Intramedullary nailing to ream or not to ream


- Slides: 27
Intramedullary nailing— to ream or not to ream? AO Trauma Basic Principles Course
Learning objectives • Describe the biological effects of reaming • Recognize the indications for reamed and unreamed nails • Appreciate the evidence behind the recommendations for reaming

Why ream? • Since 1951 • Küntscher nail • Cloverleaf nail • Flexible hand reamers
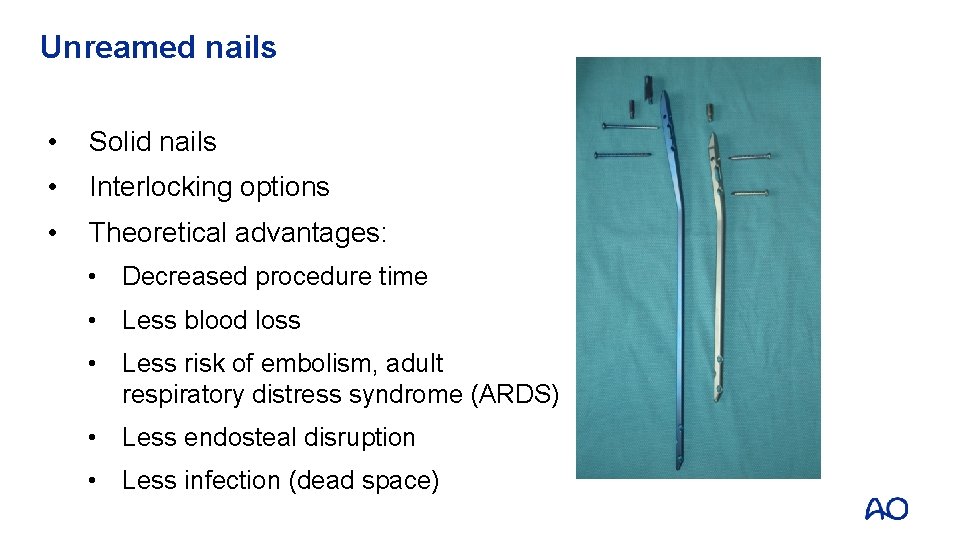
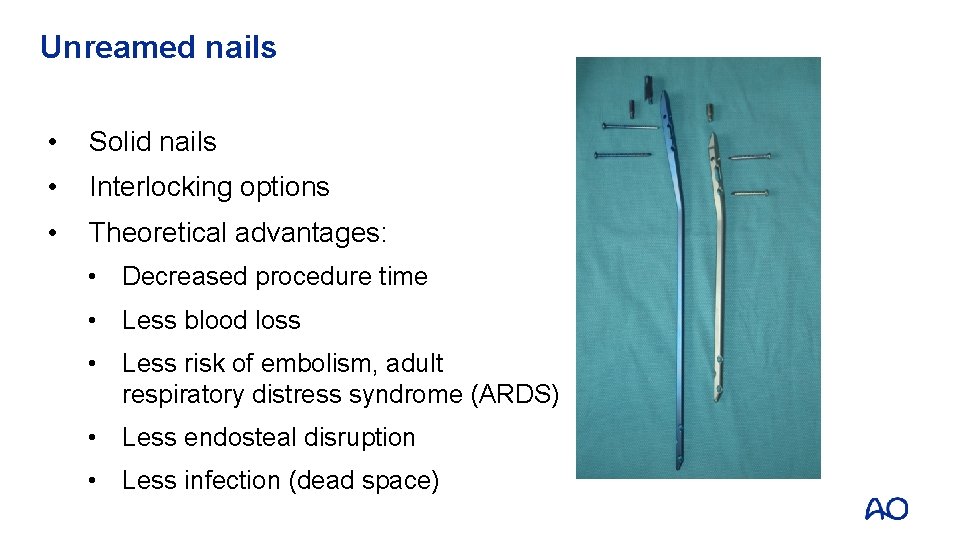
Unreamed nails • Solid nails • Interlocking options • Theoretical advantages: • Decreased procedure time • Less blood loss • Less risk of embolism, adult respiratory distress syndrome (ARDS) • Less endosteal disruption • Less infection (dead space)
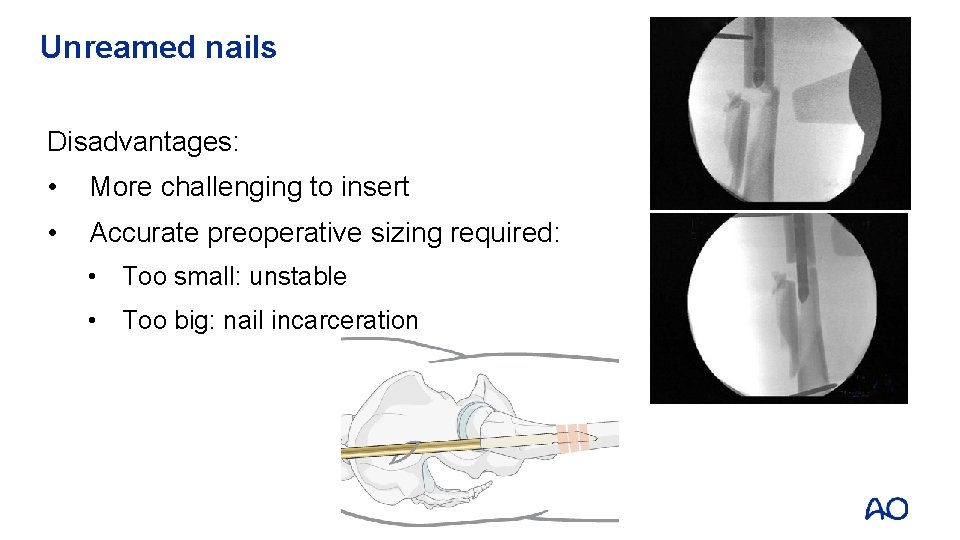
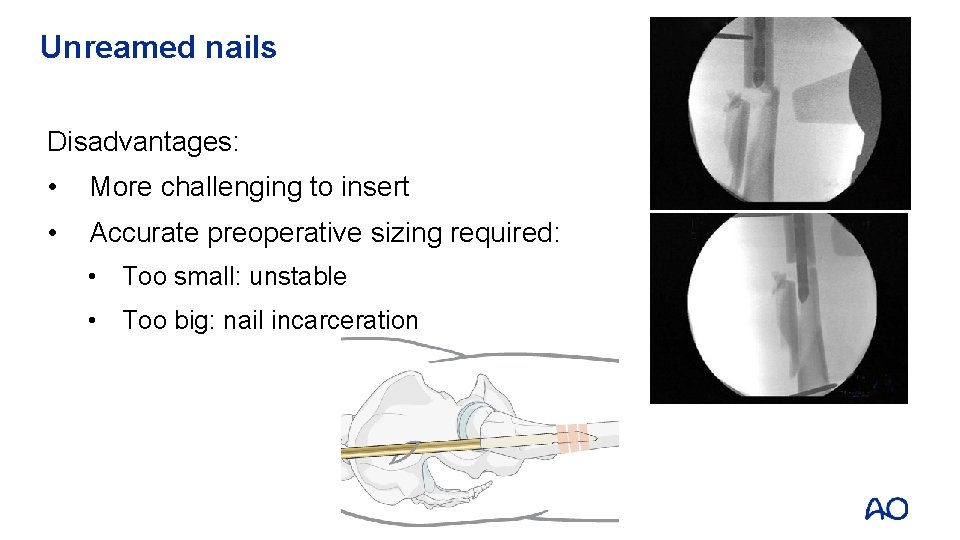
