INTRANASAL NALOXONE Education and Training Module for Whatcom
- Slides: 30
INTRANASAL NALOXONE Education and Training Module for Whatcom County EMS
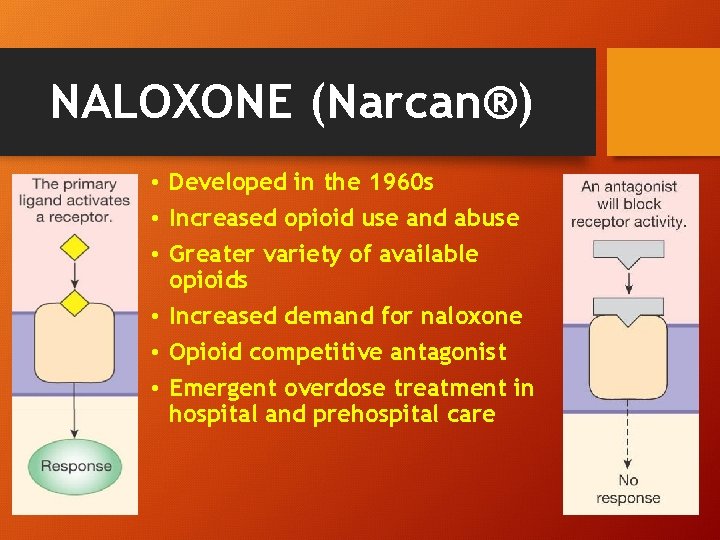
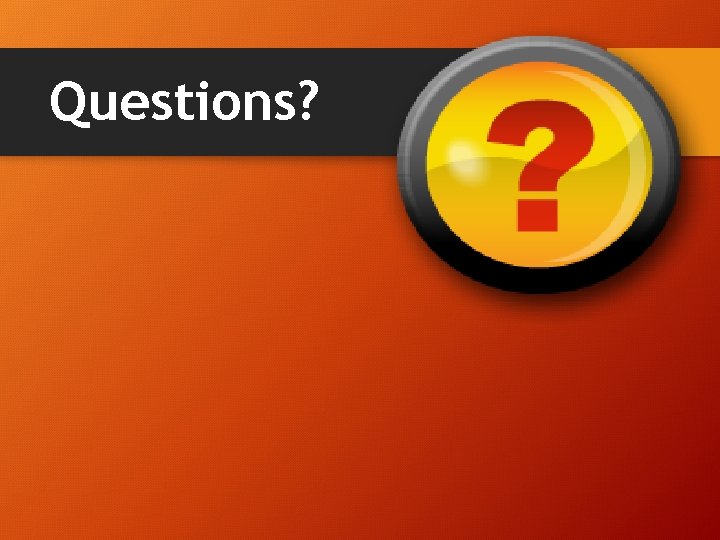
NALOXONE (Narcan®) • Developed in the 1960 s • Increased opioid use and abuse • Greater variety of available opioids • Increased demand for naloxone • Opioid competitive antagonist • Emergent overdose treatment in hospital and prehospital care
Frequently Prescribed Opioids • Buprenorphine • Codeine • Fentanyl • Hydrocodone �Hydromorphone �Methadone �Morphine �Oxycodone
Frequently Prescribed Combination Opioid Medications • Lorcet®, Lortab®, Norco®, Vicodan®: Hydrocodone + acetaminophen • Percocet®: Oxycodone + acetaminophen • Percodan®: Oxycodone + aspirin • Suboxone®: Buprenorphine + naloxone Illegal opioids • Opium • Heroin
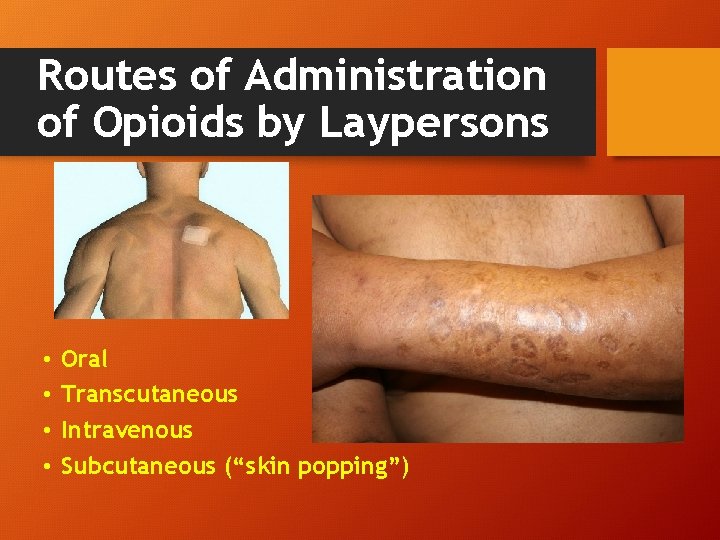
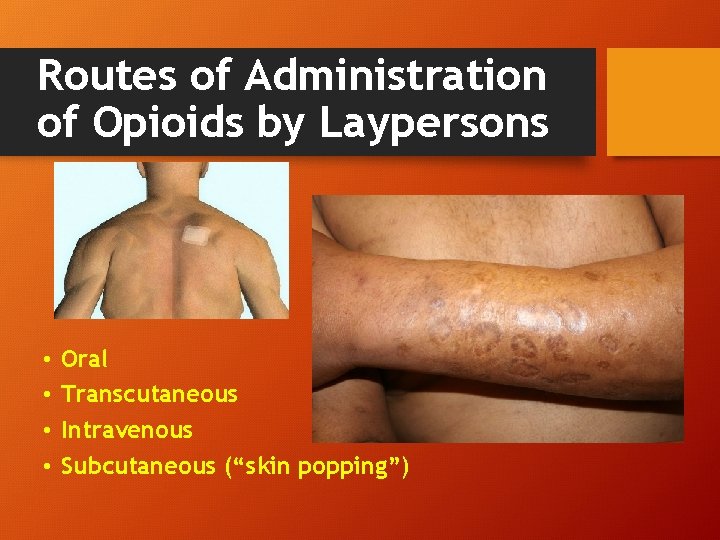
