Intracranial Pressure ICP Megan Mc Clintock MS RN
- Slides: 14
Intracranial Pressure (ICP) Megan Mc. Clintock, MS, RN 11/4/11
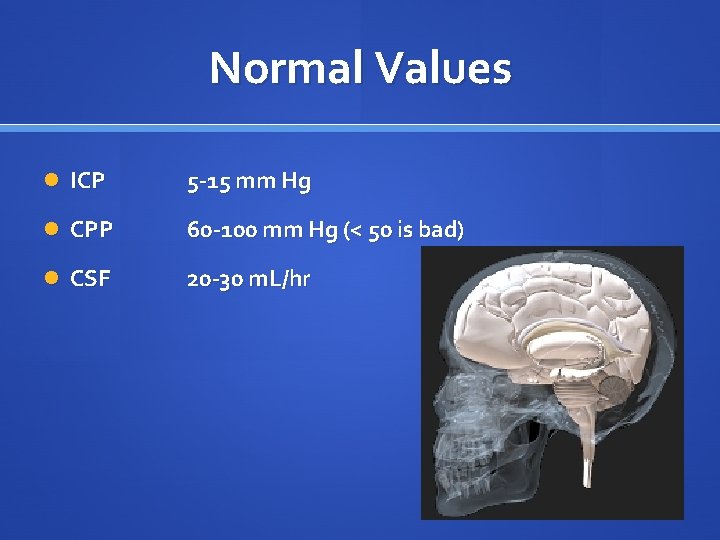
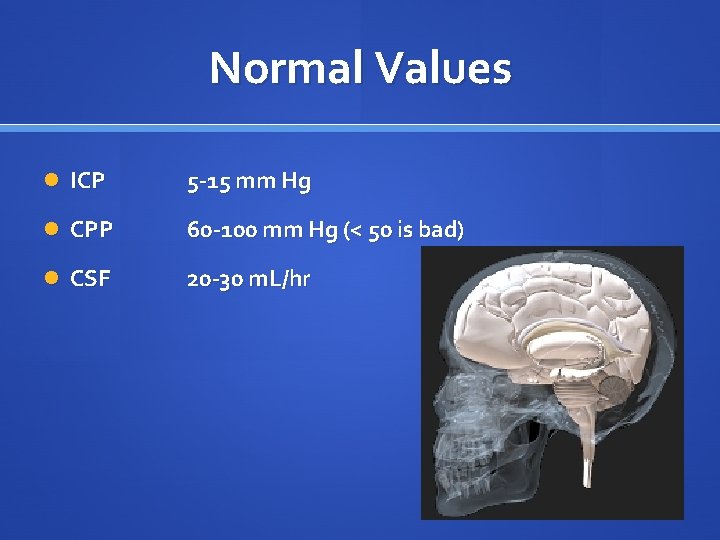
Normal Values ICP 5 -15 mm Hg CPP 60 -100 mm Hg (< 50 is bad) CSF 20 -30 m. L/hr
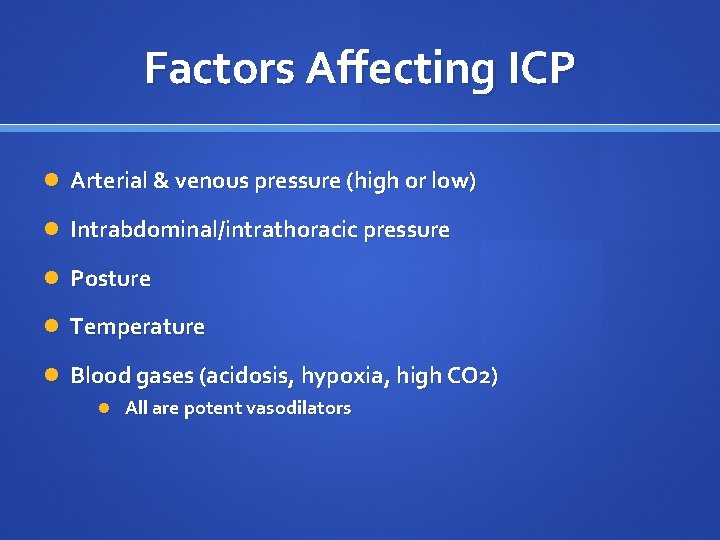
Factors Affecting ICP Arterial & venous pressure (high or low) Intrabdominal/intrathoracic pressure Posture Temperature Blood gases (acidosis, hypoxia, high CO 2) All are potent vasodilators
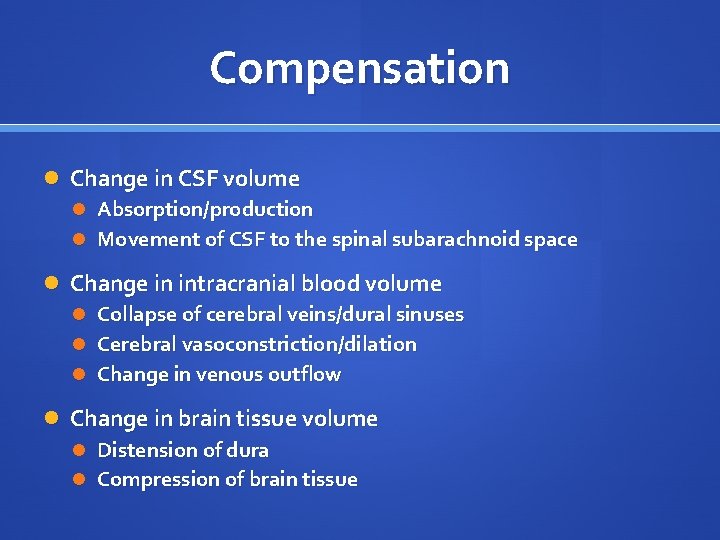
Compensation Change in CSF volume Absorption/production Movement of CSF to the spinal subarachnoid space Change in