Intracapsular Fracture Neck Femur Dr Chirag Kaspoor Consultant


- Slides: 45

Intracapsular Fracture Neck Femur Dr. Chirag Kaspoor, Consultant Orthopaedic Surgeon Dhiraj Hospital, SBKS MIRC SUMANDEEP VIDYAPEETH
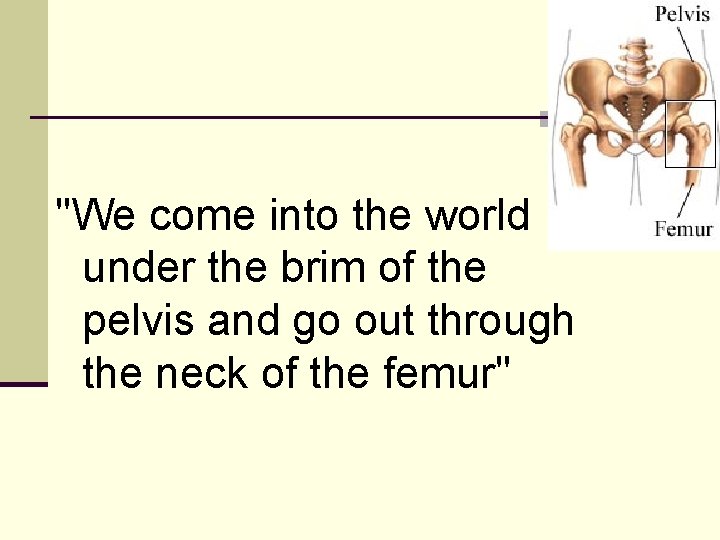
"We come into the world under the brim of the pelvis and go out through the neck of the femur"
Termed “the unsolved fracture” by Sir Astley Cooper and Sir Ambroise Paré in 1819, but the term still holds good today!
Incidence n Very high incidence among elderly population- In last decade, it was primarily a geriatric fracture n Young Population- Road accidents lead to high energy fractures
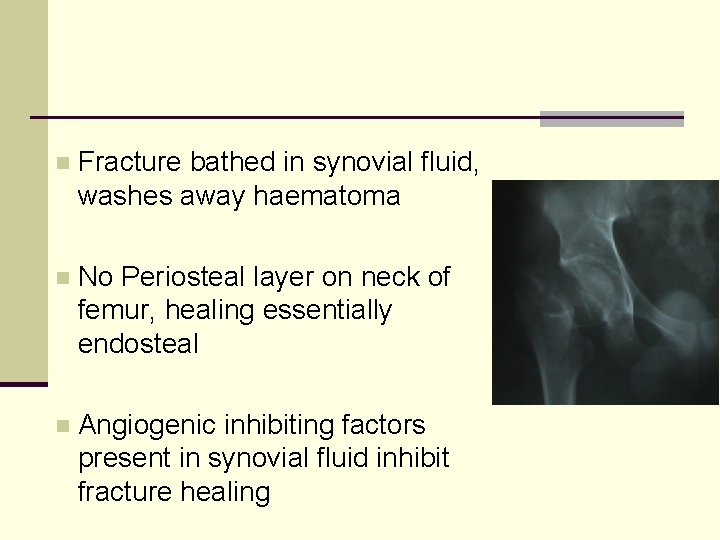
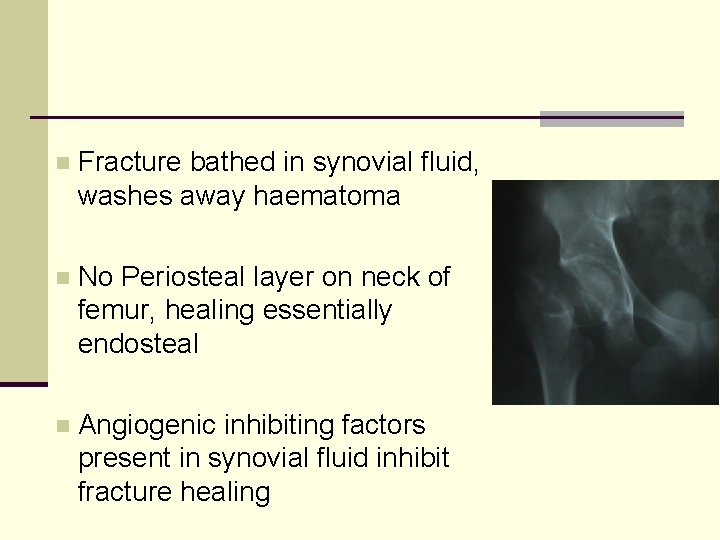
n Fracture bathed in synovial fluid, washes away haematoma n No Periosteal layer on neck of femur, healing essentially endosteal n Angiogenic inhibiting factors present in synovial fluid inhibit fracture healing
• Increased Intracapsular Pressure. • Seen in undisplaced fractures. • Kinking of arteries
Why Unsolved ? n Treatment n No consensus amongst surgeons n Avascular necrosis n High rate of delayed and nonunion
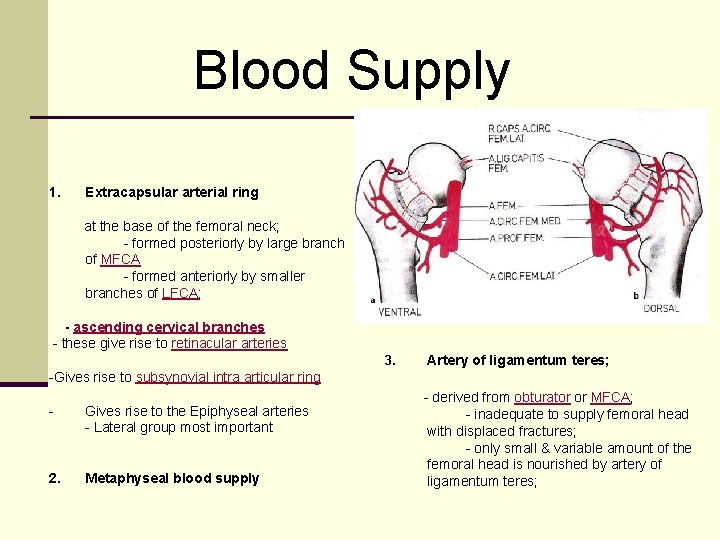
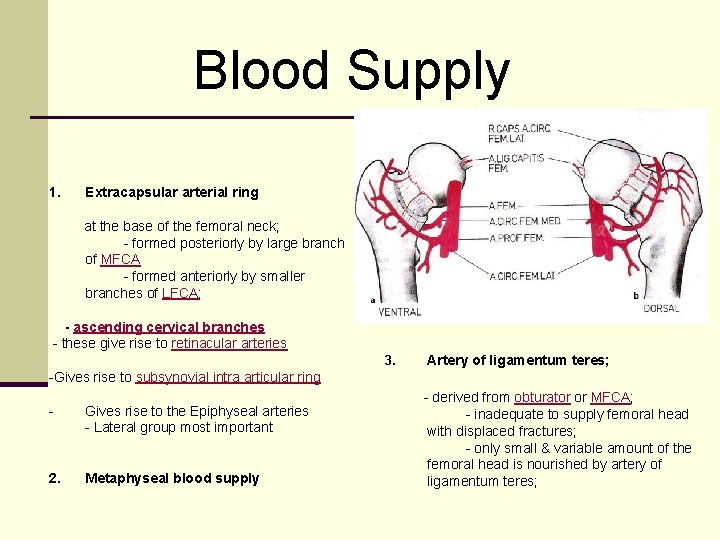
Blood Supply 1. Extracapsular arterial ring at the base of the femoral neck; - formed posteriorly by large branch of MFCA - formed anteriorly by smaller branches of LFCA; - ascending cervical branches - these give rise to retinacular arteries 3. Artery of ligamentum teres; -Gives rise to subsynovial intra articular ring - Gives rise to the Epiphyseal arteries - Lateral group most important 2. Metaphyseal blood supply - derived from obturator or MFCA; - inadequate to supply femoral head with displaced fractures; - only small & variable amount of the femoral head is nourished by artery of ligamentum teres;
Avascular Necrosis n Correlates with the extent of initial trauma & displacement of fracture n ? ? Tamponading effect of the intracapsular haemarthrosis n Can be prevented by ‘Urgent’ ( within 6 to 12 hours), ‘gentle’ reduction & rigid internal fixation
Decision Making? n Treatment decisions difficult n Dictated By n n n ‘Time since fracture’ Type of fracture Age of the Patient n n n Physiological Chronological Associated injuries in Femur/ limb n Making the right decision at the right time can make a big difference to outcome & quality of life.