Routes of Administration of Opioids by Laypersons • • Oral Transcutaneous Intravenous Subcutaneous (“skin popping”)
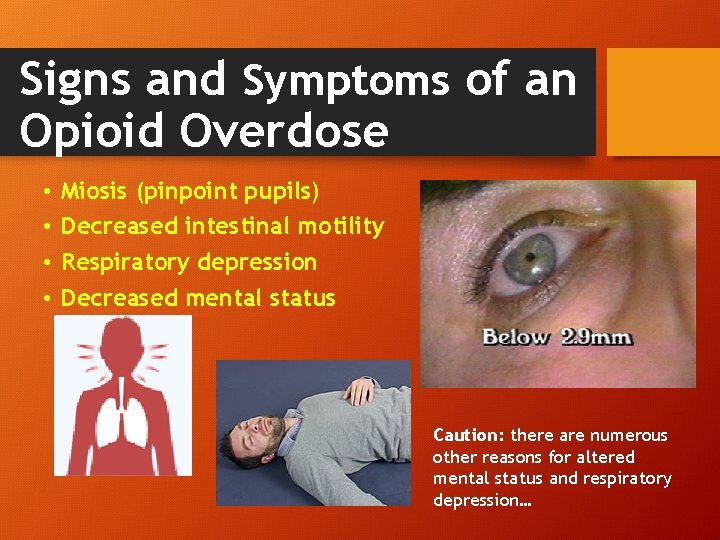
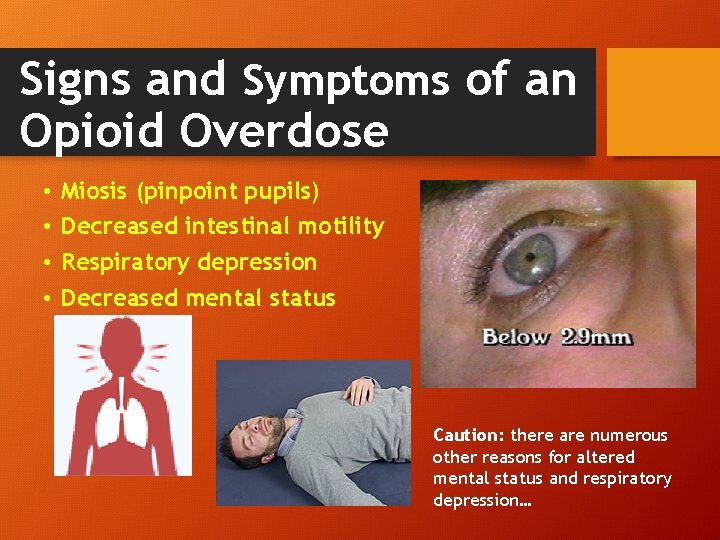
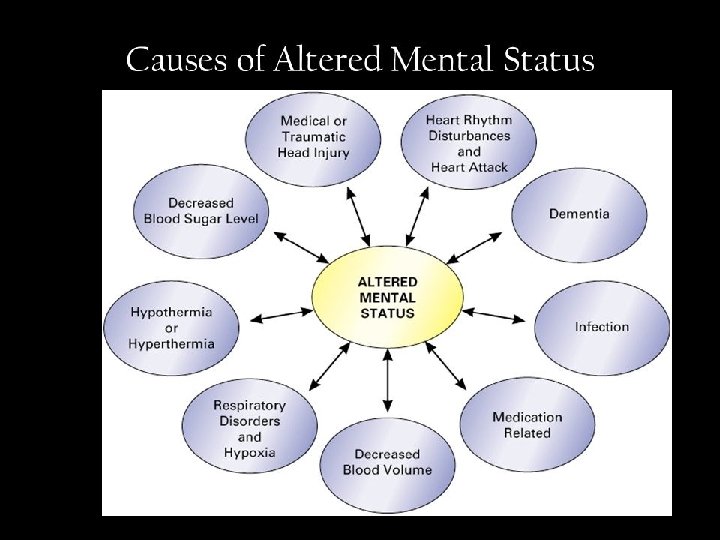
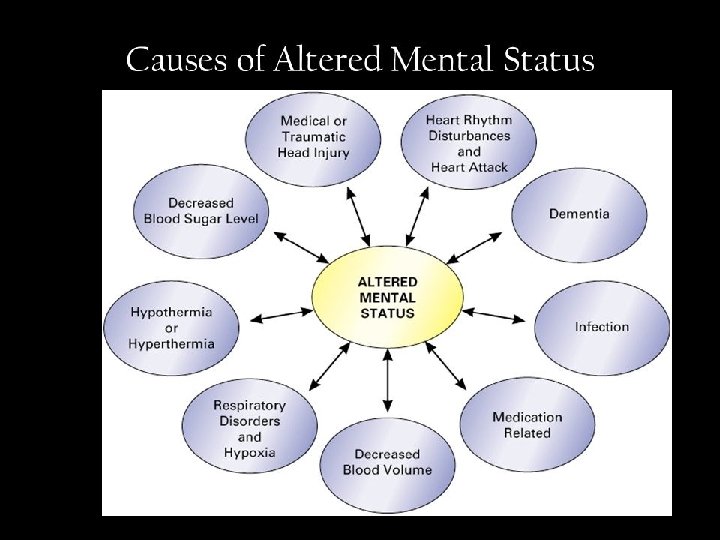
Signs and Symptoms of an Opioid Overdose • • Miosis (pinpoint pupils) Decreased intestinal motility Respiratory depression Decreased mental status Caution: there are numerous other reasons for altered mental status and respiratory depression…
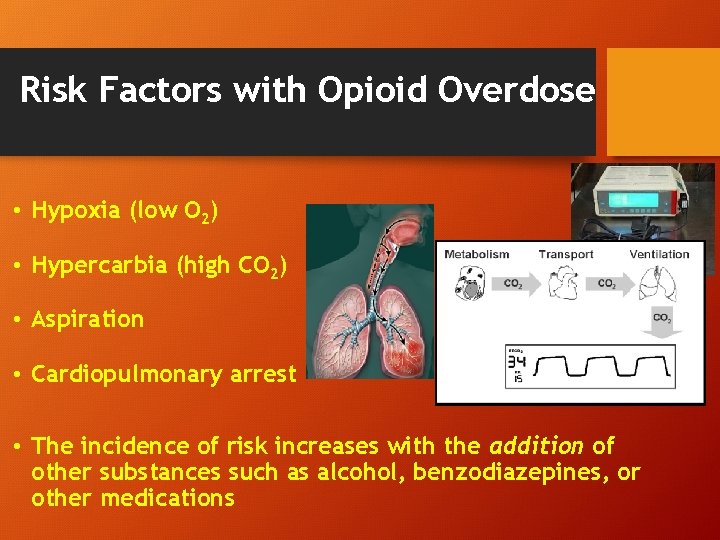
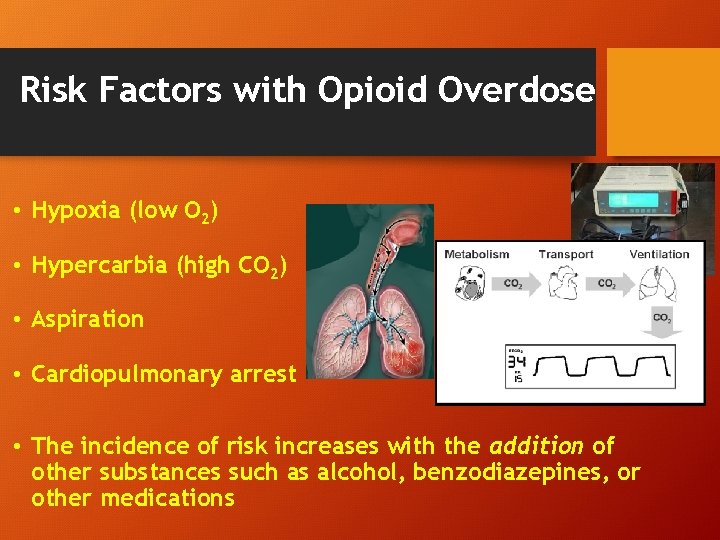
Risk Factors with Opioid Overdose • Hypoxia (low O 2) • Hypercarbia (high CO 2) • Aspiration • Cardiopulmonary arrest • The incidence of risk increases with the addition of other substances such as alcohol, benzodiazepines, or other medications
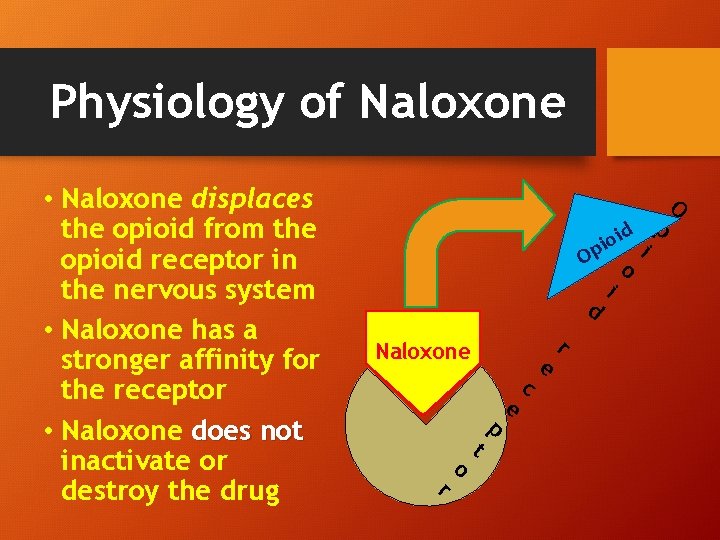