intracranial blood volume Collapse of cerebral veins/dural sinuses Cerebral vasoconstriction/dilation Change in venous outflow Change in brain tissue volume Distension of dura Compression of brain tissue
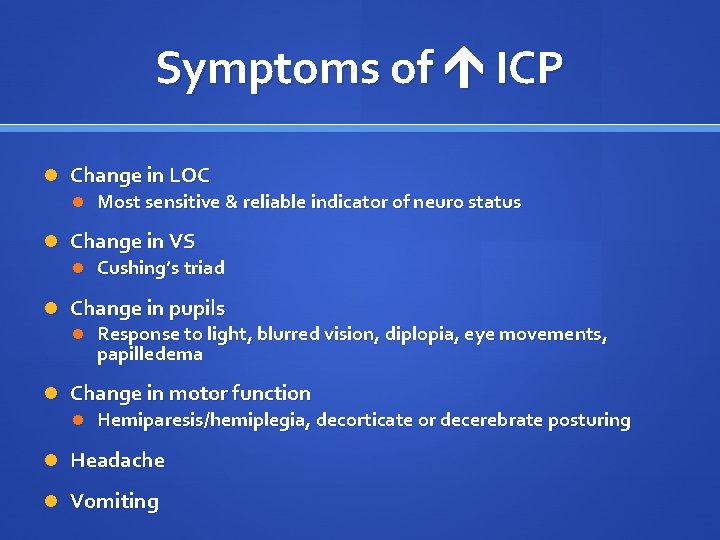
Symptoms of ICP Change in LOC Most sensitive & reliable indicator of neuro status Change in VS Cushing’s triad Change in pupils Response to light, blurred vision, diplopia, eye movements, papilledema Change in motor function Hemiparesis/hemiplegia, decorticate or decerebrate posturing Headache Vomiting
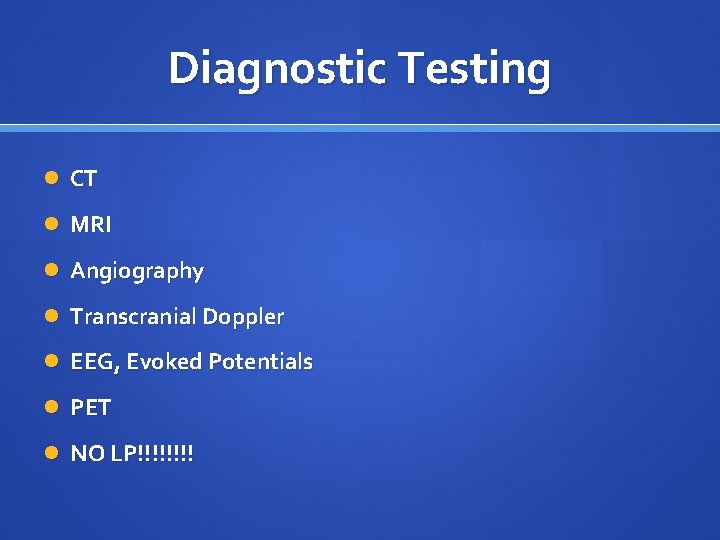
Diagnostic Testing CT MRI Angiography Transcranial Doppler EEG, Evoked Potentials PET NO LP!!!!
