INTRODUCTION TO DOCUMENTATION Concepts in Occupation Fall 2019












































- Slides: 45

INTRODUCTION TO DOCUMENTATION Concepts in Occupation Fall 2019 Sara Walters, MOT, LOTR

Objectives • Describe the importance of documentation • Classify the purpose of documentation • Explain the relationship of the ICF and clinical documentation in OT • Examine legal and ethical implications of documentation • Identify professional documents that guide clinical documentation • Justify use of OTPF in documentation • Demonstrate understanding of FOR as treatment guide • Identify important components and types of documentation • Explain what is meant by a skilled intervention • Discuss components needed to document skilled services • Distinguish OT’s role in documentation • Apply principles of clinical reasoning • Describe the acceptable method of correcting errors in the medical record • Discuss consequences of poor documentation

Purpose of Documentation • A communication tool for health care team, client and family • A means of providing facts about a client from an OT perspective • Justification or rationale for OT services, outcomes, clinical reasoning, professional judgment, and reimbursement Meriando & Latella (2016), p. 18 -20

Purpose of Documentation A chronological record of client care and status regarding OT services • Accountability • Ethical responsibility • Method of recording • Documents baseline of results • Method of measuring progress • Required legal document • Validate reimbursement by third-party payers function • Provides continuity of care • Permanent record of occurrences • Informs other team members • Provides data for research Meriando & Latella (2016), p. 18 -20

Good Documentation Supports • Patient/client care • Continuity of care • Record integrity • Accurate professional billing • Accurate facility billing

Importance of Documentation 1. 2.

General Guidelines for Documentation • Be accurate and complete • Must be clear, concise, and comprehensive • Use proper spelling and grammar • Avoid jargon • Be careful of buzzwords and “red flag” words Meriando & Latella (2016), p. 20 -21

General Guidelines for Documentation • Paint a verbal picture • Focus on function • underlying cause • progress • Safety • Different information is needed by different people Meriando & Latella (2016), p. 20 -21

Who is looking and reading? Medical Professional s • Chronological record of care • Continuity of Care • Communication across shifts Educational Professional s Payers • IFSP • IEP • Reimbursement Legal • Malpractice • Fraud Client • Record review • Follow through

World Health Organization’s International Classification of Functioning, Disability, & Health ICF Health Condition (disease or disorder) Describes the actual disease or disorder and is extremely relevant to therapeutic intervention. Body Function and Structure (impairment) Includes physiological functions of body systems or anatomical parts of the body and their components. Critical to therapist’s assessment and treatment. Activities and Participation Activity – learning, self-care, interpersonal interactions, community, social and civic life. Documentation describes outcomes or changes in client’s activities. Environmental Factors – important in the safe and therapeutic management of the client’s condition. Personal Factors – gender, age, coping style and education

OTPF • Performance in Areas of Occupation • Performance Skills • Performance Patterns • Context • Activity Demands • Client Factors

Quality of Documentation Thorough Meets facility guidelines Timely Accurate Meets client needs Reflects OT Process Reflects best practice Relevant Clear Concise Grammatically correct

Documenting the Process of Service Delivery • Evaluation or Screening Report • Reevaluation Report • Intervention • Intervention Plan • Provision of Service Contacts • Progress Report • Transition Plan • Outcomes • Discharge/Discontinuation Report

What’s included in patient documentation? • Evaluation report • Demographic data • Referral information • Diagnosis • History • Rehab potential • Reason for OT • Person responsible for carrying out program • Expected timelines • Assessment results • Contact, treatment, or visit note • Progress note • Re-evaluation report • Discharge or discontinuation report • Discharge summary: path of intervention must be summarized

Skill in Documentation • Skill in documentation is the hallmark of a professional approach to therapy and is one of the characteristics that distinguishes a professional from a technician. • Not only is the logic of clinical reasoning reflected in documentation, but documentation itself shapes the process of clinical reasoning. Acknowledge: Rhonda Lane, LOTR