Factors affecting outcome 1. Extent of injury n Amount of displacement n Amount of comminution n Compromise of blood supply 2. Adequacy of reduction 3. Adequacy of fixation
Classification n. Garden n. Pauwels n. Comprehensive
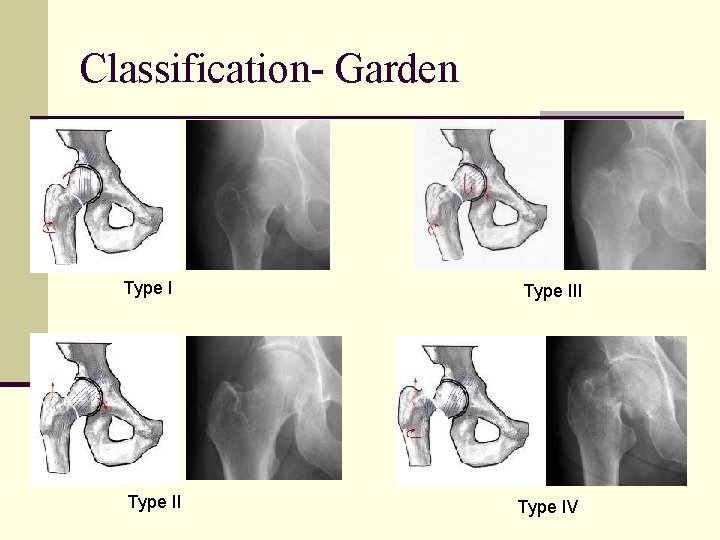
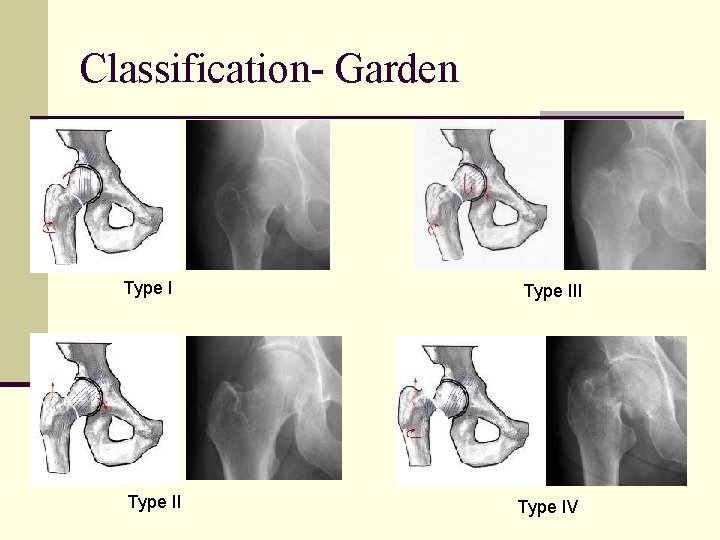
Classification- Garden Type III Type IV
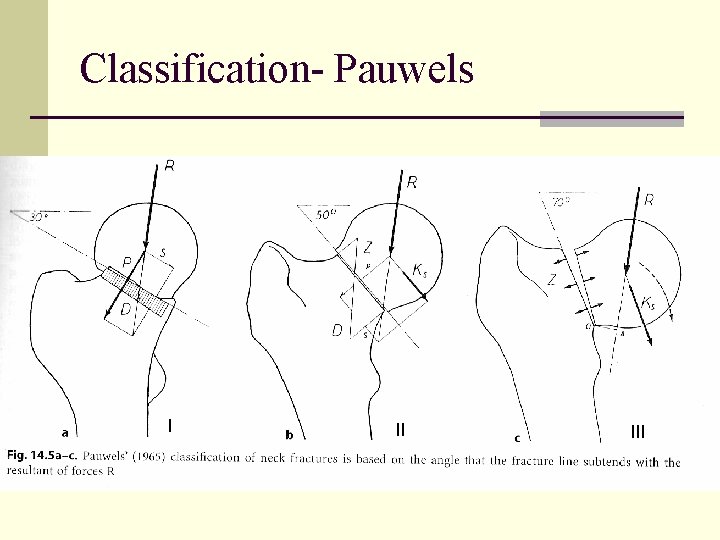
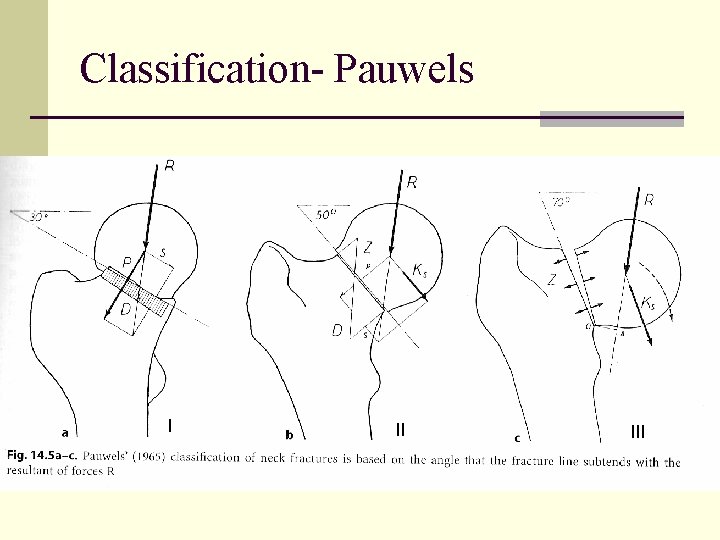
Classification- Pauwels I II III
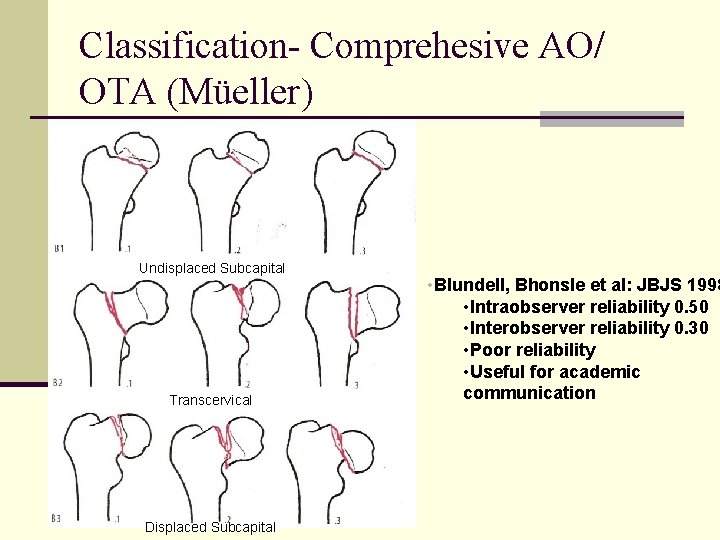
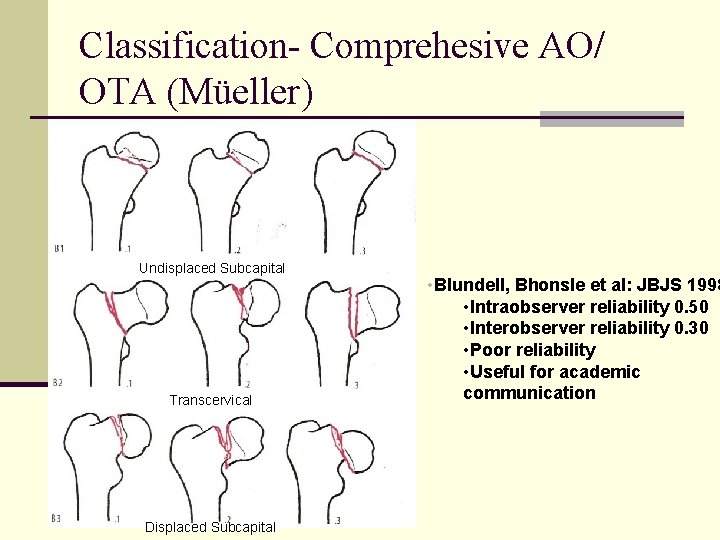
Classification- Comprehesive AO/ OTA (Müeller) Undisplaced Subcapital Transcervical Displaced Subcapital • Blundell, Bhonsle et al: JBJS 1998 • Intraobserver reliability 0. 50 • Interobserver reliability 0. 30 • Poor reliability • Useful for academic communication
Investigations n X-ray n Pelvis with Both Hips AP View n ‘Cross table’ lateral view of affected hip n MRI scan n Bone Scan
