Intracranial Hemorrhage Emergency Management of Increased ICP Emergency

- Slides: 59
Intracranial Hemorrhage & Emergency Management of Increased ICP Emergency Neurology Lecture Series Amy Yu August 5 th 2009
ICH by numbers Result of a rupture of blood vessel in the brain n Accounts for 10 -15% of all cerebrovascular accidents n 2 million strokes every year worldwide n Rise of admissions in the past 10 years by 18% n Prognosis is poor: estimated mortality n 30% at 7 days n 60% at 1 year n 82% at 10 years n
Outline n Intracranial hemorrhage n Mechanism and pathophysiology n Clinical features n Management principles n Intracranial hypertension n Monitoring n Management principles
Mechanisms of ICH n n n n Hypertension Vascular malformations Intracranial tumors Bleeding diathesis, anticoagulation, fibrinolysis Cerebral amyloid angiopathy Granulomatous angiitis & vasculitides Sympathomimetic agents (amphetamine, cocaine) Hemorrhagic infarction
Clinical features n Features of intracranial hypertension Headache, vomiting, decreased LOC n Correlated with hematoma size and prognosis n Progressive over time n Seizures in lobar ICH n n Focal neurological deficits depending on the location of ICH
POP QUIZ When are patients most likely to suffer from primary ICH? a) b) c) d) Midnight (excessive partying…) 8 AM (don’t want to go to work) Noon (excessive hunger) 5 PM (too much excitement from ending work)
POP QUIZ When are patients most likely to suffer from primary ICH? a) b) c) d) Midnight (excessive partying…) 8 AM (don’t want to go to work) Noon (excessive hunger) 5 PM (too much excitement from ending work)
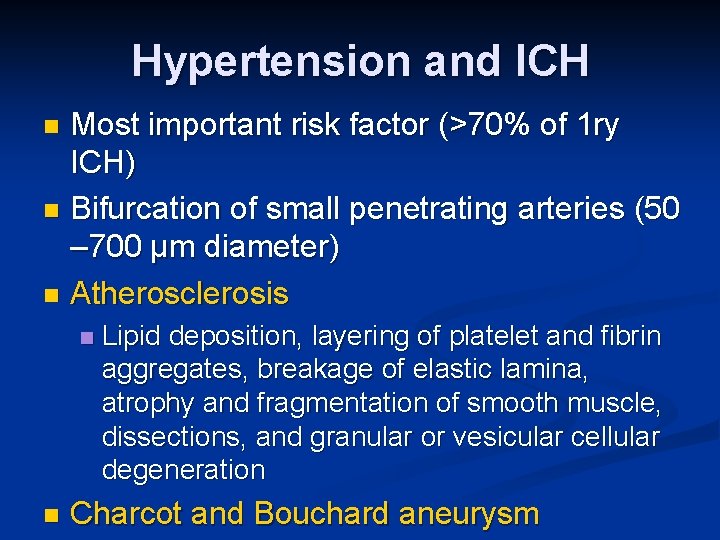
Hypertension and ICH Most important risk factor (>70% of 1 ry ICH) n Bifurcation of small penetrating arteries (50 – 700 μm diameter) n Atherosclerosis n n n Lipid deposition, layering of platelet and fibrin aggregates, breakage of elastic lamina, atrophy and fragmentation of smooth muscle, dissections, and granular or vesicular cellular degeneration Charcot and Bouchard aneurysm
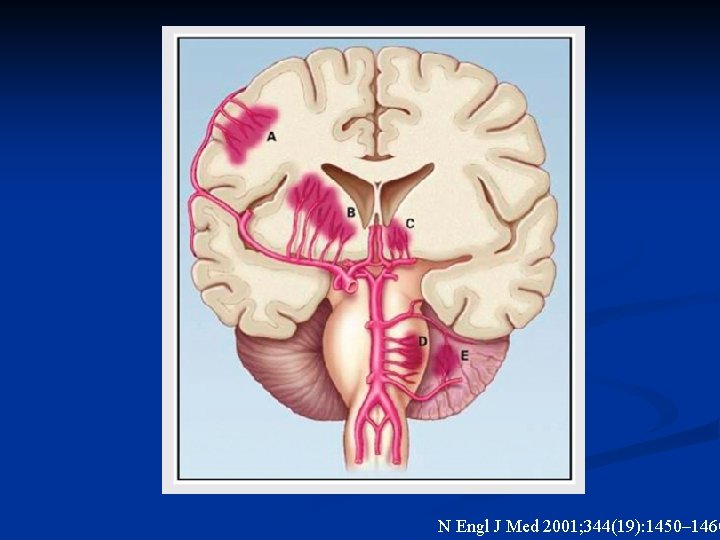
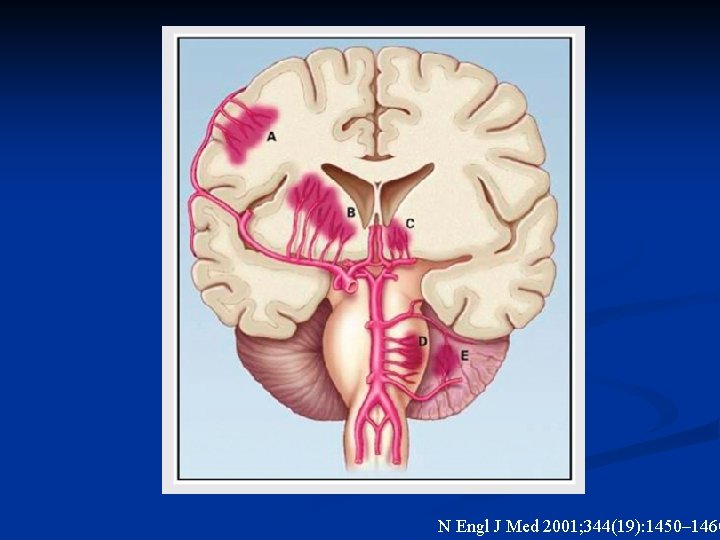
N Engl J Med 2001; 344(19): 1450– 1460
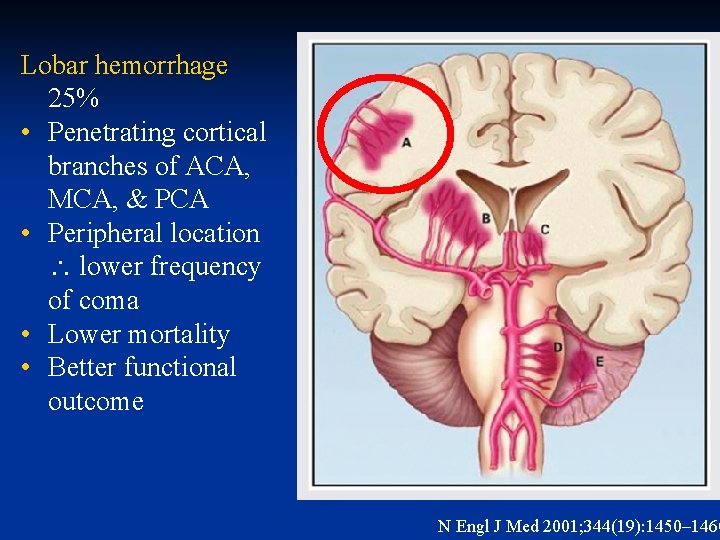
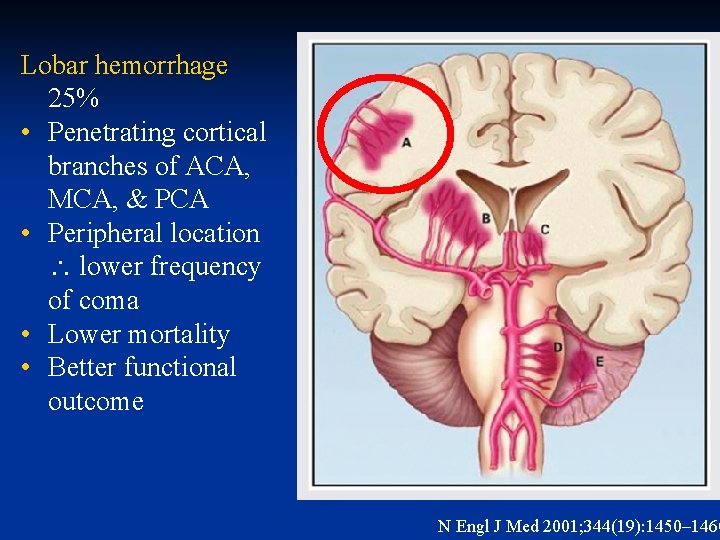
Lobar hemorrhage 25% • Penetrating cortical branches of ACA, MCA, & PCA • Peripheral location lower frequency of coma • Lower mortality • Better functional outcome N Engl J Med 2001; 344(19): 1450– 1460