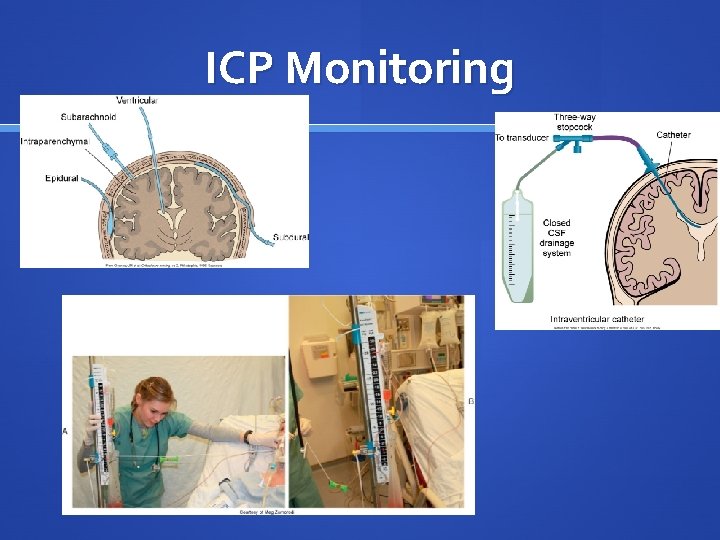
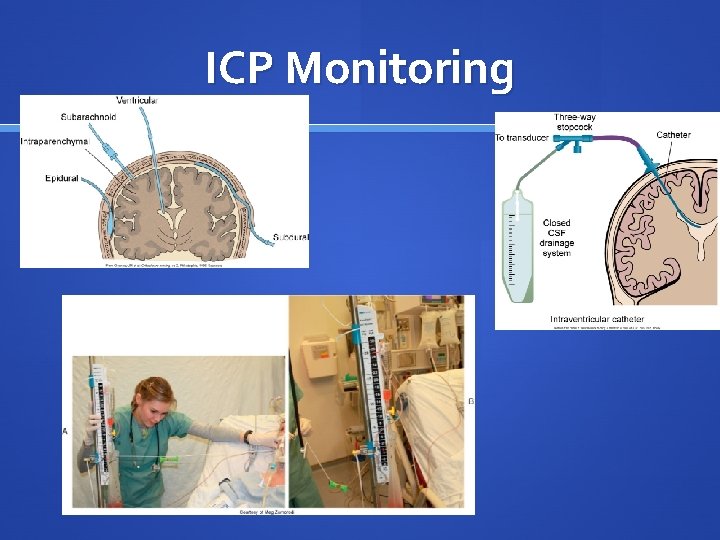
ICP Monitoring
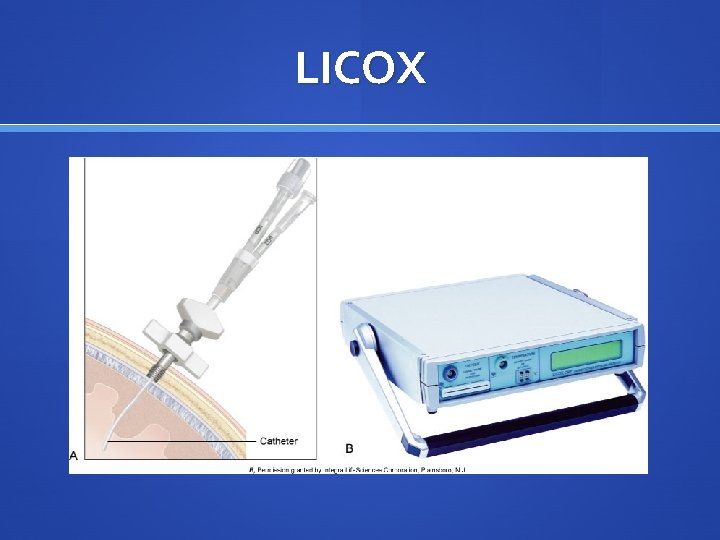
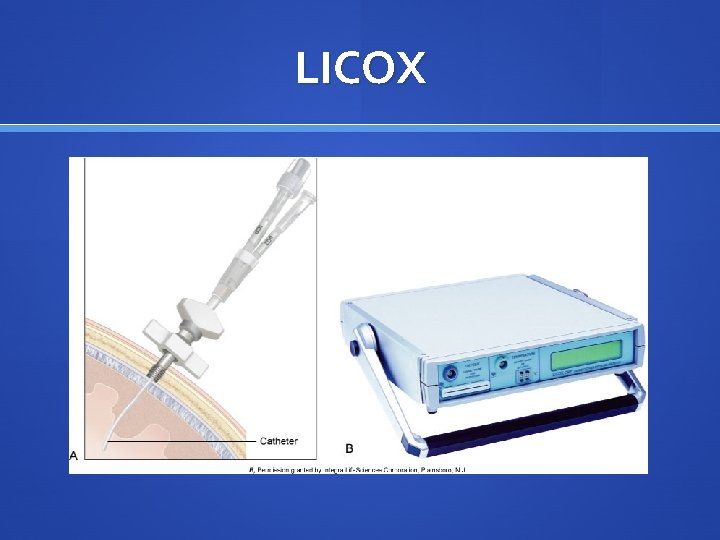
LICOX
Assessment Glasgow Coma Scale Pupils Cranial Nerves Eye movement Motor strength Vital signs (including respiratory pattern - pg 1435)
Treatment CSF drain, ICP monitoring ET tube/trach to keep Pa. O 2 at 100, Pa. CO 2 30 -35 Surgical removal of mass Hemicraniectomy Only light sedation (ie. Versed, Ativan) Be careful with drugs that alter the neuro state Rapid-acting opioids (Morphine, Fentanyl) are best Propofol is good (rapid-acting, short half-life) Avoid benzodiazepines
