INTRAPARTUM ANTIBIOTIC PROPHYLAXIS FOR GROUP B STREPTOCOCCAL INFECTION
INTRAPARTUM ANTIBIOTIC PROPHYLAXIS FOR GROUP B STREPTOCOCCAL INFECTION Jeanine Spielberger MD 9/23/2013

GOALS AND OBJECTIVES Recite indications and non-indications for intrapartum GBS prophylaxis to prevent early onset GBS disease. Select appropriate antibiotics for intrapartum GBS prophylaxis. Manage a patient with suspected preterm labor and unknown GBS status.

WHY THIS TOPIC? Early-onset GBS Disease is leading cause of neonatal sepsis in U. S. § Annual incidence in 2008: 0. 28 cases / 1, 000 live births § Estimated 1, 200 cases in 2008 Case fatality rate § 1970 s: As high as 50% § 4 -6% in recent years "Image courtesy of Praisaeng/ Free. Digital. Photos. net".

GROUP B STREPTOCOCCUS Gram positive, beta hemolytic bacteria § Common colonizer of human gastrointestinal and genitourinary tracts § Recognized as causing disease in humans in the 1930 s § Emerged as most common cause of sepsis and meningitis in infants <3 months in the 1970 s
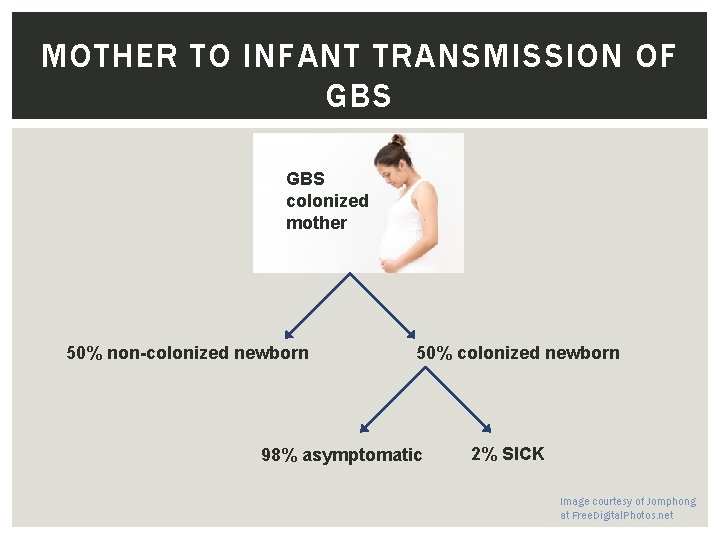
MOTHER TO INFANT TRANSMISSION OF GBS colonized mother 50% non-colonized newborn 50% colonized newborn 98% asymptomatic 2% SICK Image courtesy of Jomphong at Free. Digital. Photos. net
INDICATIONS FOR INTRAPARTUM ANTIBIOTIC PROPHYLAXIS Indicated? Image courtesy of Anitapeppers at morguefile. com
INDICATIONS FOR INTRAPARTUM ANTIBIOTIC PROPHYLAXIS Indicated? Previous infant with invasive GBS disease GBS bacteriuria current pregnancy Positive vaginal-rectal GBS screening culture current pregnancy Unknown GBS status at onset of labor and any of the following: § Delivery <37 weeks’ gestation § ROM >/=18 hours § Intrapartum test positive for GBS § Intrapartum temperature >/= 100. 4°F
NONINDICATIONS FOR INTRAPARTUM ANTIBIOTIC PROPHYLAXIS Not Indicated? Image courtesy of Anitapeppers at morguefile. com
NONINDICATIONS FOR INTRAPARTUM ANTIBIOTIC Not Indicated Colonization with GBS during a previous pregnancy* GBS bacteriuria during a previous pregnancy* Negative vaginal-rectal GBS screening culture in late gestation during current pregnancy, regardless of intrapartum risk factors Cesarean delivery before onset of labor with intact amniotic membranes *unless an indication for GBS prophylaxis is present for current pregnancy