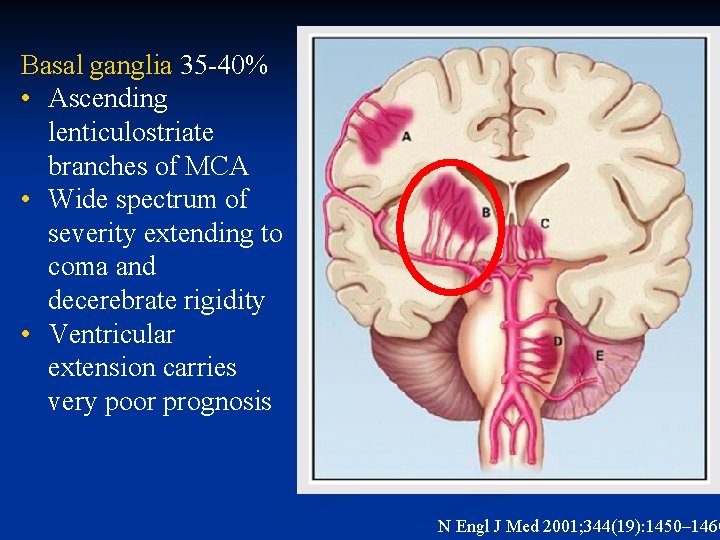
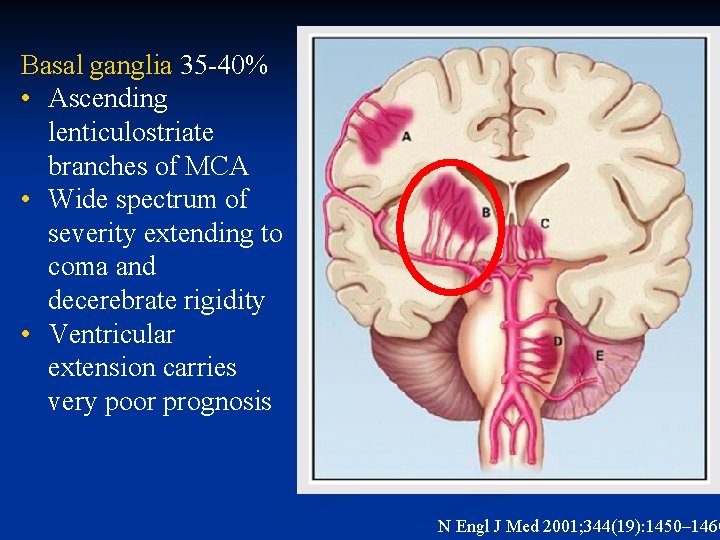
Basal ganglia 35 -40% • Ascending lenticulostriate branches of MCA • Wide spectrum of severity extending to coma and decerebrate rigidity • Ventricular extension carries very poor prognosis N Engl J Med 2001; 344(19): 1450– 1460
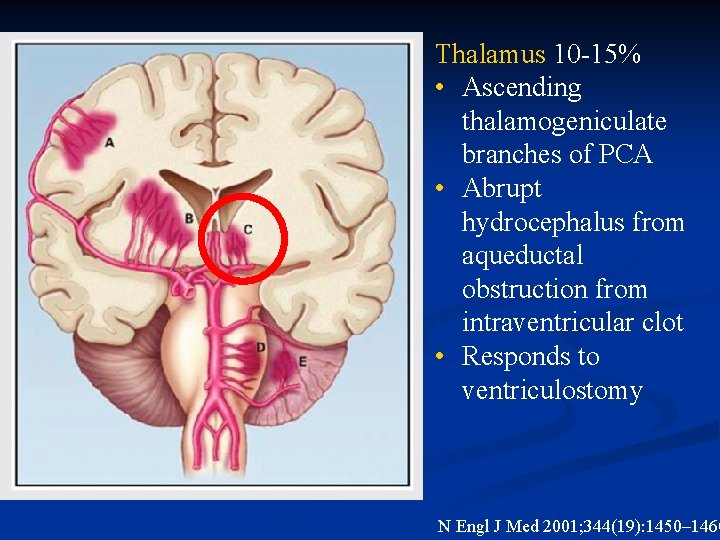
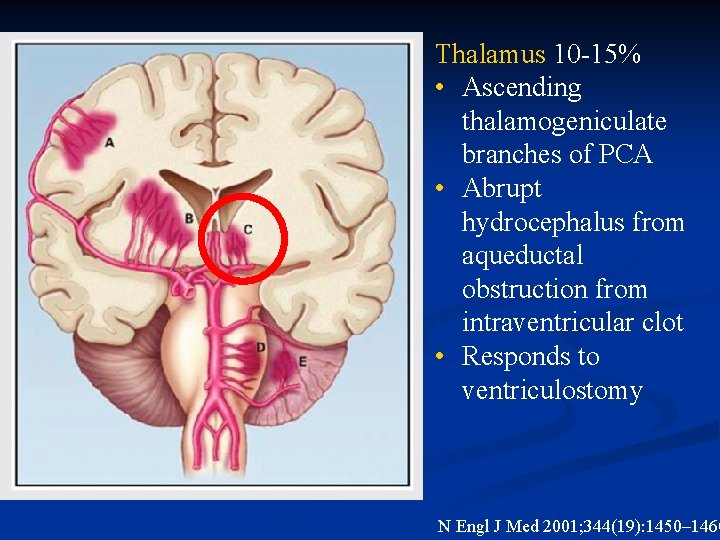
Thalamus 10 -15% • Ascending thalamogeniculate branches of PCA • Abrupt hydrocephalus from aqueductal obstruction from intraventricular clot • Responds to ventriculostomy N Engl J Med 2001; 344(19): 1450– 1460
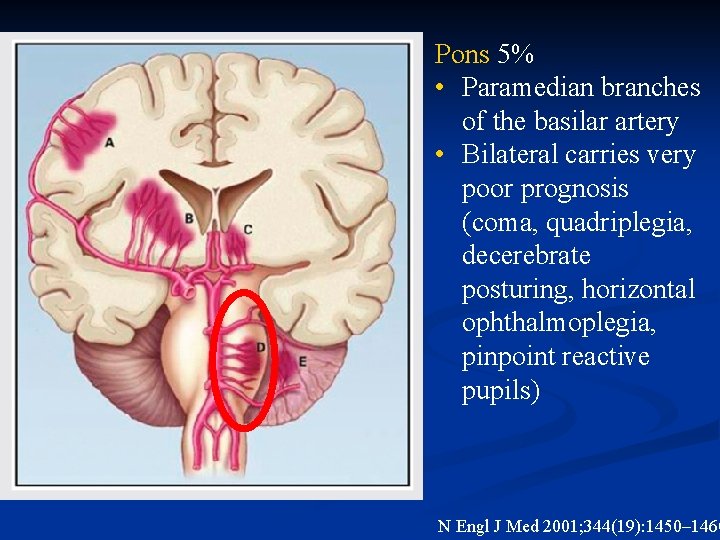
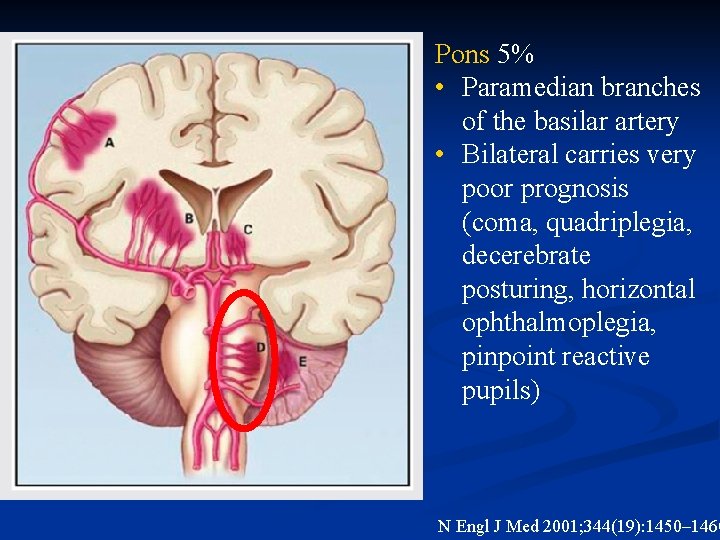
Pons 5% • Paramedian branches of the basilar artery • Bilateral carries very poor prognosis (coma, quadriplegia, decerebrate posturing, horizontal ophthalmoplegia, pinpoint reactive pupils) N Engl J Med 2001; 344(19): 1450– 1460
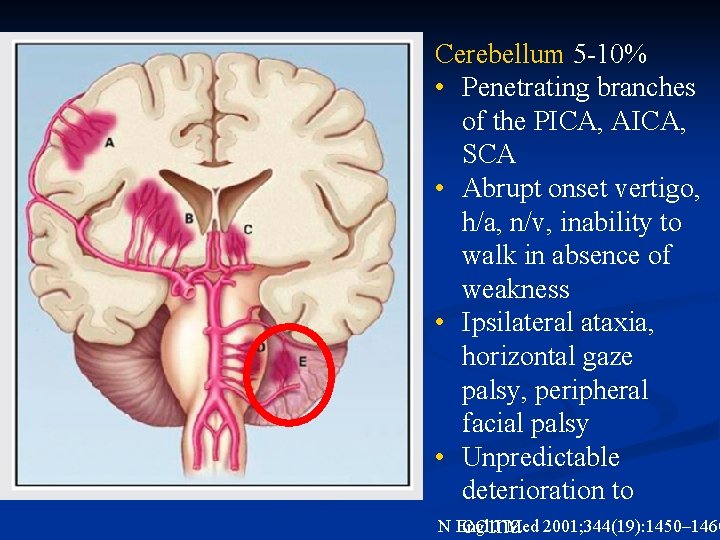
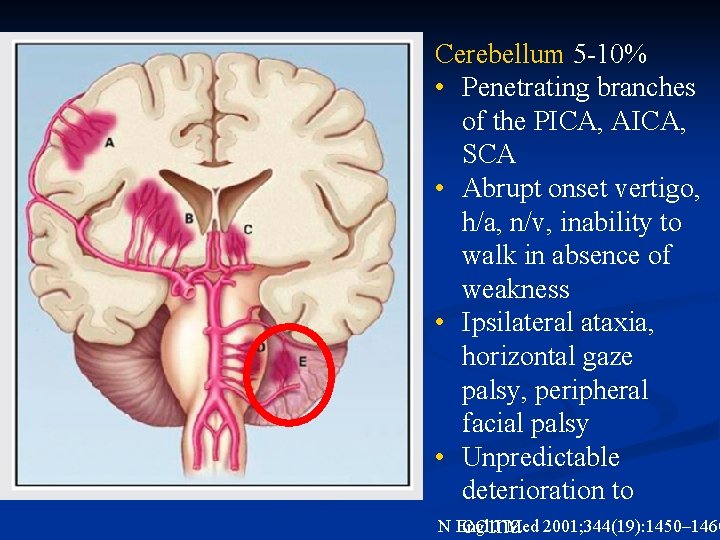
Cerebellum 5 -10% • Penetrating branches of the PICA, AICA, SCA • Abrupt onset vertigo, h/a, n/v, inability to walk in absence of weakness • Ipsilateral ataxia, horizontal gaze palsy, peripheral facial palsy • Unpredictable deterioration to N Engl J Med 2001; 344(19): 1450– 1460 coma
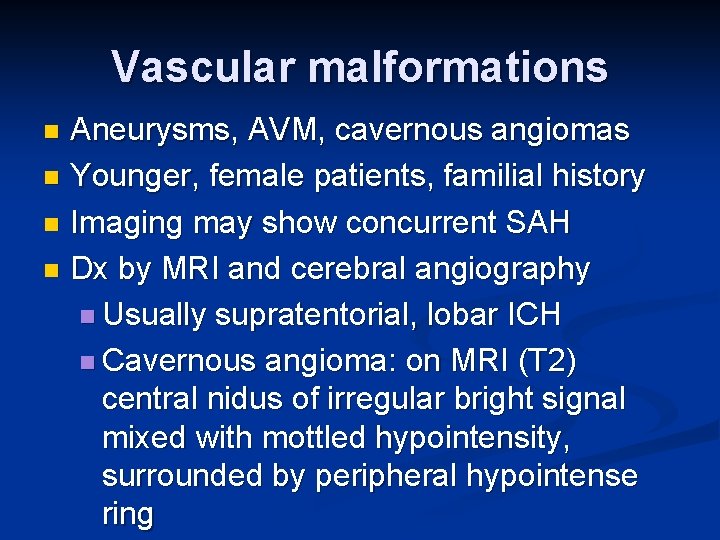
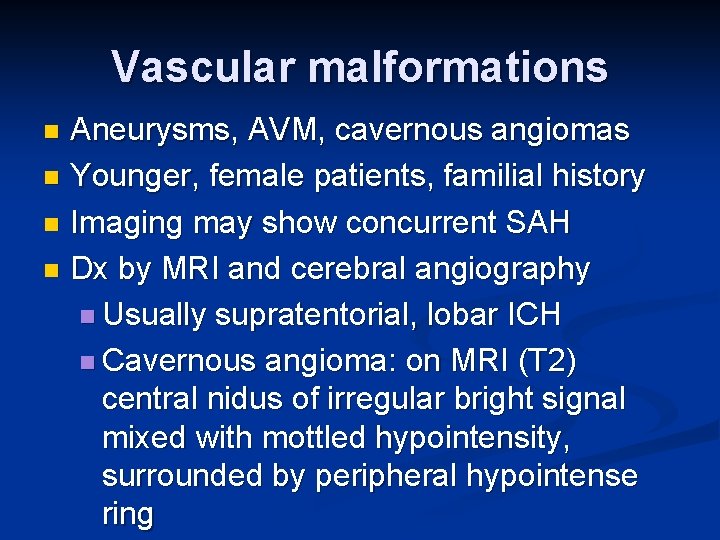
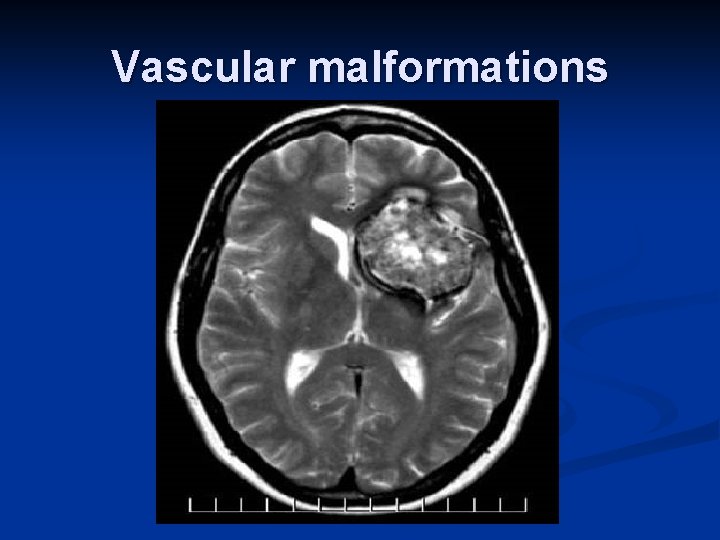
Vascular malformations Aneurysms, AVM, cavernous angiomas n Younger, female patients, familial history n Imaging may show concurrent SAH n Dx by MRI and cerebral angiography n Usually supratentorial, lobar ICH n Cavernous angioma: on MRI (T 2) central nidus of irregular bright signal mixed with mottled hypointensity, surrounded by peripheral hypointense ring n
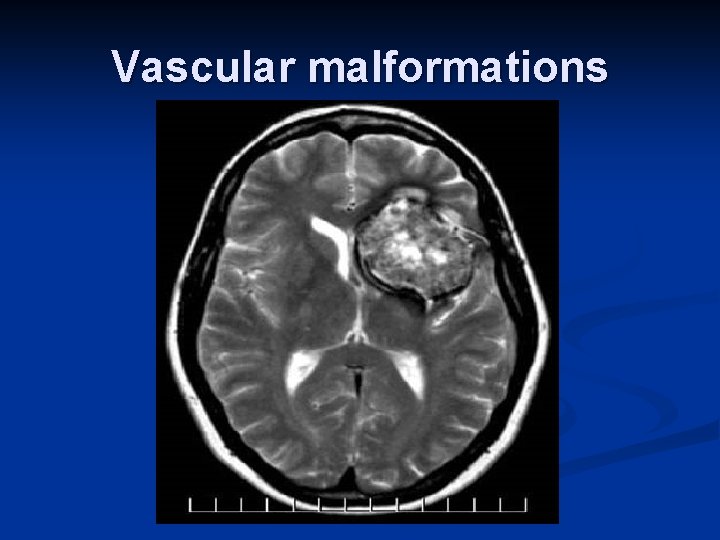
Vascular malformations
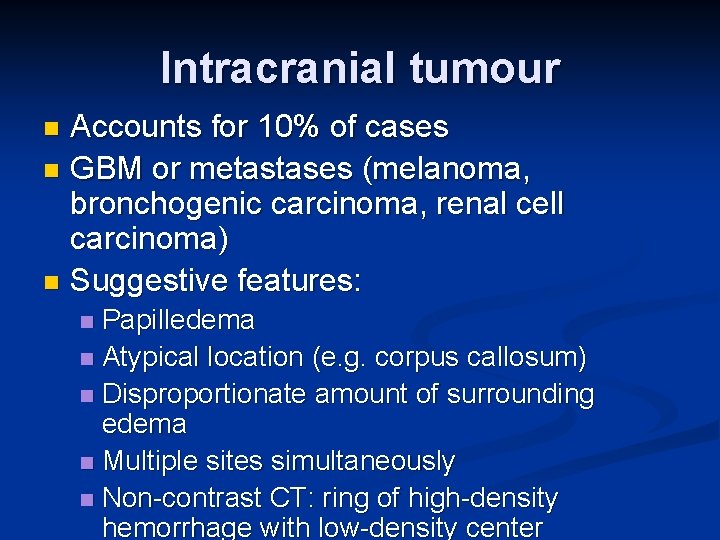
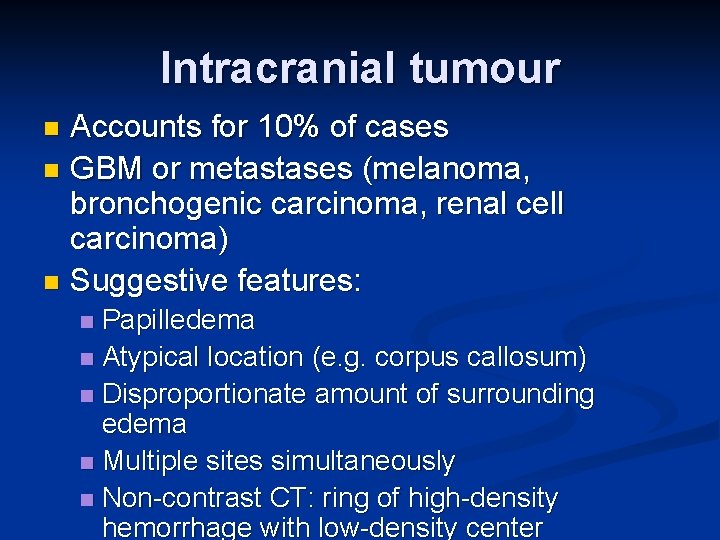
Intracranial tumour Accounts for 10% of cases n GBM or metastases (melanoma, bronchogenic carcinoma, renal cell carcinoma) n Suggestive features: n Papilledema n Atypical location (e. g. corpus callosum) n Disproportionate amount of surrounding edema n Multiple sites simultaneously n Non-contrast CT: ring of high-density hemorrhage with low-density center n
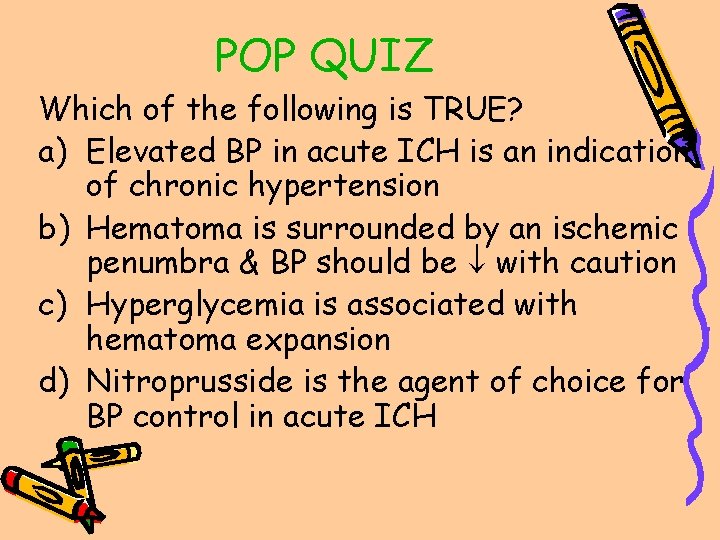
