Introduction to Health Assessment Interviewing History Techniques of
- Slides: 51
Introduction to Health Assessment Interviewing History Techniques of Physical Assessment
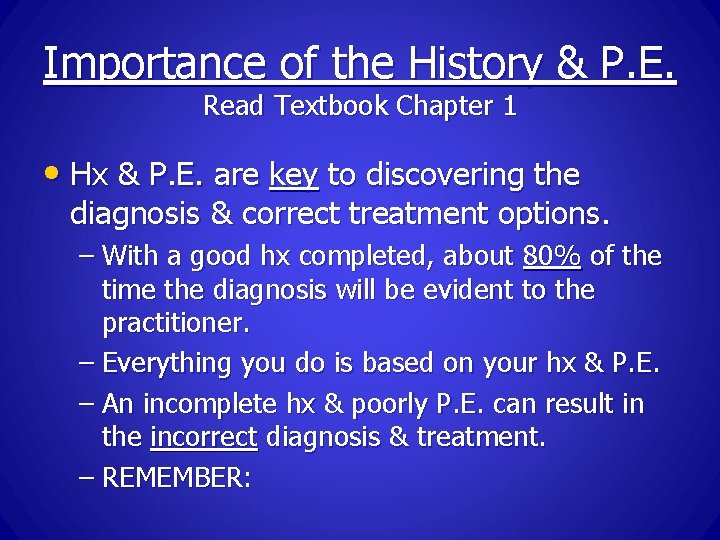
Importance of the History & P. E. Read Textbook Chapter 1 • Hx & P. E. are key to discovering the diagnosis & correct treatment options. – With a good hx completed, about 80% of the time the diagnosis will be evident to the practitioner. – Everything you do is based on your hx & P. E. – An incomplete hx & poorly P. E. can result in the incorrect diagnosis & treatment. – REMEMBER:
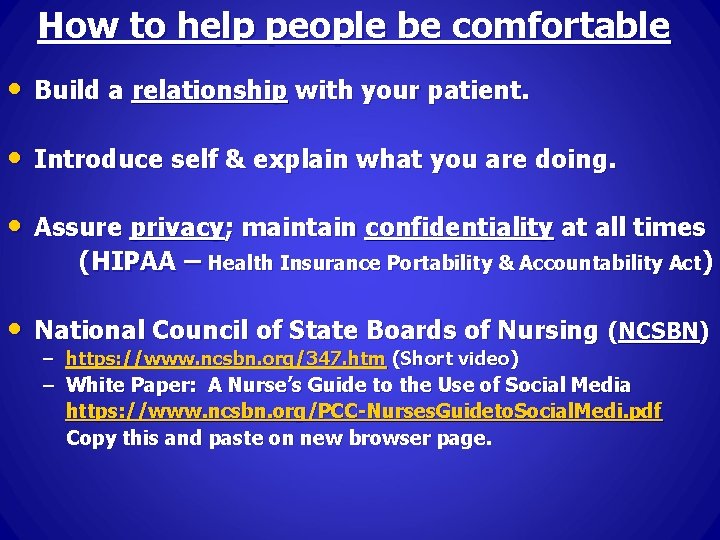
How to help people be comfortable • Build a relationship with your patient. • Introduce self & explain what you are doing. • Assure privacy; maintain confidentiality at all times (HIPAA – Health Insurance Portability & Accountability Act) • National Council of State Boards of Nursing (NCSBN) – https: //www. ncsbn. org/347. htm (Short video) – White Paper: A Nurse’s Guide to the Use of Social Media https: //www. ncsbn. org/PCC-Nurses. Guideto. Social. Medi. pdf Copy this and paste on new browser page.
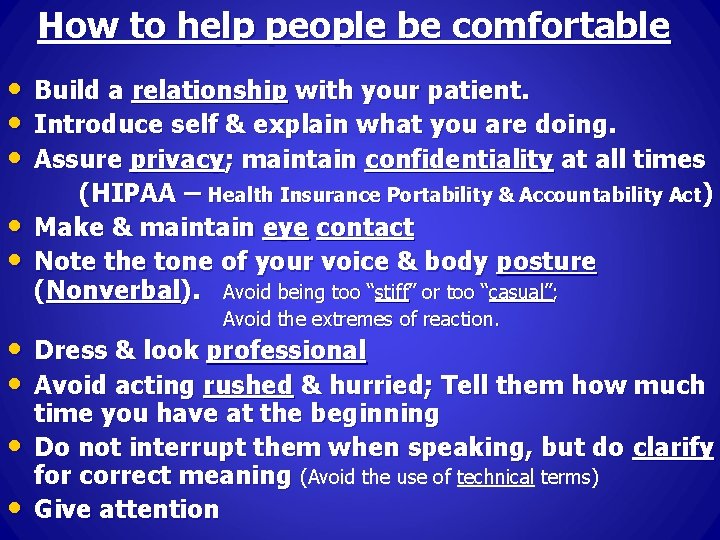
How to help people be comfortable • • • Build a relationship with your patient. Introduce self & explain what you are doing. Assure privacy; maintain confidentiality at all times (HIPAA – Health Insurance Portability & Accountability Act) Make & maintain eye contact Note the tone of your voice & body posture (Nonverbal). Avoid being too “stiff” or too “casual”; Avoid the extremes of reaction. • Dress & look professional • Avoid acting rushed & hurried; Tell them how much • • time you have at the beginning Do not interrupt them when speaking, but do clarify for correct meaning (Avoid the use of technical terms) Give attention