Unreamed nails Disadvantages: • More challenging to insert • Accurate preoperative sizing required: • Too small: unstable • Too big: nail incarceration
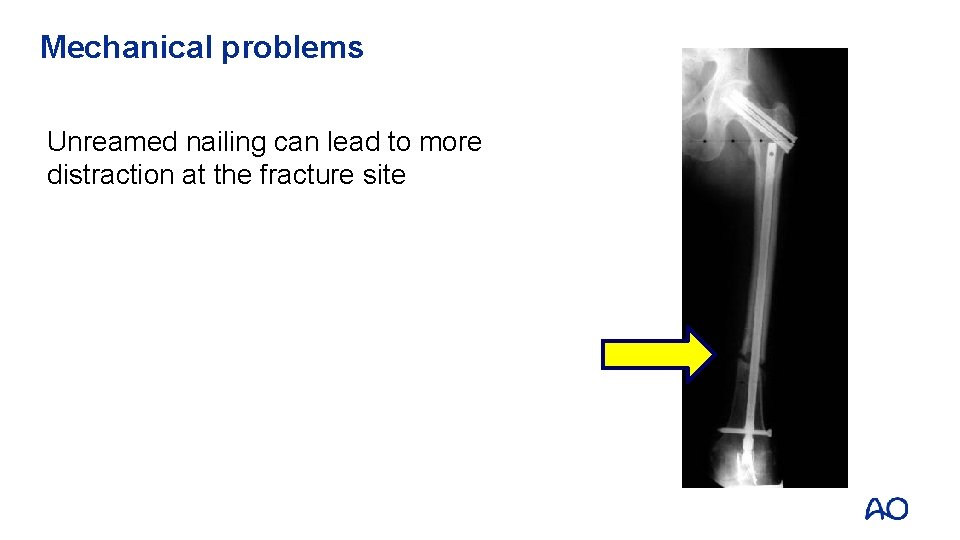
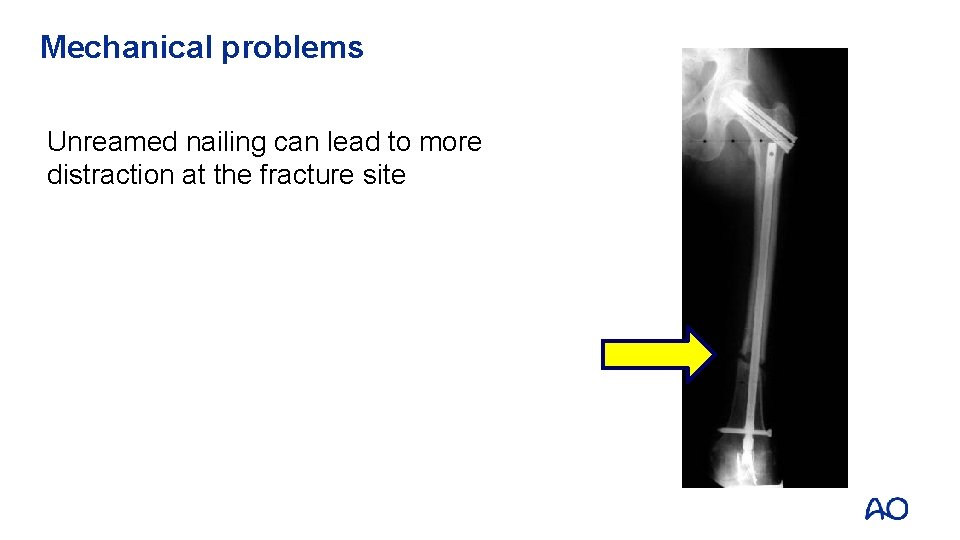
Mechanical problems Unreamed nailing can lead to more distraction at the fracture site

Mechanical problems • Small diameter unreamed nails: • Prone to fatigue failure • Less confidence for early weight bearing
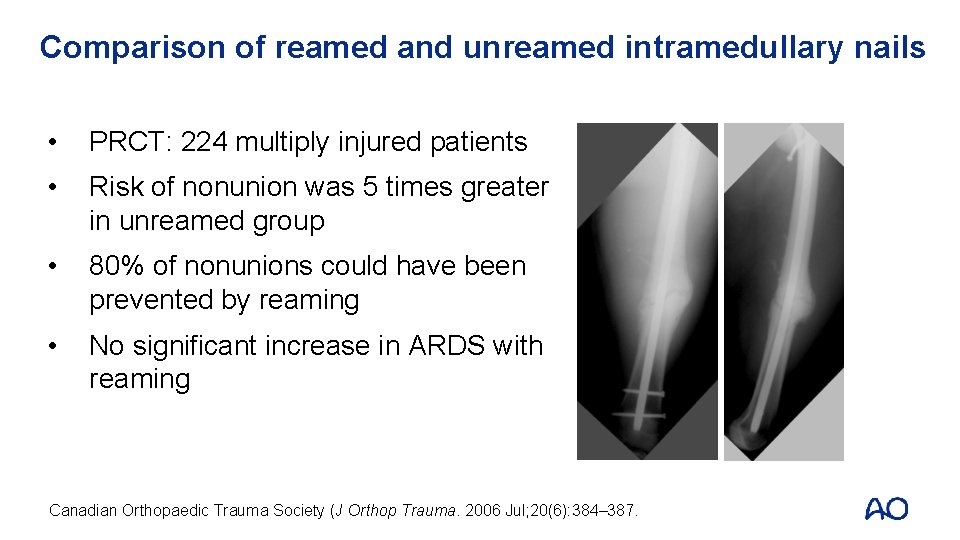
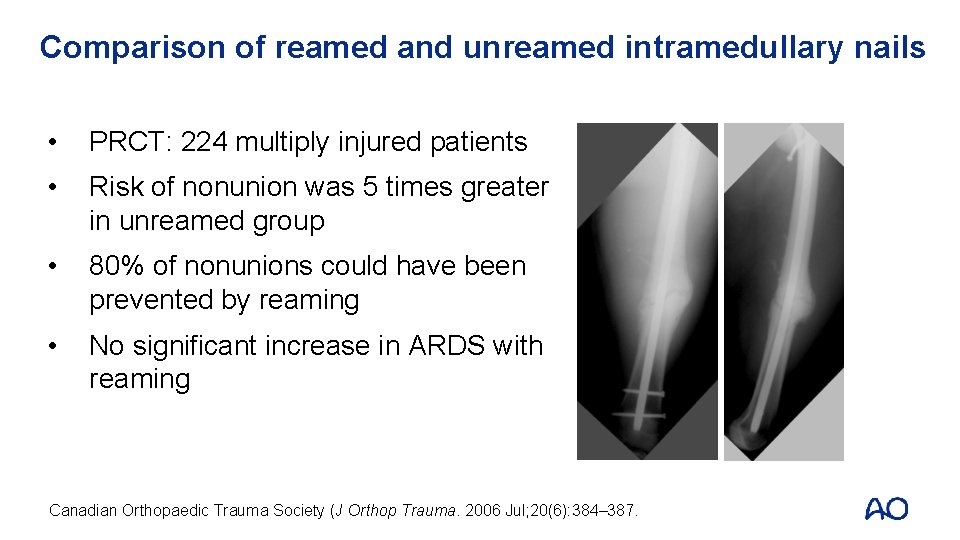
Comparison of reamed and unreamed intramedullary nails • PRCT: 224 multiply injured patients • Risk of nonunion was 5 times greater in unreamed group • 80% of nonunions could have been prevented by reaming • No significant increase in ARDS with reaming Canadian Orthopaedic Trauma Society (J Orthop Trauma. 2006 Jul; 20(6): 384– 387.
