Intravitreous injection of tissue plasminogen activator in induction
- Slides: 1
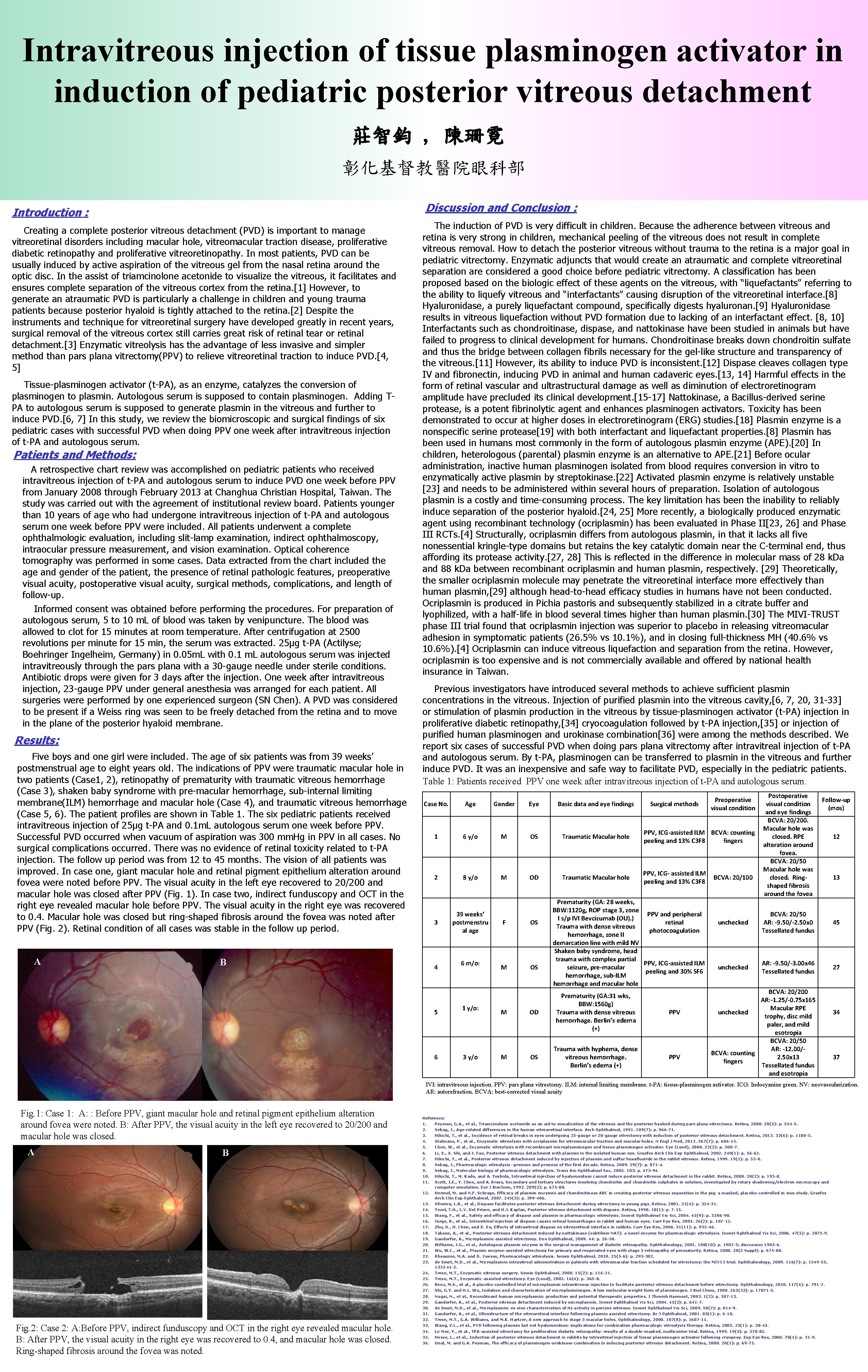
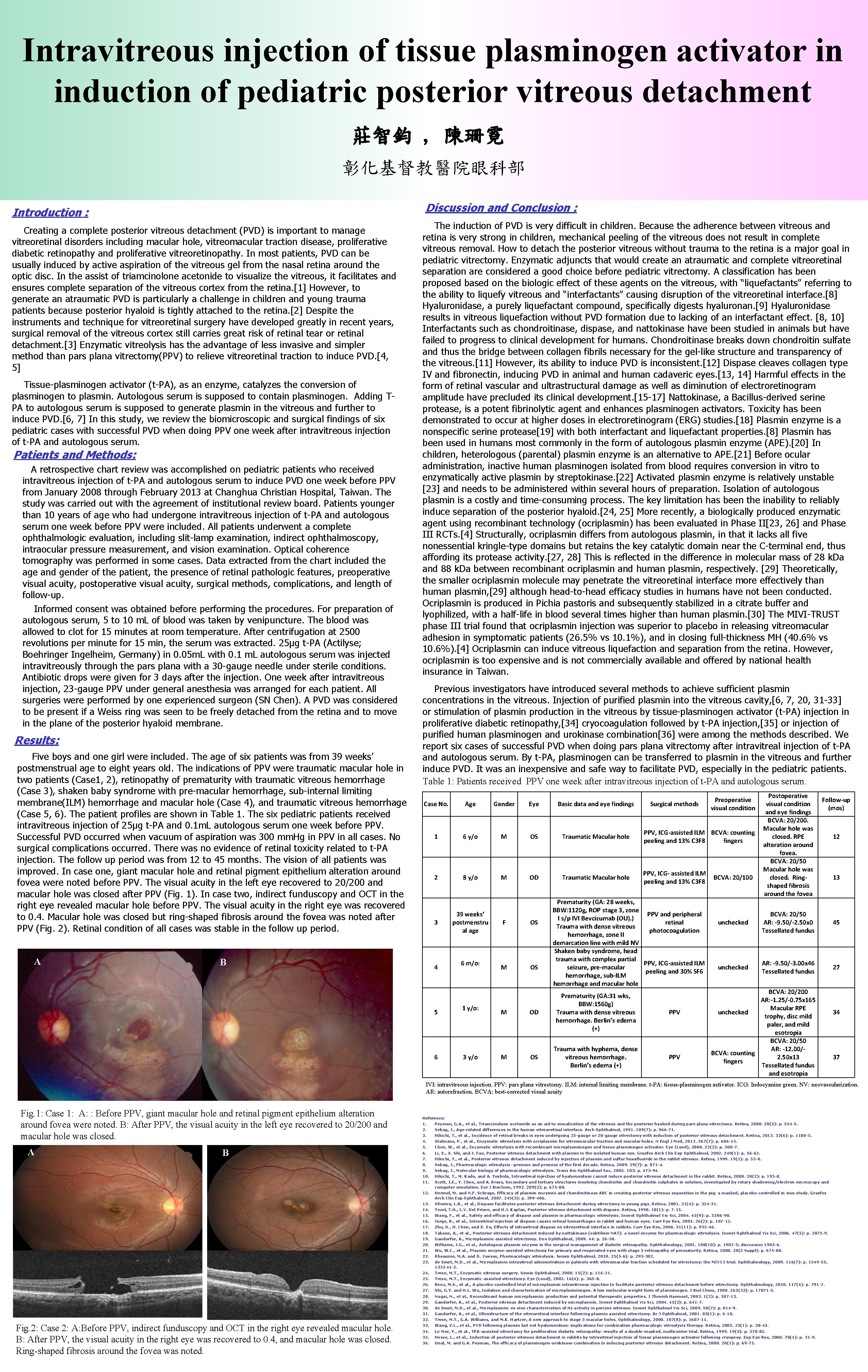
Intravitreous injection of tissue plasminogen activator in induction of pediatric posterior vitreous detachment 莊智鈞 , 陳珊霓 彰化基督教醫院眼科部 Discussion and Conclusion : Introduction : Creating a complete posterior vitreous detachment (PVD) is important to manage vitreoretinal disorders including macular hole, vitreomacular traction disease, proliferative diabetic retinopathy and proliferative vitreoretinopathy. In most patients, PVD can be usually induced by active aspiration of the vitreous gel from the nasal retina around the optic disc. In the assist of triamcinolone acetonide to visualize the vitreous, it facilitates and ensures complete separation of the vitreous cortex from the retina. [1] However, to generate an atraumatic PVD is particularly a challenge in children and young trauma patients because posterior hyaloid is tightly attached to the retina. [2] Despite the instruments and technique for vitreoretinal surgery have developed greatly in recent years, surgical removal of the vitreous cortex still carries great risk of retinal tear or retinal detachment. [3] Enzymatic vitreolysis has the advantage of less invasive and simpler method than pars plana vitrectomy(PPV) to relieve vitreoretinal traction to induce PVD. [4, 5] Tissue-plasminogen activator (t-PA), as an enzyme, catalyzes the conversion of plasminogen to plasmin. Autologous serum is supposed to contain plasminogen. Adding TPA to autologous serum is supposed to generate plasmin in the vitreous and further to induce PVD. [6, 7] In this study, we review the biomicroscopic and surgical findings of six pediatric cases with successful PVD when doing PPV one week after intravitreous injection of t-PA and autologous serum. Patients and Methods: A retrospective chart review was accomplished on pediatric patients who received intravitreous injection of t-PA and autologous serum to induce PVD one week before PPV from January 2008 through February 2013 at Changhua Christian Hospital, Taiwan. The study was carried out with the agreement of institutional review board. Patients younger than 10 years of age who had undergone intravitreous injection of t-PA and autologous serum one week before PPV were included. All patients underwent a complete ophthalmologic evaluation, including slit-lamp examination, indirect ophthalmoscopy, intraocular pressure measurement, and vision examination. Optical coherence tomography was performed in some cases. Data extracted from the chart included the age and gender of the patient, the presence of retinal pathologic features, preoperative visual acuity, postoperative visual acuity, surgical methods, complications, and length of follow-up. Informed consent was obtained before performing the procedures. For preparation of autologous serum, 5 to 10 m. L of blood was taken by venipuncture. The blood was allowed to clot for 15 minutes at room temperature. After centrifugation at 2500 revolutions per minute for 15 min, the serum was extracted. 