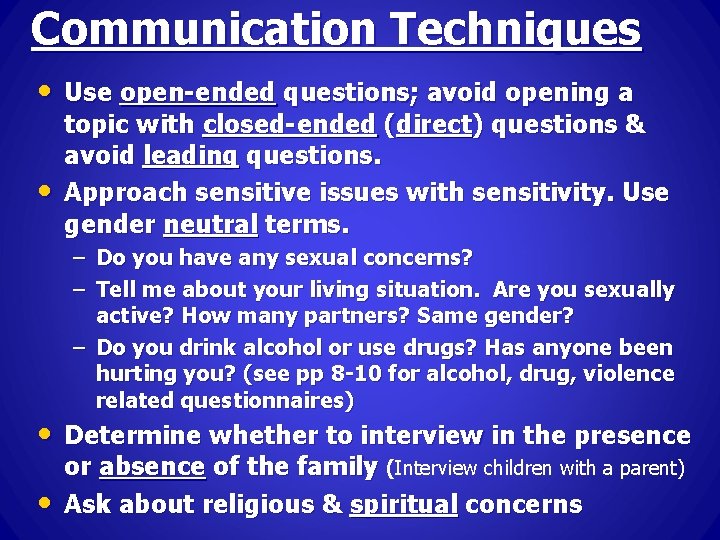
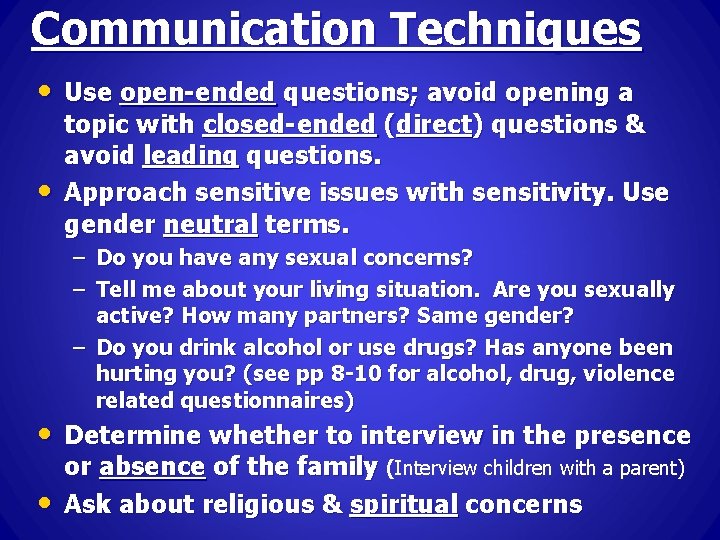
Communication Techniques • Use open-ended questions; avoid opening a • topic with closed-ended (direct) questions & avoid leading questions. Approach sensitive issues with sensitivity. Use gender neutral terms. – Do you have any sexual concerns? – Tell me about your living situation. Are you sexually active? How many partners? Same gender? – Do you drink alcohol or use drugs? Has anyone been hurting you? (see pp 8 -10 for alcohol, drug, violence related questionnaires) • Determine whether to interview in the presence • or absence of the family (Interview children with a parent) Ask about religious & spiritual concerns
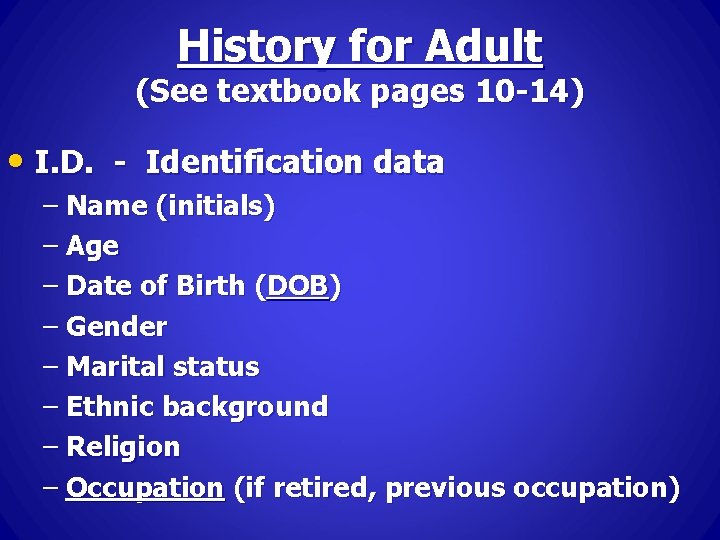
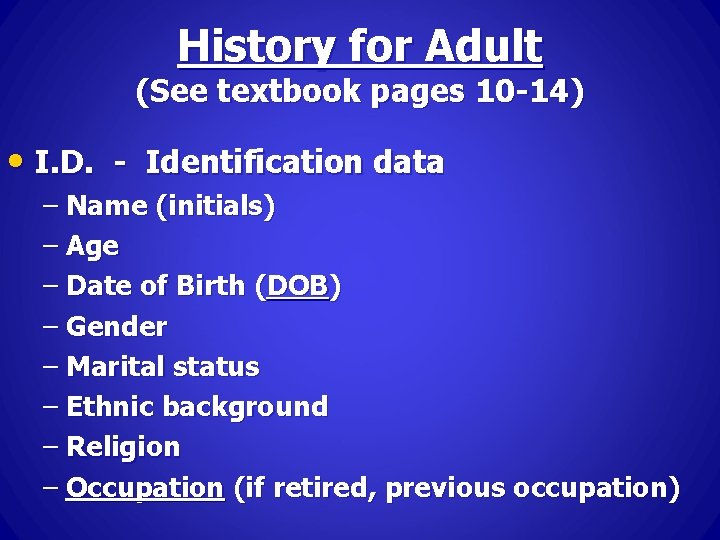
History for Adult (See textbook pages 10 -14) • I. D. - Identification data – Name (initials) – Age – Date of Birth (DOB) – Gender – Marital status – Ethnic background – Religion – Occupation (if retired, previous occupation)
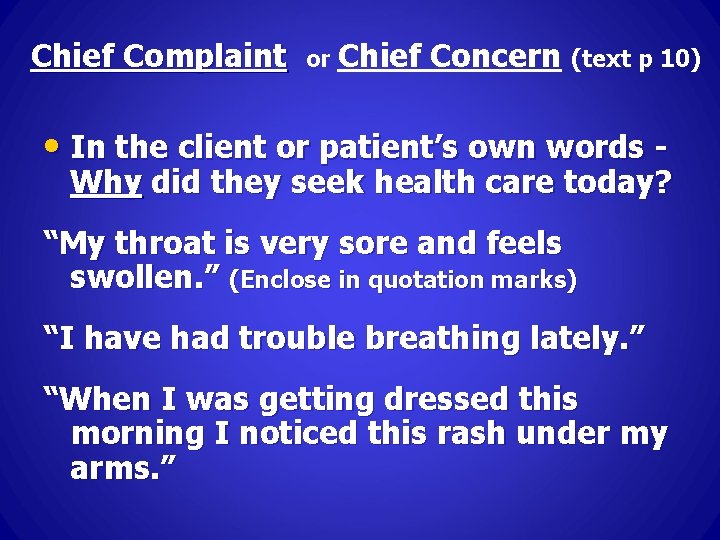
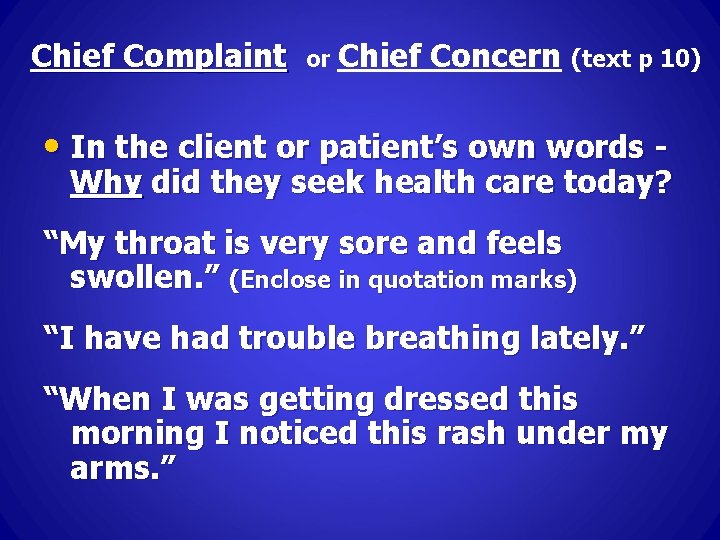
Chief Complaint or Chief Concern (text p 10) • In the client or patient’s own words - Why did they seek health care today? “My throat is very sore and feels swollen. ” (Enclose in quotation marks) “I have had trouble breathing lately. ” “When I was getting dressed this morning I noticed this rash under my arms. ”
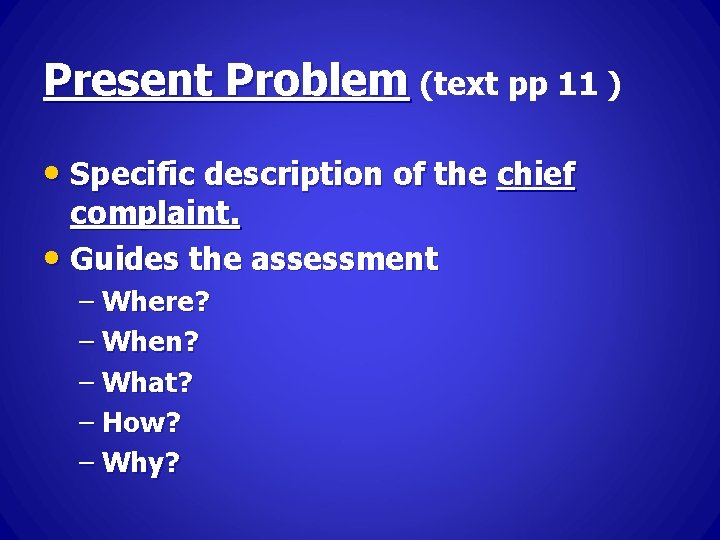
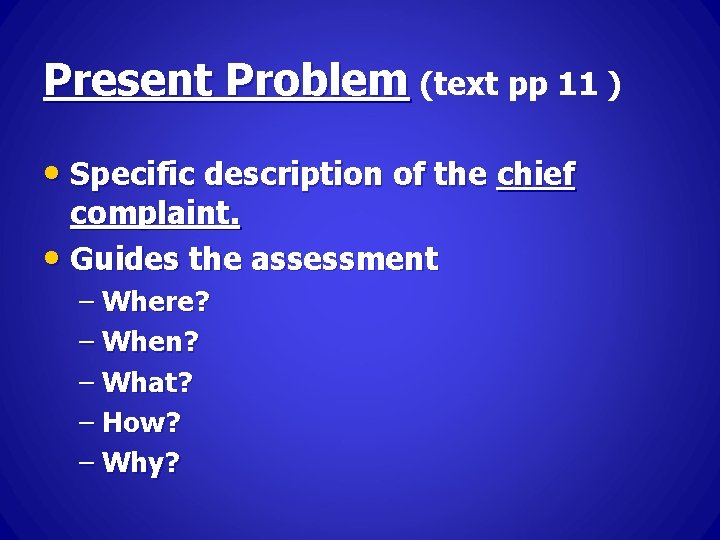
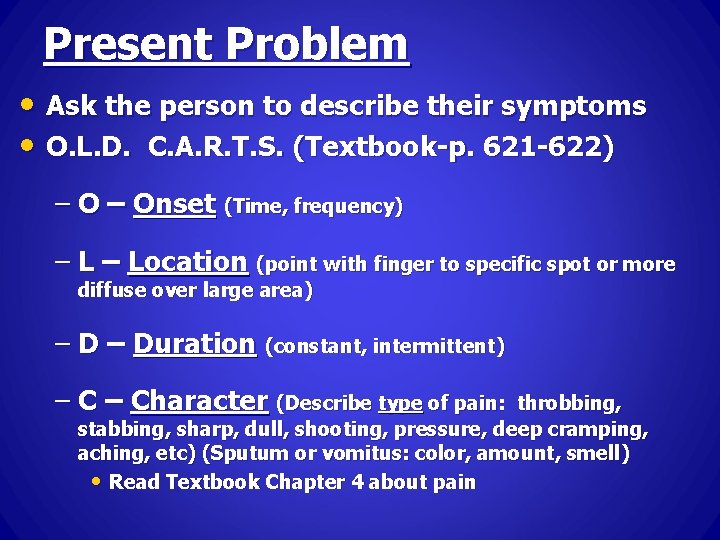
Present Problem (text pp 11 ) • Specific description of the chief complaint. • Guides the assessment – Where? – When? – What? – How? – Why?