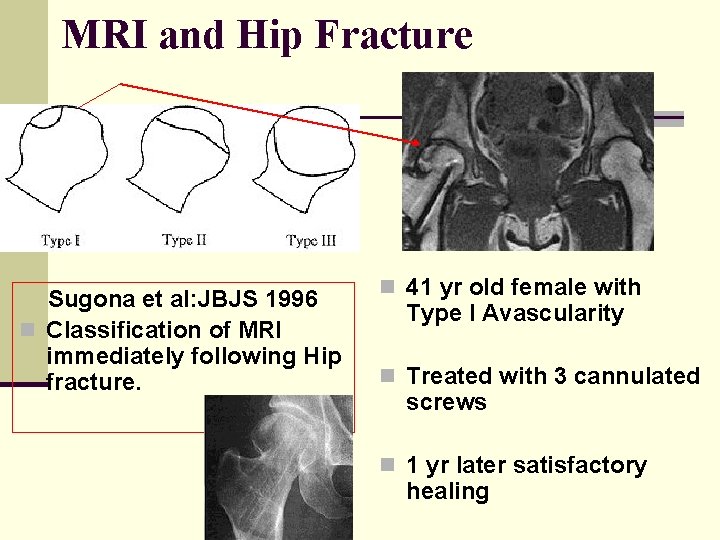
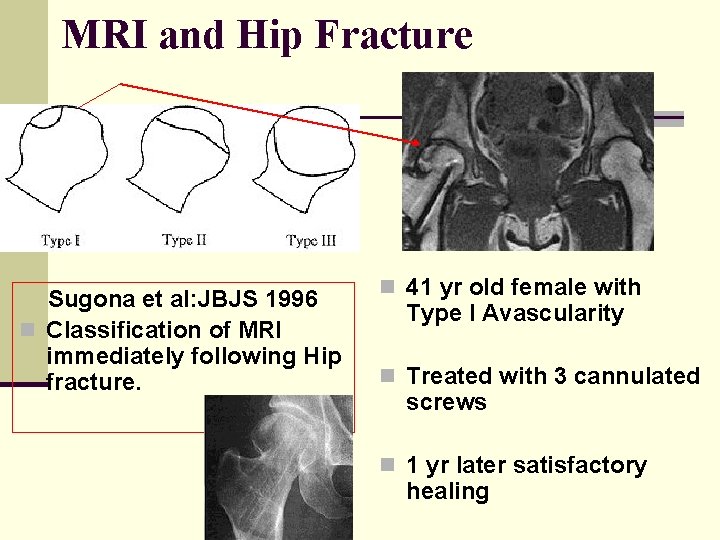
MRI and Hip Fracture Sugona et al: JBJS 1996 n Classification of MRI immediately following Hip fracture. n 41 yr old female with Type I Avascularity n Treated with 3 cannulated screws n 1 yr later satisfactory healing
Use of Bone Scan in Fracture neck Femur n Postoperative bone scan correlates with the eventual rates of AVN and non union if done within 2 weeks of fracture & again 2 months after fracture. n Decreased uptake correlates with poor outcome
-Femoral Neck Fracture -Displaced -Physiologically Young + age < 70 yrs n Goal “Rigid” fixation after anatomical reduction, no matter what extent the displacement or duration since injury. n Use Closed or open reduction, but aim to conserve the head
Reduction of the displaced fracture Closed Reduction: Leadbetter technique Affected limb flexed 90º & thigh internally rotated slightly before applying upward traction Limb