Introduction This presentation Hospital Response Following a Terrorist







- Slides: 47
Introduction This presentation, “Hospital Response Following a Terrorist Incident Involving Radioactive Material, ” was prepared as a public service by the Medical Response Subcommittee of the Health Physics Society Homeland Security Committee for hospital staff training. The presentation can be copied for use by using the tool bar. On the File menu, click "Save As" a Power. Point file to your computer. The presentation can be edited to fit the needs of the user. The authors request that appropriate attribution be given for this material and would like to know who is presenting it and to what groups. That information and comments may be sent to Marcia Hartman, at mbhartman@ucdavis. edu. Ver 1. 5
Hospital Response Following a Terrorist Incident Involving Radioactive Material Medical Response Subcommittee of the Health Physics Society Homeland Security Committee
Emergency Preparedness • Medical stabilization is the highest priority – Contamination control should not delay critical medical care • Be prepared for multiple hazards, including chemical, radiological and biological hazards • Be prepared for multiple incidents, e. g. , a 1 st incident followed by 2 nd incident used to harm the first responders • Be prepared for – large numbers of potentially contaminated individuals – large numbers of uninjured and uncontaminated but concerned citizens
Emergency Preparedness • Triage Goals for Mass Casualty – Evaluate & sort patients by immediacy of treatment – Do the greatest good for the most people • In mass casualty incidents, may need to deal with thousands of persons in need of decontamination and exposure assessment • Pre-plan to ensure adequate supplies and survey instruments are available • Training and drills are essential to competence and confidence

Radiological Medical Emergency Response Plan • Required by The Joint Commission – EM. 02. 05 Emergency Management - means for radioactive, biological, and chemical isolation and decontamination • Information available: – Radiation Emergency Assistance Center/ Training Site (REAC/TS) – website and training classes http: //orise. orau. gov/reacts/ – NCRP 111, Developing Radiation Emergency Plans for Academic, Medical or Industrial Facilities – NCRP 138, Management of Terrorist Events Involving Radioactive Material – NCRP 165, Responding To A Radiological of Nuclear Terrorism Incident: A Guide for Decision Makers 4
Radiological Medical Emergency Response Plan • Interim Guidelines for Hospital Response to Mass Casualties from a Radiological Incident, http: //emergency. cdc. gov/radiation/ • Health Physics Society Homeland Security website information – Training presentations: "Emergency Department Management of Radiation Casualties " https: //hps. org/hsc/documents/emergency. ppt
Visit http: //emergency. cdc. gov/radiation/
Visit http: //remm. nlm. gov/ Mobile REMM Application also available for I-Phone
Visit http: //hps. org/hsc/responsemed. html
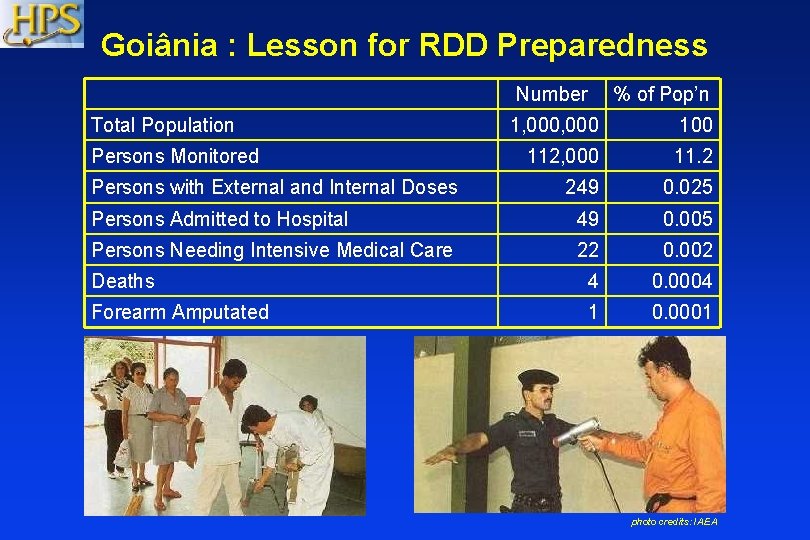
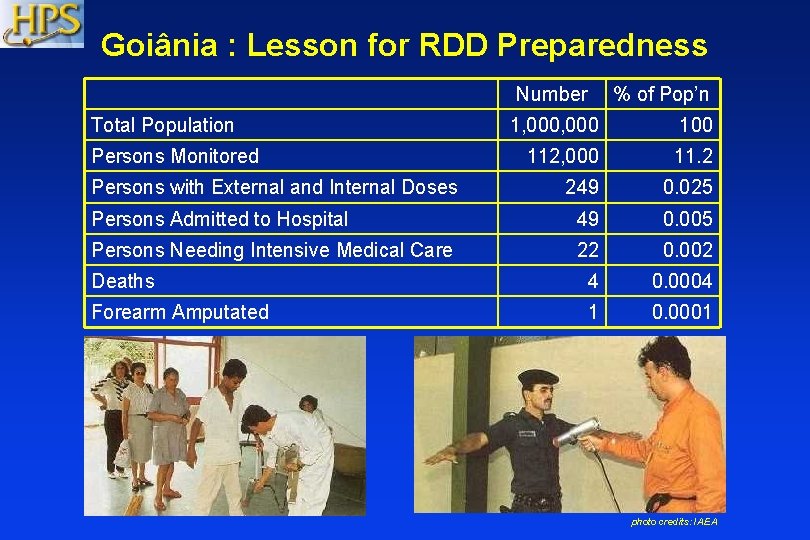
Goiânia : Lesson for RDD Preparedness Number Total Population % of Pop’n 1, 000 100 112, 000 11. 2 249 0. 025 Persons Admitted to Hospital 49 0. 005 Persons Needing Intensive Medical Care 22 0. 002 Deaths 4 0. 0004 Forearm Amputated 1 0. 0001 Persons Monitored Persons with External and Internal Doses photo credits: IAEA
Mass Casualties, Potentially Contaminated but Uninjured Individuals • An incident caused by nuclear terrorism may create large numbers of the public coming to hospitals: – potentially contaminated people who are not injured and – concerned citizens who may not be injured or contaminated. • Measures must be taken to deal effectively with these individuals while preventing them from heading to and overwhelming the emergency department (ED).