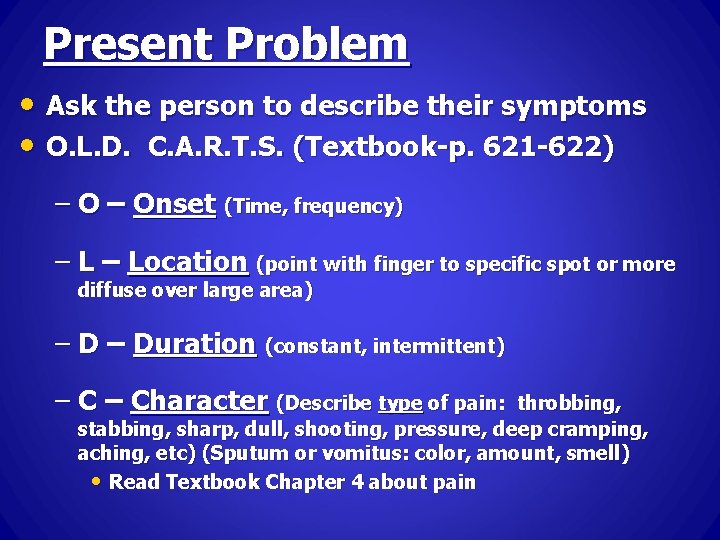
Present Problem • Ask the person to describe their symptoms • O. L. D. C. A. R. T. S. (Textbook-p. 621 -622) – Onset (Time, frequency) – Location (point with finger to specific spot or more diffuse over large area) – Duration (constant, intermittent) – Character (Describe type of pain: throbbing, stabbing, sharp, dull, shooting, pressure, deep cramping, aching, etc) (Sputum or vomitus: color, amount, smell) • Read Textbook Chapter 4 about pain
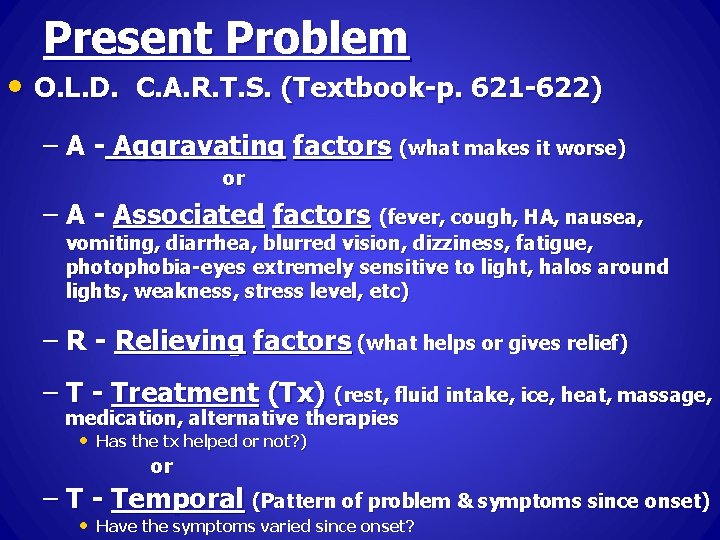
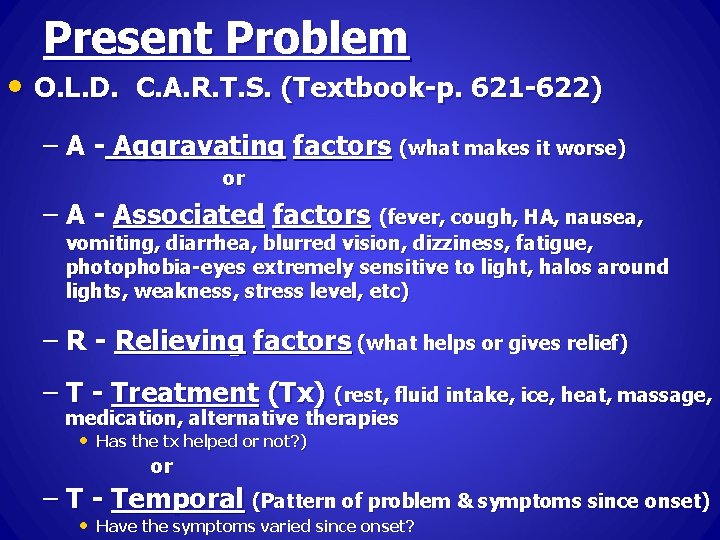
Present Problem • O. L. D. C. A. R. T. S. (Textbook-p. 621 -622) – A - Aggravating factors (what makes it worse) or – A - Associated factors (fever, cough, HA, nausea, vomiting, diarrhea, blurred vision, dizziness, fatigue, photophobia-eyes extremely sensitive to light, halos around lights, weakness, stress level, etc) – R - Relieving factors (what helps or gives relief) – T - Treatment (Tx) (rest, fluid intake, ice, heat, massage, medication, alternative therapies • Has the tx helped or not? ) or – T - Temporal (Pattern of problem & symptoms since onset) • Have the symptoms varied since onset?
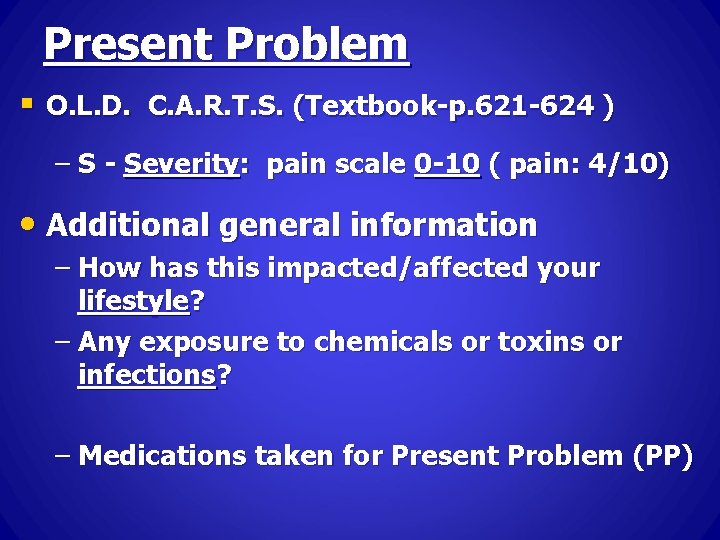
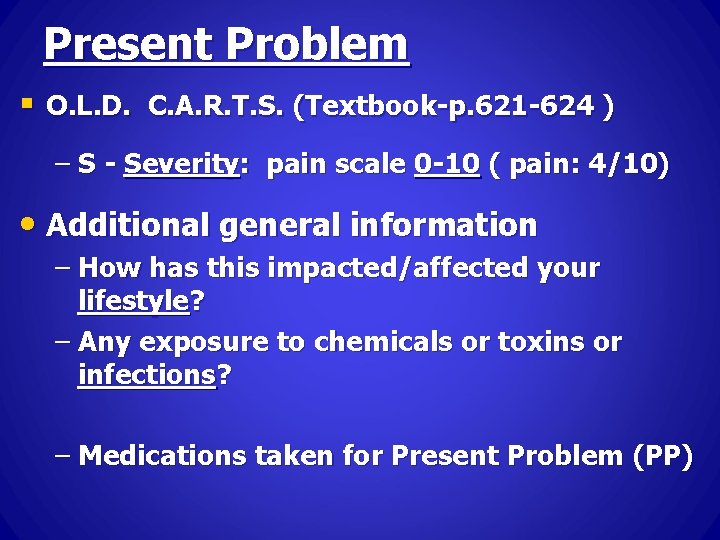
Present Problem § O. L. D. C. A. R. T. S. (Textbook-p. 621 -624 ) – S - Severity: pain scale 0 -10 ( pain: 4/10) • Additional general information – How has this impacted/affected your lifestyle? – Any exposure to chemicals or toxins or infections? – Medications taken for Present Problem (PP)
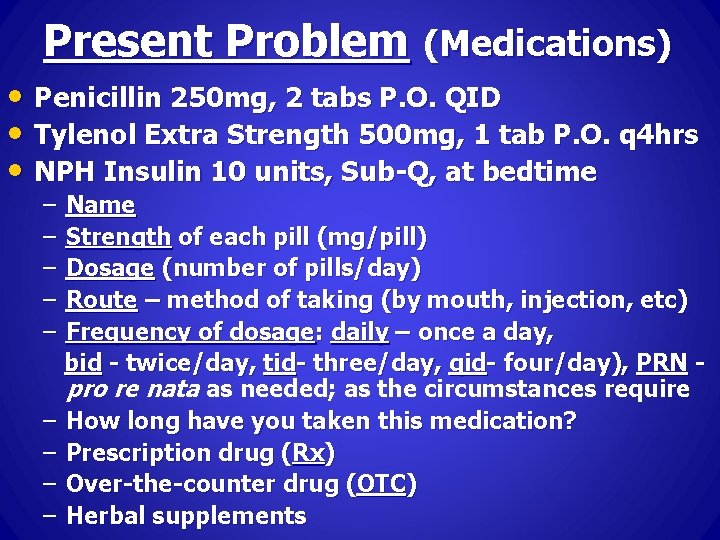
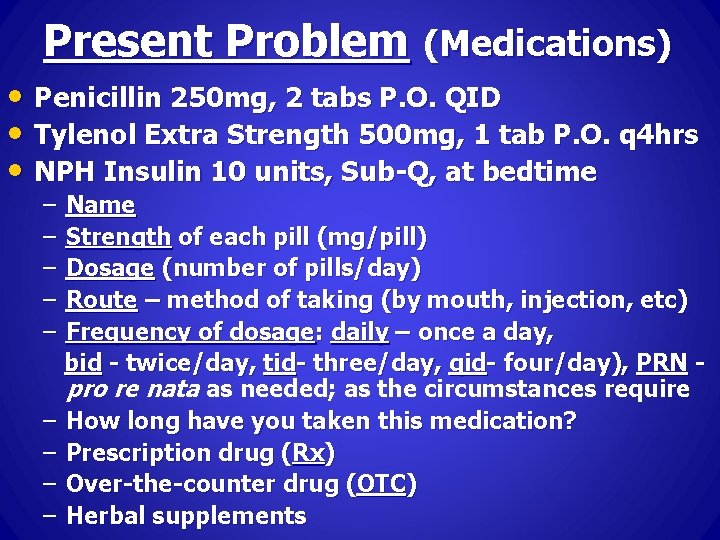
Present Problem (Medications) • Penicillin 250 mg, 2 tabs P. O. QID • Tylenol Extra Strength 500 mg, 1 tab P. O. q 4 hrs • NPH Insulin 10 units, Sub-Q, at bedtime – – – Name Strength of each pill (mg/pill) Dosage (number of pills/day) Route – method of taking (by mouth, injection, etc) Frequency of dosage: daily – once a day, bid - twice/day, tid- three/day, qid- four/day), PRN pro re nata as needed; as the circumstances require – How long have you taken this medication? – Prescription drug (Rx) – Over-the-counter drug (OTC) – Herbal supplements
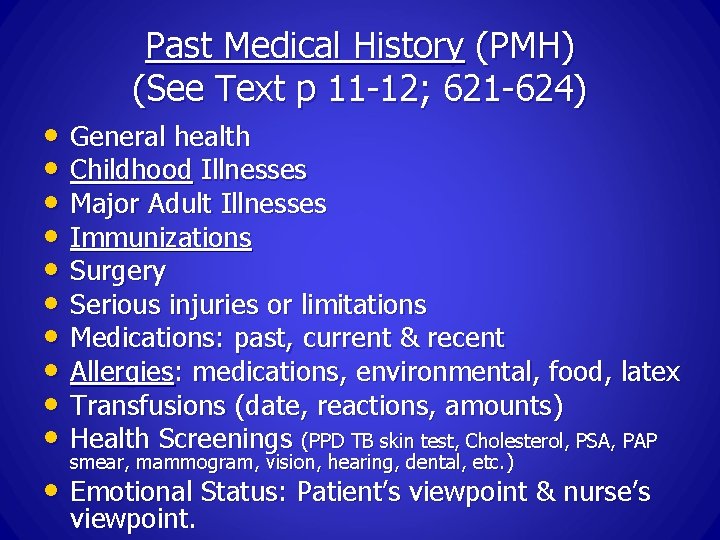
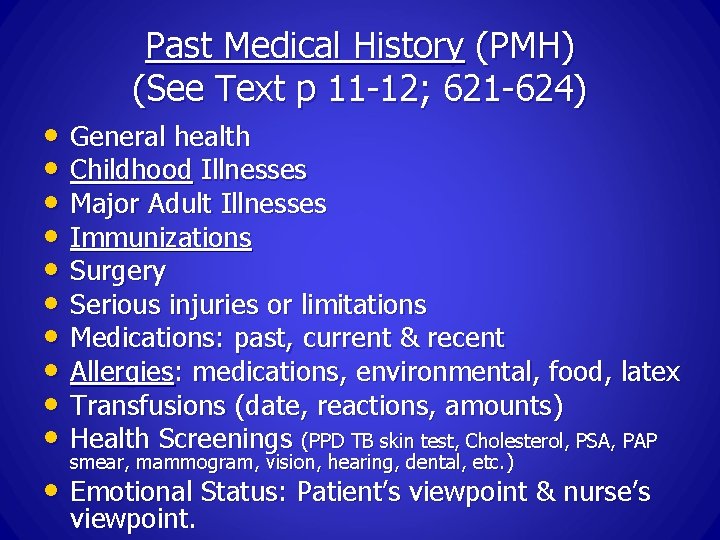
Past Medical History (PMH) (See Text p 11 -12; 621 -624) • General health • Childhood Illnesses • Major Adult Illnesses • Immunizations • Surgery • Serious injuries or limitations • Medications: past, current & recent • Allergies: medications, environmental, food, latex • Transfusions (date, reactions, amounts) • Health Screenings (PPD TB skin test, Cholesterol, PSA, PAP smear, mammogram, vision, hearing, dental, etc. ) • Emotional Status: Patient’s viewpoint & nurse’s viewpoint.
