INTRACRANIAL PRESSURE Intracranial Pressure Refers to the pressure


- Slides: 24

INTRACRANIAL PRESSURE
Intracranial Pressure • Refers to the pressure contained within the cranial cavity. • The normal range is between 0 to 15 mm. Hg. • ICP over 20 mm/Hg is considered elevated ICP, also known as intracranial hypertension. • The management team becomes concerned whenever a patient’s ICP is over 15 mm/Hg, but is especially concerned when it reaches levels of intracranial hypertension.
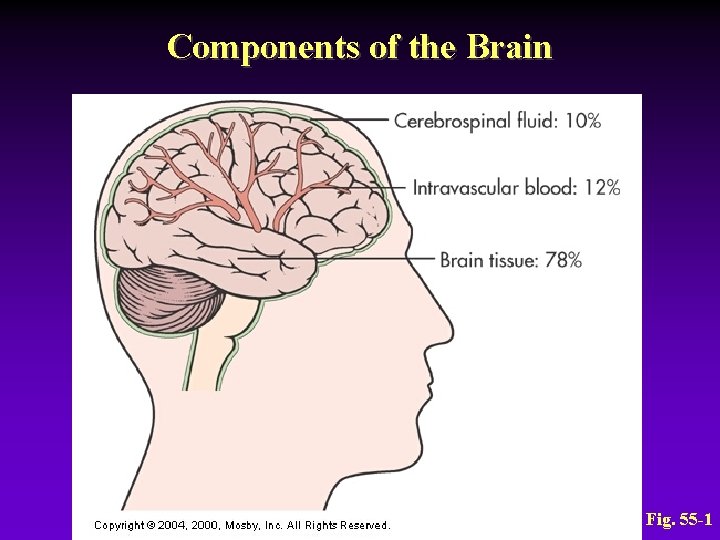
Intracranial Pressure • Skull has three essential components: - Brain tissue = 78% - Blood = 12% - Cerebrospinal fluid (CSF) = 10% • Any increase in any of these tissues causes increased ICP
