechanical energy to generate force, perform work, and produce movement.
Properties of muscles • Electrical excitability • Contractility – Isometric vs. Isotonic • Extensibility • Elasticity
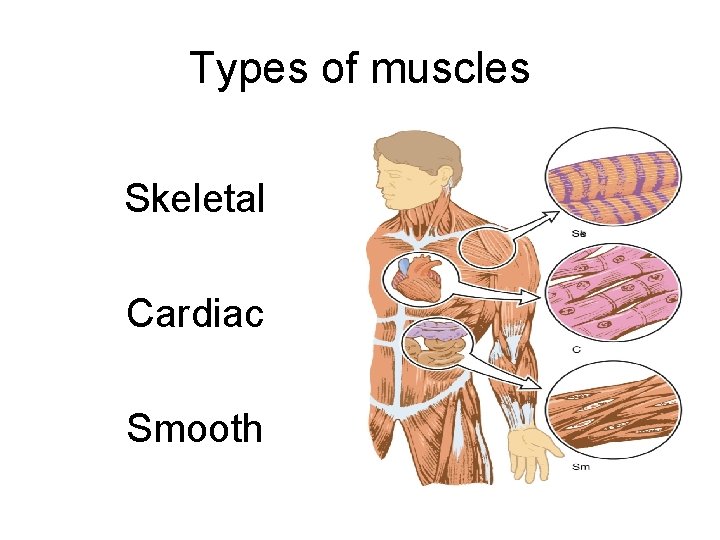
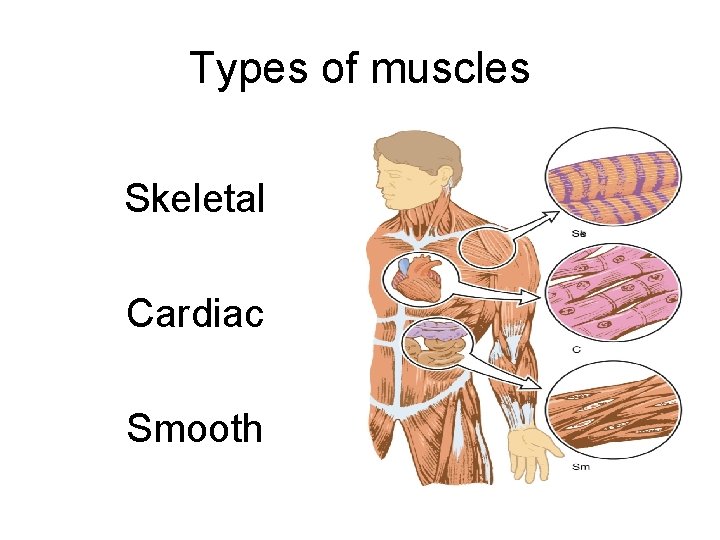
Types of muscles Skeletal Cardiac Smooth
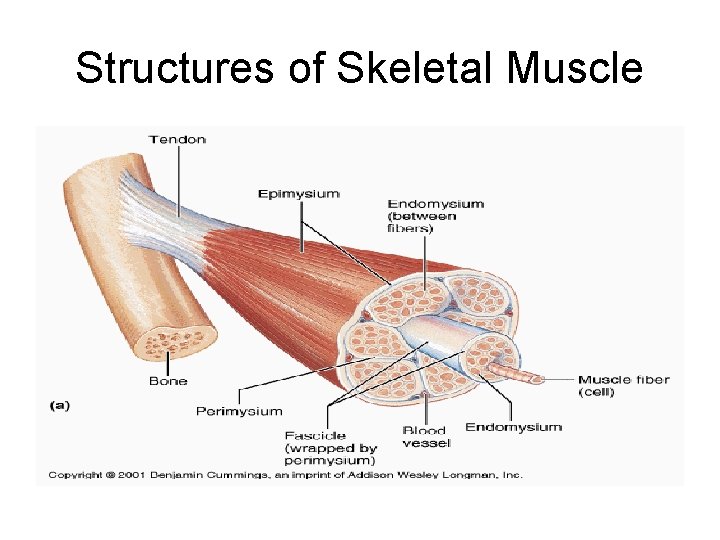
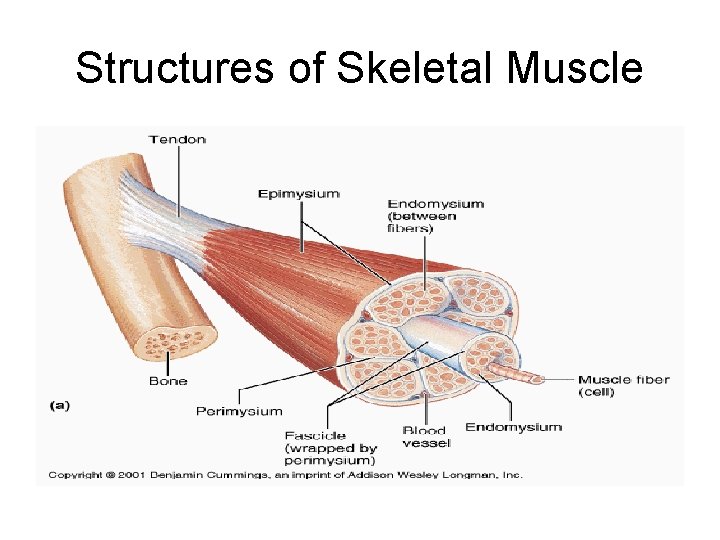
Structures of Skeletal Muscle
Connective tissue components • Fascia (bandage): a sheet or broad band of connective tissue that supports and surrounds muscles and other organs in the body. • 2 types of fascia: – Superficial fascia – Deep fascia
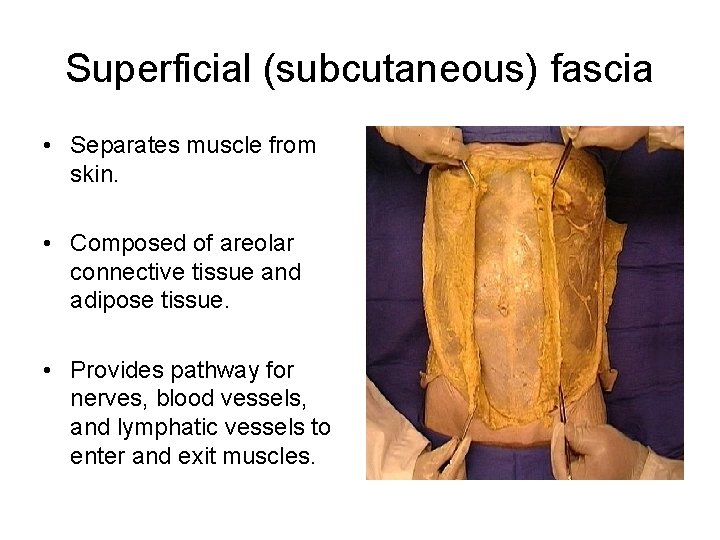
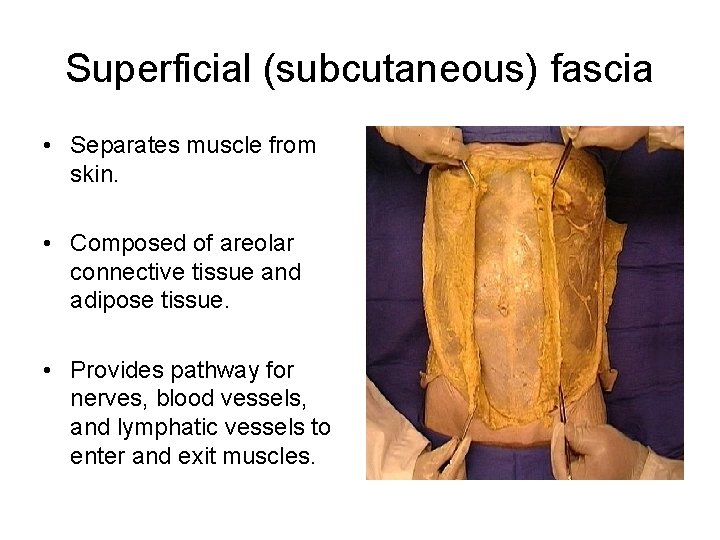
Superficial (subcutaneous) fascia • Separates muscle from skin. • Composed of areolar connective tissue and adipose tissue. • Provides pathway for nerves, blood vessels, and lymphatic vessels to enter and exit muscles.
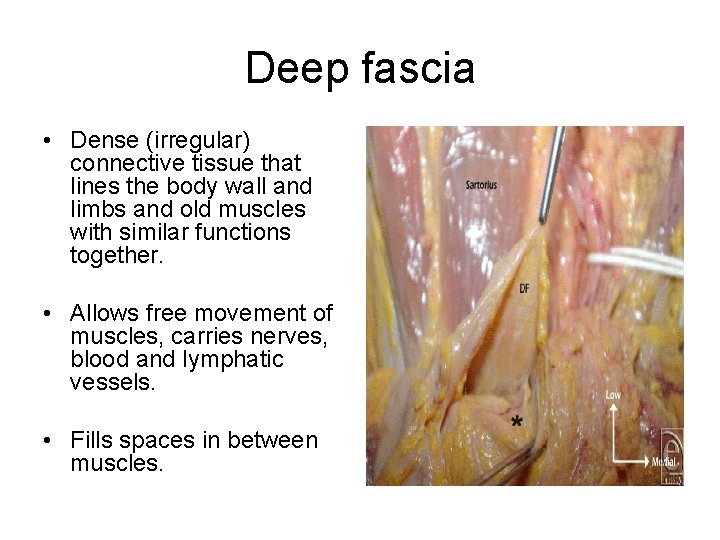
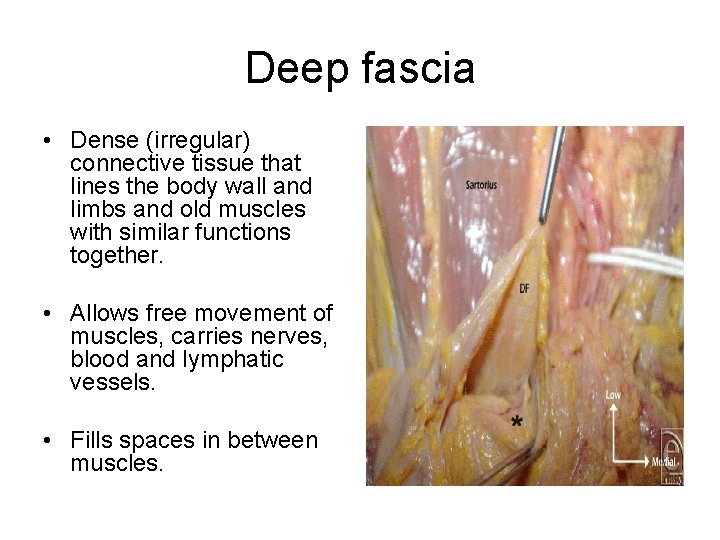
Deep fascia • Dense (irregular) connective tissue that lines the body wall and limbs and old muscles with similar functions together. • Allows free movement of muscles, carries nerves, blood and lymphatic vessels. • Fills spaces in between muscles.