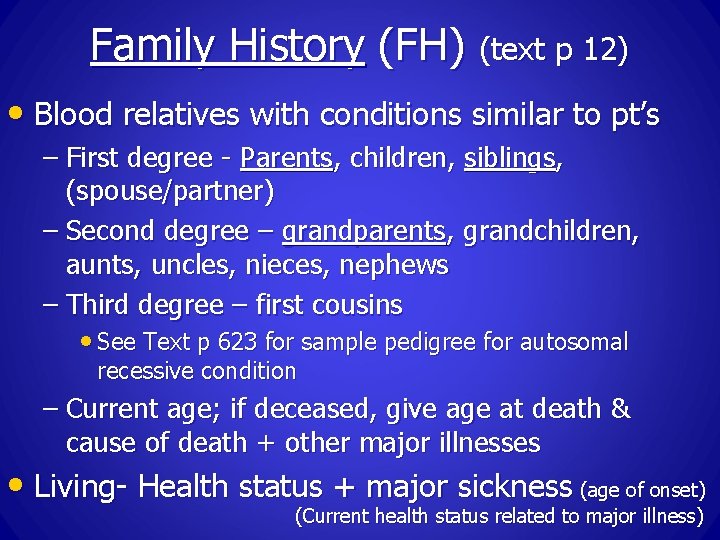
Family History (FH) (text p 12) • Blood relatives with conditions similar to pt’s – First degree - Parents, children, siblings, (spouse/partner) – Second degree – grandparents, grandchildren, aunts, uncles, nieces, nephews – Third degree – first cousins • See Text p 623 for sample pedigree for autosomal recessive condition – Current age; if deceased, give age at death & cause of death + other major illnesses • Living- Health status + major sickness (age of onset) (Current health status related to major illness)
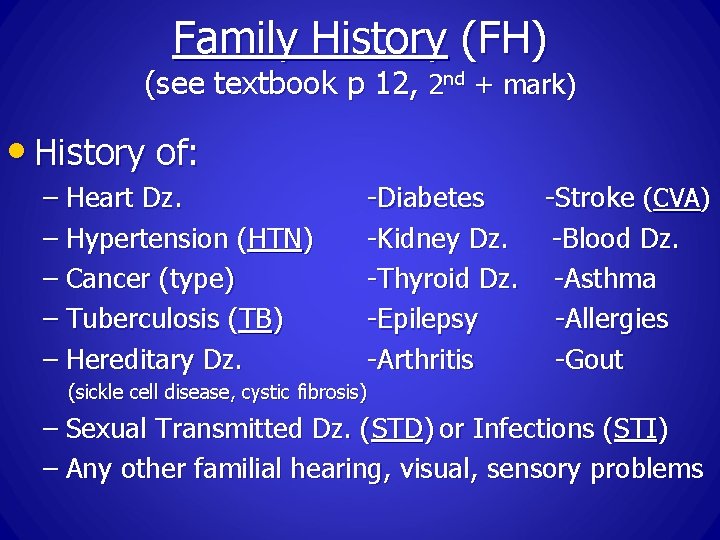
Family History (FH) (see textbook p 12, 2 nd + mark) • History of: – Heart Dz. – Hypertension (HTN) – Cancer (type) – Tuberculosis (TB) – Hereditary Dz. -Diabetes -Stroke (CVA) -Kidney Dz. -Blood Dz. -Thyroid Dz. -Asthma -Epilepsy -Allergies -Arthritis -Gout (sickle cell disease, cystic fibrosis) – Sexual Transmitted Dz. (STD) or Infections (STI) – Any other familial hearing, visual, sensory problems
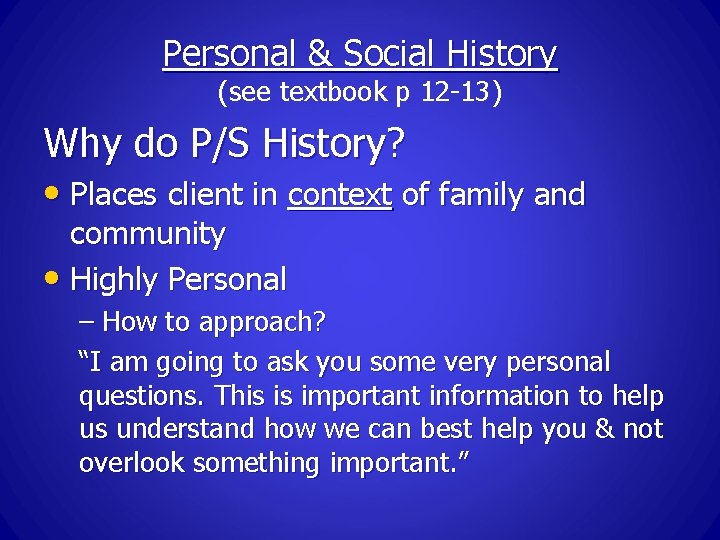
Personal & Social History (see textbook p 12 -13) Why do P/S History? • Places client in context of family and community • Highly Personal – How to approach? “I am going to ask you some very personal questions. This is important information to help us understand how we can best help you & not overlook something important. ”
Marital Status • Possible indicator of support system • Do not assume an unmarried person lacks adequate support • Close companion, Friend, Caregiver, Significant other • Life satisfaction • Stress in relationships - spouse, in-laws, etc
Education • How many years school completed? • Never make assumptions about intellectual abilities or understanding of current condition based solely on educational level • Important with any teaching
Occupation • Socioeconomic class (Patient’s words!!!) • Type of work: can give clues about work-related health hazards: Asbestos exposure, Chronic back pain, Eye strain, Sun exposure, Chemical/toxin exposure, heat/cold, stress, physical/mental strain, etc. • Military record (branch, places of service, length, known exposure to toxins, diseases, injuries) • Insurance: Health (Private/Medicare/Medicaid), Life, Disability • If unemployed are they able to pay for food, meds, healthcare, etc. ?