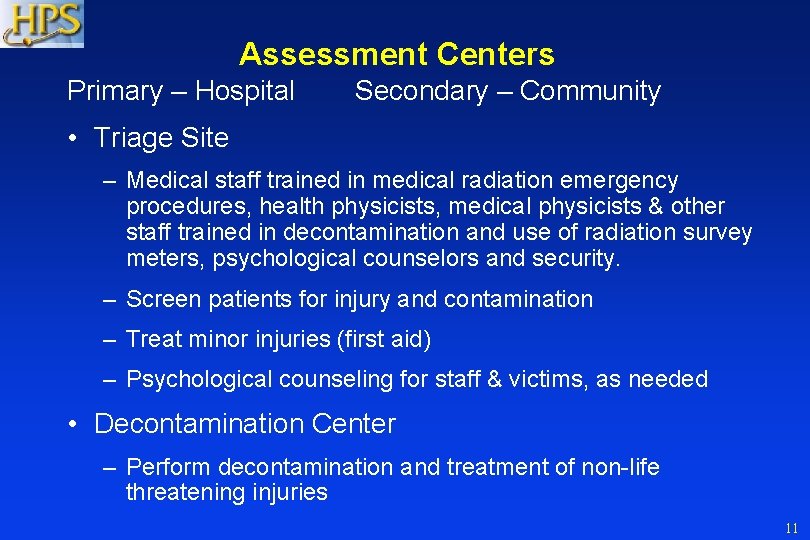
Assessment Centers Primary – Hospital Secondary – Community • Triage Site – Medical staff trained in medical radiation emergency procedures, health physicists, medical physicists & other staff trained in decontamination and use of radiation survey meters, psychological counselors and security. – Screen patients for injury and contamination – Treat minor injuries (first aid) – Psychological counseling for staff & victims, as needed • Decontamination Center – Perform decontamination and treatment of non-life threatening injuries 11
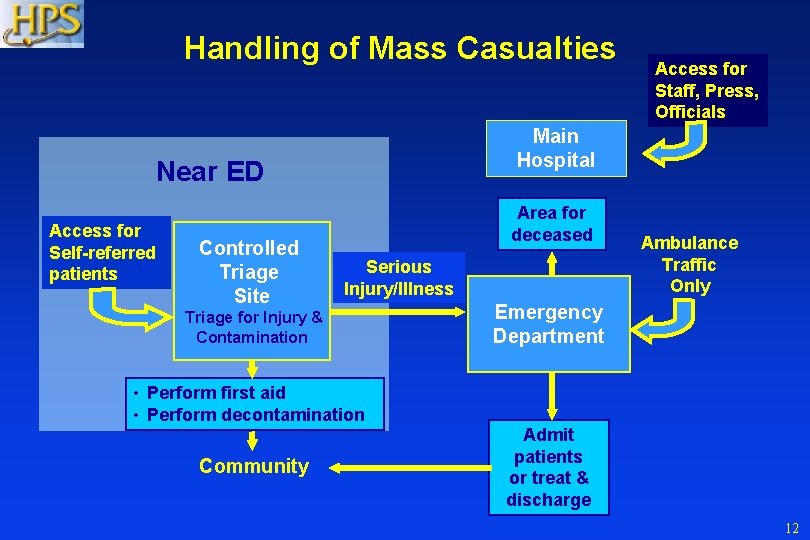
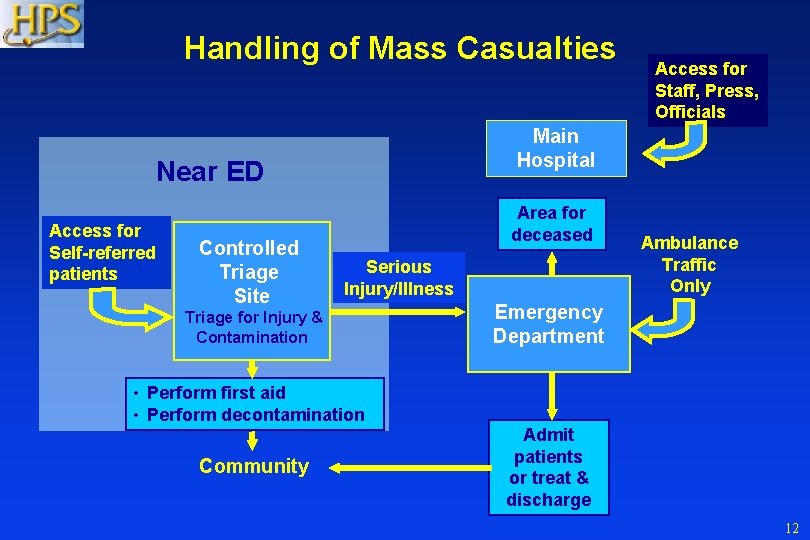
Handling of Mass Casualties Main Hospital Near ED Access for Self-referred patients Controlled Triage Site Access for Staff, Press, Officials Area for deceased Serious Injury/Illness Triage for Injury & Contamination Ambulance Traffic Only Emergency Department • Perform first aid • Perform decontamination Community Admit patients or treat & discharge 12

Triage Site Information • Develop prepared information packets with Media Relations in advance with message for incidents involving radiation. • CDC website has Emergency Instructions for Individuals and Families titled, “FAQ About a Radiation Emergency” Available in English Español Deutsch Français Tagalog Chinese photo credits: CDC 13

Mass Casualties, Potentially Contaminated but Uninjured Individuals
Systematic Approach • A systematic approach to handling large numbers of potentially contaminated individuals is necessary. • Such an approach should provide for surveying, mass decontamination, resurveying, advanced decontamination (if necessary), resurveying and additional decontamination or ED care as indicated. • Depending on weather, decontamination sites may have to be established indoors or in a temporary shelter. 15
