Introduction to Blood Bank Rotation What is Transfusion
Introduction to Blood Bank Rotation
What is Transfusion Medicine? TM is the practice of laboratory and clinical medicine concerned with all aspects of blood transfusion (scientific basis, selection, recruitment of blood donors, utilization and quality control, preparation of blood componenets, pretransfusion testing, transfusion of components, adverse effects), autoimmunity, transplantation, histocomatibility, therapeutic apheresis, blood substitutes, management of aspects of blood services (regulatory). TM needs a strong foundation in laboratory medicine and clinical medicine.
Scope of TM is broad? • • Immunohematology Hemostasis HLA Blood collection operations Apheresis Stem cell collection Cellular therapies/cell processing Tissue services
How to maximize your time on the blood bank? • Active engagement in TM! – Question and answer during didactic teaching session – Take notes! Especially on facts unfamiliar to you! – Use clinical scenario to spur additional content reading – Identify gaps in knowledge base and request specific lectures/didactic session
What Do I Need To Know? • The Serologic work ups, transfusion reactions • The Pager • The Platelets • The Patients • The Project
What Do I Need To Know? • The Paperwork • The Pager • The Platelets • Patients • Apheresis • ECP • RBC exchange • Benchwork: Please organize with attending and lead staff • ARC rotation: Please arrange rotation at Nashville ARC with Dr. Meena-Leist (Young) in second month of rotation through BB • The Project
1. Pick up paperwork in AM
ABO type/Antibody Screen • Please understand the work-up. If you don’t, please know that you are encouraged to talk to staff. • Antibody screen looks for alloantibodies other than ABO that can cause hemolysis – involves adding patient plasma to two or three O- test cells that are chosen to represent all clinically significant antigens – any positive screen must be worked-up with antibody panel to identify responsible antibody
Antibody Panel • Similar to antibody screen except involves usually 10 different test cells – antigens on negative test cells are not responsible for positive screen – identify alloantibody present by process of elimination
DAT • Positive DAT means something is coating the patient’s red blood cells – That may target this cell for destruction –check Hgb/Hct trend, LDH, indirect (or total) bilirubin, haptoglobin, hemoglobinuria, reticulocyte count, and peripheral blood smear findings – check clinical status of patient –Please do not come to rounds without looking these up. Please do not state in your note only the results of the test without any guidance
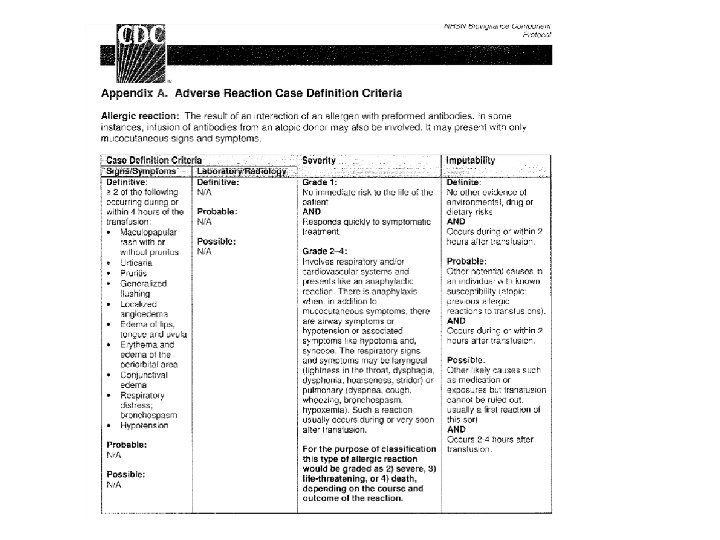
Transfusion Reactions • Paperwork appears after the resident on call has been notified (usually the next day) • Look up clinical history and appropriate labs – which product is implicated? how much volume? – changes in vital signs? Are the changes unique to the transfusion? – changes in Hgb/Hct, LDH, bilirubin, haptoglobin, etc. – how was the patient managed by clinical team (did they give Benadryl or Tylenol, or subsequent transfusions)? – how is the patient currently doing?
