Introduction to Curriculum Curricular reforms CISP Dr Suman









- Slides: 84
Introduction to Curriculum, Curricular reforms & CISP Dr Suman P Singh Microbiology, PS Medical College Karamsad
Curriculum Vs Syllabus
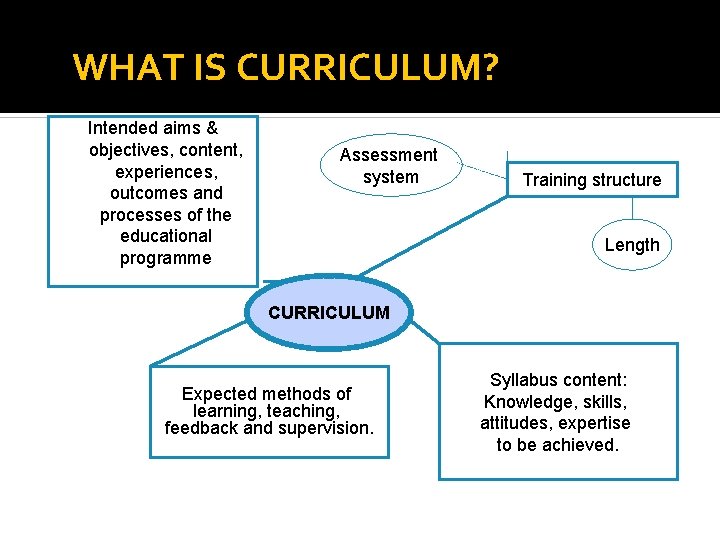
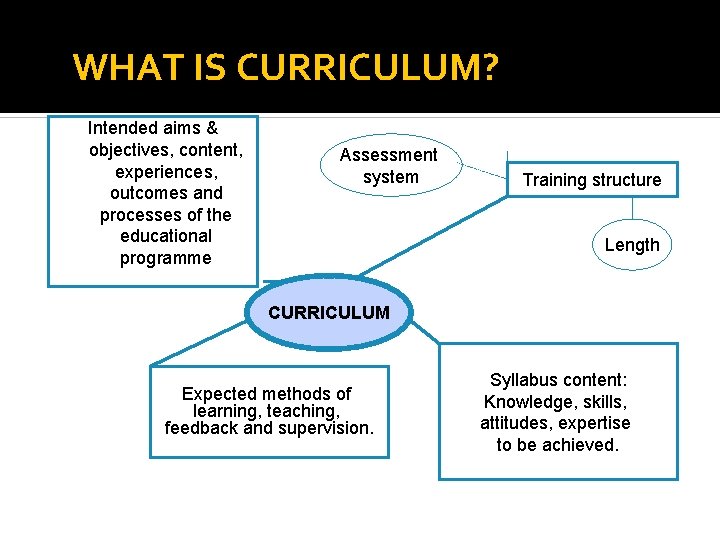
WHAT IS CURRICULUM? Intended aims & objectives, content, experiences, outcomes and processes of the educational programme Assessment system Training structure Length CURRICULUM Expected methods of learning, teaching, feedback and supervision. Syllabus content: Knowledge, skills, attitudes, expertise to be achieved.
Curriculum Formal plan of educational experiences and activities offered to a learner under the guidance of an educational institution. 4
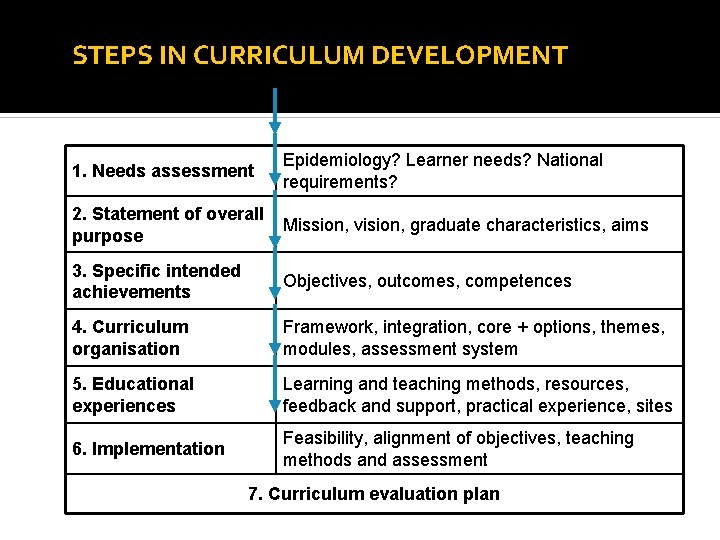
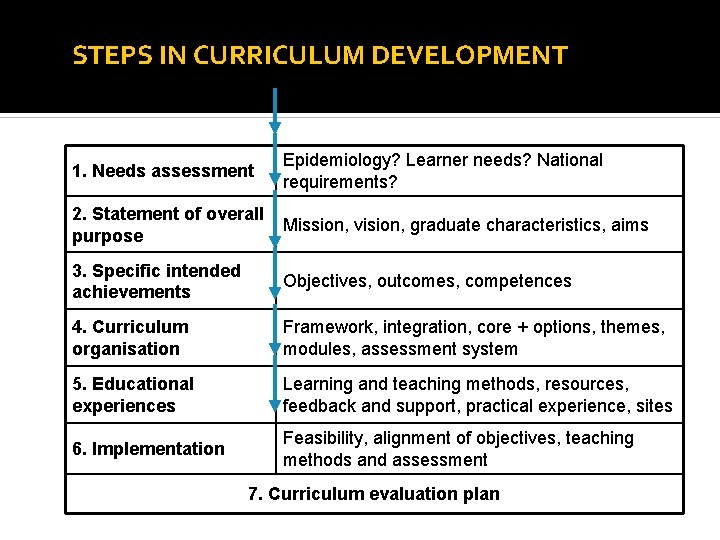
STEPS IN CURRICULUM DEVELOPMENT 1. Needs assessment Epidemiology? Learner needs? National requirements? 2. Statement of overall purpose Mission, vision, graduate characteristics, aims 3. Specific intended achievements Objectives, outcomes, competences 4. Curriculum organisation Framework, integration, core + options, themes, modules, assessment system 5. Educational experiences Learning and teaching methods, resources, feedback and support, practical experience, sites 6. Implementation Feasibility, alignment of objectives, teaching methods and assessment 7. Curriculum evaluation plan

Effective Curriculum Produces specific outcome as defined or expected Is efficient in terms of man, money and minutes Is open and responsive to change 7