Documentation Must Show…. . • Skilled Therapy/Medical Necessity • Written treatment plan • Specific therapy goals • Accepted methods of treatment • Treatment that is reasonable for patient’s illness or injury Acknowledge: Rhonda Lane, LOTR

Documenting Skilled Intervention Activity Analysis Problem Identificatio n Skilled Treatment • Breaking down task • Up/Down grades • Components • Contextual factors • FOR • EBP Intervention Strategies

Frequency and Duration of Treatment • How often • How long per session • How many # of visits “Pt. will be seen for 45 min. , 2 x/wk, for 6 wks. ”

Tips for Good Documentation • Clarity • Accuracy • Relevance • Exceptions (Sames, 2010 p. 47)

Relationship of Documentation to Reimbursement Skilled Service • Provided by one with broad knowledge base of human functioning and occupational performance • Decision-making; complex tasks/activities • Must show progress and benefit to patient Non-skilled Service • Routine/maintenance tasks that another can be trained to do • Claims for non-skilled services will always be denied

Results of Poor Documentation • Inaccurate or incomplete medical record • May lose medical malpractice suit • Difficult for anotherapist or other professional to get whole picture • Wrong tx for patient • No reimbursement from insurance company, Medicare, Medicaid, etc. • You may lose your OT license • Inability to provide facility with accurate and/or needed statistics & information • Decreases funding for programs • Outcome studies are compromised

Confidentiality • ALL INFO IS CONFIDENTIAL; NO EXCEPTIONS! • Cannot release info to anyone without following proper procedures • Cannot discuss with friends/family, in the elevator, at lunch, etc. • May not take home paperwork bearing the client’s name.

HIPPA • Health Insurance Portability and Accountability Act • Right to review own health record • Right to request revision • Right to know health information • Right to decide if used for research • Right to authorize release of information • Right to file a complaint

Documentation Basics • Problem Statements • Identification of strengths & weaknesses • Assistance Levels • Goals • COAST format • Treatment documentation • SOAP format • Correct use of abbreviations

Abbreviations • Documentation Manual to Occupational Therapy • Abbreviations and Symbols list – Chapter 4, Table 4 -3 • These are the only allowed/approved abbreviations for this curriculum.
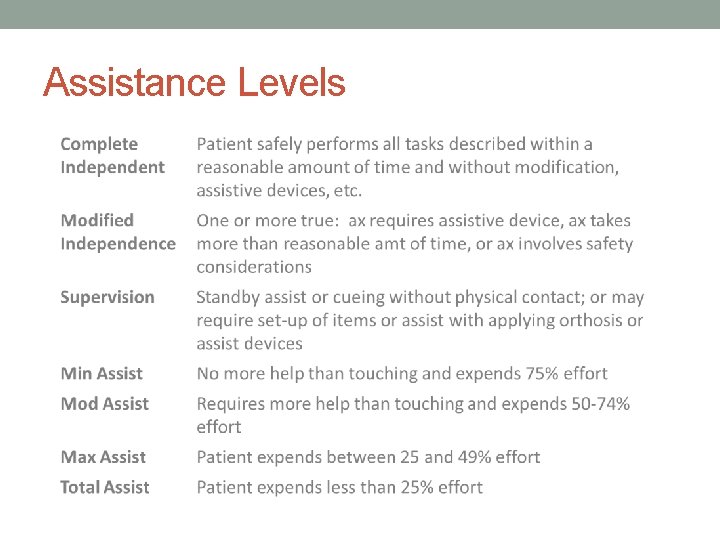
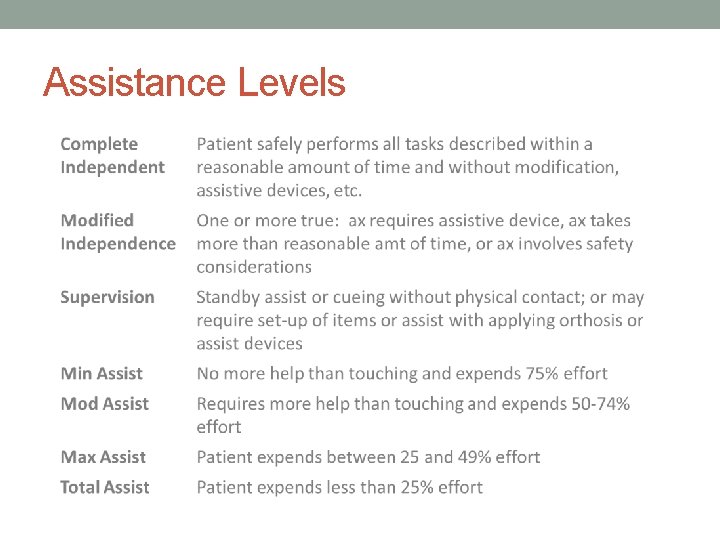
Assistance Levels