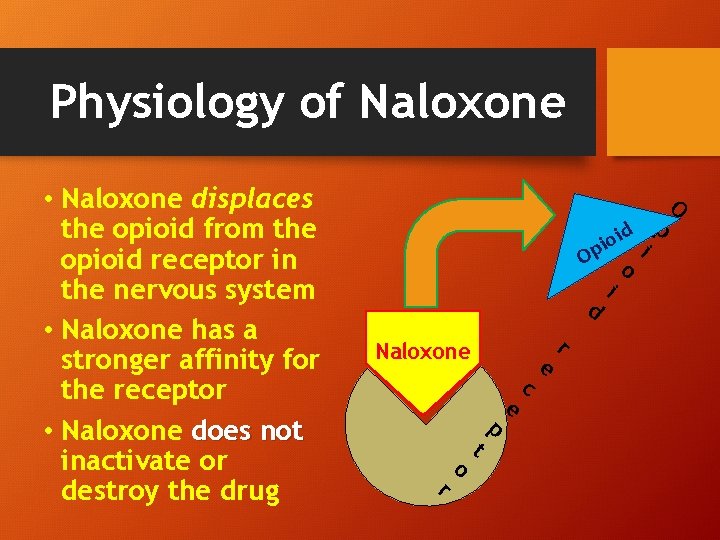
Physiology of Naloxone • Naloxone displaces the opioid from the opioid receptor in the nervous system • Naloxone has a stronger affinity for the receptor • Naloxone does not inactivate or destroy the drug p d i io i p O d Naloxone r o t p e c e r i o O
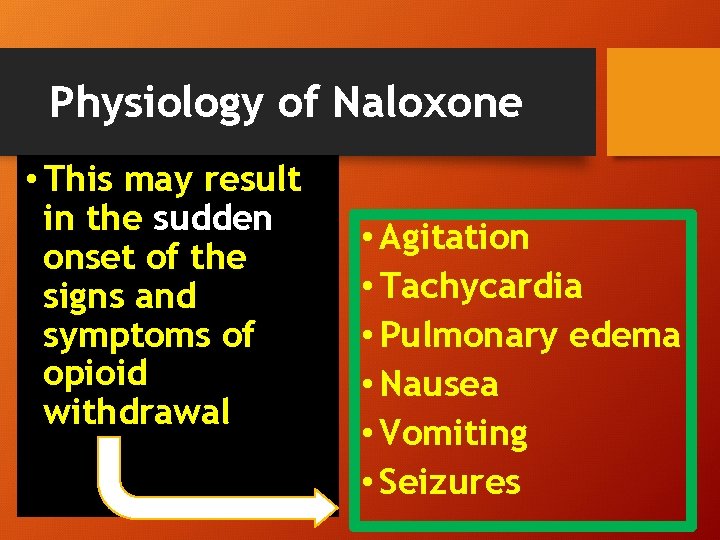
Physiology of Naloxone • This may result in the sudden onset of the signs and symptoms of opioid withdrawal • Agitation • Tachycardia • Pulmonary edema • Nausea • Vomiting • Seizures
Routes of Administration of Naloxone • Endotracheal • Intramuscular • Intranasal • Intravenous
Benefits of Intranasal Route of Naloxone Administration • Equivalent clinical efficacy to intravenous naloxone • Intravenous access may be impossible to establish in chronic drug abusers
Benefits of Intranasal Route of Naloxone Administration • Intranasal atomizers facilitate administration of naloxone • Reduces the risk of needle stick and associated infectious disease exposure