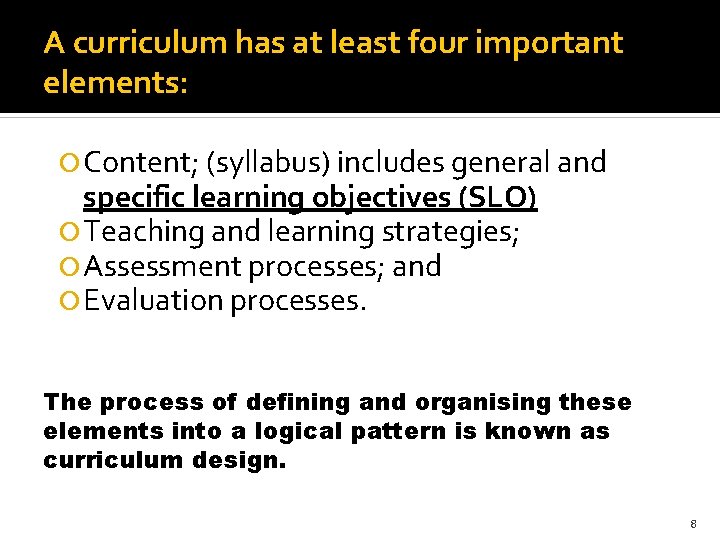
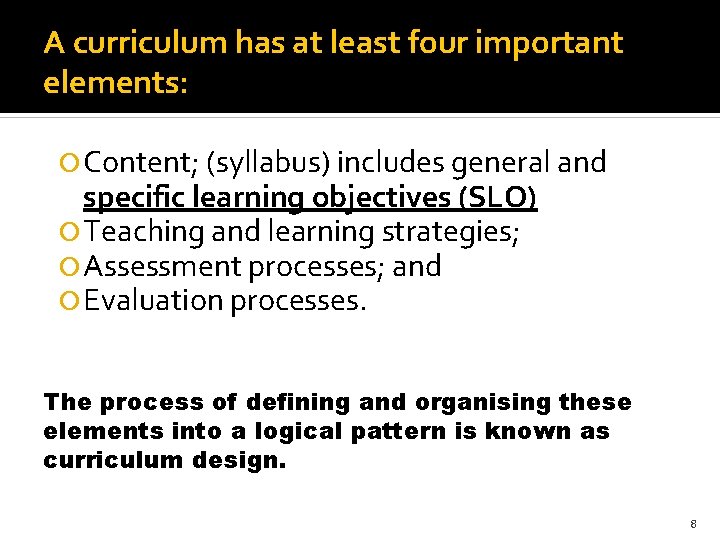
A curriculum has at least four important elements: Content; (syllabus) includes general and specific learning objectives (SLO) Teaching and learning strategies; Assessment processes; and Evaluation processes. The process of defining and organising these elements into a logical pattern is known as curriculum design. 8
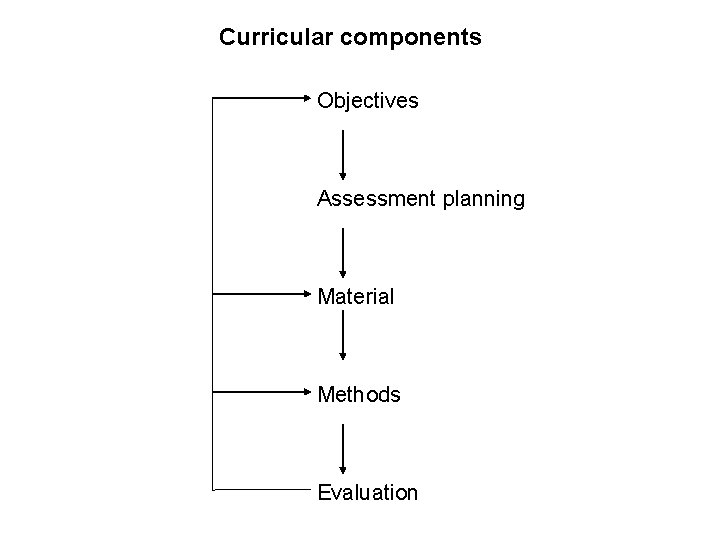
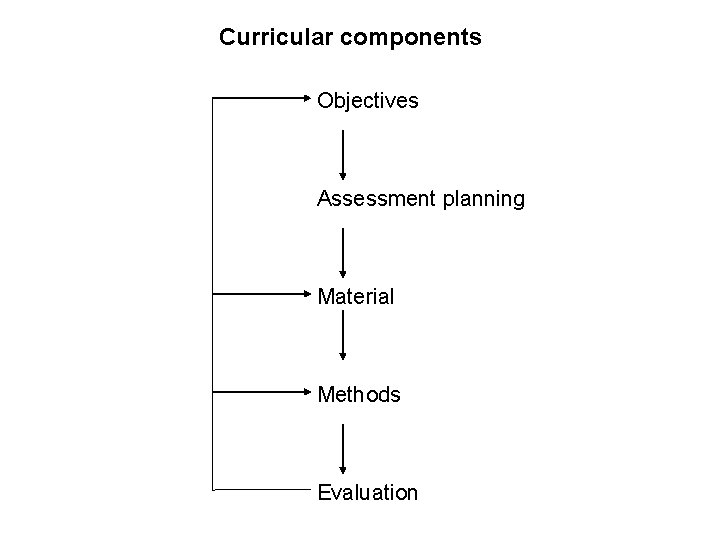
Curricular components Objectives Assessment planning Material Methods Evaluation
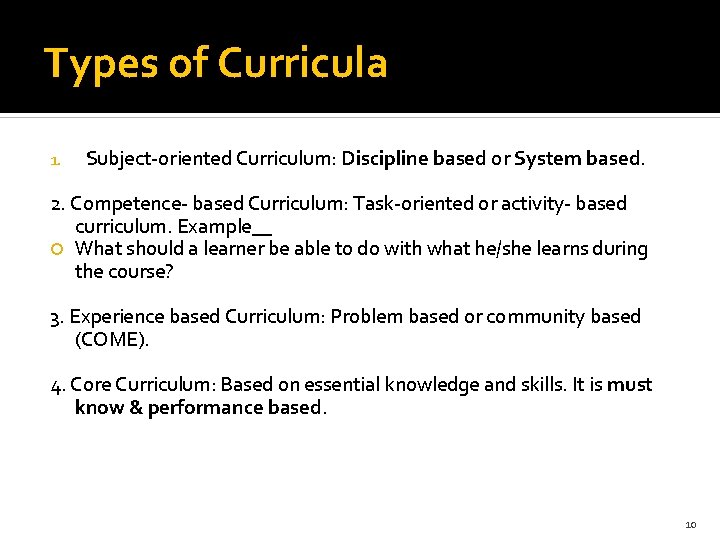
Types of Curricula 1. Subject-oriented Curriculum: Discipline based or System based. 2. Competence- based Curriculum: Task-oriented or activity- based curriculum. Example__ What should a learner be able to do with what he/she learns during the course? 3. Experience based Curriculum: Problem based or community based (COME). 4. Core Curriculum: Based on essential knowledge and skills. It is must know & performance based. 10
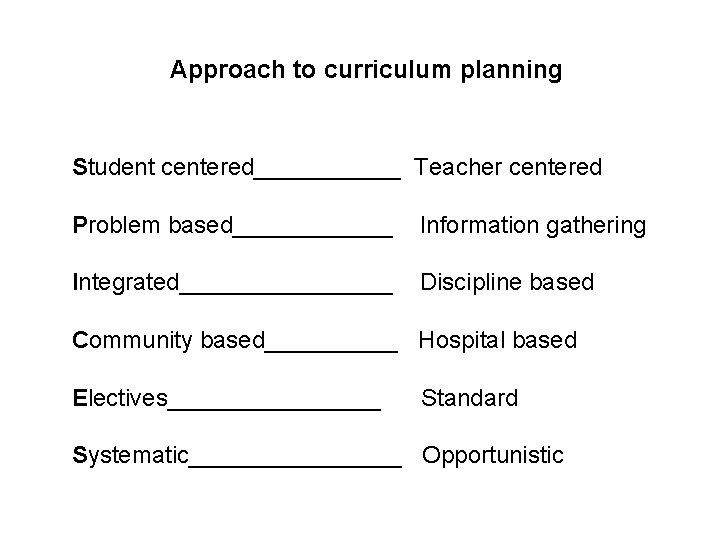
Approach to curriculum planning Student centered______ Teacher centered Problem based______ Information gathering Integrated________ Discipline based Community based_____ Hospital based Electives________ Standard Systematic________ Opportunistic

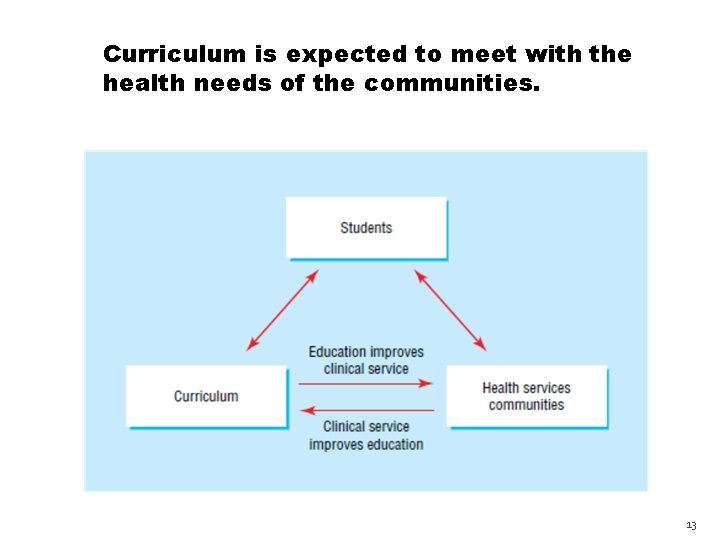
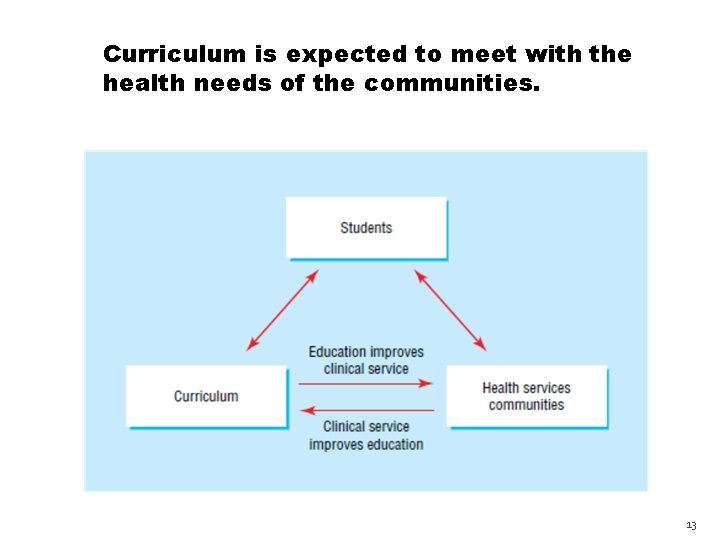
Curriculum is expected to meet with the health needs of the communities. 13
Vision 2015 – Where it Stands ?