Functional Problem Statements • Problem List • Identifies major areas of occupation that are affected by the client’s condition • This can be used to prioritize treatment with the client/family **Diagnosis is not the problem but the contributing factors may be a result of the diagnosis. • Consider strengths & weaknesses of the client

Functional Problem Statements 1. Client requires _____ in __________ (assist level) (what occupational task) due to __________. (contributing factor) Examples: • Child requires mod A to hold scissors to complete art activities in school due to high tone in R UE. • Consumer requires 6 verbal cues to complete 3 -step lunch preparation due to decreased sequencing and problem-solving skills. • Client requires max A to complete upper body dressing due to ½ AROM in B UE.

Functional Problem Statements 2. Client unable to ____________ due to (engage in what occupational task) ________. (what contributing factor) Examples: • Client is unable to perform jumping jacks to participate in gym class due to motor planning deficits. • Client is unable to sustain employment longer than 2 weeks due to absence of stress management skills.

Functional Problem Statements 3. _________ results in _________. (Contributing factor) (what occupational deficit) Tips: • Problem statements should always focus on deficits you can address through OT services. Examples: • Inability to perform simple math calculations results in need for caregiver assistance in IADL tasks such as balancing the checkbook. • Aggressive behavior results in limited opportunities for social participation and repeated involvement with the juvenile justice system. • 5/10 elbow pain results in client needing maximum assistance to brush hair.


Types of Assistance • Physical/tactile or verbal cues: BE SPECIFIC. • Verbal cues – clarity comes with specific number of cues. • When providing an assistance level – always state what the assistance is for: Completes upper body dressing with maximum assistance sequencing? sitting balance? attention to task? motor planning? coordination?

GOALS • Outcomes that determine efficacy of our services. • Must focus on functional improvement in occupational performance. • Long Term Goals (LTG) or Outcomes • Short Term Goals (STG) or Objectives • Various methods available for goal writing; our program utilized the COAST method.

COAST • C • O • A • S • T- Client Occupation Assist Level Specific Condition Timeline Client will perform what occupation? With what level assist/independence? under what condition? by when? Client will perform upper body dressing with <3 verbal cues to sequence hemi-dressing techniques within one week.

Pulling it all together… • Problem Statement: Client is unable to fasten ½” buttons due to 2+ strength in right hand. • LTG: Client will fasten all buttons on shirt independently within 3 weeks. • STG: Client will fasten 3 buttons on shirt using button hook with minimal assistance.