Transfusion Reactions • usually workup is underway/completed by the time resident is paged • workup includes: – stop the transfusion! – paperwork & bag check for clerical errors – check blood for hemolysis (visually) for hemoglobin –perform DAT (and compare to pretransfusion sample) – send bag and blood sample for culture if indicated
AHTR-clinical evaluation
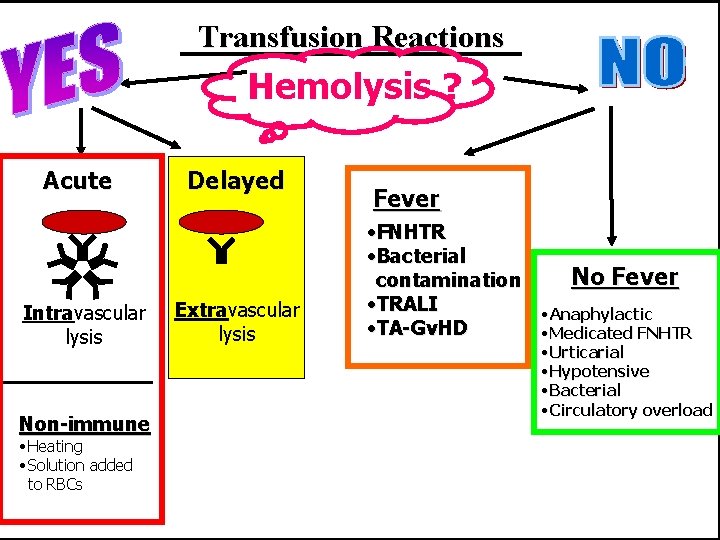
Transfusion Reactions Hemolysis ? Acute Intravascular lysis Non-immune • Heating • Solution added to RBCs Delayed Extravascular lysis Fever • FNHTR • Bacterial No Fever contamination • TRALI • Anaphylactic • TA-Gv. HD • Medicated FNHTR • Urticarial • Hypotensive • Bacterial • Circulatory overload
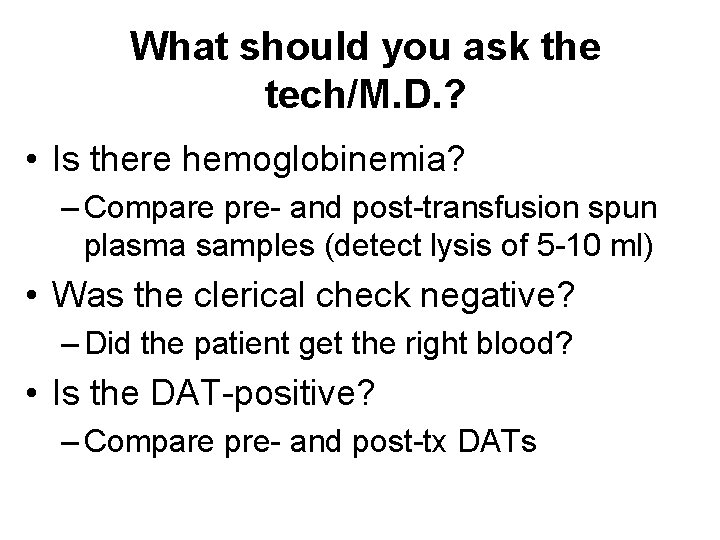
What should you ask the tech/M. D. ? • Is there hemoglobinemia? – Compare pre- and post-transfusion spun plasma samples (detect lysis of 5 -10 ml) • Was the clerical check negative? – Did the patient get the right blood? • Is the DAT-positive? – Compare pre- and post-tx DATs
What should you be asking yourself? • Is it a hemolytic reaction ? ? !!
Additional lab work • Repeat ABO/Rh, Ab screen, crossmatch • Urinalysis for hemoglobinuria • Coag studies if indicated • Review prior to approving next transfusion
Clinical management 1. STOP TRANSFUSION keep line open 2. Monitor vital signs, urine output 3. Evidence of a severe reaction? • AHTR, septic shock, anaphylaxis 4. Perform nursing clerical check 5. Return product to BB with new samples
Clinical management 6. Hypotension – Saline, Dopamine (1 mg/kg/hr) 7. Renal failure – Monitor urine output: keep >100 ml/hr X 24 hr – Monitor BUN, crt, lytes – Treat hypotension to prevent renal ischemia – Furosemide (20 -100 mg/12 hrs) – Dialysis
Clinical management 8. DIC – Monitor PT, PTT, fibrinogen, FSP, platelet ct – Heparin 40 IU/kg loading, 5 -6000 IU/12 hr – Transfuse as needed (FFP, plt)
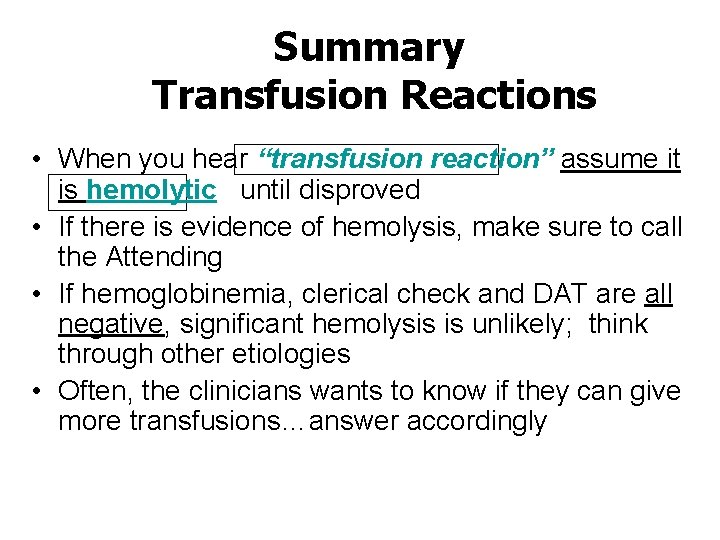
Summary Transfusion Reactions • When you hear “transfusion reaction” assume it is hemolytic until disproved • If there is evidence of hemolysis, make sure to call the Attending • If hemoglobinemia, clerical check and DAT are all negative, significant hemolysis is unlikely; think through other etiologies • Often, the clinicians wants to know if they can give more transfusions…answer accordingly
Biovigilance paperwork

What Do I Need To Know? • The Paperwork • The Pager • The Platelets • The Patients • The Project
Pager Responsibility • Contact the blood bank attending with any issue about which you are unsure • Contact the attending about any mistransfusion, wrong blood in tube, anaphylactic/serious reactions, serious patient issues which if left not taken care of will result in morbidity or mortality
Ways to present to your attending on-call in general • When you call the attending make sure you have a one-liner about what is going on • Know the age, gender, race, diagnosis, and the problem • Have all ducks in a row - know as much information as possible (labs, etc. ) This means calling not only the techs but also the clinicians prior to calling TMP attending. • Have a plan of your own if possible(read a little)
Follow-up and Continuity • Critical as physicians • Check out to the TM day team if you were on call • Call me if there any issues overnight • During the day find out what happened to your patient. Do not wait a week to follow-up.
Paperwork/case handoff between residents • At the conclusion of the day and rotation it is not uncommon to have pending cases still being evaluated (i. e. cultures for transfusion reactions, additional immunohematology panels, etc…) • These cases must be discussed and properly handed off to the incoming resident • Keeping track of the paperwork is key! This is an FDA requirement!!!!