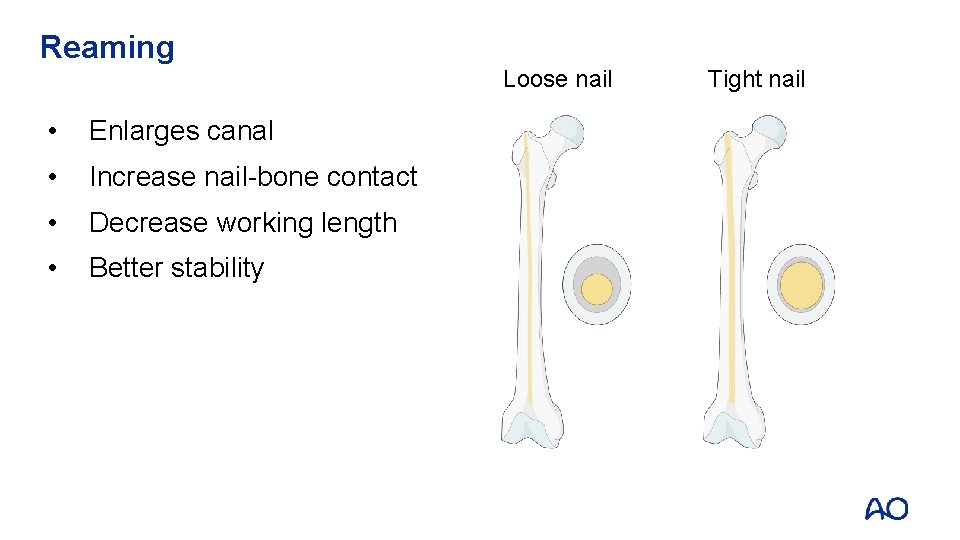
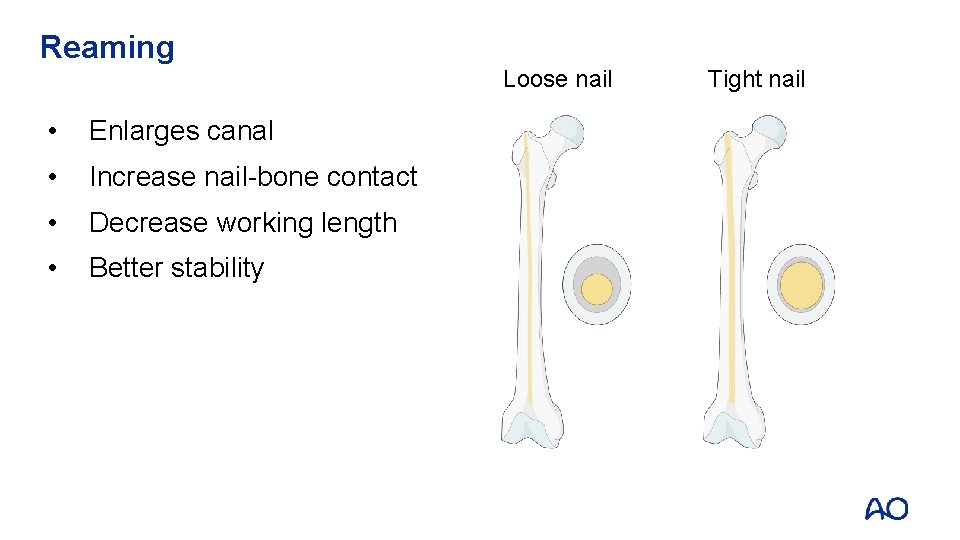
Reaming Loose nail • Enlarges canal • Increase nail-bone contact • Decrease working length • Better stability Tight nail
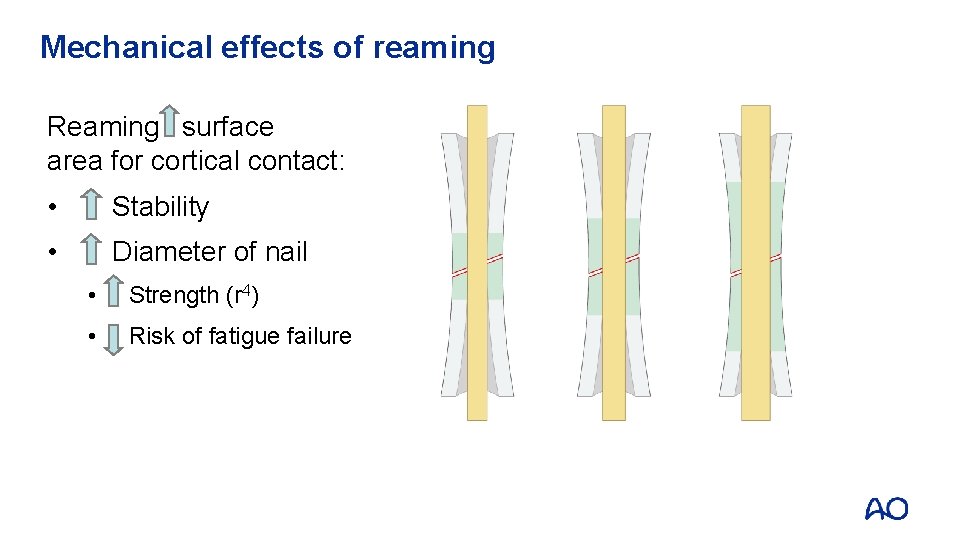
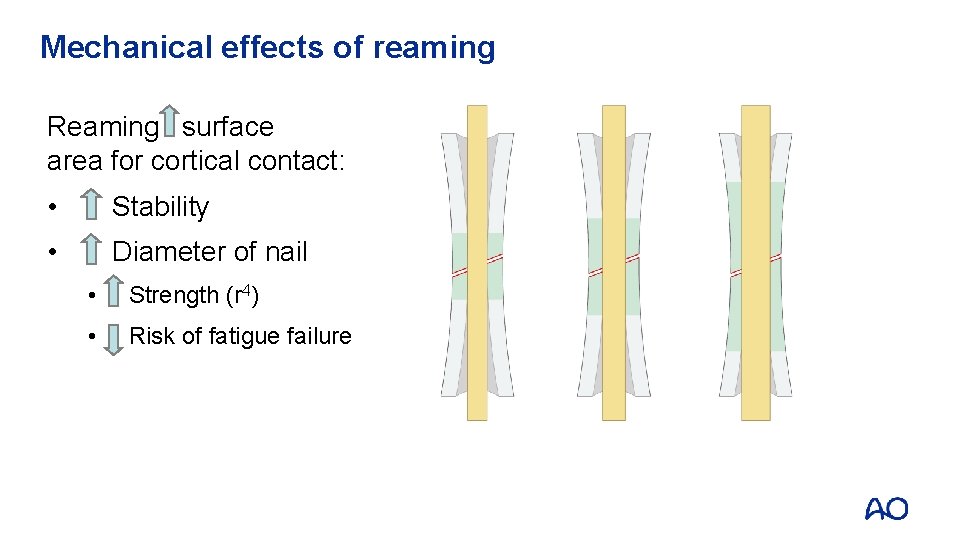
Mechanical effects of reaming Reaming surface area for cortical contact: • Stability • Diameter of nail • Strength (r 4) • Risk of fatigue failure
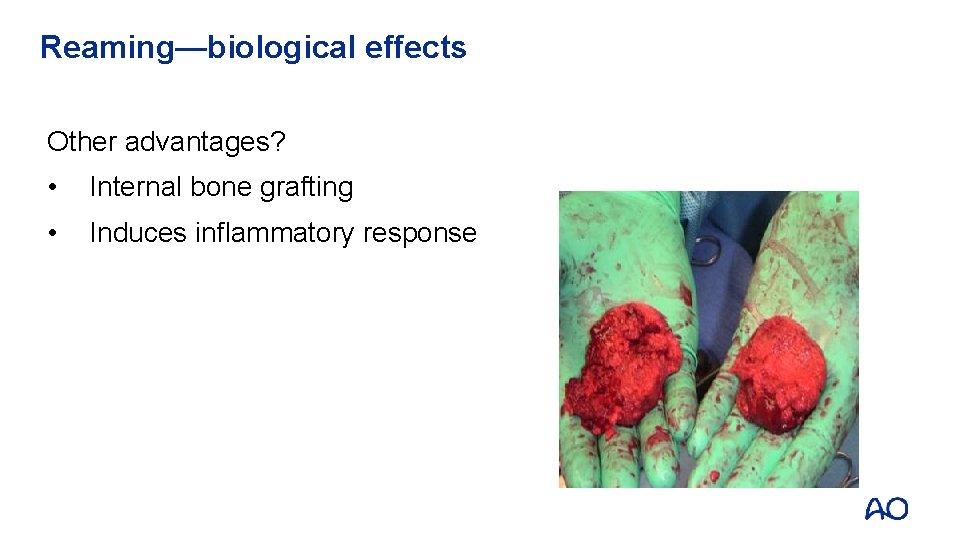
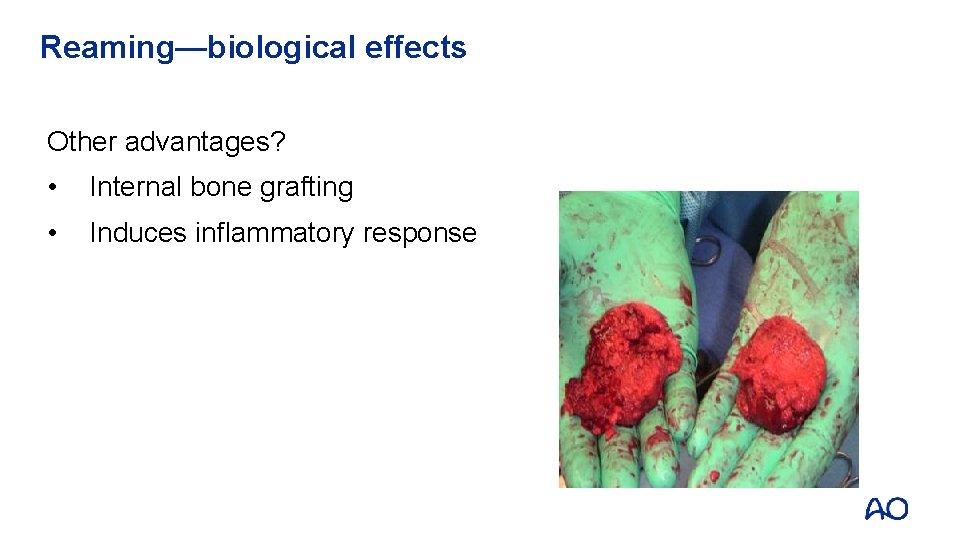
Reaming—biological effects Other advantages? • Internal bone grafting • Induces inflammatory response
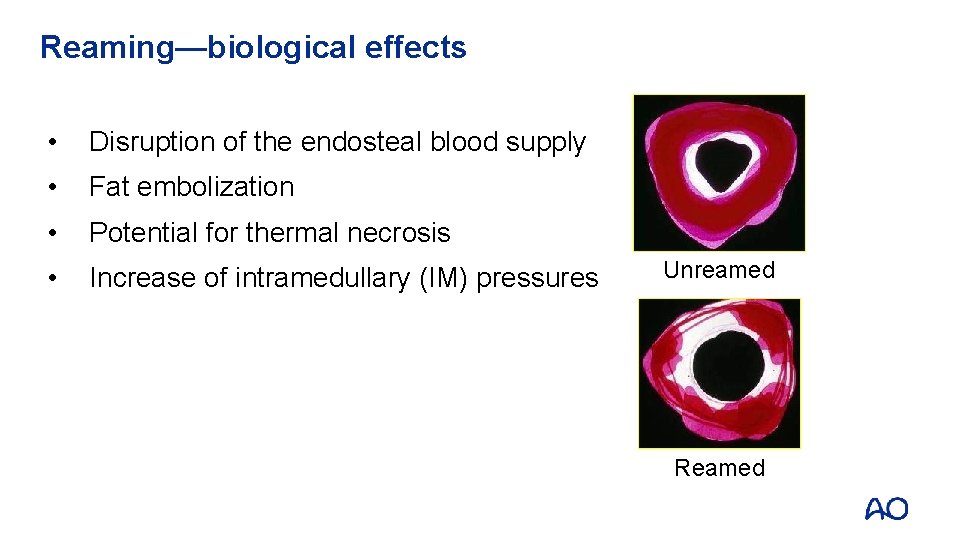
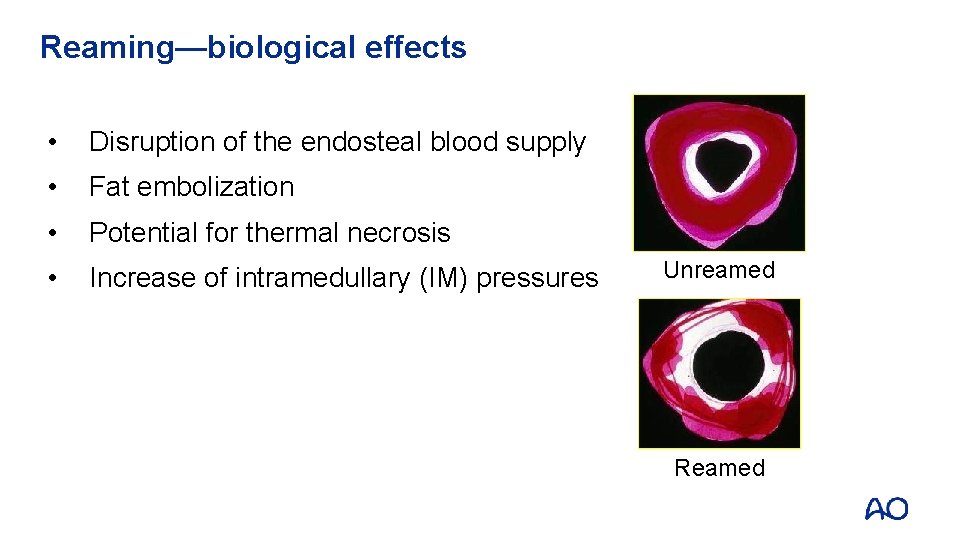