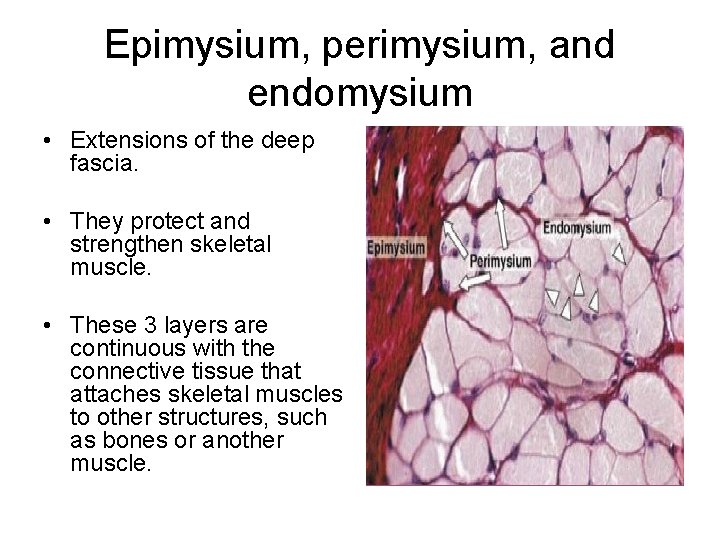
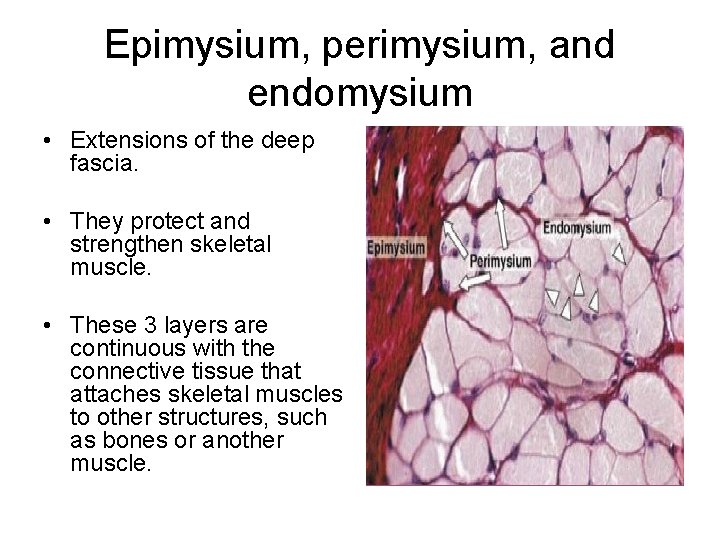
Epimysium, perimysium, and endomysium • Extensions of the deep fascia. • They protect and strengthen skeletal muscle. • These 3 layers are continuous with the connective tissue that attaches skeletal muscles to other structures, such as bones or another muscle.
Just because is fun … • All three connective tissue layers may extend beyond the muscle fibers to form a tendon – a cord of dense c. t. that attaches muscles to the periosteum of a bone. • Epimysium (epi: upon) is the outermost layer. • Perimysium (peri: around) surrounds groups of 10 to 100 or more individuals fibers, separating them into bundles known as fascicles. • Endomysium (endo: within) separates individual muscle fibers or cells.
Naming muscles • Location • Shape • Action • Number of origins • Size • Direction of fibers
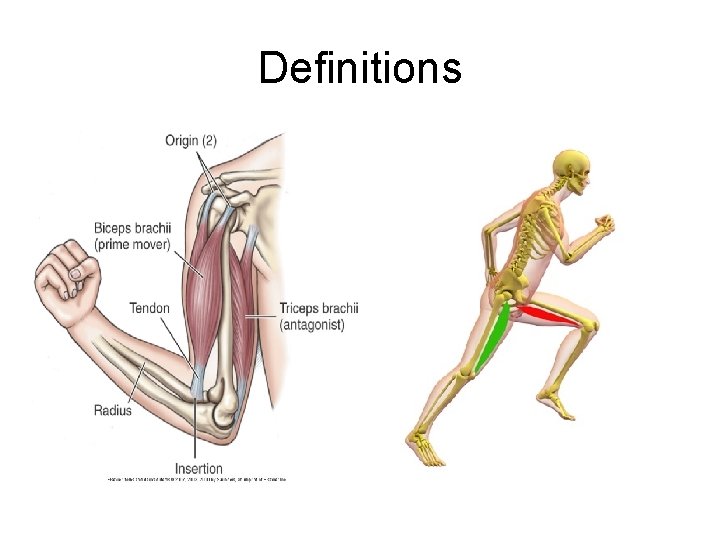
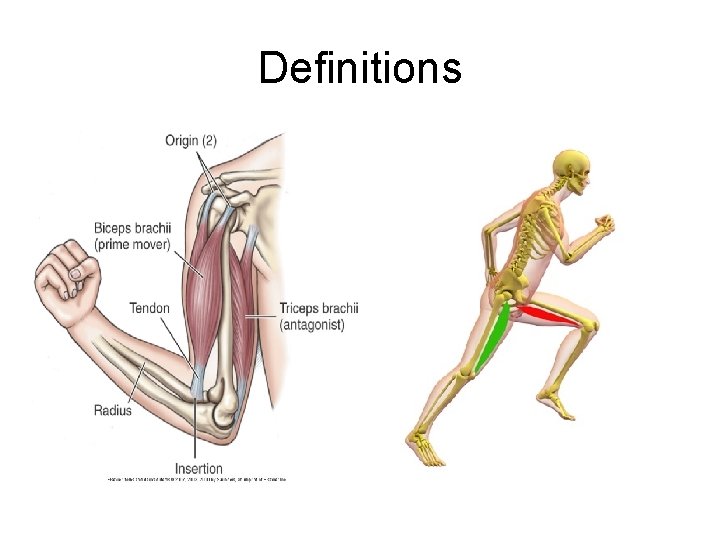
Definitions
Body movements • Flexion/Extension • Abduction/Adduction • Pronation/Supination • Elevation/Depression • Rotation/Circumduction • Dorsiflexion/plantar • Inversion/Eversion • Protraction/Retraction
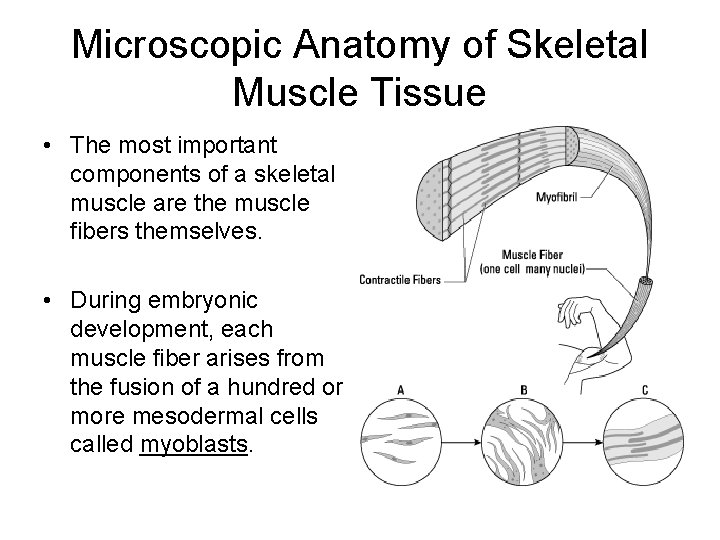
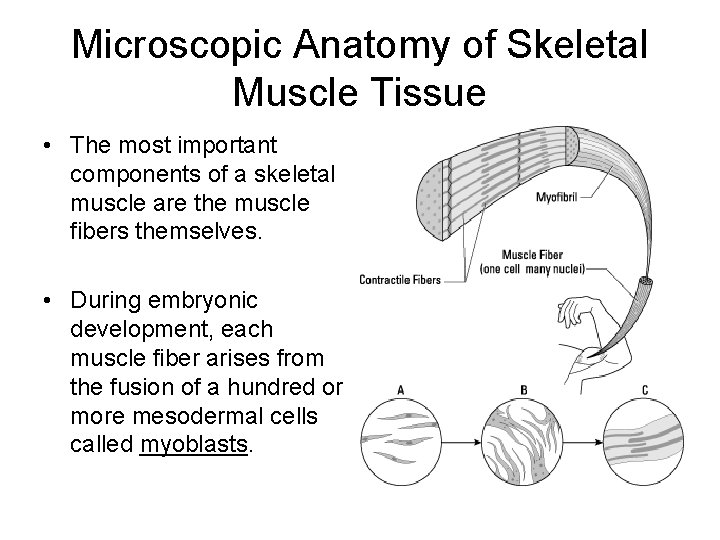
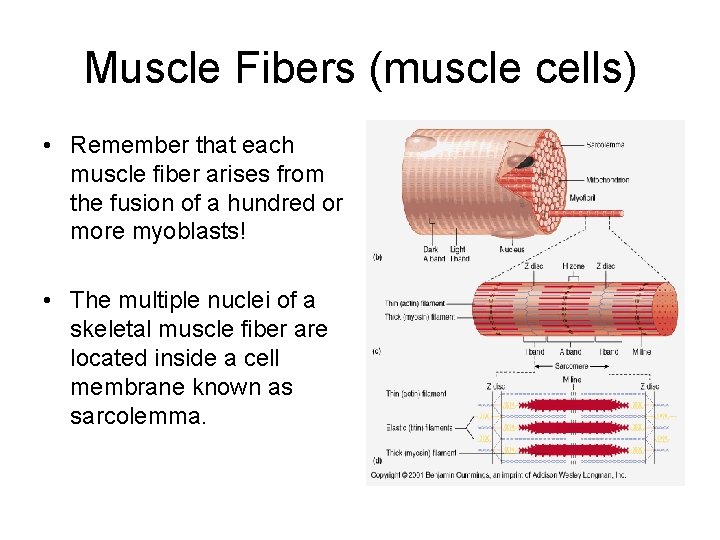
Microscopic Anatomy of Skeletal Muscle Tissue • The most important components of a skeletal muscle are the muscle fibers themselves. • During embryonic development, each muscle fiber arises from the fusion of a hundred or more mesodermal cells called myoblasts.
Microscopic Anatomy (cont. ) • Hence, each muscle fiber has a hundred or more nuclei. • Once fusion has occurred, the muscle fiber loses its ability to undergo mitosis. • Thus, the number of skeletal muscle fibers is set before birth, and most of these cells last a lifetime.
F. Y. I. • The drastic muscle growth that occurs after birth occurs mainly by enlargement of existing muscle fibers. • During childhood, human growth hormone and other hormones stimulate an increase in the size of skeletal muscle fibers. • The hormone testosterone (from the testes in males and other tissues in females) promotes further enlargement of muscle fibers.
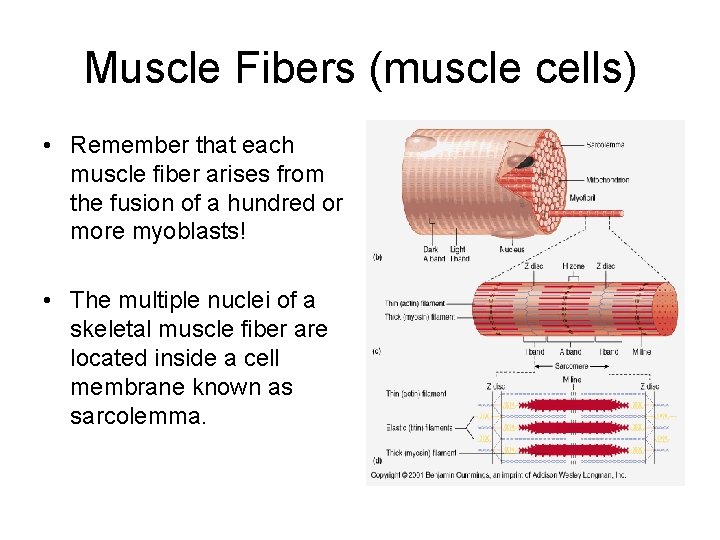
Muscle Fibers (muscle cells) • Remember that each muscle fiber arises from the fusion of a hundred or more myoblasts! • The multiple nuclei of a skeletal muscle fiber are located inside a cell membrane known as sarcolemma.
