Introduction to Haemodialysis and HDF Anna Drinkwater UHNS


![Dialysis Adequacy Ø Urea Reduction Ratio (URR) [aim for URR > 65%] Ø Kt/v Dialysis Adequacy Ø Urea Reduction Ratio (URR) [aim for URR > 65%] Ø Kt/v](https://slidetodoc.com/presentation_image/e38d9e0f5051492737d4a08aab64e126/image-15.jpg)

- Slides: 35
Introduction to Haemodialysis and HDF Anna Drinkwater UHNS

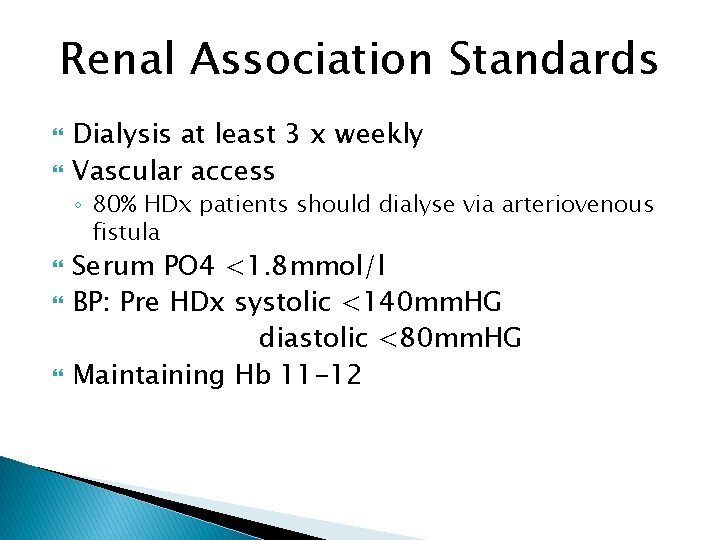
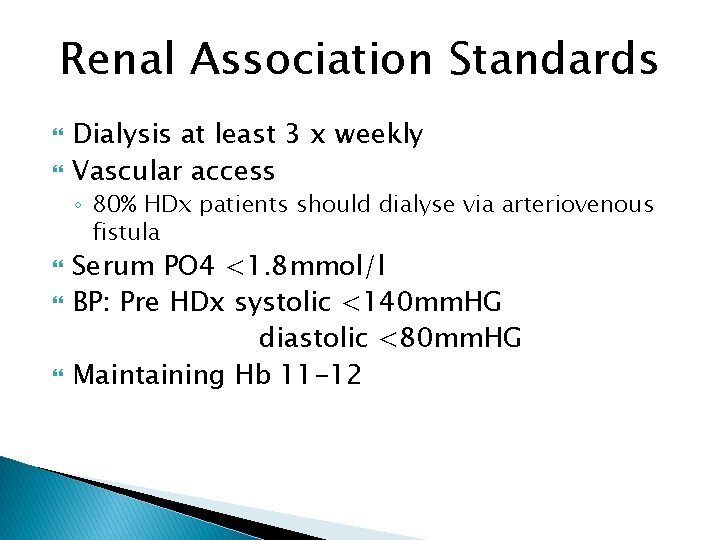
Renal Association Standards Dialysis at least 3 x weekly Vascular access ◦ 80% HDx patients should dialyse via arteriovenous fistula Serum PO 4 <1. 8 mmol/l BP: Pre HDx systolic <140 mm. HG diastolic <80 mm. HG Maintaining Hb 11 -12
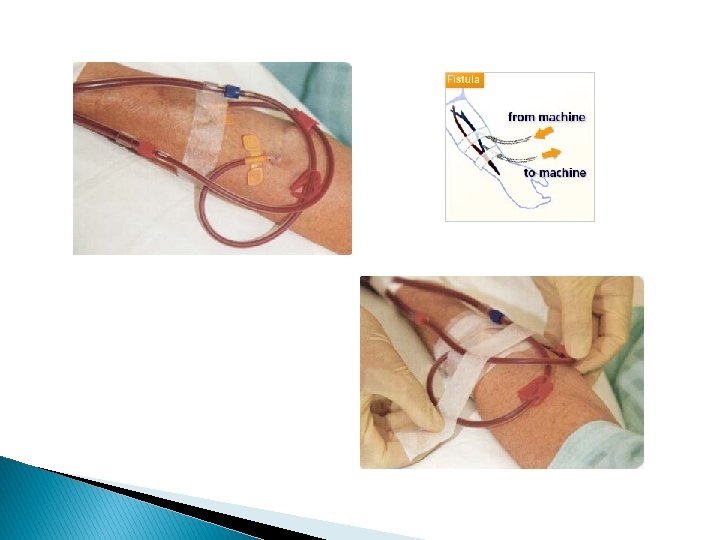
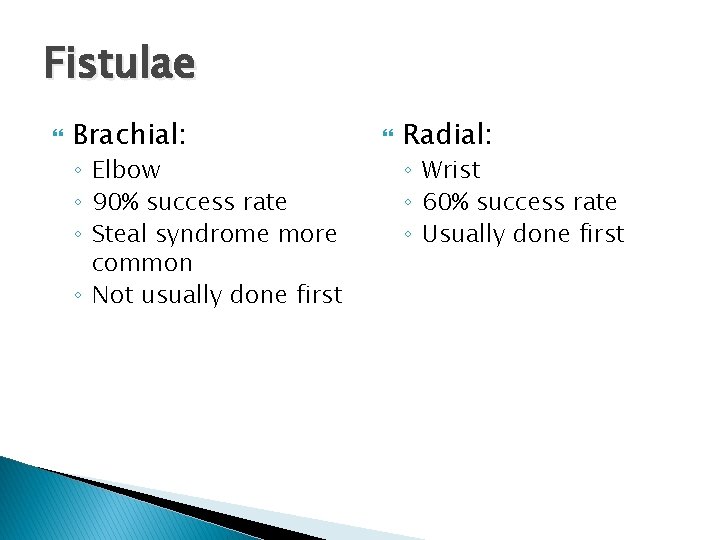
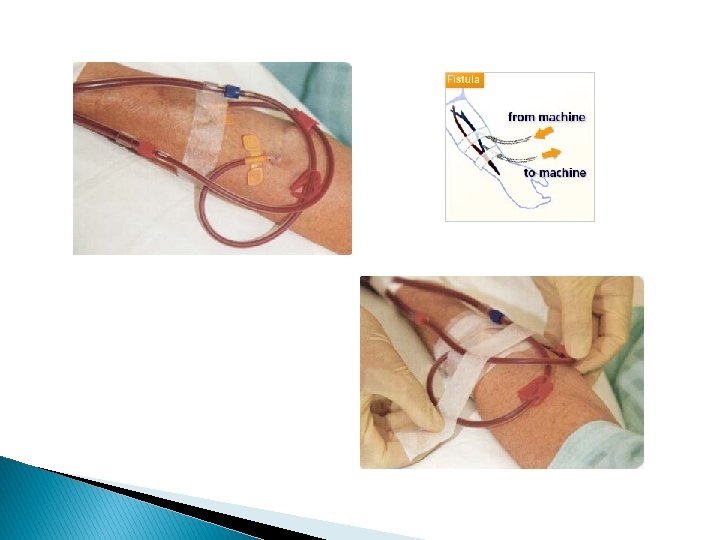
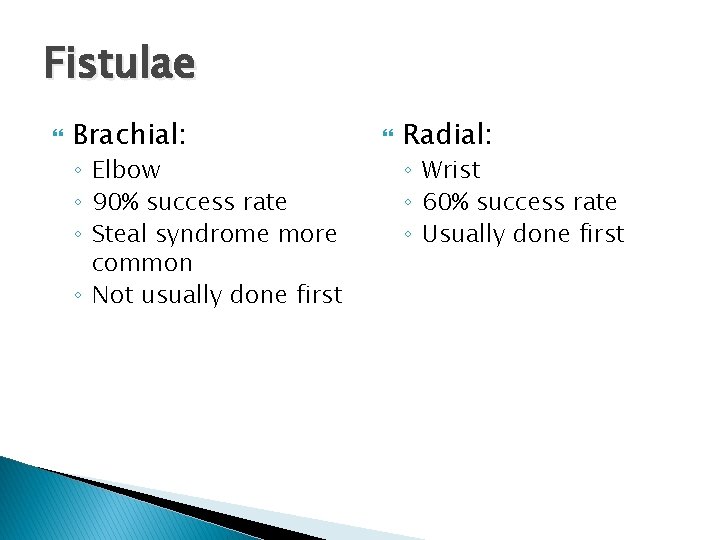
Fistulae Brachial: ◦ Elbow ◦ 90% success rate ◦ Steal syndrome more common ◦ Not usually done first Radial: ◦ Wrist ◦ 60% success rate ◦ Usually done first