POP QUIZ Which of the following is TRUE? a) Elevated BP in acute ICH is an indication of chronic hypertension b) Hematoma is surrounded by an ischemic penumbra & BP should be with caution c) Hyperglycemia is associated with hematoma expansion d) Nitroprusside is the agent of choice for BP control in acute ICH
POP QUIZ Which of the following is TRUE? a) Elevated BP in acute ICH is an indication of chronic hypertension b) Hematoma is surrounded by an ischemic penumbra & BP should be with caution c) Hyperglycemia is associated with hematoma expansion d) Nitroprusside is the agent of choice for BP control in acute ICH
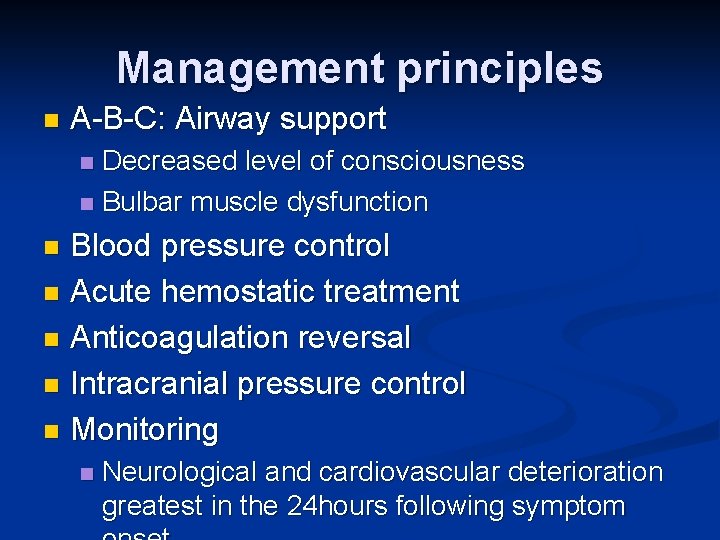
Management principles n A-B-C: Airway support Decreased level of consciousness n Bulbar muscle dysfunction n Blood pressure control n Acute hemostatic treatment n Anticoagulation reversal n Intracranial pressure control n Monitoring n n Neurological and cardiovascular deterioration greatest in the 24 hours following symptom
Blood pressure & ICH n BP is elevated on admission even in patients who have no history of hypertension n MAP > 120 mm. Hg in over 2/3 of patients Precipitant of the hemorrhage? n Reflection of chronic hypertension? n Attempt to maintain CPP? n Sympathetic activation 2 ry to pain & anxiety? n
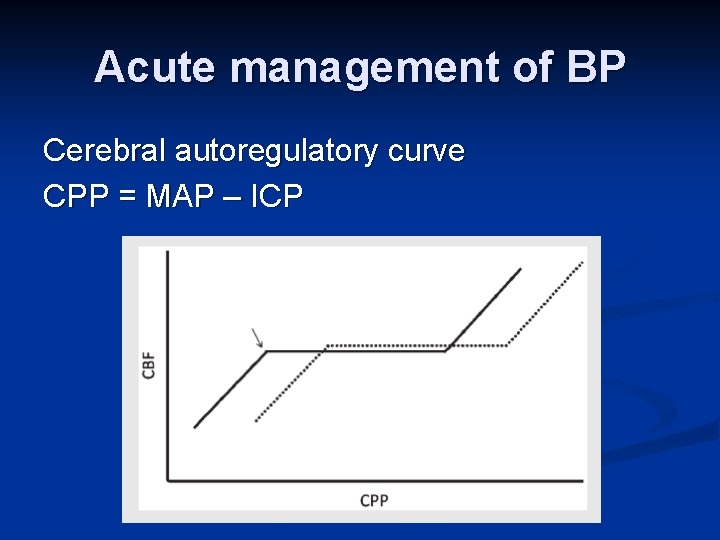
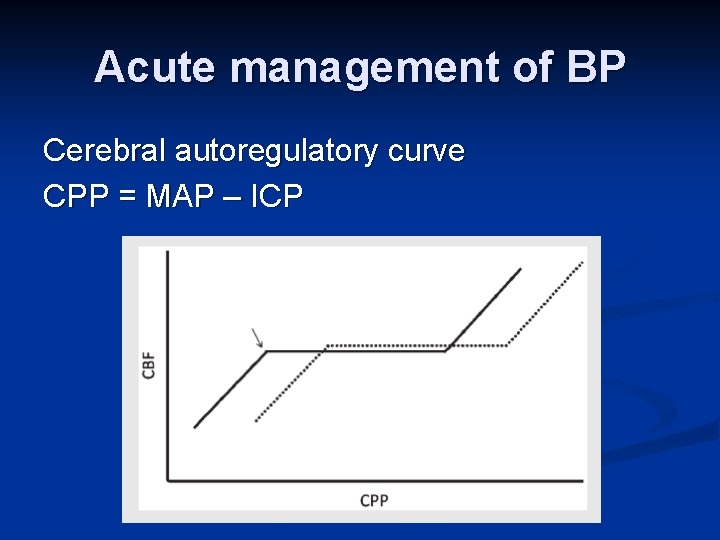
Acute management of BP Cerebral autoregulatory curve CPP = MAP – ICP
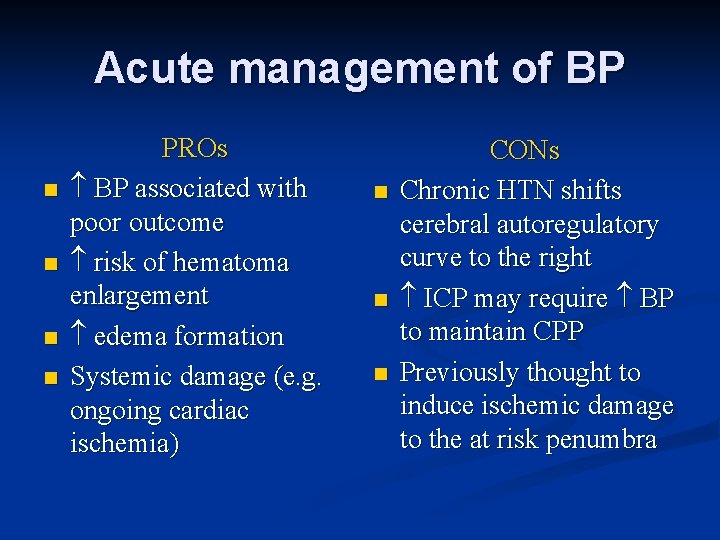
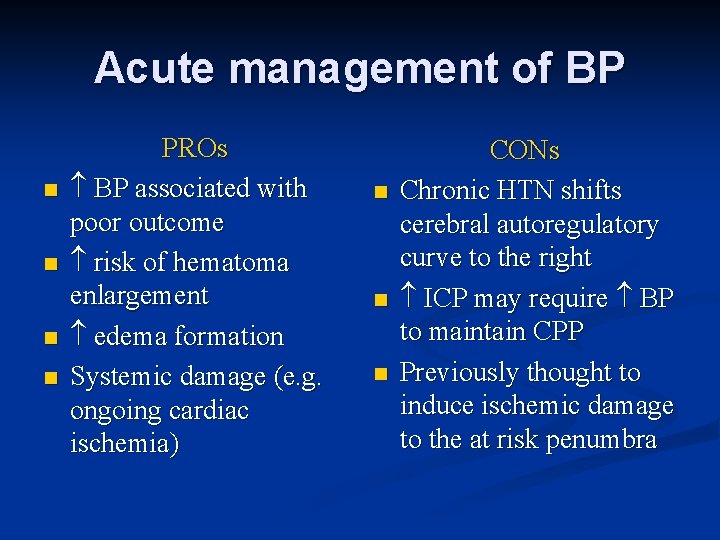
Acute management of BP n n PROs BP associated with poor outcome risk of hematoma enlargement edema formation Systemic damage (e. g. ongoing cardiac ischemia) n n n CONs Chronic HTN shifts cerebral autoregulatory curve to the right ICP may require BP to maintain CPP Previously thought to induce ischemic damage to the at risk penumbra
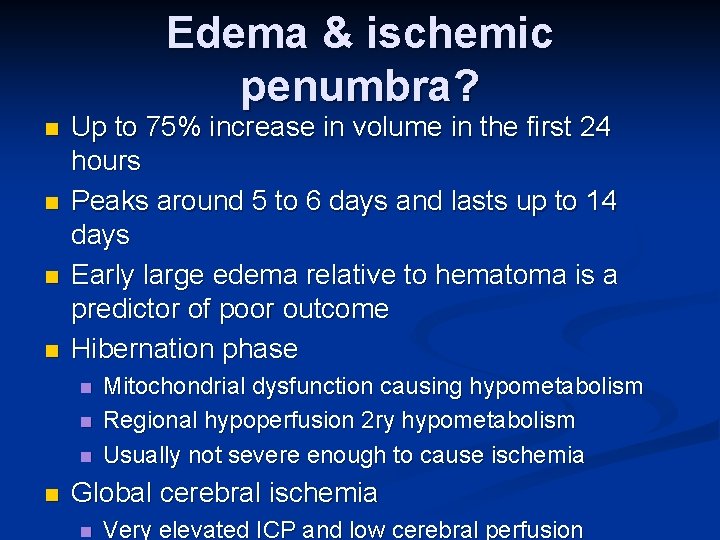
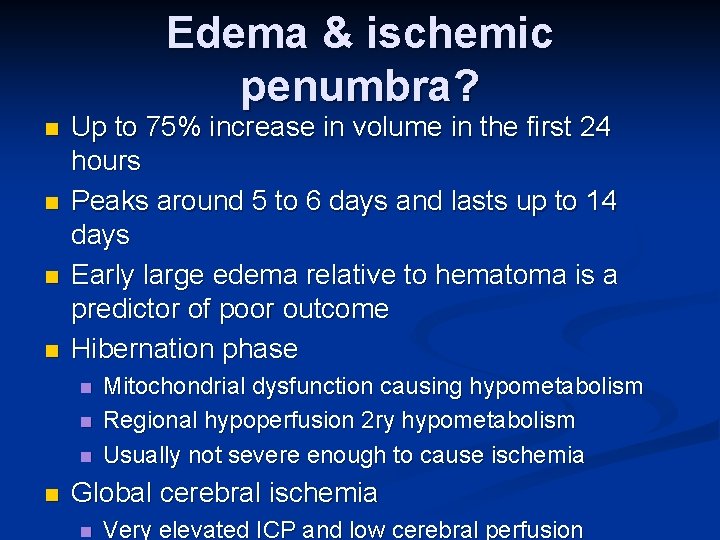
Edema & ischemic penumbra? n n Up to 75% increase in volume in the first 24 hours Peaks around 5 to 6 days and lasts up to 14 days Early large edema relative to hematoma is a predictor of poor outcome Hibernation phase n n Mitochondrial dysfunction causing hypometabolism Regional hypoperfusion 2 ry hypometabolism Usually not severe enough to cause ischemia Global cerebral ischemia n Very elevated ICP and low cerebral perfusion
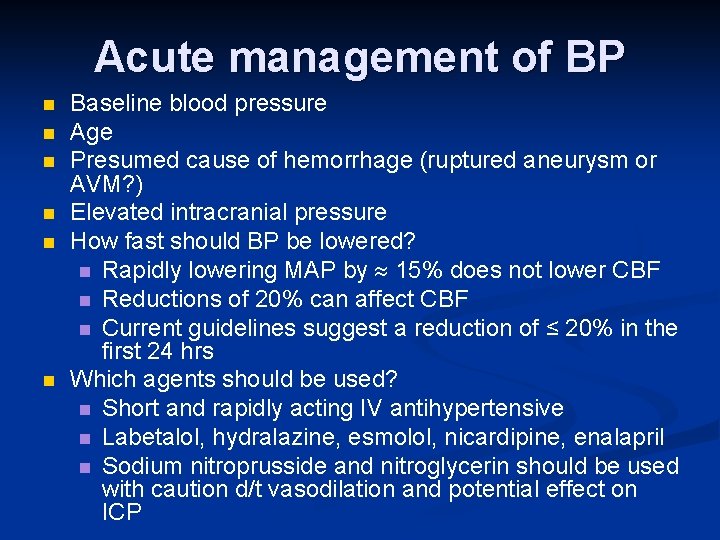
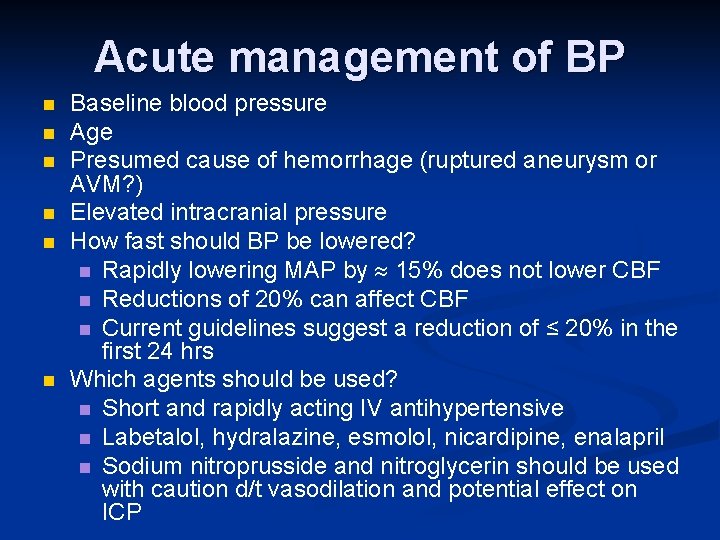