Handoff Duties • Inform weekend resident and the next month’s resident of any patients with ongoing product needs or other issues they will likely encounter • Give them any paperwork they might need in managing those patients
What Do I Need To Know? • The Paperwork • The Pager • The Platelets, product usages/product manipulations • The Patients • The Project
Platelets • Each day the blood bank staff will provide a list of all ABO (out of group) and Rh (incompatible) platelet transfusions – Review clinical history to determine impact of ABO out of group transfusions • Passive mediated hemolytic transfusion reaction evaluation – Rh- see Rh. IG evaluation
Improper Product Usage • Multiple Platelet Units – ideally a post-transfusion platelet count should be checked before administering additional platelet products • ensures patient is benefitting from transfusion • avoids alloantibody formation and/or potential transfusion reactions associated with a product that might not be of benefit to the patient • clinicians typically receptive to this request – exceptions DO EXIST: use clinical judgment
Platelet Refractoriness • progressive diminution in platelet increase following transfusion • arises due to alloimmunization in patients who have required multiple transfusions, most often associated with chemotherapy • other etiologies: systemic infection, splenomegaly, drugs, platelet consumption (DIC)
American Red Cross • Phone number: 615 -346 -7935 • Discuss platelet needs with clinicians – what are their goals? – when are platelets needed (generally ASAP)? – how many transfusions are anticipated daily? • Stay ahead of the game! – ARC needs notification and bloodwork by noon in order to get platelets for the next day – be proactive on Fridays in preparation for weekend transfusion needs
Apheresis Platelets • contain at least 3 x 1011 platelets • minimizes alloimmunization since only one donor exposure • expected platelet increase: ~30, 000/µL – consider refractoriness when increments progressively decrease – must prove refractoriness with two post-transfusion platelet counts obtained 15 minutes to 1 hour posttransfusion – if refractory to cross-matched platelets or attempt HLA-matched platelets
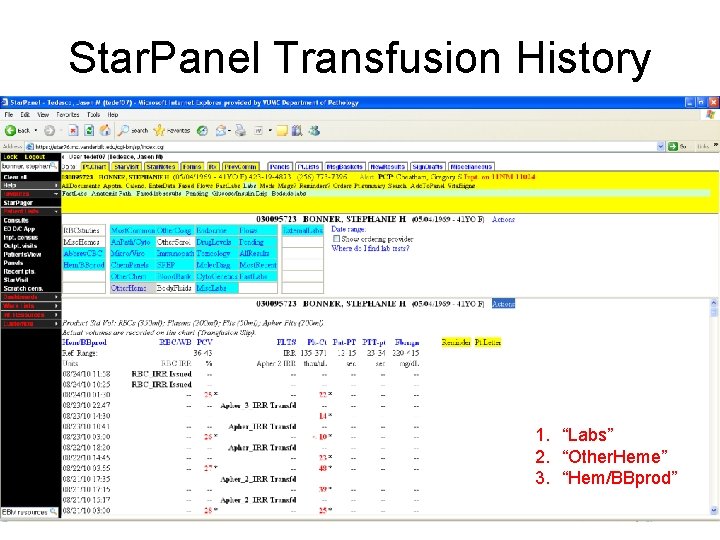
Star. Panel Transfusion History 1. “Labs” 2. “Other. Heme” 3. “Hem/BBprod”
Improper Product Usage • Washed Red Blood Cells – indications: • prevention of allergic reactions in Ig. A-deficient recipients • May also be indicated in severe allergic reactions • transfusion to neonates from a parent or from ABO incompatible plasma or to reduce K+ – NOT indications: • prevention of hemolytic transfusion reactions • prevention of alloimmunization • prevention of CMV transmission
What Do I Need To Know? • The Paperwork • The Pager • The Platelets • The Patients • The Project