Controlled Triage Site • A controlled triage site should be established away from the ED to intercept the large numbers of contaminated people who are not injured and uncontaminated but worried people and divert them to appropriate locations. • These locations may be Hospital Reception & Decontamination Centers (HRDC) or local reception centers. 16
Triage Site Control • Control of movement through the site is necessary to minimize the potential for contaminating clean areas of the site. • Radiation portal monitors should be used to facilitate rapid screening of large numbers of victims. • The triage site should be staffed with medical staff, radiation monitors, social workers and security personnel. • Precautions should be taken so that people cannot avoid the triage center and go directly to the ED. 17

Movement Through the Triage/Decontamination Areas • The path through the triage/decontamination area must be clearly marked and individuals assigned to keep traffic moving in the right direction and to prevent potentially contaminated individuals from walking into clean areas, except by the designated route. photo credits: M. Meehan 18
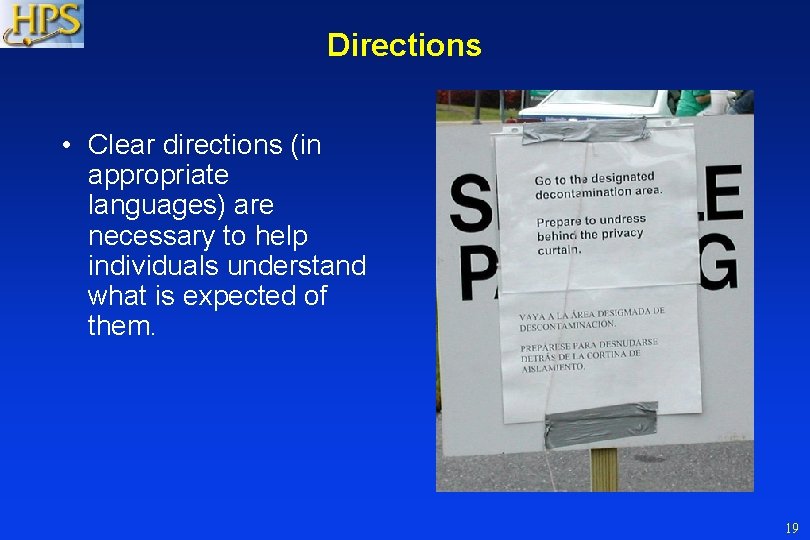
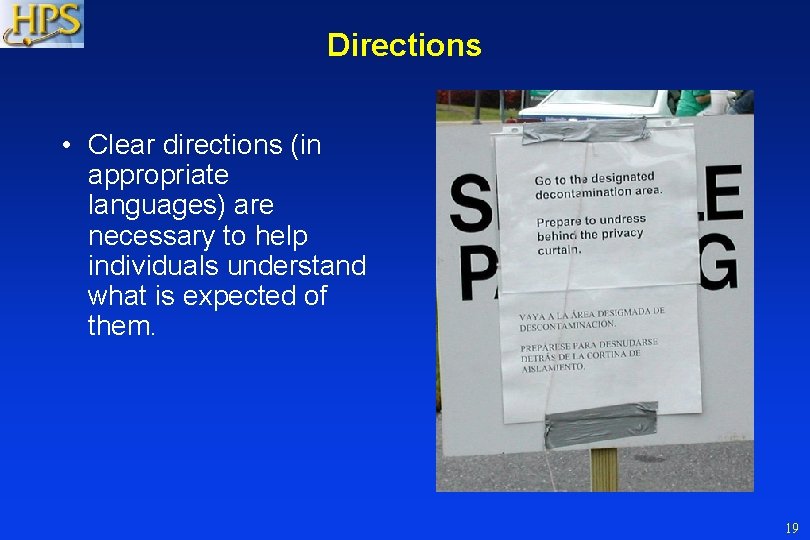
Directions • Clear directions (in appropriate languages) are necessary to help individuals understand what is expected of them. 19
Decontamination Center • Establish a Decontamination Center where staff can survey people to identify who are contaminated, but not significantly injured. – Center should provide showers for many people. – Replacement clothing must be available. – Provisions to transport or shelter people after decontamination may be necessary. 20
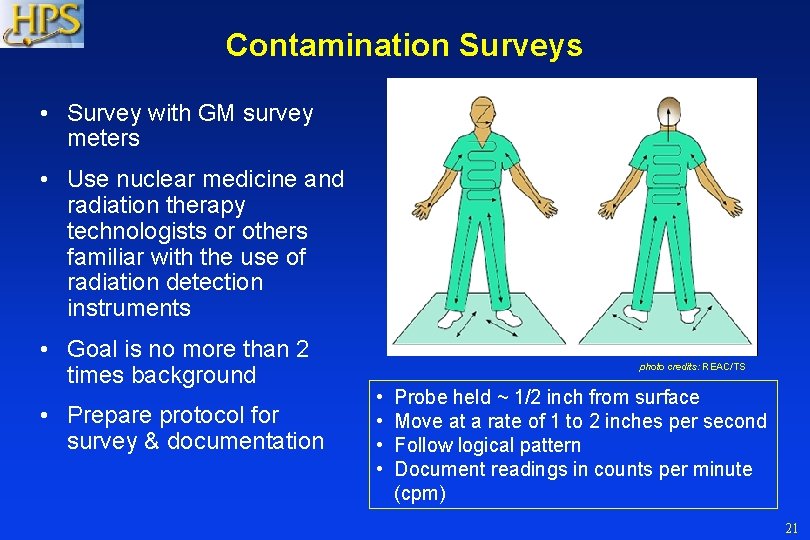
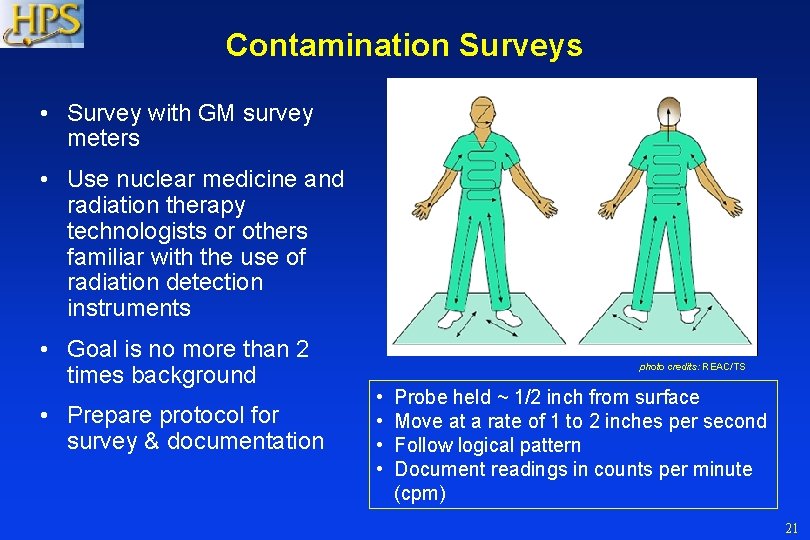
Contamination Surveys • Survey with GM survey meters • Use nuclear medicine and radiation therapy technologists or others familiar with the use of radiation detection instruments • Goal is no more than 2 times background • Prepare protocol for survey & documentation photo credits: REAC/TS • • Probe held ~ 1/2 inch from surface Move at a rate of 1 to 2 inches per second Follow logical pattern Document readings in counts per minute (cpm) 21