25µg t-PA (Actilyse; Boehringer Ingelheim, Germany) in 0. 05 m. L with 0. 1 m. L autologous serum was injected intravitreously through the pars plana with a 30 -gauge needle under sterile conditions. Antibiotic drops were given for 3 days after the injection. One week after intravitreous injection, 23 -gauge PPV under general anesthesia was arranged for each patient. All surgeries were performed by one experienced surgeon (SN Chen). A PVD was considered to be present if a Weiss ring was seen to be freely detached from the retina and to move in the plane of the posterior hyaloid membrane. Results: Five boys and one girl were included. The age of six patients was from 39 weeks’ postmenstrual age to eight years old. The indications of PPV were traumatic macular hole in two patients (Case 1, 2), retinopathy of prematurity with traumatic vitreous hemorrhage (Case 3), shaken baby syndrome with pre-macular hemorrhage, sub-internal limiting membrane(ILM) hemorrhage and macular hole (Case 4), and traumatic vitreous hemorrhage (Case 5, 6). The patient profiles are shown in Table 1. The six pediatric patients received intravitreous injection of 25µg t-PA and 0. 1 m. L autologous serum one week before PPV. Successful PVD occurred when vacuum of aspiration was 300 mm. Hg in PPV in all cases. No surgical complications occurred. There was no evidence of retinal toxicity related to t-PA injection. The follow up period was from 12 to 45 months. The vision of all patients was improved. In case one, giant macular hole and retinal pigment epithelium alteration around fovea were noted before PPV. The visual acuity in the left eye recovered to 20/200 and macular hole was closed after PPV (Fig. 1). In case two, indirect funduscopy and OCT in the right eye revealed macular hole before PPV. The visual acuity in the right eye was recovered to 0. 4. Macular hole was closed but ring-shaped fibrosis around the fovea was noted after PPV (Fig. 2). Retinal condition of all cases was stable in the follow up period. A The induction of PVD is very difficult in children. Because the adherence between vitreous and retina is very strong in children, mechanical peeling of the vitreous does not result in complete vitreous removal. How to detach the posterior vitreous without trauma to the retina is a major goal in pediatric vitrectomy. Enzymatic adjuncts that would create an atraumatic and complete vitreoretinal separation are considered a good choice before pediatric vitrectomy. A classification has been proposed based on the biologic effect of these agents on the vitreous, with “liquefactants” referring to the ability to liquefy vitreous and “interfactants” causing disruption of the vitreoretinal interface. [8] Hyaluronidase, a purely liquefactant compound, specifically