INTRODUCTION Hemodynamic monitoring is an invasive technology which

- Slides: 19
INTRODUCTION “Hemodynamic monitoring is an invasive technology which provides quantitative information about vascular capacity, blood volume, pump effectiveness and tissue perfusion”. It is based on the invasive measurement of systemic, pulmonary arterial and venous pressures, and of cardiac output. It allows us to accurately measure the blood pressure inside the veins, heart, and arteries.
PURPOSE • The main aim of hemodynamic monitoring in cardiac surgery is to maintain the balance between tissue oxygen demand supply. • It helps the healthcare professionals to identify abnormal physiology and intervene before complications, including organ failure and mortality.
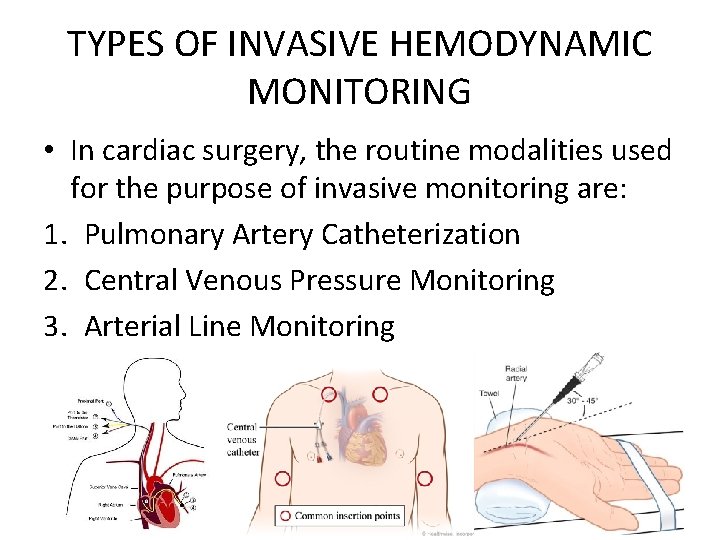
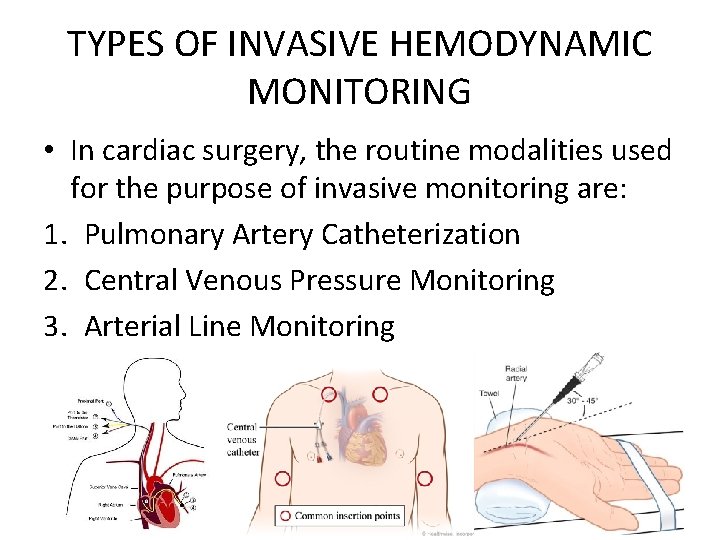
TYPES OF INVASIVE HEMODYNAMIC MONITORING • In cardiac surgery, the routine modalities used for the purpose of invasive monitoring are: 1. Pulmonary Artery Catheterization 2. Central Venous Pressure Monitoring 3. Arterial Line Monitoring
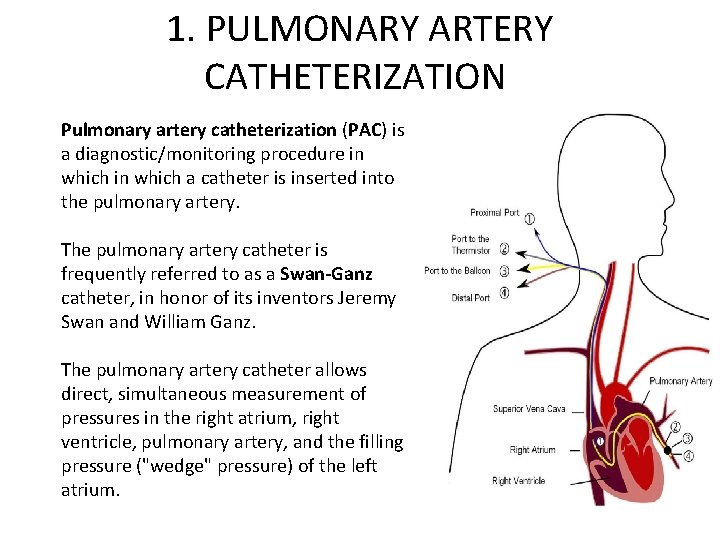
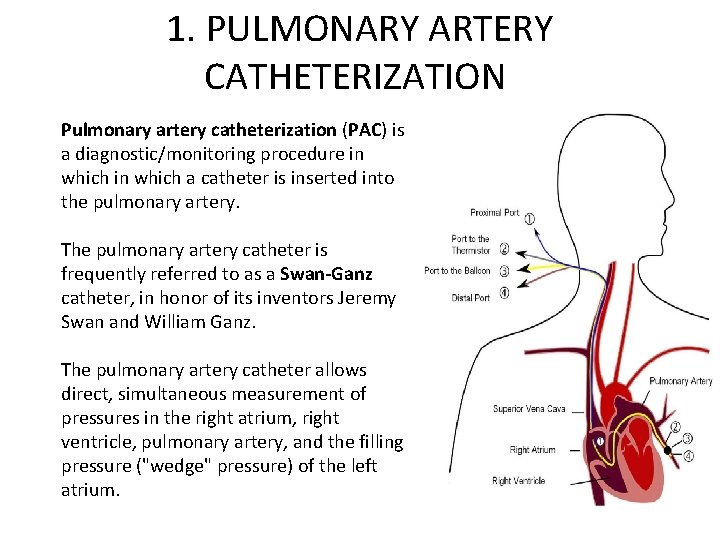