Acute management of BP n n n Baseline blood pressure Age Presumed cause of hemorrhage (ruptured aneurysm or AVM? ) Elevated intracranial pressure How fast should BP be lowered? n Rapidly lowering MAP by 15% does not lower CBF n Reductions of 20% can affect CBF n Current guidelines suggest a reduction of ≤ 20% in the first 24 hrs Which agents should be used? n Short and rapidly acting IV antihypertensive n Labetalol, hydralazine, esmolol, nicardipine, enalapril n Sodium nitroprusside and nitroglycerin should be used with caution d/t vasodilation and potential effect on ICP
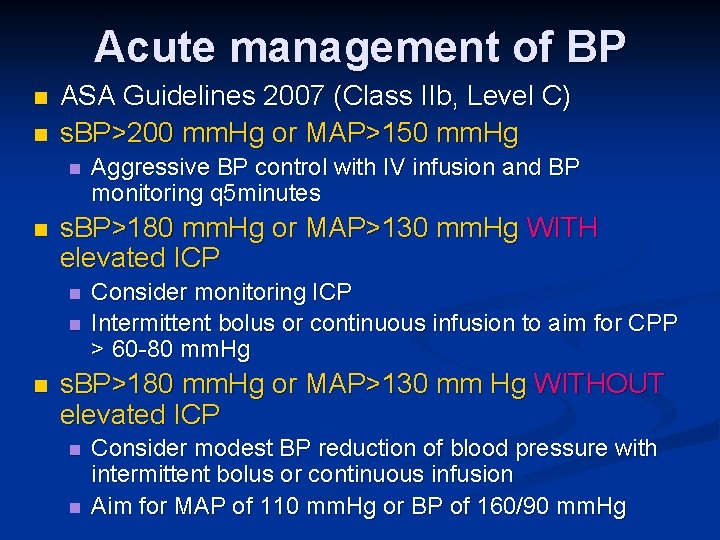
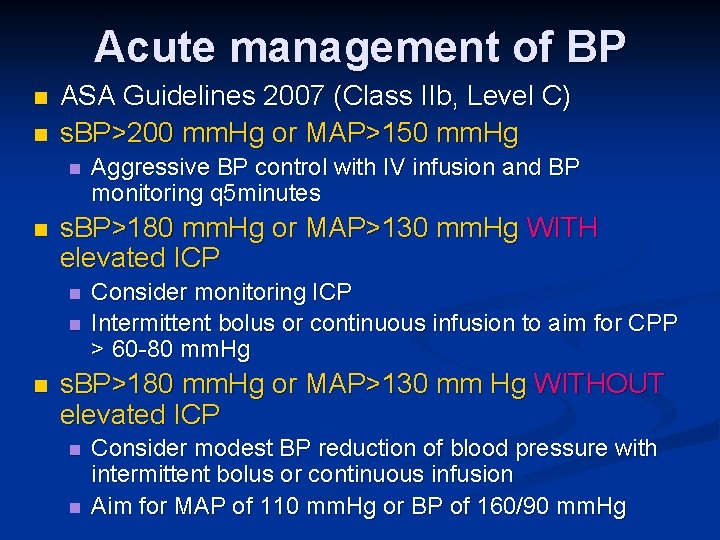
Acute management of BP n n ASA Guidelines 2007 (Class IIb, Level C) s. BP>200 mm. Hg or MAP>150 mm. Hg n n s. BP>180 mm. Hg or MAP>130 mm. Hg WITH elevated ICP n n n Aggressive BP control with IV infusion and BP monitoring q 5 minutes Consider monitoring ICP Intermittent bolus or continuous infusion to aim for CPP > 60 -80 mm. Hg s. BP>180 mm. Hg or MAP>130 mm Hg WITHOUT elevated ICP n n Consider modest BP reduction of blood pressure with intermittent bolus or continuous infusion Aim for MAP of 110 mm. Hg or BP of 160/90 mm. Hg
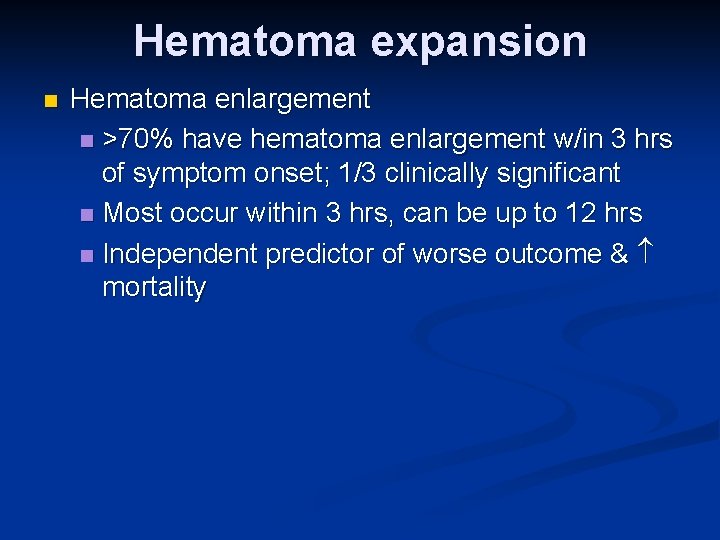
Hematoma expansion n Hematoma enlargement n >70% have hematoma enlargement w/in 3 hrs of symptom onset; 1/3 clinically significant n Most occur within 3 hrs, can be up to 12 hrs n Independent predictor of worse outcome & mortality
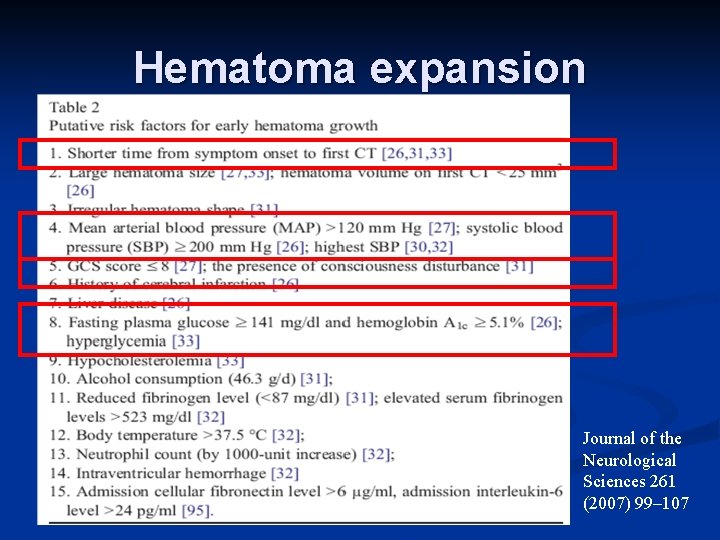
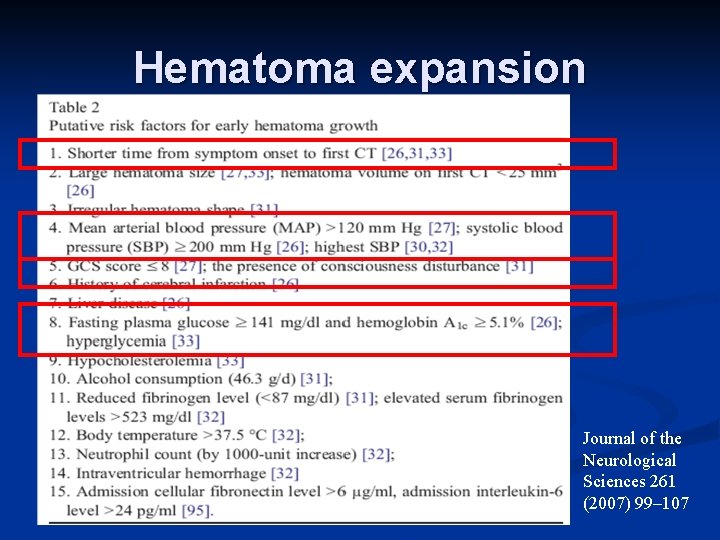
Hematoma expansion Journal of the Neurological Sciences 261 (2007) 99– 107
Recombinant Factor VIIa n n n Factor VIIa has locally action at sites of tissue injury and vascular-wall disruption by binding tissue factor & generating thrombin and activating platelets Recombinant FVIIa directly activates f. X on the surface of activated plts resulting in acceleration of coagulation Factor Seven for Acute Hemorrhagic Stroke (FAST) trial, N Engl J Med 2008; 358: 2127 -37 n n n 841 patients, within 4 hours of onset of stroke Placebo vs. 20 μg/kg vs. 80 μg/kg of r. FVIIa 1 ry end point: 90 -day functional outcome or death
Recombinant Factor VIIa n n Significant reduction in growth of hematoma volume in the 80 μg/kg group No significant difference in functional outcome and mortality Venous thromboembolic events were similar in all three groups Arterial thromboembolic events were significantly more frequent in the 80 μg/kg group