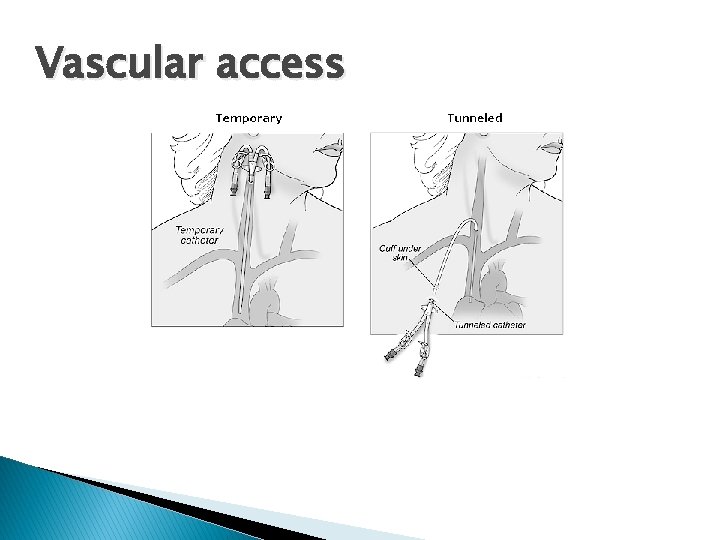
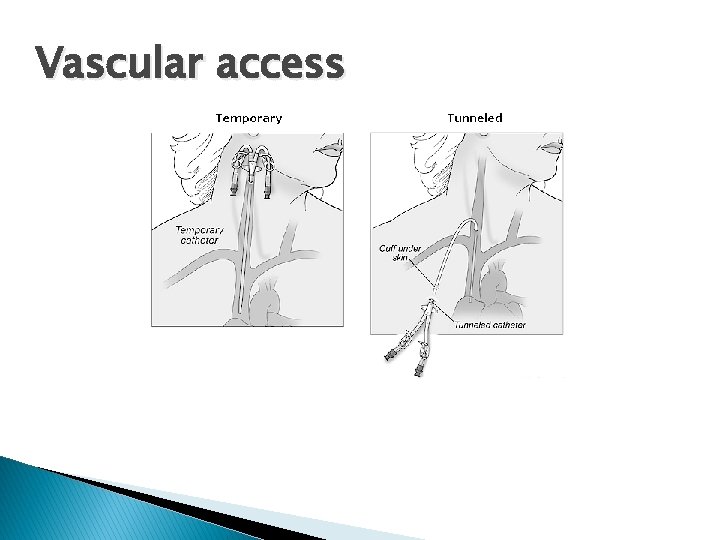
Vascular access
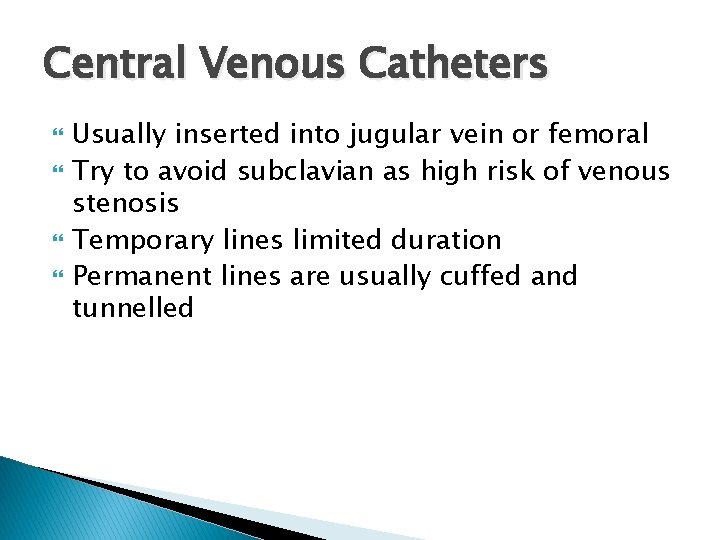
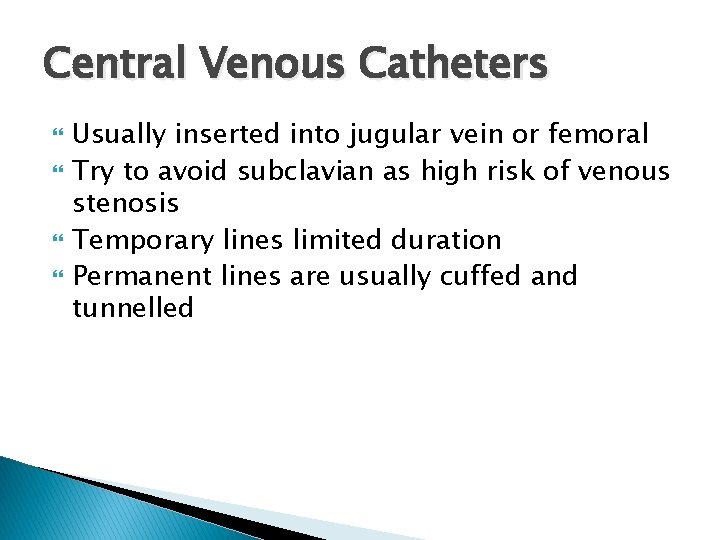
Central Venous Catheters Usually inserted into jugular vein or femoral Try to avoid subclavian as high risk of venous stenosis Temporary lines limited duration Permanent lines are usually cuffed and tunnelled

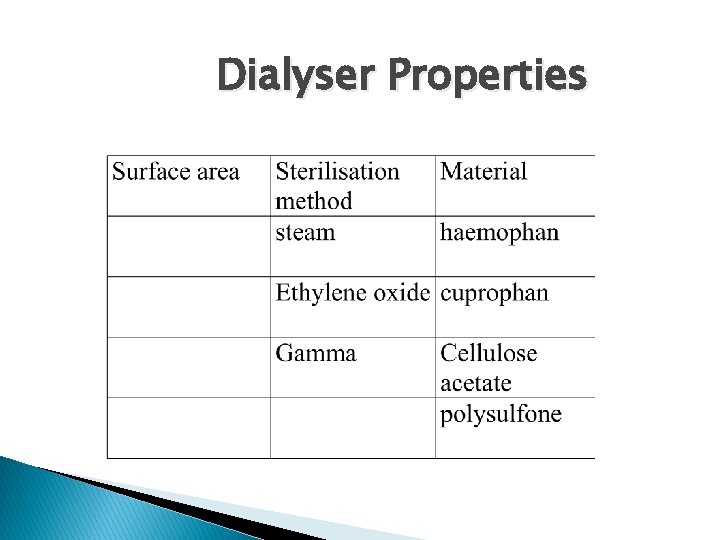
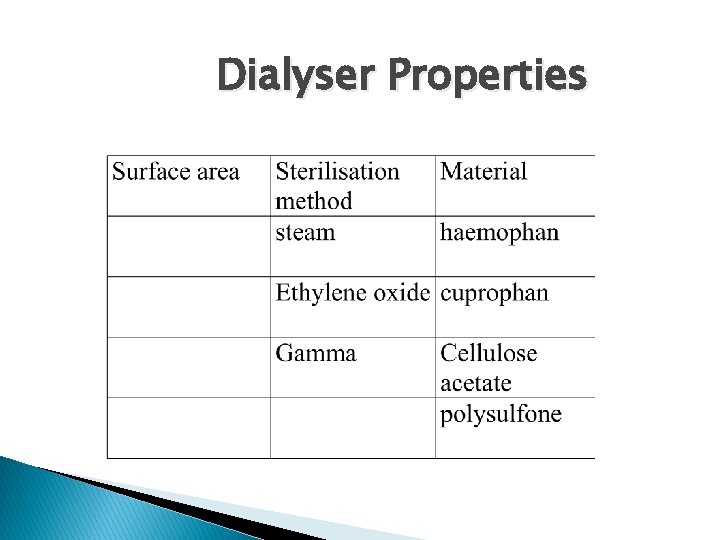
Dialyser Properties
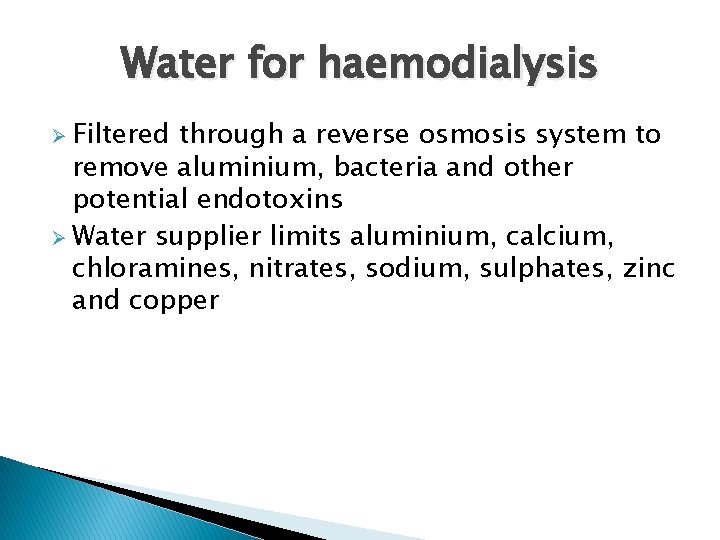
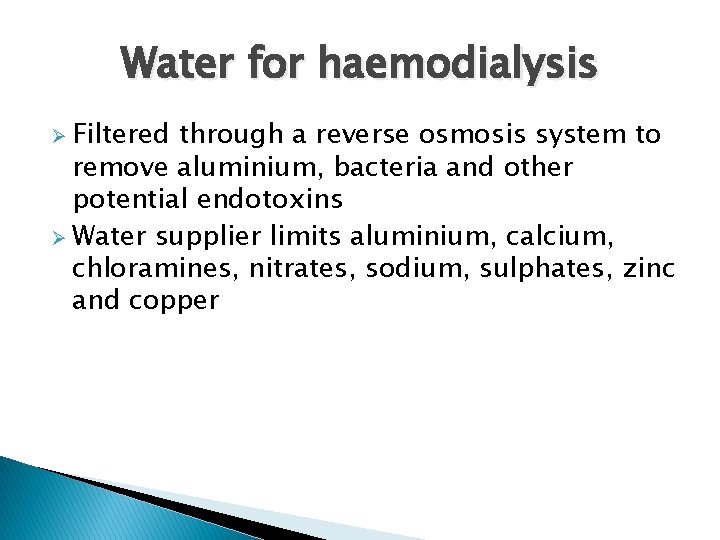
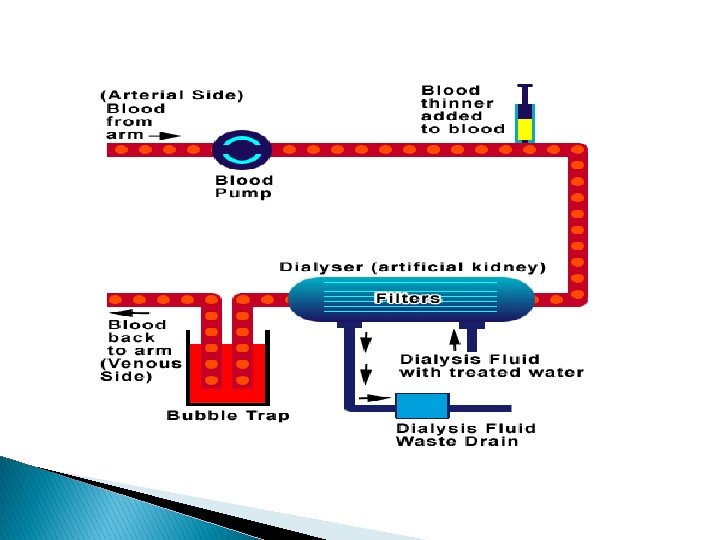
Water for haemodialysis Ø Filtered through a reverse osmosis system to remove aluminium, bacteria and other potential endotoxins Ø Water supplier limits aluminium, calcium, chloramines, nitrates, sodium, sulphates, zinc and copper
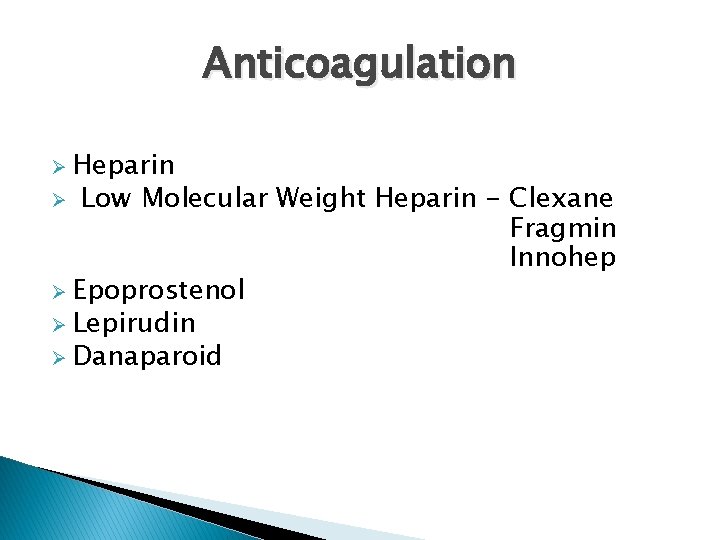
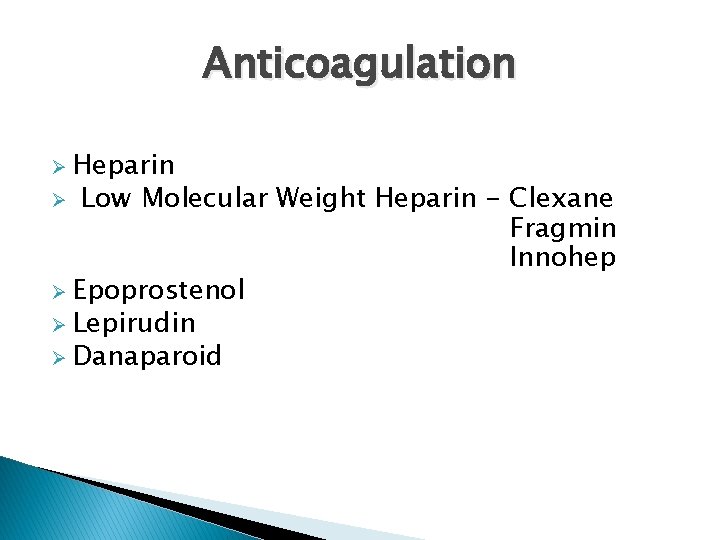