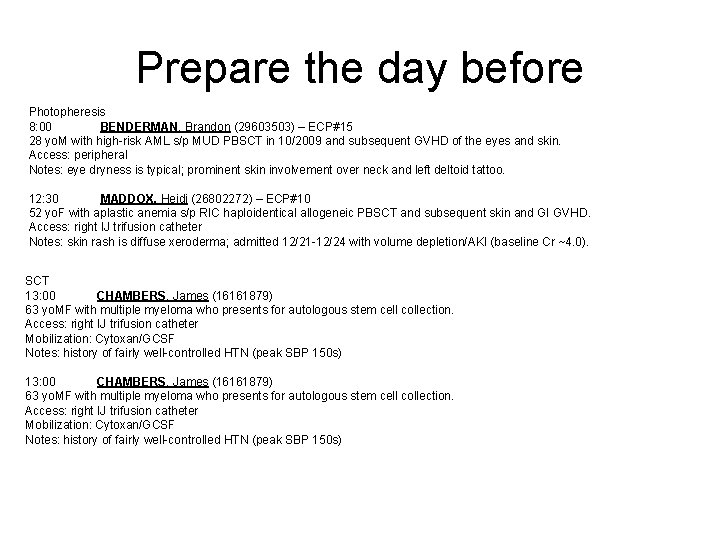
Prepare the day before Photopheresis 8: 00 BENDERMAN, Brandon (29603503) – ECP#15 28 yo. M with high-risk AML s/p MUD PBSCT in 10/2009 and subsequent GVHD of the eyes and skin. Access: peripheral Notes: eye dryness is typical; prominent skin involvement over neck and left deltoid tattoo. 12: 30 MADDOX, Heidi (26802272) – ECP#10 52 yo. F with aplastic anemia s/p RIC haploidentical allogeneic PBSCT and subsequent skin and GI GVHD. Access: right IJ trifusion catheter Notes: skin rash is diffuse xeroderma; admitted 12/21 -12/24 with volume depletion/AKI (baseline Cr ~4. 0). SCT 13: 00 CHAMBERS, James (16161879) 63 yo. MF with multiple myeloma who presents for autologous stem cell collection. Access: right IJ trifusion catheter Mobilization: Cytoxan/GCSF Notes: history of fairly well-controlled HTN (peak SBP 150 s)
SCT/Photopheresis • Stem cells are collected from peripheral blood from patients as well donors after appropriate mobilization of these cells from the bone marrow. • The collection is by apheresis • Patients who are suffering from chronic GVHD or solid organ transplant rejection (more rare) occasionally receive extra corporeal photopheresis. This involves treating buffy coat with 6 -MOP under UV to effect immunomodulations. • Responsibilities include – See each patient – Establish working relationship with nurses • Write note (template available) on the day of the procedure (M-F) • Address any mild adverse reactions
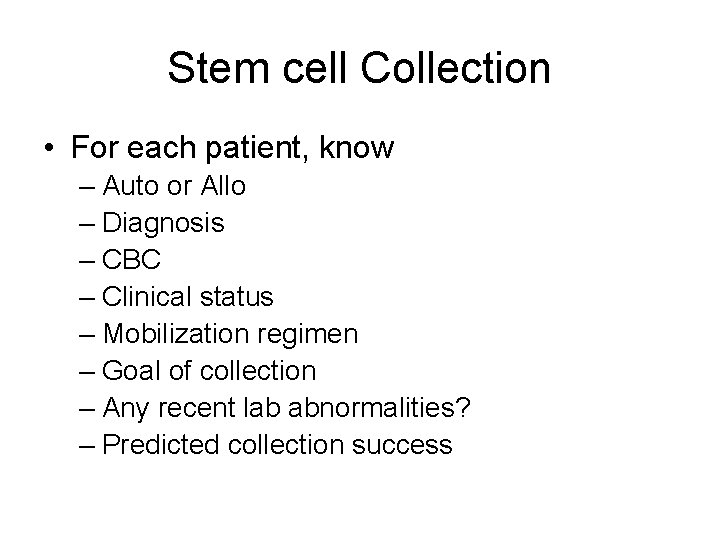
Stem cell Collection • For each patient, know – Auto or Allo – Diagnosis – CBC – Clinical status – Mobilization regimen – Goal of collection – Any recent lab abnormalities? – Predicted collection success
Photopheresis • For each patient, know – Clinical status (how stable are they? ) – Reason for photopheresis • What are their clinical manifestations – Number of procedures thus far – CBC – Any recent lab abnormalities
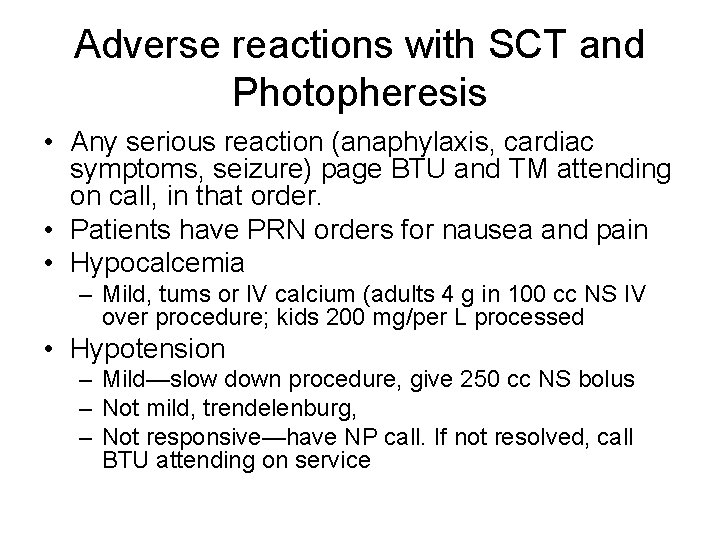
Adverse reactions with SCT and Photopheresis • Any serious reaction (anaphylaxis, cardiac symptoms, seizure) page BTU and TM attending on call, in that order. • Patients have PRN orders for nausea and pain • Hypocalcemia – Mild, tums or IV calcium (adults 4 g in 100 cc NS IV over procedure; kids 200 mg/per L processed • Hypotension – Mild—slow down procedure, give 250 cc NS bolus – Not mild, trendelenburg, – Not responsive—have NP call. If not resolved, call BTU attending on service
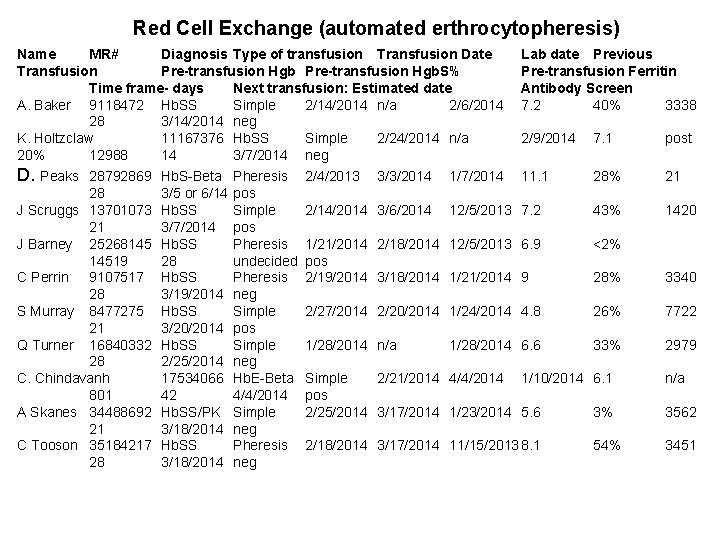