digests hyaluronan. [9] Hyaluronidase results in vitreous liquefaction without PVD formation due to lacking of an interfactant effect. [8, 10] Interfactants such as chondroitinase, dispase, and nattokinase have been studied in animals but have failed to progress to clinical development for humans. Chondroitinase breaks down chondroitin sulfate and thus the bridge between collagen fibrils necessary for the gel-like structure and transparency of the vitreous. [11] However, its ability to induce PVD is inconsistent. [12] Dispase cleaves collagen type IV and fibronectin, inducing PVD in animal and human cadaveric eyes. [13, 14] Harmful effects in the form of retinal vascular and ultrastructural damage as well as diminution of electroretinogram amplitude have precluded its clinical development. [15 -17] Nattokinase, a Bacillus-derived serine protease, is a potent fibrinolytic agent and enhances plasminogen activators. Toxicity has been demonstrated to occur at higher doses in electroretinogram (ERG) studies. [18] Plasmin enzyme is a nonspecific serine protease[19] with both interfactant and liquefactant properties. [8] Plasmin has been used in humans most commonly in the form of autologous plasmin enzyme (APE). [20] In children, heterologous (parental) plasmin enzyme is an alternative to APE. [21] Before ocular administration, inactive human plasminogen isolated from blood requires conversion in vitro to enzymatically active plasmin by streptokinase. [22] Activated plasmin enzyme is relatively unstable [23] and needs to be administered within several hours of preparation. Isolation of autologous plasmin is a costly and time-consuming process. The key limitation has been the inability to reliably induce separation of the posterior hyaloid. [24, 25] More recently, a biologically produced enzymatic agent using recombinant technology (ocriplasmin) has been evaluated in Phase II[23, 26] and Phase III RCTs. [4] Structurally, ocriplasmin differs from autologous plasmin, in that it lacks all five nonessential kringle-type domains but retains the key catalytic domain near the C-terminal end, thus affording its protease activity. [27, 28] This is reflected in the difference in molecular mass of 28 k. Da and 88 k. Da between recombinant ocriplasmin and human plasmin, respectively. [29] Theoretically, the smaller ocriplasmin molecule may penetrate the vitreoretinal interface more effectively than human plasmin, [29] although head-to-head efficacy studies in humans have not been conducted. Ocriplasmin is produced in Pichia pastoris and subsequently stabilized in a citrate buffer and lyophilized, with a half-life in blood several times higher than human plasmin. [30] The MIVI-TRUST phase III trial found that ocriplasmin injection was superior to placebo in releasing vitreomacular adhesion in symptomatic patients (26. 5% vs 10. 1%), and in closing full-thickness MH (40. 6% vs 10. 