Vision 2015 Addressing the areas of graduate and postgraduate medical education including examination patterns ethics of medical practice, equivalence of various degrees and courses enhancement of remunerations for medical teachers and setting up standards for accreditation of medical colleges. .
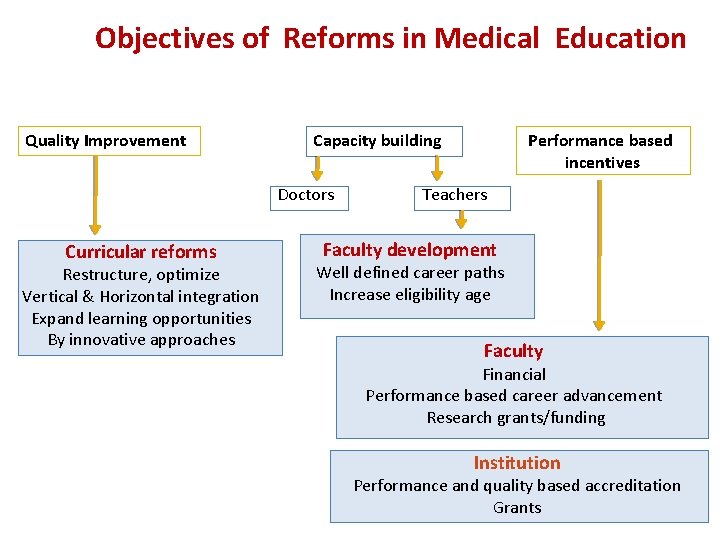
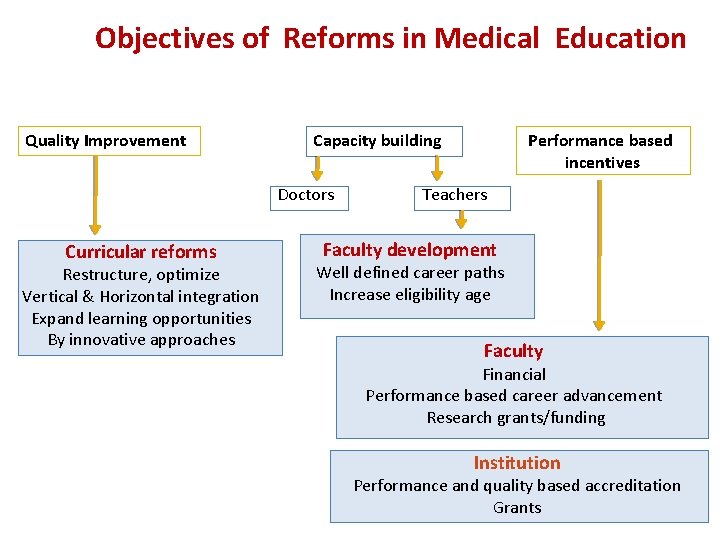
Objectives of Reforms in Medical Education Quality Improvement Capacity building Doctors Curricular reforms Restructure, optimize Vertical & Horizontal integration Expand learning opportunities By innovative approaches Performance based incentives Teachers Faculty development Well defined career paths Increase eligibility age Faculty Financial Performance based career advancement Research grants/funding Institution Performance and quality based accreditation Grants
Vision 2015 To standardize the output of graduate medical education in the form of an ‘Indian Medical Graduate’ A skilled and motivated basic doctor.
Vision 2015 These reforms focus on enhancing integration, clinical competency, flexibility and improvement in quality of training
Theme Global Trends Indian context Locally relevant and feasible changes
Curricular reforms To systematically address issues Develop strategies to strengthen the medical education and health care system So that indian medical graduates match or better the international standards.
Recommendations of UG group Foundation Course Early Clinical Exposure Integration – Vertical and Horizontal Skill Training / Competency based Training Electives Student doctor method of Clinical Training Secondary Hospital Exposure Newer teaching techniques – skill labs etc Community Oriented Education
Recommendations of UG group Foundation Course Early Clinical Exposure Integration – Vertical and Horizontal Skill Training / Competency based Training Electives Student doctor method of Clinical Training Secondary Hospital Exposure Newer teaching techniques – skill labs etc Community Oriented Education
Foundation course: 24
Goal Foundation Course ▪ Goal: The goal of the Foundation Course is to prepare a student to study medicine effectively. It will be of two months duration after admission.
Objectives of Foundation Course A. Orientation of student to Medical profession & physician’s role in society MBBS program Alternate health systems in country Medical ethics, attitude and professionalism Health care system and its delivery
Objectives of Foundation Course A. Orientation of student to National health priorities and policies Patient safety and biohazard safety Principles of family practice Indian medical graduate document of MCI The medical college and hospital
Objectives of Foundation Course B. Enable students to acquire skills in Language Interpersonal relationship Communication Learning skills including self directed learning Time management Stress management Use of information technology
Objectives of Foundation Course C. Train the student to provide First aid Basic life support
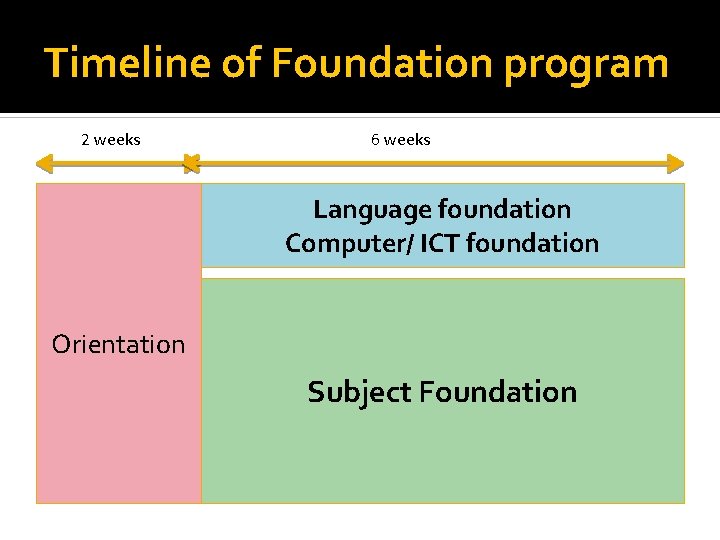
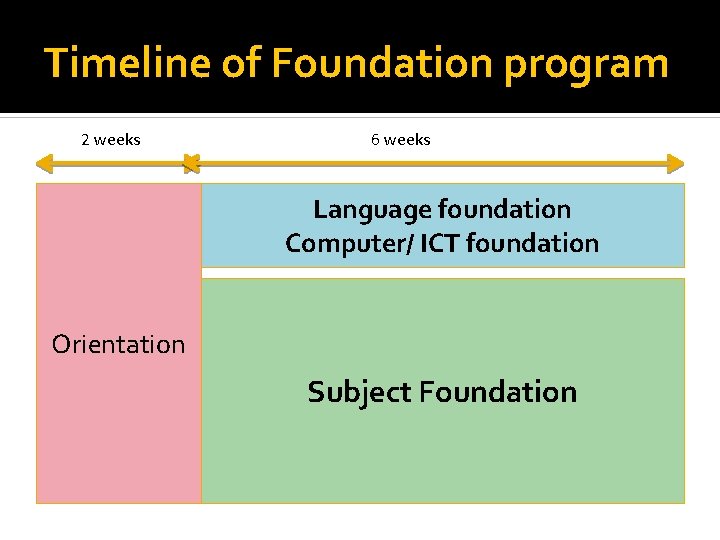
Timeline of Foundation program 2 weeks 6 weeks Language foundation Computer/ ICT foundation Orientation Subject Foundation
Early clinical exposure (ECE) 31
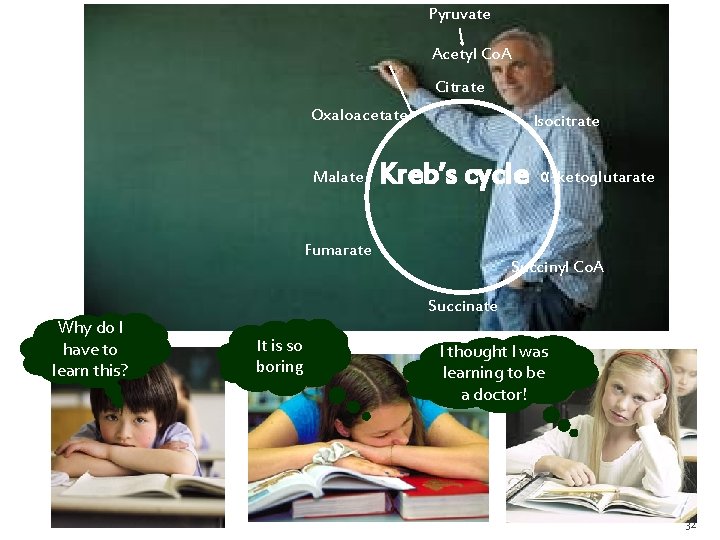
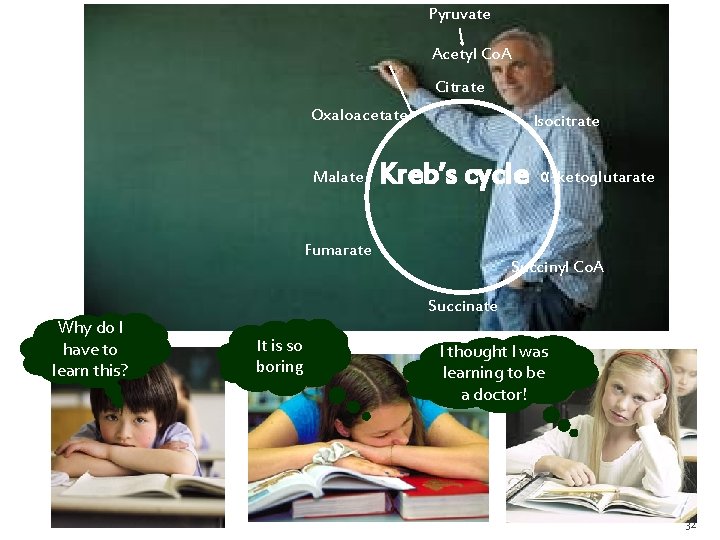
Pyruvate Acetyl Co. A Citrate Oxaloacetate Malate Isocitrate Kreb’s cycle Fumarate Why do I have to learn this? α-ketoglutarate Succinyl Co. A Succinate It is so boring I thought I was learning to be a doctor! 32
Concept and definitions 33
Early Clinical Exposure (ECE) is a teaching learning methodology, which fosters exposure of the medical students to the patients as early as the first year of medical college. Observation during Early Clinical Exposure- an effective instructional tool or a bore Elizabeth K. Medical Education. 2003, 37: 88 -89.