Red Cell Exchange (automated erthrocytopheresis) Name MR# Diagnosis Type of transfusion Transfusion Date Lab date Previous Transfusion Pre-transfusion Hgb. S% Pre-transfusion Ferritin Time frame- days Next transfusion: Estimated date Antibody Screen A. Baker 9118472 Hb. SS Simple 2/14/2014 n/a 2/6/2014 7. 2 40% 3338 28 3/14/2014 neg K. Holtzclaw 11167376 Hb. SS Simple 2/24/2014 n/a 2/9/2014 7. 1 post 20% 12988 14 3/7/2014 neg D. Peaks 28792869 Hb. S-Beta Pheresis 2/4/2013 3/3/2014 1/7/2014 11. 1 28% 21 28 3/5 or 6/14 pos J Scruggs 13701073 Hb. SS Simple 2/14/2014 3/6/2014 12/5/2013 7. 2 43% 1420 21 3/7/2014 pos J Barney 25268145 Hb. SS Pheresis 1/21/2014 2/18/2014 12/5/2013 6. 9 <2% 14519 28 undecided pos C Perrin 9107517 Hb. SS Pheresis 2/19/2014 3/18/2014 1/21/2014 9 28% 3340 28 3/19/2014 neg S Murray 8477275 Hb. SS Simple 2/27/2014 2/20/2014 1/24/2014 4. 8 26% 7722 21 3/20/2014 pos Q Turner 16840332 Hb. SS Simple 1/28/2014 n/a 1/28/2014 6. 6 33% 2979 28 2/25/2014 neg C. Chindavanh 17534066 Hb. E-Beta Simple 2/21/2014 4/4/2014 1/10/2014 6. 1 n/a 801 42 4/4/2014 pos A Skanes 34488692 Hb. SS/PK Simple 2/25/2014 3/17/2014 1/23/2014 5. 6 3% 3562 21 3/18/2014 neg C Tooson 35184217 Hb. SS Pheresis 2/18/2014 3/17/2014 11/15/2013 8. 1 54% 3451 28 3/18/2014 neg
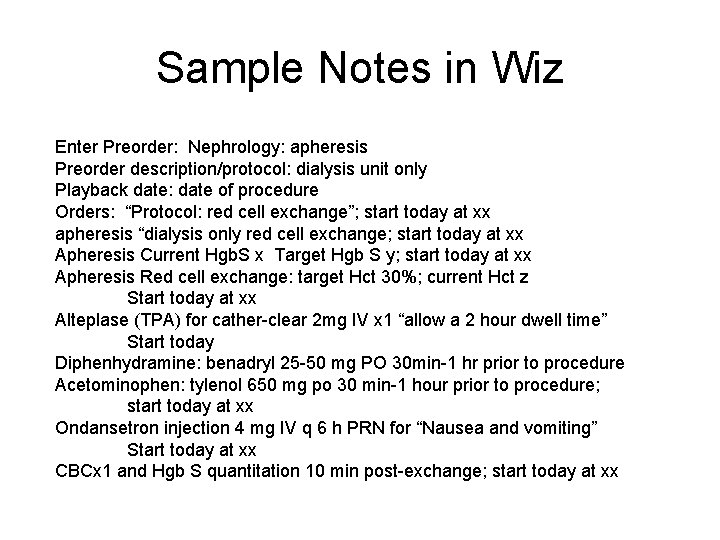
Sample Notes in Wiz Enter Preorder: Nephrology: apheresis Preorder description/protocol: dialysis unit only Playback date: date of procedure Orders: “Protocol: red cell exchange”; start today at xx apheresis “dialysis only red cell exchange; start today at xx Apheresis Current Hgb. S x Target Hgb S y; start today at xx Apheresis Red cell exchange: target Hct 30%; current Hct z Start today at xx Alteplase (TPA) for cather-clear 2 mg IV x 1 “allow a 2 hour dwell time” Start today Diphenhydramine: benadryl 25 -50 mg PO 30 min-1 hr prior to procedure Acetominophen: tylenol 650 mg po 30 min-1 hour prior to procedure; start today at xx Ondansetron injection 4 mg IV q 6 h PRN for “Nausea and vomiting” Start today at xx CBCx 1 and Hgb S quantitation 10 min post-exchange; start today at xx
What Do I Need To Know? • The Paperwork • The Pager • The Platelets • The Patients • The Project
The Project • Each resident gives a 30 minute presentation typically at 10 am at the end of the month • Topics are chosen by the attending to reflect ongoing issues in transfusion medicine • Often useful to service in guiding or exploring new policies
Interesting Case Conference • Each resident gives a 20 minute brief case presentations typically before rounds • Cases should be a balance between those occurring during each attending on service • Please present the relevant facts, your plan/assessment and a few slides of didactics/data
Daily Pages/Curbsides • How to document the onslaught of issues… – If the clinical matter is short and sweet, simply answer the question and document it in your resident call log book, notes, or whatever mechanism you have in place to verify transmission of information – If you have to look something up, speak to a medical technologist, confer with an attending, or a combination of the above, then you have to place a clinical communication in the chart!