SOAP Notes • S: Subjective • O: Objective • A: Assessment • P: Plan

S: Subjective Information obtained by the client that gives their perspective on treatment. Information obtained here should be relevant to treatment provided. • Client reports he was able to incorporate the reacher into his morning dressing routine without assistance. • Client reports having 5/10 pain in right shoulder. • Client reports concerns with completing cooking activities due to being so tired. Client reports “I cannot get my shirt on because my arm won’t work. ”

O: Objective Measureable, objective, quantifiable, and observable data that occurred during treatment session. This is the picture of the session as it occurs. • 1. Begin with statement about length, setting, purpose of session • 2. Brief overview of key deficits impacting performance. • 3. Summary of what was observed/what occurred • 4. Be concise, professional, and specific. Example: Client participated in 15 minute session in his room to for training in hemi-dressing techniques to increase independence with dressing activities. He presents with right hemiparesis and decreased postural control following a CVA. Pt sat edge of bed with minimal assistance to maintain midline posture during RUE reaching. Intermittent tactile cues were provided to facilitate lateral trunk extension during dynamic activity. He was instructed in hemi-dressing techniques for a pull-over shirt and verbalized understanding. He required 3 verbal cues to correctly sequence steps of task. He donned the shirt with minimal assistance to thread his right upper extremity successfully.

A: Assessment Your professional assessment of the client’s performance and progress, limitations, and expected benefit of OT intervention. *No new information should be presented. Example: Right hemiparesis and poor sitting balance impact client’s ability to complete upper body dressing. Incorporation of hemi-dressing techniques have increased independence in task completion as he now only requires minimal assistance to complete the task. Client continues to require minimal assistance for postural control. Progression in upper body with use of compensatory dressing techniques demonstrate good potential to increase independence in other BADL using compensatory techniques. Client will benefit from continued instruction in compensatory strategies to increase independence in other BADL as well as neuromuscular re-education to facilitate improved postural control during functional activities.

P: PLAN Document anticipated frequency and duration of services and specific interventions that will be used to achieve goals. Should relate to information in the O and A. Example: Client will be seen bid for 1 week for skilled instruction in ADL retraining, facilitation of postural control, and management of right upper extremity during functional activities. Sessions will focus on hemi-dressing techniques for lower body dressing, facilitation of postural control, and use of adaptive equipment to increase independence and safety in self-care routine prior to discharge home.

Acceptable Excuses for Poor Documentation • NONE

Legal Implications • Patient’s chart is a permanent legal record • Chart is considered the ONLY official information related to particular patient • Contents dictated by facility, its internal systems, licensing agencies, accrediting bodies, and 3 rd party payers

References • American Occupational Therapy Association. (2013). Guidelines for documentation of occupational therapy. American Journal of Occupational Therapy, 67, Number 6 (supplement). • Boyt Schell, B. A. , Gillen, G. , & Scaffa, M. E. (Eds). Willard & Spacman’s occupational therpay (12 th ed. ). Philadelphia, Wolters Kluwer/Lippincott Williams & Wilkins. • Case-Smith, J. (2010). Occupational therapy for children. (6 th ed. ) Maryland Heights, Missouri: Mosby-Elsevier. • Christiansen, C. H. , Baum, C. M. & Bass, J. D. (Eds). (2015). Occupational therapy performance, participation, and wellbeing. Thorofare, NJ: Slack. • Gately, C. A. & Borcherding, S. (2012). Documentation manual for writing SOAP notes (3 rd ed). Thorofare, NJ: Slack.

References • Kramer, P. & Hinojosa, J. (1999). Frames of reference for pediatric occupational therapy. (2 nd ed. ) Philadelphia: Lippincott Williams & Wilkins. • Mattingly, C. & Fleming, M. (1994). Clinical reasoning: forms of inquiry in a therapeutic practice. Philadelphia: F. A. Davis. • Meriano, C. & Latella, D. (2016). Occupational therapy interventions: Function and occupations. (2 nd ed. ) Thorofare, NJ: Slack. • Pedretti, L. (2013). Occupational therapy – practice skills for physical dysfunction. (7 th ed. ) St. Louis: Elsevier -Mosby. • WHO (2001). International classification of functioning, disability, and health (ICF). Geneva, Switzerland, http: //www. who. int/classifications/icf/en/