Intracerebral Hemorrhage ICH Krishna Nalleballe MD Acute Management
Intracerebral Hemorrhage (ICH) Krishna Nalleballe MD
Acute Management of ICH • Predicting hematoma expansion • Preventing hematoma expansion • • Blood pressure control Reversing INR Platelet transfusion? Metabolic • Monitoring for complications of ICH • • Seizures Hydrocephalus
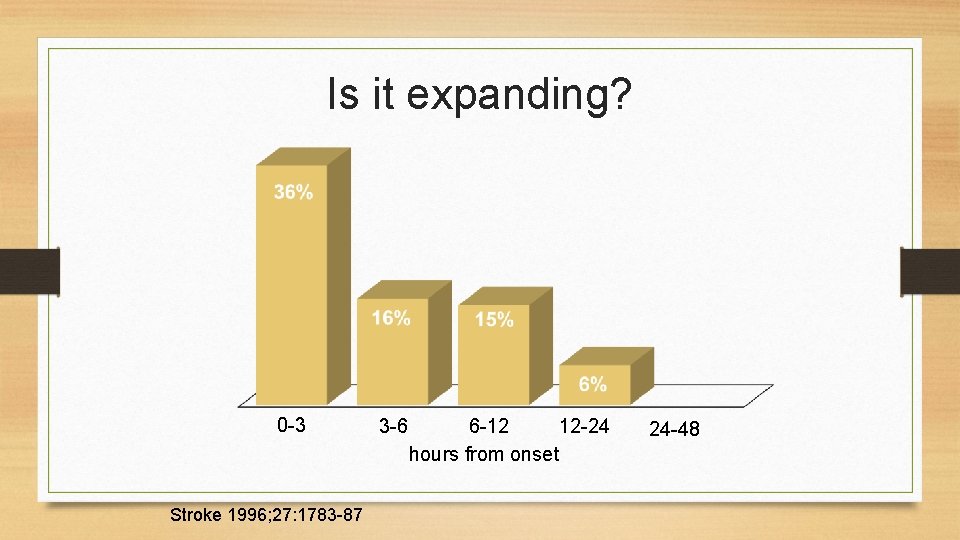
Is it expanding? 0 -3 Stroke 1996; 27: 1783 -87 3 -6 6 -12 12 -24 hours from onset 24 -48
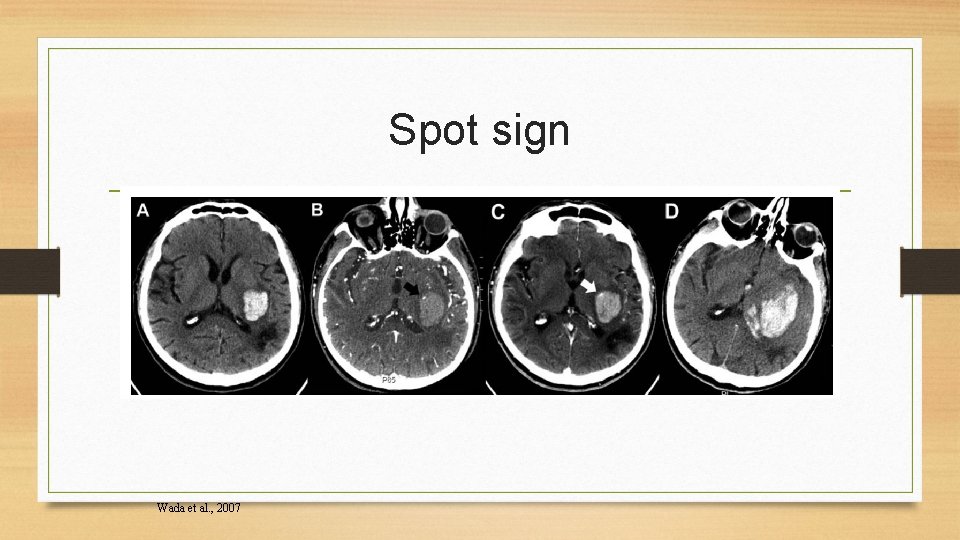
Spot sign Wada et al. , 2007
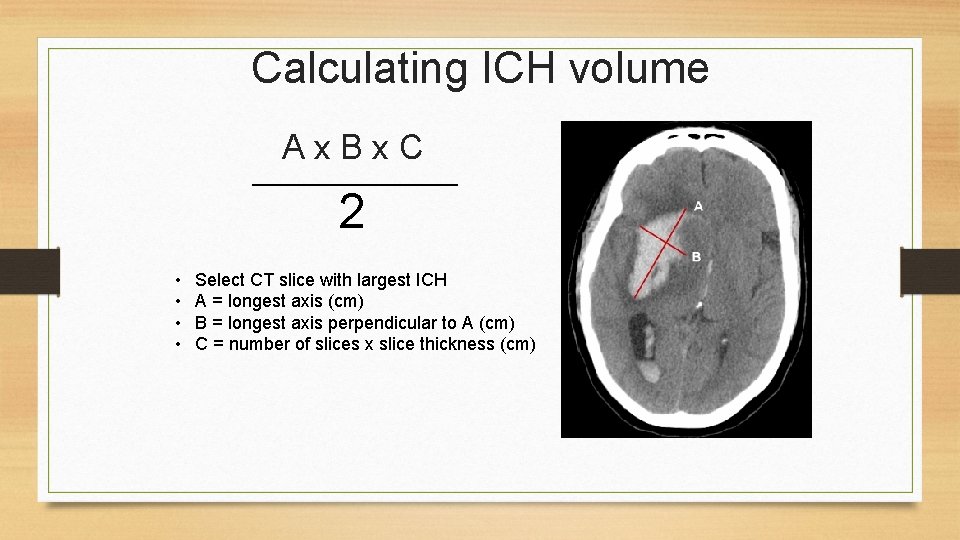
Calculating ICH volume A x B x C 2 • • Select CT slice with largest ICH A = longest axis (cm) B = longest axis perpendicular to A (cm) C = number of slices x slice thickness (cm)