1. PULMONARY ARTERY CATHETERIZATION Pulmonary artery catheterization (PAC) is a diagnostic/monitoring procedure in which a catheter is inserted into the pulmonary artery. The pulmonary artery catheter is frequently referred to as a Swan-Ganz catheter, in honor of its inventors Jeremy Swan and William Ganz. The pulmonary artery catheter allows direct, simultaneous measurement of pressures in the right atrium, right ventricle, pulmonary artery, and the filling pressure ("wedge" pressure) of the left atrium.
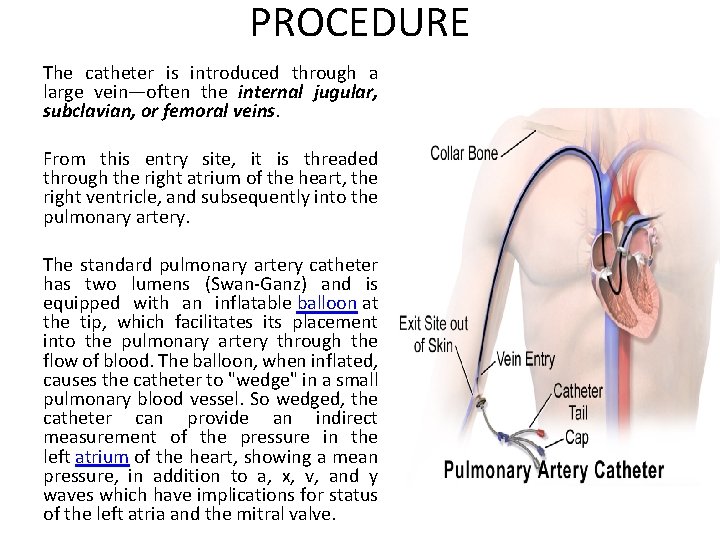
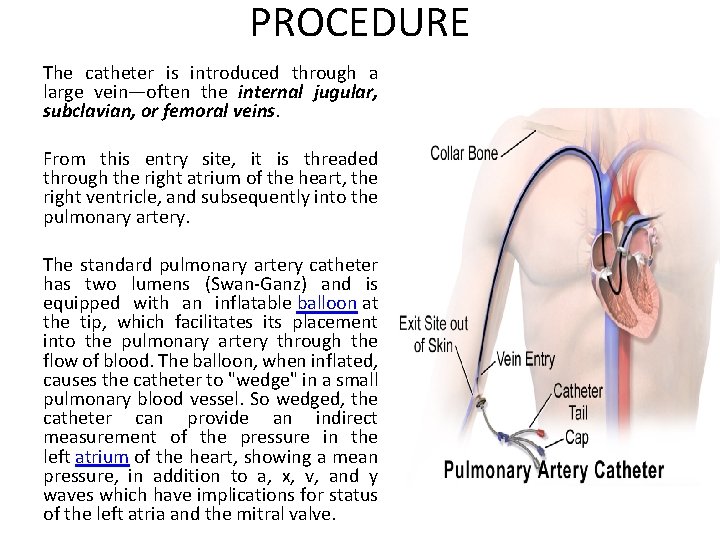
PROCEDURE The catheter is introduced through a large vein—often the internal jugular, subclavian, or femoral veins. From this entry site, it is threaded through the right atrium of the heart, the right ventricle, and subsequently into the pulmonary artery. The standard pulmonary artery catheter has two lumens (Swan-Ganz) and is equipped with an inflatable balloon at the tip, which facilitates its placement into the pulmonary artery through the flow of blood. The balloon, when inflated, causes the catheter to "wedge" in a small pulmonary blood vessel. So wedged, the catheter can provide an indirect measurement of the pressure in the left atrium of the heart, showing a mean pressure, in addition to a, x, v, and y waves which have implications for status of the left atria and the mitral valve.