Living Conditions - Housing • Describe the type & size of housing • Modern Conveniences: – Heat/Air Conditioning – Running Water – Electricity – Telephone – Smoke Detectors • Stairs • # of people in house; overcrowding • Pets - indoor or outdoor; pet’s health
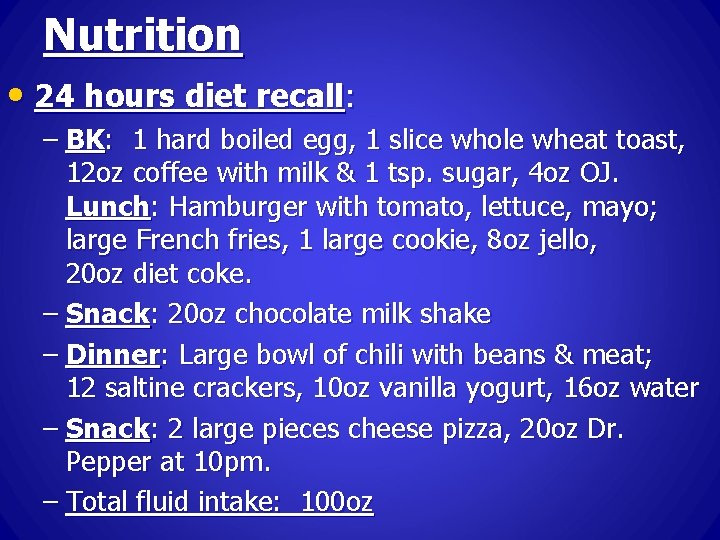
Habits: Nutrition • 24 hours diet recall: – BK: 1 hard boiled egg, 1 slice whole wheat toast, 12 oz coffee with milk & 1 tsp. sugar, 4 oz OJ. Lunch: Hamburger with tomato, lettuce, mayo; large French fries, 1 large cookie, 8 oz jello, 20 oz diet coke. – Snack: 20 oz chocolate milk shake – Dinner: Large bowl of chili with beans & meat; 12 saltine crackers, 10 oz vanilla yogurt, 16 oz water – Snack: 2 large pieces cheese pizza, 20 oz Dr. Pepper at 10 pm. – Total fluid intake: 100 oz
Habits • Nutrition – 24 hours diet recall history • Sleep Patterns • Exercise • Coffee, Tea, soft drinks, etc. – caffeine, sugar • Self-exams – BSE, TSE, skin • Alternative therapies; Home remedies; • • • supplements Recreation; Hobbies Stress Self-esteem
Cultural Background Read Textbook Chapter 2, pp 21 -29 • Ethic Group • Proscriptions – cultural or religious or food • Health beliefs & practices • Diseases common
Spirituality (Text p 10) • FICA • F = Faith, Belief, Meaning • I = Importance & Influence • C = Community • A = Address/Action in Care
Sexual History (Text p 10) • Concerns with feelings and performance • Onset & frequency of intercourse (abstinence) • Number and variety of partners • Protective measures • STD’s
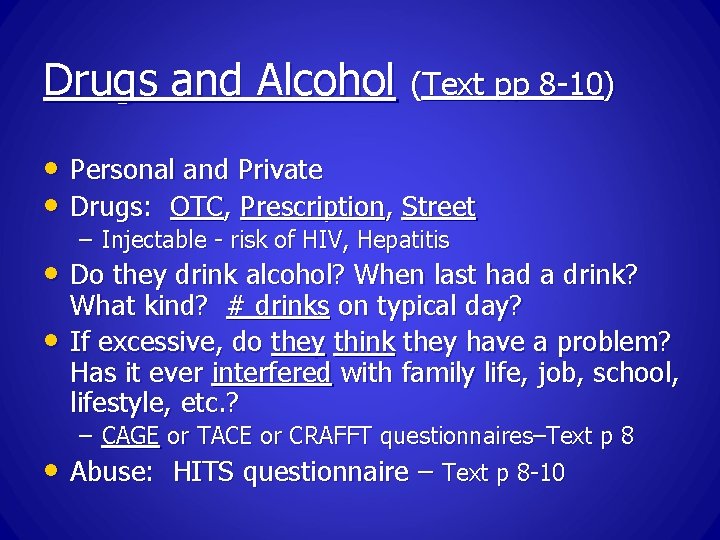
Drugs and Alcohol (Text pp 8 -10) • Personal and Private • Drugs: OTC, Prescription, Street – Injectable - risk of HIV, Hepatitis • Do they drink alcohol? When last had a drink? • • What kind? # drinks on typical day? If excessive, do they think they have a problem? Has it ever interfered with family life, job, school, lifestyle, etc. ? – CAGE or TACE or CRAFFT questionnaires–Text p 8 Abuse: HITS questionnaire – Text p 8 -10
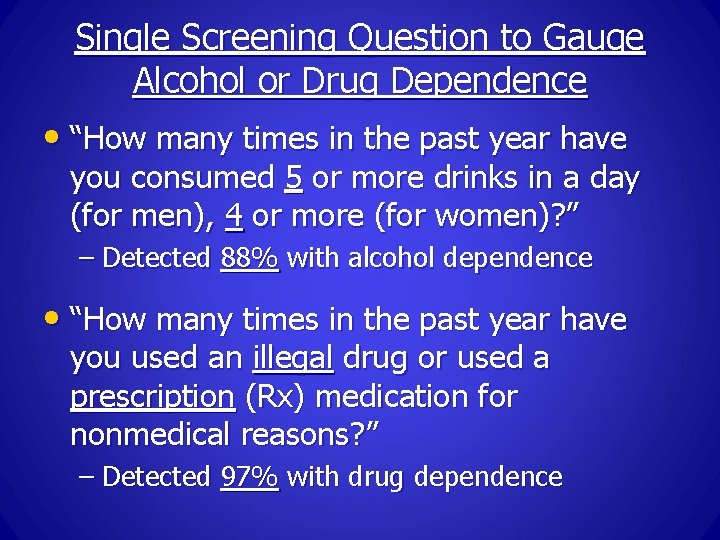
Single Screening Question to Gauge Alcohol or Drug Dependence • “How many times in the past year have you consumed 5 or more drinks in a day (for men), 4 or more (for women)? ” – Detected 88% with alcohol dependence • “How many times in the past year have you used an illegal drug or used a prescription (Rx) medication for nonmedical reasons? ” – Detected 97% with drug dependence
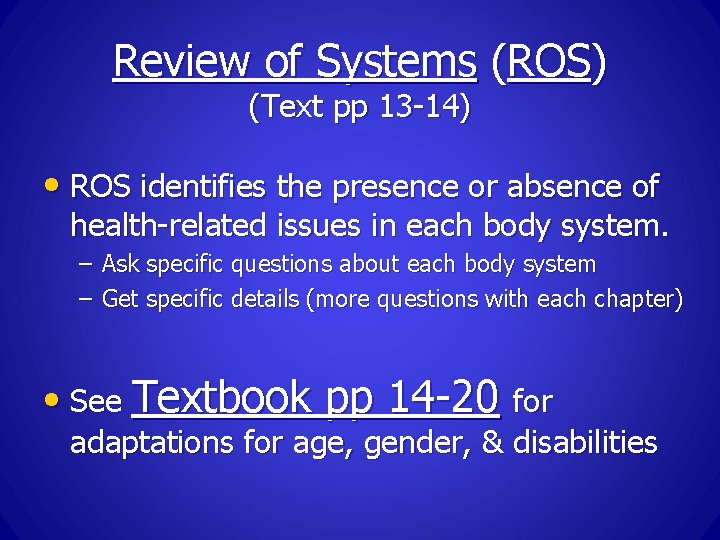
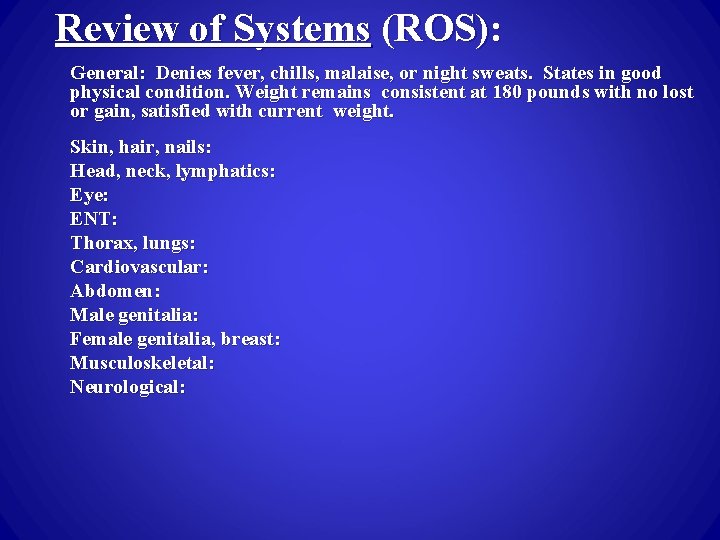
Review of Systems (ROS) (Text pp 13 -14) • ROS identifies the presence or absence of health-related issues in each body system. – Ask specific questions about each body system – Get specific details (more questions with each chapter) • See Textbook pp 14 -20 for adaptations for age, gender, & disabilities
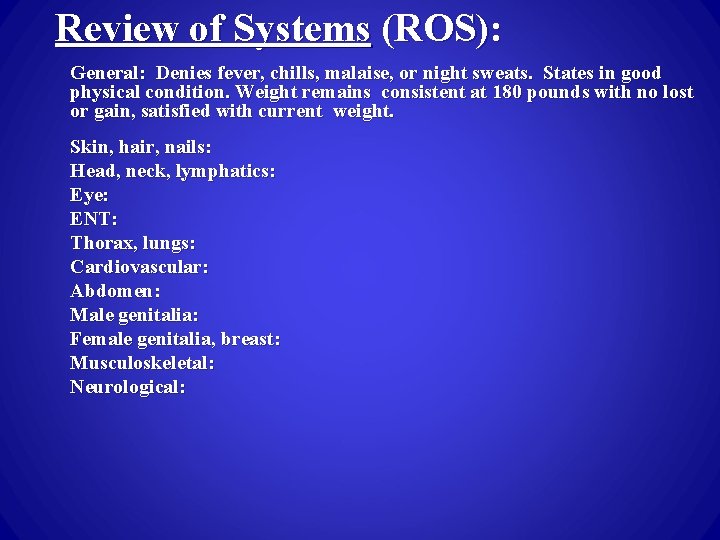
Review of Systems (ROS): General: Denies fever, chills, malaise, or night sweats. States in good physical condition. Weight remains consistent at 180 pounds with no lost or gain, satisfied with current weight. Skin, hair, nails: Head, neck, lymphatics: Eye: ENT: Thorax, lungs: Cardiovascular: Abdomen: Male genitalia: Female genitalia, breast: Musculoskeletal: Neurological:
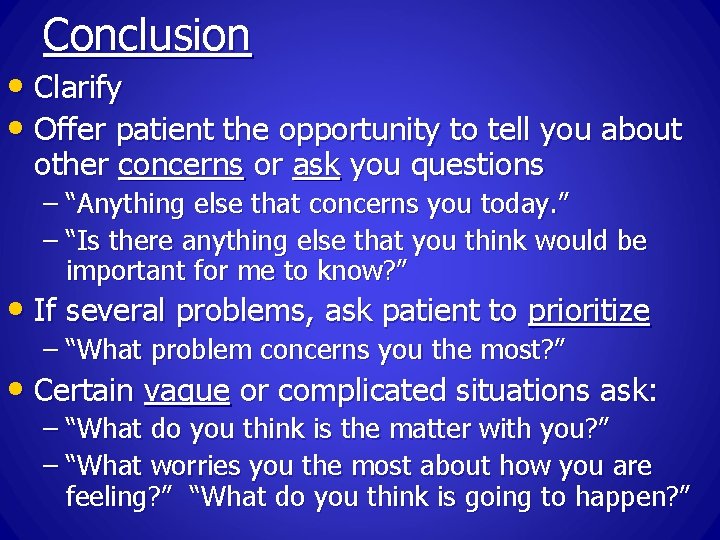
Conclusion • Clarify • Offer patient the opportunity to tell you about other concerns or ask you questions – “Anything else that concerns you today. ” – “Is there anything else that you think would be important for me to know? ” • If several problems, ask patient to prioritize – “What problem concerns you the most? ” • Certain vague or complicated situations ask: – “What do you think is the matter with you? ” – “What worries you the most about how you are feeling? ” “What do you think is going to happen? ”
