Introduction to Invasive Ventilation CATHERINE JONES PRACTICE EDUCATOR


- Slides: 29
Introduction to Invasive Ventilation CATHERINE JONES PRACTICE EDUCATOR – GICU SEPTEMBER 2018
Plan for Session • ‘normal’ mechanics of breathing • What is Invasive Ventilation? • Indications & Contraindications for Invasive Ventilation • Complications of Invasive Ventilation • Ventilator Care Bundles. . • Weaning from Invasive Ventilation • Invasive Ventilation • Modes • Parameters • Alarms • Monitoring
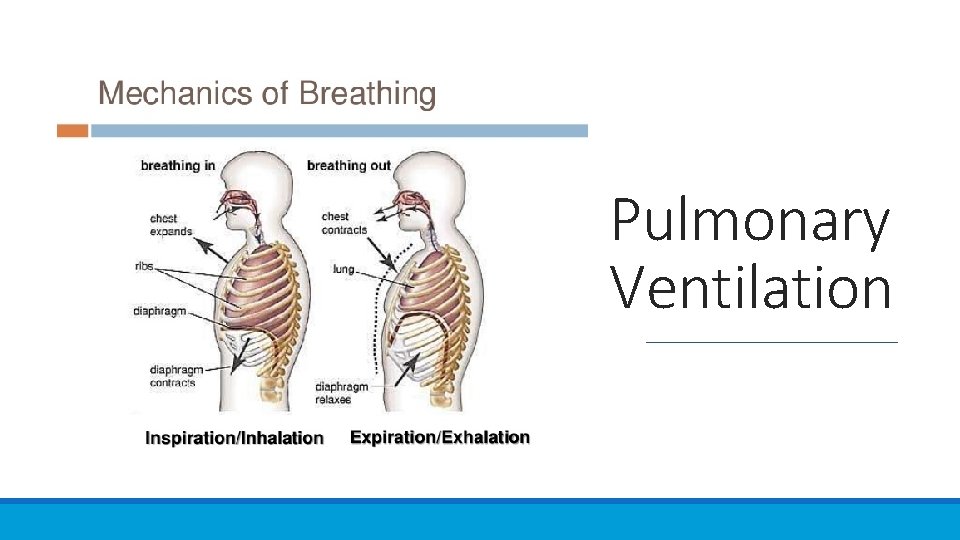
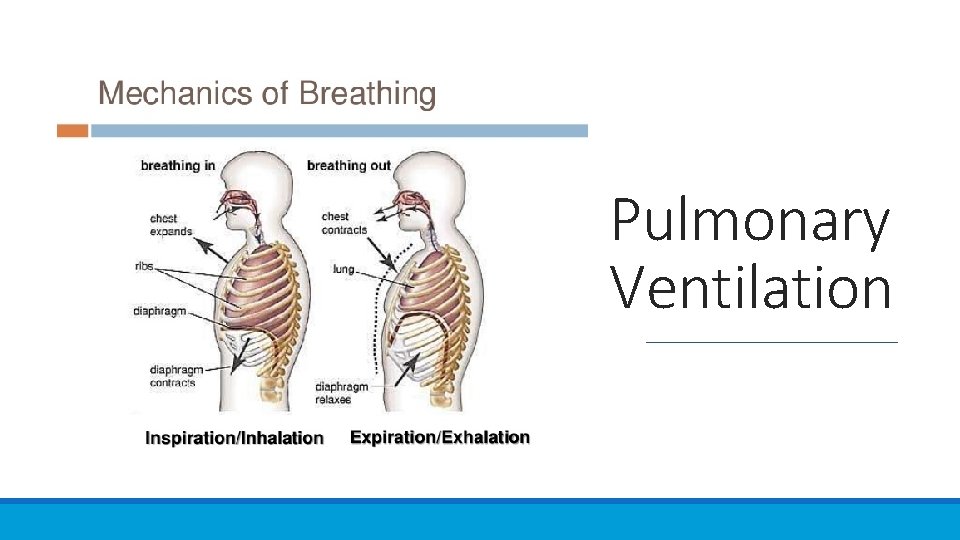
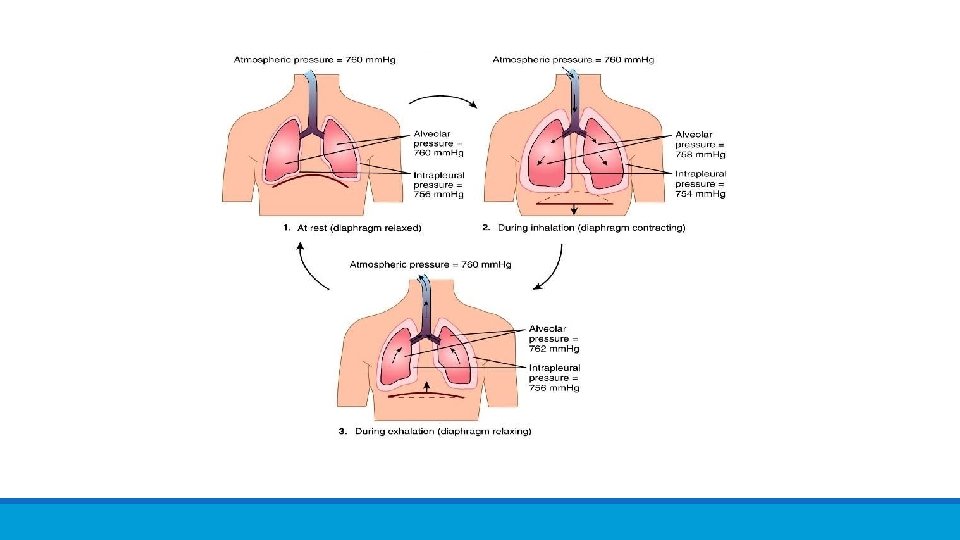
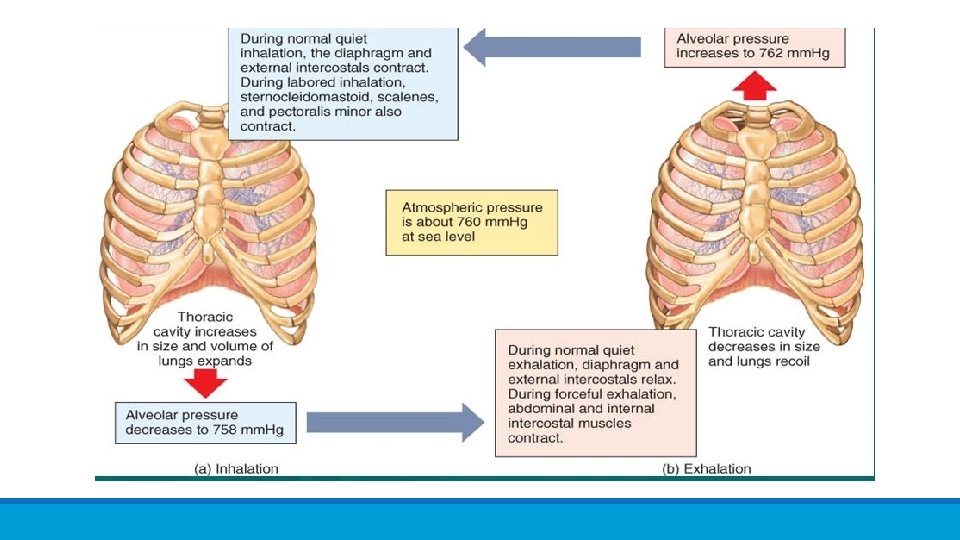