circumducted into abduction & extended while maintaining internal rotation ‘Heel Palm test’ Whitman Technique Traction on limb in extension, external rotation & abduction followed by adduction & Internal rotation
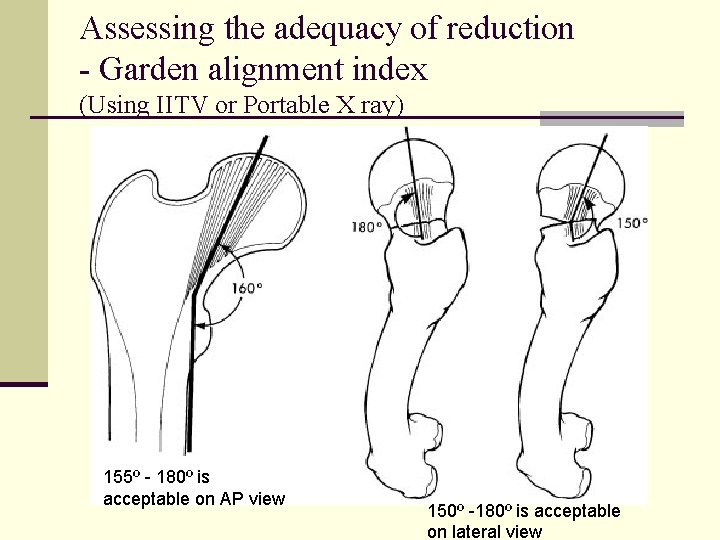
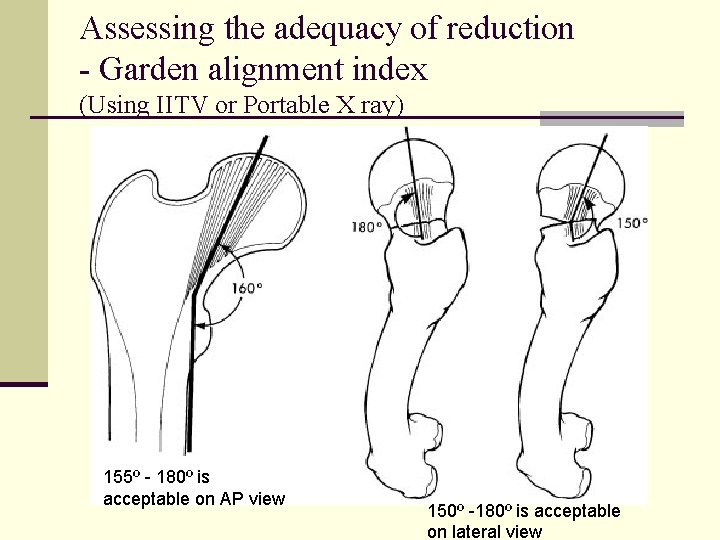
Assessing the adequacy of reduction - Garden alignment index (Using IITV or Portable X ray) 155º - 180º is acceptable on AP view 150º -180º is acceptable on lateral view
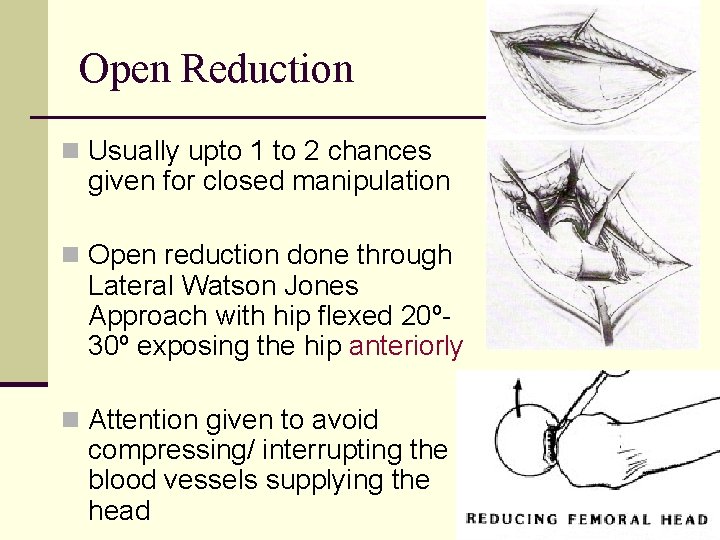
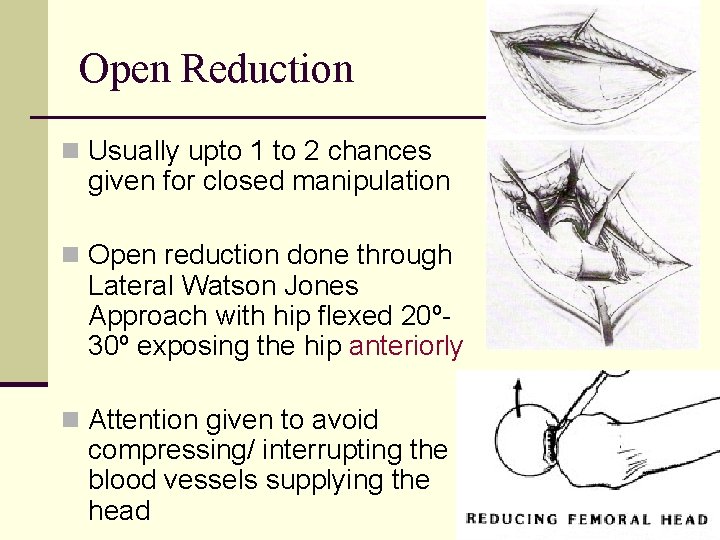
Open Reduction n Usually upto 1 to 2 chances given for closed manipulation n Open reduction done through Lateral Watson Jones Approach with hip flexed 20º 30º exposing the hip anteriorly n Attention given to avoid compressing/ interrupting the blood vessels supplying the head
Remember! Do not proceed with internal fixation UNTIL an acceptable reduction is achieved by either closed or open means.