Key Points for Intranasal Naloxone Administration • Medical program director approval is mandatory • A protocol from the medical program director is mandatory • Training is mandatory
Intranasal Administration Technique • The dose of naloxone is approximately 1 mg per nostril • Naloxone, in the form of a liquid solution, can be drawn up in a syringe or provided as a pre-filled syringe
Intranasal Administration Technique • The tip of the syringe should be placed just inside the nostril • Placement of the syringe too far inside the nasal cavity may traumatize nasal passages or cause epistaxis
Intranasal Administration Technique • If used, remove the needle from the syringe and attach the mucosal atomizer device (MAD) • If prefilled syringe attach the MAD device
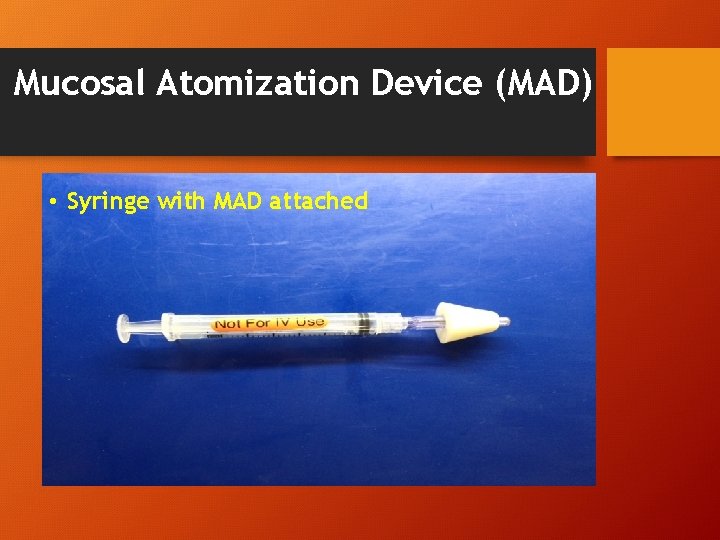
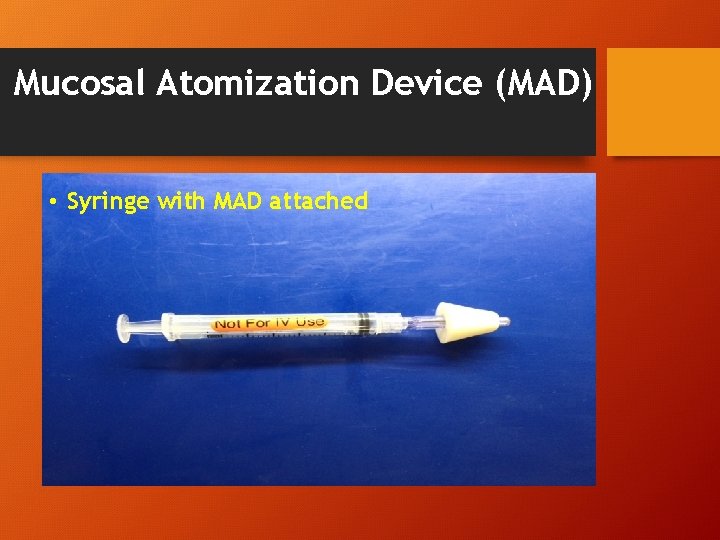