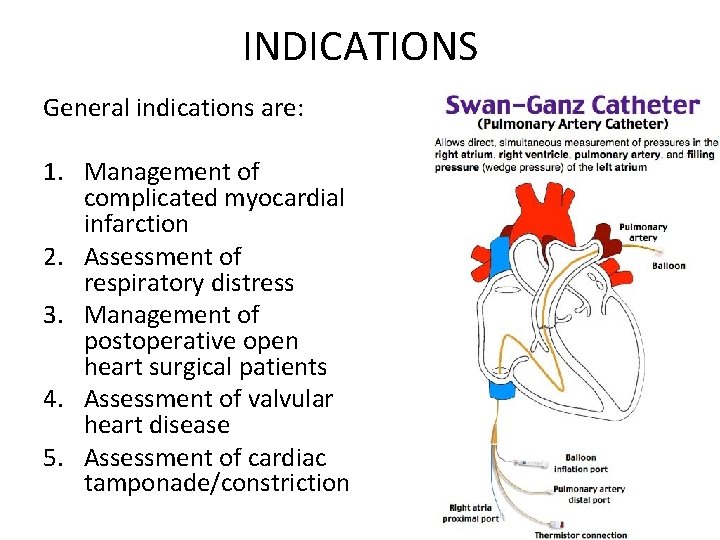
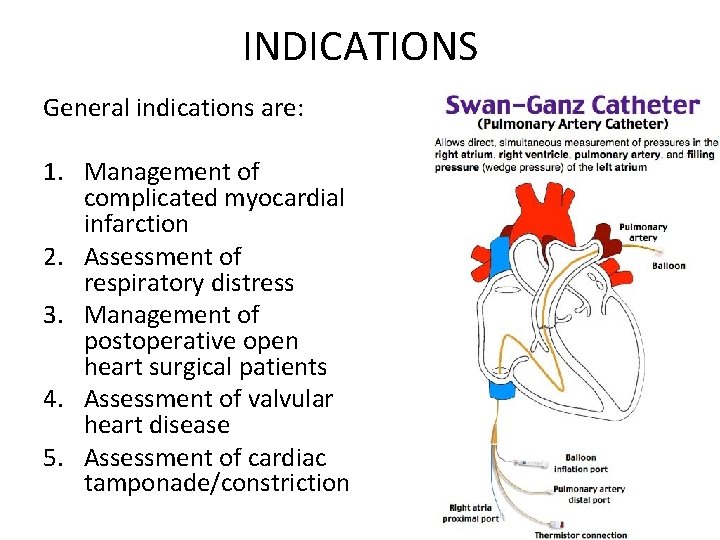
INDICATIONS General indications are: 1. Management of complicated myocardial infarction 2. Assessment of respiratory distress 3. Management of postoperative open heart surgical patients 4. Assessment of valvular heart disease 5. Assessment of cardiac tamponade/constriction
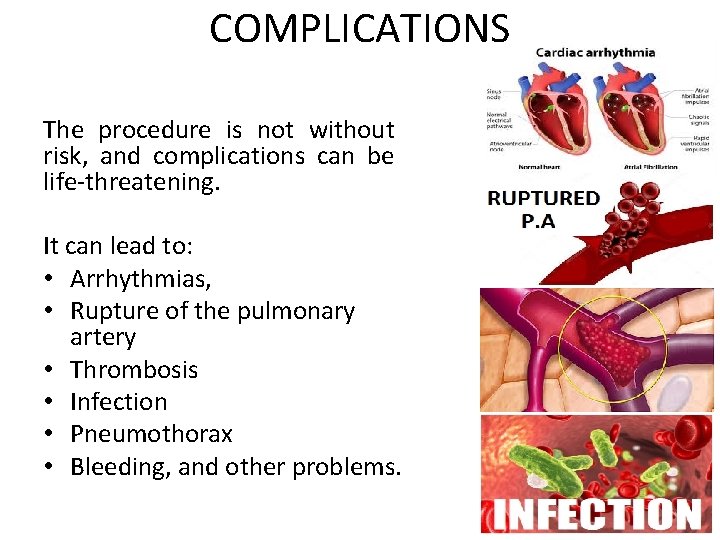
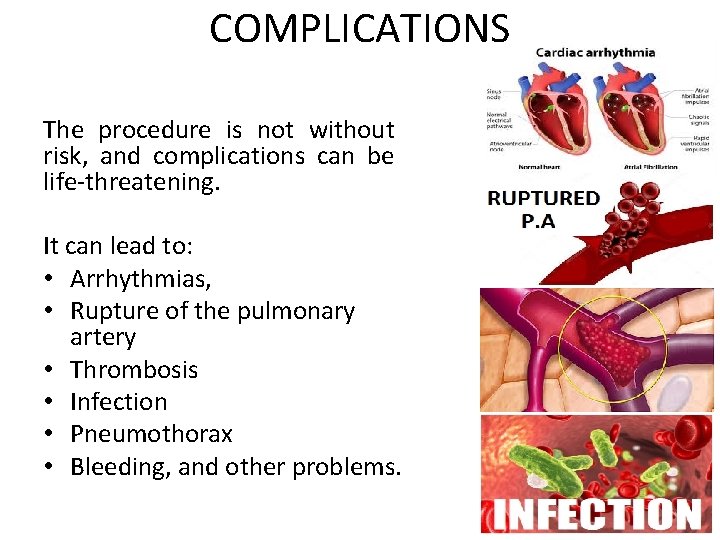
COMPLICATIONS The procedure is not without risk, and complications can be life-threatening. It can lead to: • Arrhythmias, • Rupture of the pulmonary artery • Thrombosis • Infection • Pneumothorax • Bleeding, and other problems.
RESEARCH DATA No study has definitively demonstrated improved outcome in critically ill patients managed with PA catheters. [1][2] Given that the PA catheter is a monitoring tool and not