Pre-clinical disciplines Clinical disciplines 35
ECE? Why ECE? . Elizabeth K. Medical Education. 2003, 37: 88 -89 36
ECE? The goals of ECE are to provide • context and relevance to basic science teaching • some gain in medical knowledge • few basic clinical skills and • wide range of attitudes. . Elizabeth K. Medical Education. 2003, 37: 88 -89 37
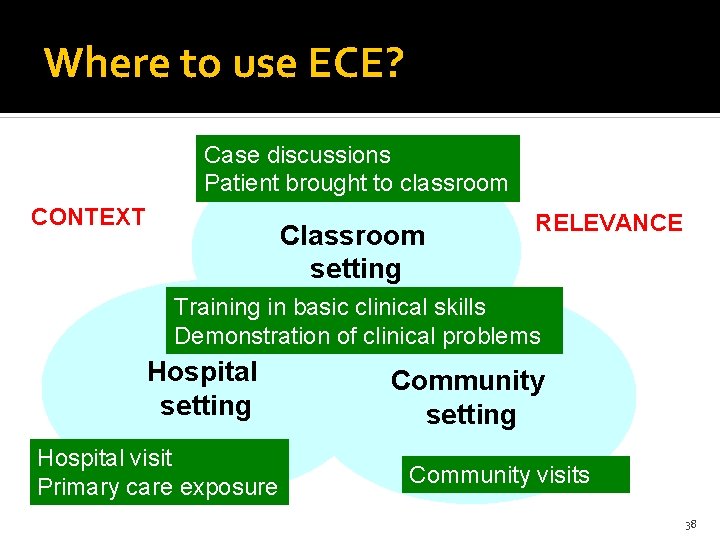
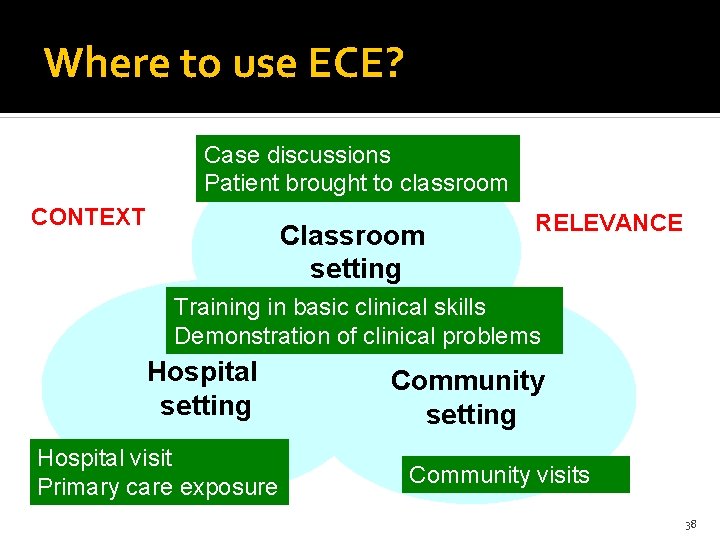
Where to use ECE? Case discussions Patient brought to classroom CONTEXT Classroom setting RELEVANCE Training in basic clinical skills Demonstration of clinical problems Hospital setting Hospital visit Primary care exposure Community setting Community visits 38
Using cases to teach in the class Paper cases Photographs X-rays Laboratory reports ECG 39
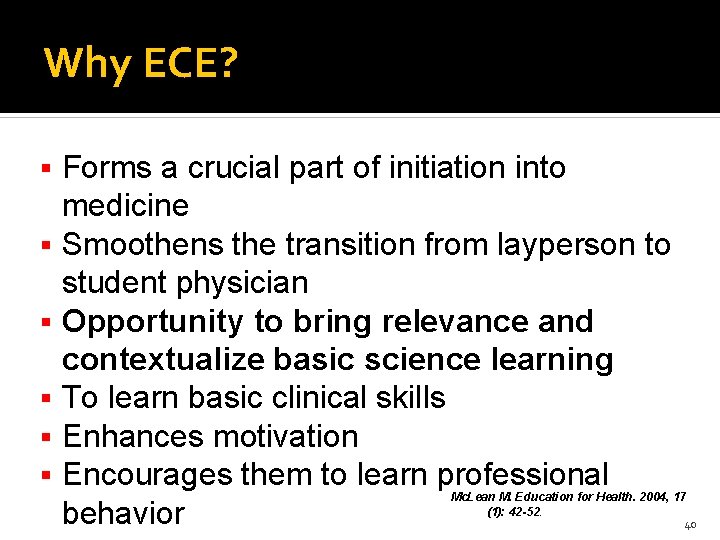
Why ECE? Forms a crucial part of initiation into medicine Smoothens the transition from layperson to student physician Opportunity to bring relevance and contextualize basic science learning To learn basic clinical skills Enhances motivation Encourages them to learn professional behavior Mc. Lean M. Education for Health. 2004, 17 (1): 42 -52. 40
Integrated Teaching & Learning

What Do you understand by Integrated teaching?
Integration is the organization of teaching matter to interrelate or unify subjects frequently taught in separate academic courses or departments (Harden et al, 1984) Occurs when relevant components of the curriculum are connected and related in meaningful ways by both the students and teachers.
Need for integration Integrated teaching just makes sense! It is just like eating biryani. . . You’d never eat rice, salt, oil, turmeric, chicken, eggs, mint and masalas separately!