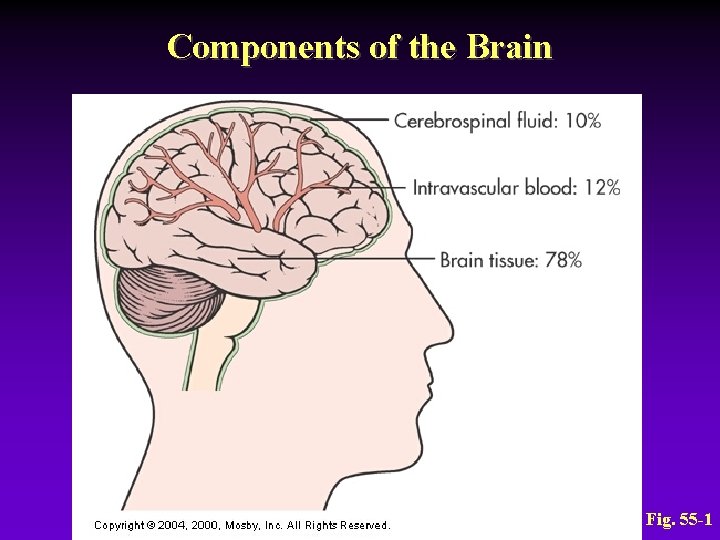
Components of the Brain Fig. 55 -1
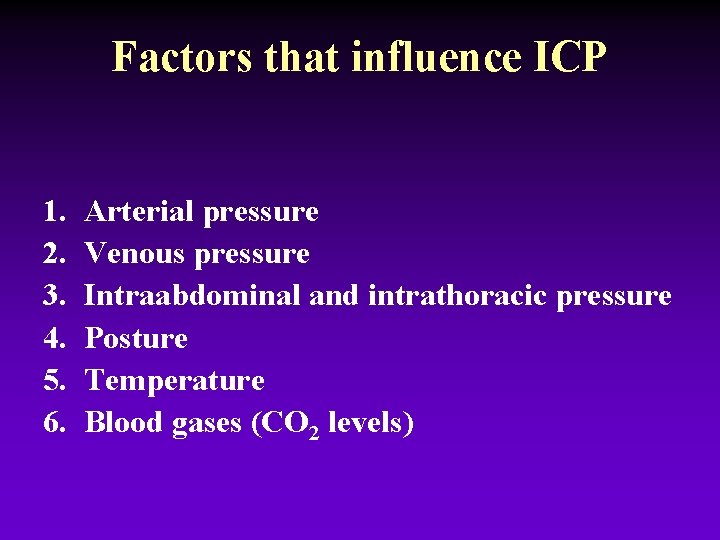
Factors that influence ICP 1. 2. 3. 4. 5. 6. Arterial pressure Venous pressure Intraabdominal and intrathoracic pressure Posture Temperature Blood gases (CO 2 levels)
Intracranial Pressure • The degree to which these factors ICP depends on the ability of the brain to accommodate to the changes
Regulation and Maintenance for ICP – If the volume in any one of the components (brain tissue, blood, and CSF) – increases