a therapy in and of itself this is not entirely surprising. Several studies in the 1980 s seemed to show a benefit of the increase in physiological information. However, there is growing evidence that the use of a PA catheter (PAC) does not necessarily lead to improved outcome. [3] Many reports showing benefit of the PA catheter are from anaesthetic, and Intensive Care settings.
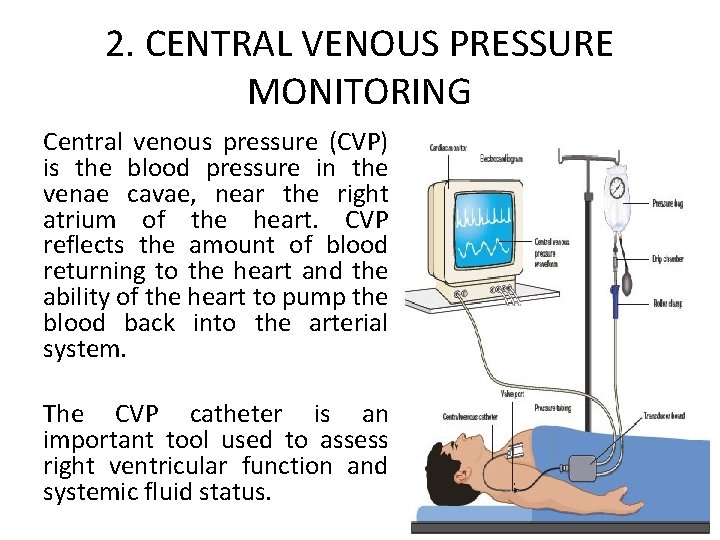
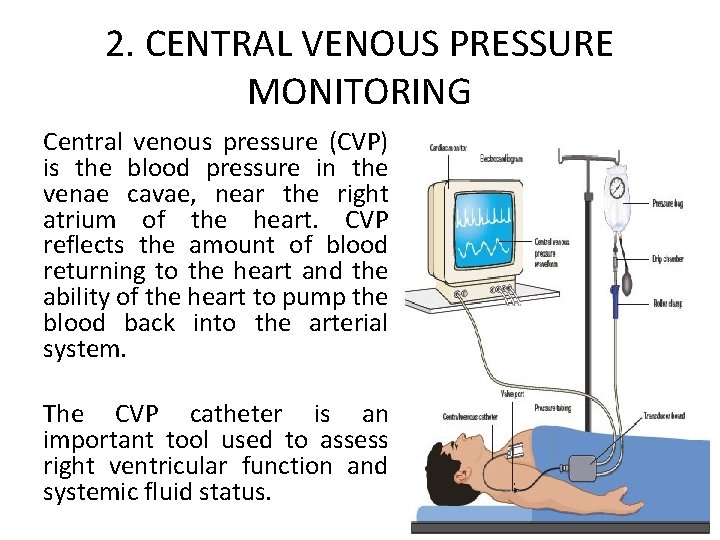
2. CENTRAL VENOUS PRESSURE MONITORING Central venous pressure (CVP) is the blood pressure in the venae cavae, near the right atrium of the heart. CVP reflects the amount of blood returning to the heart and the ability of the heart to pump the blood back into the arterial system. The CVP catheter is an important tool used to assess right ventricular function and systemic fluid status.