ICH score ICH volume > 30 cc < 30 cc 1 0 Yes No 1 0 Intraventricular extension Infratentorial location Yes No 1 0 > 80 < 80 1 0 3 -4 5 -12 13 -15 2 1 0 0 -6 Age Glasgow coma scale Total score Godoy, D. A. et al. Stroke 2006 Score 30 -day mortality 0 0% 1 13 2 26 3 72 4 97 5, 6 100
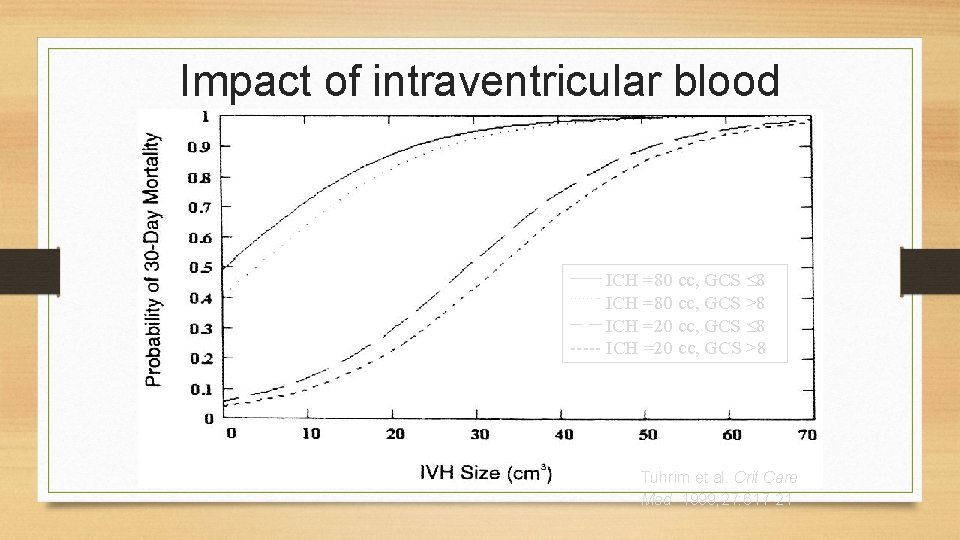
Impact of intraventricular blood _____ ICH =80 cc, GCS 8 ICH =80 cc, GCS >8 __ __ ICH =20 cc, GCS 8 ----- ICH =20 cc, GCS >8 ……. . Tuhrim et al. Crit Care Med 1999; 27: 617 -21