Anticoagulation Ø Heparin Low Molecular Weight Heparin - Clexane Fragmin Innohep Ø Epoprostenol Ø Lepirudin Ø Danaparoid Ø
![Dialysis Adequacy Ø Urea Reduction Ratio URR aim for URR 65 Ø Ktv Dialysis Adequacy Ø Urea Reduction Ratio (URR) [aim for URR > 65%] Ø Kt/v](https://slidetodoc.com/presentation_image/e38d9e0f5051492737d4a08aab64e126/image-15.jpg)
Dialysis Adequacy Ø Urea Reduction Ratio (URR) [aim for URR > 65%] Ø Kt/v [aim for Kt/V > 1. 2]
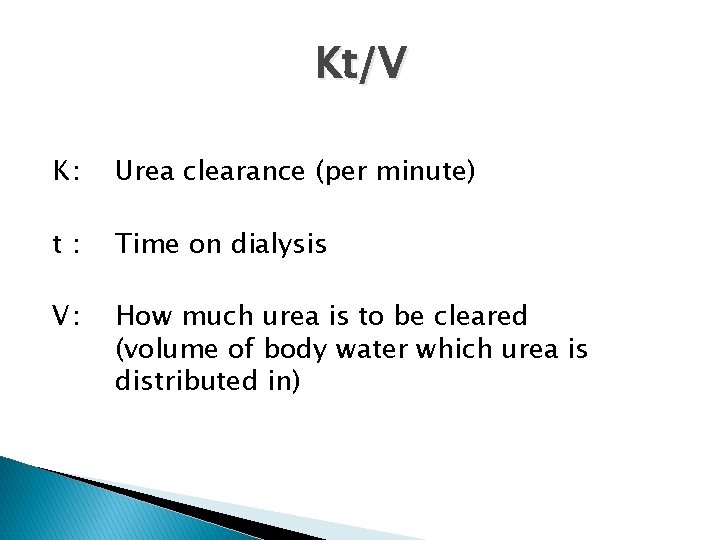
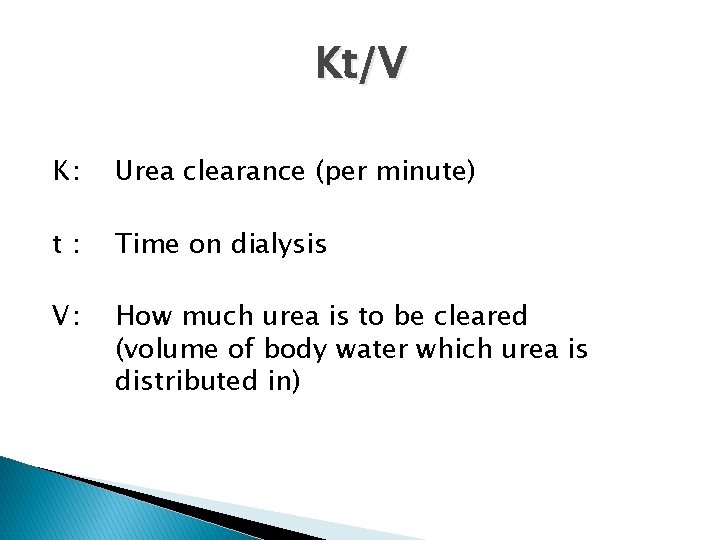
Kt/V K: Urea clearance (per minute) t: Time on dialysis V: How much urea is to be cleared (volume of body water which urea is distributed in)

Values to calculate Kt/V Ø Pre & post weight Ø Blood flow Ø Time on dialysis Ø Size of dialyser Ø Dry weight Ø Pre & post biochemistry & haematology Ø Problems with the dialysis session
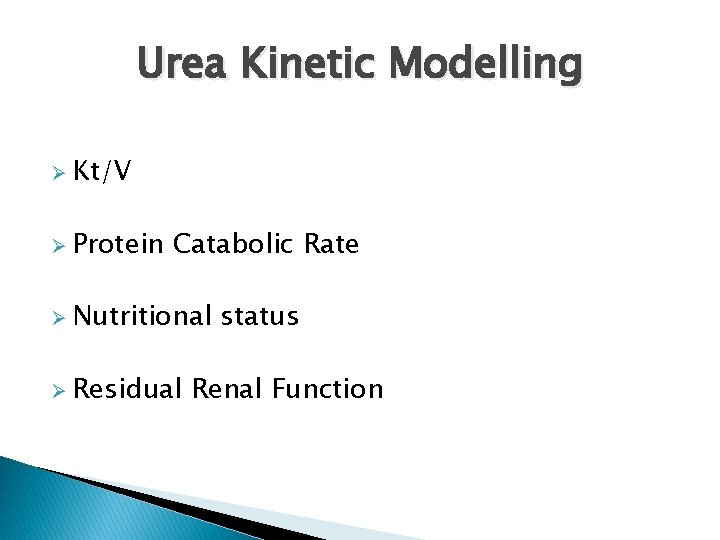
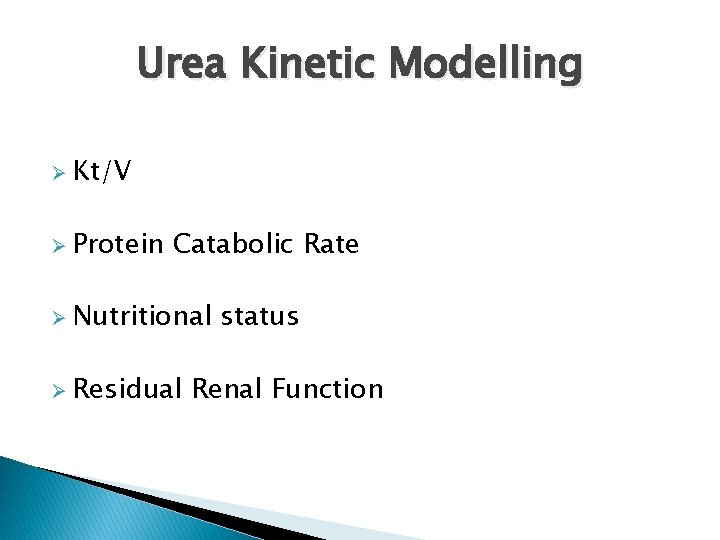