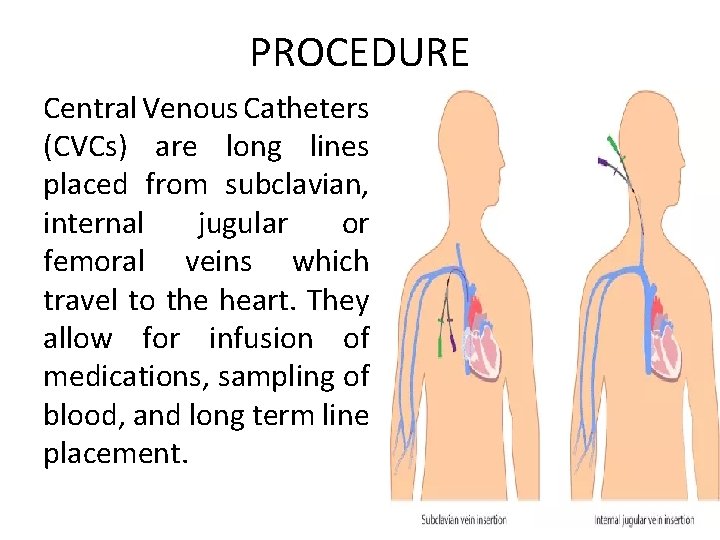
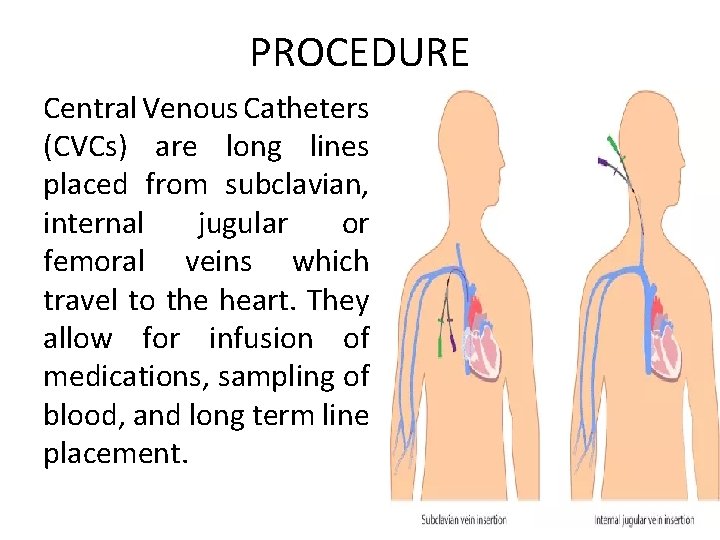
PROCEDURE Central Venous Catheters (CVCs) are long lines placed from subclavian, internal jugular or femoral veins which travel to the heart. They allow for infusion of medications, sampling of blood, and long term line placement.
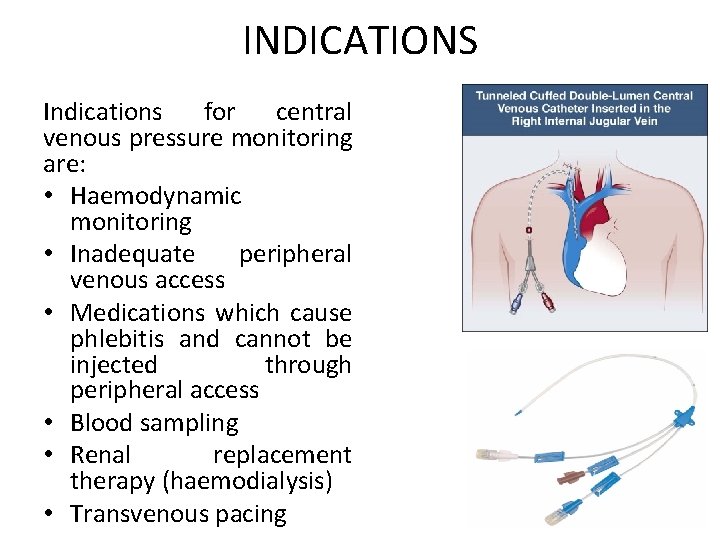
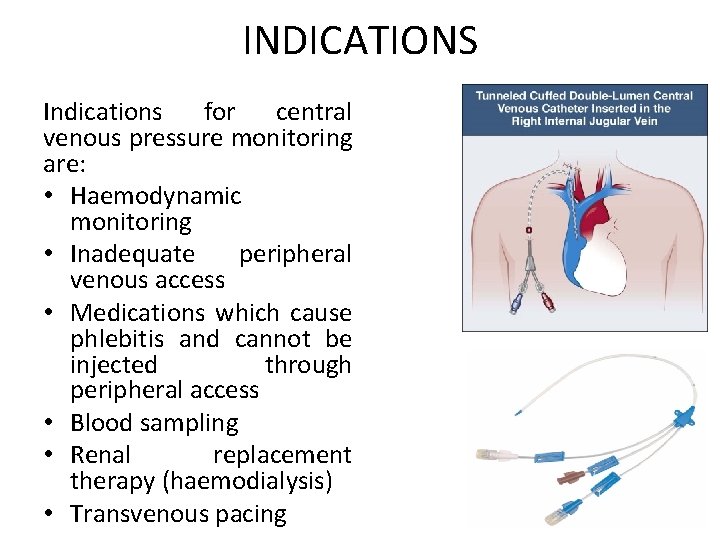
INDICATIONS Indications for central venous pressure monitoring are: • Haemodynamic monitoring • Inadequate peripheral venous access • Medications which cause phlebitis and cannot be injected through peripheral access • Blood sampling • Renal replacement therapy (haemodialysis) • Transvenous pacing
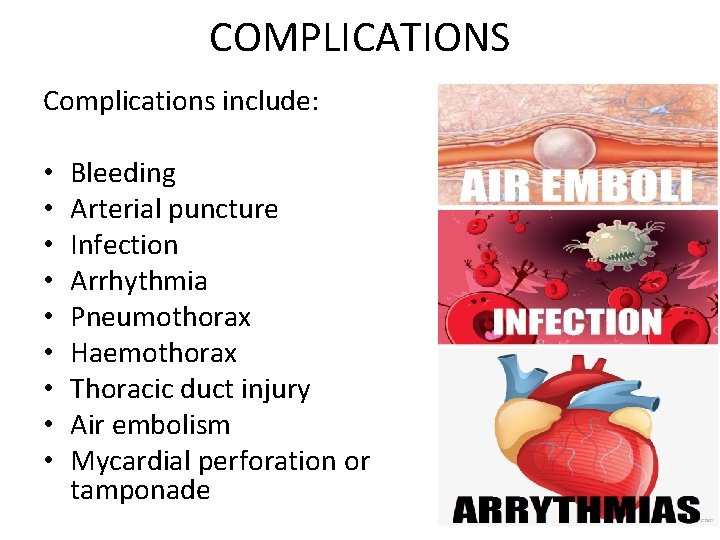