Need for integration Avoids redundancy and duplication Promotes learning in context Meaningful and relevant learning Seeks to integrate contents across basic and clinical sciences Better retention (Rosse, 1974) Promotes faculty communication
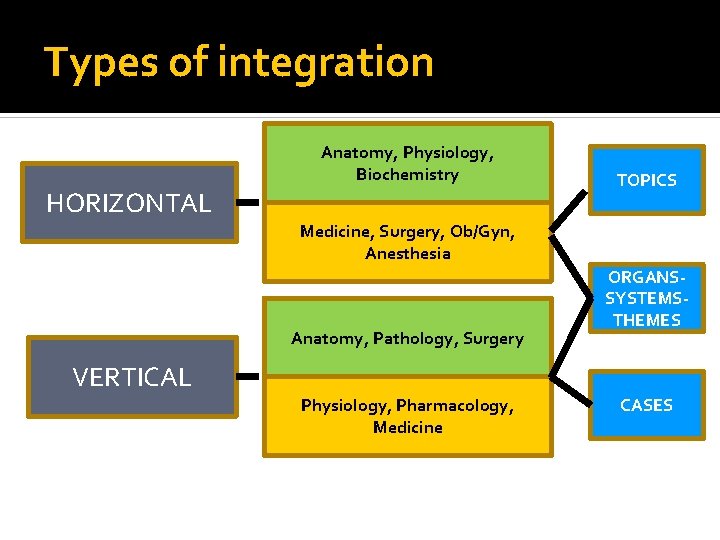
Types of integration
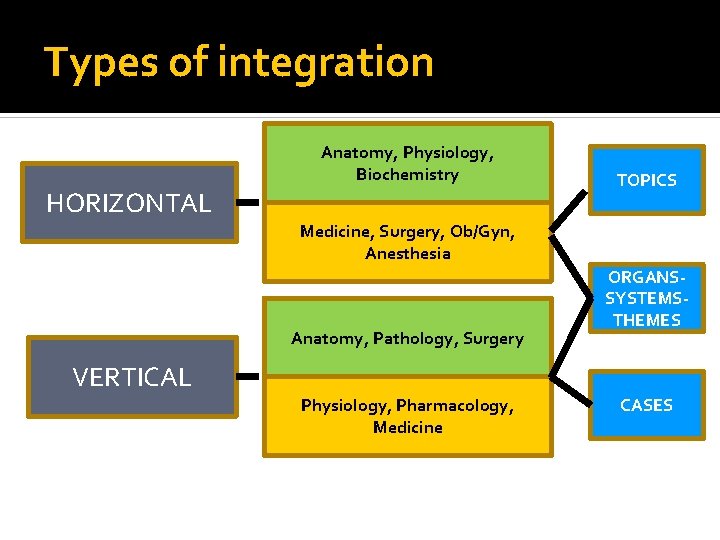
Types of integration Anatomy, Physiology, Biochemistry HORIZONTAL TOPICS Medicine, Surgery, Ob/Gyn, Anesthesia Anatomy, Pathology, Surgery ORGANS- SYSTEMSTHEMES VERTICAL Physiology, Pharmacology, Medicine CASES
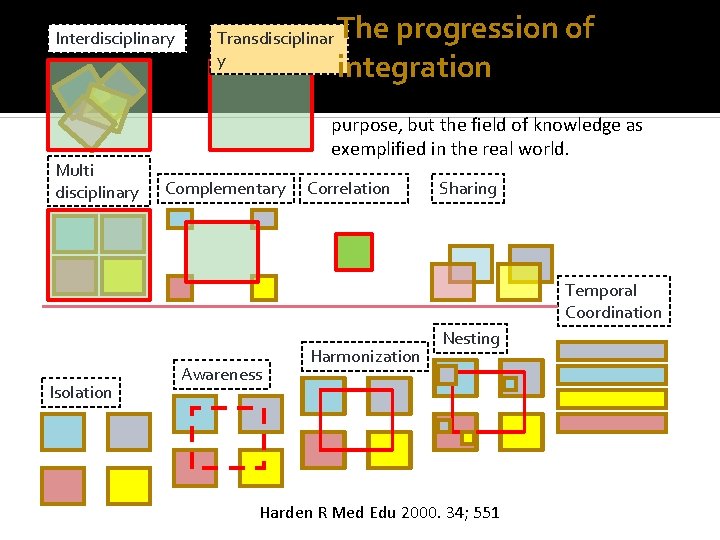
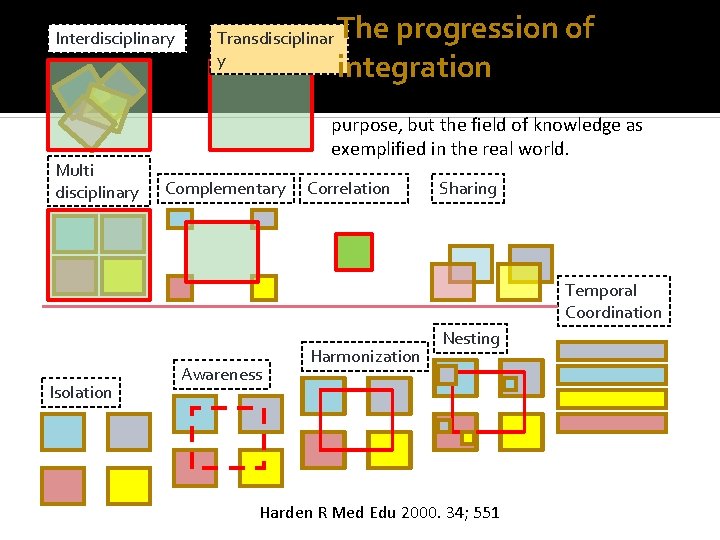
Interdisciplinary Multi disciplinary Transdisciplinar y The progression of integration not a theme or topic selected for this purpose, but the field of knowledge as exemplified in the real world. Complementary Correlation Sharing Temporal Coordination Isolation Awareness Harmonization Nesting Harden R Med Edu 2000. 34; 551
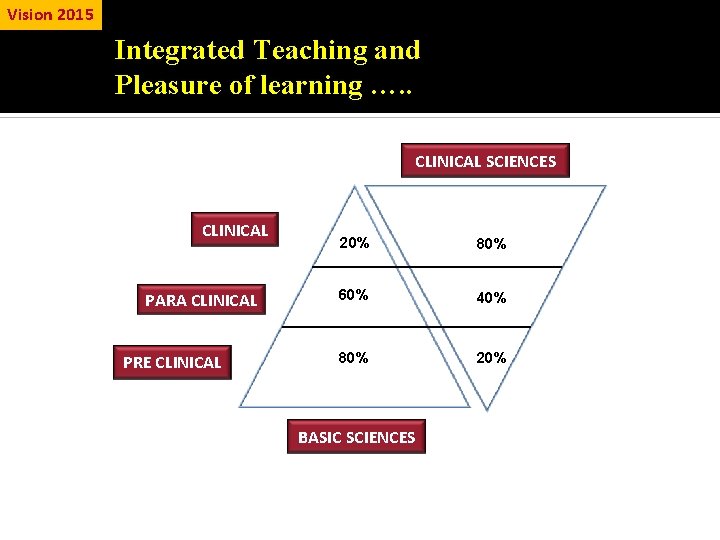
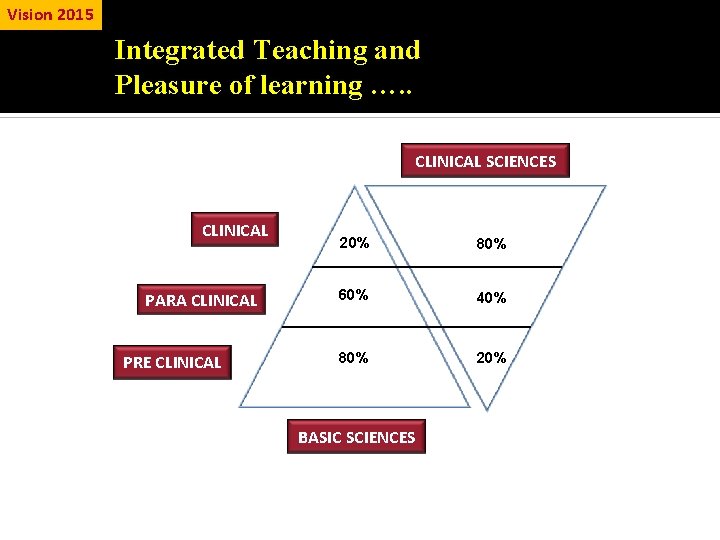
Vision 2015 Integrated Teaching and Pleasure of learning …. . CLINICAL SCIENCES CLINICAL PARA CLINICAL PRE CLINICAL 20% 80% 60% 40% 80% 20% BASIC SCIENCES
Problems in implementation
Some problems in implementation Lack of will Leadership support Infrastructure Resources Implementation of change: mindsets, resistance, more work

Strategies for implementation Integ rated Teac hing
Communication Skills Doctor – Patient Communication Interpersonal communication Team communication
Electives The elective postings are of two months each at the end of the II MBBS (elective 1) and III MBBS Part I (elective 2). 56
Some of the options: Emergency medicine Preventive cardiology Nutrition Medicolegal aspects Diabetes Sports medicine Medical education Research methodology Mental health 57
Student Doctor Method of Clinical Training Learning through clerkship/ student doctor method by involvement in patient care as a team member in investigations, management and performance of basic procedures Focus on common problem seen in OPD & emergency To provide sufficient skills development for competent practice
Student Doctor Method of Clinical Training Emphasis on a significant part of training at primary & secondary level with compulsory family medicine training. Restructuring clinical training so that parts of it would be ‘core’ requirements and others would be ‘elective’ postings.
Skill Development & Training A mandatory & desirable comprehensive list of skills has been planned and would be recommended for MBBS Graduate. Certification of skills would be necessary before licensure.
Secondary Hospital Exposure Each medical college would be linked to the local health system -including CHCs, taluka hospitals & PHC centers -that can be used as training base for medical students
Where to incorporate these changes?