6%). [4] Ocriplasmin can induce vitreous liquefaction and separation from the retina. However, ocriplasmin is too expensive and is not commercially available and offered by national health insurance in Taiwan. Previous investigators have introduced several methods to achieve sufficient plasmin concentrations in the vitreous. Injection of purified plasmin into the vitreous cavity, [6, 7, 20, 31 -33] or stimulation of plasmin production in the vitreous by tissue-plasminogen activator (t-PA) injection in proliferative diabetic retinopathy, [34] cryocoagulation followed by t-PA injection, [35] or injection of purified human plasminogen and urokinase combination[36] were among the methods described. We report six cases of successful PVD when doing pars plana vitrectomy after intravitreal injection of t-PA and autologous serum. By t-PA, plasminogen can be transferred to plasmin in the vitreous and further induce PVD. It was an inexpensive and safe way to facilitate PVD, especially in the pediatric patients. Table 1: Patients received PPV one week after intravitreous injection of t-PA and autologous serum. Case No. Age Gender Eye Basic data and eye findings 1 6 y/o M OS Traumatic Macular hole PPV, ICG-assisted ILM BCVA: counting peeling and 13% C 3 F 8 fingers 2 8 y/o M OD Traumatic Macular hole PPV, ICG- assisted ILM peeling and 13% C 3 F 8 3 B 4 5 6 39 weeks’ postmenstru al age 6 m/o: 1 y/o: 3 y/o F OS M M Surgical methods Preoperative visual condition Prematurity (GA: 28 weeks, BBW: 1120 g, ROP stage 3, zone PPV and peripheral I s/p IVI Bevcizumab (OU). ) retinal Trauma with dense vitreous photocoagulation hemorrhage, zone II demarcation line with mild NV Shaken baby syndrome, head trauma with complex partial PPV, ICG-assisted ILM seizure, pre-macular peeling and 30% SF 6 hemorrhage, sub-ILM hemorrhage and macular hole OD Prematurity (GA: 31 wks, BBW: 1560 g) Trauma with dense vitreous hemorrhage. Berlin’s edema (+) PPV OS Trauma with hyphema, dense vitreous hemorrhage. Berlin’s edema (+) PPV BCVA: 20/100 Postoperative visual condition and eye findings BCVA: 20/200. Macular hole was closed. RPE alteration around fovea. BCVA: 20/50 Macular hole was closed. Ringshaped fibrosis around the fovea Follow-up (mos) 12 13 unchecked BCVA: 20/50 AR: -9. 50/-2. 50 x 0 Tessellated fundus 45 unchecked AR: -9. 50/-3. 00 x 46 Tessellated fundus 27 BCVA: 20/200 AR: -1. 25/-0. 75 x 165 Macular RPE unchecked trophy, disc mild paler, and mild esotropia BCVA: 20/50 AR: -12. 00/BCVA: counting 2. 50 x 13 fingers Tessellated fundus and esotropia 34 37 IVI: intravitreous injection. PPV: pars plana vitrectomy. ILM: internal limiting membrane. t-PA: tissue-plasminogen activator. ICG: Indocyanine green. NV: neovascularization. AR: autorefraction. BCVA: best-corrected visual acuity Fig. 1: Case 1: A: : Before PPV, giant macular hole and retinal pigment epithelium alteration around fovea were noted. B: After PPV, the visual acuity in the left eye recovered to 20/200 and macular hole was closed. A B Fig. 2: Case 2: A: Before PPV, indirect funduscopy and OCT in the right eye revealed macular hole. B: After PPV, the visual acuity in the right eye was recovered to 0. 