Reaming—biological effects • Disruption of the endosteal blood supply • Fat embolization • Potential for thermal necrosis • Increase of intramedullary (IM) pressures Unreamed Reamed
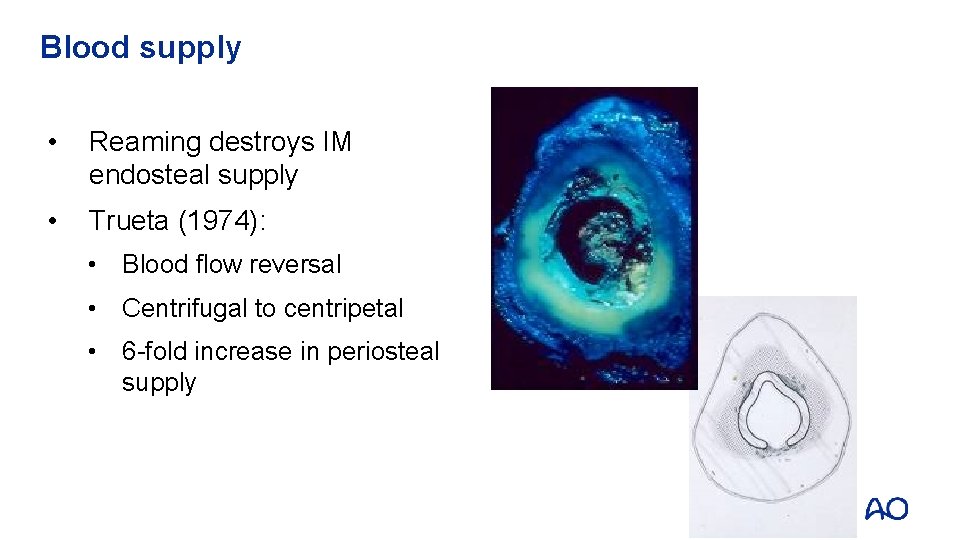
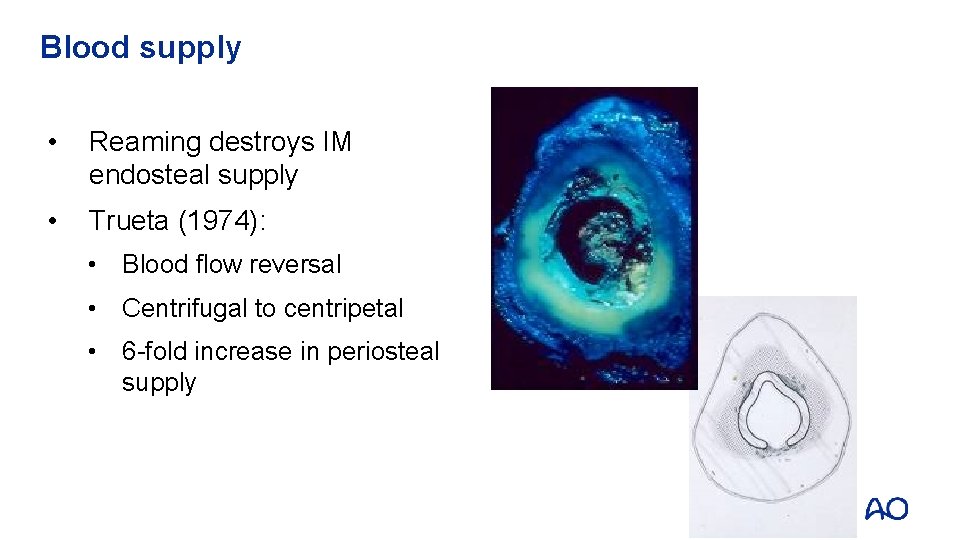
Blood supply • Reaming destroys IM endosteal supply • Trueta (1974): • Blood flow reversal • Centrifugal to centripetal • 6 -fold increase in periosteal supply
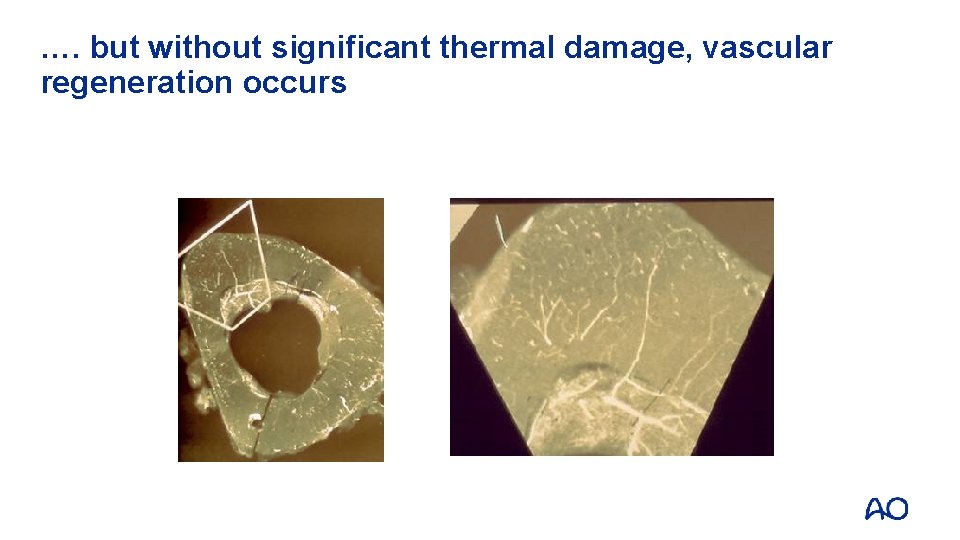
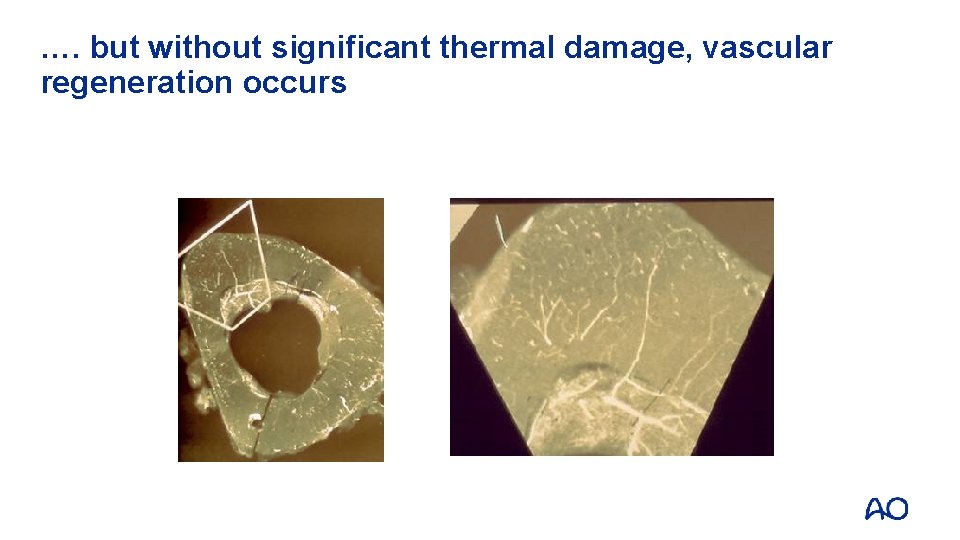
…. but without significant thermal damage, vascular regeneration occurs
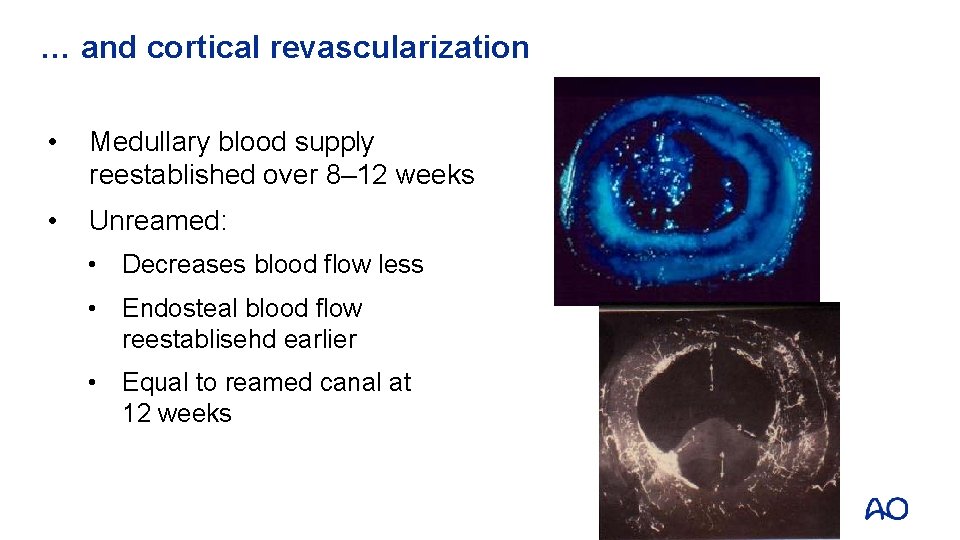
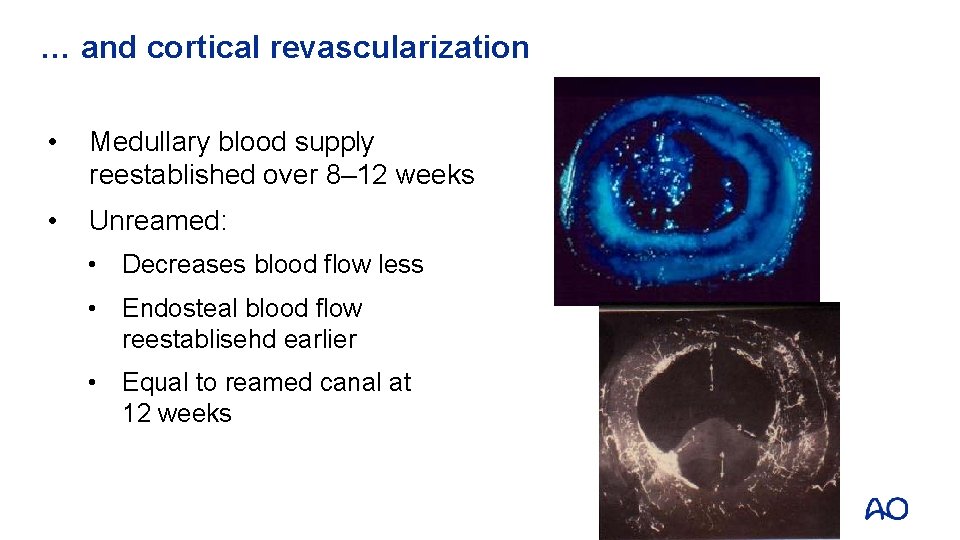
… and cortical revascularization • Medullary blood supply reestablished over 8– 12 weeks • Unreamed: • Decreases blood flow less • Endosteal blood flow reestablisehd earlier • Equal to reamed canal at 12 weeks