Urea Kinetic Modelling Ø Kt/V Ø Protein Catabolic Rate Ø Nutritional Ø Residual status Renal Function
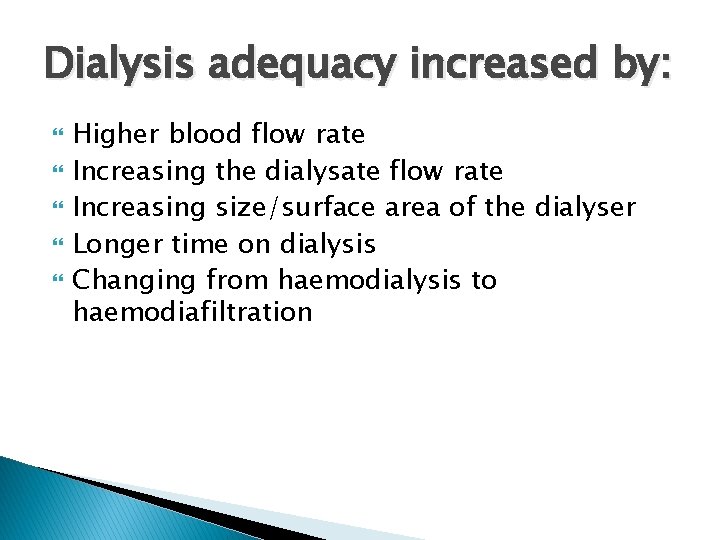
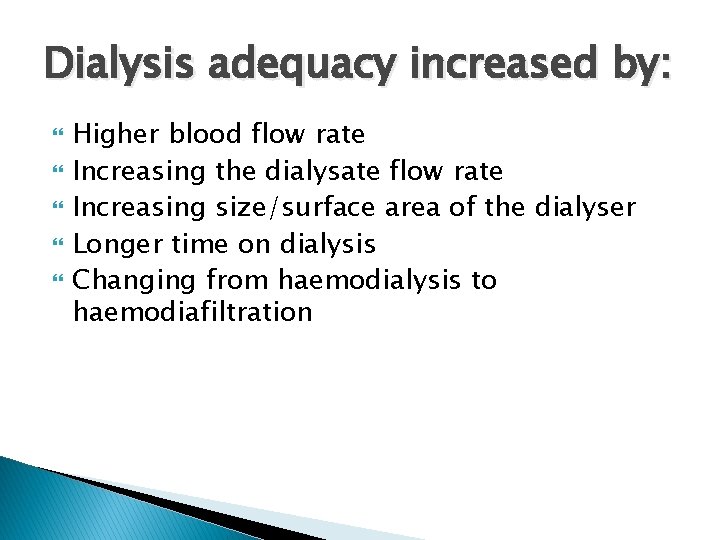
Dialysis adequacy increased by: Higher blood flow rate Increasing the dialysate flow rate Increasing size/surface area of the dialyser Longer time on dialysis Changing from haemodialysis to haemodiafiltration
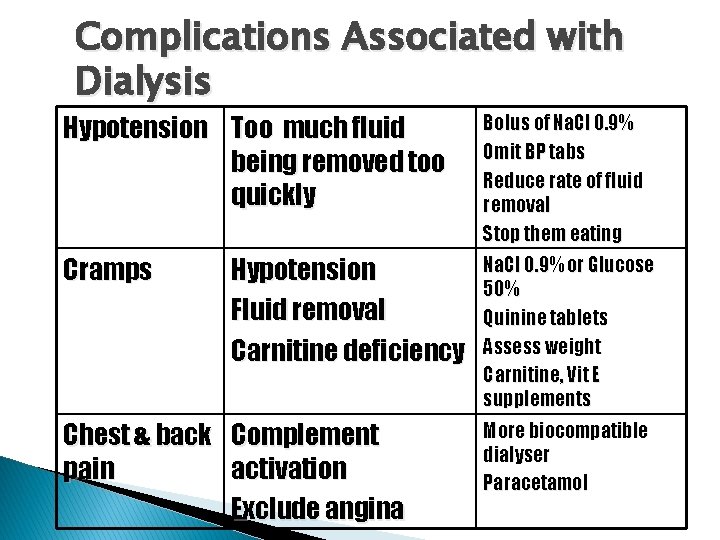
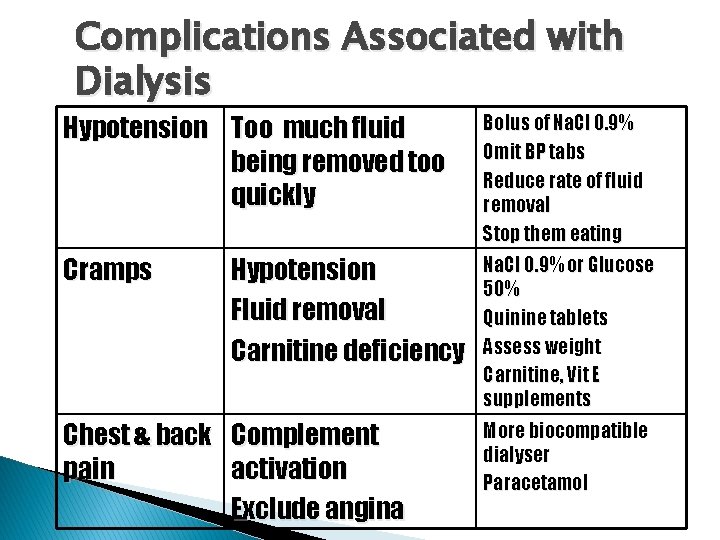
Complications Associated with Dialysis Hypotension Too much fluid being removed too quickly Bolus of Na. Cl 0. 9% Omit BP tabs Reduce rate of fluid removal Stop them eating Cramps Na. Cl 0. 9% or Glucose 50% Quinine tablets Assess weight Carnitine, Vit E supplements Hypotension Fluid removal Carnitine deficiency Chest & back Complement pain activation Exclude angina More biocompatible dialyser Paracetamol
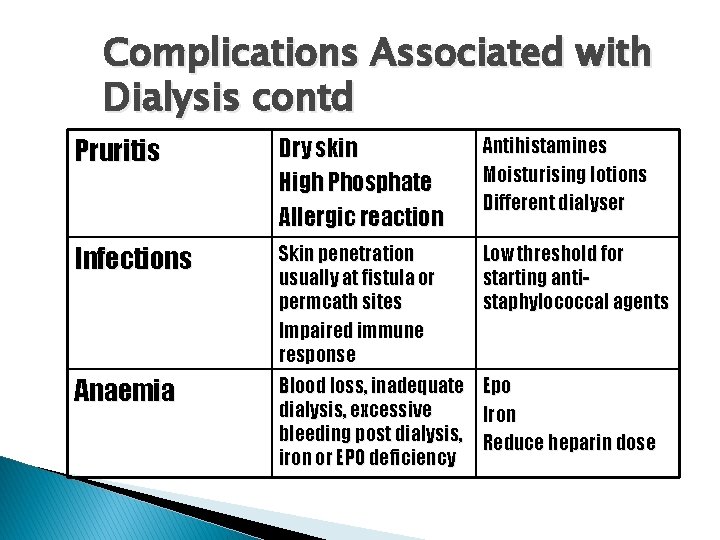
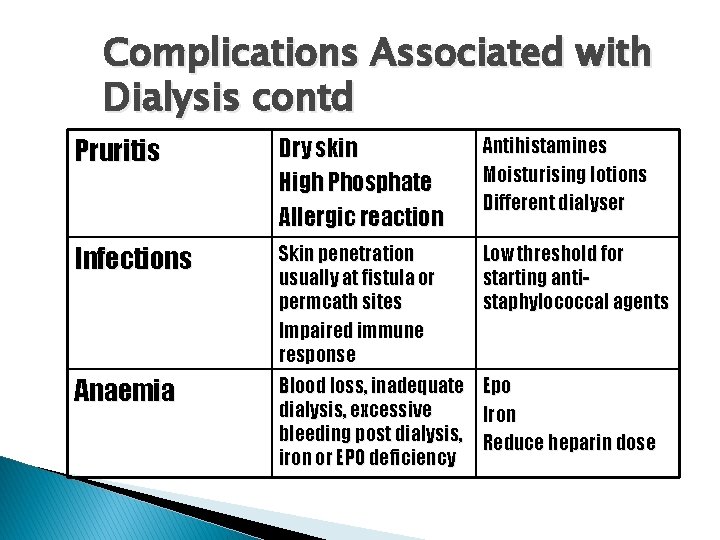