4, and macular hole was closed. Ring-shaped fibrosis around the fovea was noted. Reference: 1. Peyman, G. A. , et al. , Triamcinolone acetonide as an aid to visualization of the vitreous and the posterior hyaloid during pars plana vitrectomy. Retina, 2000. 20(5): p. 554 -5. 2. Sebag, J. , Age-related differences in the human vitreoretinal interface. Arch Ophthalmol, 1991. 109(7): p. 966 -71. 3. Hikichi, T. , et al. , Incidence of retinal breaks in eyes undergoing 23 -gauge or 20 -gauge vitrectomy with induction of posterior vitreous detachment. Retina, 2012. 32(6): p. 1100 -5. 4. Stalmans, P. , et al. , Enzymatic vitreolysis with ocriplasmin for vitreomacular traction and macular holes. N Engl J Med, 2012. 367(7): p. 606 -15. Chen, W. , et al. , Enzymatic vitreolysis with recombinant microplasminogen and tissue plasminogen activator. Eye (Lond), 2008. 22(2): p. 300 -7. 6. Li, X. Shi, and J. Fan, Posterior vitreous detachment with plasmin in the isolated human eye. Graefes Arch Clin Exp Ophthalmol, 2002. 240(1): p. 56 -62. 7. Hikichi, T. , et al. , Posterior vitreous detachment induced by injection of plasmin and sulfur hexafluoride in the rabbit vitreous. Retina, 1999. 19(1): p. 55 -8. Sebag, J. , Pharmacologic vitreolysis--premise and promise of the first decade. Retina, 2009. 29(7): p. 871 -4. 9. Sebag, J. , Molecular biology of pharmacologic vitreolysis. Trans Am Ophthalmol Soc, 2005. 103: p. 473 -94. 10. Hikichi, T. , M. Kado, and A. Yoshida, Intravitreal injection of hyaluronidase cannot induce posterior vitreous detachment in the rabbit. Retina, 2000. 20(2): p. 195 -8. 11. Scott, J. E. , Y. Chen, and A. Brass, Secondary and tertiary structures involving chondroitin and chondroitin sulphates in solution, investigated by rotary shadowing/electron microscopy and computer simulation. Eur J Biochem, 1992. 209(2): p. 675 -80. 12. Hermel, M. and N. F. Schrage, Efficacy of plasmin enzymes and chondroitinase ABC in creating posterior vitreous separation in the pig: a masked, placebo-controlled in vivo study. Graefes Arch Clin Exp Ophthalmol, 2007. 245(3): p. 399 -406. 13. Oliveira, L. B. , et al. , Dispase facilitates posterior vitreous detachment during vitrectomy in young pigs. Retina, 2001. 21(4): p. 324 -31. 14. Tezel, T. H. , L. V. Del Priore, and H. J. Kaplan, Posterior vitreous detachment with dispase. Retina, 1998. 18(1): p. 7 -15. Wang, F. , et al. , Safety and efficacy of dispase and plasmin in pharmacologic vitreolysis. Invest Ophthalmol Vis Sci, 2004. 45(9): p. 3286 -90. 16. Jorge, R. , et al. , Intravitreal injection of dispase causes retinal hemorrhages in rabbit and human eyes. Curr Eye Res, 2003. 26(2): p. 107 -12. 17. Zhu, D. , H. Chen, and X. Xu, Effects of intravitreal dispase on vitreoretinal interface in rabbits. Curr Eye Res, 2006. 