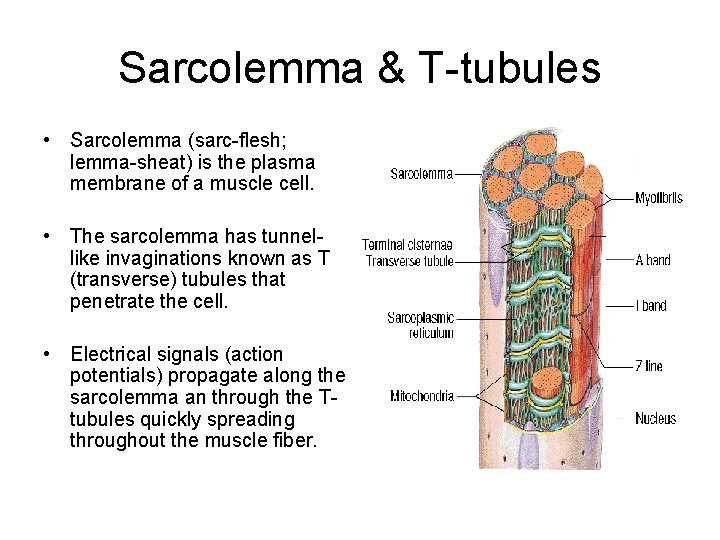
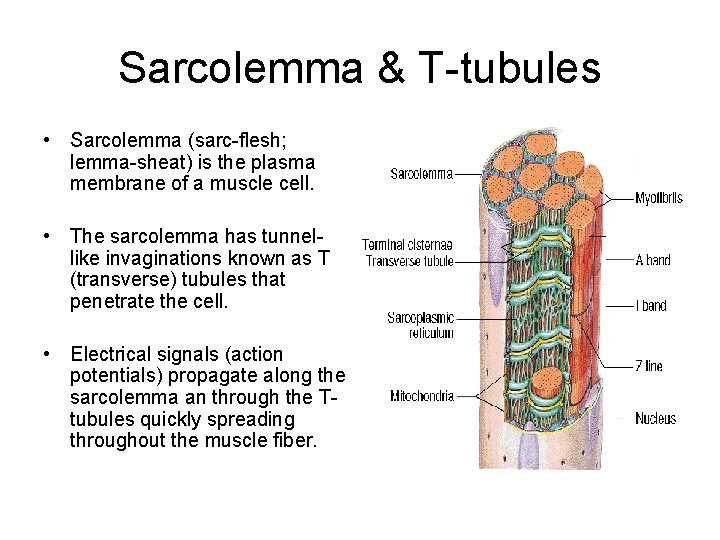
Sarcolemma & T-tubules • Sarcolemma (sarc-flesh; lemma-sheat) is the plasma membrane of a muscle cell. • The sarcolemma has tunnellike invaginations known as T (transverse) tubules that penetrate the cell. • Electrical signals (action potentials) propagate along the sarcolemma an through the Ttubules quickly spreading throughout the muscle fiber.
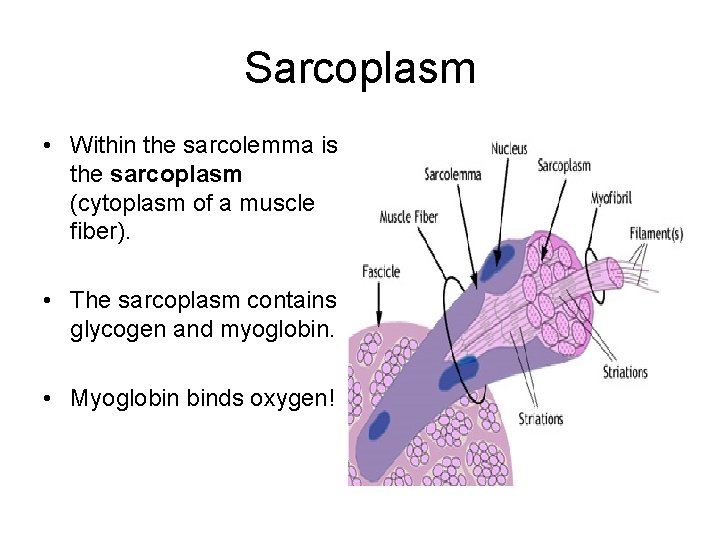
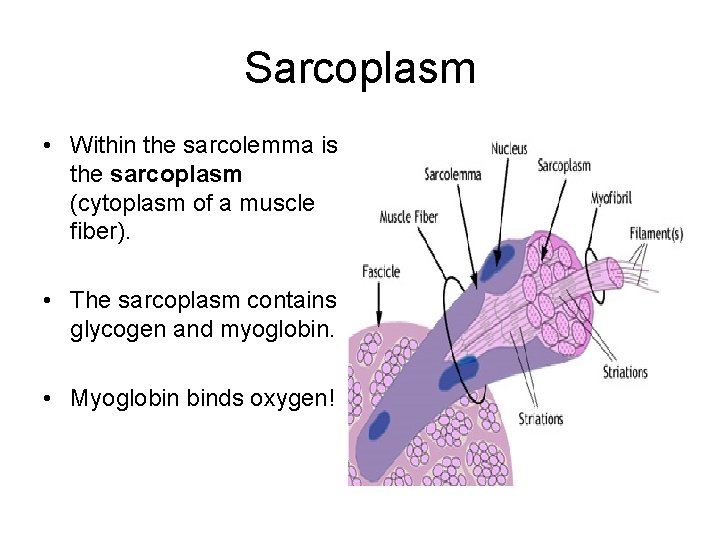
Sarcoplasm • Within the sarcolemma is the sarcoplasm (cytoplasm of a muscle fiber). • The sarcoplasm contains glycogen and myoglobin. • Myoglobin binds oxygen!
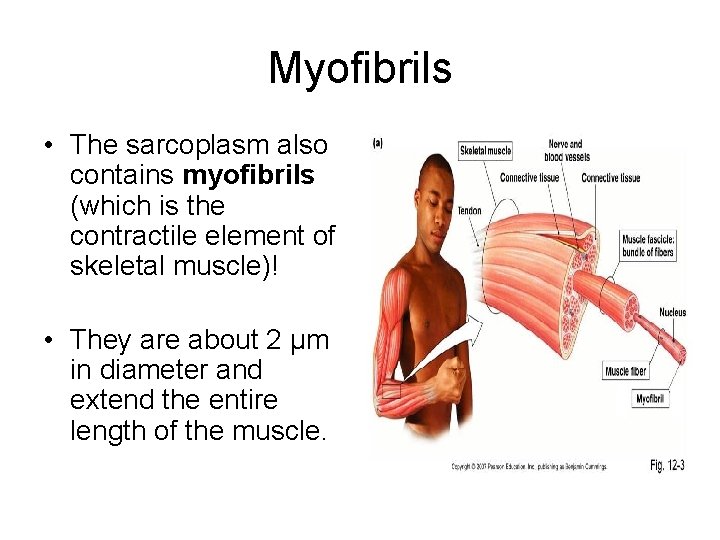
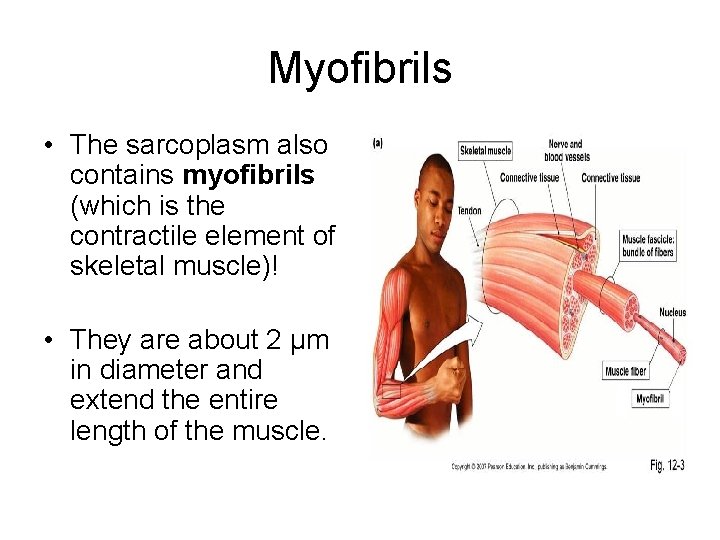
Myofibrils • The sarcoplasm also contains myofibrils (which is the contractile element of skeletal muscle)! • They are about 2 μm in diameter and extend the entire length of the muscle.
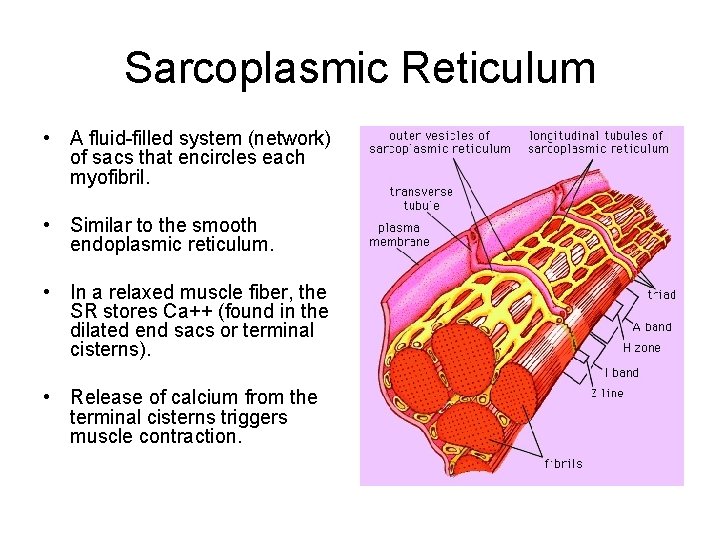
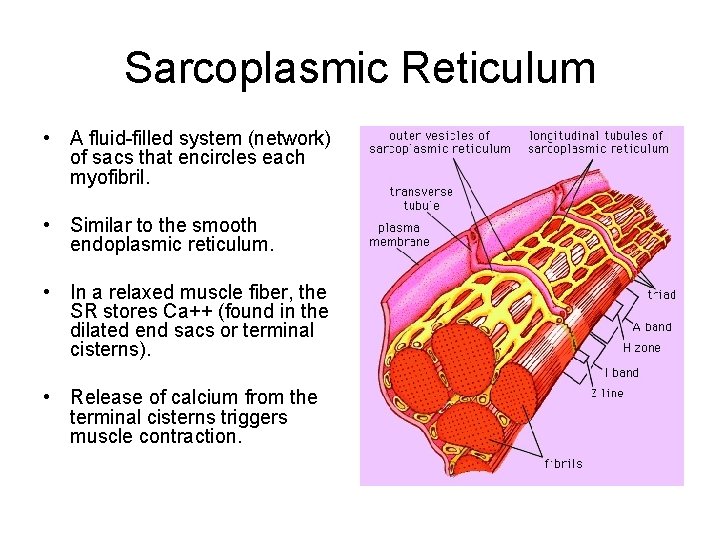
Sarcoplasmic Reticulum • A fluid-filled system (network) of sacs that encircles each myofibril. • Similar to the smooth endoplasmic reticulum. • In a relaxed muscle fiber, the SR stores Ca++ (found in the dilated end sacs or terminal cisterns). • Release of calcium from the terminal cisterns triggers muscle contraction.

Filaments & Sarcomeres • There are two (2) types of very small structures within the myofibrils known as filaments. • Thin filaments (8 nm in diameter) • Thick filaments (16 nm in diameter) • There are two thin filaments for every thick filament!

Sarcomeres • The filaments inside a myofibril DO NOT extend the entire length of a muscle fiber. • They are arranged in compartments called sarcomeres! • Sarcomeres are the basic functional unit of myofibrils!
Muscle Proteins • Myofibrils are built from three kinds of proteins: (1) contractile, which generate force during contraction; (2) regulatory, which helps switch the contraction on and off; and (3) structural proteins, which keep the thin and thick filaments in the proper alignment, give the myofibril elasticity and extensibility, and links the myofibrils to the sarcolemma and extracellular fluid.