Evolution of treatment n Langenbach first tried fixing this fracture in 1850 - patient died of Sepsis n Hey Groves- used ivory Pegs to treat Hip Fractures, same fate n König in 1875 was the first to successfully use fixation to treat fracture neck femur n Lambotte & Putti tried their own method of fixation, also met with failure
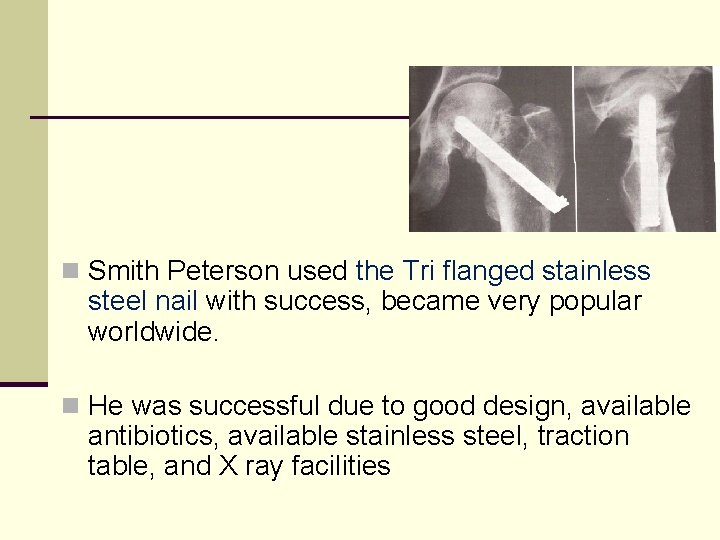
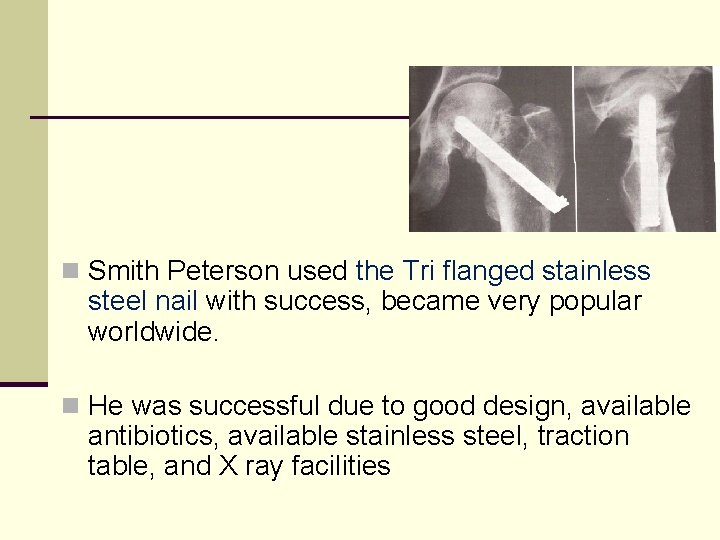
n Smith Peterson used the Tri flanged stainless steel nail with success, became very popular worldwide. n He was successful due to good design, available antibiotics, available stainless steel, traction table, and X ray facilities
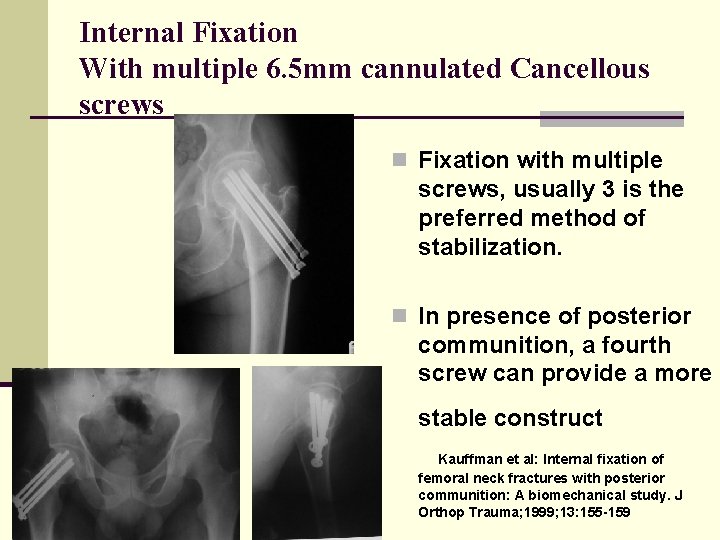
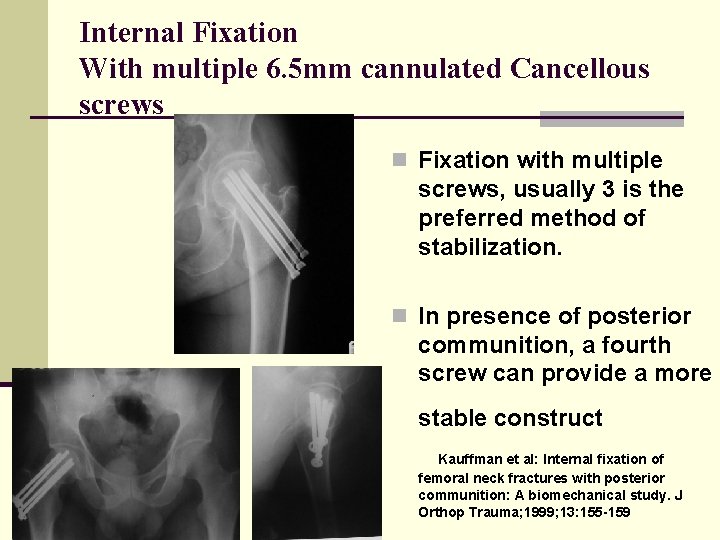
Internal Fixation With multiple 6. 5 mm cannulated Cancellous screws n Fixation with multiple screws, usually 3 is the preferred method of stabilization. n In presence of posterior communition, a fourth screw can provide a more stable construct Kauffman et al: Internal fixation of femoral neck fractures with posterior communition: A biomechanical study. J Orthop Trauma; 1999; 13: 155 -159