Mucosal Atomization Device (MAD) • Syringe with MAD attached
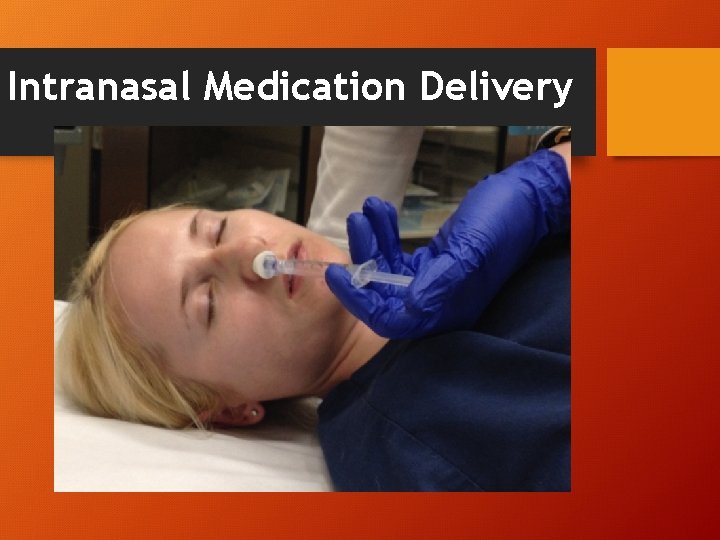
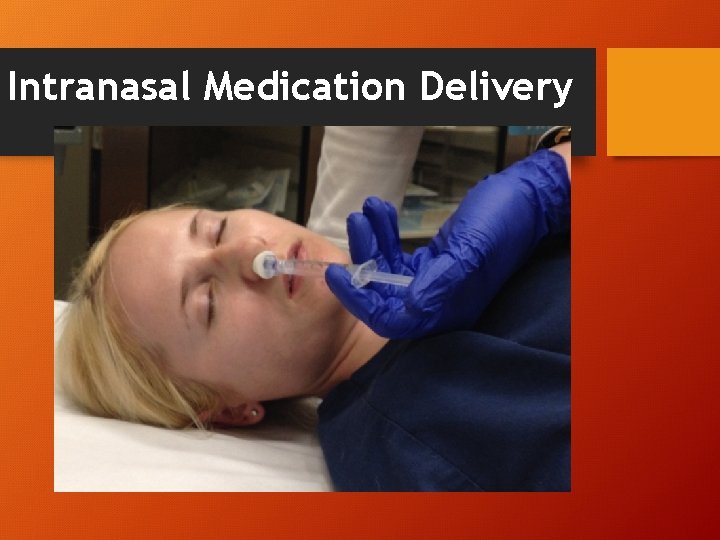
Intranasal Medication Delivery
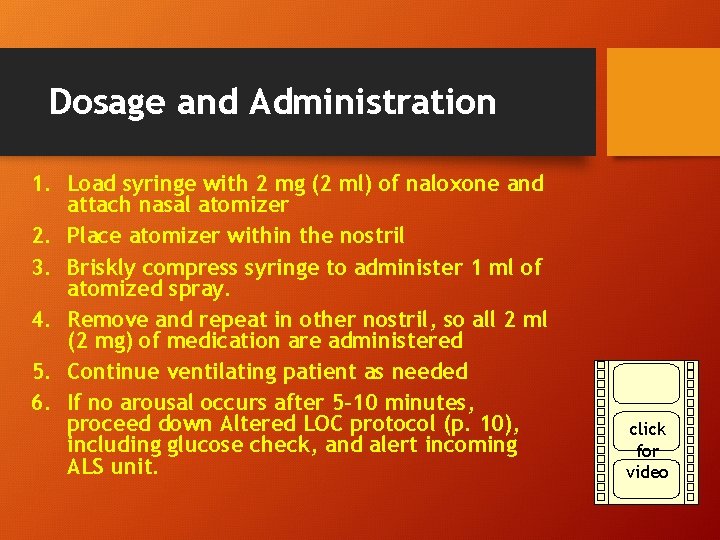
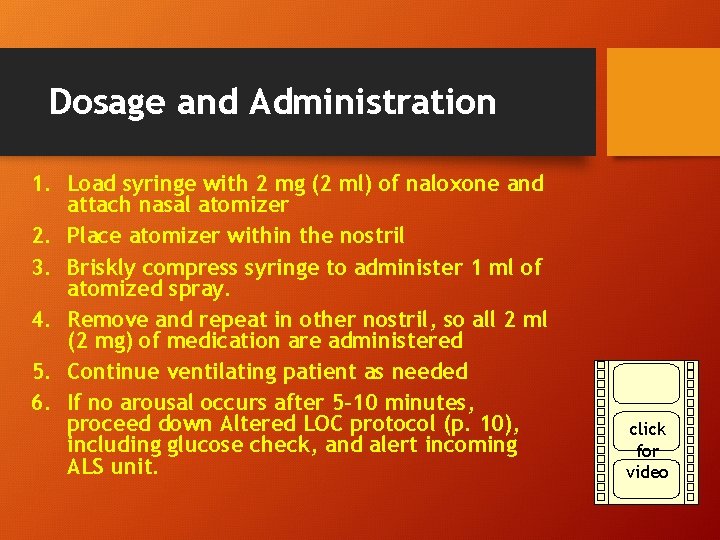
Dosage and Administration 1. Load syringe with 2 mg (2 ml) of naloxone and attach nasal atomizer 2. Place atomizer within the nostril 3. Briskly compress syringe to administer 1 ml of atomized spray. 4. Remove and repeat in other nostril, so all 2 ml (2 mg) of medication are administered 5. Continue ventilating patient as needed 6. If no arousal occurs after 5 -10 minutes, proceed down Altered LOC protocol (p. 10), including glucose check, and alert incoming ALS unit. click for video
Post-Administration • Intranasal naloxone takes 3 -5 minutes to begin working, and may not completely reverse the decreased level of consciousness associated with opioid overdose. • Patients often just