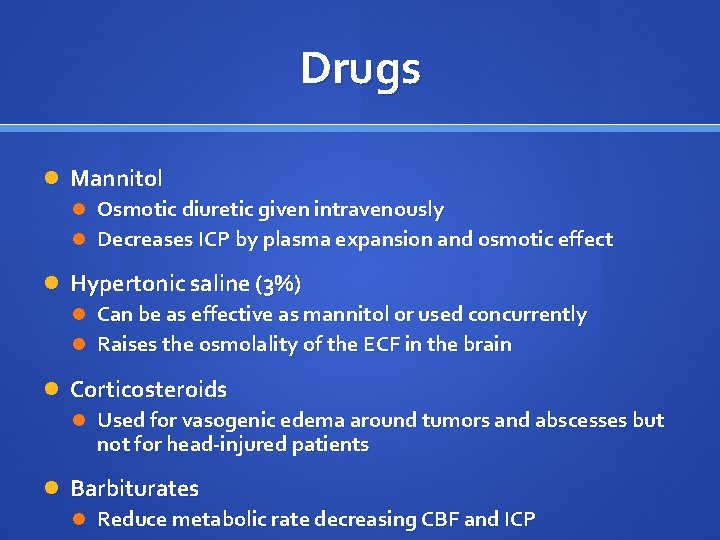
Drugs Mannitol Osmotic diuretic given intravenously Decreases ICP by plasma expansion and osmotic effect Hypertonic saline (3%) Can be as effective as mannitol or used concurrently Raises the osmolality of the ECF in the brain Corticosteroids Used for vasogenic edema around tumors and abscesses but not for head-injured patients Barbiturates Reduce metabolic rate decreasing CBF and ICP
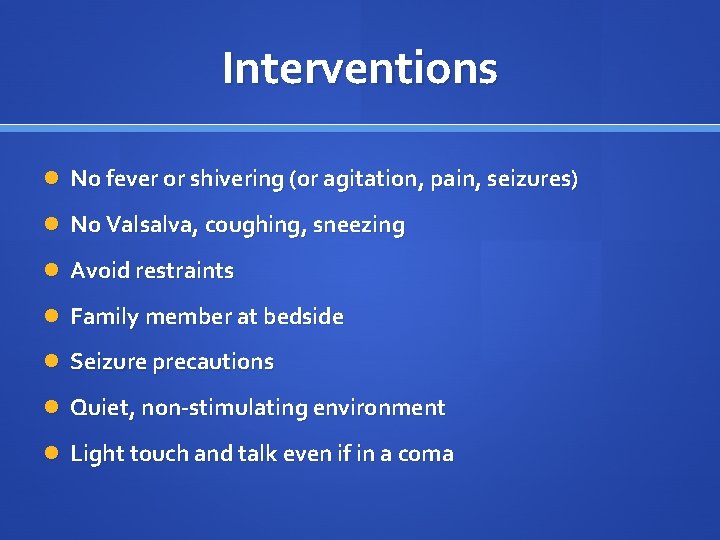
Interventions No fever or shivering (or agitation, pain, seizures) No Valsalva, coughing, sneezing Avoid restraints Family member at