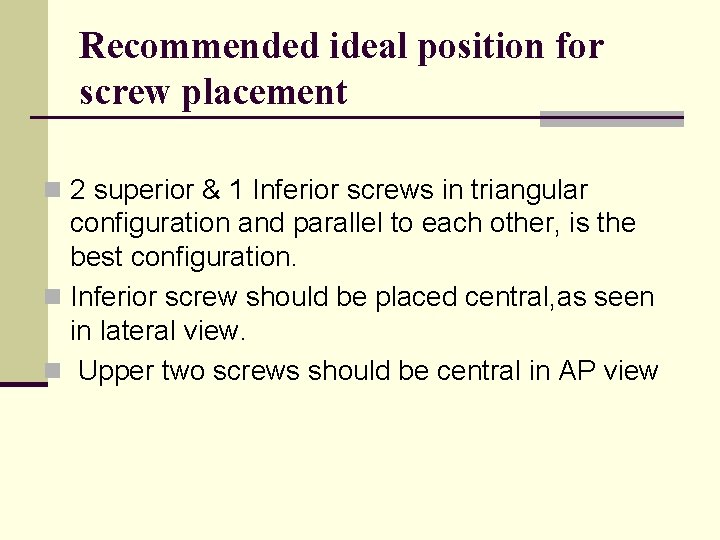
Recommended ideal position for screw placement n 2 superior & 1 Inferior screws in triangular configuration and parallel to each other, is the best configuration. n Inferior screw should be placed central, as seen in lateral view. n Upper two screws should be central in AP view
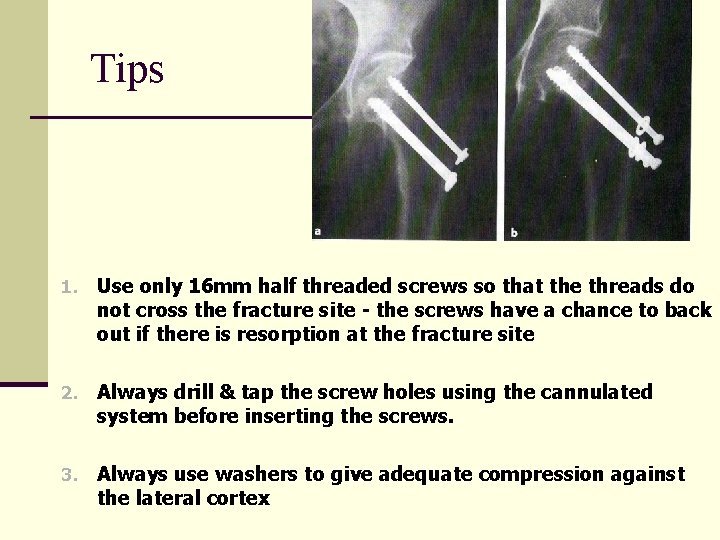
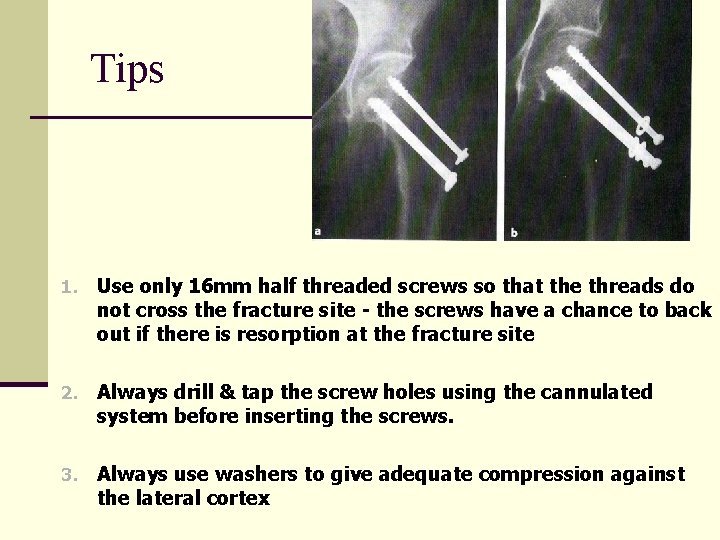
Tips 1. Use only 16 mm half threaded screws so that the threads do not cross the fracture site - the screws have a chance to back out if there is resorption at the fracture site 2. Always drill & tap the screw holes using the cannulated system before inserting the screws. 3. Always use washers to give adequate compression against the lateral cortex
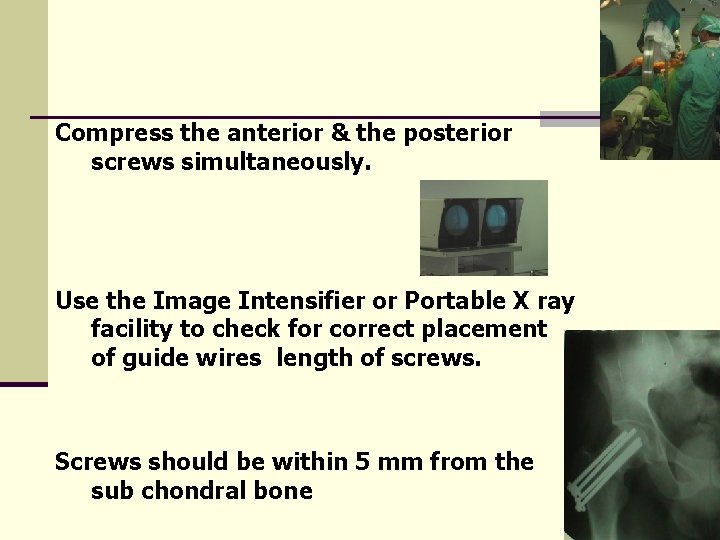
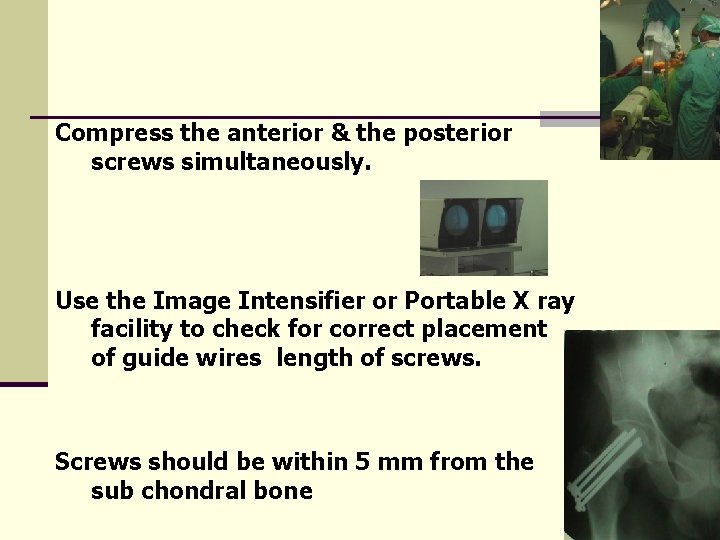