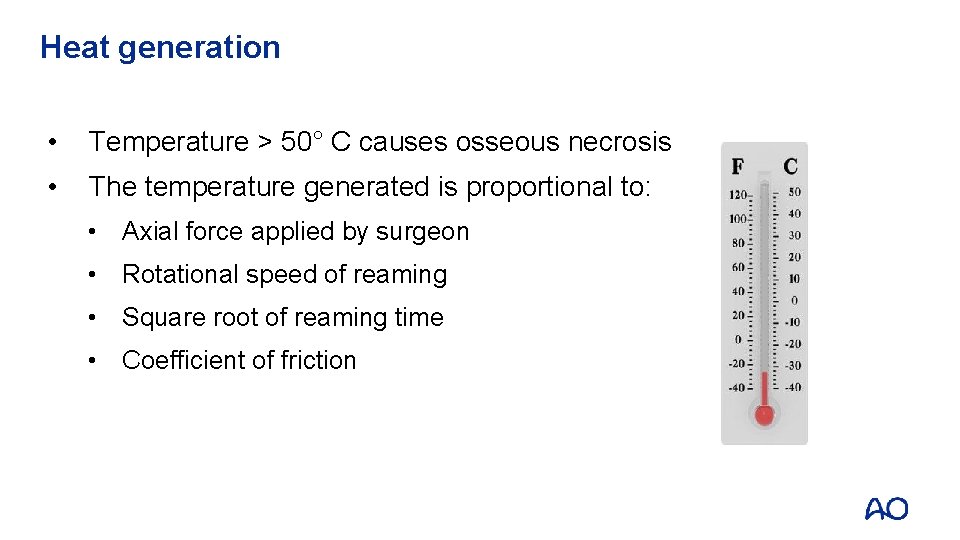
Heat generation • Temperature > 50° C causes osseous necrosis • The temperature generated is proportional to: • Axial force applied by surgeon • Rotational speed of reaming • Square root of reaming time • Coefficient of friction
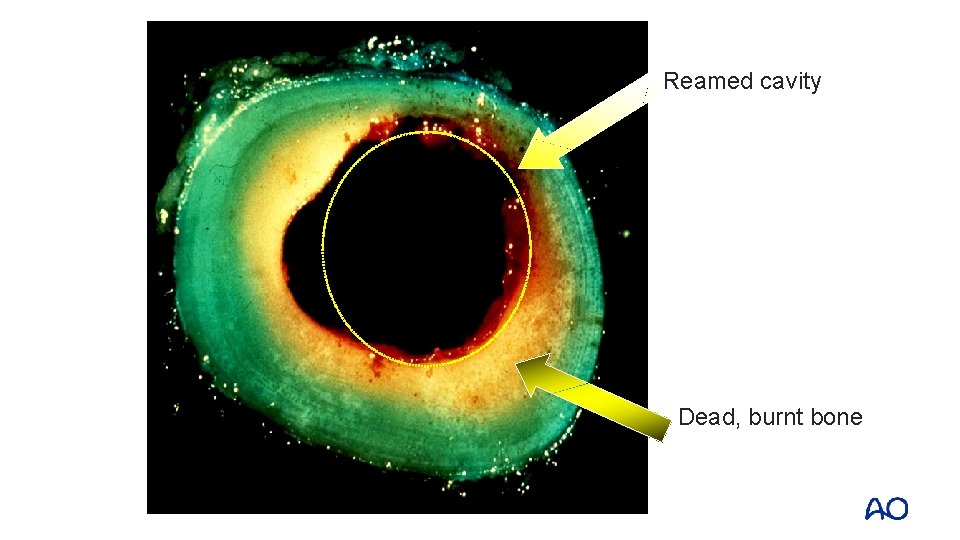
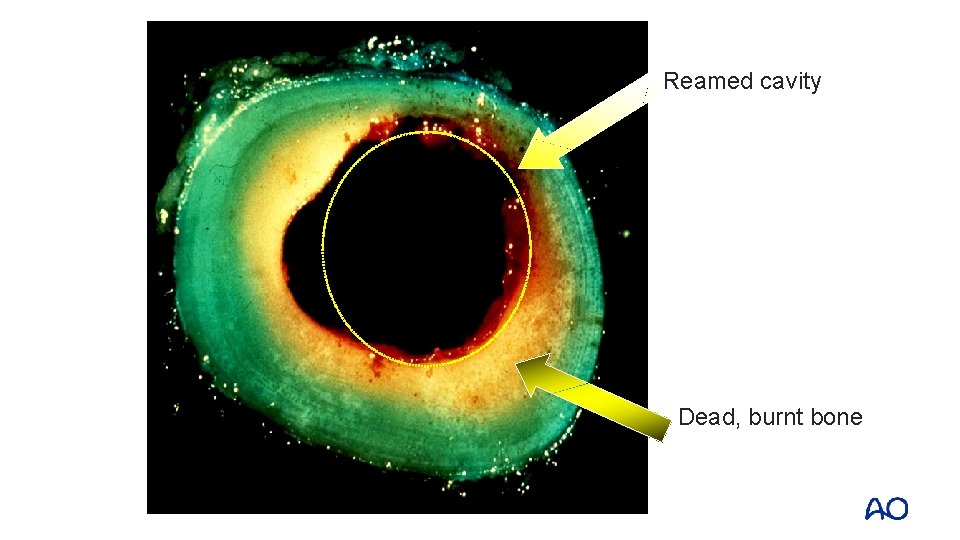
Reamed cavity Dead, burnt bone
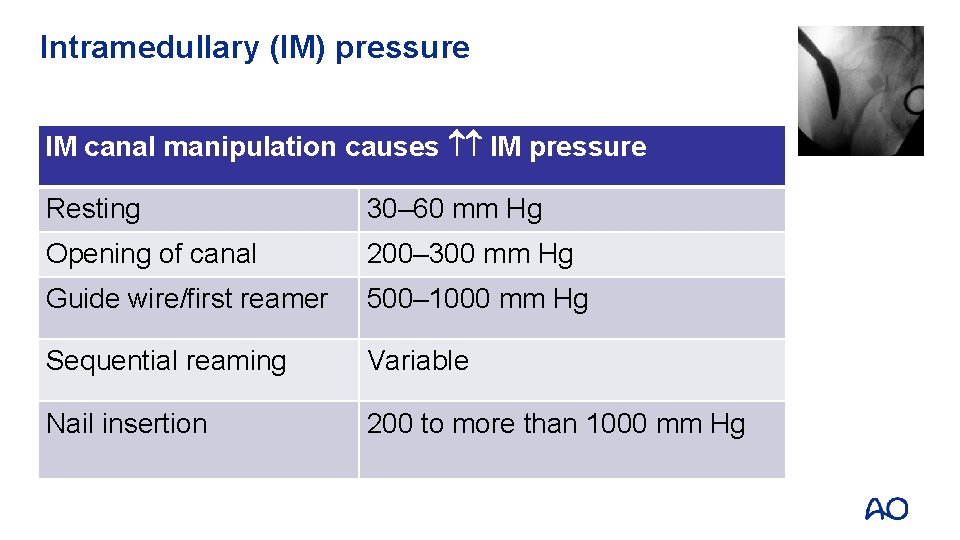
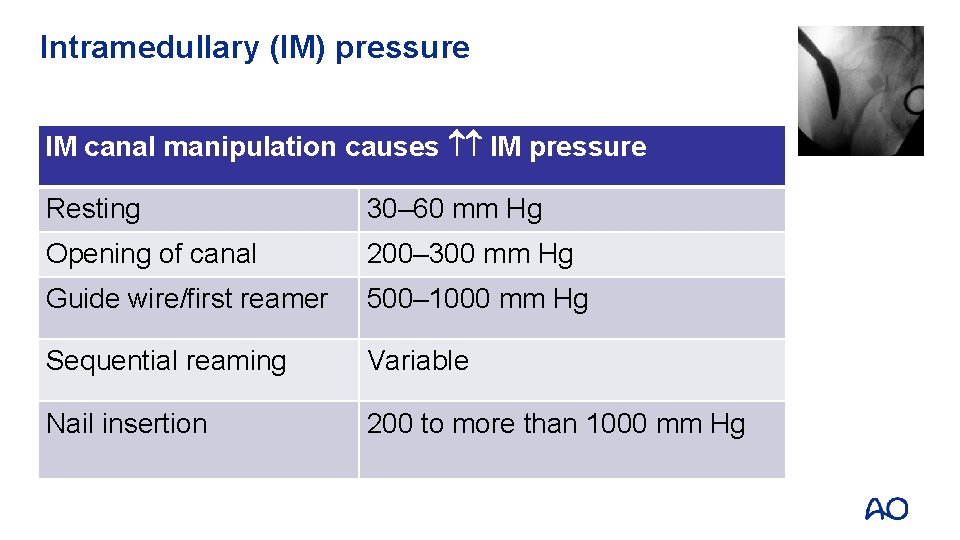
Intramedullary (IM) pressure IM canal manipulation causes IM pressure Resting 30– 60 mm Hg Opening of canal 200– 300 mm Hg Guide wire/first reamer 500– 1000 mm Hg Sequential reaming Variable Nail insertion 200 to more than 1000 mm Hg
