Introduction to Health Professions Infection Control Techniques 1





- Slides: 60
Introduction to Health Professions Infection Control Techniques 1 -1

Introduction � Patients coming to the office for treatment may be more susceptible to infections � Immunizations and patient education are important methods of infection control You will be introduced to Occupational Safety and Health Administration (OSHA) guidelines, the Blood-Borne Pathogen Standard, reporting guidelines, and isolation procedures. 33 -2
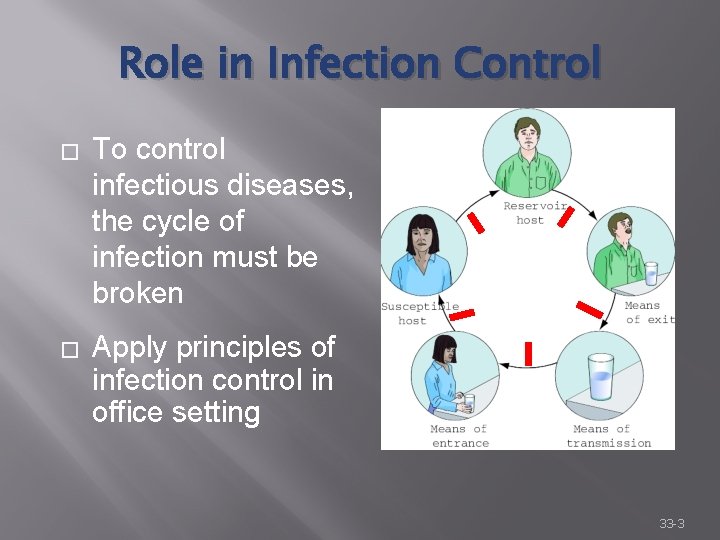
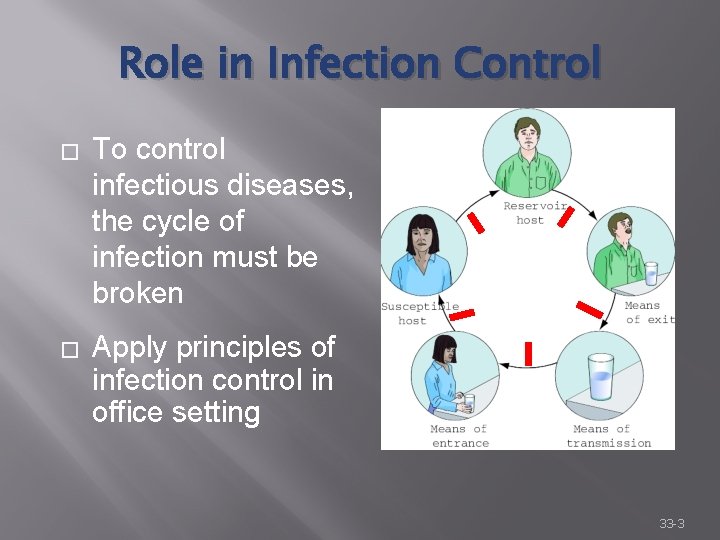
Role in Infection Control � To control infectious diseases, the cycle of infection must be broken � Apply principles of infection control in office setting 33 -3
Role in Infection Control (cont. ) � � Follow correct sanitization, disinfection, and sterilization procedures Help patients understand basic disease prevention Educate patients about immunizations Administer immunizations 33 -4
Apply Your Knowledge As a healthcare worker, what is your role in controlling infection in the medical office? ANSWER: To apply principles of infection control by following correct sanitization, disinfection, and sterilization procedures. Correct! 33 -5
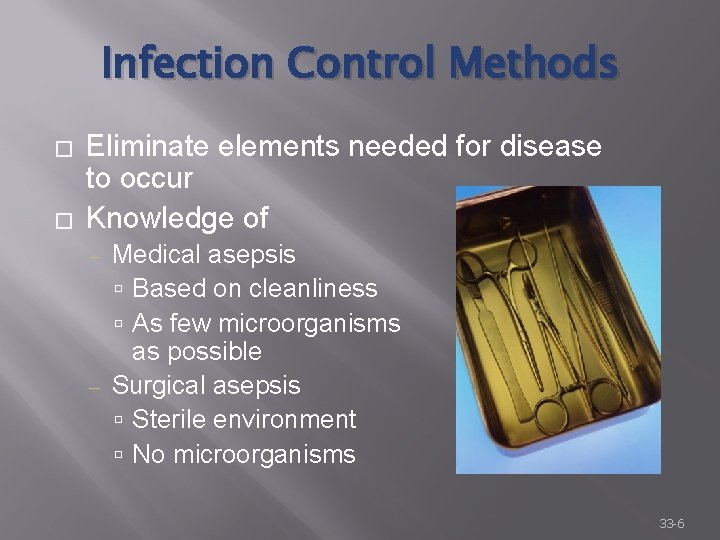
Infection Control Methods � � Eliminate elements needed for disease to occur Knowledge of Medical asepsis Based on cleanliness As few microorganisms as possible ‒ Surgical asepsis Sterile environment No microorganisms ‒ 33 -6
Medical Asepsis � Keep office clean: ‒ ‒ ‒ Reception area: sick vs. well patients Reception room clean, well lit, and ventilated Keep furniture in good repair Strict “no food or drink” policy Empty trash as necessary 33 -7
Medical Asepsis (cont. ) � During medical procedures ‒ � Prevent cross-contamination Hand washing ‒ Beginning of day ‒ After breaks ‒ Before and after each patient ‒ Before and after handling equipment or specimens ‒ After blowing your nose or coughing 33 -8
Medical Asepsis (cont. ) � Other precautions ‒ Avoid leaning against sinks, supplies, equipment ‒ Avoid touching your face and mouth ‒ Use tissues when you cough or sneeze, and always wash your hands afterward ‒ Avoid working directly with patients when you have a cold; wear gloves and mask if you must ‒ Stay home if you have a fever 33 -9
Apply Your Knowledge Describe the difference between medical and surgical asepsis. ANSWER: Medical asepsis is based on cleanliness and reducing the number of microorganisms as much as possible. Surgical asepsis is maintaining a sterile environment by eliminating all microorganisms. Good answer! 33 -10
Sanitization � Scrubbing with a brush and detergent to remove blood, mucus, and other contaminants or media where pathogens can grow � For cleaning items that touch only healthy, intact skin � OR First step in disinfection and sterilization for other equipment 33 -11
Sanitization (cont. ) � Collect items for sanitization ‒ Place in water and special detergent solution ‒ Use utility gloves ‒ Separate sharps from other equipment � Scrub items ‒ Follow manufacturers’ guidelines ‒ Dry thoroughly ‒ Examine carefully 33 -12