Radiation Levels to Initiate Decontamination • Decontamination (skin and clothing) should always be performed when the contamination level is: • >0. 1 m. R/hr exposure rate (~1 μGy/hr air-kerma rate) at 10 cm • >600, 000 dpm/cm 2 (10, 000 Bq/cm 2) beta and gamma surface contamination • >60, 000 dpm/cm 2 (1, 000 Bq/cm 2) for alpha surface contamination. • Facial contamination should initiate potential medical treatment for internal contamination. 22 22
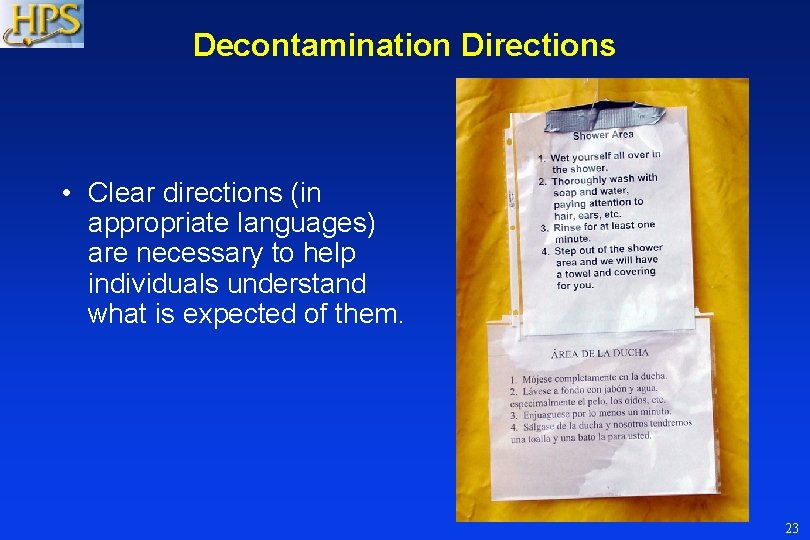
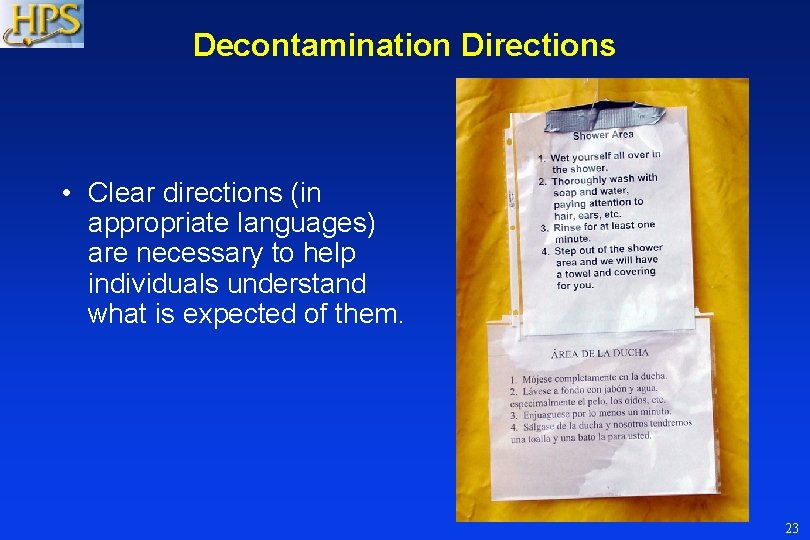
Decontamination Directions • Clear directions (in appropriate languages) are necessary to help individuals understand what is expected of them. 23
Surveying After Each Decontamination Procedure • Provisions must be provided for repeat surveying of individuals after each decontamination procedure to determine success of efforts and when individuals can be routed out of the decontamination center. photo credits: REAC/TS 24
Mass Decontamination Facilities • Where possible, the decontamination of many contaminated individuals should be carried out in existing shower facilities (e. g. , at a fire house, school locker room, or public campground) • When such facilities are not immediately available, field decontamination capabilities may have to be implemented. 25

Mass Decontamination
• Runoff Mass Decontamination – Responders should closely monitor the direction of runoff to prevent cross contamination between lanes and between zones. If possible, the decontamination area should contain a storm water drain or be on a slope that allows control of water runoff. • EPA and Runoff – The EPA has stated that they will not hold responders liable for run-off in a chemical or biological incident caused by a terrorist event. (EPA letter dated 9/17/00) – Your Emergency Management Plan must have a contingency to contain runoff; the EPA only allows an exception if you exceed your planned holding capacity. – Protection of human life and health is primary goal.