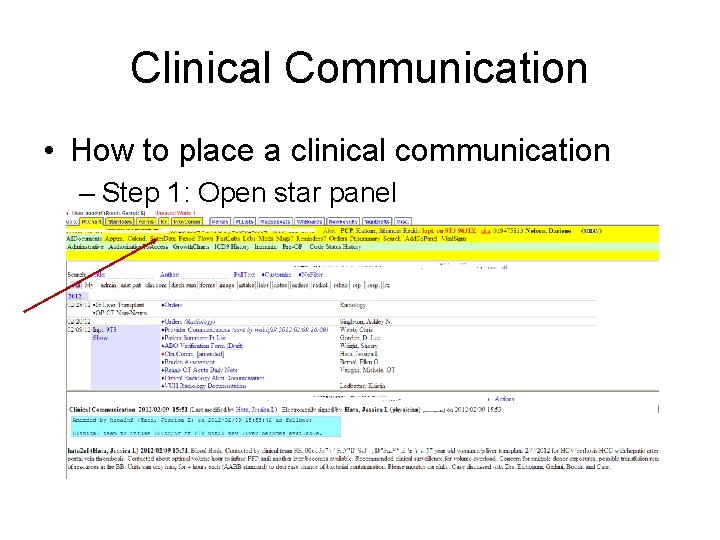
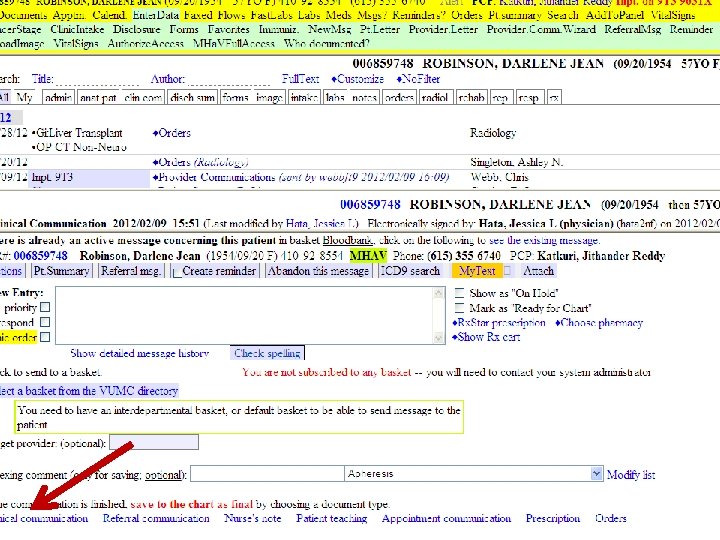
Clinical Communication • How to place a clinical communication – Step 1: Open star panel
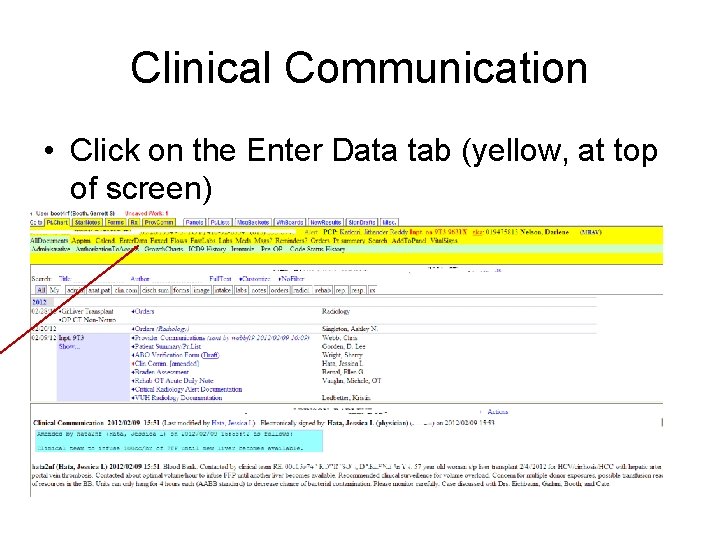
Clinical Communication • Click on the Enter Data tab (yellow, at top of screen)
Clinical Communication • Enter relevant information regarding the issue you were paged on • Click “New. Msg”
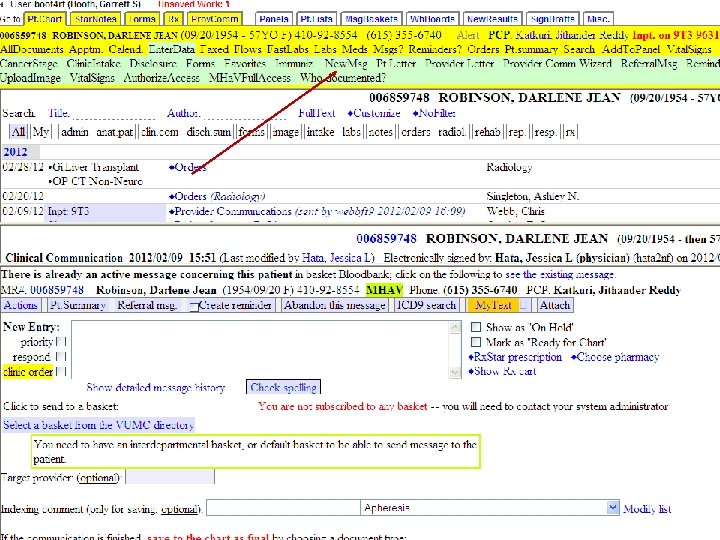
Clinical Communication • Enter the text in the “New Entry” section
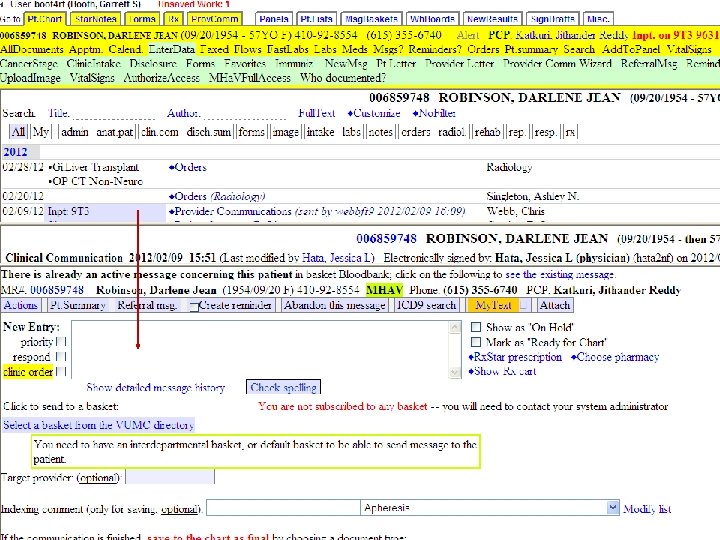
Clinical Communication • Save the information
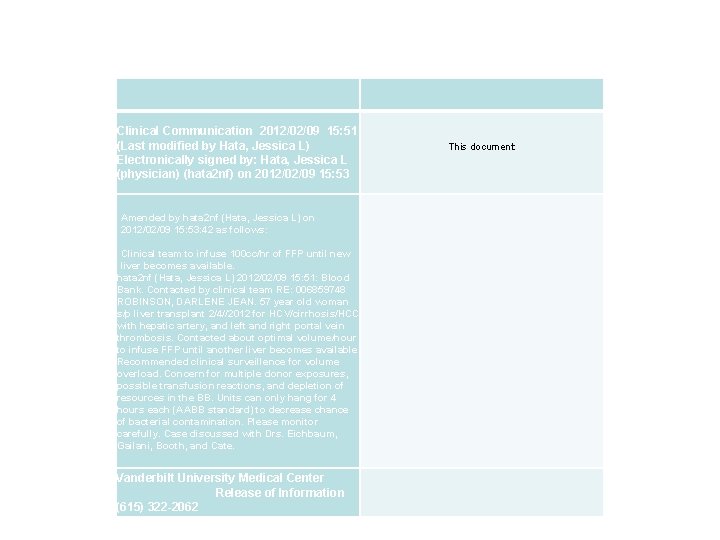
Clinical Communication 2012/02/09 15: 51 (Last modified by Hata, Jessica L) Electronically signed by: Hata, Jessica L (physician) (hata 2 nf) on 2012/02/09 15: 53 Amended by hata 2 nf (Hata, Jessica L) on 2012/02/09 15: 53: 42 as follows: Clinical team to infuse 100 cc/hr of FFP until new liver becomes available. hata 2 nf (Hata, Jessica L) 2012/02/09 15: 51: Blood Bank. Contacted by clinical team RE: 006859748 