Pulmonary Ventilation
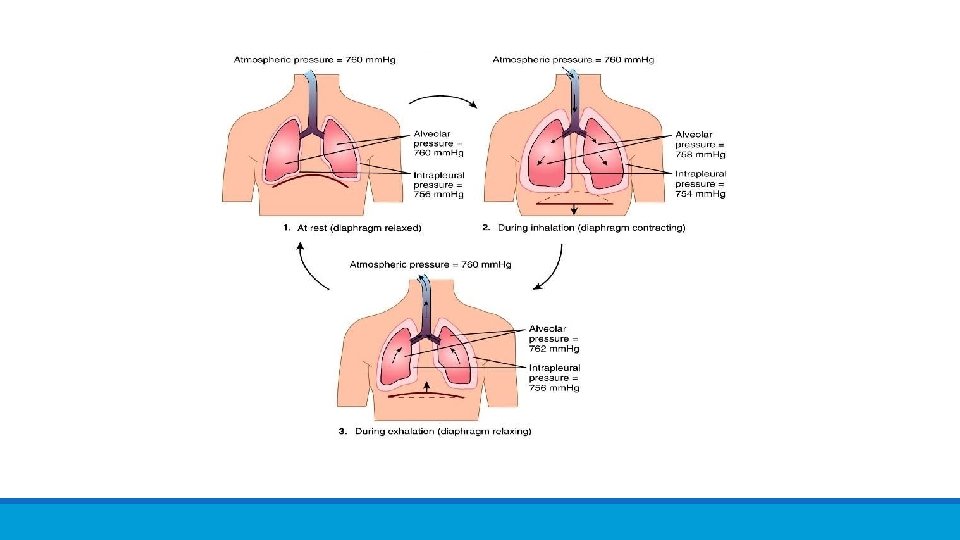
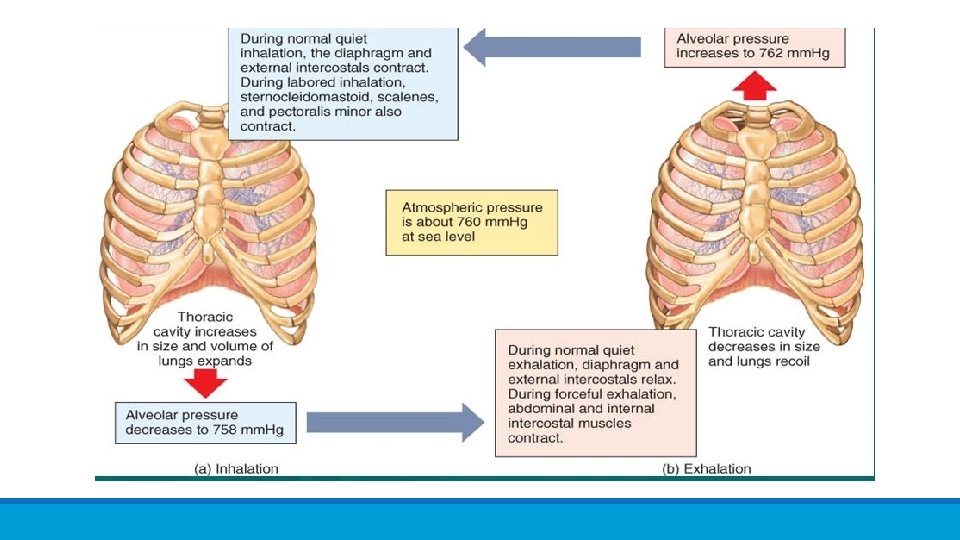
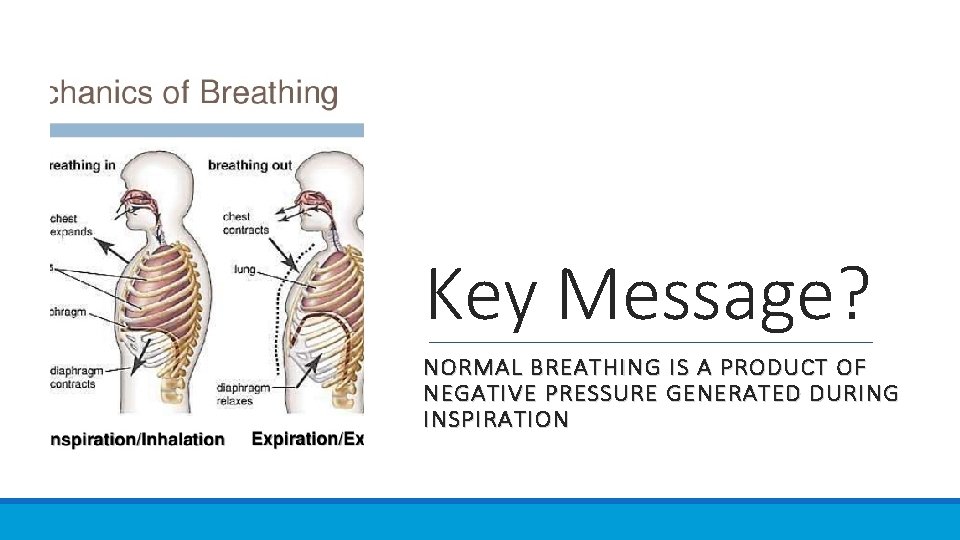
Key Message? NORMAL BREATHING IS A PRODUCT OF NEGATIVE PRESSURE GENERATED DURING INSPIRATION

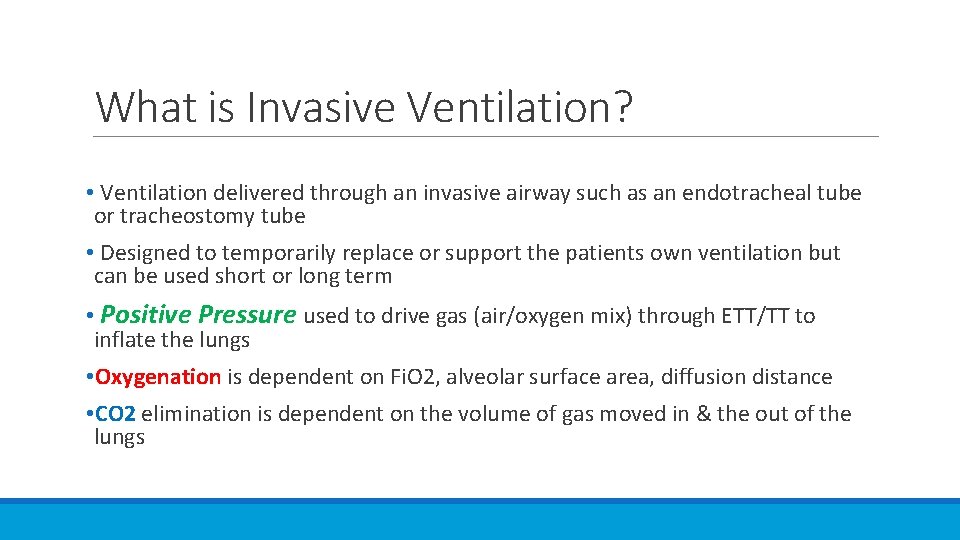
What is Invasive Ventilation?