RECOMMENDED ANTIBIOTICS Penicillin G § 5 million units IV, followed by 2. 5 - 3. 0 million units IV every four hours Ampicillin is an acceptable alternative
RECOMMENDED ANTIBIOTICS- PENICILLIN ALLERGY ? "Image courtesy of arztsamui/ Free. Digital. Photos. net".
RECOMMENDED ANTIBIOTIC- PENICILLIN ALLERGIC NOT high risk for anaphylaxis- Cefazolin "Image courtesy of moggara 12/ Free. Digital. Photos. net".
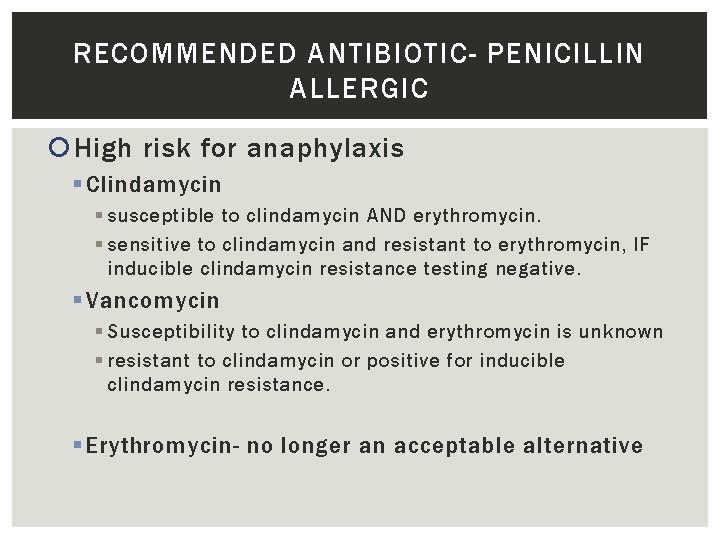
RECOMMENDED ANTIBIOTIC- PENICILLIN ALLERGIC High risk for anaphylaxis § Clindamycin § susceptible to clindamycin AND erythromycin. § sensitive to clindamycin and resistant to erythromycin, IF inducible clindamycin resistance testing negative. § Vancomycin § Susceptibility to clindamycin and erythromycin is unknown § resistant to clindamycin or positive for inducible clindamycin resistance. § Erythromycin- no longer an acceptable alternative
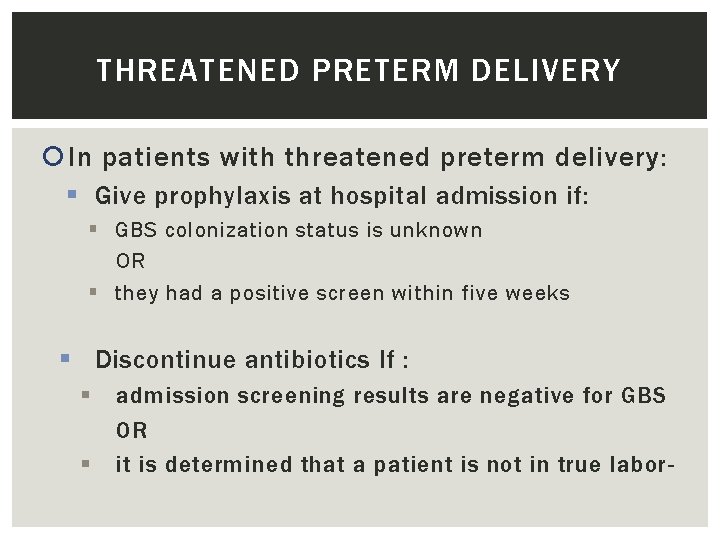
THREATENED PRETERM DELIVERY In patients with threatened preterm delivery: § Give prophylaxis at hospital admission if: § GBS colonization status is unknown OR § they had a positive screen within five weeks § Discontinue antibiotics If : § § admission screening results are negative for GBS OR it is determined that a patient is not in true labor-

MISSED PREVENTION OPPORTUNITIES Infants born preterm 50% screened prior to admission 18% of GBS unknown screened on admission Preterm 20% less likely to receive IAP when indicated than term Van Dyke, NEJM 2009, 360: 2626 -36.
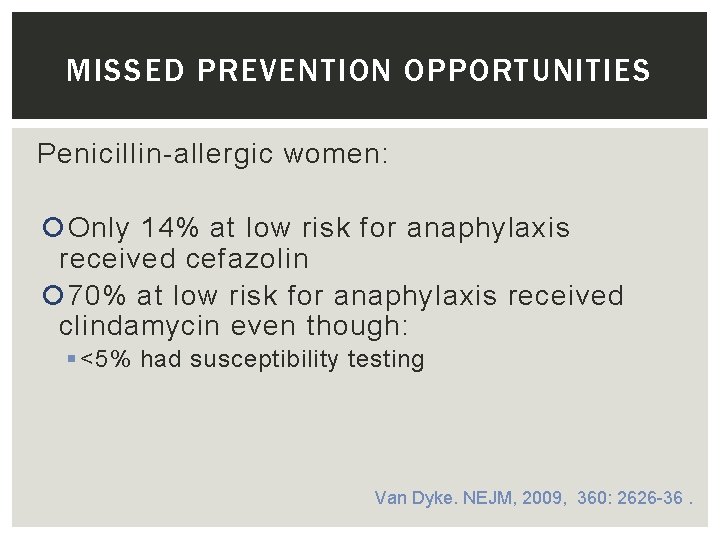
MISSED PREVENTION OPPORTUNITIES Penicillin-allergic women: Only 14% at low risk for anaphylaxis received cefazolin 70% at low risk for anaphylaxis received clindamycin even though: § <5% had susceptibility testing Van Dyke. NEJM, 2009, 360: 2626 -36.

THERE’S AN APP FOR THAT!
CONCLUSIONS PENICILLIN is first line for intrapartum prophylaxis against early onset GBS disease. CEFAZOLIN provides adequate prophylaxis in women who have PCN allergy who are LOW RISK for anaphylaxis. Clindamycin should be used ONLY if appropriate susceptibility testing has been done, otherwise use vancomycin. Obtain GBS testing and start antibiotics in ANY woman who is admitted in preterm labor who does not have an available GBS result. Indications and non-indications for intrapartum prophylaxis are available through CDC app and web site.
- Slides: 19