Compress the anterior & the posterior screws simultaneously. Use the Image Intensifier or Portable X ray facility to check for correct placement of guide wires length of screws. Screws should be within 5 mm from the sub chondral bone
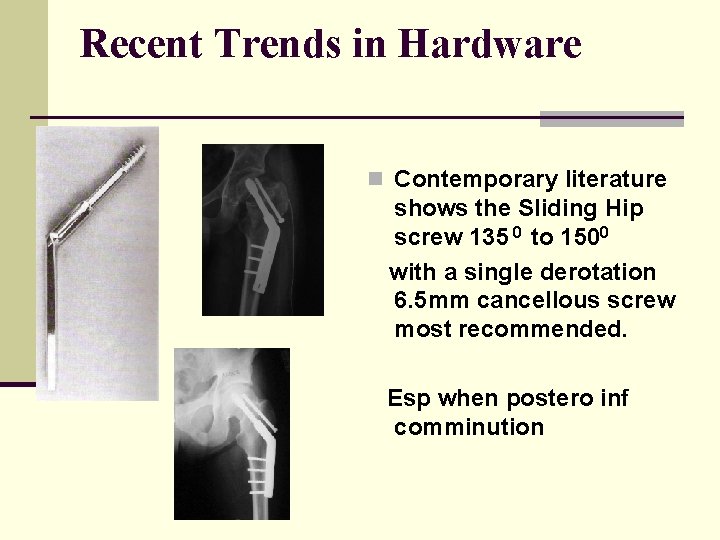
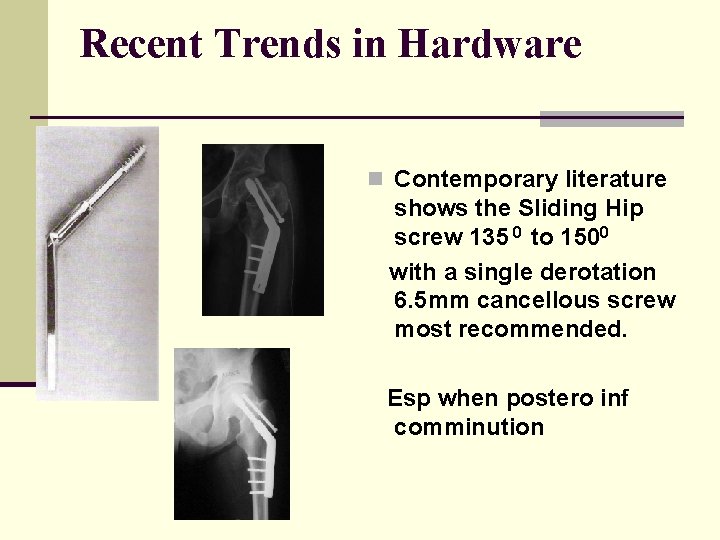
Recent Trends in Hardware n Contemporary literature shows the Sliding Hip screw 135 0 to 1500 with a single derotation 6. 5 mm cancellous screw most recommended. Esp when postero inf comminution
Delayed Presentation- Aim n Augment Vascularity n Abduction Osteotomy
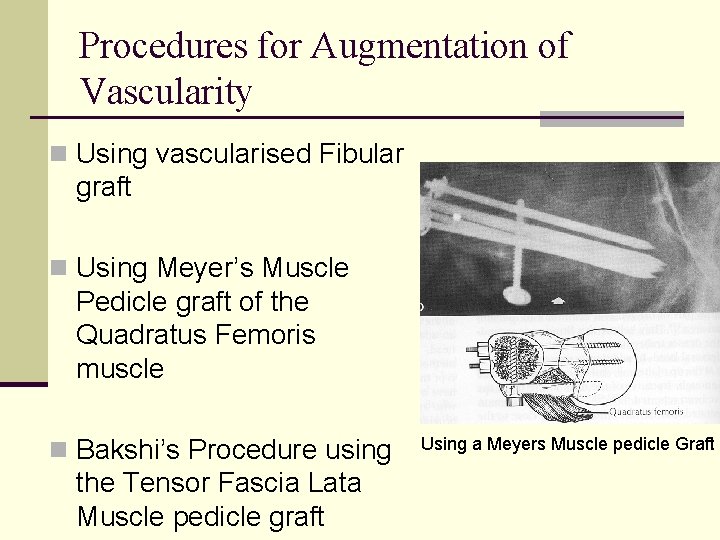
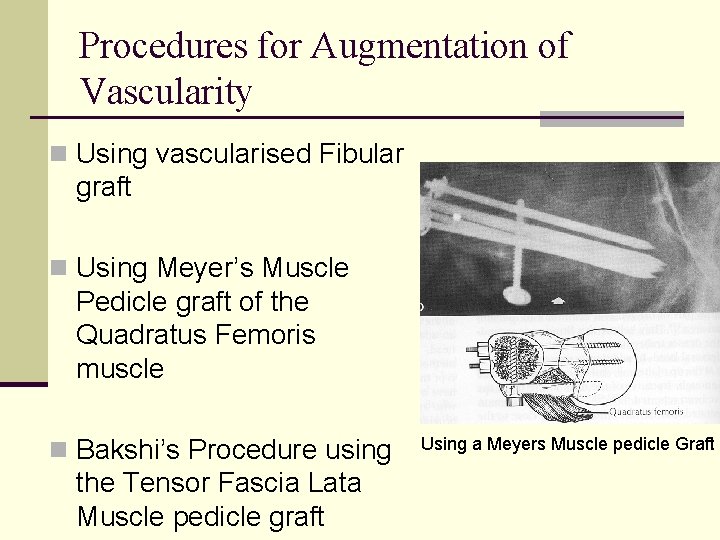
Procedures for Augmentation of Vascularity n Using vascularised Fibular graft n Using Meyer’s Muscle Pedicle graft of the Quadratus Femoris muscle n Bakshi’s Procedure using the Tensor Fascia Lata Muscle pedicle graft Using a Meyers Muscle pedicle Graft
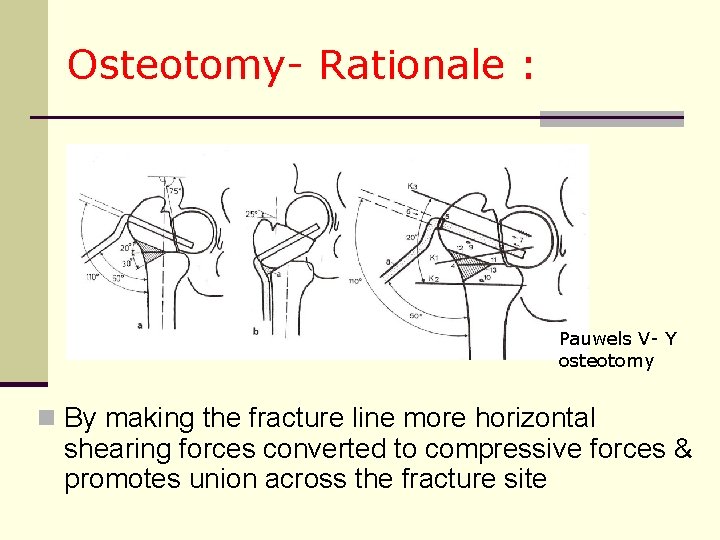
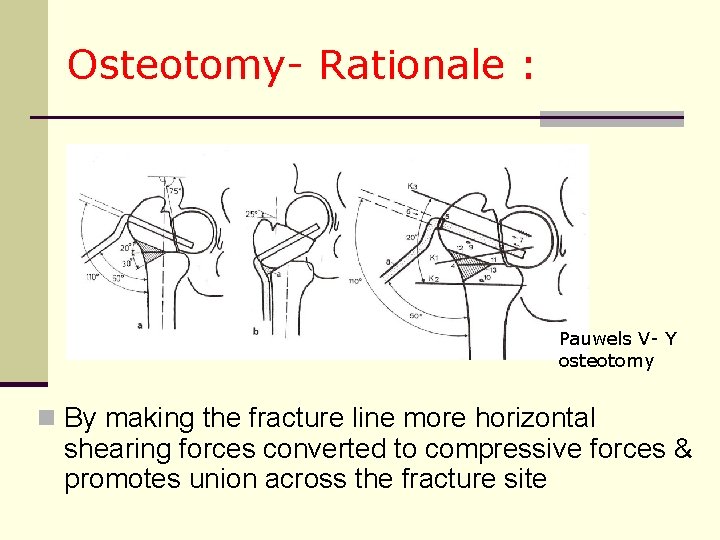