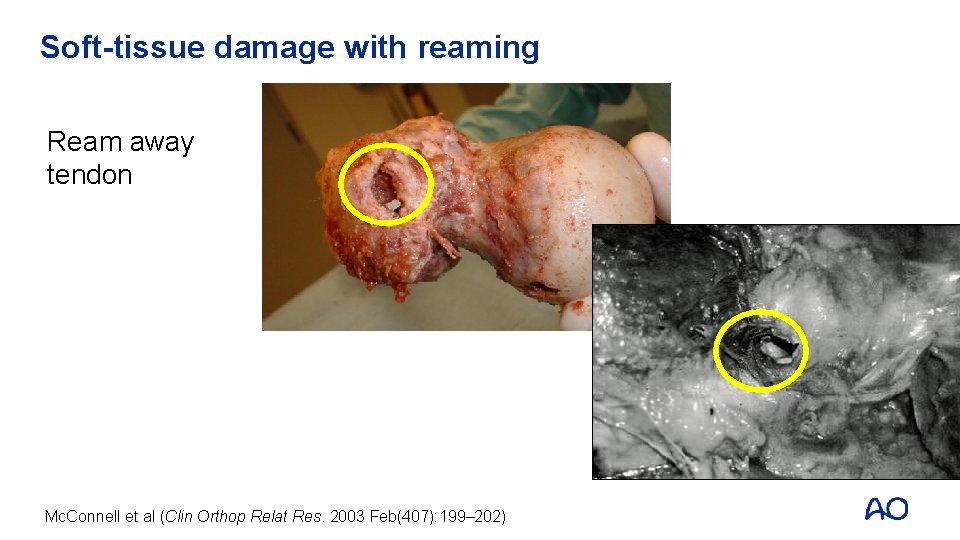
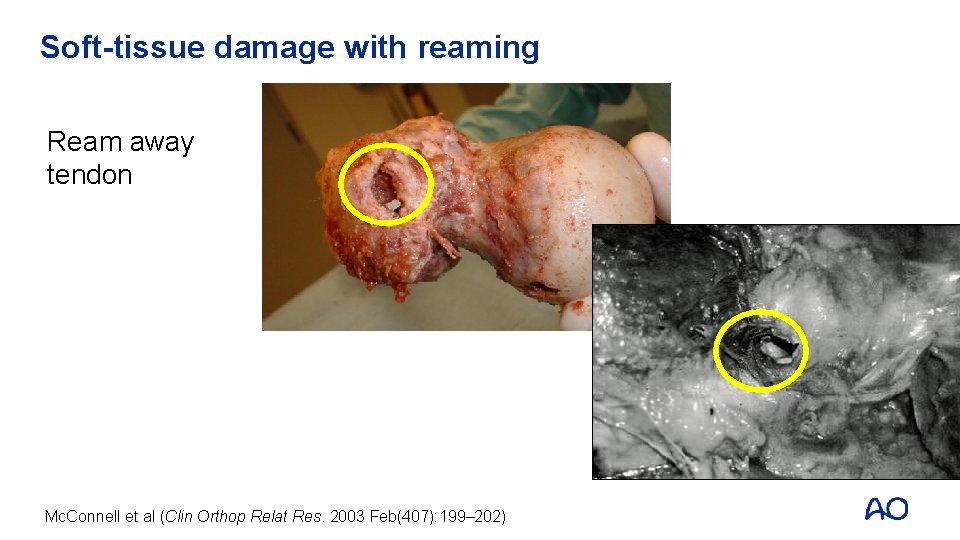
Soft-tissue damage with reaming Ream away tendon Mc. Connell et al (Clin Orthop Relat Res. 2003 Feb(407): 199– 202)
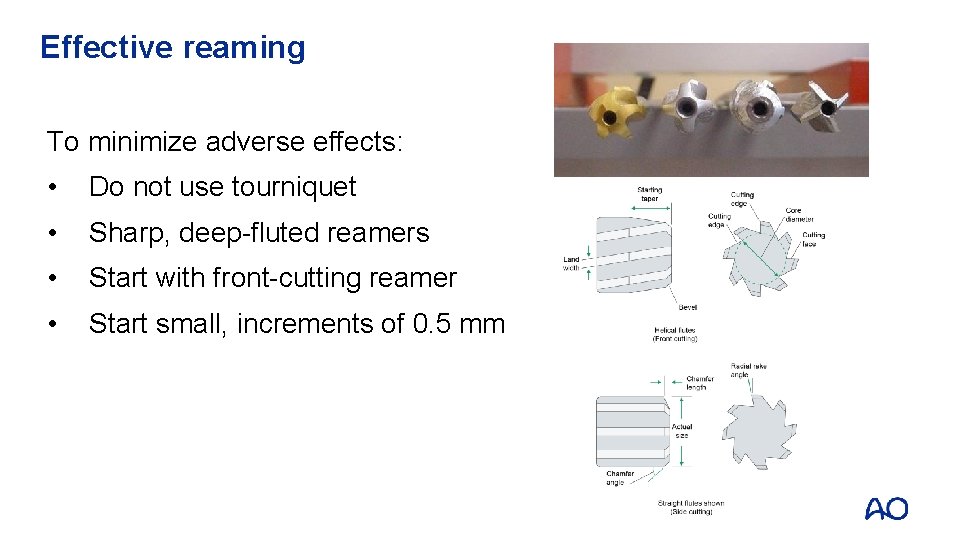
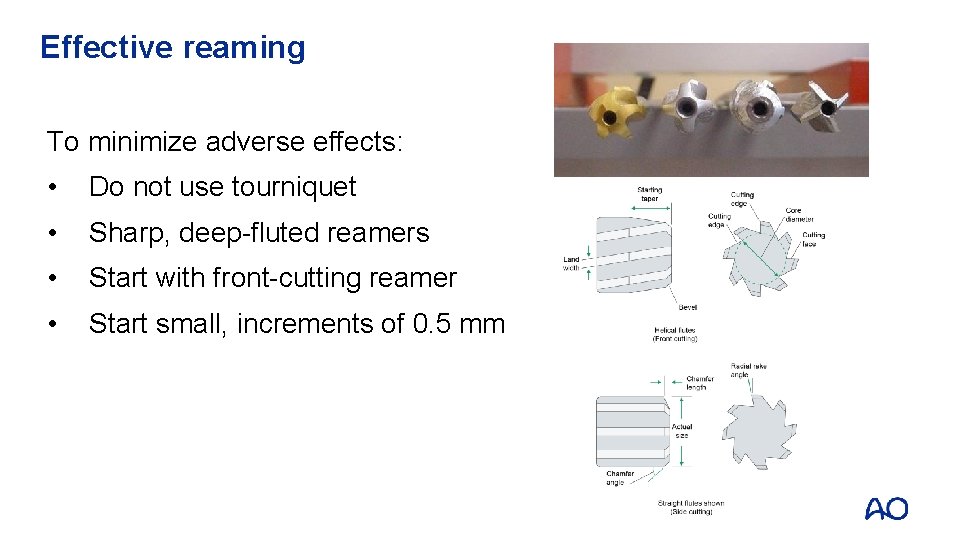
Effective reaming To minimize adverse effects: • Do not use tourniquet • Sharp, deep-fluted reamers • Start with front-cutting reamer • Start small, increments of 0. 5 mm
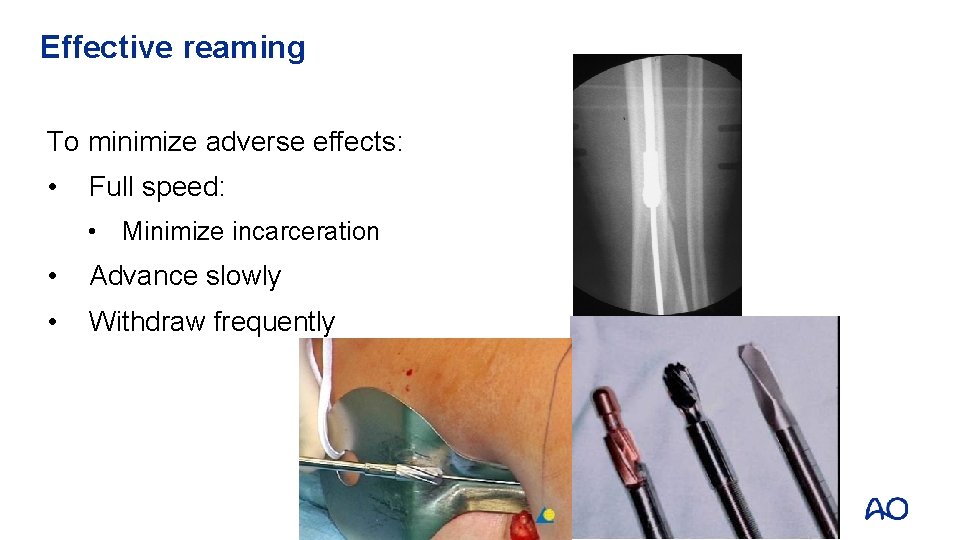
Effective reaming To minimize adverse effects: • Full speed: • Minimize incarceration • Advance slowly • Withdraw frequently
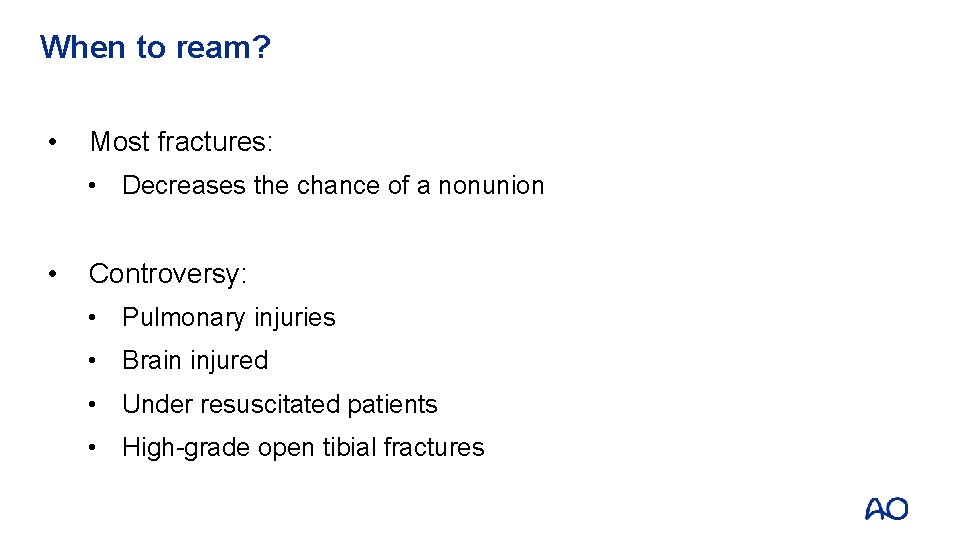
When to ream? • Most fractures: • Decreases the chance of a nonunion • Controversy: • Pulmonary injuries • Brain injured • Under resuscitated patients • High-grade open tibial fractures