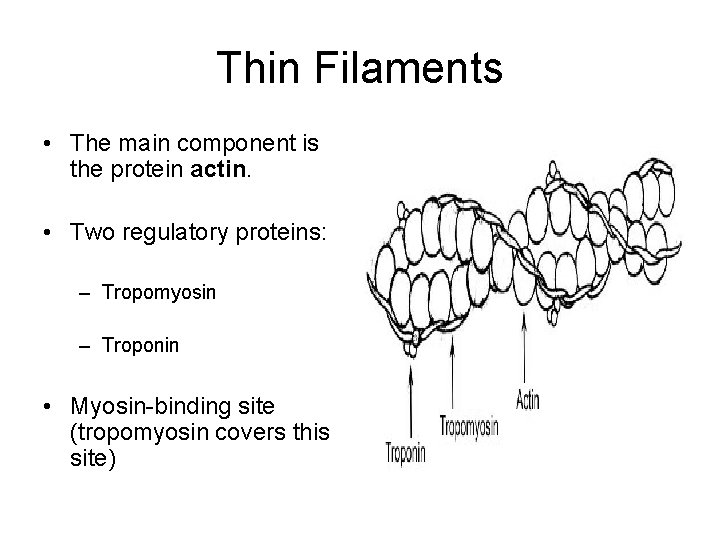
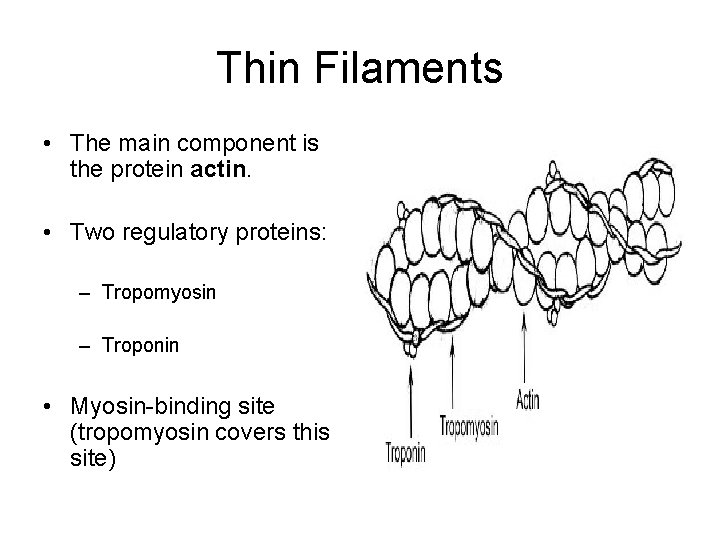
Thin Filaments • The main component is the protein actin. • Two regulatory proteins: – Tropomyosin – Troponin • Myosin-binding site (tropomyosin covers this site)
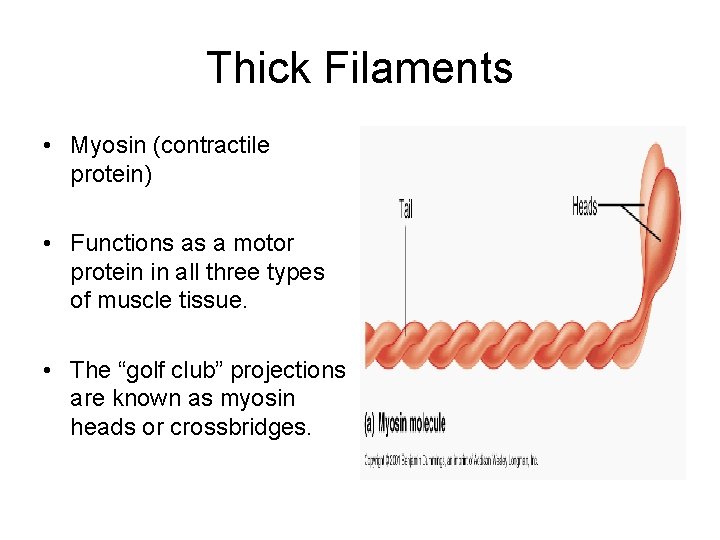
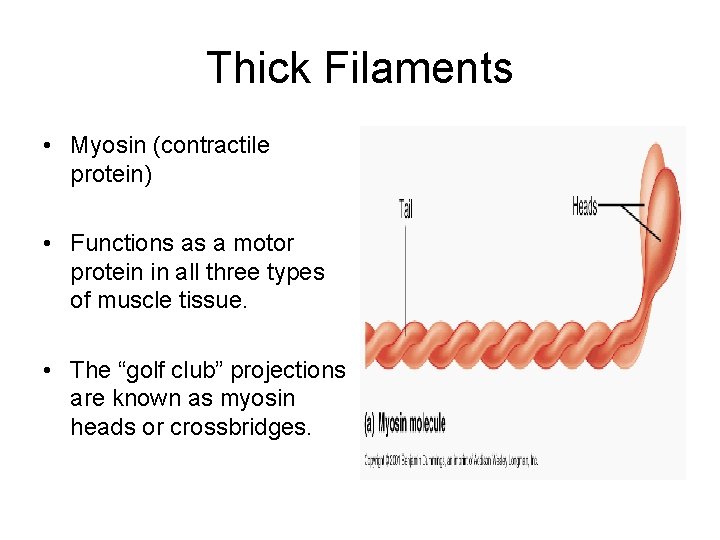
Thick Filaments • Myosin (contractile protein) • Functions as a motor protein in all three types of muscle tissue. • The “golf club” projections are known as myosin heads or crossbridges.


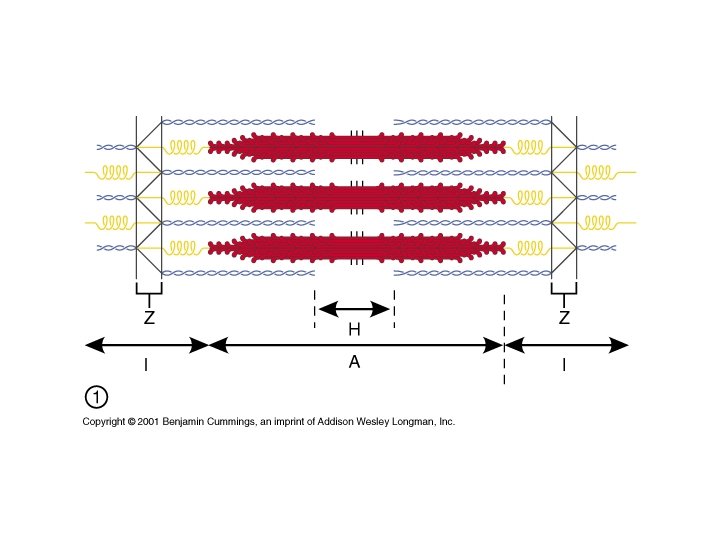
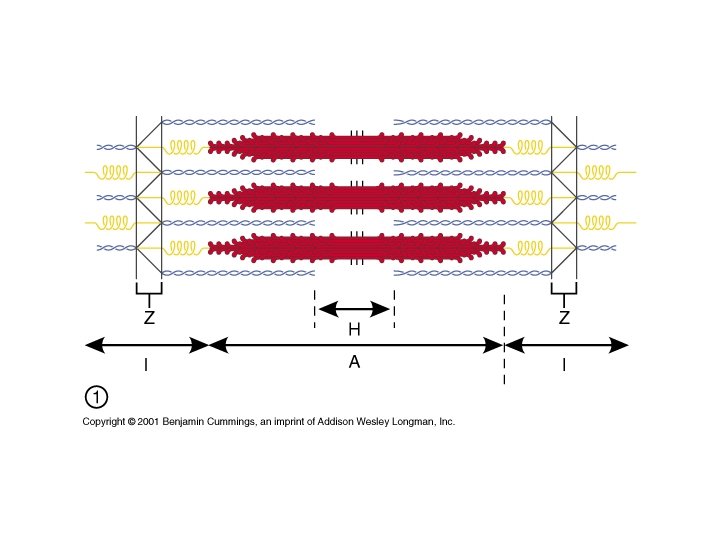
I-BANDS Z-LINES A-BANDS H-ZONES (disks)
Sarcomeres • A sarcomere extends from Z-line to Z-line • I-Bands contain only thin filaments • A-Bands contain thick and thin filaments • H-Zone contain only thick filaments
The Sliding Filament Mechanism • Myosin heads attach to and “walk” along the thin filaments at both ends of the sarcomere, progressively pulling the thin filament toward the center of the sarcomere.



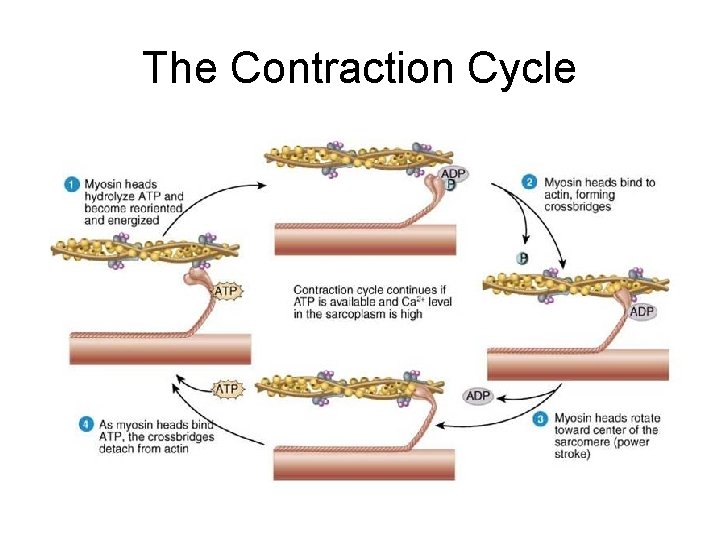
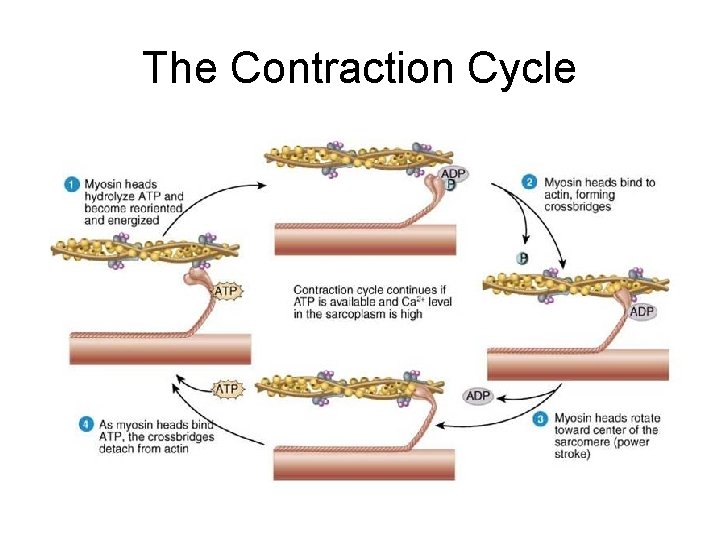
The Contraction Cycle • ATP hydrolysis. • Attachment of myosin to actin to form crossbridges. • Power stroke. • Detachment of myosin from actin.