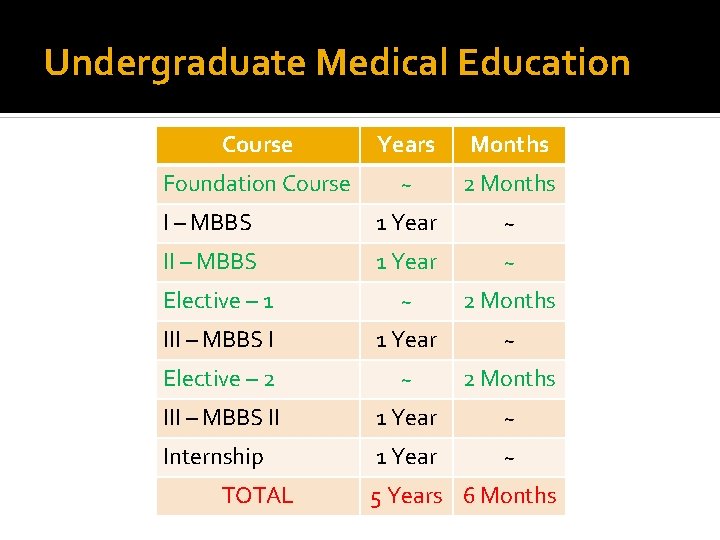
Improving quality of training Restructuring the Undergraduate medical course total duration of MBBS course will remain 5 ½ years. course will be restructured to enable student to be more participatory and competent.
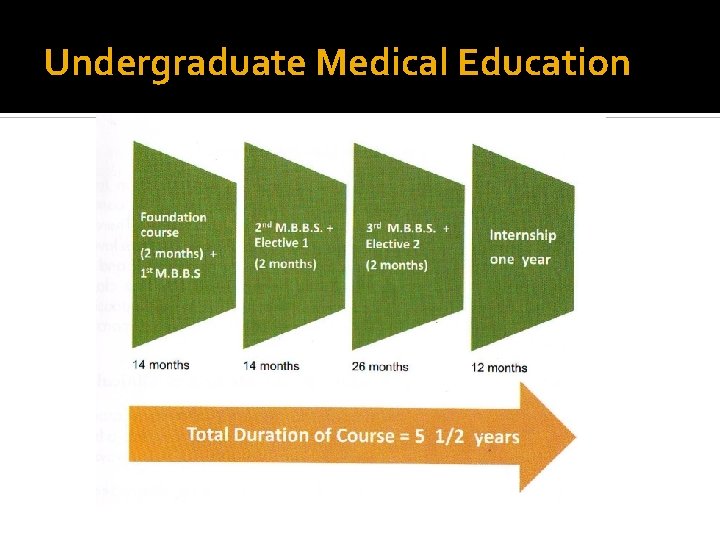
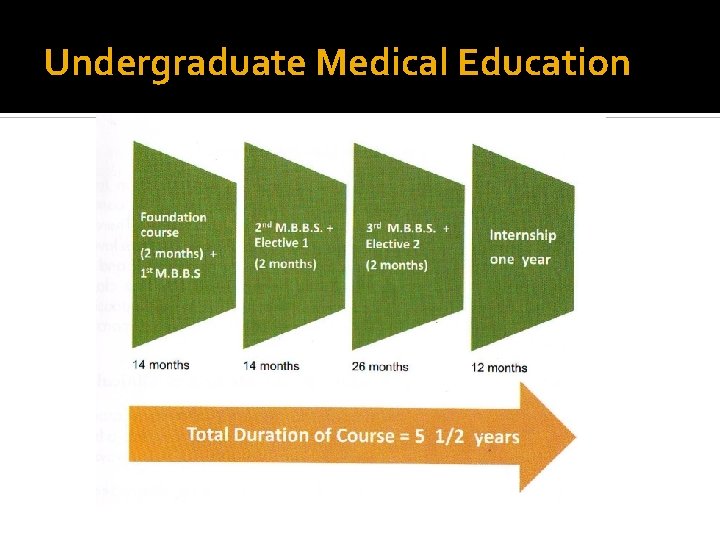
Undergraduate Medical Education
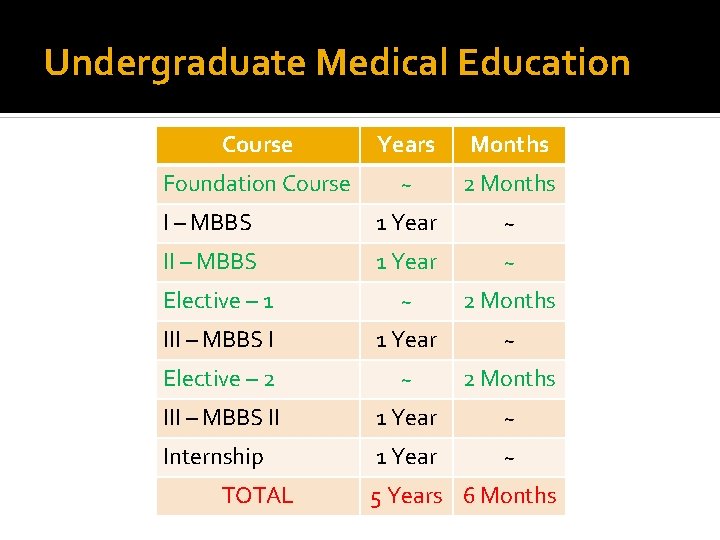
Undergraduate Medical Education Course Years Months Foundation Course ~ 2 Months I – MBBS 1 Year ~ II – MBBS 1 Year ~ Elective – 1 ~ 2 Months III – MBBS I 1 Year ~ Elective – 2 ~ 2 Months III – MBBS II 1 Year ~ Internship 1 Year ~ TOTAL 5 Years 6 Months
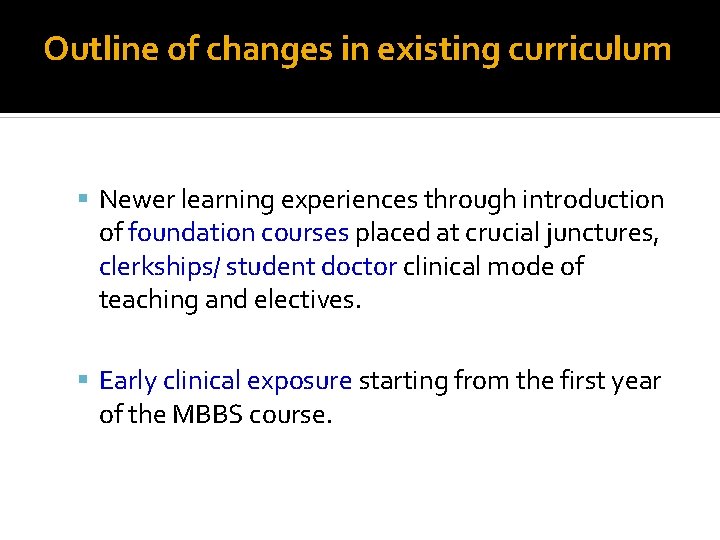
Outline of changes in existing curriculum Newer learning experiences through introduction of foundation courses placed at crucial junctures, clerkships/ student doctor clinical mode of teaching and electives. Early clinical exposure starting from the first year of the MBBS course.
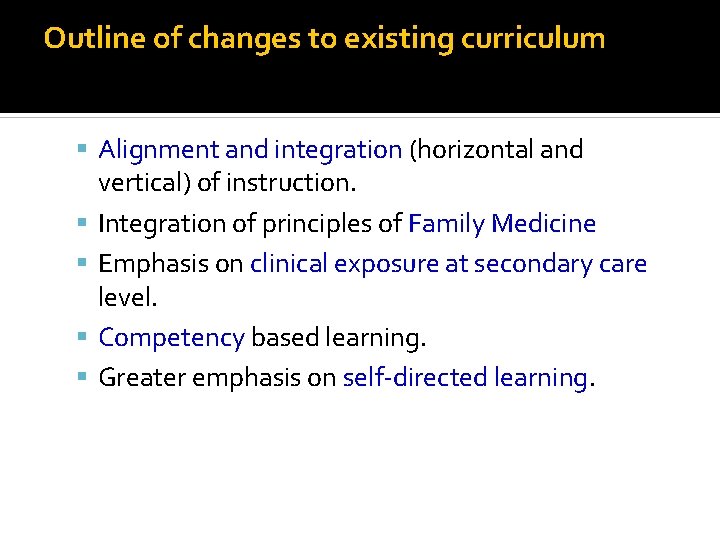
Outline of changes to existing curriculum Alignment and integration (horizontal and vertical) of instruction. Integration of principles of Family Medicine Emphasis on clinical exposure at secondary care level. Competency based learning. Greater emphasis on self-directed learning.