Complications Associated with Dialysis contd Pruritis Dry skin High Phosphate Allergic reaction Antihistamines Moisturising lotions Different dialyser Infections Skin penetration usually at fistula or permcath sites Impaired immune response Low threshold for starting antistaphylococcal agents Anaemia Blood loss, inadequate Epo dialysis, excessive Iron bleeding post dialysis, Reduce heparin dose iron or EPO deficiency
Complications of haemodialysis Air embolism Dysrrhythmias Clotting + blocked lines Haemorrhage
Psychological impact of treatment First phase euphoria Second phase depressive reaction Third phase realistic adjustment Abram HS (1970) Survival by machine; the psychological stress of chronic haemodialysis. Psychiatric Medicine, 1: 37
Long term complications Anaemia Osteodystrophy Cardiac problems Uraemia
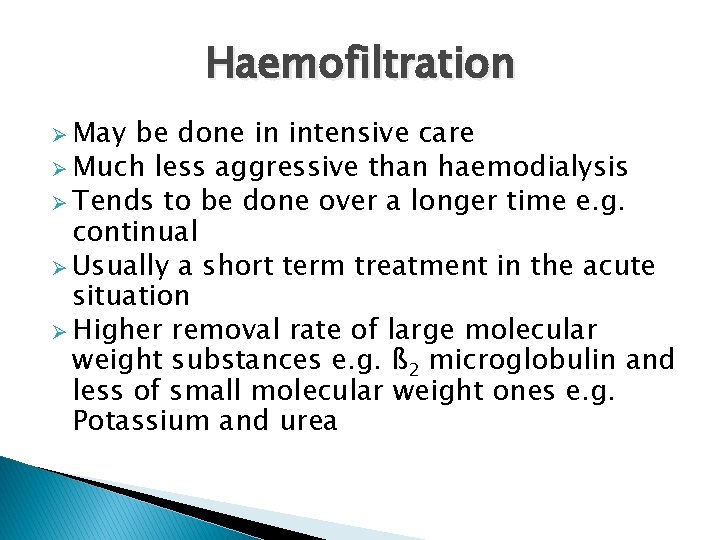
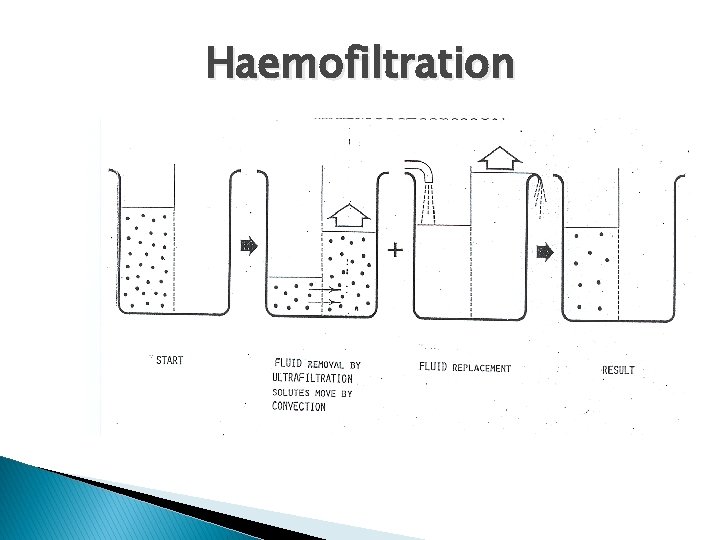
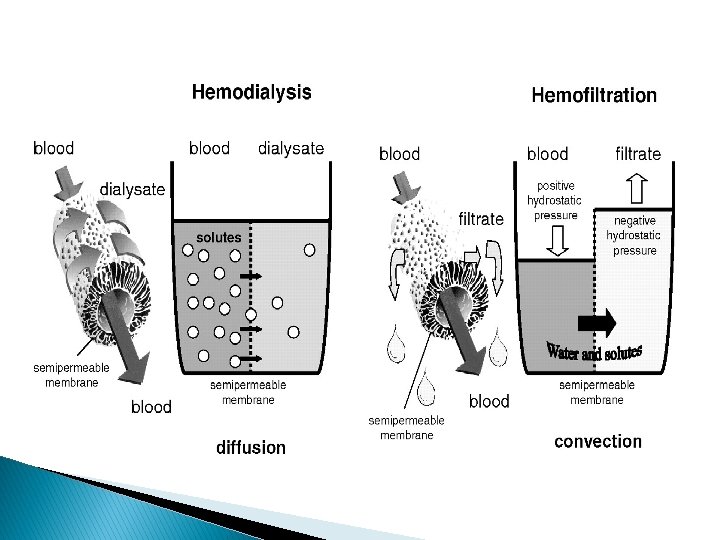