within the cranial vault and the volume from another component is displaced, the total intracranial volume will not change
Intracranial Pressure Regulation and Maintenance • Normal compensatory adaptations – Alteration of CSF absorption or production – Shunting of CSF into spinal subarachnoid space – Shunting of venous blood out of the skull
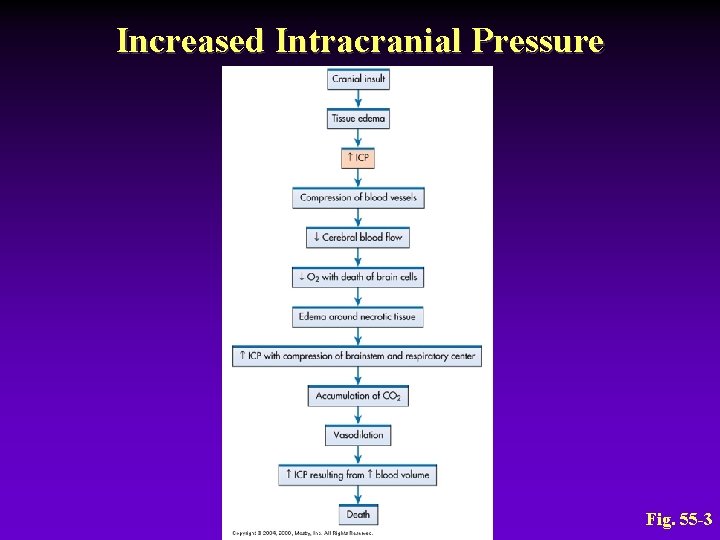
Mechanisms of Increased ICP • Causes – Mass lesion – Cerebral edema – Head injury – Brain inflammation – Metabolic insult
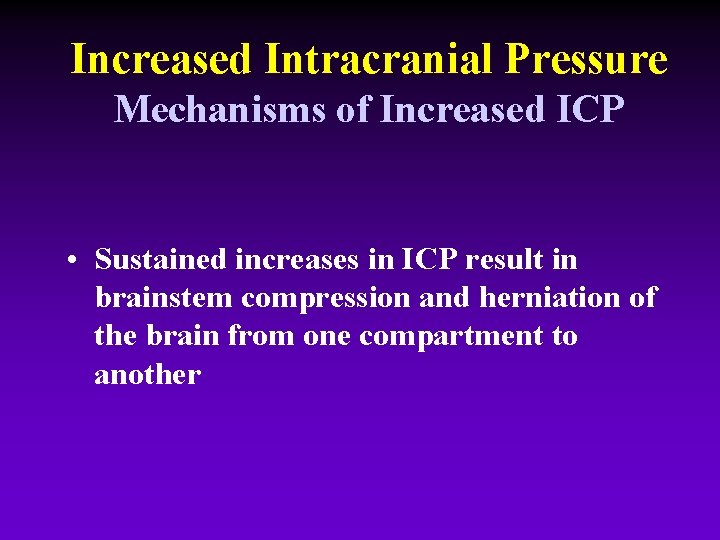
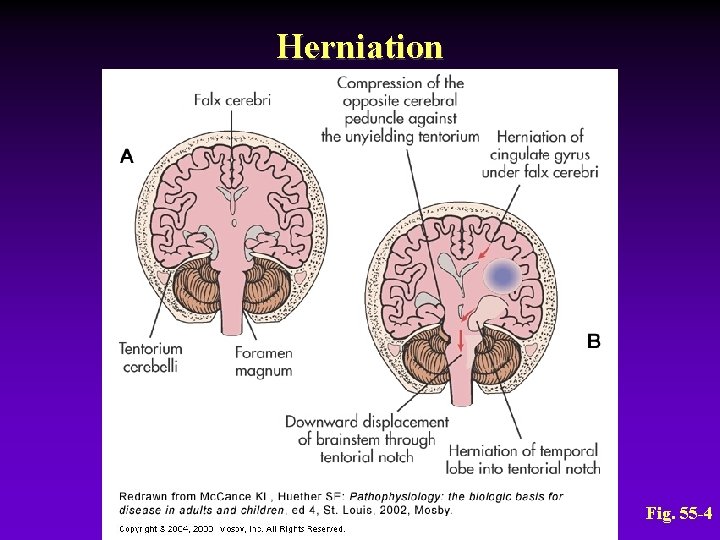