COMPLICATIONS Complications include: • • • Bleeding Arterial puncture Infection Arrhythmia Pneumothorax Haemothorax Thoracic duct injury Air embolism Mycardial perforation or tamponade
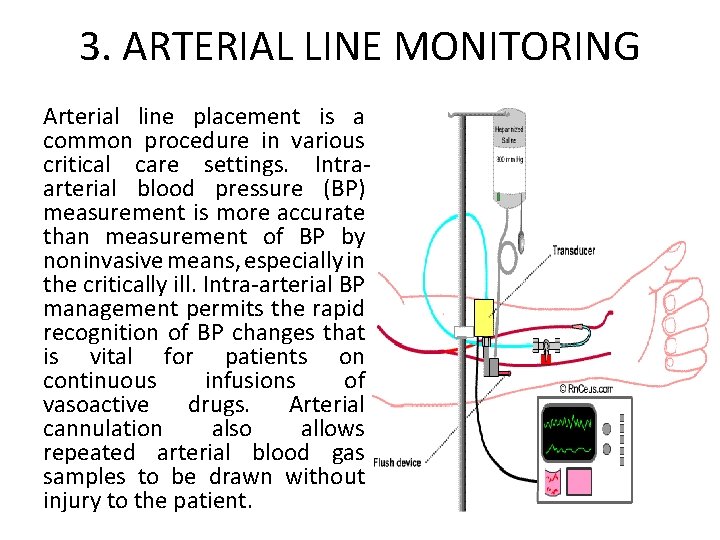
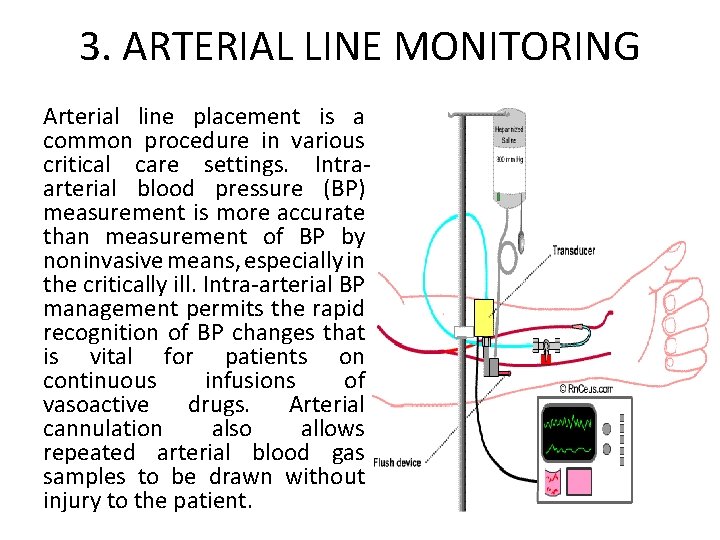
3. ARTERIAL LINE MONITORING Arterial line placement is a common procedure in various critical care settings. Intraarterial blood pressure (BP) measurement is more accurate than measurement of BP by noninvasive means, especially in the critically ill. Intra-arterial BP management permits the rapid recognition of BP changes that is vital for patients on continuous infusions of vasoactive drugs. Arterial cannulation also allows repeated arterial blood gas samples to be drawn without injury to the patient.