Before we move forward … • Neuromuscular junction • Motor Unit • Acetylcholine (ACh) • Acetylcholinesterase (ACh. E)
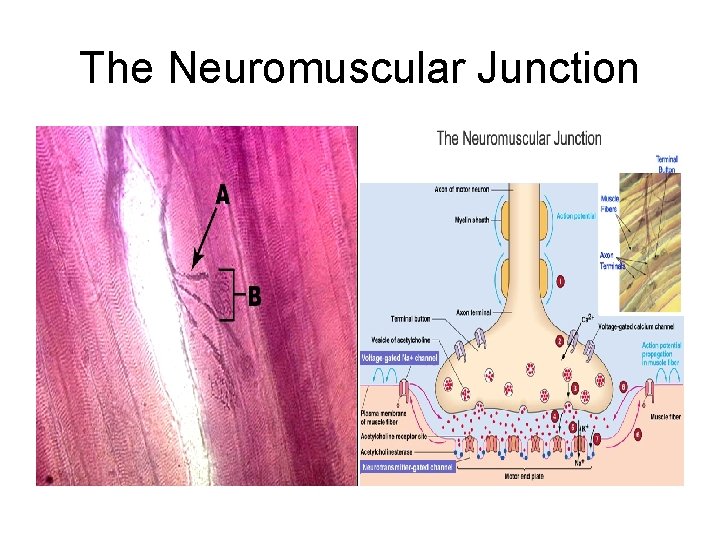
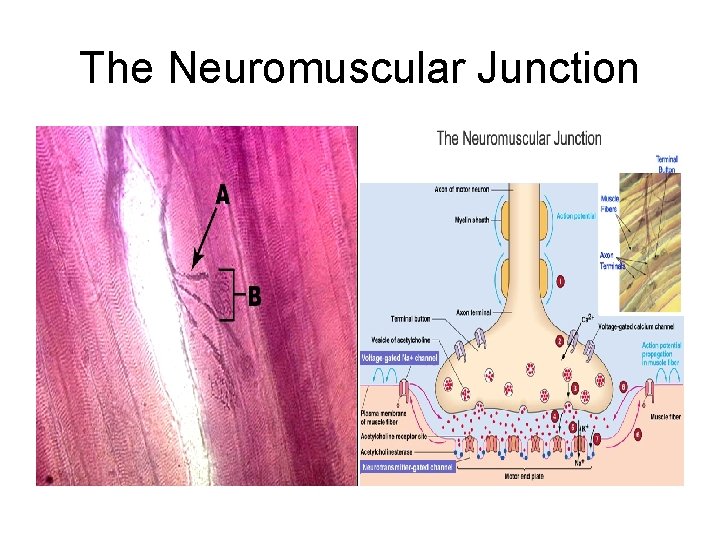
The Neuromuscular Junction
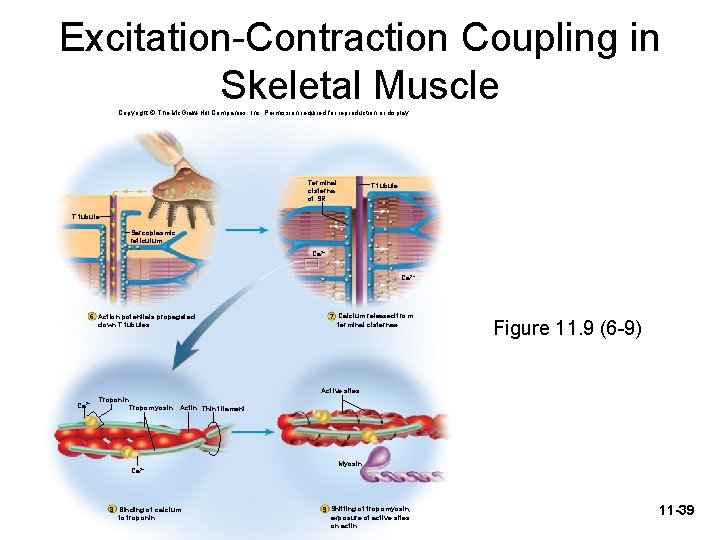
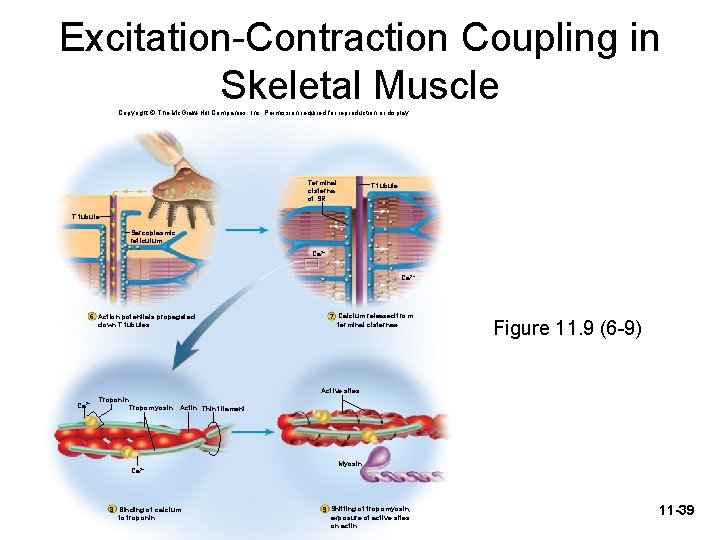
Excitation-Contraction Coupling in Skeletal Muscle Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Terminal cisterna of SR T tubule Sarcoplasmic reticulum Ca 2+ 6 Action potentials propagated down T tubules 7 Calcium released from terminal cisternae Figure 11. 9 (6 -9) Active sites Ca 2+ Troponin Tropomyosin Actin Thin filament Ca 2+ 8 Binding of calcium to troponin Myosin 9 Shifting of tropomyosin; exposure of active sites on actin 11 -39
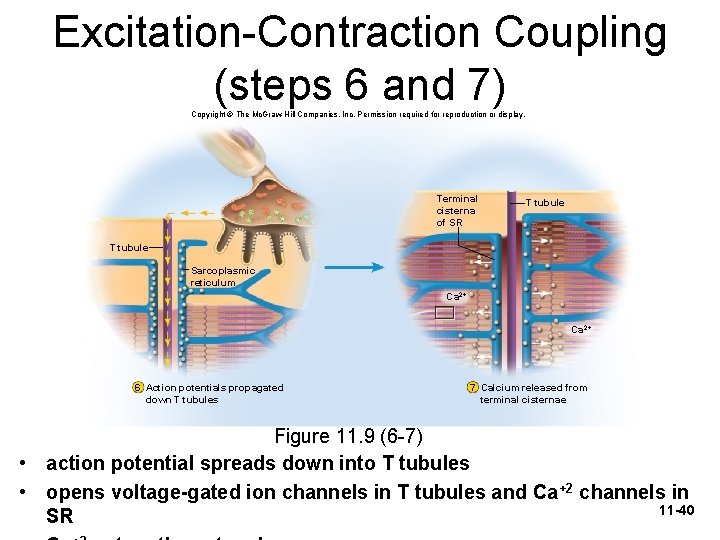
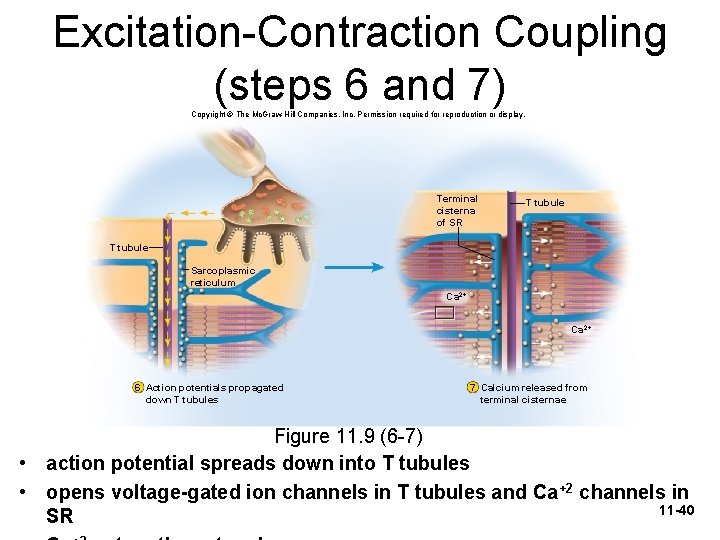
Excitation-Contraction Coupling (steps 6 and 7) Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Terminal cisterna of SR T tubule Sarcoplasmic reticulum Ca 2+ 6 Action potentials propagated down T tubules 7 Calcium released from terminal cisternae Figure 11. 9 (6 -7) • action potential spreads down into T tubules • opens voltage-gated ion channels in T tubules and Ca+2 channels in 11 -40 SR
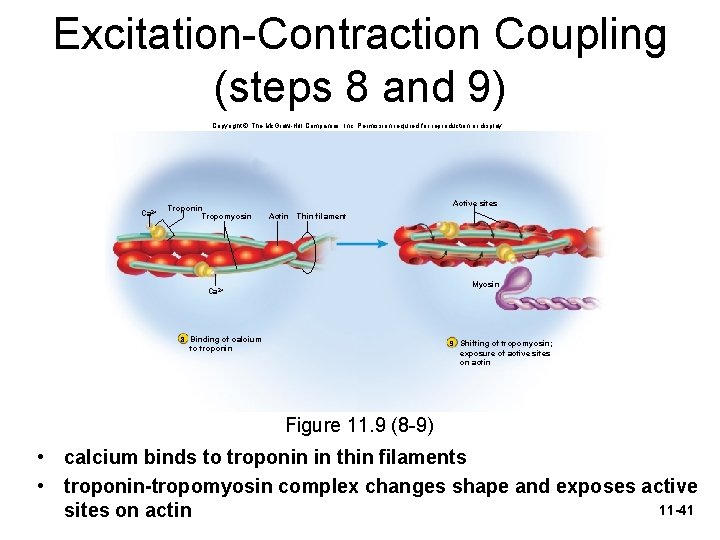
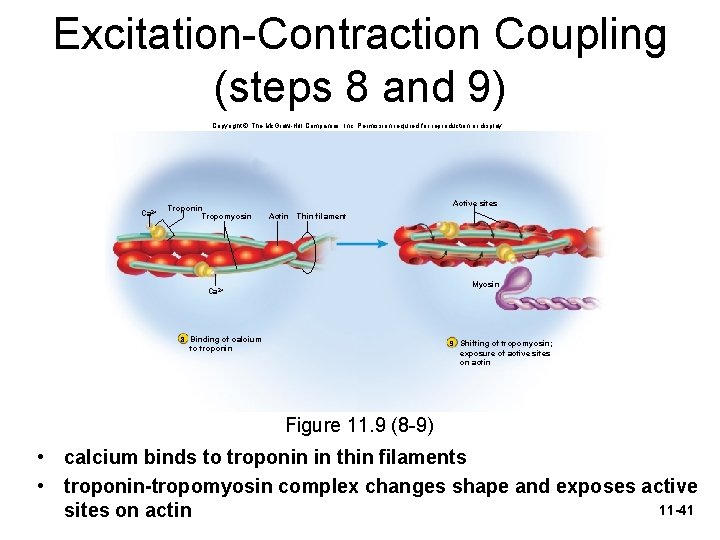
Excitation-Contraction Coupling (steps 8 and 9) Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Ca 2+ Troponin Tropomyosin Active sites Actin Thin filament Myosin Ca 2+ 8 Binding of calcium 9 Shifting of tropomyosin; to troponin exposure of active sites on actin Figure 11. 9 (8 -9) • calcium binds to troponin in thin filaments • troponin-tropomyosin complex changes shape and exposes active 11 -41 sites on actin
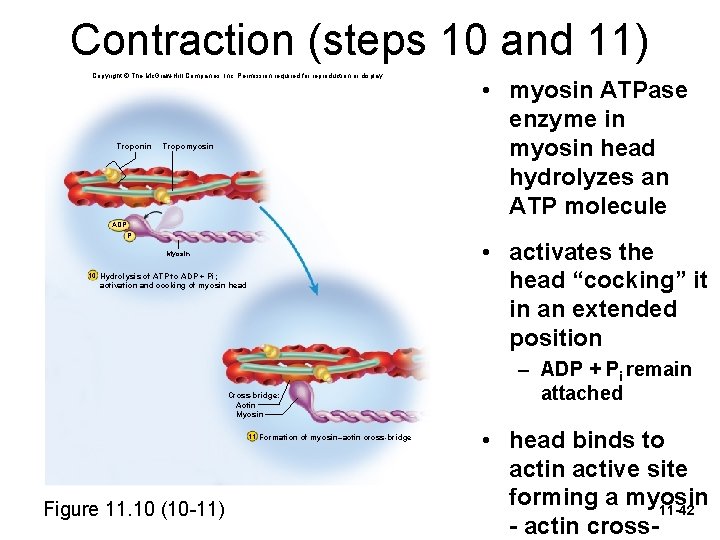
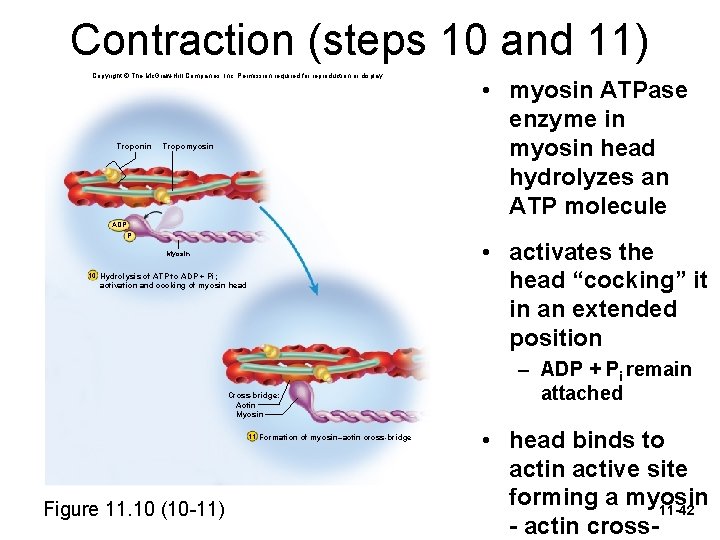
Contraction (steps 10 and 11) Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Troponin Tropomyosin ADP Pi • activates the head “cocking” it in an extended position Myosin 10 Hydrolysis of ATP to ADP + Pi; activation and cocking of myosin head Cross-bridge: Actin Myosin 11 Formation of myosin–actin cross-bridge Figure 11. 10 (10 -11) • myosin ATPase enzyme in myosin head hydrolyzes an ATP molecule – ADP + Pi remain attached • head binds to actin active site forming a myosin 11 -42 - actin cross-
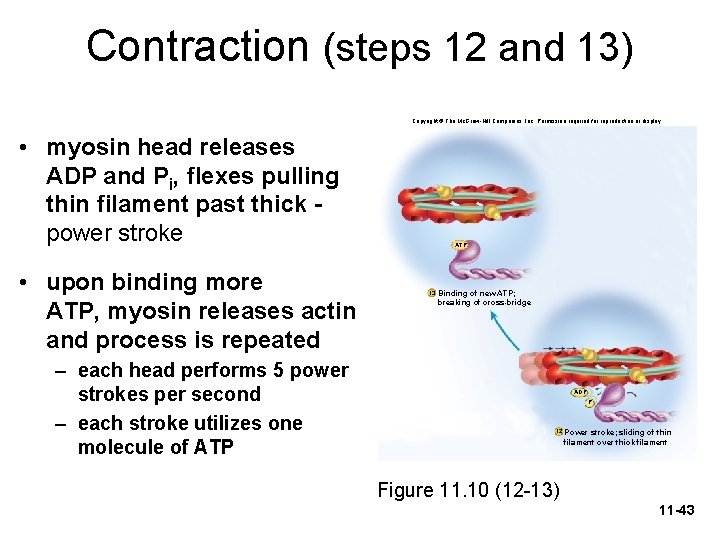
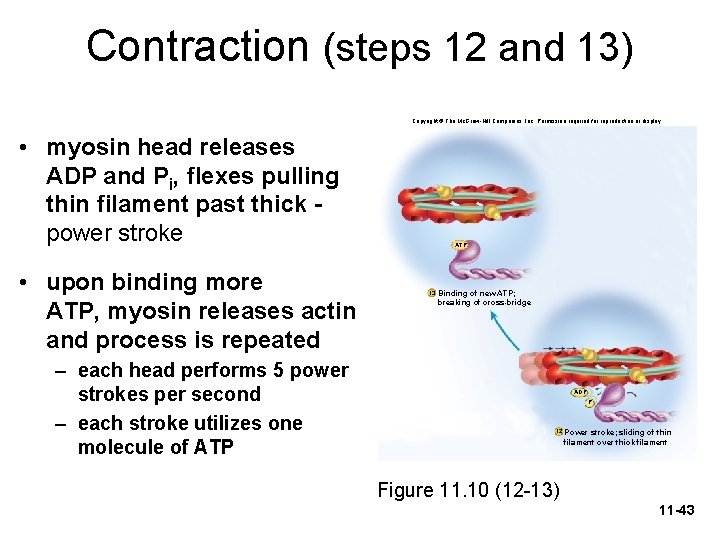