Haemofiltration Ø May be done in intensive care Ø Much less aggressive than haemodialysis Ø Tends to be done over a longer time e. g. continual Ø Usually a short term treatment in the acute situation Ø Higher removal rate of large molecular weight substances e. g. ß 2 microglobulin and less of small molecular weight ones e. g. Potassium and urea
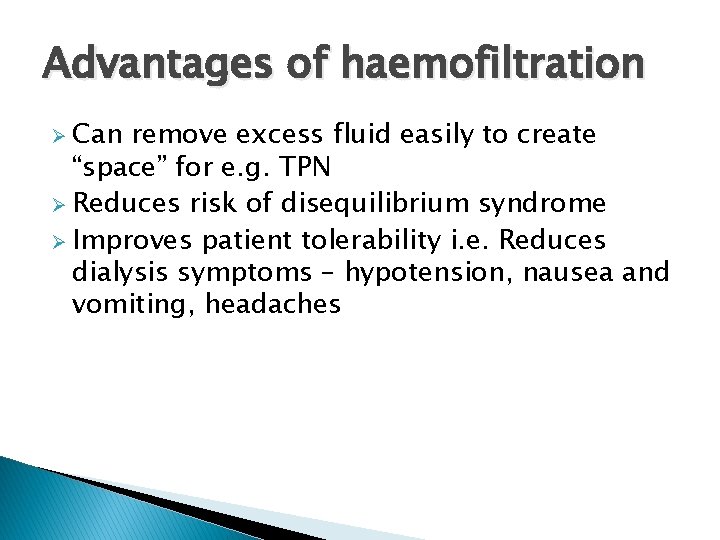
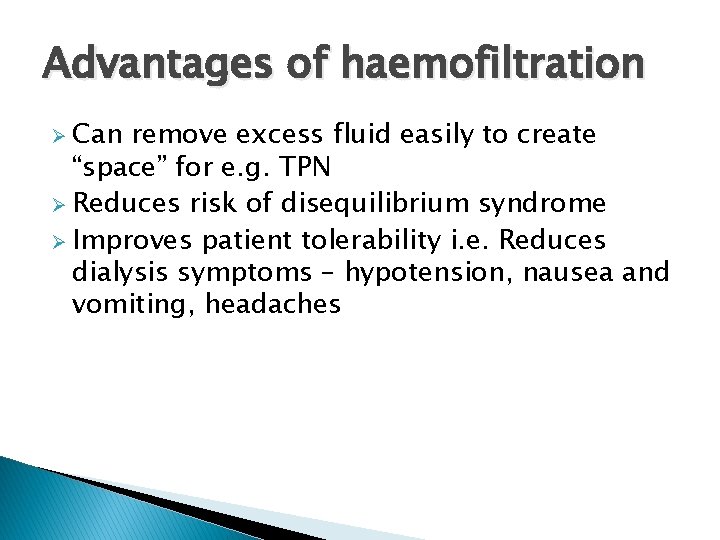
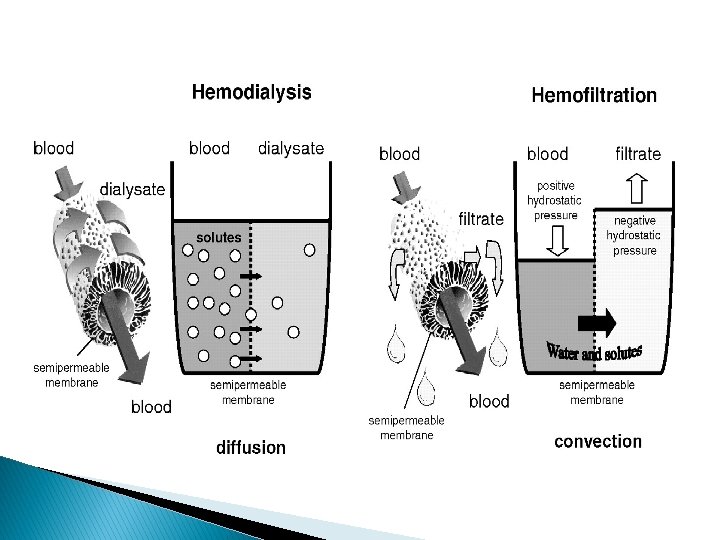
Advantages of haemofiltration Ø Can remove excess fluid easily to create “space” for e. g. TPN Ø Reduces risk of disequilibrium syndrome Ø Improves patient tolerability i. e. Reduces dialysis symptoms – hypotension, nausea and vomiting, headaches
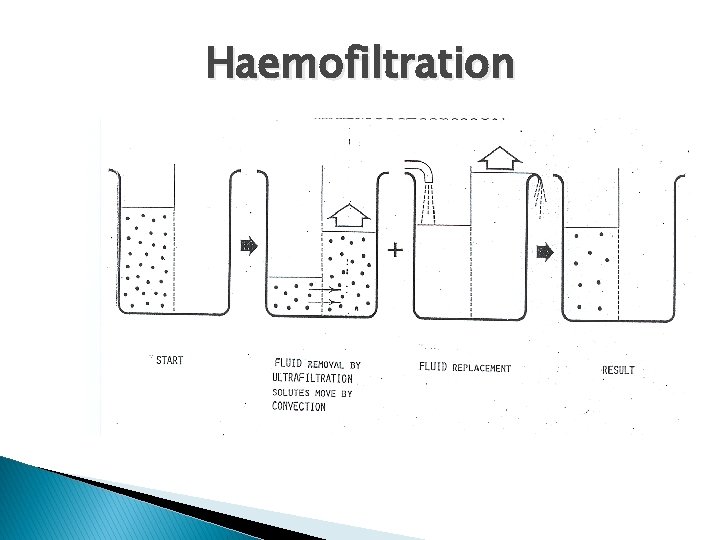
Haemofiltration
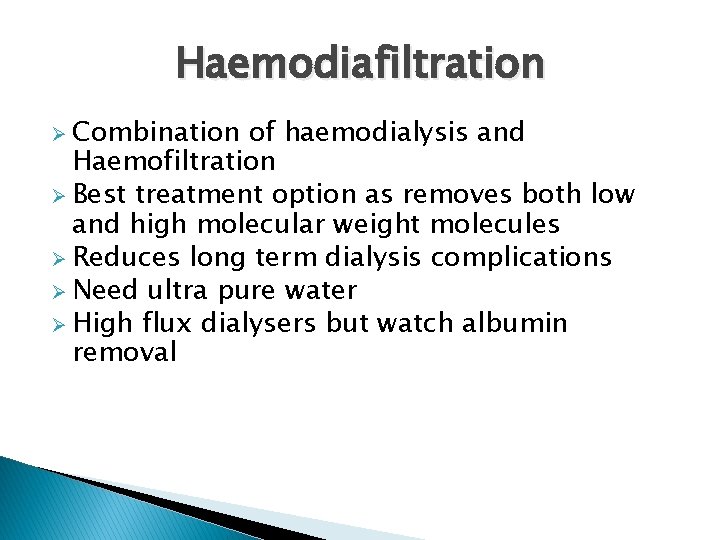
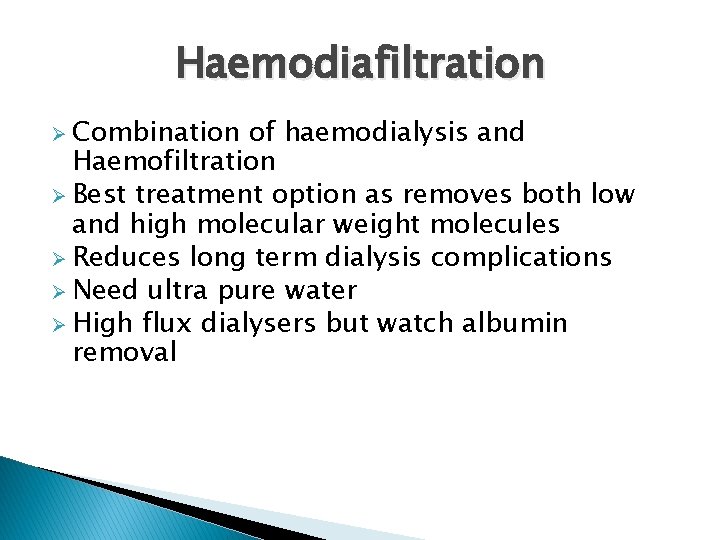
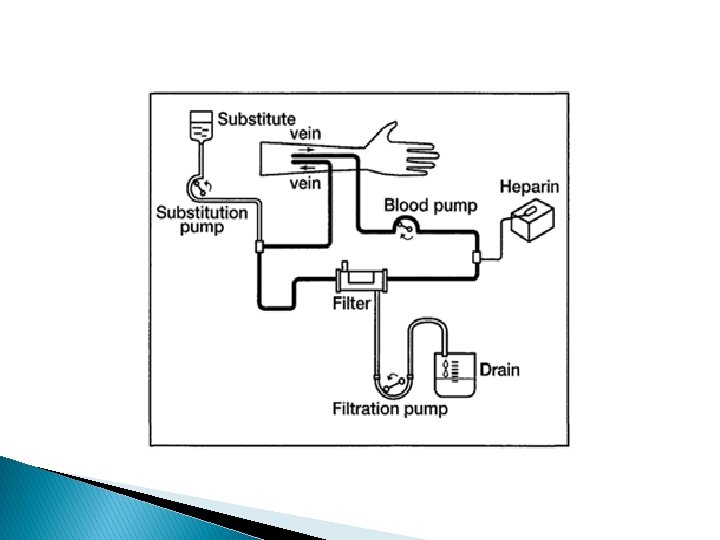
Haemodiafiltration Ø Combination of haemodialysis and Haemofiltration Ø Best treatment option as removes both low and high molecular weight molecules Ø Reduces long term dialysis complications Ø Need ultra pure water Ø High flux dialysers but watch albumin removal