What is Invasive Ventilation? • Ventilation delivered through an invasive airway such as an endotracheal tube or tracheostomy tube • Designed to temporarily replace or support the patients own ventilation but can be used short or long term • Positive Pressure used to drive gas (air/oxygen mix) through ETT/TT to inflate the lungs • Oxygenation is dependent on Fi. O 2, alveolar surface area, diffusion distance • CO 2 elimination is dependent on the volume of gas moved in & the out of the lungs
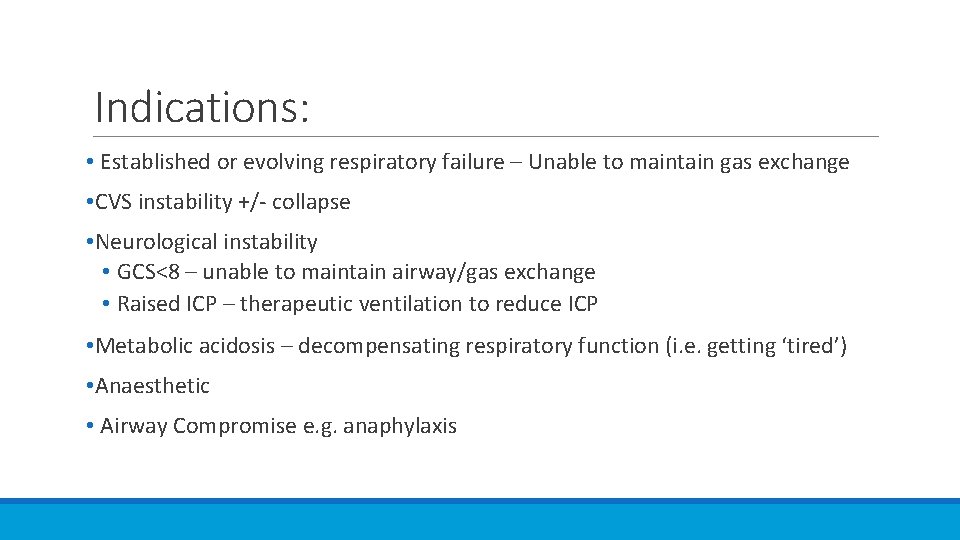
Indications: • Established or evolving respiratory failure – Unable to maintain gas exchange • CVS instability +/- collapse • Neurological instability • GCS<8 – unable to maintain airway/gas exchange • Raised ICP – therapeutic ventilation to reduce ICP • Metabolic acidosis – decompensating respiratory function (i. e. getting ‘tired’) • Anaesthetic • Airway Compromise e. g. anaphylaxis