Second Stage Decontamination Ambulatory Patients • When surveying shows that preliminary decontamination of individuals has not been complete, they should be sent to a second stage decontamination facility (e. g. , specialized decontamination tent). 28
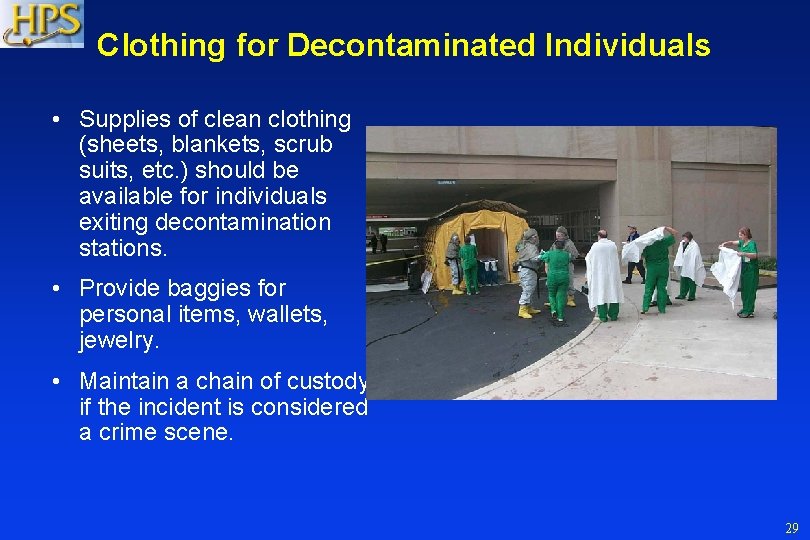
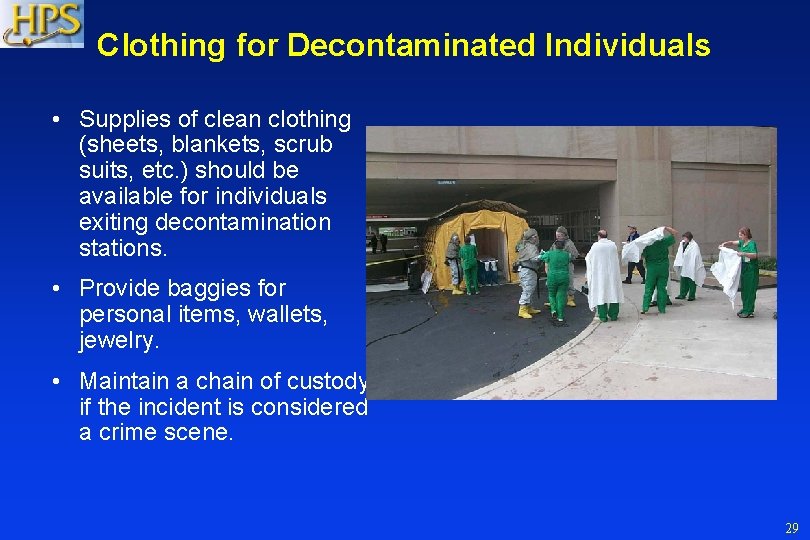
Clothing for Decontaminated Individuals • Supplies of clean clothing (sheets, blankets, scrub suits, etc. ) should be available for individuals exiting decontamination stations. • Provide baggies for personal items, wallets, jewelry. • Maintain a chain of custody if the incident is considered a crime scene. 29
Second Stage Decontamination Non-Ambulatory Patients • Some specialized decontamination tents permit capabilities for decontamination of non-ambulatory patients as well as those who can walk. 30
Gowning Capabilities • Patients exiting second stage decontamination facilities need to be provided with clean clothes (hospital gowns, coveralls, sheets or blankets). 31
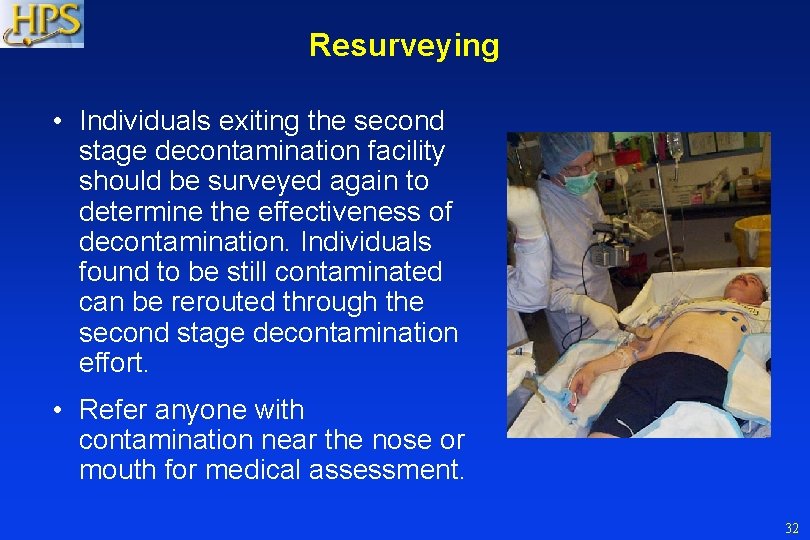
Resurveying • Individuals exiting the second stage decontamination facility should be surveyed again to determine the effectiveness of decontamination. Individuals found to be still contaminated can be rerouted through the second stage decontamination effort. • Refer anyone with contamination near the nose or mouth for medical assessment. 32
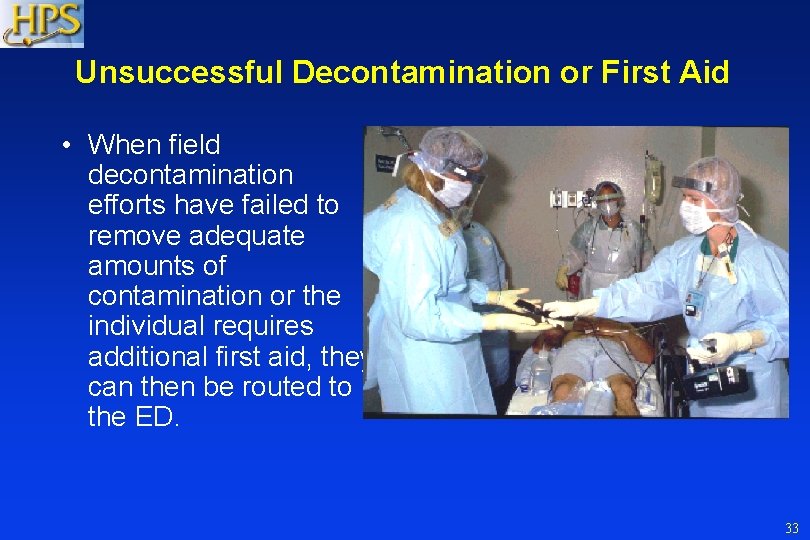
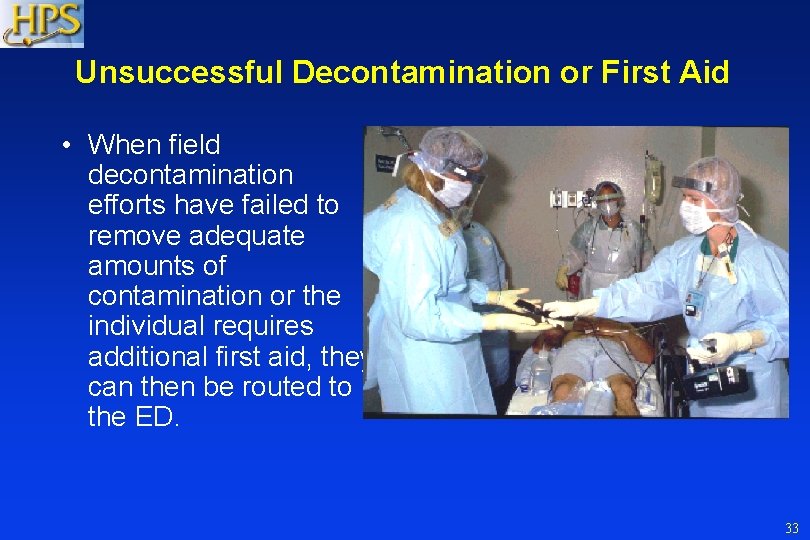
Unsuccessful Decontamination or First Aid • When field decontamination efforts have failed to remove adequate amounts of contamination or the individual requires additional first aid, they can then be routed to the ED. 33
Hospital Preparation • Activate hospital plan – Alert key personnel – Obtain radiation emergency supplies – Obtain radiation survey meters – Call for additional support • Radiation Safety/ Health Physics • Medical Physicists • Radiation Oncology • Nuclear Medicine • Researchers 34