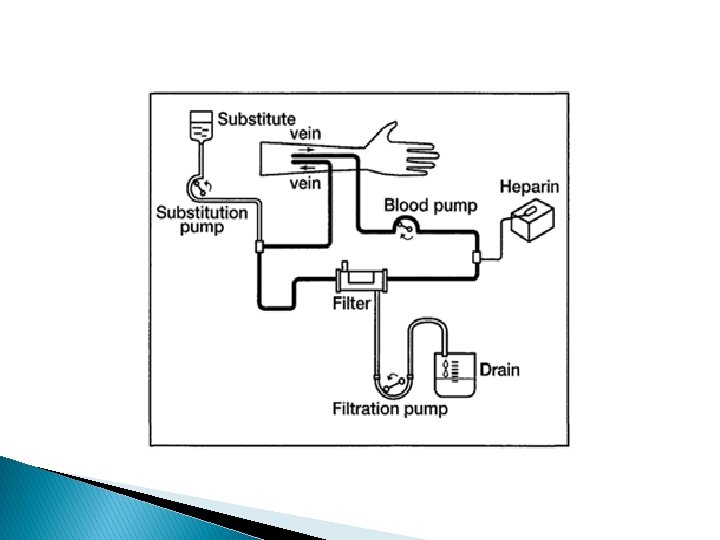
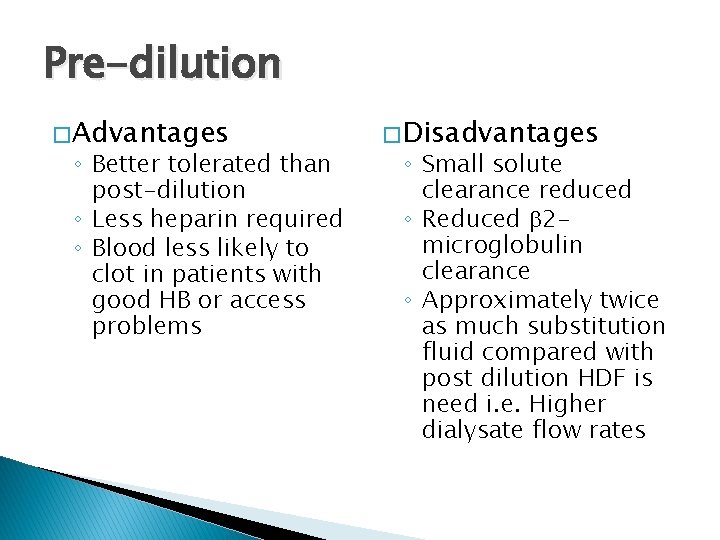
Pre-dilution The blood is diluted by the substitution fluid before going through the dialyser and was the original form of HDF
Pre-dilution � Advantages ◦ Better tolerated than post-dilution ◦ Less heparin required ◦ Blood less likely to clot in patients with good HB or access problems � Disadvantages ◦ Small solute clearance reduced ◦ Reduced b 2 microglobulin clearance ◦ Approximately twice as much substitution fluid compared with post dilution HDF is need i. e. Higher dialysate flow rates
Post-dilution The more traditional method now: blood is diluted by substitution fluid after going through the dialyser
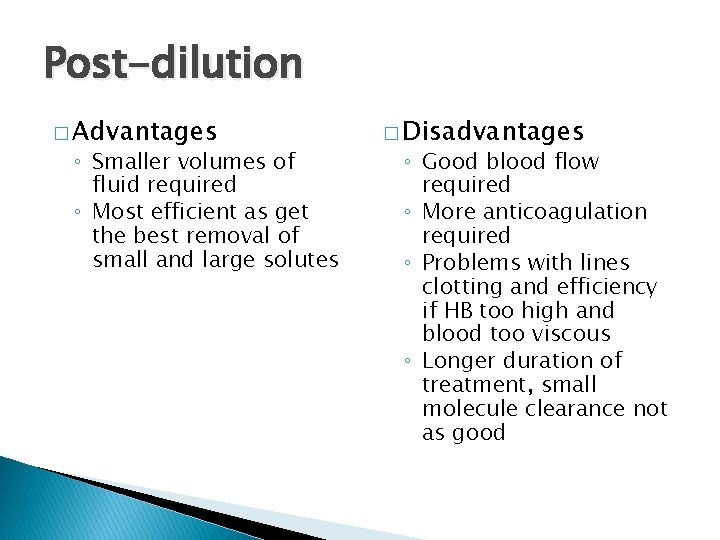