Preventing hematoma expansion • • Blood pressure control Reversing INR ? Platelet transfusion Metabolic
Preventing Hematoma Expansion • Blood Pressure Control
Target blood pressure 140 systolic? INTERACT 2 trial • Patients within 6 hours of onset of ICH • Treatment arm: SBP <140 • Control arm: SBP <180
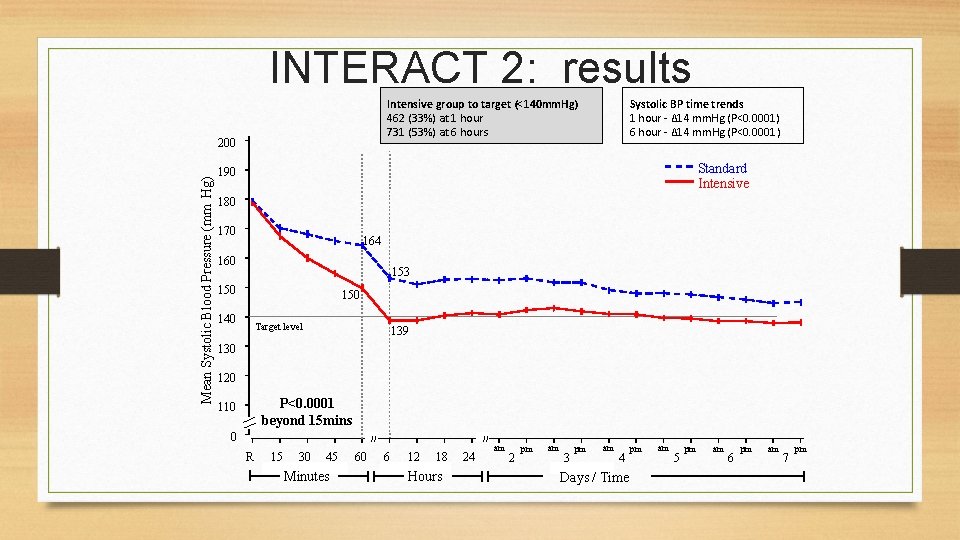
INTERACT 2: results Intensive group to target (<140 mm. Hg) 462 (33%) at 1 hour 731 (53%) at 6 hours Mean Systolic Blood Pressure (mm Hg) 200 Systolic BP time trends 1 hour - Δ 14 mm. Hg (P<0. 0001) 6 hour - Δ 14 mm. Hg (P<0. 0001) Standard Intensive 190 180 170 164 160 153 150 140 Target level 139 130 120 P<0. 0001 beyond 15 mins 110 0 // R 15 30 45 Minutes 60 // 6 12 18 Hours 24 am 2 pm am 3 pm am 4 Days / Time pm am 5 pm am 6 pm am 7 pm
INTERACT 2: results • No difference between groups in death or major disability • Intensive blood pressure lowering resulted in better functional outcomes at 90 days than standard therapy