Hospital Preparation • Treating life threatening injuries is the 1 st priority – Contamination control should not delay critical medical care • Plan for contamination control – Ensure staff are properly gowned and remind them to use standard precautions – Establish multiple receptacles for contaminated waste – Protect floor with covering if time allows – For transport of contaminated patients into ED, designate separate entrance, designate one side of corridor, or transfer to clean gurney before entering, if time allows
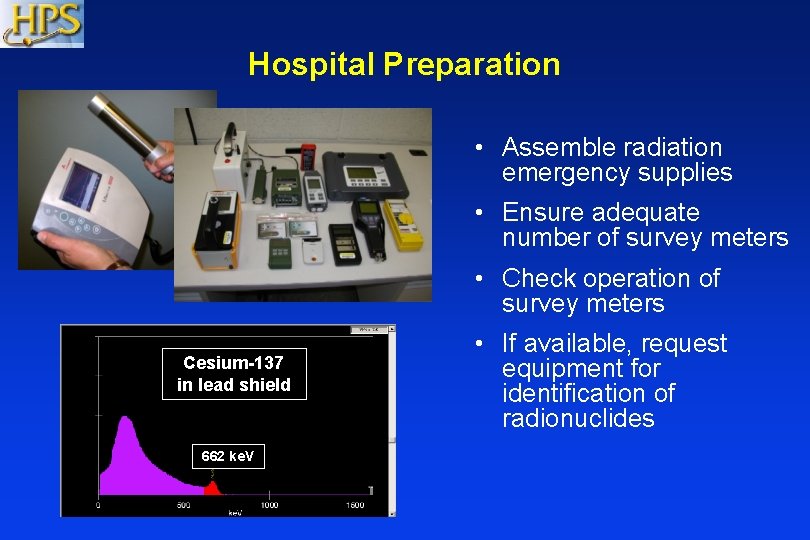
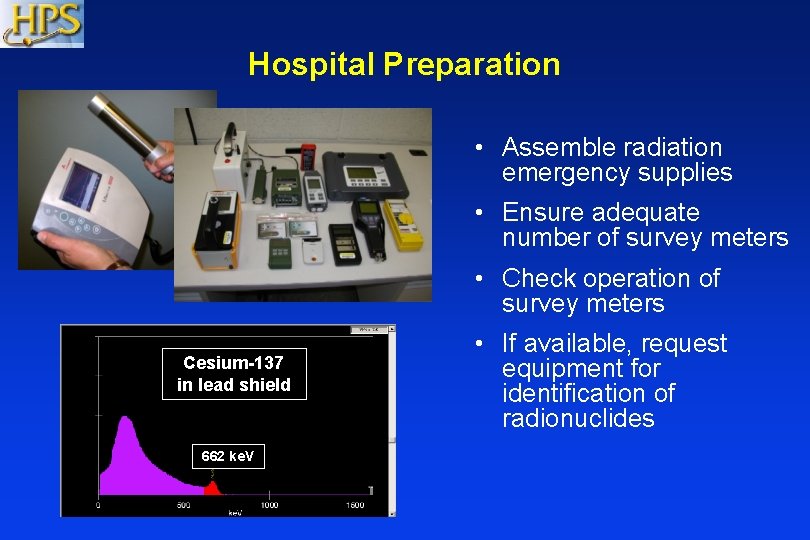
Hospital Preparation • Assemble radiation emergency supplies • Ensure adequate number of survey meters • Check operation of survey meters Cesium-137 in lead shield 662 ke. V • If available, request equipment for identification of radionuclides
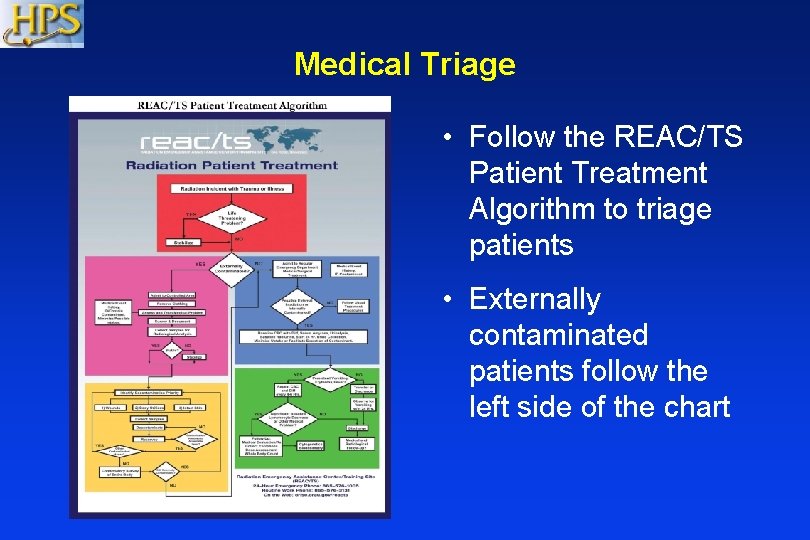
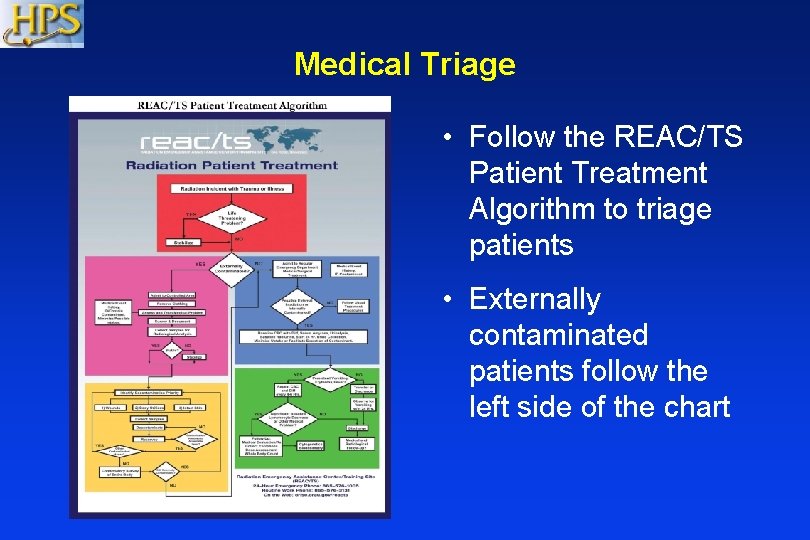
Medical Triage • Follow the REAC/TS Patient Treatment Algorithm to triage patients • Externally contaminated patients follow the left side of the chart
Other Considerations • Victims may include the terrorist(s) • In most cases, standard precautions is all that is necessary to protect the staff – Risk to caregivers, who would likely receive low doses, is very small – Hospital staff doses at Chernobyl < 1 rem – 25 rem increases the risk of fatal cancer by ~ 1% – 25 rem increases the risk of severe hereditary effects by ~ 0. 1% • Pre-plan who will be given radiation dosimeters – ED staff, surgery staff 38

Other Considerations • Larger hospitals or large metropolitan areas should consider stocking decorporation agents • Dose rates to first responders 20 cm from patient with uniform surface contamination: – Cs-137, 100 µCi/cm 2 – 1 rem/hr – Co-60, 100 µCi/cm 2 – 3. 9 rem/hr • Dose rates to surgeon standing 20 cm from patient with radioactive fragment (0. 2 mm long, 0. 2 mm radius, embedded 20 cm deep) – Co-60, 1 Ci - 2. 5 rem/hr 39