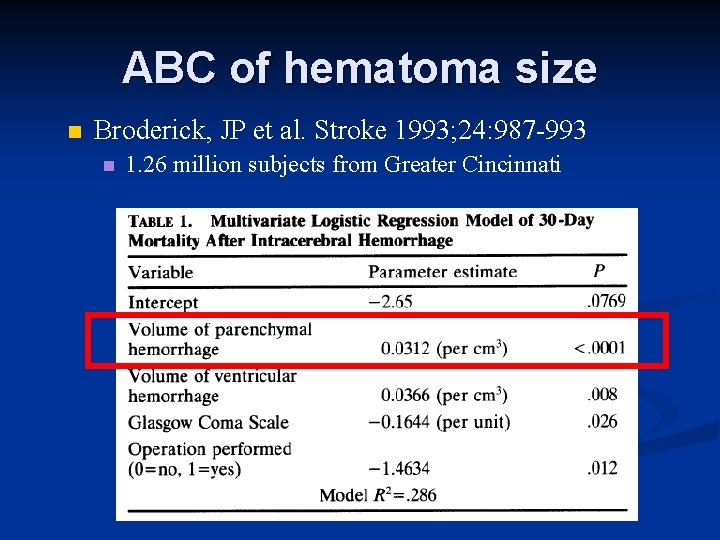
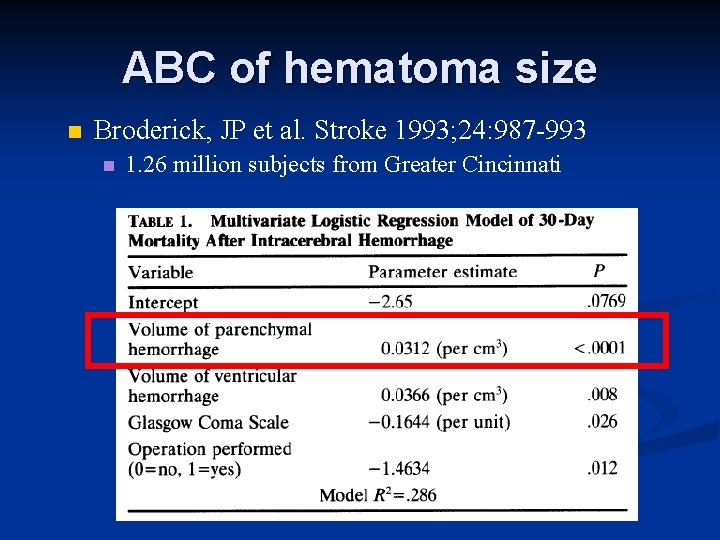
ABC of hematoma size n Broderick, JP et al. Stroke 1993; 24: 987 -993 n 1. 26 million subjects from Greater Cincinnati
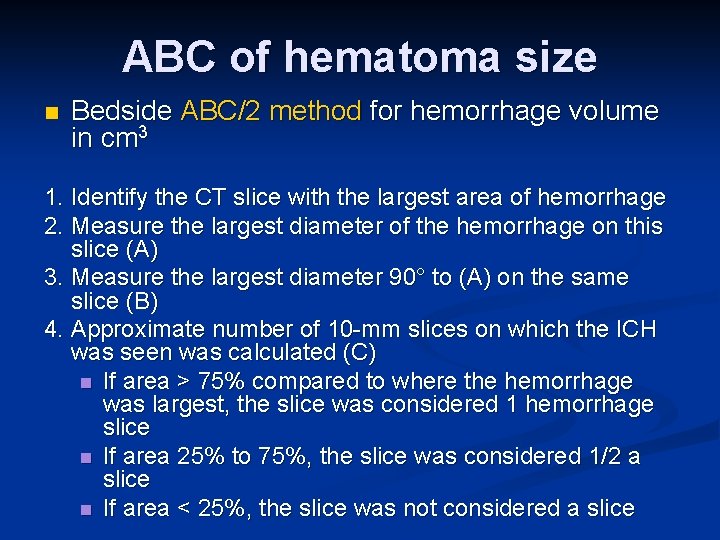
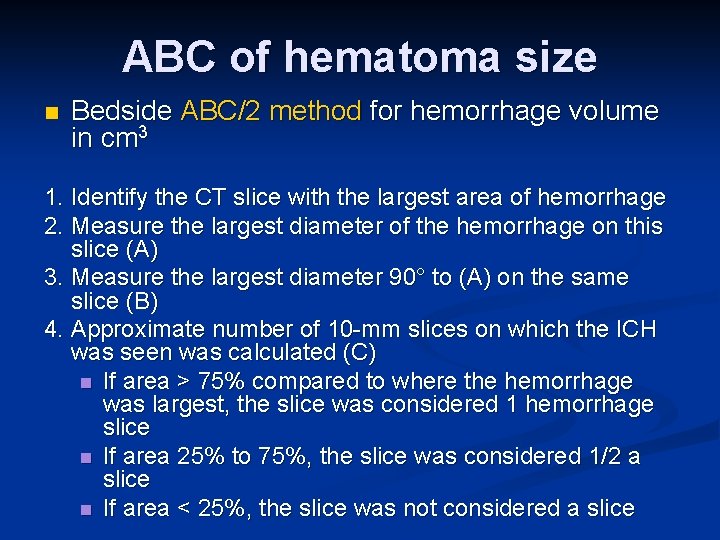
ABC of hematoma size n Bedside ABC/2 method for hemorrhage volume in cm 3 1. Identify the CT slice with the largest area of hemorrhage 2. Measure the largest diameter of the hemorrhage on this slice (A) 3. Measure the largest diameter 90° to (A) on the same slice (B) 4. Approximate number of 10 -mm slices on which the ICH was seen was calculated (C) n If area > 75% compared to where the hemorrhage was largest, the slice was considered 1 hemorrhage slice n If area 25% to 75%, the slice was considered 1/2 a slice n If area < 25%, the slice was not considered a slice
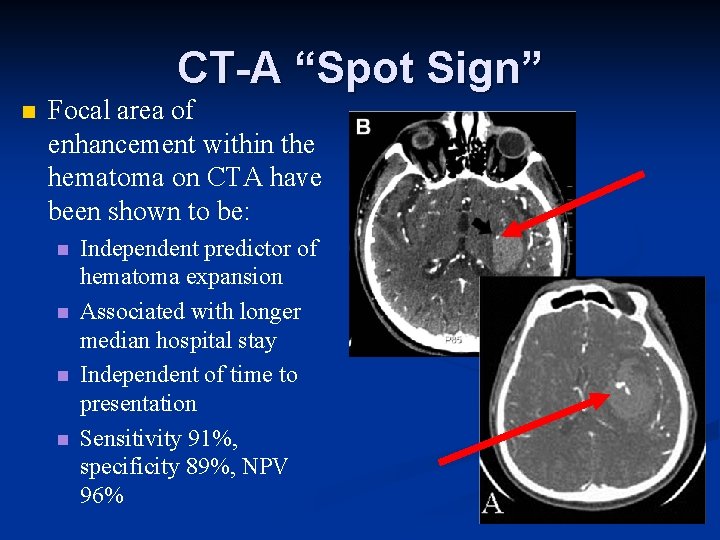
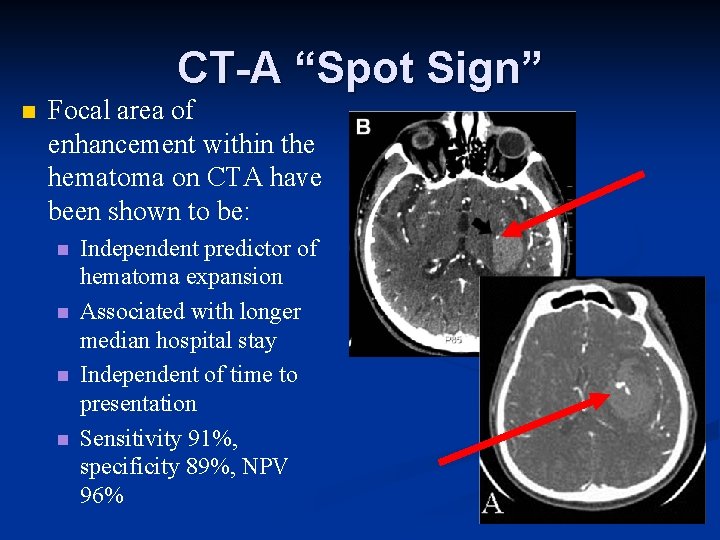
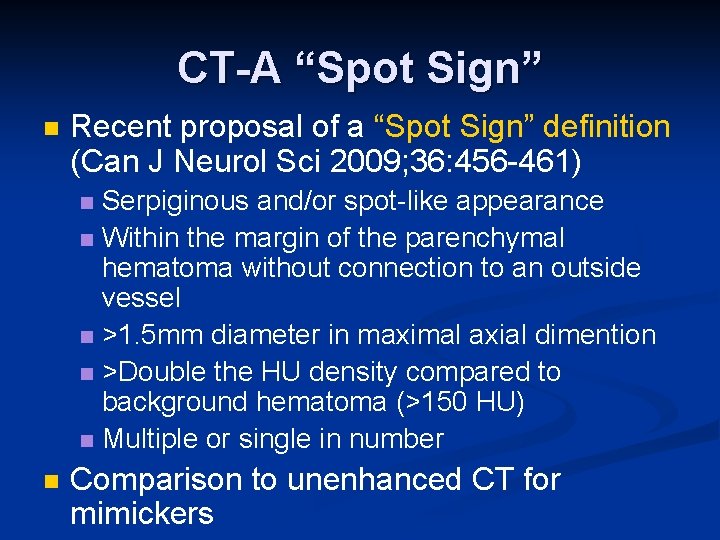
CT-A “Spot Sign” n Focal area of enhancement within the hematoma on CTA have been shown to be: n n Independent predictor of hematoma expansion Associated with longer median hospital stay Independent of time to presentation Sensitivity 91%, specificity 89%, NPV 96%
CT-A “Spot Sign” n Recent proposal of a “Spot Sign” definition (Can J Neurol Sci 2009; 36: 456 -461) Serpiginous and/or spot-like appearance n Within the margin of the parenchymal hematoma without connection to an outside vessel n >1. 5 mm diameter in maximal axial dimention n >Double the HU density compared to background hematoma (>150 HU) n Multiple or single in number n n Comparison to unenhanced CT for mimickers
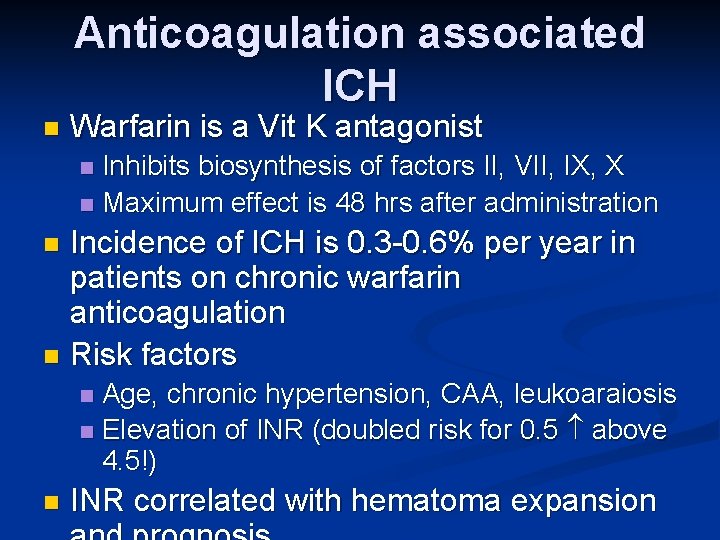
Anticoagulation associated ICH n Warfarin is a Vit K antagonist Inhibits biosynthesis of factors II, VII, IX, X n Maximum effect is 48 hrs after administration n Incidence of ICH is 0. 3 -0. 6% per year in patients on chronic warfarin anticoagulation n Risk factors n Age, chronic hypertension, CAA, leukoaraiosis n Elevation of INR (doubled risk for 0. 5 above 4. 5!) n n INR correlated with hematoma expansion
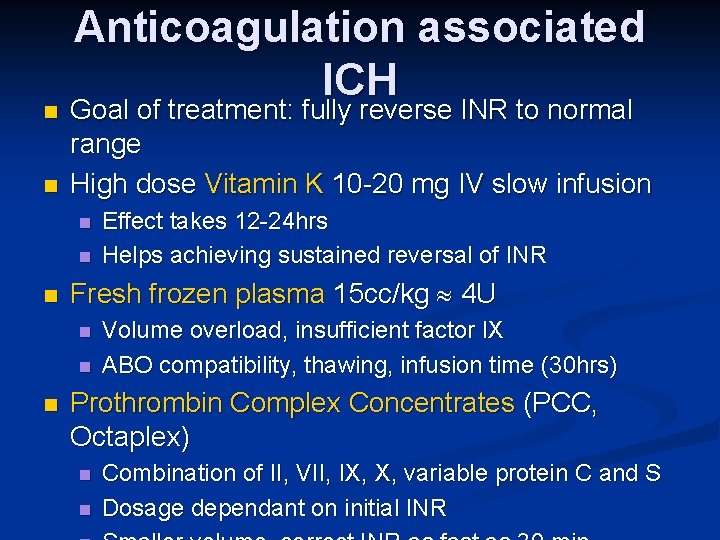