Contraindications: Futility…
Goals of Mechanical Ventilation Maintaining alveolar ventilation I. e. CO 2 elimination Delivering appropriate oxygen concentrations Support the patients respiratory status until they are able to self ventilate, unsupported
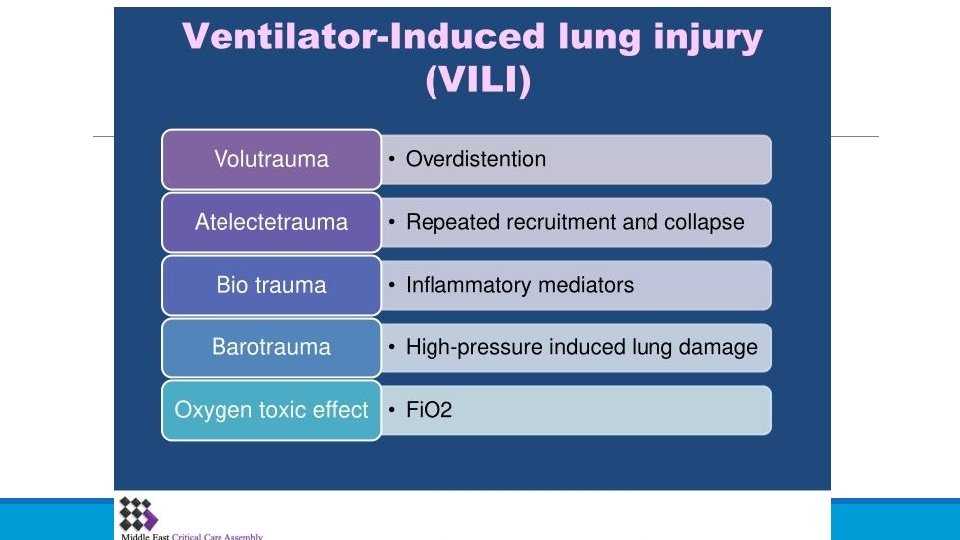
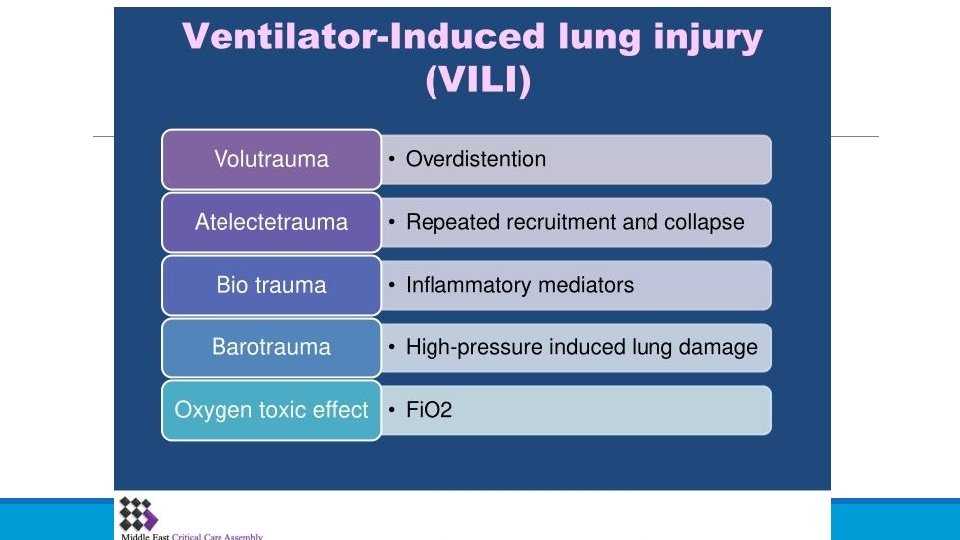
Complications of Invasive Ventilation • Aspiration & VAP • Decreased cardiac output & venous return • What you’ll see ↓BP, ↑HR, ↓UO, worsening metabolic acidosis • Increased intrathoracic pressure reduces venous return → increases Right ventricular afterload → reduced output from R & L ventricles (↓ CO) • Decreased Urine Output as a result of ↓ CO • Ventilator Induced Lung Injury • Volutrauma, Atelectatrauma, Biotrauma, Barotrauma, Oxygen Toxicity • Psychological Sequalae • PTSD, delirium
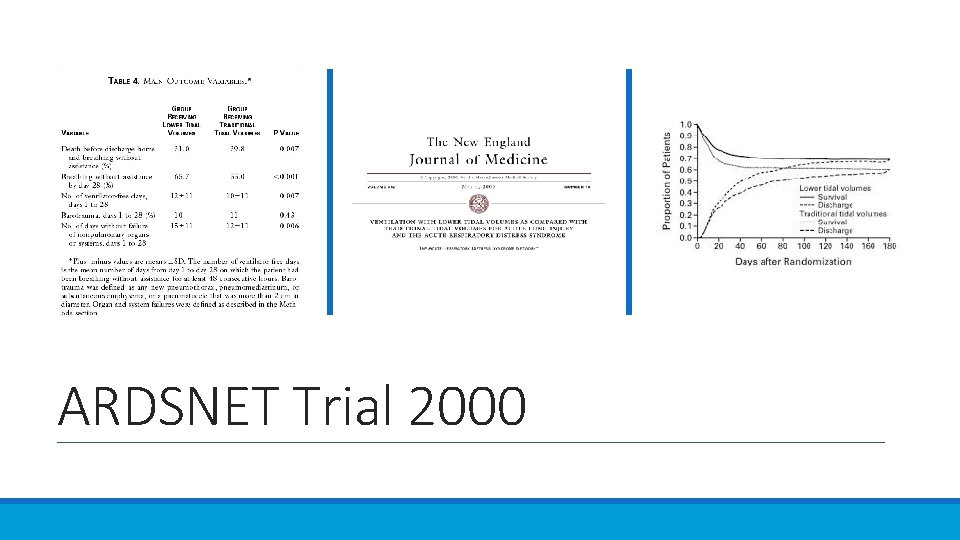
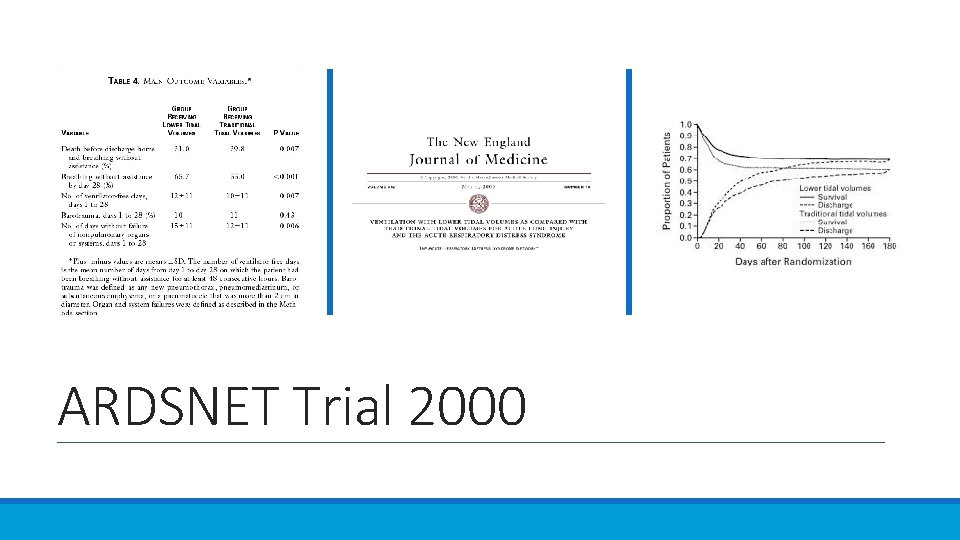
ARDSNET Trial 2000