Support for Concerned Citizens • Fear of radiation and misunderstanding of consequences • Long term psychological effects could arise hours or days after an incident • Counsel on acute and potential long term physical and psychological effects • Psychological effects include: Anxiety disorders Post traumatic stress disorder Depression Insomnia Traumatic neurosis Acute stress disorder
Support for Concerned Citizens & Workers • Provide psychological counseling to staff, victims and their families • High-Risk groups: emergency workers, children, mothers w/ small children, cleanup workers • Provide exposed patients with a “sense of control of their health” • Resources: The National Center for Post Traumatic Stress Disorder http: //www. ptsd. va. gov/
Contaminated Corpses • Disaster Mortuary Operational Response Teams (DMORT) • Restrict autopsies of highly radioactive corpses • No embalming or cremation • Health Physics assistance for autopsies – Use contamination control – Wear protective clothing
Key Points • Medical stabilization is the highest priority – Lifesaving activities take priority over radiological concerns • Pre-plan to ensure adequate supplies and survey instruments are available • Train/drill to ensure competence and confidence • Make sure that you have prepared your personal family plan - http: //www. ready. gov/ • Do what works for your facility and available resources • The first 24 hours are the worst, then many other experts will be available to help
Additional Resources Agencies that are available 24/7 to assist with medical management: – Radiation Emergency Assistance Center/ Training Site (REAC/TS), (865) 576 -1005, http: //orise. orau. gov/reacts/ – Medical Radiobiology Advisory Team (MRAT) Armed Forces Radiobiology Research Institute (AFRRI) (301) 295 -0530, http: //www. afrri. usuhs. mil/ Websites: – Response to Radiation Emergencies by the Center for Disease Control, http: //emergency. cdc. gov/radiation/ – Medical Response information on the Health Physics Society website, http: //hps. org/hsc/responsemed. html – Disaster Preparedness for Radiology Professionals by American College of Radiology, http: //www. acr. org/, search “disaster”