N 203 Health Assessment SAMPLE HISTORY
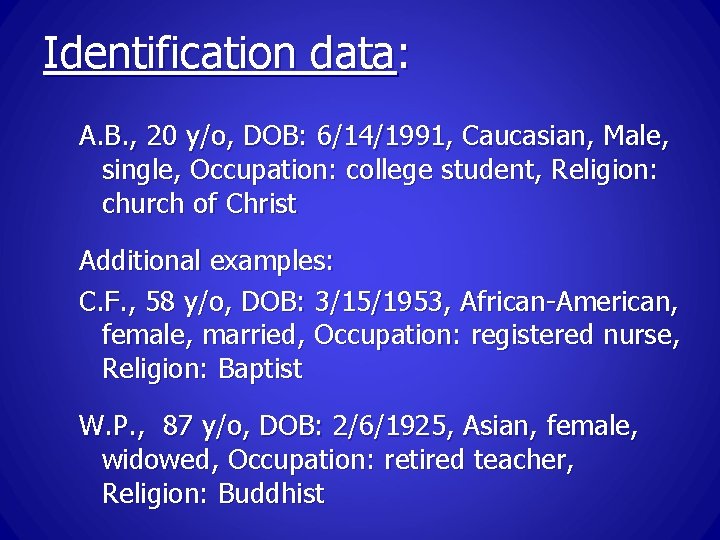
Identification data: A. B. , 20 y/o, DOB: 6/14/1991, Caucasian, Male, single, Occupation: college student, Religion: church of Christ Additional examples: C. F. , 58 y/o, DOB: 3/15/1953, African-American, female, married, Occupation: registered nurse, Religion: Baptist W. P. , 87 y/o, DOB: 2/6/1925, Asian, female, widowed, Occupation: retired teacher, Religion: Buddhist
Chief Complaint (CC) • “I have a red rash all over my body which itches like crazy. ”
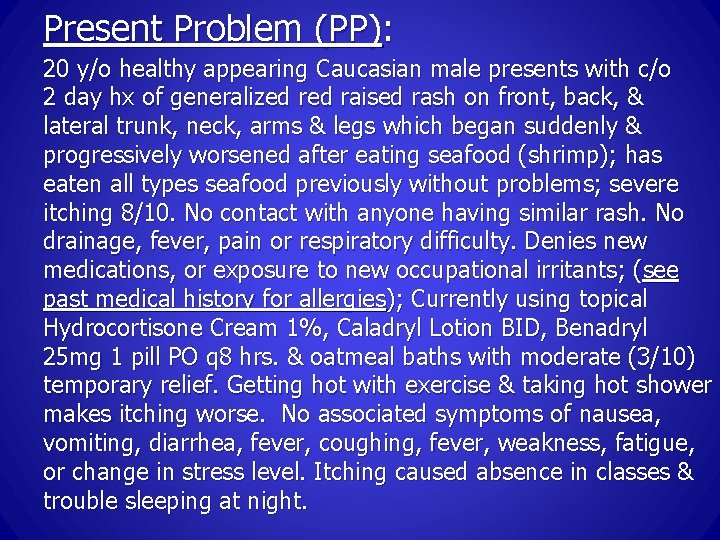
Present Problem (PP): 20 y/o healthy appearing Caucasian male presents with c/o 2 day hx of generalized raised rash on front, back, & lateral trunk, neck, arms & legs which began suddenly & progressively worsened after eating seafood (shrimp); has eaten all types seafood previously without problems; severe itching 8/10. No contact with anyone having similar rash. No drainage, fever, pain or respiratory difficulty. Denies new medications, or exposure to new occupational irritants; (see past medical history for allergies); Currently using topical Hydrocortisone Cream 1%, Caladryl Lotion BID, Benadryl 25 mg 1 pill PO q 8 hrs. & oatmeal baths with moderate (3/10) temporary relief. Getting hot with exercise & taking hot shower makes itching worse. No associated symptoms of nausea, vomiting, diarrhea, fever, coughing, fever, weakness, fatigue, or change in stress level. Itching caused absence in classes & trouble sleeping at night.
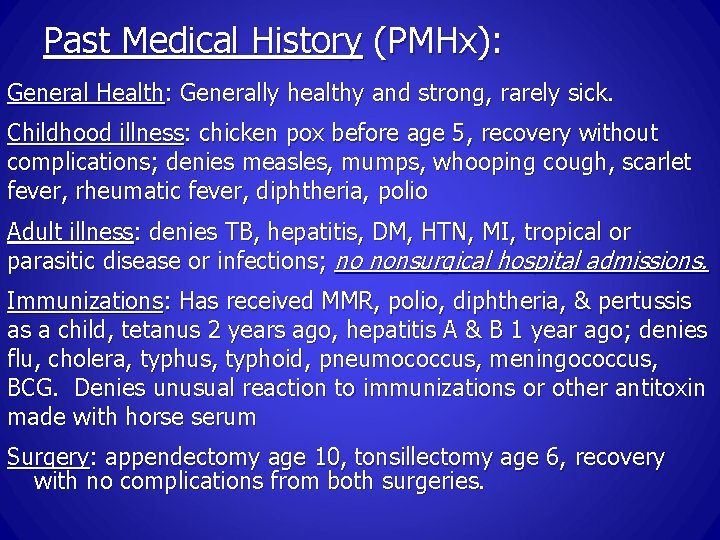
Past Medical History (PMHx): General Health: Generally healthy and strong, rarely sick. Childhood illness: chicken pox before age 5, recovery without complications; denies measles, mumps, whooping cough, scarlet fever, rheumatic fever, diphtheria, polio Adult illness: denies TB, hepatitis, DM, HTN, MI, tropical or parasitic disease or infections; no nonsurgical hospital admissions. Immunizations: Has received MMR, polio, diphtheria, & pertussis as a child, tetanus 2 years ago, hepatitis A & B 1 year ago; denies flu, cholera, typhus, typhoid, pneumococcus, meningococcus, BCG. Denies unusual reaction to immunizations or other antitoxin made with horse serum Surgery: appendectomy age 10, tonsillectomy age 6, recovery with no complications from both surgeries.
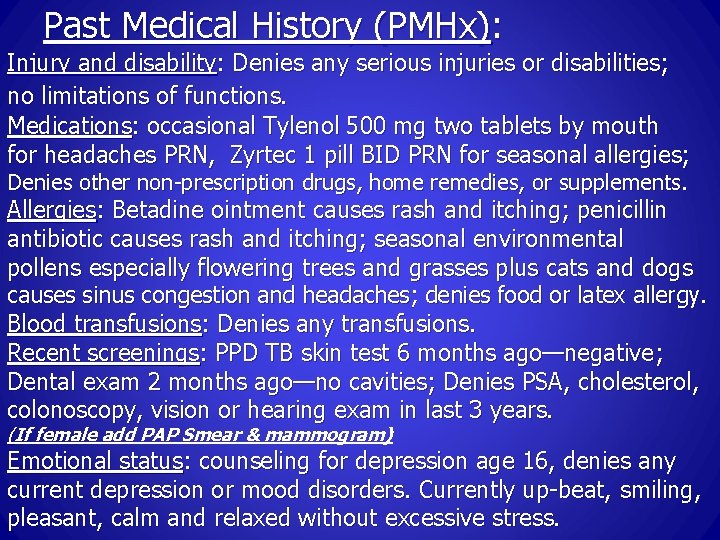
Past Medical History (PMHx): Injury and disability: Denies any serious injuries or disabilities; no limitations of functions. Medications: occasional Tylenol 500 mg two tablets by mouth for headaches PRN, Zyrtec 1 pill BID PRN for seasonal allergies; Denies other non-prescription drugs, home remedies, or supplements. Allergies: Betadine ointment causes rash and itching; penicillin antibiotic causes rash and itching; seasonal environmental pollens especially flowering trees and grasses plus cats and dogs causes sinus congestion and headaches; denies food or latex allergy. Blood transfusions: Denies any transfusions. Recent screenings: PPD TB skin test 6 months ago—negative; Dental exam 2 months ago—no cavities; Denies PSA, cholesterol, colonoscopy, vision or hearing exam in last 3 years. (If female add PAP Smear & mammogram) Emotional status: counseling for depression age 16, denies any current depression or mood disorders. Currently up-beat, smiling, pleasant, calm and relaxed without excessive stress.