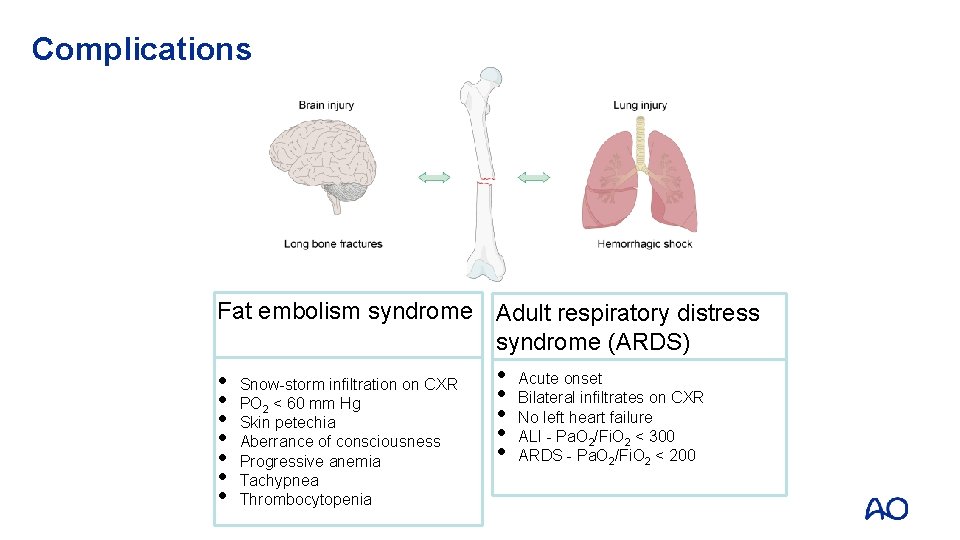
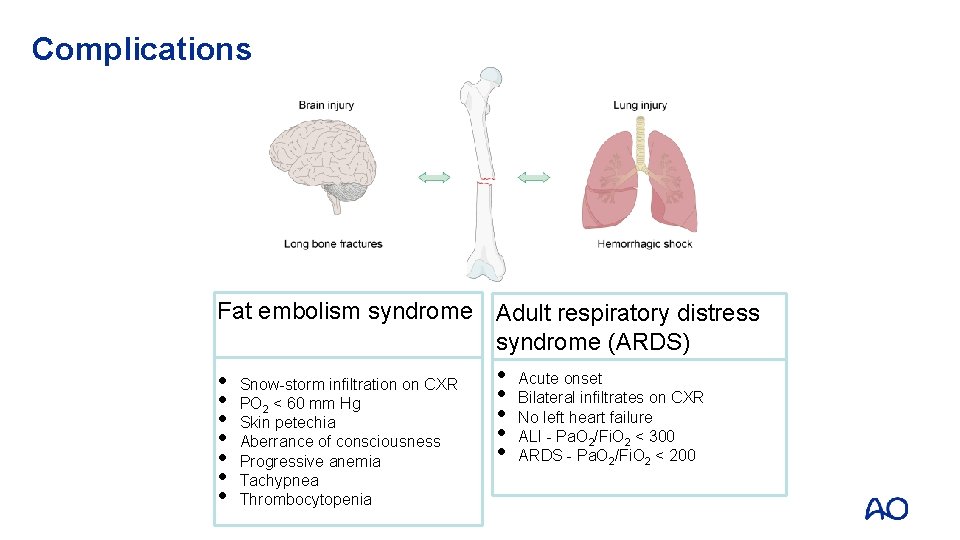
Complications Fat embolism syndrome Adult respiratory distress syndrome (ARDS) • • Snow-storm infiltration on CXR PO 2 < 60 mm Hg Skin petechia Aberrance of consciousness Progressive anemia Tachypnea Thrombocytopenia • • • Acute onset Bilateral infiltrates on CXR No left heart failure ALI - Pa. O 2/Fi. O 2 < 300 ARDS - Pa. O 2/Fi. O 2 < 200
Animal studies • Intramedullary nailing does adversely affect pulmonary physiology and increases inflammatory mediator load • Does nailing have an adverse effect on clinical outcome?
Conclusions from clinical literature • Infection—open and closed fractures: • No difference between unreamed versus reamed nails • Reamed nails better than unreamed nails: • Time to union • Nonunion rates • Reoperation rates • Thoracic injury is the major determinant of pulmonary complications, NOT the use of a reamed IM nail • In patients with severe head injuries, reamed nailing did not worsen outcomes
Role for unreamed nailing • Small canals • Unstable polytrauma patients: • Damage control nailing (Higgins, 2007) Higgins et al (J Orthop Trauma. 2007 Aug; 21(7): 477– 481; dicussion 481– 474)
Take-home messages • Reaming has a biological price, know how to minimize it • Good evidence to support reaming in most femoral and tibial fractures • Be wary in unstable, underresuscitated polytrauma patients • Limited role for unreamed nails