31(11): p. 935 -46. 18. Takano, A. , et al. , Posterior vitreous detachment induced by nattokinase (subtilisin NAT): a novel enzyme for pharmacologic vitreolysis. Invest Ophthalmol Vis Sci, 2006. 47(5): p. 2075 -9. 19. Gandorfer, A. , Microplasmin-assisted vitrectomy. Dev Ophthalmol, 2009. 44: p. 26 -30. 20. Williams, J. G. , et al. , Autologous plasmin enzyme in the surgical management of diabetic retinopathy. Ophthalmology, 2001. 108(10): p. 1902 -5; discussion 1905 -6. 21. Wu, W. C. , et al. , Plasmin enzyme-assisted vitrectomy for primary and reoperated eyes with stage 5 retinopathy of prematurity. Retina, 2008. 28(3 Suppl): p. S 75 -80. 22. Rheaume, M. A. and D. Vavvas, Pharmacologic vitreolysis. Semin Ophthalmol, 2010. 25(5 -6): p. 295 -302. 23. de Smet, M. D. , et al. , Microplasmin intravitreal administration in patients with vitreomacular traction scheduled for vitrectomy: the MIVI I trial. Ophthalmology, 2009. 116(7): p. 1349 -55, 1355 e 1 -2. 24. Trese, M. T. , Enzymatic vitreous surgery. Semin Ophthalmol, 2000. 15(2): p. 116 -21. 25. Trese, M. T. , Enzymatic-assisted vitrectomy. Eye (Lond), 2002. 16(4): p. 365 -8. 26. Benz, M. S. , et al. , A placebo-controlled trial of microplasmin intravitreous injection to facilitate posterior vitreous detachment before vitrectomy. Ophthalmology, 2010. 117(4): p. 791 -7. 27. Shi, G. Y. and H. L. Wu, Isolation and characterization of microplasminogen. A low molecular weight form of plasminogen. J Biol Chem, 1988. 263(32): p. 17071 -5. 28. Nagai, N. , et al. , Recombinant human microplasmin: production and potential therapeutic properties. J Thromb Haemost, 2003. 1(2): p. 307 -13. 29. Gandorfer, A. , et al. , Posterior vitreous detachment induced by microplasmin. Invest Ophthalmol Vis Sci, 2004. 45(2): p. 641 -7. 30. de Smet, M. D. , et al. , Microplasmin: ex vivo characterization of its activity in porcine vitreous. Invest Ophthalmol Vis Sci, 2009. 50(2): p. 814 -9. 31. Gandorfer, A. , et al. , Ultrastructure of the vitreoretinal interface following plasmin assisted vitrectomy. Br J Ophthalmol, 2001. 85(1): p. 6 -10. 32. Trese, M. T. , G. A. Williams, and M. K. Hartzer, A new approach to stage 3 macular holes. Ophthalmology, 2000. 107(8): p. 1607 -11. 33. Wang, Z. L. , et al. , PVD following plasmin but not hyaluronidase: implications for combination pharmacologic vitreolysis therapy. Retina, 2005. 25(1): p. 38 -43. 34. Le Mer, Y. , et al. , TPA-assisted vitrectomy for proliferative diabetic retinopathy: results of a double-masked, multicenter trial. Retina, 1999. 19(5): p. 378 -82. 35. Hesse, L. , et al. , Induction of posterior vitreous detachment in rabbits by intravitreal injection of tissue plasminogen activator following cryopexy. Exp Eye Res, 2000. 70(1): p. 31 -9. 36. Unal, M. and G. A. Peyman, The efficacy of plasminogen-urokinase combination in inducing posterior vitreous detachment. Retina, 2000. 20(1): p. 69 -75.