bedside Seizure precautions Quiet, non-stimulating environment Light touch and talk even if in a coma
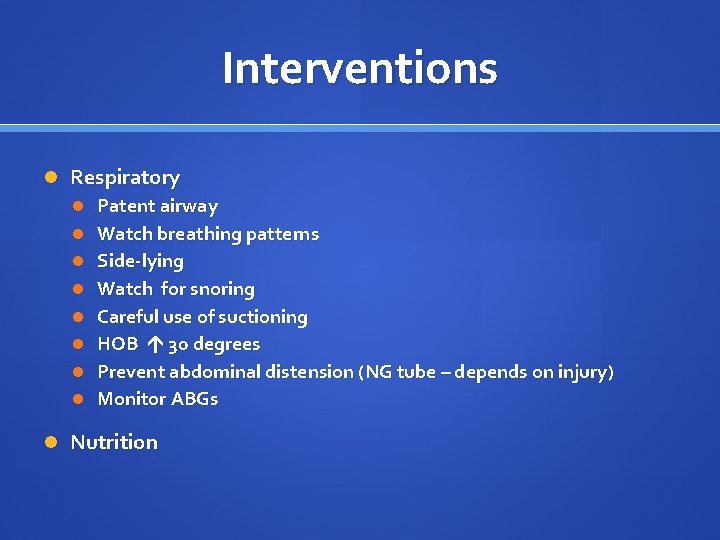
Interventions Respiratory Patent airway Watch breathing patterns Side-lying Watch for snoring Careful use of suctioning HOB 30 degrees Prevent abdominal distension (NG tube – depends on injury) Monitor ABGs Nutrition
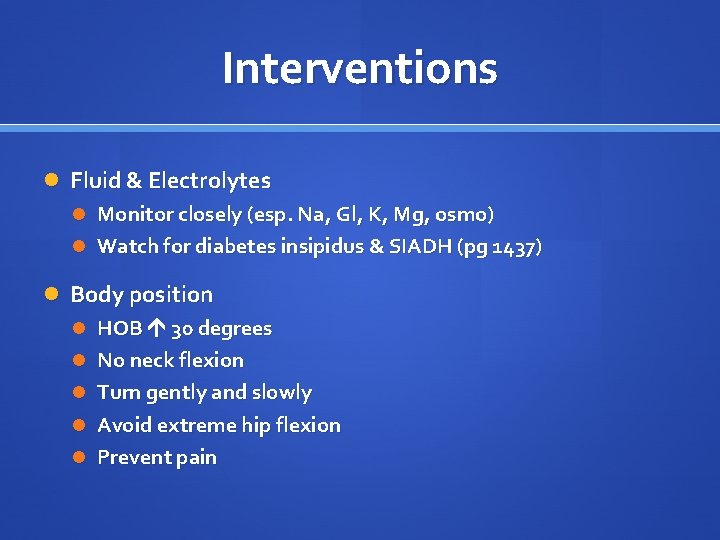
Interventions Fluid & Electrolytes Monitor closely (esp. Na, Gl, K, Mg, osmo) Watch for diabetes insipidus & SIADH (pg 1437) Body position HOB 30 degrees No neck flexion Turn gently and slowly Avoid extreme hip flexion Prevent pain