Sanitization (cont. ) � Rubber and plastic items � Syringes and needles – use disposable whenever possible � Ultrasonic cleaning ‒ For delicate instruments and those with moving parts ‒ Sound waves generated through a cleaning solution to loosen contaminants 33 -13

Apply Your Knowledge What is sanitation, and what types of items is it adequate for cleaning? ANSWER: Sanitation is scrubbing with a brush and detergent to remove blood, mucus, and other contaminants or media where pathogens can grow. It is adequate for cleaning items that touch only healthy, intact skin. Nice job! 33 -14
Disinfection � Adequate for instruments that do not penetrate skin or mucous membranes and surfaces not considered sterile OR � Second step in infection control prior to sterilization � Will not kill spores, certain viruses 33 -15
Disinfection (cont. ) � Using disinfectants ‒ Cleaning products applied to inanimaterials to reduce or eliminate infectious organisms Antiseptics are antiinfective cleaning agents used on human tissue ‒ Follow manufacturers’ guidelines 33 -16
Disinfection (cont. ) ‒ Factors impacting effectiveness of disinfectants Number of times solution is used Wet items – surface moisture may dilute solution Traces of soap left from sanitization – alters chemical composition Evaporation 33 -17
Disinfection (cont. ) � Choose the correct disinfectant ‒ Germicidal soap products ‒ Alcohol ‒ Acid products ‒ Formaldehyde ‒ Glutaraldehyde – “cold disinfection” ‒ Bleach ‒ Iodine and iodine compounds 33 -18

Disinfection (cont. ) � Handling disinfected supplies ‒ Prevent contamination with other surfaces ‒ Use sterile transfer forceps ‒ Wear gloves ‒ Store in clean, moisture-free environment 33 -19
Apply Your Knowledge What is the difference between a disinfectant and an antiseptic? ANSWER: Disinfectants are cleaning products applied to inanimaterials to reduce or eliminate infectious organisms. Antiseptics are anti-infective cleaning agents used on human tissue. Excellent! 33 -20
Surgical Asepsis � Goal is to keep the surgical environment completely free of all microorganisms � Used for even minor operations and injections � The more extensive the procedure, the greater the risk of infection 33 -21
Sterilization � Required for all instruments or supplies that Penetrate the skin ‒ Contact normally sterile areas of the body ‒ � Object is either sterile or not sterile ‒ � If unsure of sterility, consider it not sterile Prior to sterilization Sanitize ‒ Disinfect ‒ 33 -22
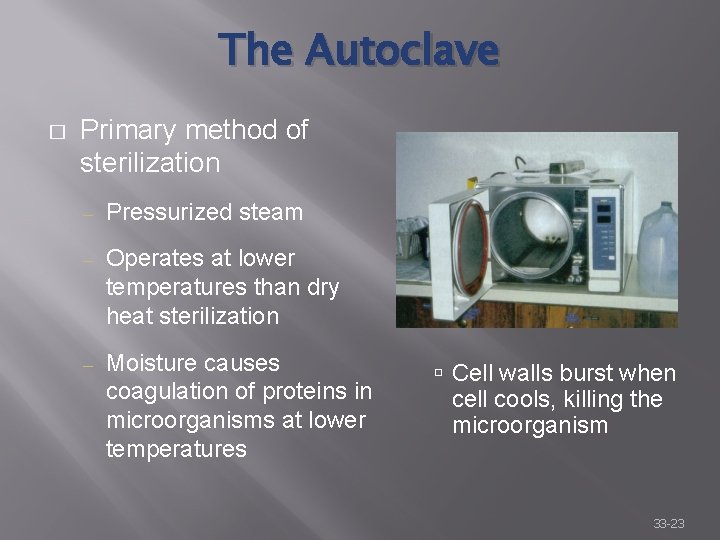
The Autoclave � Primary method of sterilization ‒ Pressurized steam ‒ Operates at lower temperatures than dry heat sterilization ‒ Moisture causes coagulation of proteins in microorganisms at lower temperatures Cell walls burst when cell cools, killing the microorganism 33 -23
The Autoclave (cont. ) � � � Wrap sanitized and disinfected items ‒ Special porous fabric, paper, or plastic ‒ Items should not touch ‒ Label Check water level – distilled water only Preheat, but do not overheat 33 -24