Increased Intracranial Pressure Mechanisms of Increased ICP • Sustained increases in ICP result in brainstem compression and herniation of the brain from one compartment to another
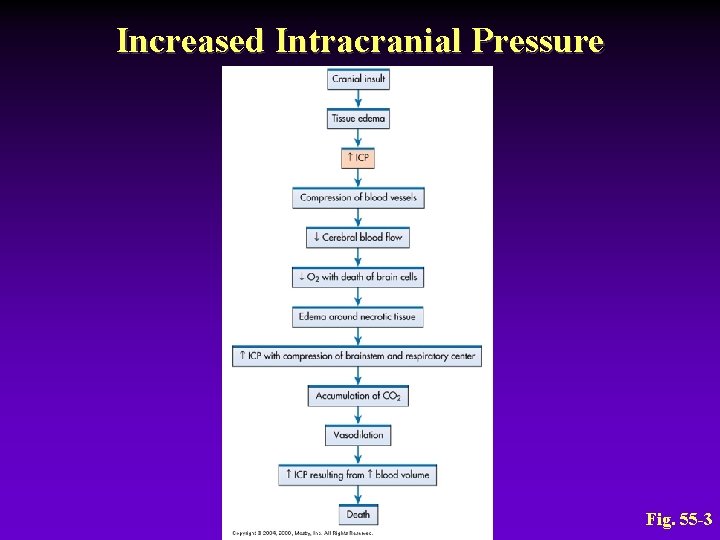
Increased Intracranial Pressure Fig. 55 -3
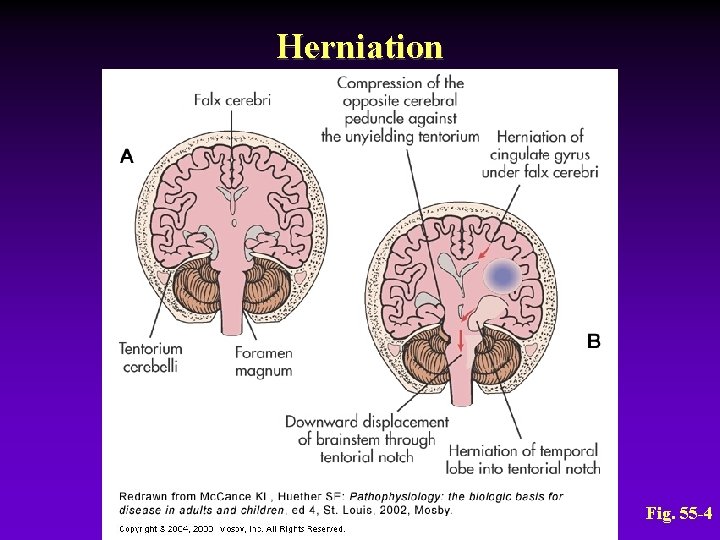
Herniation Fig. 55 -4
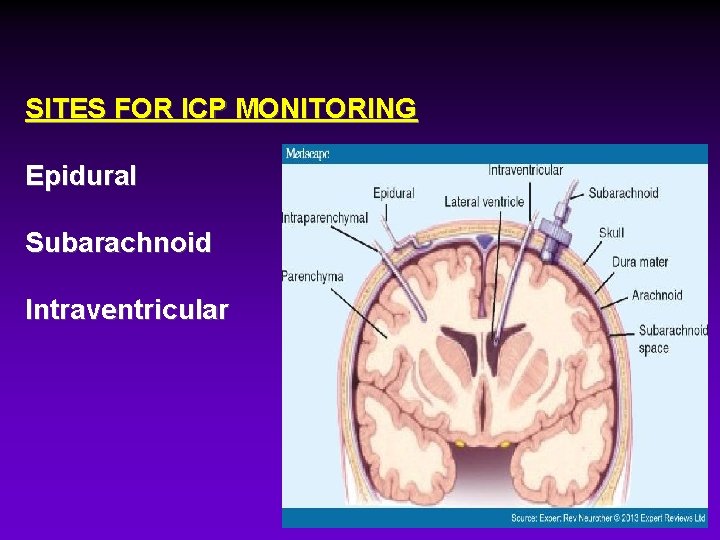
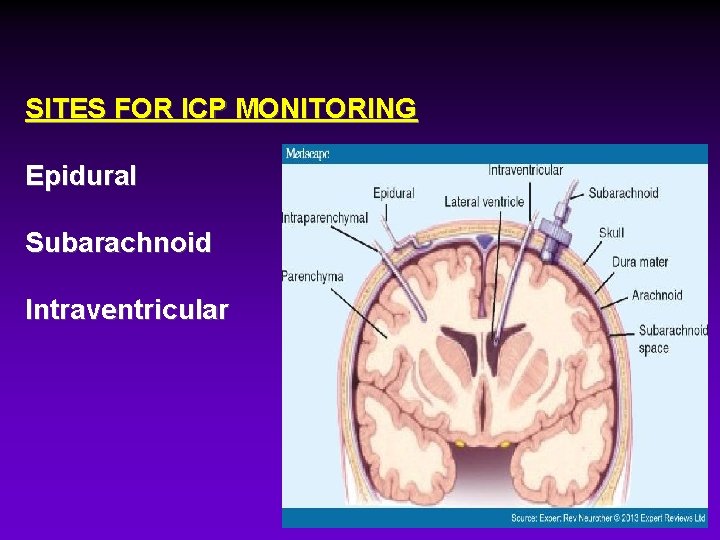
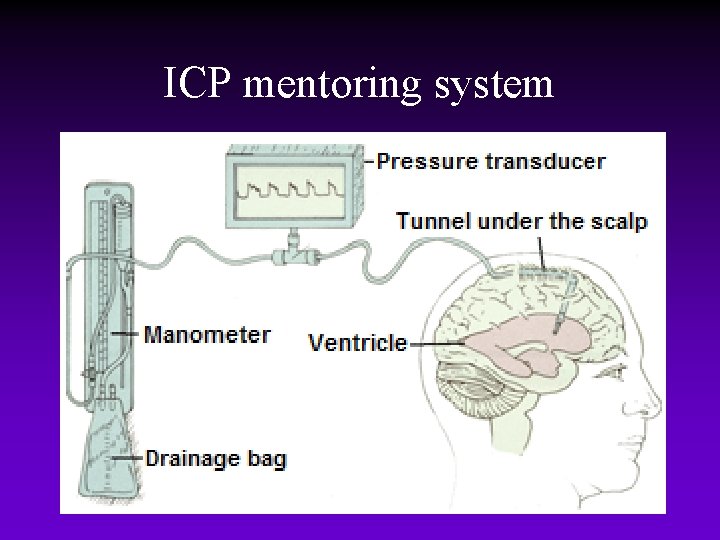
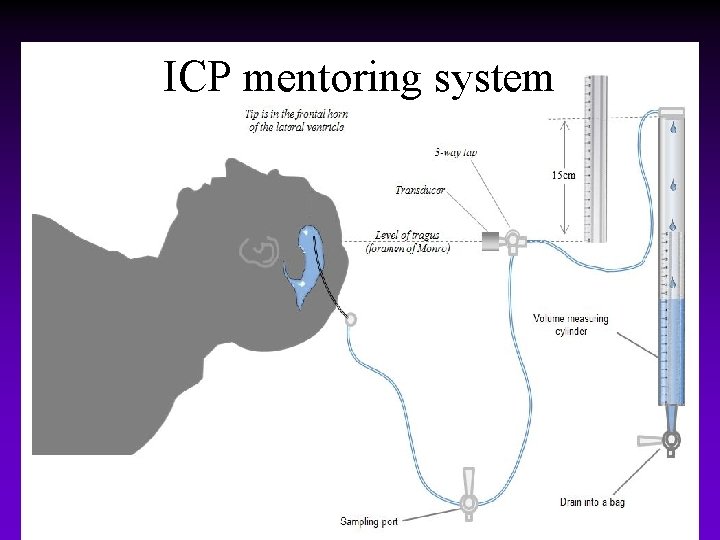
SITES FOR ICP MONITORING Epidural Subarachnoid Intraventricular
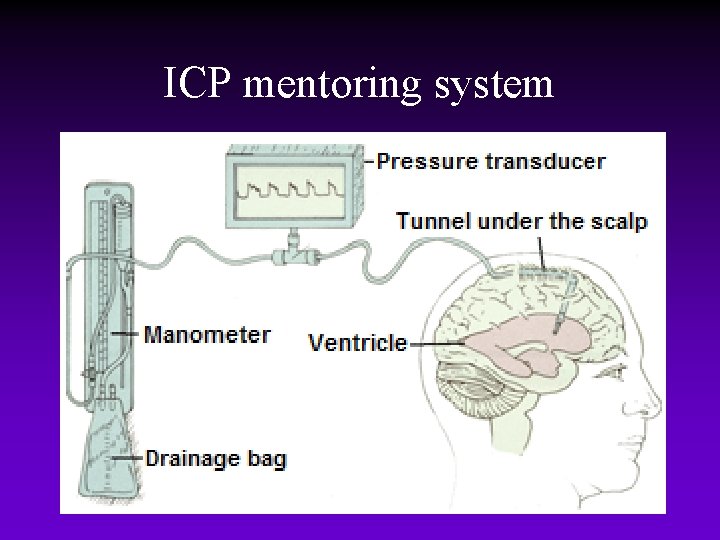
ICP mentoring system
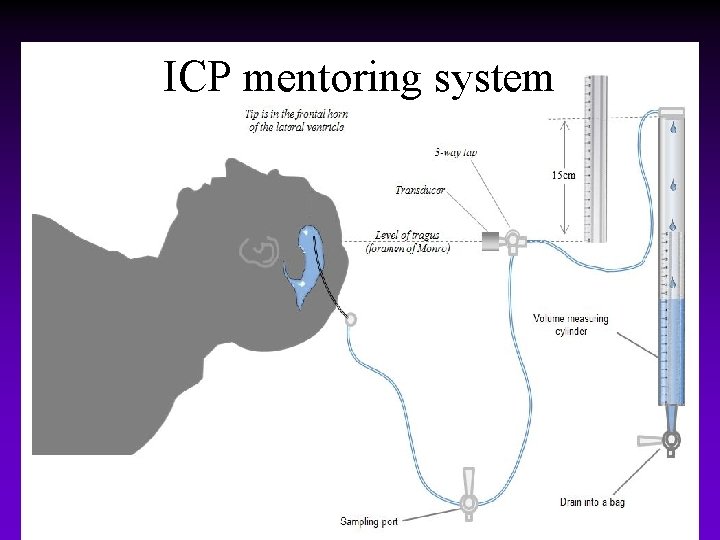