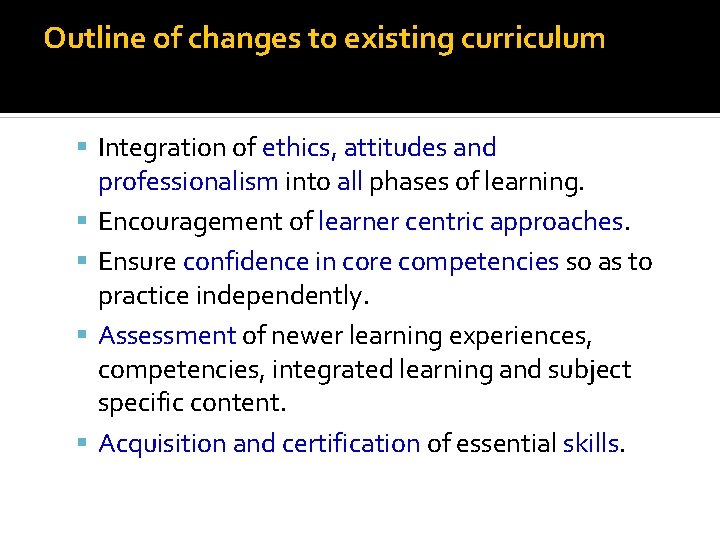
Outline of changes to existing curriculum Integration of ethics, attitudes and professionalism into all phases of learning. Encouragement of learner centric approaches. Ensure confidence in core competencies so as to practice independently. Assessment of newer learning experiences, competencies, integrated learning and subject specific content. Acquisition and certification of essential skills.




Implementation 73
Task -25 min Divide into 4 groups Discuss your implementation Do force field analysis • Foundation course • ECE • Integrated system • Clinical skill Present to the class strategies 74
Challenges of Implementation Multiple level – Change, Multiple Stakeholders Cost of Change Making change happen at departmental level
Change Involves Shedding beliefs Cognitive structuring Faculty development
Curriculum Implementation Support Program 77
Approach- CISP Faculty Development Program to support curricular Innovations Capacity development across the country Develop guidelines and supportive documents
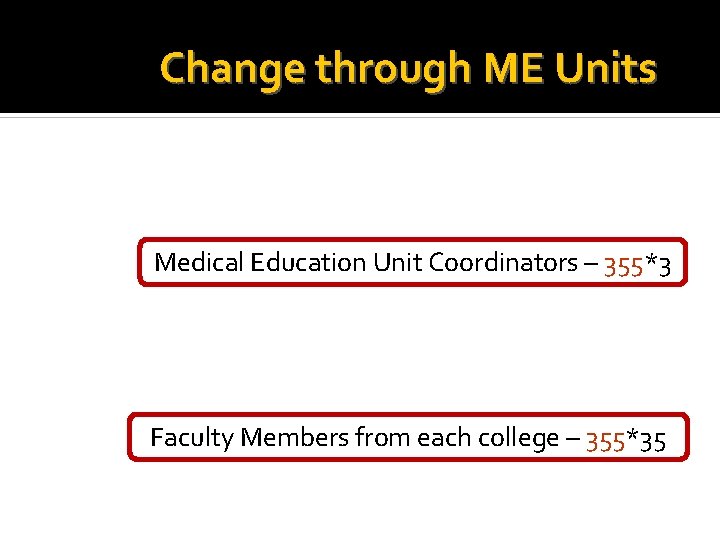
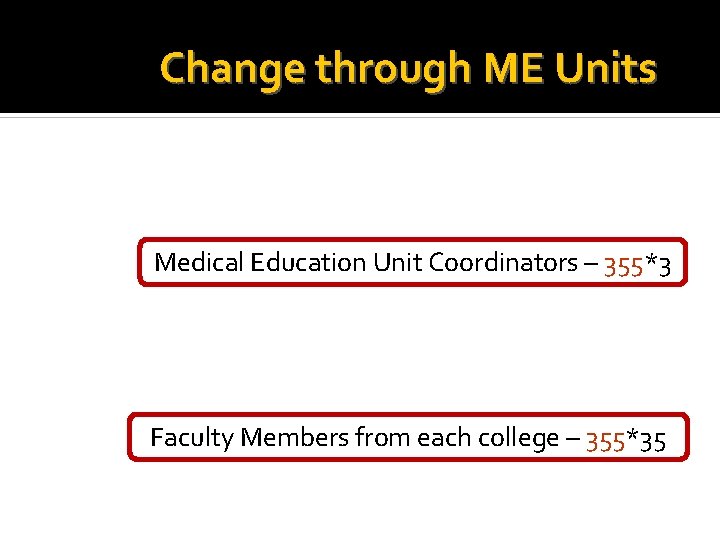
Change through ME Units Medical Education Unit Coordinators – 355*3 Faculty Members from each college – 355*35

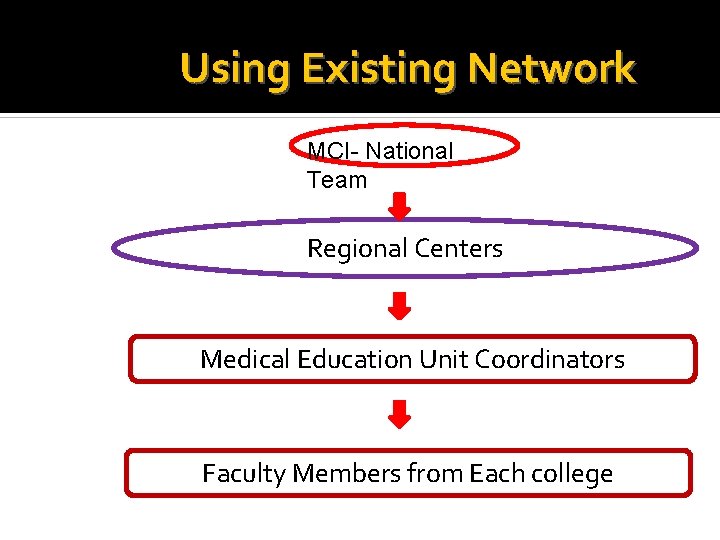
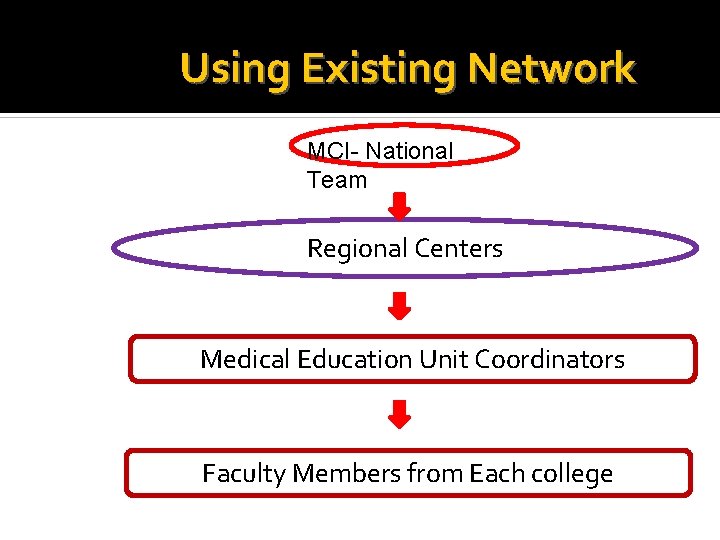