The Autoclave (cont. ) � Load, choose correct setting, run cycle ‒ Temperature 250°to 270°F ‒ Pressure 15 to 30 pounds � Unload � Store items properly ‒ Clean, dry location ‒ Shelf life based on packaging, but generally 30 days 33 -25
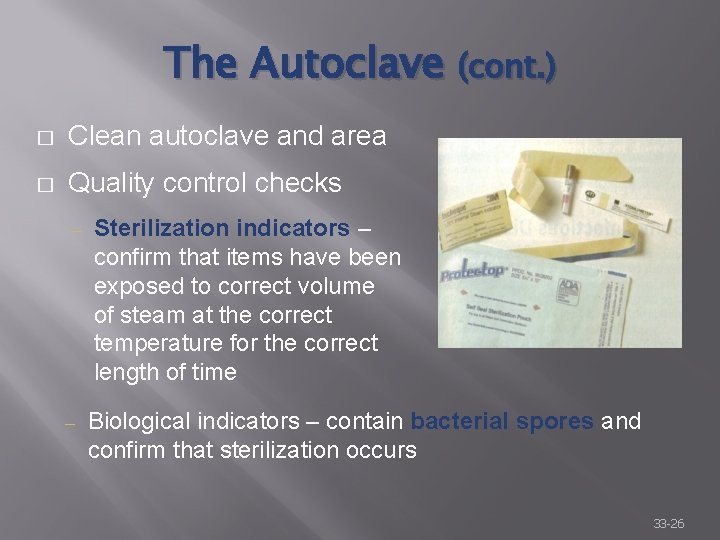
The Autoclave (cont. ) � Clean autoclave and area � Quality control checks ‒ ‒ Sterilization indicators – confirm that items have been exposed to correct volume of steam at the correct temperature for the correct length of time Biological indicators – contain bacterial spores and confirm that sterilization occurs 33 -26
The Autoclave (cont. ) � � Prevent incomplete sterilization ‒ Correct timing ‒ Adequate temperature ‒ Properly wrapped packs ‒ Adequate steam levels Timing ‒ Preset for load types ‒ Use sterilization indicators 33 -27
The Autoclave (cont. ) � Temperature ‒ Too high – steam too little moisture ‒ Too low – steam too much moisture � Do not overcrowd autoclave � Steam level ‒ If incorrect, items will not be sterile at end of cycle 33 -28
Sterile Technique � � Strict adherence to set order of procedures ‒ Sterile against sterile ‒ Clean against clean ‒ Unclean against unclean Surgical scrub 33 -29
Surgical Asepsis � During surgical procedures ‒ Do not touch sterile items without sterile gloves or transfer forceps ‒ Aseptic technique Throughout surgical procedures Caring for surgical wounds 33 -30
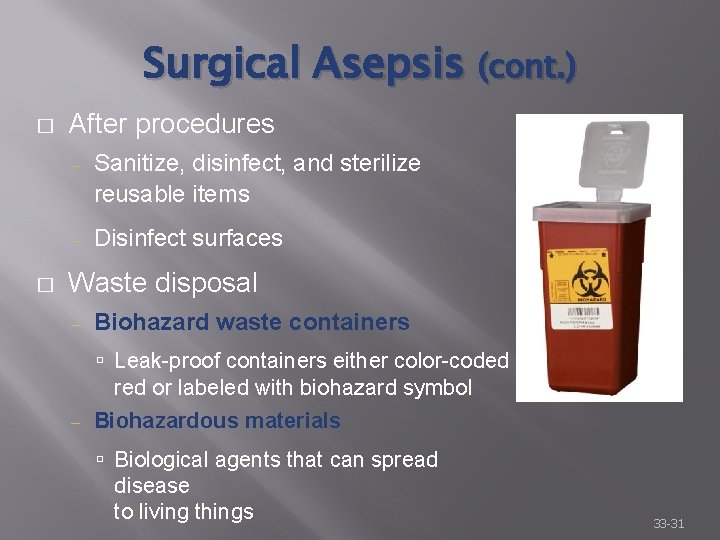
Surgical Asepsis (cont. ) � � After procedures ‒ Sanitize, disinfect, and sterilize reusable items ‒ Disinfect surfaces Waste disposal ‒ Biohazard waste containers Leak-proof containers either color-coded red or labeled with biohazard symbol ‒ Biohazardous materials Biological agents that can spread disease to living things 33 -31
Apply Your Knowledge 1. What items need to be sterilized? ANSWER: Sterilization is required for all instruments or supplies that penetrate the skin or come in contact with normally sterile areas of the body. 33 -32
Apply Your Knowledge 2. The physician is going to remove a small growth from your patient’s back. In order to prepare for this procedure, what steps would you take to prevent the spread of infection? ANSWER: Use medical asepsis while preparing the patient, and then use surgical asepsis during the procedure. Excellent! 33 -33
OSHA Guidelines � Blood-Borne Pathogen Standards ‒ Protect health-care workers from health hazards on the job ‒ Also protect patients and others who come to medical facilities ‒ Dictate how to handle or potentially wastes infectious Discarded Held for processing 33 -34
OSHA Guidelines (cont. ) � Blood-Borne Pathogen Standards ‒ Measures to prevent the spread of infection ‒ Provide a margin of safety by ensuring that medical facilities meet minimal standards for asepsis ‒ Requirements for training, keeping records, housekeeping, and personal protective gear 33 -35
OSHA Guidelines (cont. ) � Universal Precautions ‒ Prevent health-care workers from exposure to infections ‒ Assume that all blood and body fluids are infected with blood-borne pathogens 33 -36