begin breathing; do not always expect full arousal. • The goal is to improve breathing, but EMS should support ventilations until breathing is adequate. • If the patient wakes up, explain that they have experienced an overdose and were given Naloxone
Safety Considerations • Administration of naloxone may result in the rapid onset of signs and symptoms of opioid withdrawal • This may place the patient and bystanders at risk • Education on managing the after effects of naloxone should be discussed • • • Agitation Tachycardia Pulmonary edema Nausea Vomiting Seizures
Safety Considerations • Patients should be assessed for other causes of altered mental status and/or respiratory depression (hypoxia, hypoglycemia, head injury, shock, stroke) • Prior to the administration of naloxone, all patients should initially receive appropriate medical interventions, and support of airway and circulation (ABCs)
Safety Considerations Due to potential adverse effects, the administration of naloxone by BLS is reserved to SICK patients with known or suspected opioid overdose with: -Impending cardiopulmonary arrest, -Respiratory depression (RR <6 pm), or -Circulatory Shock
Safety Considerations • The half-life of naloxone is relatively brief (as short as 30 min) • All patients should be monitored for recurrent symptoms, including altered mental status, respiratory depression, and circulatory compromise
Practice Case #1 • You respond to a known drug abuser who is found unconscious with a hypodermic needle inserted into her arm. Her pupils are pinpoint and she does not respond to painful stimuli. Upon assessment of vital signs, her blood pressure is 110/70, pulse is 60, respiratory rate is 2, and pulse ox reading 84%. • What is the first action you should take?
Practice Case #1 • Patient is apneic as evidenced by her RR of 2. Appropriate initial action is to open the airway and administer oxygen via bag valve mask. • Therapeutic interventions to support the airway, breathing, and circulation should be initiated prior to the administration of naloxone.
Practice Case #2 • You respond to the home of a diabetic hospice cancer patient. He has decreased mental status and pinpoint pupils. His wife checked his glucose prior to calling 9 -11 and it is 170. The patient was at his baseline mental status until she applied a transcutaneous fentanyl patch 8 hrs ago recently prescribed for pain control. Blood pressure 130/80, pulse of 70, respiratory rate of 18, and a pulse oximetry reading of 95%. • What action should you take?
Practice Case #2 • This patient has stable vital signs. You may be direct to remove the fentanyl patch, and await ALS arrival. • Intranasal Naloxone would only be indicated if respiratory depression or cardiovascular collapse occurred.
Questions?