Key Message? TIDAL VOLUME AIM 6 ML/KG OF IDEAL BODY WEIGHT
Ventilator Care Bundle (s) • Head of Bed elevation 30 -45˚ • Stress Ulcer Prophlaxis • Daily Sedation Hold • Oral Decontamination • Venous Thromboprophylaxis • ? Sub-glottic aspiration http: //www. ihi. org/resources/Pages/Tools/Howto. Guide. Prevent. VAP. aspx
Weaning • Process through which the patient is ‘liberated’ from the ventilator • Can be rapid or sloooow – Patient & condition dependent • Traditional Weaning methods • Incremental down titration of Mandatory breaths/Fi. O 2/PS/PEEP • Spontaneous Breathing Trial • Weaning ‘Sprints’ to build up stamina & muscle strength
INVASIVE VENTILATION: MODES, SETTINGS, MONITORING, ALARMS
Mechanical Ventilation - MODES Pressure Vs Volume ◦ Pressure Mode ◦ Vent delivers gas until a predetermined pressure is achieved. ◦ Often used ◦ Volume Mode ◦ Vent delivers gas until a predetermined volume is achieved. ◦ Rarely Used
Mechanical Ventilation - MODES Spontaneous, Controlled & Intermittent. ◦ Spontaneous ◦ All breaths ‘triggered’ by patient. ◦ CPAP & Pressure Support ◦ Controlled (or Mandatory) ◦ Predetermined respiratory rate is set & delivered by vent. O ◦ Overrides any spontaneous effort from patient. ◦ Intermittent ◦ vent synchronises to any spontaneous effort by patient thereby delivering both mandatory & spontaneous breaths. ◦ PCV+, PSIMV, PC-SIMV
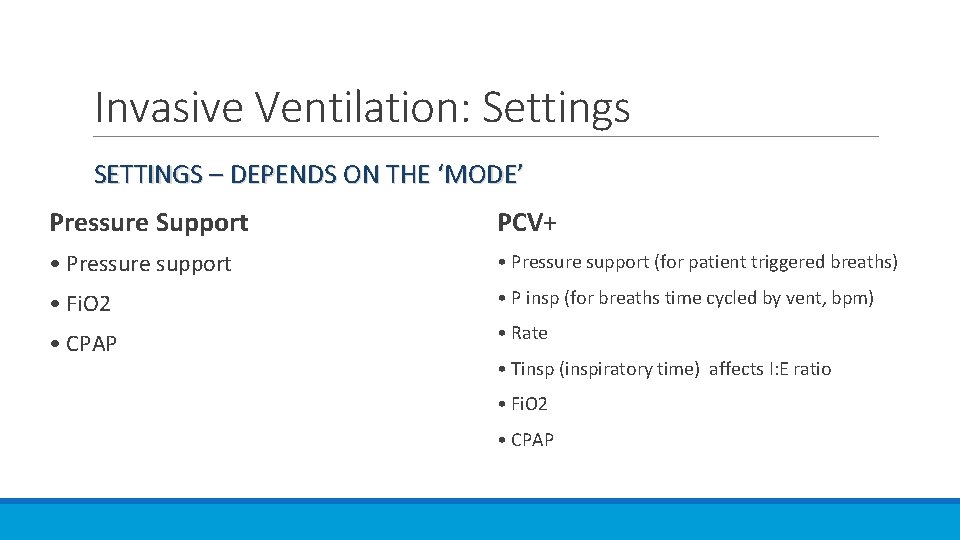
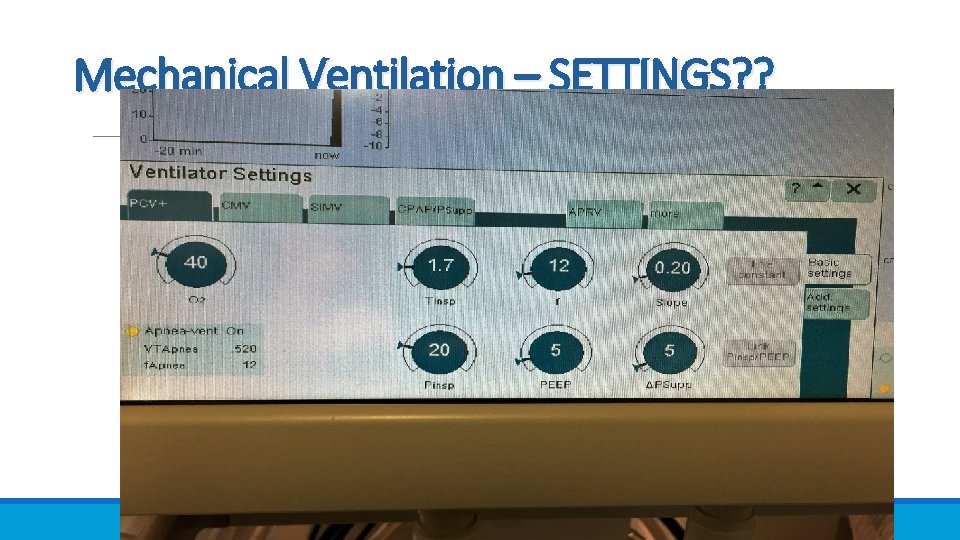
Invasive Ventilation: Settings SETTINGS – DEPENDS ON THE ‘MODE’ Pressure Support PCV+ • Pressure support (for patient triggered breaths) • Fi. O 2 • P insp (for breaths time cycled by vent, bpm) • CPAP • Rate • Tinsp (inspiratory time) affects I: E ratio • Fi. O 2 • CPAP
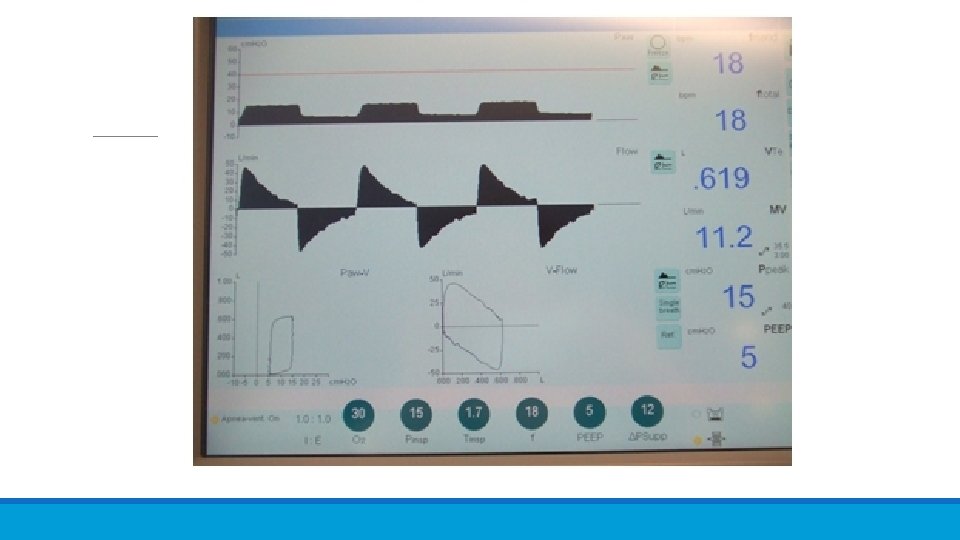
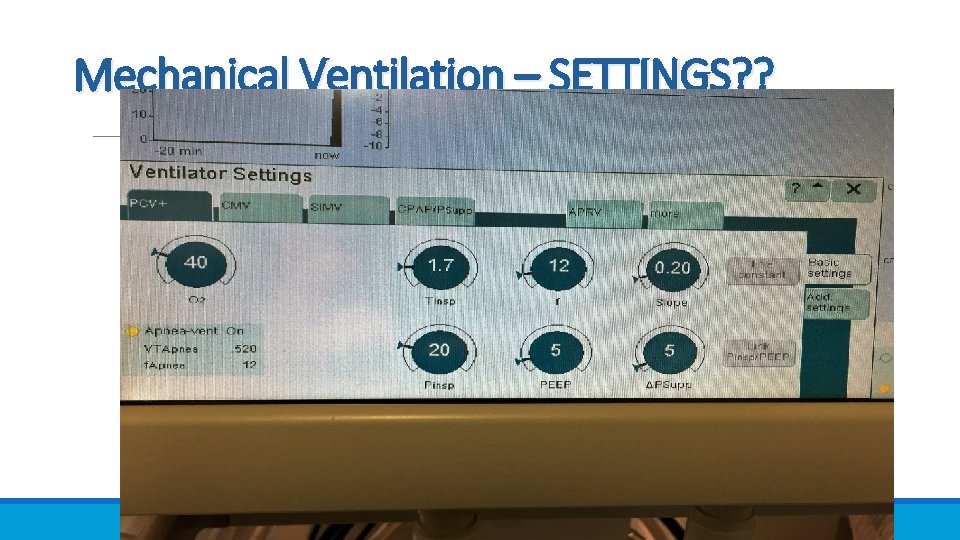
Mechanical Ventilation – SETTINGS? ?