n n Anticoagulation associated ICH Goal of treatment: fully reverse INR to normal range High dose Vitamin K 10 -20 mg IV slow infusion n Fresh frozen plasma 15 cc/kg 4 U n n n Effect takes 12 -24 hrs Helps achieving sustained reversal of INR Volume overload, insufficient factor IX ABO compatibility, thawing, infusion time (30 hrs) Prothrombin Complex Concentrates (PCC, Octaplex) n n Combination of II, VII, IX, X, variable protein C and S Dosage dependant on initial INR
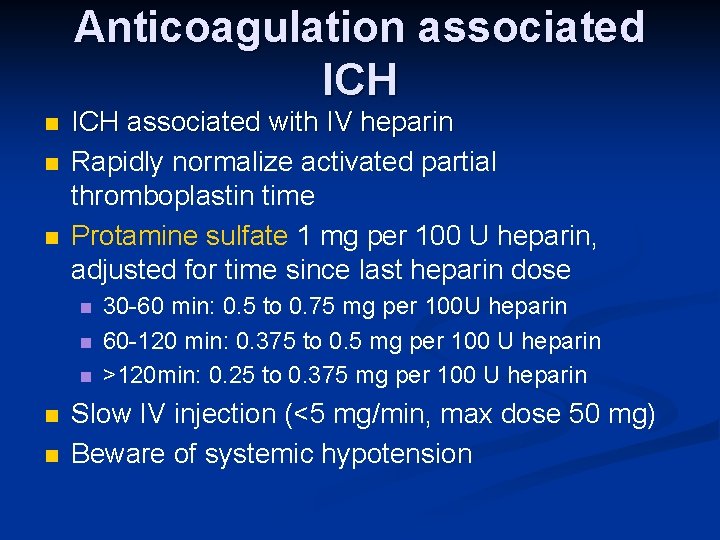
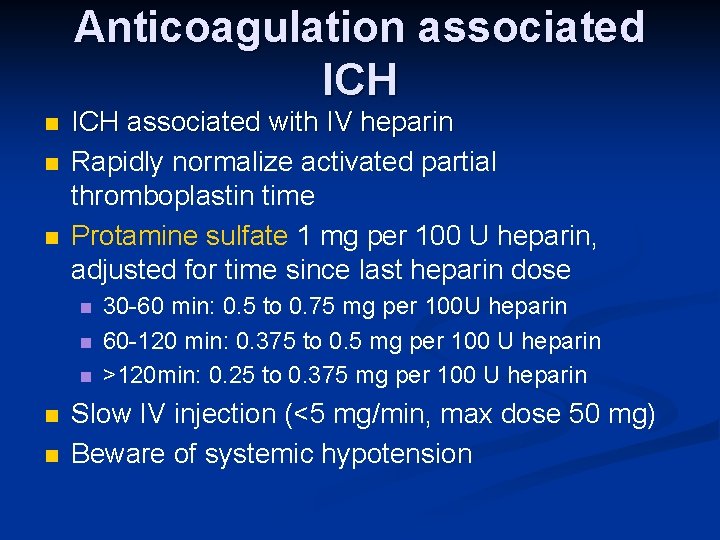
Anticoagulation associated ICH n n n ICH associated with IV heparin Rapidly normalize activated partial thromboplastin time Protamine sulfate 1 mg per 100 U heparin, adjusted for time since last heparin dose n n n 30 -60 min: 0. 5 to 0. 75 mg per 100 U heparin 60 -120 min: 0. 375 to 0. 5 mg per 100 U heparin >120 min: 0. 25 to 0. 375 mg per 100 U heparin Slow IV injection (<5 mg/min, max dose 50 mg) Beware of systemic hypotension
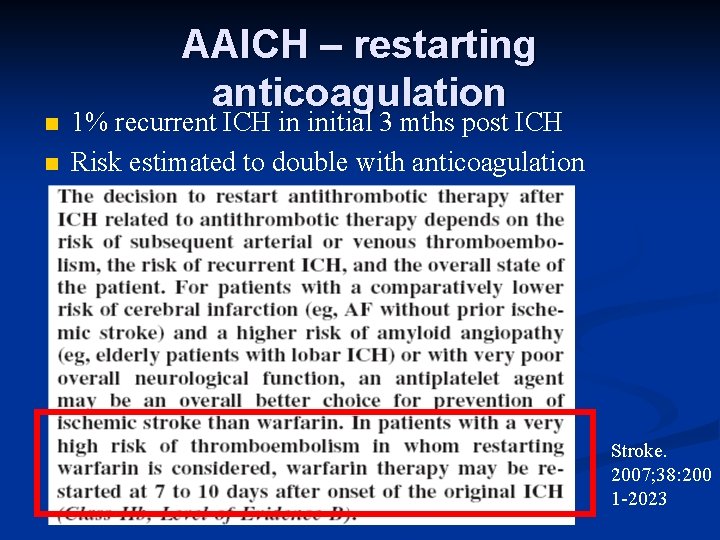
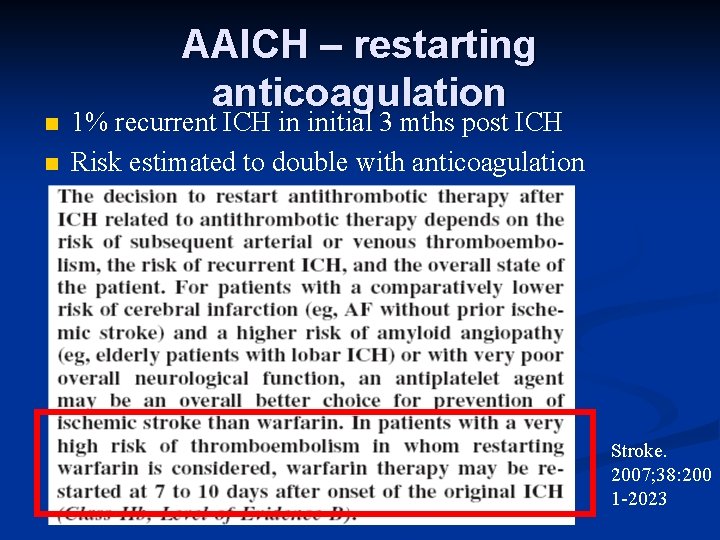
n n AAICH – restarting anticoagulation 1% recurrent ICH in initial 3 mths post ICH Risk estimated to double with anticoagulation Stroke. 2007; 38: 200 1 -2023
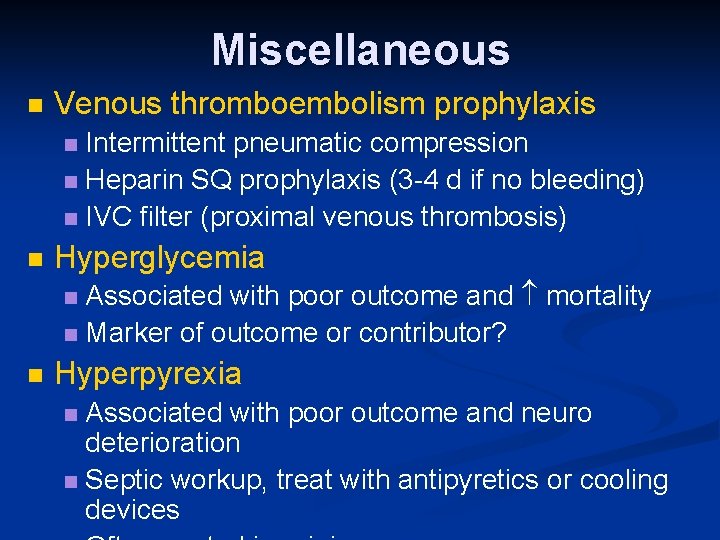
Miscellaneous n Venous thromboembolism prophylaxis Intermittent pneumatic compression n Heparin SQ prophylaxis (3 -4 d if no bleeding) n IVC filter (proximal venous thrombosis) n n Hyperglycemia Associated with poor outcome and mortality n Marker of outcome or contributor? n n Hyperpyrexia Associated with poor outcome and neuro deterioration n Septic workup, treat with antipyretics or cooling devices n
Part II: Management of Increased Intracranial Pressure
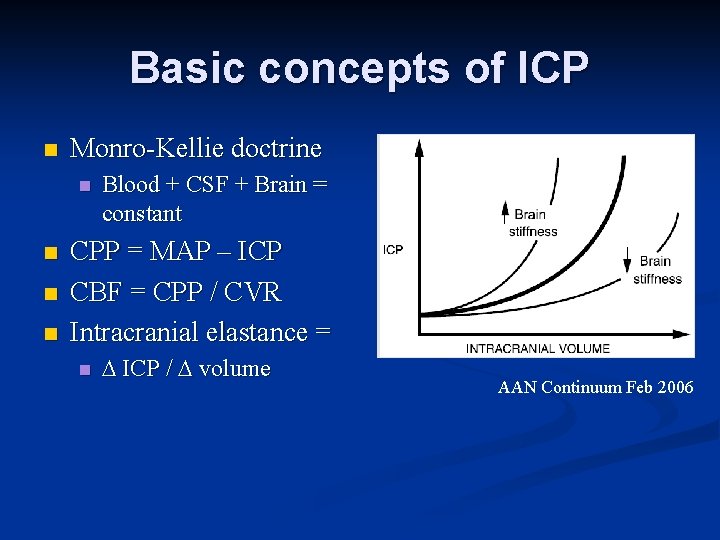
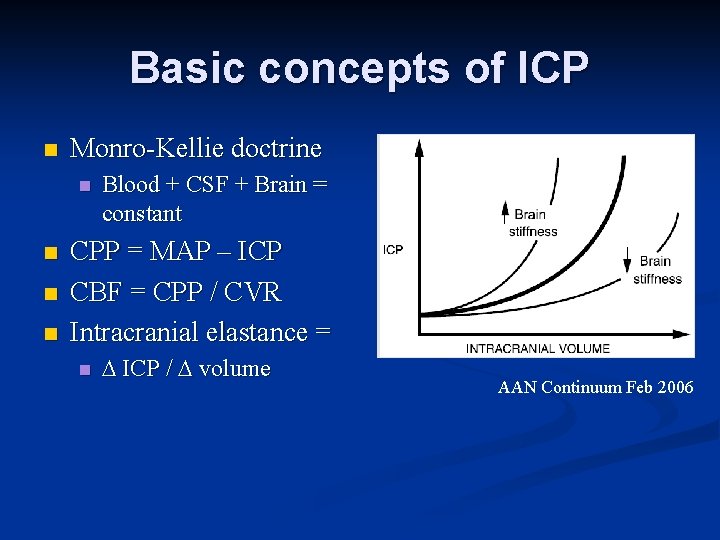
Basic concepts of ICP n Monro-Kellie doctrine n n Blood + CSF + Brain = constant CPP = MAP – ICP CBF = CPP / CVR Intracranial elastance = n ICP / volume AAN Continuum Feb 2006
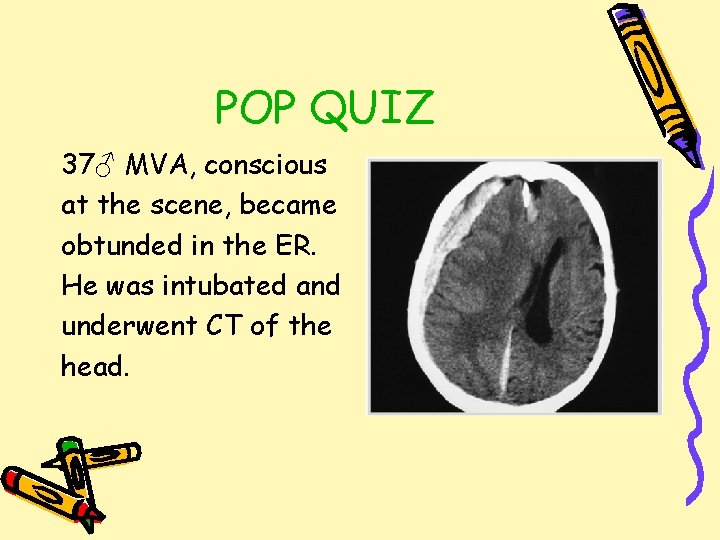
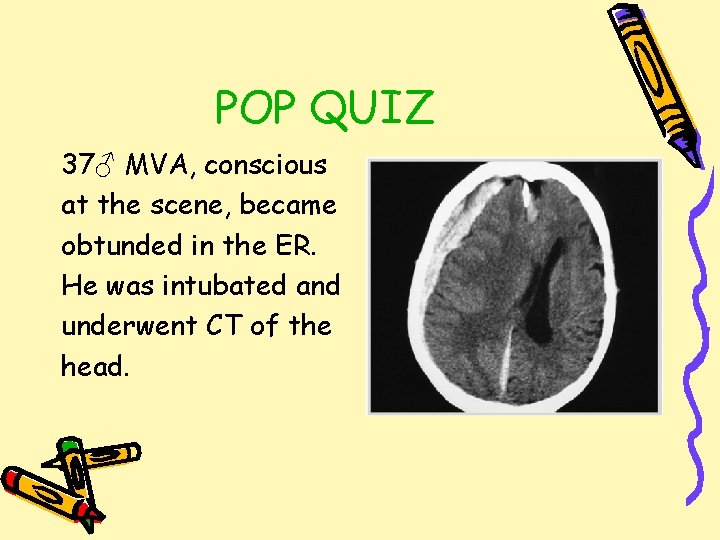
POP QUIZ 37♂ MVA, conscious at the scene, became obtunded in the ER. He was intubated and underwent CT of the head.
POP QUIZ Should this candidate have invasive intracranial pressure monitoring? a) Yes b) No c) It depends
POP QUIZ Should this candidate have invasive intracranial pressure monitoring? a) Yes b) No c) It depends
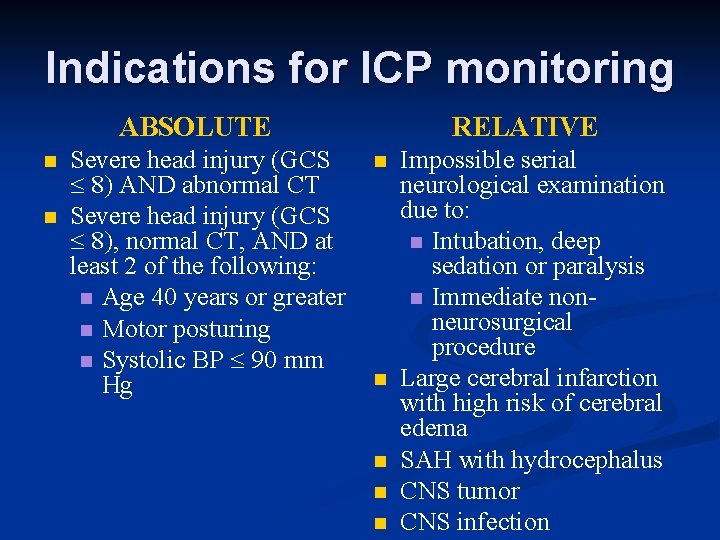
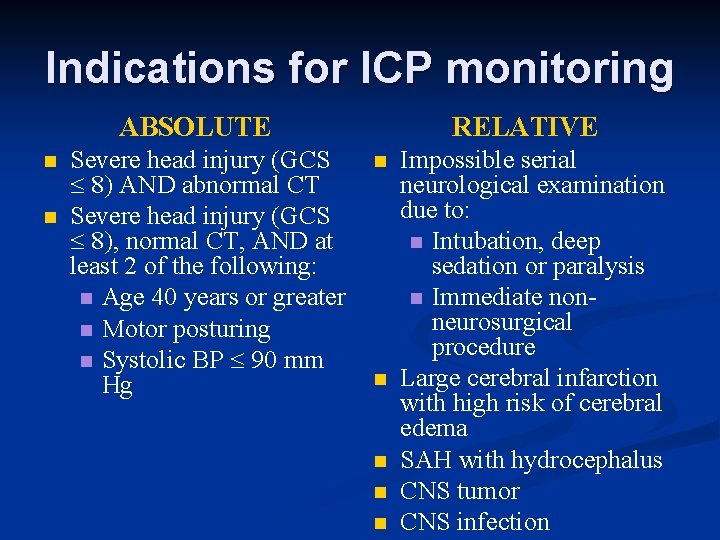