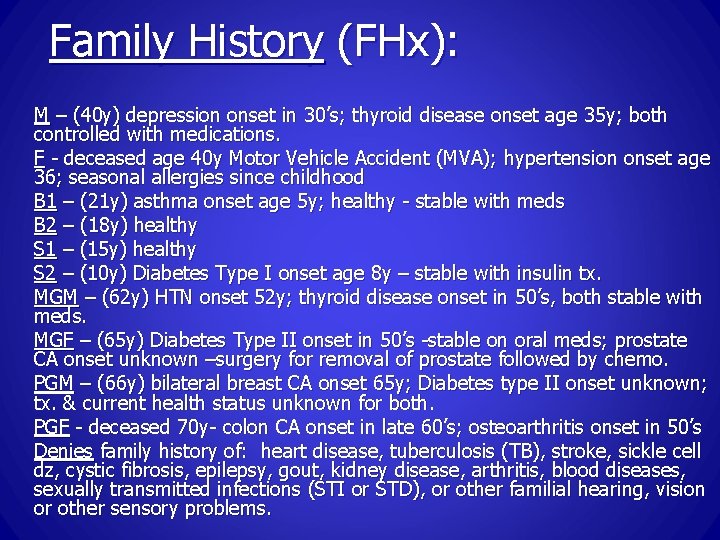
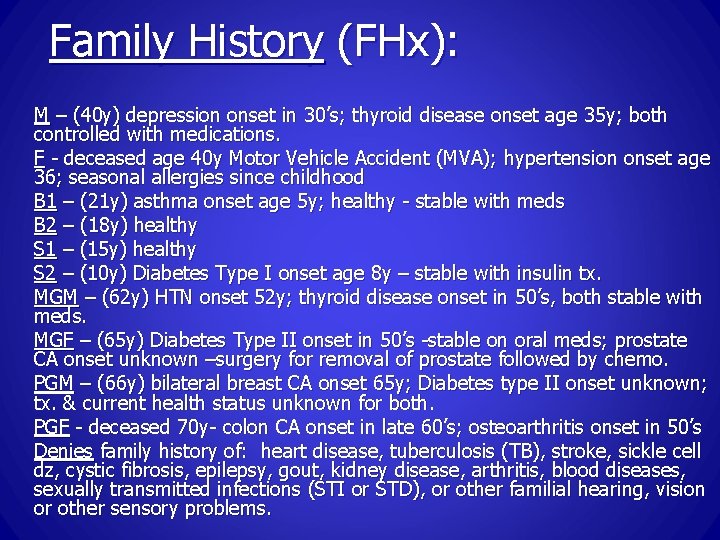
Family History (FHx): M – (40 y) depression onset in 30’s; thyroid disease onset age 35 y; both controlled with medications. F - deceased age 40 y Motor Vehicle Accident (MVA); hypertension onset age 36; seasonal allergies since childhood B 1 – (21 y) asthma onset age 5 y; healthy - stable with meds B 2 – (18 y) healthy S 1 – (15 y) healthy S 2 – (10 y) Diabetes Type I onset age 8 y – stable with insulin tx. MGM – (62 y) HTN onset 52 y; thyroid disease onset in 50’s, both stable with meds. MGF – (65 y) Diabetes Type II onset in 50’s -stable on oral meds; prostate CA onset unknown –surgery for removal of prostate followed by chemo. PGM – (66 y) bilateral breast CA onset 65 y; Diabetes type II onset unknown; tx. & current health status unknown for both. PGF - deceased 70 y- colon CA onset in late 60’s; osteoarthritis onset in 50’s Denies family history of: heart disease, tuberculosis (TB), stroke, sickle cell dz, cystic fibrosis, epilepsy, gout, kidney disease, arthritis, blood diseases, sexually transmitted infections (STI or STD), or other familial hearing, vision or other sensory problems.
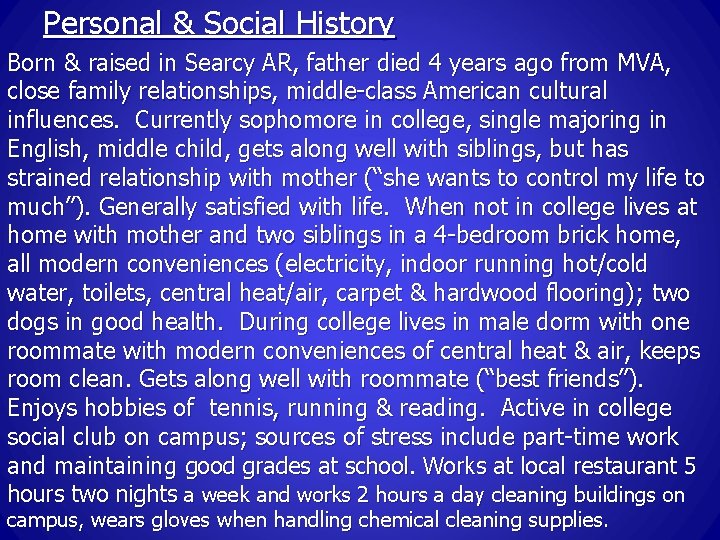
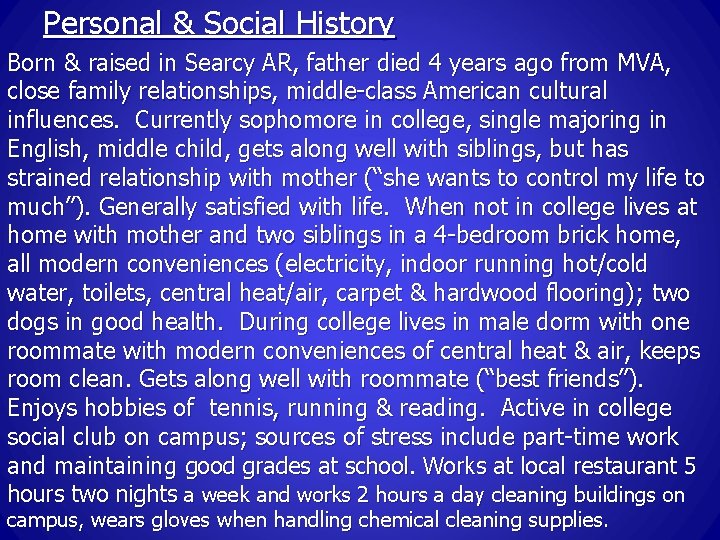
Personal & Social History Born & raised in Searcy AR, father died 4 years ago from MVA, close family relationships, middle-class American cultural influences. Currently sophomore in college, single majoring in English, middle child, gets along well with siblings, but has strained relationship with mother (“she wants to control my life to much”). Generally satisfied with life. When not in college lives at home with mother and two siblings in a 4 -bedroom brick home, all modern conveniences (electricity, indoor running hot/cold water, toilets, central heat/air, carpet & hardwood flooring); two dogs in good health. During college lives in male dorm with one roommate with modern conveniences of central heat & air, keeps room clean. Gets along well with roommate (“best friends”). Enjoys hobbies of tennis, running & reading. Active in college social club on campus; sources of stress include part-time work and maintaining good grades at school. Works at local restaurant 5 hours two nights a week and works 2 hours a day cleaning buildings on campus, wears gloves when handling chemical cleaning supplies.
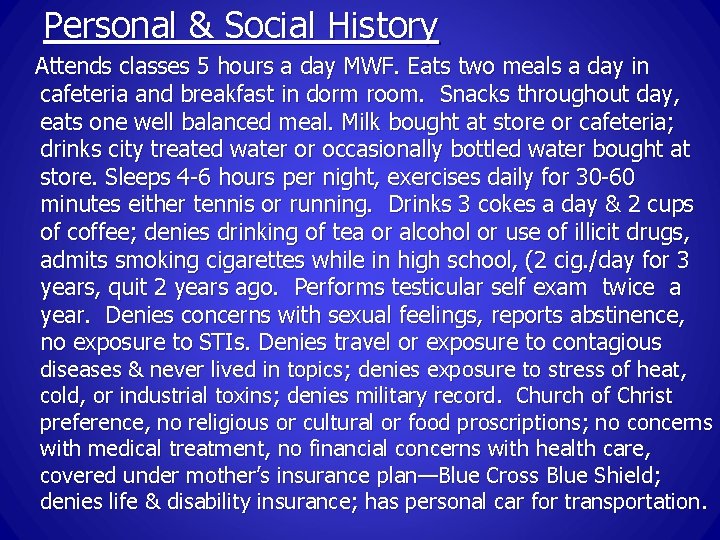
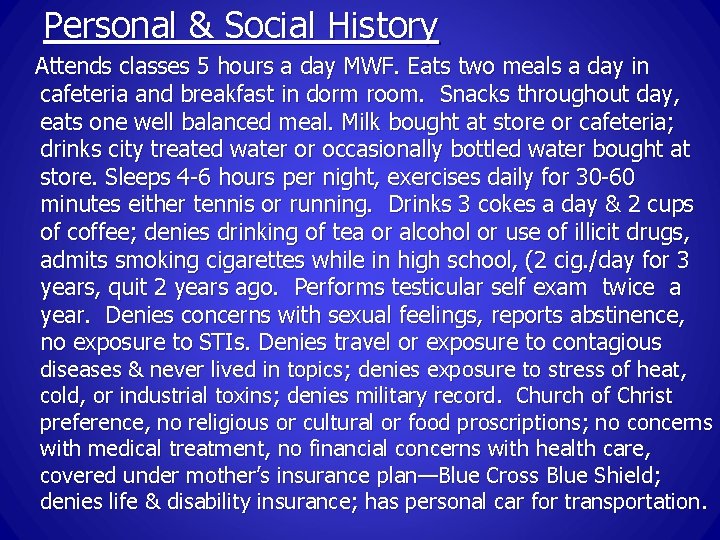
Personal & Social History Attends classes 5 hours a day MWF. Eats two meals a day in cafeteria and breakfast in dorm room. Snacks throughout day, eats one well balanced meal. Milk bought at store or cafeteria; drinks city treated water or occasionally bottled water bought at store. Sleeps 4 -6 hours per night, exercises daily for 30 -60 minutes either tennis or running. Drinks 3 cokes a day & 2 cups of coffee; denies drinking of tea or alcohol or use of illicit drugs, admits smoking cigarettes while in high school, (2 cig. /day for 3 years, quit 2 years ago. Performs testicular self exam twice a year. Denies concerns with sexual feelings, reports abstinence, no exposure to STIs. Denies travel or exposure to contagious diseases & never lived in topics; denies exposure to stress of heat, cold, or industrial toxins; denies military record. Church of Christ preference, no religious or cultural or food proscriptions; no concerns with medical treatment, no financial concerns with health care, covered under mother’s insurance plan—Blue Cross Blue Shield; denies life & disability insurance; has personal car for transportation.