ROBINSON, DARLENE JEAN. 57 year old woman s/p liver transplant 2/4//2012 for HCV/cirrhosis/HCC with hepatic artery, and left and right portal vein thrombosis. Contacted about optimal volume/hour to infuse FFP until another liver becomes available. Recommended clinical surveillence for volume overload. Concern for multiple donor exposures, possible transfusion reactions, and depletion of resources in the BB. Units can only hang for 4 hours each (AABB standard) to decrease chance of bacterial contamination. Please monitor carefully. Case discussed with Drs. Eichbaum, Gailani, Booth, and Cate. Vanderbilt University Medical Center Release of Information (615) 322 -2062 This document:
Clinical Communication • To add this Clinical Communication into the electronic medical record, you must click on the bottom of the screen – Click Clinical Communication – You can index these communications by inserting “Blood Bank”, “Rh. Ig recommendations”, “Apheresis”, etc…
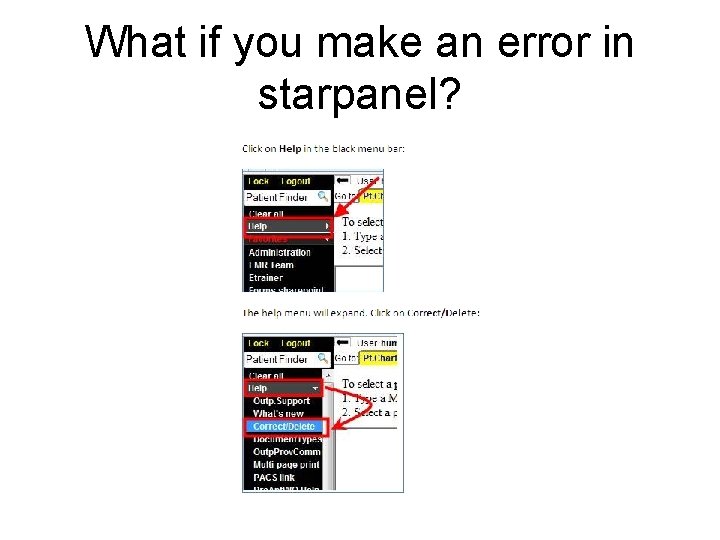
What if you make an error in starpanel?