OSHA Guidelines (cont. ) � Standard Precautions ‒ Combination of Universal Precautions and Body Substance Isolation guidelines ‒ Used in health-care facilities to prevent transmission of disease 33 -37
OSHA Guidelines (cont. ) Categories of tasks � I. Tasks that expose a worker to blood, body fluids, or tissues and require specific protective measures II. Tasks that usually do not involve risk of exposure but require precautions in certain situations III. Tasks that have no risk of exposure, so no special protection is required 33 -38
Respiratory Hygiene/Cough Etiquette � Guidelines established by CDC ‒ Education ‒ Posting signs ‒ Controlling source or transmission ‒ Proper hand hygiene ‒ Separating patients with respiratory infections from other patients 33 -39
Personal Protective Equipment � Protective gear worn to protect against physical hazards � Employers must provide PPE at no charge to the employee Disposable, sterile exam and utility gloves Masks and protective eyewear or face shields Protective clothing � � � 33 -40
Postprocedure Cleanup � Decontaminate all exposed surfaces � Replace protective coverings on surfaces or equipment � Decontaminate receptacles � Pick up any broken glass with tongs � Discard all potentially infectious waste materials 33 -41
OSHA Guidelines (cont. ) � � Apply guidelines daily on the job Exposure incidents Contact with infectious substance ‒ Rules apply to all serious infections – HIV, HBV ‒ HBV vaccine ‒ � Transmission to patients ‒ Nosocomial infection – an infection acquired by a patient in a health-care facility 33 -42
Apply Your Knowledge OSHA divides medical tasks by level of risk. What are these risk categories? ANSWER: There are three categories of risk: Category 1: Expose a worker to blood, body fluids, or tissues and require specific protective measures Category 2: Usually do not involve risk of exposure, but precautions are required in certain situations Category 3: No risk of exposure, so no special protection is required Fantastic! 33 -43

Reporting Guidelines � Certain diseases must be reported to state or county health department � Information is forwarded to the CDC – control of the spread of infection 33 -44
Reporting Guidelines (cont. ) � National Notifiable Disease Surveillance System ‒ Examples HIV/AIDS Rubella Legionellosis Mumps Tetanus Cholera Hepatitis Lyme Disease Smallpox Tuberculosis 33 -45
Apply Your Knowledge How is the information on reportable diseases used by the CDC? ANSWER: The CDC uses the information reported to them to help control the spread of infection. Good answer! 33 -46
Isolation Guidelines � CDC guidelines ‒ Types of precautions needed ‒ Patients requiring precautions � Create an environment that protects against pathogens � Standard Precautions 33 -47
Isolation Guidelines (cont. ) � Select appropriate PPE ‒ Gloves ‒ Masks, face shields, respirators ‒ Gowns 33 -48