Post-dilution � Advantages ◦ Smaller volumes of fluid required ◦ Most efficient as get the best removal of small and large solutes � Disadvantages ◦ Good blood flow required ◦ More anticoagulation required ◦ Problems with lines clotting and efficiency if HB too high and blood too viscous ◦ Longer duration of treatment, small molecule clearance not as good
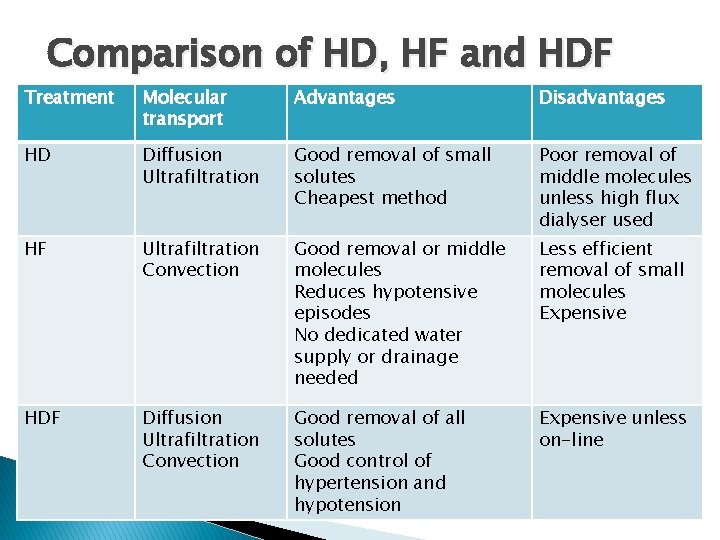
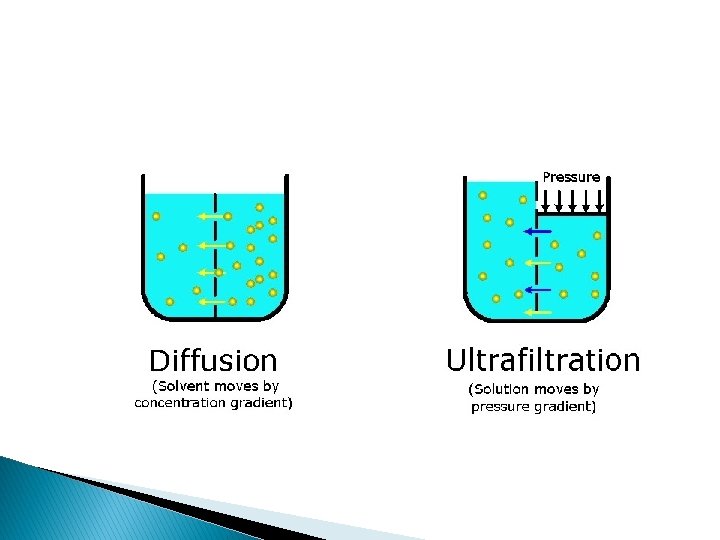
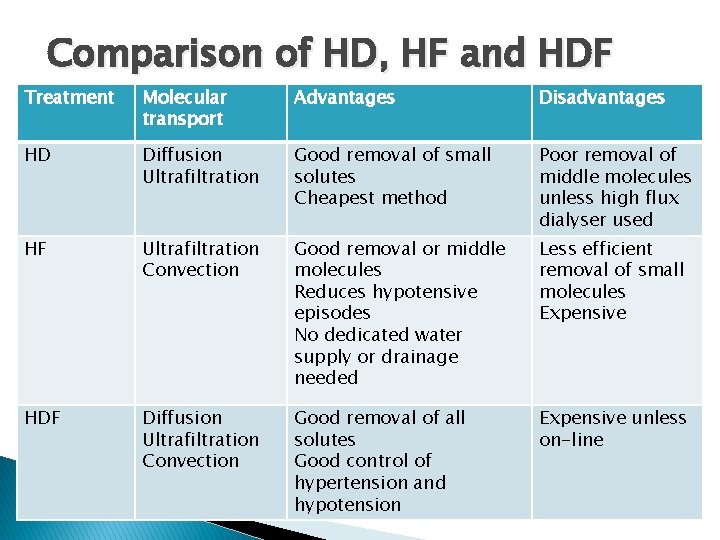
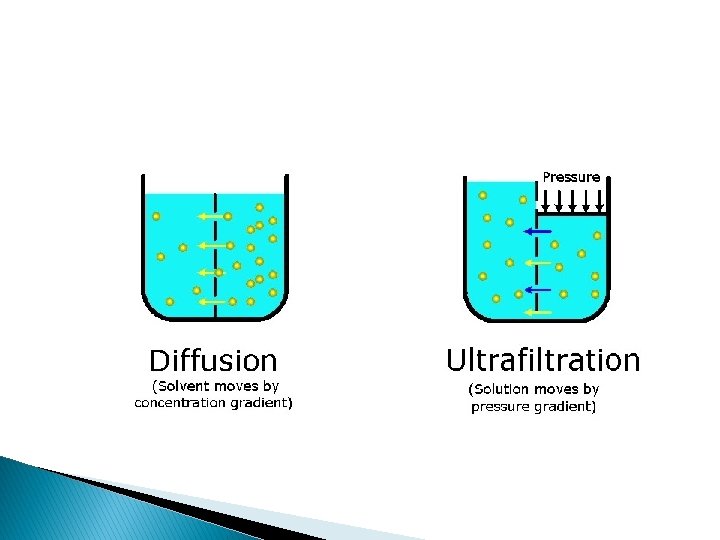
Comparison of HD, HF and HDF Treatment Molecular transport Advantages Disadvantages HD Diffusion Ultrafiltration Good removal of small solutes Cheapest method Poor removal of middle molecules unless high flux dialyser used HF Ultrafiltration Convection Good removal or middle molecules Reduces hypotensive episodes No dedicated water supply or drainage needed Less efficient removal of small molecules Expensive HDF Diffusion Ultrafiltration Convection Good removal of all solutes Good control of hypertension and hypotension Expensive unless on-line