BP Control • AHA Statement: • For ICH patients presenting with SBP between 150 -220 mm Hg and with out contraindication to acute BP treatment, lowering of SBP to 140 mm Hg is safe (class 1; Level of Evidence A) and can be effective for improving functional out come (class 2 a; Level of Evidence B) • For ICH patients presenting with SBP>220 mm Hg, it may be reasonable to consider aggressive reduction of BP with a continuous intravenous infusion and frequent BP monitoring (class 2 a; Level of Evidence C)

Preventing Hematoma Expansion • Reversing Anticoagulation

Reversing the INR • • • No more fresh frozen plasma Choose prothrombin complex concentrate Kcentra Vitamin K dependent coagulation factors II, VII, IX, X and protein C+S Give vitamin K IV along with it

Kcentra vs. FFP • Patients with INR ≥ 2 requiring reversal of INR for an acute major bleeding event • Primary endpoints: • Hemostatic efficacy within 24 hours of the infusion (excellent, good, poor, none) • INR half hour after the infusion

Results • Effective hemostasis in 72. 4% of the 4 -factor PCC group vs. 65. 4% of the FFP group • PCC non-inferior to FFP • INR ≤ 1. 3 at half an hour after the end of the infusion in 62. 2% of the PCC group vs. 9. 6% of the FFP group • PCC superior to FFP

Adverse events • Kcentra • ischemic stroke • DVT • FFP • 2 MIs • fluid overload • respiratory failure

Advantages of PCC • Less volume • Rapid reversal of the INR to less than 1. 3 within 30 minutes • Rapid infusion rate – 8. 4 m. L/minute

Kcentra dose Usually 25 units/ m. L Therefore 3500 units = 140 m. L FFP would have been 1050 m. L (15 m. L/kg)

Reversal • AHA Statement: • Patients with ICH whose INR is elevated because of VKA should have their VKA withheld, receive therapy to replace vitamin Kdependent factors and correct the INR and receive intravenous vitamin K (class 1; Level of Evidence C). • PCCs may have fewer complications and correct the INR more rapidly than FFP and might be considered over FFP (class 2 b; Level of Evidence B) • r. F 7 a does not replace all clotting factors and so is not recommended
NOAC • AHA Statement: • For patients with ICH who are taking dabigatran, rivaroxaban, or apixaban, treatment with FEIBA, other PCCs, or r. F 7 a might be considered on an individual basis. Activated charcoal might be used if most recent dose was taken <2 hours earlier. • FEIBA is anti-inhibitor coagulant complex used approved for hemophilia • Praxbind is Idarucizumab is humanized monoclonal ab , 5 g IV (2 doses of 2. 5 gms, no more than 15 mins apart)

Heparin • AHA Statement: • Protamine Sulfate may be considered to reverse heparin in patients with acute ICH (Class 2 b; Level of Evidence C)

AHA guidelines: ICH on heparin • Protamine sulfate 1 mg per 100 units heparin • Dose decreases depending on time since IV heparin was stopped • 30 -60 min: • 60 -120 min: • >120 min: 0. 5 -0. 75 mg/100 units heparin 0. 375 -0. 5 mg/100 units heparin 0. 25 mg/100 units heparin • Slow IV infusion, max rate 5 mg/min (high risk of severe hypotension if faster)

Preventing Hematoma Expansion • Platelet Transfusion

Platelet transfusion for ASA use? • 282 ICH cases imaged at onset and at 72 hours, including 70 (25%) taking antiplatelet medication • No difference in baseline hematoma volume • No difference in hematoma growth at 72 hours • No difference in need for surgical evacuation • No difference in Rankin score at 90 days • No difference in mortality
Platelet Transfusion • AHA Statement: • The usefulness of platelet transfusions in ICH patients with a history of antiplatelet use is uncertain (class 2 b: Level of Evidence C) • Patients with a severe coagulation factor deficiency or severe thrombocytopenia should receive appropriate factor replacement therapy or platelets, respectively (class 1; Level of Evidence C)