Contraction (steps 12 and 13) Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. • myosin head releases ADP and Pi, flexes pulling thin filament past thick power stroke • upon binding more ATP, myosin releases actin and process is repeated – each head performs 5 power strokes per second – each stroke utilizes one molecule of ATP 13 Binding of new ATP; breaking of cross-bridge ADP PPii 12 Power stroke; sliding of thin filament over thick filament Figure 11. 10 (12 -13) 11 -43
The Contraction Cycle

What about muscle relaxation? • Nerve impulse stops • What happens to calcium? • What do I need ATP for? • What about troponin? • What about the troponintropomyosin complex?
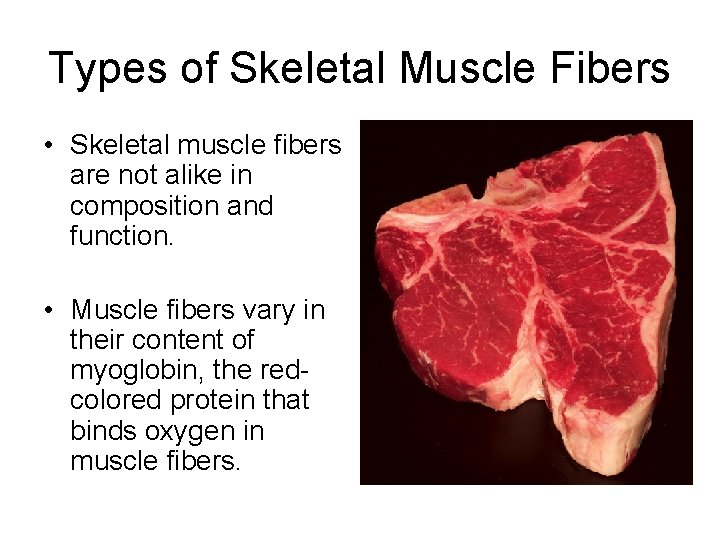
Types of Skeletal Muscle Fibers • Skeletal muscle fibers are not alike in composition and function. • Muscle fibers vary in their content of myoglobin, the redcolored protein that binds oxygen in muscle fibers.
Slow Oxidative Fibers (SO) • SO fibers are the smallest in diameter and thus are the least powerful type of muscle fibers. • They appear dark red because they contain large amounts of myoglobin and many blood capillaries. • They have many large mitochondria. • They generate ATP by aerobic cellular respiration, which is why they are called oxidative fibers.
Fast Glycolytic Fibers • FG fibers are larger in diameter and contain the most myofibrils. • Hence, they can generate the most powerful contraction. • FG fibers have low myoglobin content, relatively few blood capillaries, few mitochondria, and appear white in color.

FG and SO Muscle Fibers Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. FG SO Figure 11. 20 11 -49
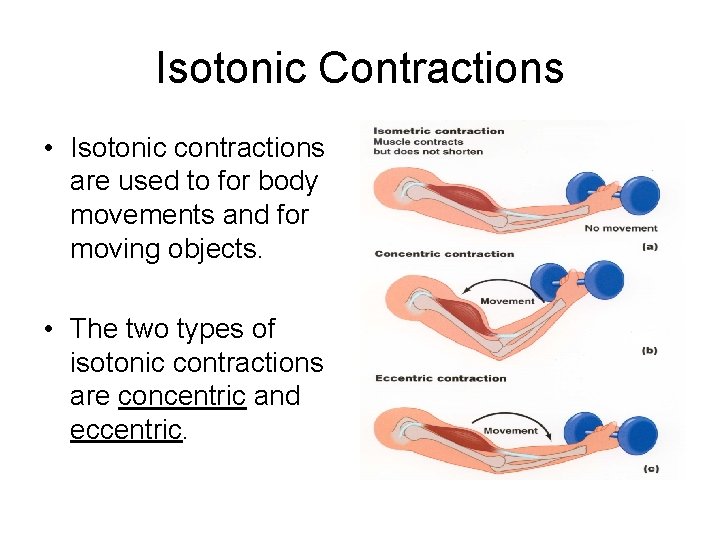
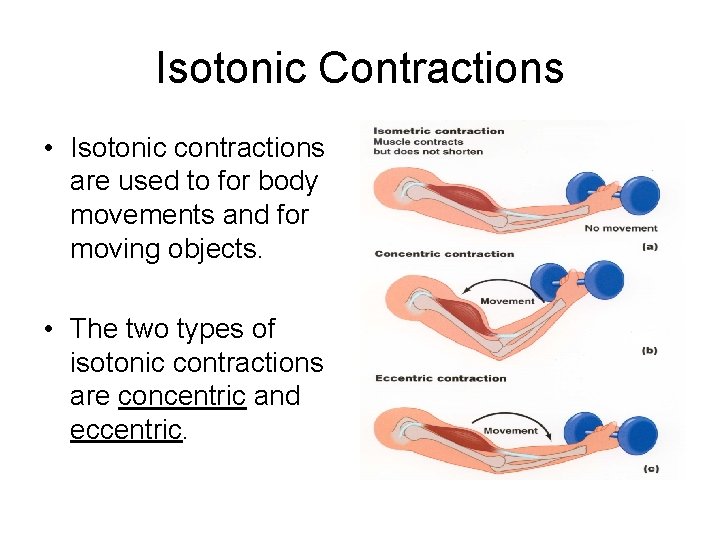
Isotonic Contractions • Isotonic contractions are used to for body movements and for moving objects. • The two types of isotonic contractions are concentric and eccentric.

Concentric Isotonic Contractions • In a concentric contraction, a muscle shortens and pulls on another structure, such as a tendon, to produce movement and the reduce the angle of the joint. • Picking a book off a table involves concentric isotonic contractions of the biceps brachii muscle.

Eccentric Isotonic Contractions • When the length of a muscle increases during a contraction.
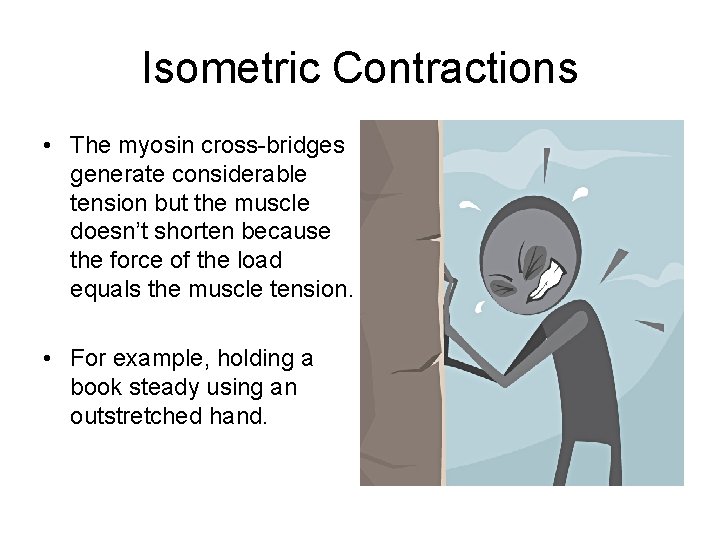
Isometric Contractions • The myosin cross-bridges generate considerable tension but the muscle doesn’t shorten because the force of the load equals the muscle tension. • For example, holding a book steady using an outstretched hand.