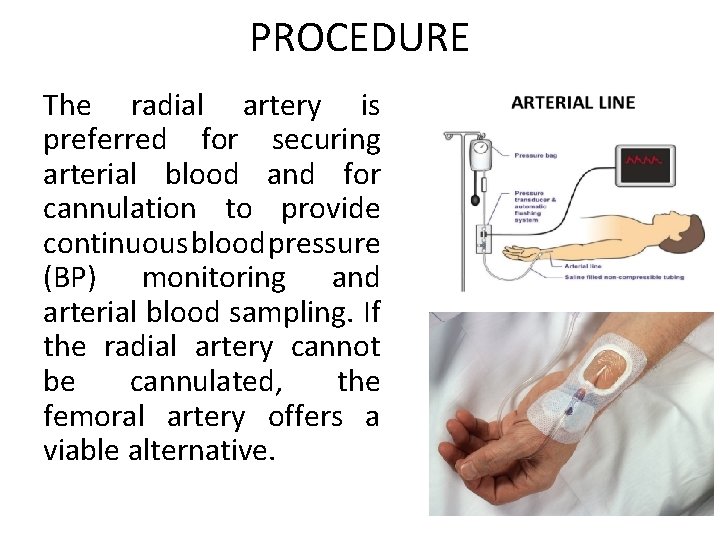
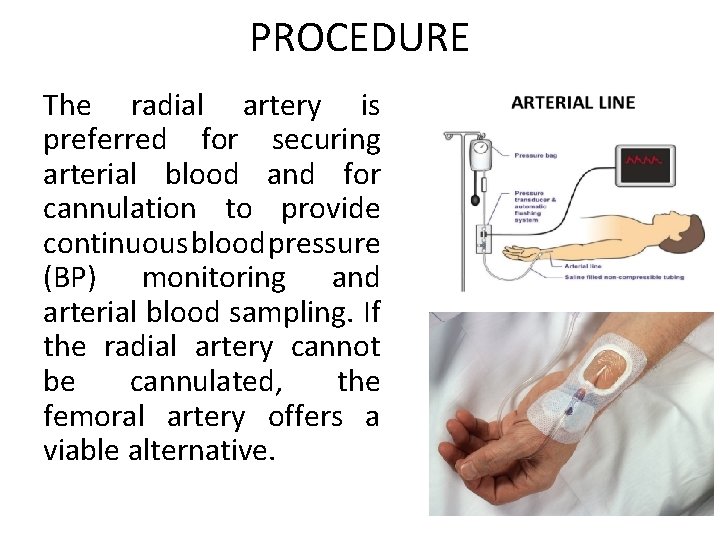
PROCEDURE The radial artery is preferred for securing arterial blood and for cannulation to provide continuous blood pressure (BP) monitoring and arterial blood sampling. If the radial artery cannot be cannulated, the femoral artery offers a viable alternative.