Apply Your Knowledge Mrs. Findley brings her child with chickenpox into the medical office. What type of personal protective equipment should you use when caring for this child? ANSWER: Chickenpox requires airborne and contact precautions, so you should use gloves and a mask and goggles or a respirator. Nice! 33 -49
Immunizations � Immunization ‒ � Administration of a vaccine or toxoid to protect susceptible individuals from infectious diseases Reduces risk of infection spread ‒ Decreases the susceptibility of the host 33 -50
Immunization Recommendations � � Immunization schedules for children ‒ Advisory Committee on Immunization Practices ‒ American Academy of Pediatrics ‒ American Academy of Family Physicians Immunization schedules for adults ‒ The National Coalition of Adult Immunization (NCAI) 33 -51
Immunizations (cont. ) � When administering, you must explain ‒ The need for immunization ‒ Side effects Soreness at site Low-grade fever General malaise 33 -52
Immunizations (cont. ) � Concerns ‒ Pediatric patients Do not give if child has fever Informed consent – explain benefits and risks Contraindications – symptoms that render the use of a remedy or procedure inadvisable because of the risk Immunization records �National Childhood Vaccine Injury Act of 1988 �Instruct parents keep record as proof of immunization 33 -53
Immunizations (cont. ) ‒ Pregnant patients Avoid live virus vaccines FDA categories A, B, C, D, and X ‒ Elderly Dispel common misconception and cost concerns More likely to develop side effects 33 -54
Immunizations (cont. ) ‒ Immunocompromised patients May experience minimal to dangerous effects Adjust dosage or delay administration Must also consider immunization status of family and caregivers ‒ Health-care workers Hepatitis B vaccination offered by employer at no cost to employee 33 -55
Apply Your Knowledge What is an immunization? ANSWER: An immunization is the administration of a vaccine or toxoid to protect susceptible individuals from infectious diseases. Great! 33 -56
Preventing Disease Transmission � � Patient education ‒ Health promotion ‒ Disease prevention ‒ Disease treatment Healthcare worker role in patient education ‒ Share responsibility ‒ Reinforce and explain instructions 33 -57
Preventing Disease Transmission (cont. ) � Educate patient on ‒ Nutrition and diet ‒ Exercise and weight control ‒ Prevention of STDs ‒ Smoking cessation ‒ Alcohol and drug abuse prevention and treatment ‒ Proper use of medications and prescribed treatments ‒ Stress-reduction techniques 33 -58
Preventing Disease Transmission (cont. ) � Goal of patient education ‒ � Help patients take care of themselves Encourage patients to participate actively in their own health care 33 -59
Apply Your Knowledge What three areas should patient education focus on? What is the medical assistant’s role in patient education? ANSWER: Patient education should focus on health promotion, disease prevention, and disease treatment. The medical assistant shares responsibility with the physician and other staff members and should reinforce and explain instructions given by others. Bravo! 33 -60