Factor VII for acute ICH • Used for hemophiliacs with Factor VIII antibodies • FAST Trial • • Phase 3 trial of Factor VII for acute ICH (not on warfarin) Primary outcome: severe disability or death at 90 days 821 patients randomized to placebo, 20, or 80 mcg/kg Treatment started within 4 hours of onset NEJM 2008; 358: 2127 -2137

Factor VII reduced ICH growth • Reduced ICH growth with 80 mcg/kg vs placebo • Time mattered: earlier treatment => less growth
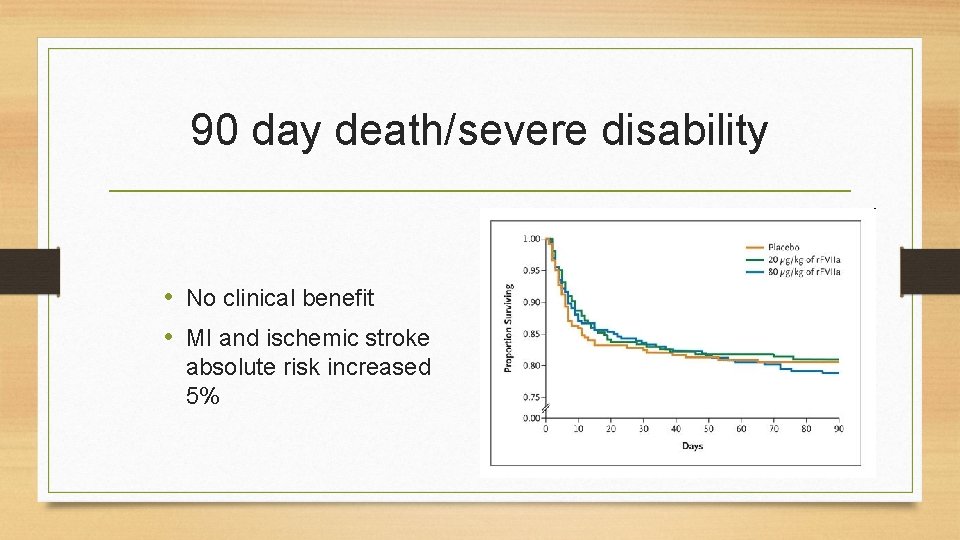
90 day death/severe disability • No clinical benefit • MI and ischemic stroke absolute risk increased 5%

Factor 7 • AHA Statement: • Although rfactor 7 a can limit the extent of hematoma expansion in noncoagulopathic ICH patients, there is an increase in thromboembolic risk with r. F 7 a and no clear clinical benefit in unselected patients. This r. F 7 a is not recommended (class 3; Level of Evidence A)

Preventing Hematoma Expansion • Metabolic

Metabolic • Glucose should be monitored. Both hyperglycemia and hypoglycemia should be avoided (class 1; Level C) • Treatment of fever after ICH may be reasonable (class 2 b; Level C) • Systemic screening for MI with ECG and cardiac enzyme testing after ICH is reasonable (class 2 a; Level C) • A formal dysphagia screen should be performed in all patients before initiating oral intake to reduce pneumonia risk (class 1; Level B)
Complications of ICH • Seizures • Hydrocephalus • DVT/PE

Seizures • Prophylactic antiseizure medication is not recommended (class 3; Level B) • Clinical Seizures should be treated with antiseizure meds (Class 1; Level A) • Continuous EEG monitoring is probably indicated in ICH patients with depressed mental status that’s out of proportion to degree of brain injury (Class 2 a; Level C) and should be treated with antiseizure meds if found to have electrographic seizures on EEG (class 1; Level C)

Hydrocephalus

Clinical manifestations of Hydrocephalus • Headache • Vomiting • Drowsiness → Coma

Indications for EVD • EVD as treatment for hydrocephalus is reasonable, esp. in patients with decreased level of consciousness (class 2 a; Level B)