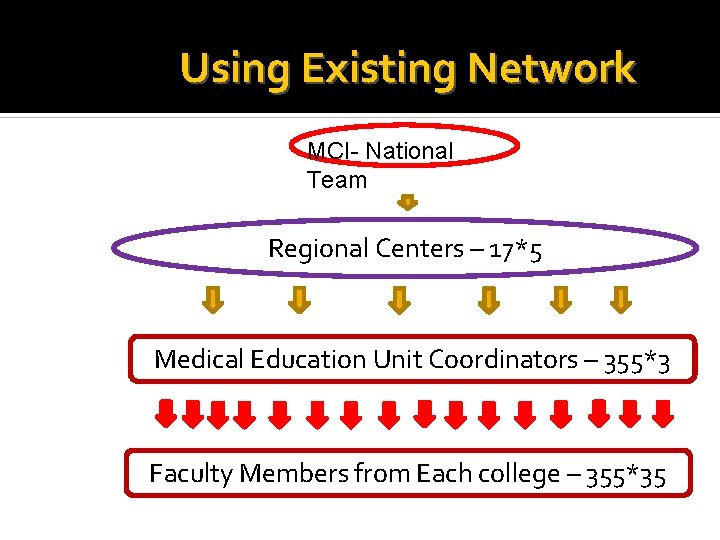
Using Existing Network MCI- National Team Regional Centers Medical Education Unit Coordinators Faculty Members from Each college
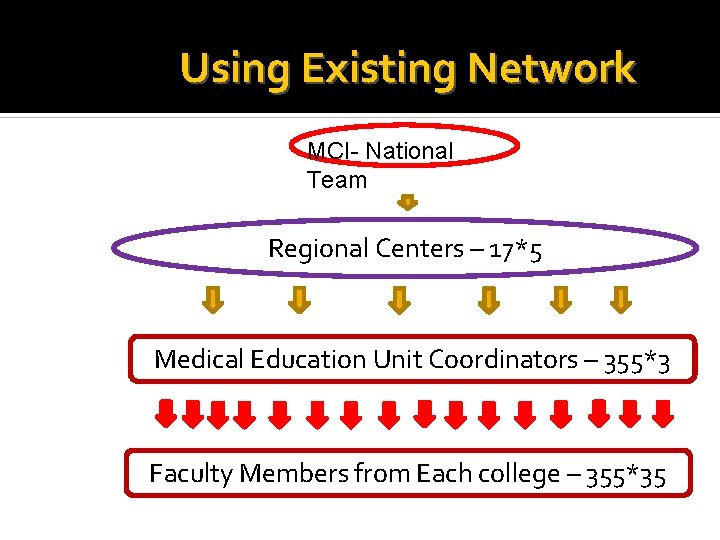
Using Existing Network MCI- National Team Regional Centers – 17*5 Medical Education Unit Coordinators – 355*3 Faculty Members from Each college – 355*35
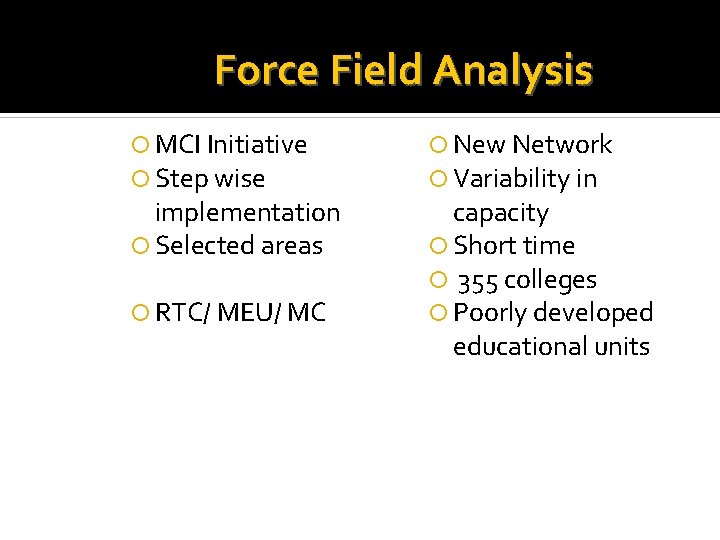
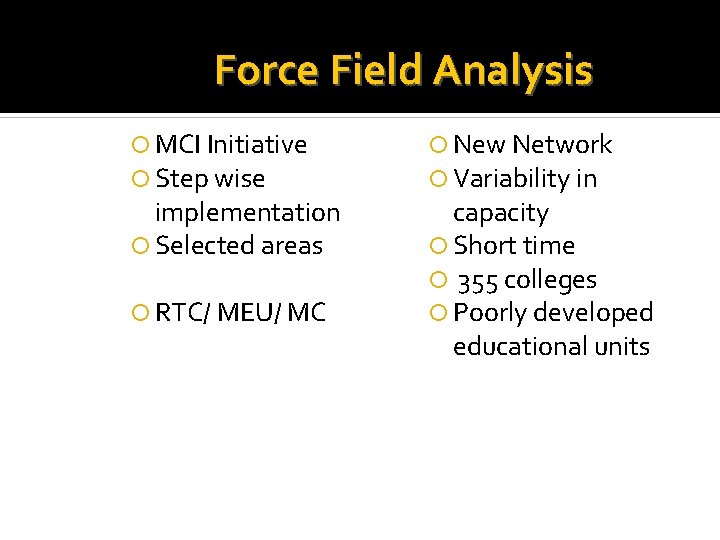
Force Field Analysis MCI Initiative Step wise implementation Selected areas RTC/ MEU/ MC New Network Variability in capacity Short time 355 colleges Poorly developed educational units
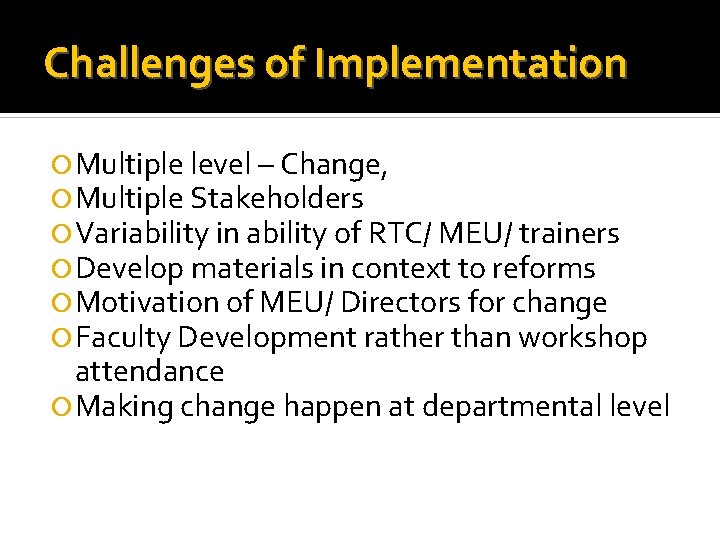
Challenges of Implementation Multiple level – Change, Multiple Stakeholders Variability in ability of RTC/ MEU/ trainers Develop materials in context to reforms Motivation of MEU/ Directors for change Faculty Development rather than workshop attendance Making change happen at departmental level
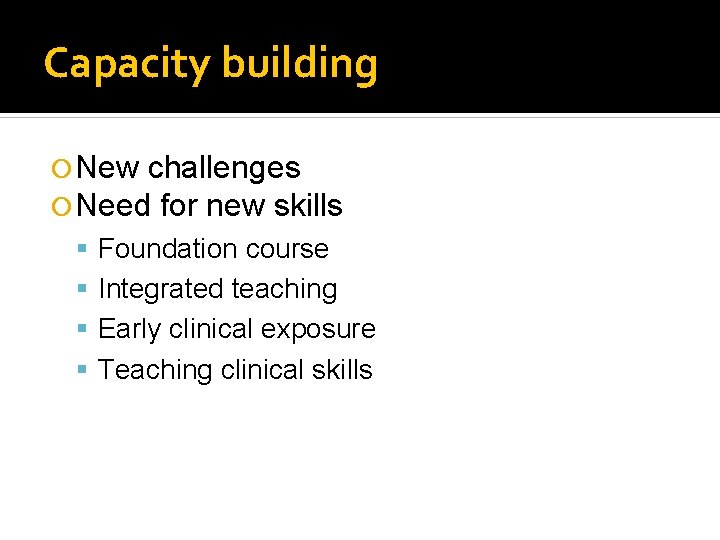
Capacity building New challenges Need for new skills Foundation course Integrated teaching Early clinical exposure Teaching clinical skills
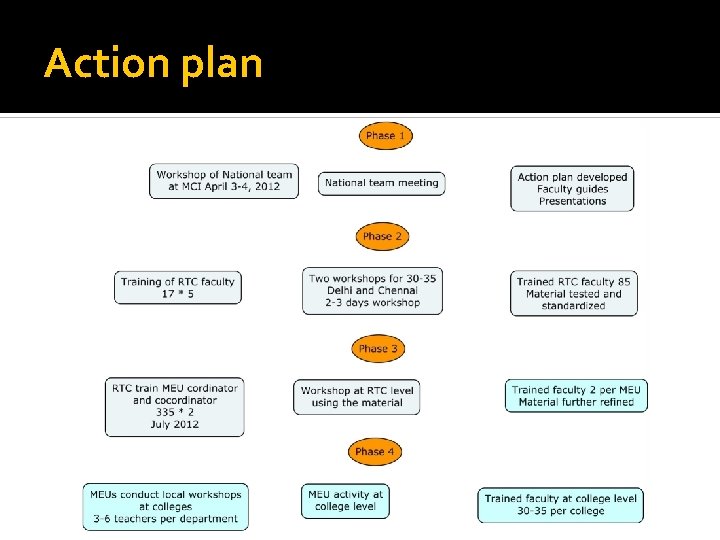
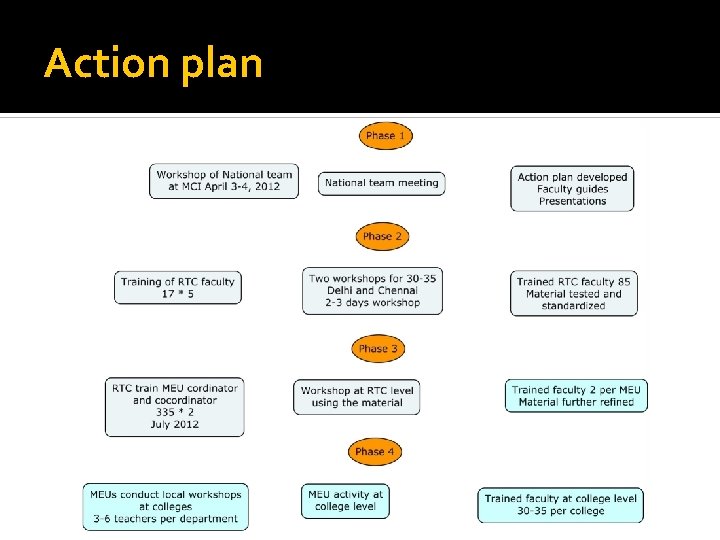
Action plan
At the end of each year 88
Enthusiasm is the father of excellence. B. A. Johnson 89