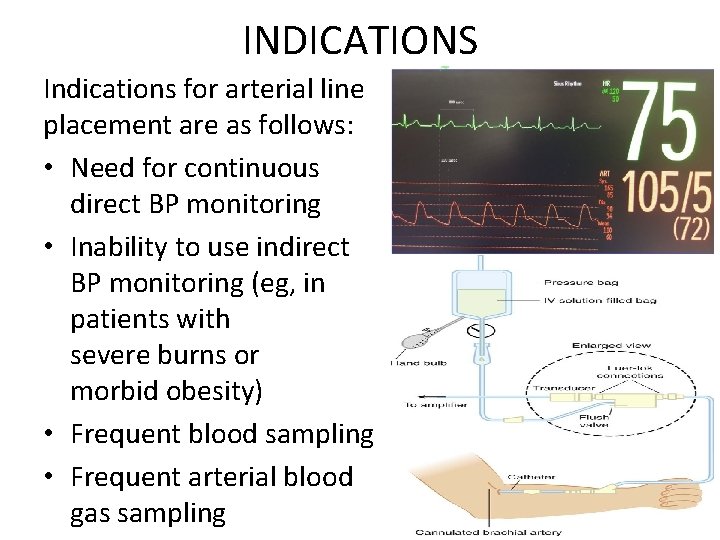
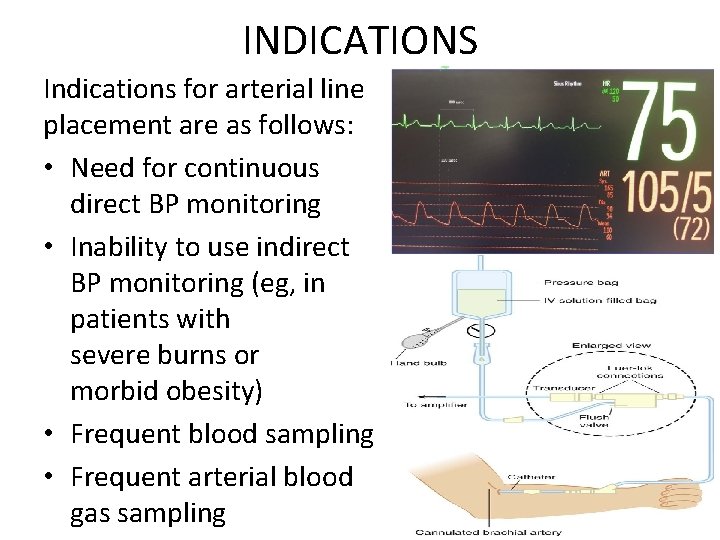
INDICATIONS Indications for arterial line placement are as follows: • Need for continuous direct BP monitoring • Inability to use indirect BP monitoring (eg, in patients with severe burns or morbid obesity) • Frequent blood sampling • Frequent arterial blood gas sampling
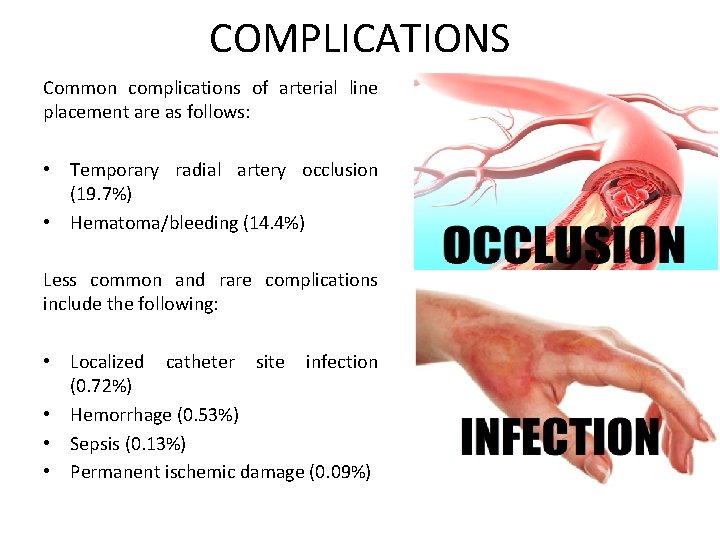
COMPLICATIONS Common complications of arterial line placement are as follows: • Temporary radial artery occlusion (19. 7%) • Hematoma/bleeding (14. 4%) Less common and rare complications include the following: • Localized catheter site infection (0. 72%) • Hemorrhage (0. 53%) • Sepsis (0. 13%) • Permanent ischemic damage (0. 09%)
REFERENCES 1. 2. 3. Shah, MR; Hasselblad, V; Stevenson, LW; Binanay, C; et al. (October 5, 2005). "Impact of the pulmonary artery catheter in critically ill patients: Meta-analysis of randomized clinical trials". JAMA. 294(13): 1664– 70. doi: 10. 1001/jama. 294. 13. 1664. PMID 16204666. Rajaram, SS; Desai, NK; Kalra, A; Gajera, M; et al. (2013). "Pulmonary artery catheters for adult patients in intensive care". Cochrane Anaesthesia Group. Cochrane Database of Systematic Reviews. 2. CD 003408. doi: 10. 1002/14651858. CD 003408. pub 3. PMID 234505 39. Sandham, JD; Hull, RD; Brant, RF; Knox, L; et al. (January 2, 2003). "A randomized, controlled trial of the use of pulmonary-artery catheters in high-risk surgical patients". The New England Journal of Medicine. 348 (1): 5– 14. doi: 10. 1056/NEJMoa 021108. PMID 12510037.

THANK YOU!