Indications for ICP monitoring ABSOLUTE n n Severe head injury (GCS 8) AND abnormal CT Severe head injury (GCS 8), normal CT, AND at least 2 of the following: n Age 40 years or greater n Motor posturing n Systolic BP 90 mm Hg RELATIVE n n n Impossible serial neurological examination due to: n Intubation, deep sedation or paralysis n Immediate nonneurosurgical procedure Large cerebral infarction with high risk of cerebral edema SAH with hydrocephalus CNS tumor CNS infection
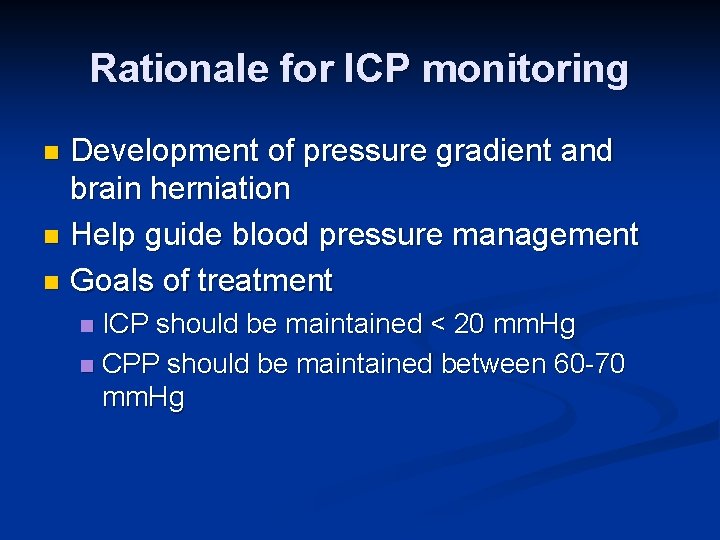
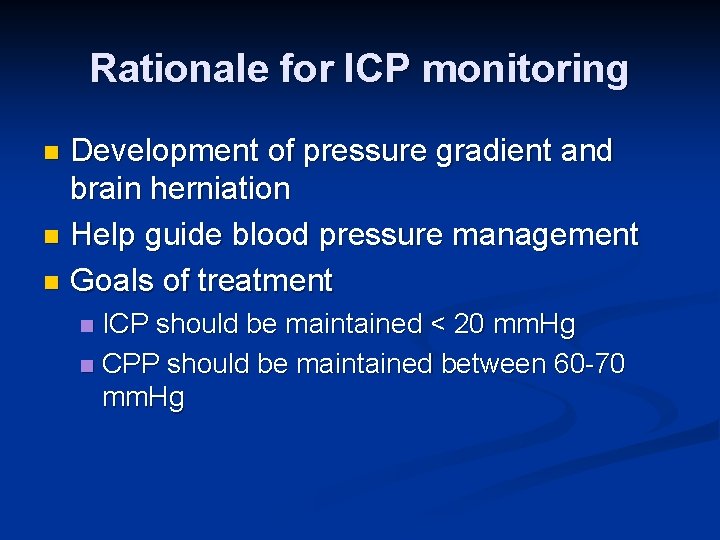
Rationale for ICP monitoring Development of pressure gradient and brain herniation n Help guide blood pressure management n Goals of treatment n ICP should be maintained < 20 mm. Hg n CPP should be maintained between 60 -70 mm. Hg n
POP QUIZ What is the most appropriate next step in management in the ER pending neurosurgical evaluation? a) Immediate insertion of an external ventricular drain b) Hyperventilation c) Mannitol followed by hypertonic saline d) Head elevation
POP QUIZ What is the most appropriate next step in management in the ER pending neurosurgical evaluation? a) Immediate insertion of an external ventricular drain b) Hyperventilation c) Mannitol followed by hypertonic saline d) Head elevation
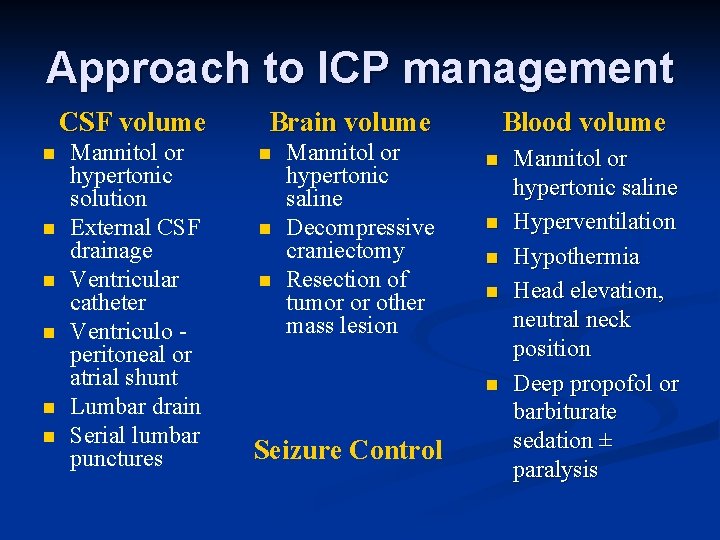
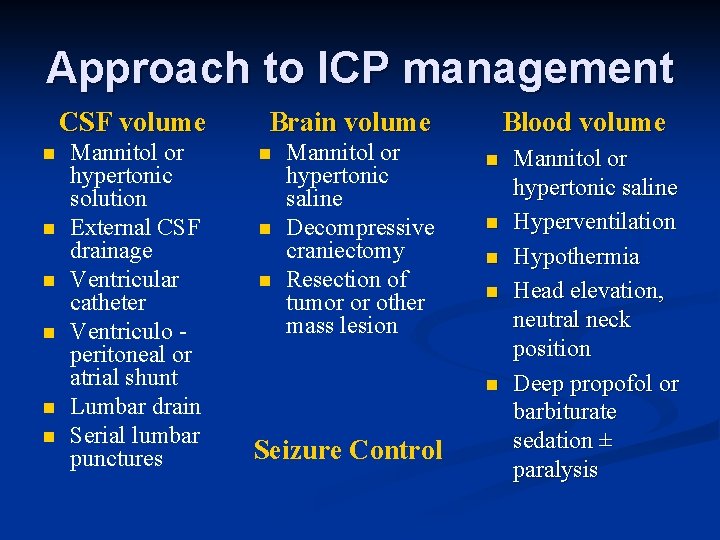
Approach to ICP management CSF volume n n n Mannitol or hypertonic solution External CSF drainage Ventricular catheter Ventriculo peritoneal or atrial shunt Lumbar drain Serial lumbar punctures Blood volume Brain volume n n n Mannitol or hypertonic saline Decompressive craniectomy Resection of tumor or other mass lesion n n Seizure Control Mannitol or hypertonic saline Hyperventilation Hypothermia Head elevation, neutral neck position Deep propofol or barbiturate sedation ± paralysis
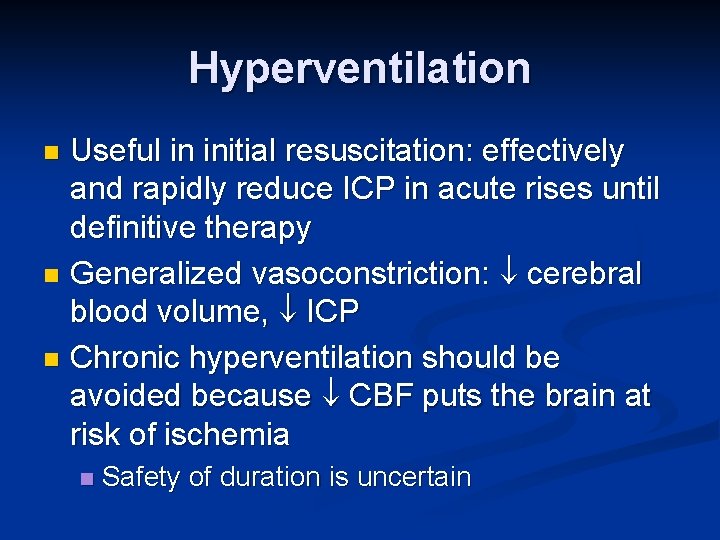
Hyperventilation Useful in initial resuscitation: effectively and rapidly reduce ICP in acute rises until definitive therapy n Generalized vasoconstriction: cerebral blood volume, ICP n Chronic hyperventilation should be avoided because CBF puts the brain at risk of ischemia n n Safety of duration is uncertain
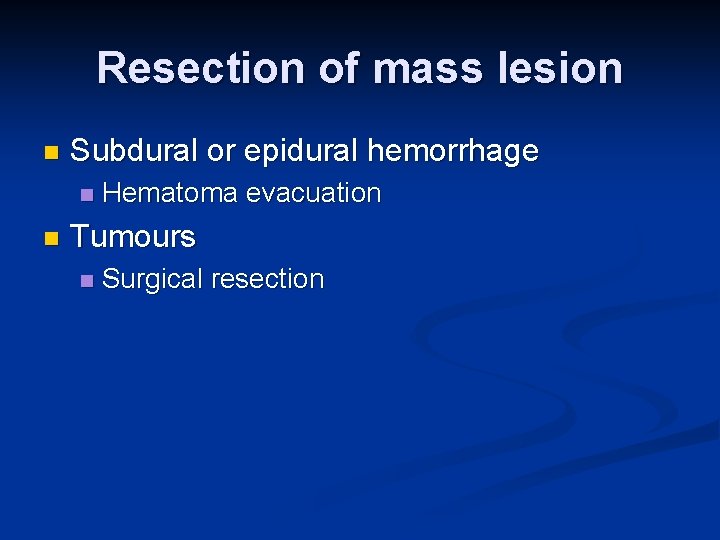
Resection of mass lesion n Subdural or epidural hemorrhage n n Hematoma evacuation Tumours n Surgical resection
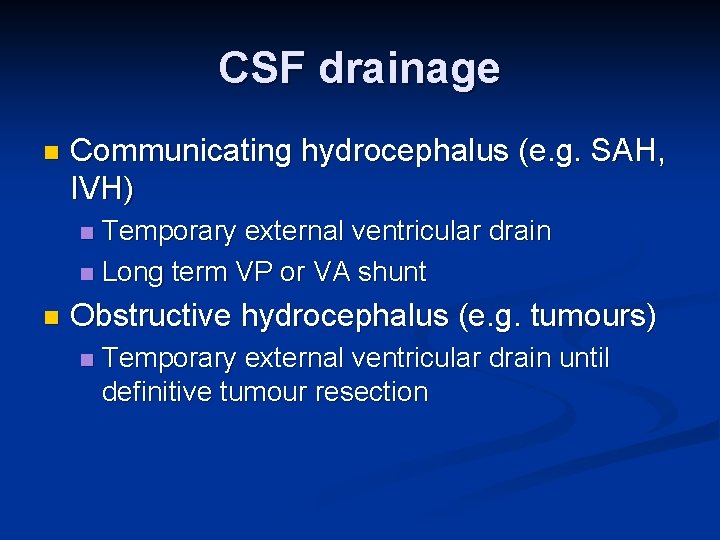
CSF drainage n Communicating hydrocephalus (e. g. SAH, IVH) Temporary external ventricular drain n Long term VP or VA shunt n n Obstructive hydrocephalus (e. g. tumours) n Temporary external ventricular drain until definitive tumour resection