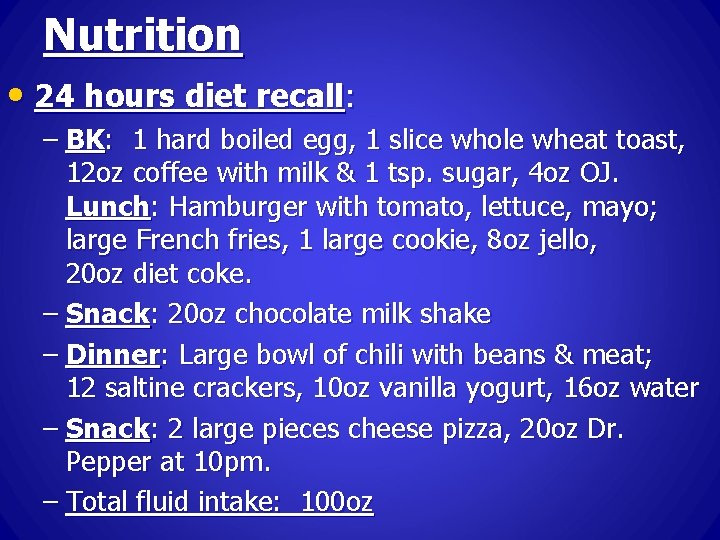
Nutrition • 24 hours diet recall: – BK: 1 hard boiled egg, 1 slice whole wheat toast, 12 oz coffee with milk & 1 tsp. sugar, 4 oz OJ. Lunch: Hamburger with tomato, lettuce, mayo; large French fries, 1 large cookie, 8 oz jello, 20 oz diet coke. – Snack: 20 oz chocolate milk shake – Dinner: Large bowl of chili with beans & meat; 12 saltine crackers, 10 oz vanilla yogurt, 16 oz water – Snack: 2 large pieces cheese pizza, 20 oz Dr. Pepper at 10 pm. – Total fluid intake: 100 oz
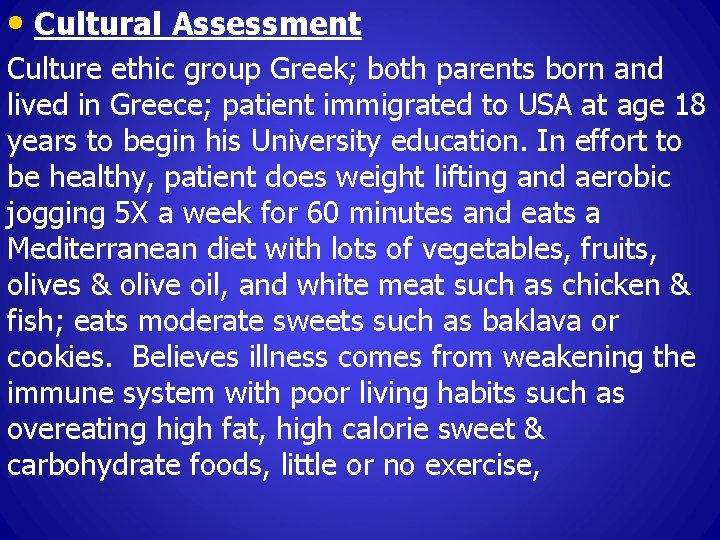
• Cultural Assessment Culture ethic group Greek; both parents born and lived in Greece; patient immigrated to USA at age 18 years to begin his University education. In effort to be healthy, patient does weight lifting and aerobic jogging 5 X a week for 60 minutes and eats a Mediterranean diet with lots of vegetables, fruits, olives & olive oil, and white meat such as chicken & fish; eats moderate sweets such as baklava or cookies. Believes illness comes from weakening the immune system with poor living habits such as overeating high fat, high calorie sweet & carbohydrate foods, little or no exercise,
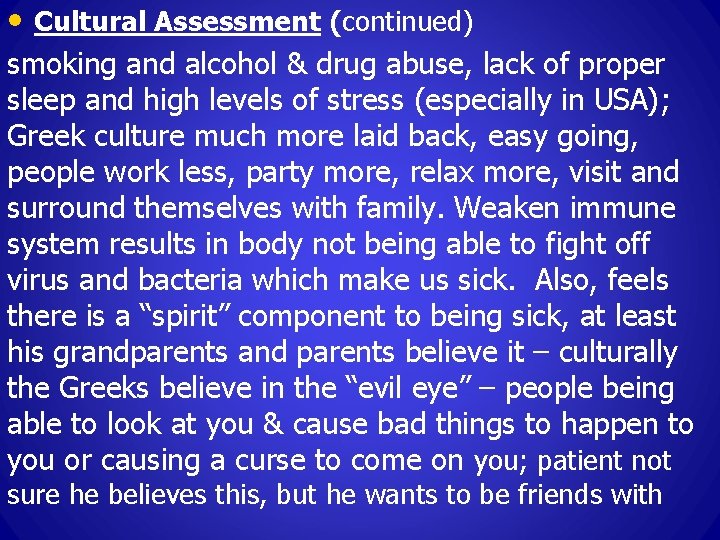
• Cultural Assessment (continued) smoking and alcohol & drug abuse, lack of proper sleep and high levels of stress (especially in USA); Greek culture much more laid back, easy going, people work less, party more, relax more, visit and surround themselves with family. Weaken immune system results in body not being able to fight off virus and bacteria which make us sick. Also, feels there is a “spirit” component to being sick, at least his grandparents and parents believe it – culturally the Greeks believe in the “evil eye” – people being able to look at you & cause bad things to happen to you or causing a curse to come on you; patient not sure he believes this, but he wants to be friends with
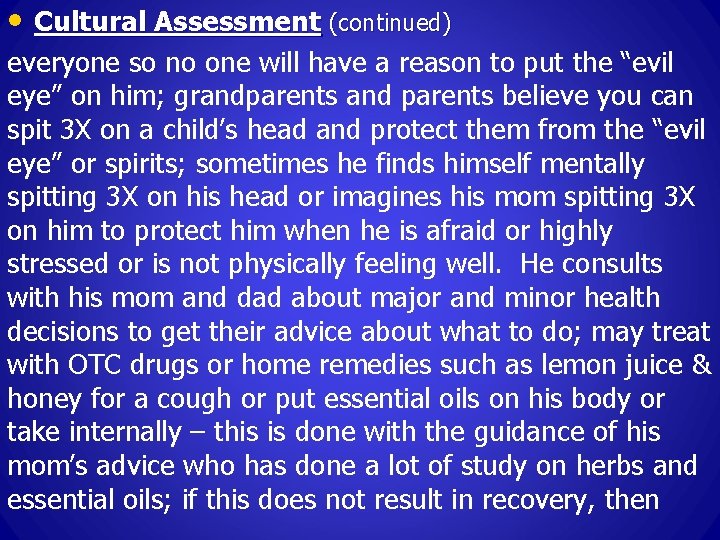
• Cultural Assessment (continued) everyone so no one will have a reason to put the “evil eye” on him; grandparents and parents believe you can spit 3 X on a child’s head and protect them from the “evil eye” or spirits; sometimes he finds himself mentally spitting 3 X on his head or imagines his mom spitting 3 X on him to protect him when he is afraid or highly stressed or is not physically feeling well. He consults with his mom and dad about major and minor health decisions to get their advice about what to do; may treat with OTC drugs or home remedies such as lemon juice & honey for a cough or put essential oils on his body or take internally – this is done with the guidance of his mom’s advice who has done a lot of study on herbs and essential oils; if this does not result in recovery, then
• Cultural Assessment (continued) goes to University health center to see nurses or to a local Family Practice doctor. Family very supportive during illness by calling, emailing, & texting daily to check on him; also has many friends on campus to encourage & do things for him when sick – especially club brothers from his social club. When sick he want healthcare providers to be compassionate & understanding & kind in providing high quality health care for him; but also want them to seek higher power intervention by praying to God for him & helping him have a Bible to read; if hospitalized - arranging a time for friends to come to visit & worship with him would be very encouraging.
• Spiritual Assessment Sees himself as a spiritual & religious person; has been raised to believe in God as the Creator & sustainer of this world & everything in it, including people; was taken to church by his parents at least once a month & sometimes more – always went to church on Christmas & Easter for the special worship services in the Greek Orthodox Church – would take communion on those special occasions also. Prayer & meditation help him deal with stress, helping him to remember he has a God who cares & has promised to be with him in all things; also stress reduced by being willing to forgive & promised to be with him in all things; also stress reduced by being
• Spiritual Assessment (continued) willing to forgive & not hold anger or grudges against others & not to seek revenge when he has been mistreated or wronged. His Faith helps give him courage & strength for each day, showing him how to treat others & care for others. The Bible says the “human body is the temple of God & that God dwells within us”. Therefore, he wants to take good care of his body & mind so that God’s temple (his body) will be as good as possible (like you want your house or room clean or your clothes clean & nice when someone important is coming to visit you). Patient believes prayer is important in his recovery
• Spiritual Assessment (continued) from illness. Medication, rest, good food, exercise etc. is great & important but prayer invites God’s spirit & power to work within you & cause these things to take on a special healing power by causing these to benefit your body; God can also heal you supernaturally, if he thinks it best; we should always pray that God’s will be done because he knows better than us. No religious proscriptions identified concerning foods, medical care or spiritual needs; however he feels staying away for real fatty foods, excess carbohydrates & sweets is one of the best things to do to help your health
• Spiritual Assessment (continued) in general – that is why he eats a Mediterranean diet – as best as he can considering having to take all his meals in the University cafeteria. No Greek Orthodox Church close (about 50 miles away) – he has visited there 2 X in the past two years – at Easter; at Christmas attended home church in Greece while visiting family; has visited many times with friends to local churches of Christ (almost every Sunday) & attends many devotionals on campus; worship here much different than in Greece Orthodox Church where the priest is in charge of all the worship activities & you just listen & respond at
• Spiritual Assessment (continued) the right times as the liturgy demands; he likes the way there is interaction & participation by the people in the Protestant church worship services; has been having Bible studies with friends in the dorm & sees there are lots of things he never knew or considered before; this is exciting to him & he loves getting to know more about God & how he has such a great plan of salvation for people to enjoy. His family really loves him – Greek families are big & loud & really care for each other – they fight sometimes, but in the end they still love & want the best for each other; also his many friends, both male & female at the university, are
• Spiritual Assessment (continued) such an encouragement & support to him when healthy or ill; people at the churches in town are really caring also – have invited him into their homes for meals, devotionals – if he really needed sometime important he feels he could go to one or two of them. He wants healthcare providers to do their jobs really well when he is sick so he can get well quickly – diagnosis his sickness quickly, give him the correct treatment or medications whether at home or in the hospital; but also wants them as people of spiritual faith to pray & ask God to bless their efforts so that healing can occur. Believes all healing ultimately come from God. Jerry Myhan, APRN