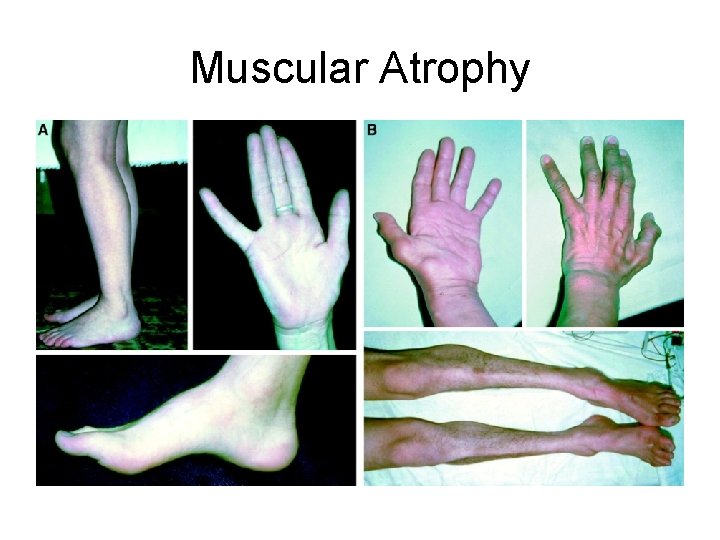
Muscular Atrophy • A: without; trophy: nourishment – is a wasting away of muscles. • Individual muscle fibers decrease in size because of progressive loss of myofibrils. • Disuse atrophy: if muscle are not used! • Denervation atrophy: if the nerve supply is cut or disrupted. In about 6 months to 2 years, the muscle will be one-quarter of its original size, and the muscle fibers will be replaced by fibrous tissue. The transition to connective tissue, when complete, cannot be reversed.
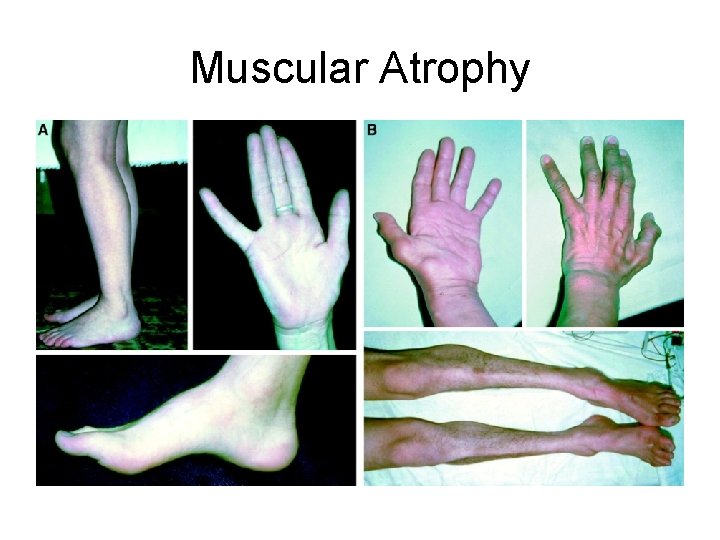
Muscular Atrophy
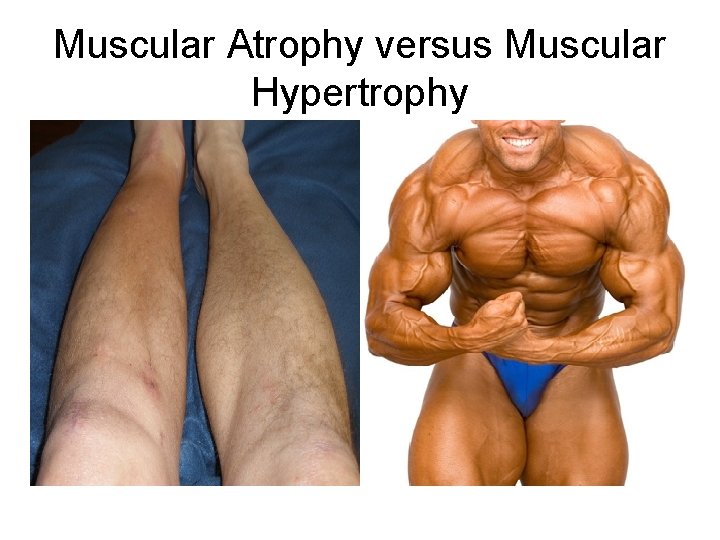
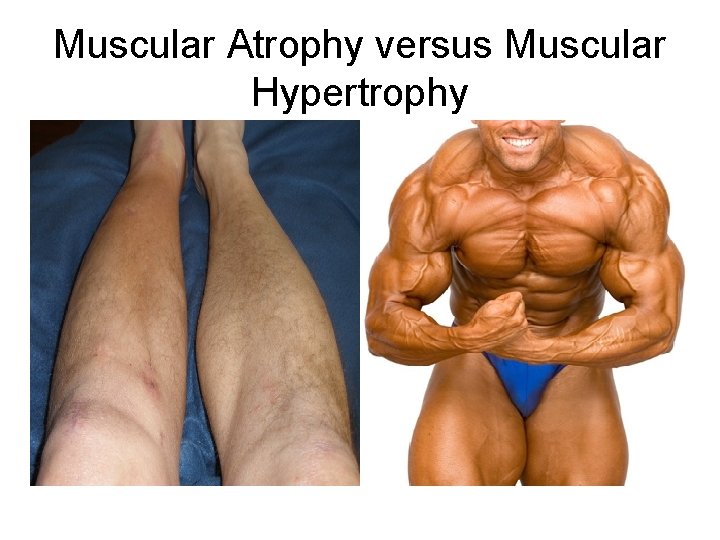
Muscular Atrophy versus Muscular Hypertrophy
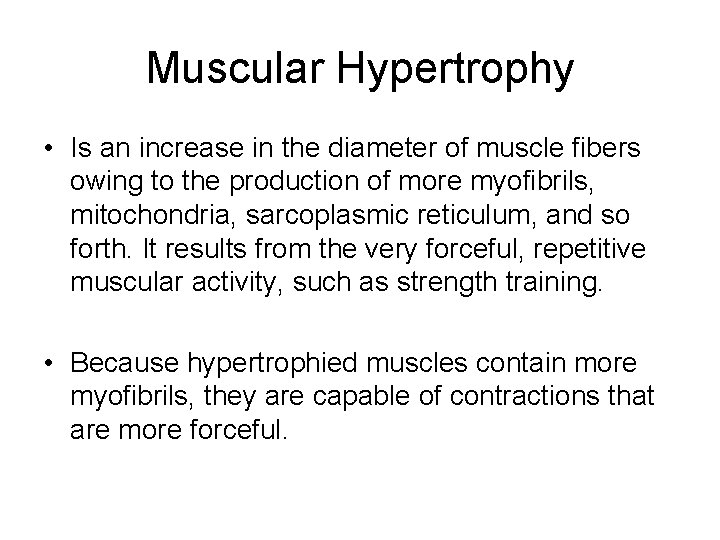
Muscular Hypertrophy • Is an increase in the diameter of muscle fibers owing to the production of more myofibrils, mitochondria, sarcoplasmic reticulum, and so forth. It results from the very forceful, repetitive muscular activity, such as strength training. • Because hypertrophied muscles contain more myofibrils, they are capable of contractions that are more forceful.
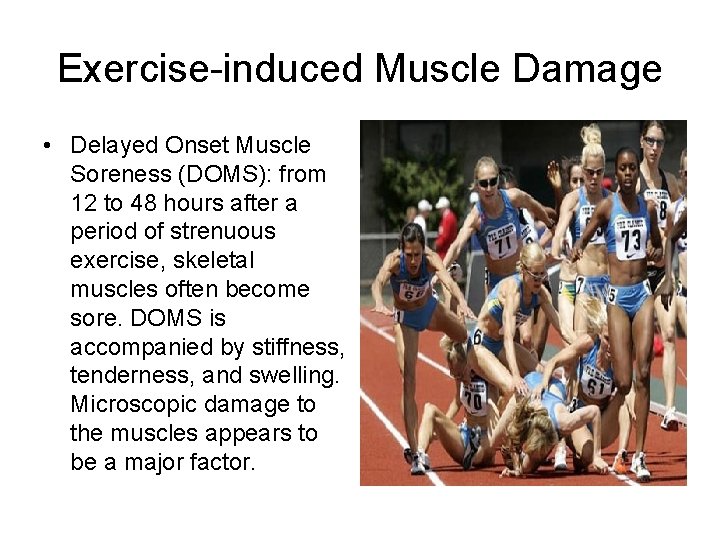
Exercise-induced Muscle Damage • Delayed Onset Muscle Soreness (DOMS): from 12 to 48 hours after a period of strenuous exercise, skeletal muscles often become sore. DOMS is accompanied by stiffness, tenderness, and swelling. Microscopic damage to the muscles appears to be a major factor.
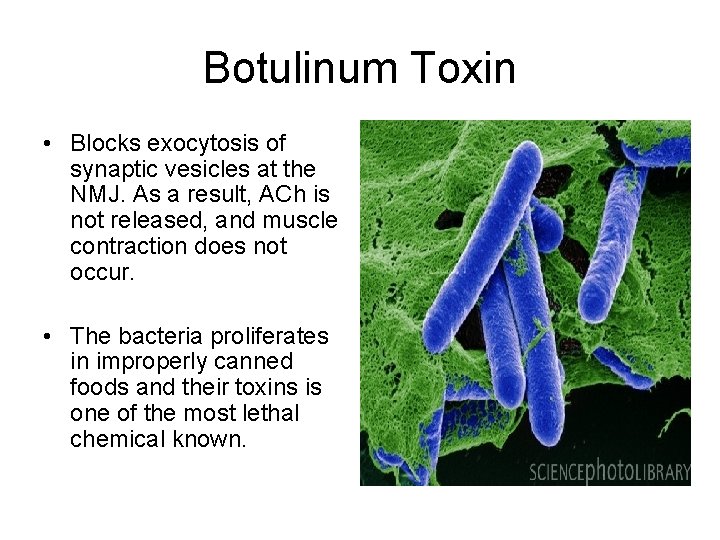
Botulinum Toxin • Blocks exocytosis of synaptic vesicles at the NMJ. As a result, ACh is not released, and muscle contraction does not occur. • The bacteria proliferates in improperly canned foods and their toxins is one of the most lethal chemical known.
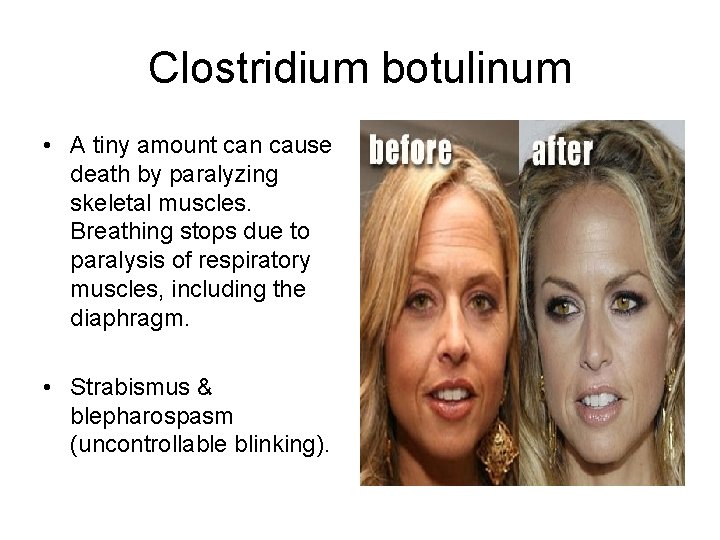
Clostridium botulinum • A tiny amount can cause death by paralyzing skeletal muscles. Breathing stops due to paralysis of respiratory muscles, including the diaphragm. • Strabismus & blepharospasm (uncontrollable blinking).