ICP mentoring system
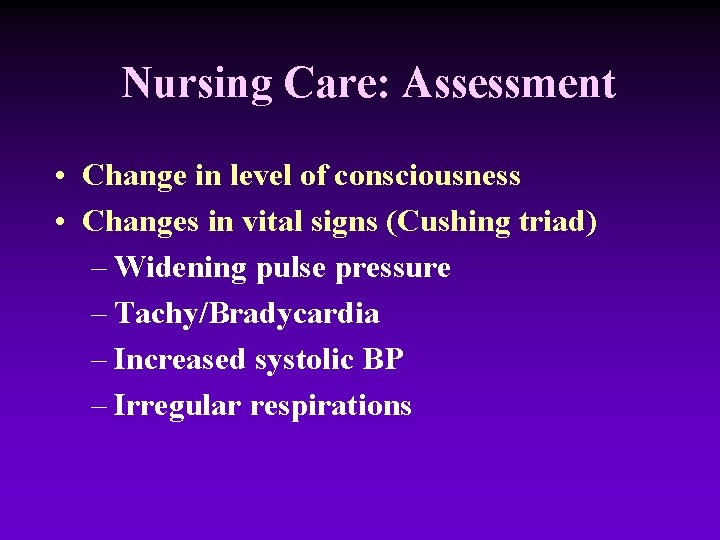
Nursing Care: Assessment • Change in level of consciousness • Changes in vital signs (Cushing triad) – Widening pulse pressure – Tachy/Bradycardia – Increased systolic BP – Irregular respirations
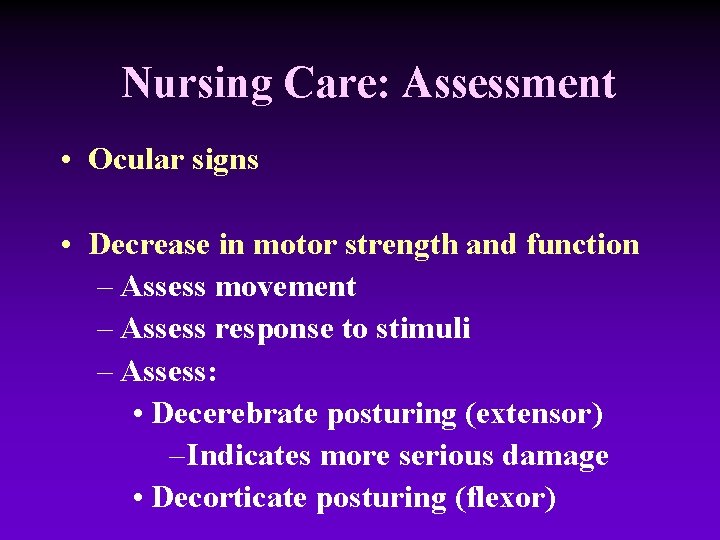
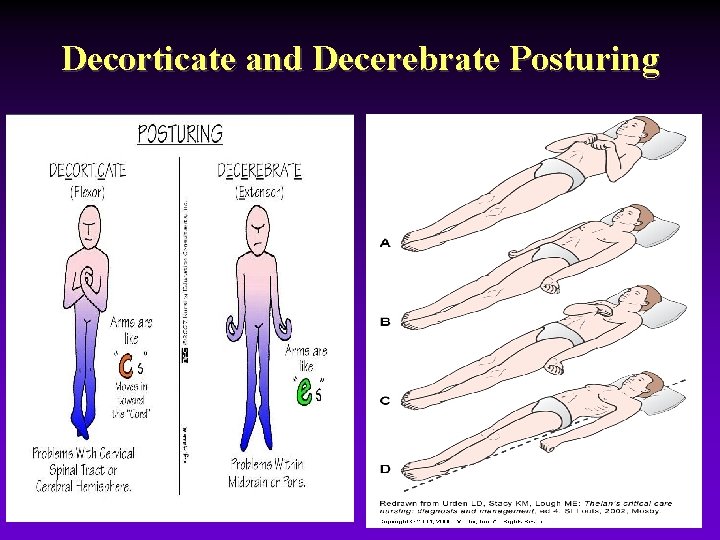
Nursing Care: Assessment • Ocular signs • Decrease in motor strength and function – Assess movement – Assess response to stimuli – Assess: • Decerebrate posturing (extensor) – Indicates more serious damage • Decorticate posturing (flexor)
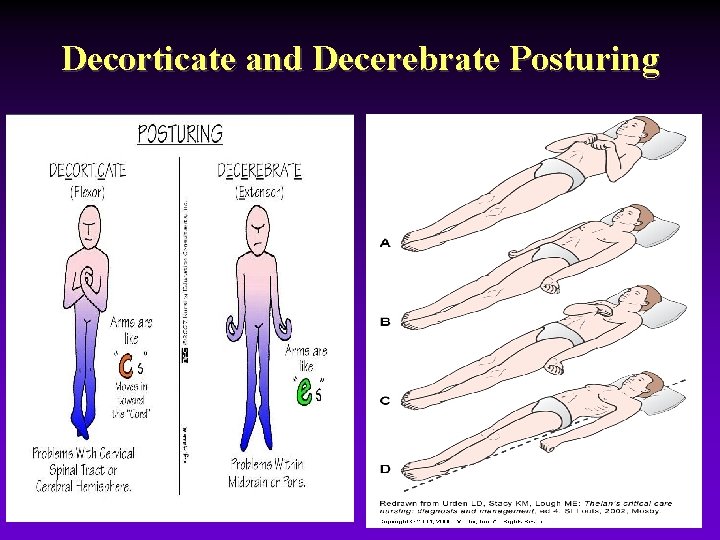
Decorticate and Decerebrate Posturing
Nursing Care: Assessment • Headache – Often continuous and worse in the morning • Vomiting – Not preceded by nausea – Projectile
Increased Intracranial Pressure Collaborative Care • Hyperventilation therapy: suctioning → hyperventilate with 100% oxygen • Adequate oxygenation – Pa. O 2 maintenance at 100 mm Hg or greater – ABG analysis guides the oxygen therapy – May require mechanical ventilator

Increased Intracranial Pressure Collaborative Care • Drug therapy – Mannitol – Loop diuretics – Corticosteroids – Barbiturates – Antiseizure drugs
Increased Intracranial Pressure Collaborative Care • Nutritional therapy – Patient is in hypermetabolic and hypercatabolic state – Need for glucose – Keep patient normovolemic • IV 0. 45% or 0. 9% sodium chloride
Increased Intracranial Pressure Nursing Management Overall goals: • ICP WNL • Maintain patent airway • Normal fluid and electrolyte balance • No complications secondary to immobility • Respiratory function • Fluid and electrolyte balance
Increased Intracranial Pressure Nursing Management Overall goals (cont’d) • Body position maintained in head-up position: elevate HOB 30° • Protection from injury: positioning/turning • Pain control • Psychological considerations