Head elevation Head of bed at 20 to 30 is optimizes cerebral venous return n Ensure neutral neck position n Caution in hypovolemic patients to avoid reduction in MAP and therefore CPP n n CPP = MAP – ICP
Paralysis, Sedation, Hypothermia n To prevent excess motor activity (posturing, n n coughing, straining against ventilator) To cerebral metabolic rate and CBF (must maintain MAP to improve CPP caution in HD unstable patients) Role of EEG n n n Rule out ongoing seizure activity Titration of sedation with goal of achieving burst suppression Hypothermia, controversial n n Attenuates deleterious biochemical cascade cerebral metabolic rate
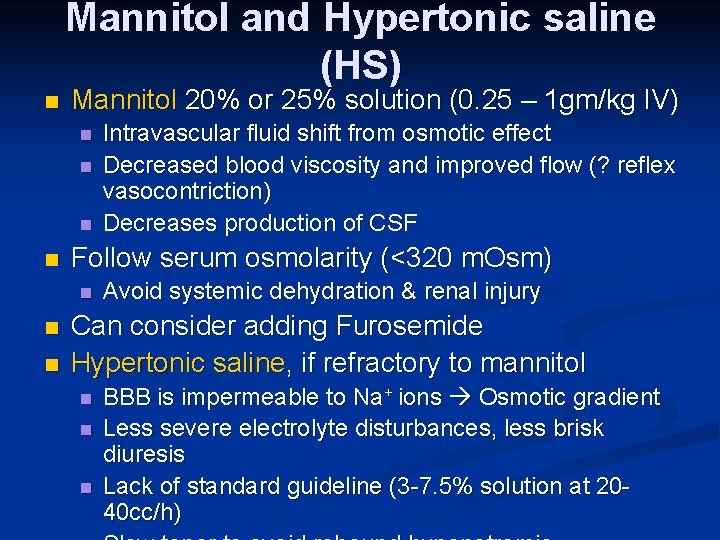
Mannitol and Hypertonic saline (HS) n Mannitol 20% or 25% solution (0. 25 – 1 gm/kg IV) n n Follow serum osmolarity (<320 m. Osm) n n n Intravascular fluid shift from osmotic effect Decreased blood viscosity and improved flow (? reflex vasocontriction) Decreases production of CSF Avoid systemic dehydration & renal injury Can consider adding Furosemide Hypertonic saline, if refractory to mannitol n n n BBB is impermeable to Na+ ions Osmotic gradient Less severe electrolyte disturbances, less brisk diuresis Lack of standard guideline (3 -7. 5% solution at 2040 cc/h)
Decompressive craniectomy Surgical removal of cranial bone flap to relieve intracranial pressure n Useful in large ischemic CVA with profound edema n Role in traumatic brain injury still needs to be established n
Conclusions ICH has an increasing incidence, but continues to have a very poor prognosis n Hypertension is a major risk factor n Acute BP reduction of 15 -20% is safe n Anticoagulation should be reversed ASAP n Absolute indications for ICP monitoring n Major categories of increased ICP management n

Thank you!
References n n n Goldstein, JN et al. Contrast extravasation on CT angiography predicts hematoma expansion in intracerebral hemorrhage, Neurology 2007; 68: 889– 894 Qureshi AI et al. Intracerebral hemorrhage, Lancet 2009; 373: 1632– 44 Wada, R et al. CT Angiography “Spot Sign” Predicts Hematoma Expansion in Acute Intracerebral Hemorrhage, Stroke 2007; 38: 1257 -1262 Diringer MN. Update on intracerebral hemorrhage, AAN Continuum, 2009 Kincaid MS and Lam AM, Monitoring and managing ICP, AAN Continuum, 2006