Curare • A plant derivative poison used by South American Indians on arrows and blowgun darts. • Causes muscle paralysis by binding to and blocking the ACh receptors. In the presence of curare, the ion channels do not open. • Curare-like drugs are often used during surgery to relax skeletal muscles.
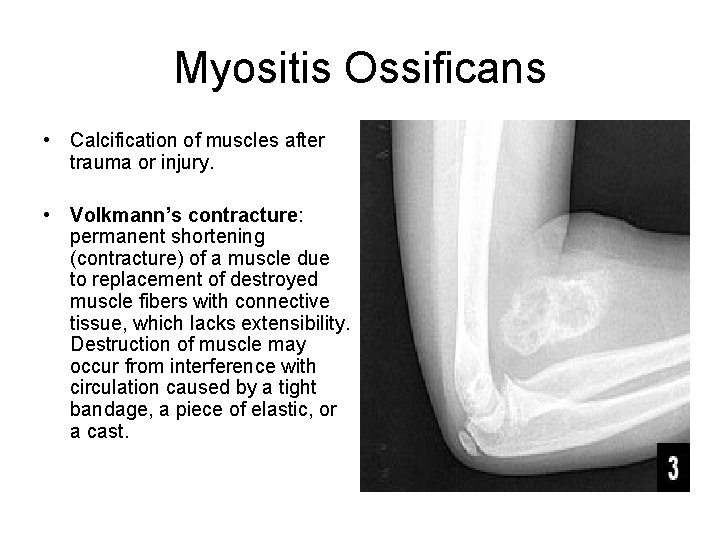
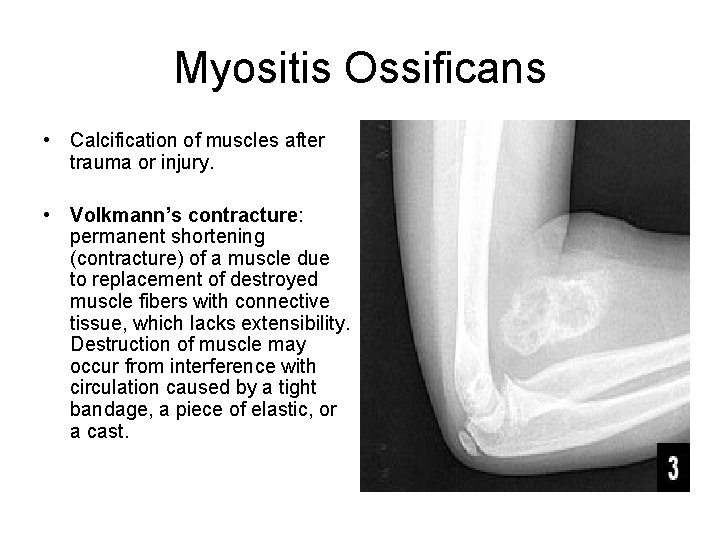
Myositis Ossificans • Calcification of muscles after trauma or injury. • Volkmann’s contracture: permanent shortening (contracture) of a muscle due to replacement of destroyed muscle fibers with connective tissue, which lacks extensibility. Destruction of muscle may occur from interference with circulation caused by a tight bandage, a piece of elastic, or a cast.
Rigor Mortis • After death, cellular membranes start to become leaky. Calcium ions leak out of the SR into the cytosol and allow heads to bind to actin. ATP synthesis has ceased, however, so the cross-bridges cannot detach from actin. As a result, the muscles are in a state of rigidity (cannot contract or stretch). • Begins 3 -4 hours after death and lasts about 24 hours. • The proteolytic enzymes from lysosomes digest the crossbridges.
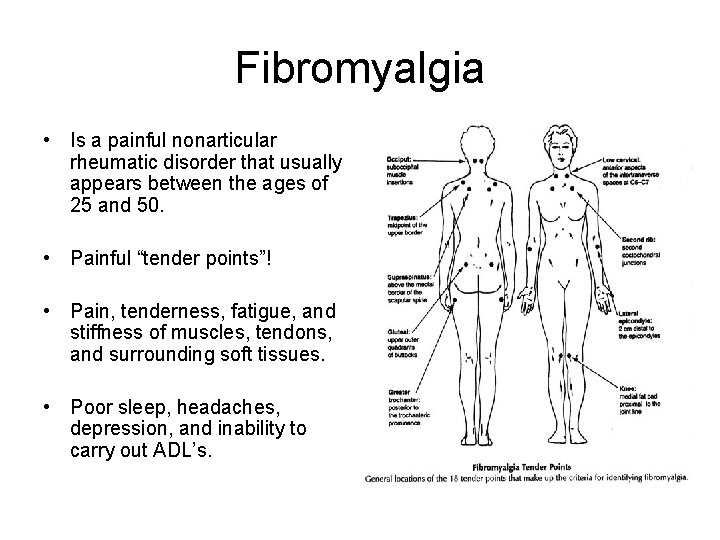
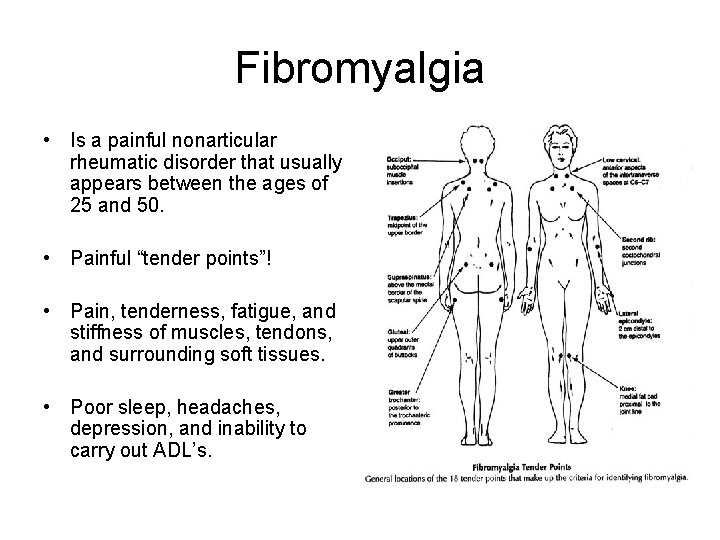
Fibromyalgia • Is a painful nonarticular rheumatic disorder that usually appears between the ages of 25 and 50. • Painful “tender points”! • Pain, tenderness, fatigue, and stiffness of muscles, tendons, and surrounding soft tissues. • Poor sleep, headaches, depression, and inability to carry out ADL’s.
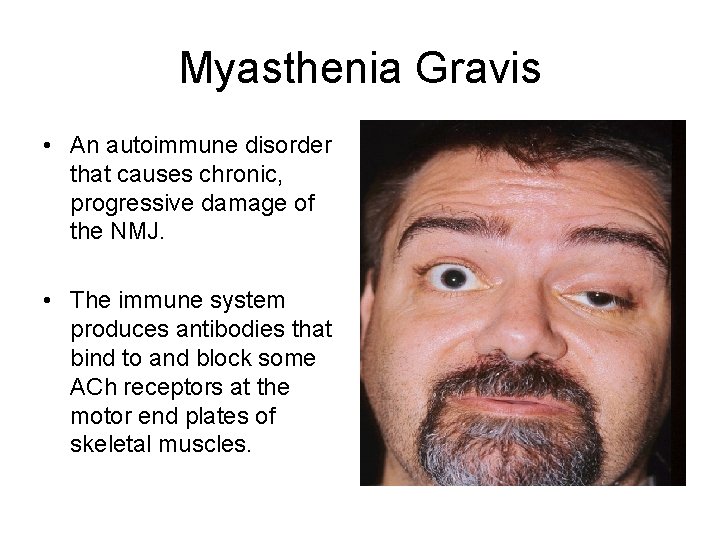
Myasthenia Gravis • An autoimmune disorder that causes chronic, progressive damage of the NMJ. • The immune system produces antibodies that bind to and block some ACh receptors at the motor end plates of skeletal muscles.
 Mussels anatomy
Mussels anatomy Waistline
Waistline Chapter 1 introduction to anatomy and physiology
Chapter 1 introduction to anatomy and physiology Human anatomy and physiology seventh edition marieb
Human anatomy and physiology seventh edition marieb Holes essential of human anatomy and physiology
Holes essential of human anatomy and physiology Chapter 2 human reproductive anatomy and physiology
Chapter 2 human reproductive anatomy and physiology Paratubular cyst
Paratubular cyst Human anatomy & physiology edition 9
Human anatomy & physiology edition 9 Cephalic cranial
Cephalic cranial How do clams reproduce
How do clams reproduce Invertebrates including snails slugs and mussels
Invertebrates including snails slugs and mussels Different market forms of shellfish
Different market forms of shellfish Invertebrates including snails slugs and mussels
Invertebrates including snails slugs and mussels Parts of the upper respiratory tract
Parts of the upper respiratory tract Tattoo anatomy and physiology
Tattoo anatomy and physiology Anatomy science olympiad
Anatomy science olympiad Perfect vs imperfect flower
Perfect vs imperfect flower Anatomy and physiology bones
Anatomy and physiology bones Anatomy of peptic ulcer
Anatomy of peptic ulcer Cantlie line
Cantlie line Hypogastric region
Hypogastric region Epigastric region
Epigastric region Google image
Google image Chapter 14 anatomy and physiology
Chapter 14 anatomy and physiology Http://anatomy and physiology
Http://anatomy and physiology Appendicitis anatomy and physiology
Appendicitis anatomy and physiology Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 2
Aohs foundations of anatomy and physiology 2 Anatomical planes
Anatomical planes Anatomy and physiology chapter 8 special senses
Anatomy and physiology chapter 8 special senses Chapter 13 anatomy and physiology of pregnancy
Chapter 13 anatomy and physiology of pregnancy Agriscience unit 26 self evaluation answers
Agriscience unit 26 self evaluation answers Science olympiad forensics cheat sheet
Science olympiad forensics cheat sheet Anatomy and physiology chapter 2
Anatomy and physiology chapter 2 Gastric emptying ppt
Gastric emptying ppt Physiology
Physiology Heat and cold
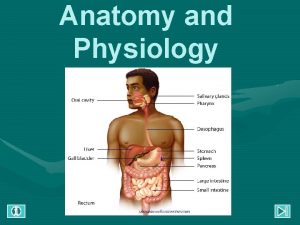
Heat and cold Chapter 14 the digestive system and body metabolism
Chapter 14 the digestive system and body metabolism Chapter 10 blood anatomy and physiology
Chapter 10 blood anatomy and physiology Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 What produces bile
What produces bile Anatomy and physiology chapter 15
Anatomy and physiology chapter 15 Cornell notes for anatomy and physiology
Cornell notes for anatomy and physiology Necessary life functions anatomy and physiology
Necessary life functions anatomy and physiology Holes anatomy and physiology chapter 1
Holes anatomy and physiology chapter 1 Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Gi tract histology
Gi tract histology Anatomy and physiology
Anatomy and physiology The speed at which the body consumes energy
The speed at which the body consumes energy Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Anatomy and physiology exam 1
Anatomy and physiology exam 1 Welcome to anatomy and physiology
Welcome to anatomy and physiology Physiology of the foot and ankle
Physiology of the foot and ankle Anatomy and physiology of psoriasis
Anatomy and physiology of psoriasis Pse4u
Pse4u Pancreas anatomy and physiology
Pancreas anatomy and physiology Anatomy and physiology vocabulary
Anatomy and physiology vocabulary Anatomy and physiology
Anatomy and physiology Muschiul subclavicular
Muschiul subclavicular Anatomy and physiology
Anatomy and physiology Body landmarks diagram
Body landmarks diagram Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Thyroid anatomy
Thyroid anatomy Dorsifelxion
Dorsifelxion Figure 11-8 arteries
Figure 11-8 arteries