Acknowledgements The Medical Response Subcommittee members when issued: Jerrold T. Bushberg, Ph. D, DABMP, Chair, UC Davis Medical Center Marcia Hartman, MS, UC Davis Medical Center Linda Kroger, MS, UC Davis Medical Center John J. Lanza, MD, Ph. D, MPH, FAAP, Florida County Health Department Edwin M. Leidholdt, Jr. , Ph. D, ABR, Western Region Veterans Affairs Mark A. Melanson, Ph. D, CHP, Walter Reed Army Medical Center Kenneth L. Miller, MS, CHP, CMHP, Hershey Medical Center

Health Physics Society* Version 1. 5 Disclaimer: The information contained herein was current as of August 8, 2011, and is intended for educational purposes only. The authors and the Health Physics Society (HPS) do not assume any responsibility for the accuracy of the information presented herein. The authors and the HPS are not liable for any legal claims or damages that arise from acts or omissions that occur based on its use. *The Health Physics Society is a non profit scientific professional organization whose mission is to promote the practice of radiation safety. Since its formation in 1956, the Society has grown to nearly 5, 000 scientists, physicians, engineers, lawyers, and other professionals representing academia, industry, government, national laboratories, the department of defense, and other organizations. Society activities include encouraging research in radiation science, developing standards, and disseminating radiation safety information. Society members are involved in understanding, evaluating, and controlling the potential risks from radiation relative to the benefits. Official position statements are prepared and adopted in accordance with standard policies and procedures of the Society. The Society may be contacted at: 1313 Dolley Madison Blvd. , Suite 402, Mc. Lean, VA 22101; phone: 703 -790 -1745; FAX: 703 -790 -2672; email: HPS@Burk. Inc. com.