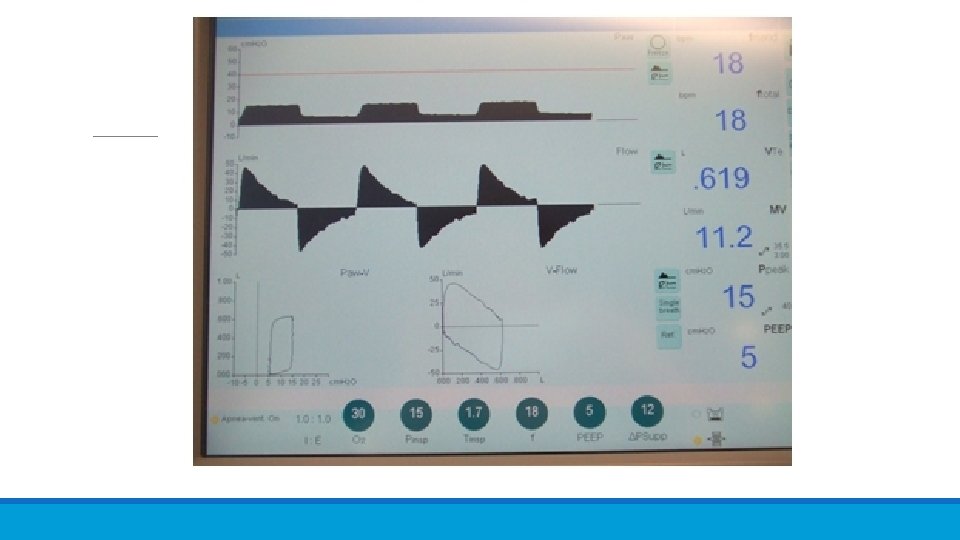
Invasive Ventilation: Monitoring • F = Respiratory rate (total and patient triggered) • Fmand (number of set breaths) • F total (total number of breaths per minute) • Vt – tidal volume • MV - (minute volume) • P peak (peak pressure reached on inspiration) • PEEP • I: E ratio (only if you set a respiratory rate) • Also: Sp. O 2, Et. CO 2, ABG, RR • Chart sticker – mls / kg (normally 6 ml/kg) of ideal body weight or predicted body weight.
Invasive Ventilation: Alarms • VT (tidal volume) • MV (minute volume) • Pressure (peak) – unless you have a good reason make sure this does not go above 30 mm. Hg • Respiratory rate (check current rate from chart) • Apnea time (normally 15 seconds or RR=4) �Don’t switch this off – only very exceptional circumstances i. e speaking valve with trachy, you must be present • Look at patients current values and check with someone if you are not sure.
Quick Quiz! • Does normal breathing rely on negative pressure or positive pressure? • Does invasive ventilation rely on negative pressure or positive pressure? • When would you not ventilate somebody? • What are complications of Invasive Ventilation? • What is v. T & how much should it be? • Describe what the vent is delivering with • CPAP/PS • PC-SIMV • If your patient has a problem with oxygenation what settings might be tweaked in consultation with Docs? • If your patient has a problem with CO 2 elimination what settings might be tweaked in consultation with Docs?
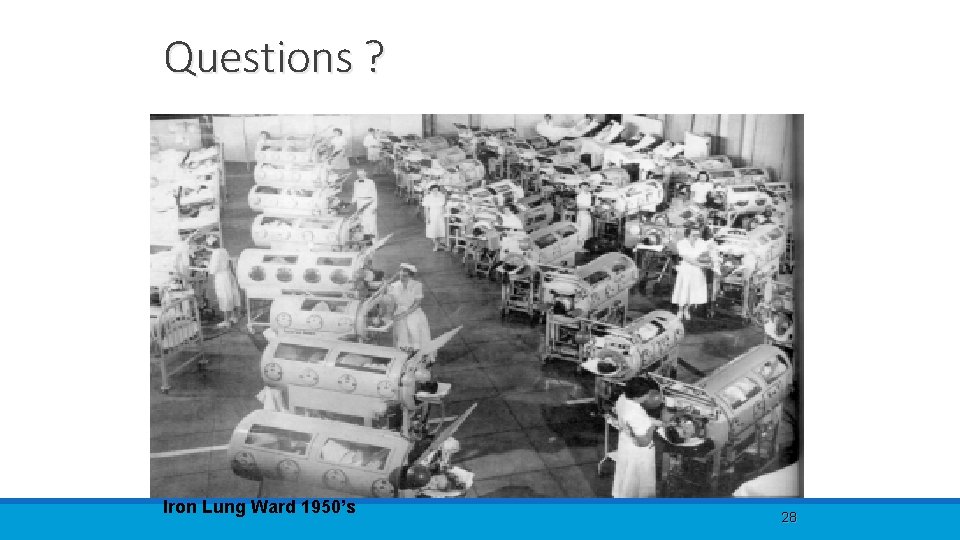
Questions ? Iron Lung Ward 1950’s 28
References Coombs et al (2013) Assessment, monitoring & interventions for the respiratory system. In Mallett, Albarron & Richardson Eds: Critical Care Manual of Clinical Procedures & Competencies. (Wiley & Sons, West Sussex) Intensive Care Foundation (2015) Handbook of Mechanical Ventilation – A Users Guide (Intensive Care Society, London) file: ///C: /Users/User/Downloads/Ventilation%20 handbook%20(1). pdf (downloaded August 2016) 29