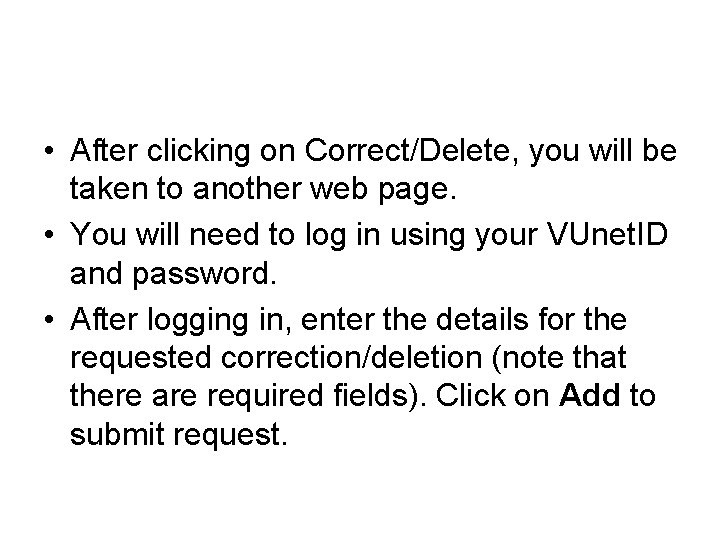
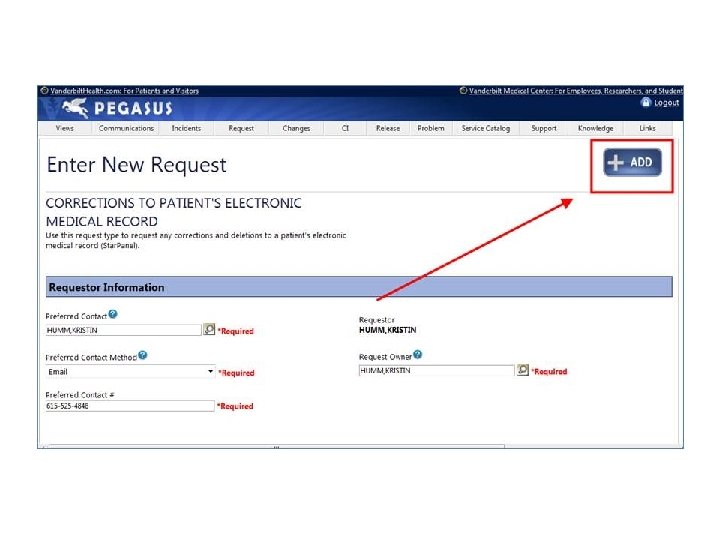
• After clicking on Correct/Delete, you will be taken to another web page. • You will need to log in using your VUnet. ID and password. • After logging in, enter the details for the requested correction/deletion (note that there are required fields). Click on Add to submit request.
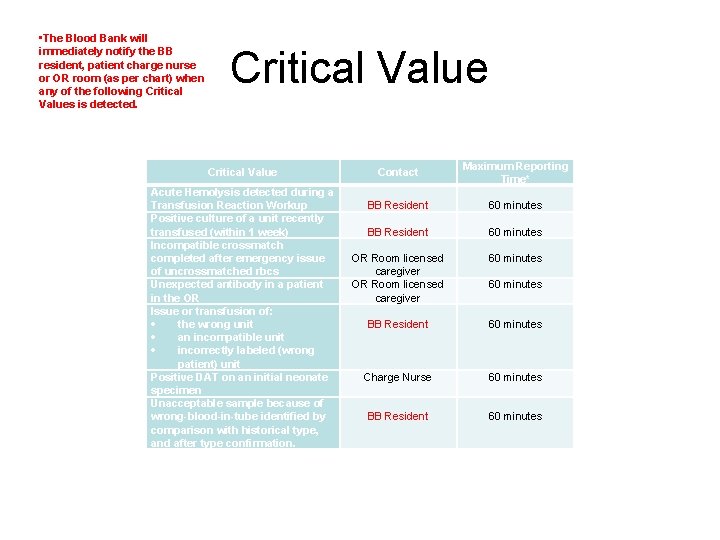
• The Blood Bank will immediately notify the BB resident, patient charge nurse or OR room (as per chart) when any of the following Critical Values is detected. Critical Value Contact Acute Hemolysis detected during a Transfusion Reaction Workup Positive culture of a unit recently transfused (within 1 week) Incompatible crossmatch completed after emergency issue of uncrossmatched rbcs Unexpected antibody in a patient in the OR Issue or transfusion of: the wrong unit an incompatible unit incorrectly labeled (wrong patient) unit Positive DAT on an initial neonate specimen Unacceptable sample because of wrong-blood-in-tube identified by comparison with historical type, and after type confirmation. BB Resident OR Room licensed caregiver BB Resident Maximum Reporting Time* 60 minutes 60 minutes Charge Nurse 60 minutes BB Resident 60 minutes
Resources
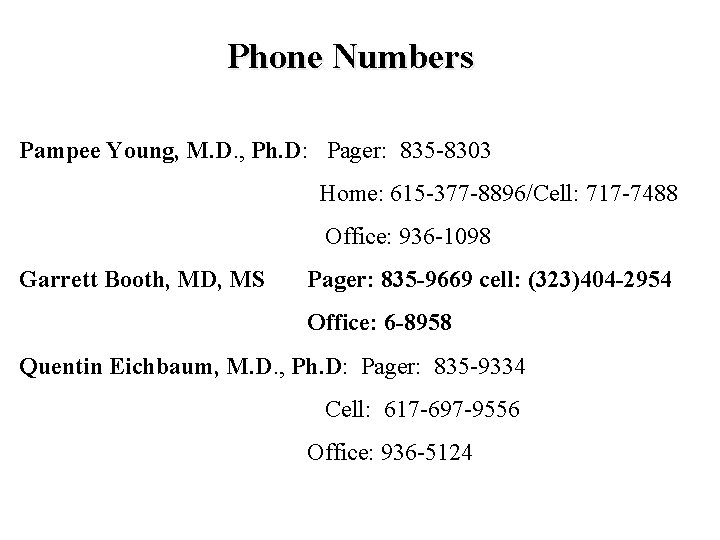
Phone Numbers Pampee Young, M. D. , Ph. D: Pager: 835 -8303 Home: 615 -377 -8896/Cell: 717 -7488 Office: 936 -1098 Garrett Booth, MD, MS Pager: 835 -9669 cell: (323)404 -2954 Office: 6 -8958 Quentin Eichbaum, M. D. , Ph. D: Pager: 835 -9334 Cell: 617 -697 -9556 Office: 936 -5124
- Slides: 68