Steroids for ICH: NO!!! • Single-center, double-blind randomized trial • Dexamethasone versus placebo within 48 hours of onset for 9 days total • Trial halted after enrollment of 93 patients due to high rate of complications and no clinical benefit NEJM 1987; 316: 1229 -1233
DVT • Risk of DVT in hemiplegic patients is 10 -50% during acute hospitalization • Intermittent pneumatic compression must be used immediately (class 1; Level A) • Graduated compression stockings are not beneficial to reduce DVT or improve out comes (class 3; Level A) • After 1 -4 days from onset LMW heparin or unfractionated heparin.
Intraventricular Hemorrhage • Although intraventricular administration of rt. PA in IVH appears to have a fairly low complication rate, the efficacy and safety of this treatment are uncertain (class 2 b; Level B) • The efficacy of endoscopic treatment of IVH is uncertain (class 2 b; Level B)
STICH Trial • Multicenter international randomized trial of early surgery versus medical management for ICH • Crossover to surgery possible, so NOT strictly a trial of surgery versus medicine • Surgeon uncertain about benefit of surgery • Randomization within 72 hours of ICH; surgery within 24 hours of randomization • Supratentorial ICH only • 1033 patients randomized Mendelow et al. Lancet 2005

STICH Results

Surgery • Patients with cerebellar hemorrhage who are deteriorating neurologically or have brain stem compression or hydrocephalus should under go surgical removal as soon as possible (class 1; Level C) • Initial treatment of these patients with ventricular drainage rather than surgical evacuation is not recommended (class 3; Level C) • For most patients with supratentorial ICH, usefulness of surgery is not well established (class 2 b; Level A)

Surgery • Policy of early hematoma evacuation is not clearly beneficial compared to hematoma evacuation when patient deteriorates (Class 2 b; Level A)


Deep ICH is like lacunar infarct • Deep ICH occurs in: • Basal ganglia and thalamus • Pons • Cerebellum • Pathology is similar to lacunar infarct • Lipohyalinosis • Charcot-Bouchard aneurysms—may be artifactual • After deep ICH, annual risk of recurrence is: Neurology 2001; 56: 773 -777 2. 1%

Cerebral amyloid angiopathy • The most common risk factor for lobar ICH • Infiltration of cortical vessels by amyloid protein • Probable CAA: age>55 with recurrent lobar ICH • After a first lobar ICH, the 2 -year cumulative incidence of a second ICH is… 21% N Engl J Med 2000; 342: 240 -245

CAA-Boston Diagnostic Criteria

ICH 30 -Day Mortality: 30 -50%
Restarting AC • Avoidance of long term AC as treatment for nonvalvular afib is probably recommended after AC associated spontaneous lobar ICH due to relatively high risk of recurrence (class 2 a; Level B) • AC after nonlobar ICH and antiplatelet therapy after an ICH might be considered, particularly when there is strong indication (class 2 b; Level B) • Optimal timing to resume AC after ICH is uncertain. Avoidance of AC for at least 4 weeks in patients with out mechanical valves, might decrease ICH recurrence (class 2 b; Level B)

Table 9 -1 Copyright © 2017 American Academy of Neurology 52
References • Anderson et al. Rapid blood pressure lowering in patients with acute intracerebral hemorrhage. NEJM. 2013; 368: 2355 -65. • Kazui et al. Enlargement of spontaneous intracerebral hemorrhage. Stroke. 1996; 27(10): 1783 -87. • Morgenstern et al. Guidelines for the management of spontaneous intracerebral hemorrhage. Stroke. 2010; 41: 2108 -2129. • Sarode et al. Efficacy and safety of a 4 -factor PCC in patients on vitamin K antagonists presenting with major bleeding. Circulation. 2013; 128: 1234 -43. • Wada et al. CT angiography “spot sign” predicts hematoma expansion in acute intracerebral hemorrhage. Stroke. 2007; 38: 1257 -62.
- Slides: 53