Osteotomy- Rationale : Pauwels V- Y osteotomy n By making the fracture line more horizontal shearing forces converted to compressive forces & promotes union across the fracture site
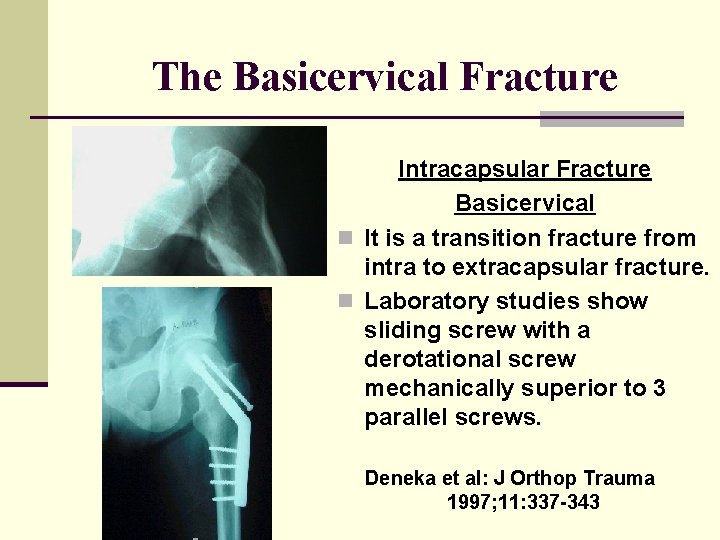
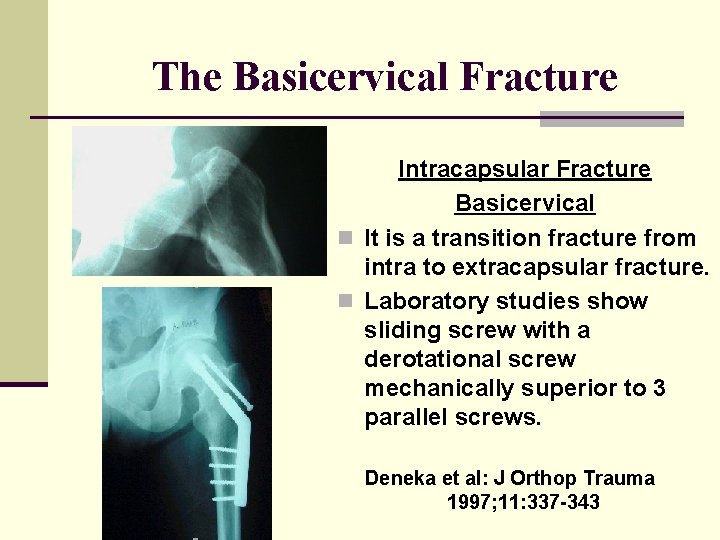
The Basicervical Fracture Intracapsular Fracture Basicervical n It is a transition fracture from intra to extracapsular fracture. n Laboratory studies show sliding screw with a derotational screw mechanically superior to 3 parallel screws. Deneka et al: J Orthop Trauma 1997; 11: 337 -343
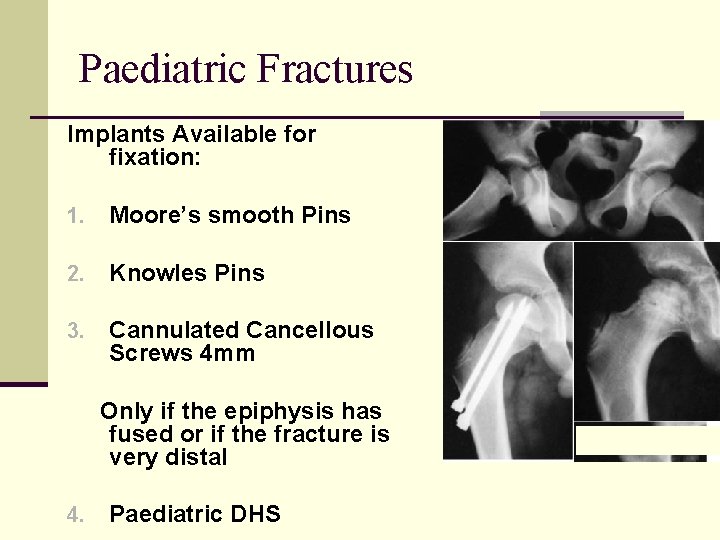
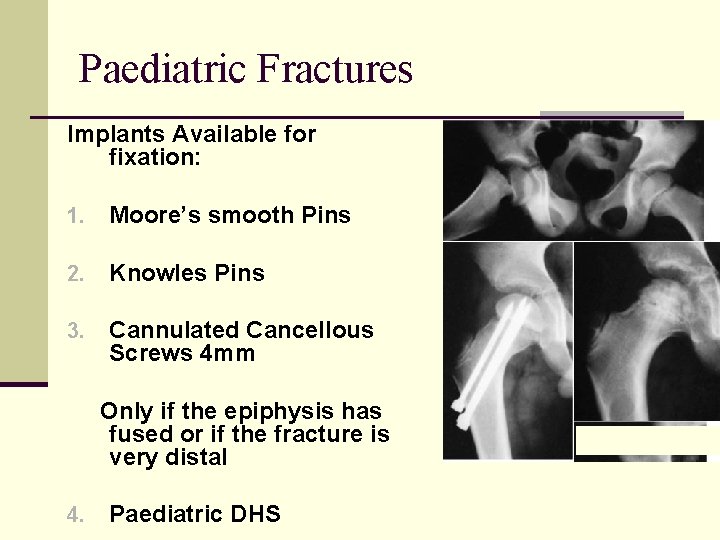
Paediatric Fractures Implants Available for fixation: 1. Moore’s smooth Pins 2. Knowles Pins 3. Cannulated Cancellous Screws 4 mm Only if the epiphysis has fused or if the fracture is very distal 4. Paediatric DHS
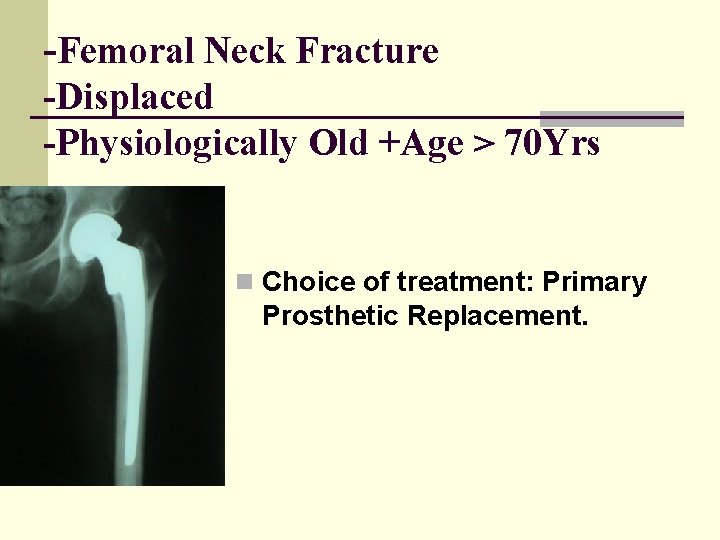
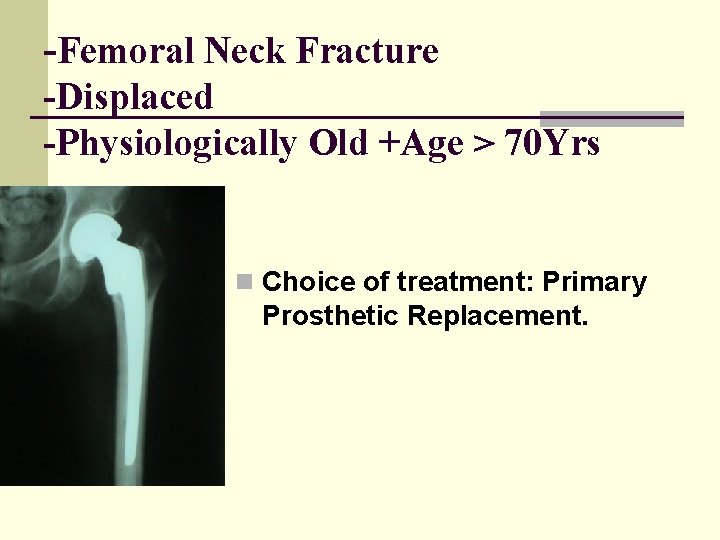
-Femoral Neck Fracture -Displaced -Physiologically Old +Age > 70 Yrs n Choice of treatment: Primary Prosthetic Replacement.
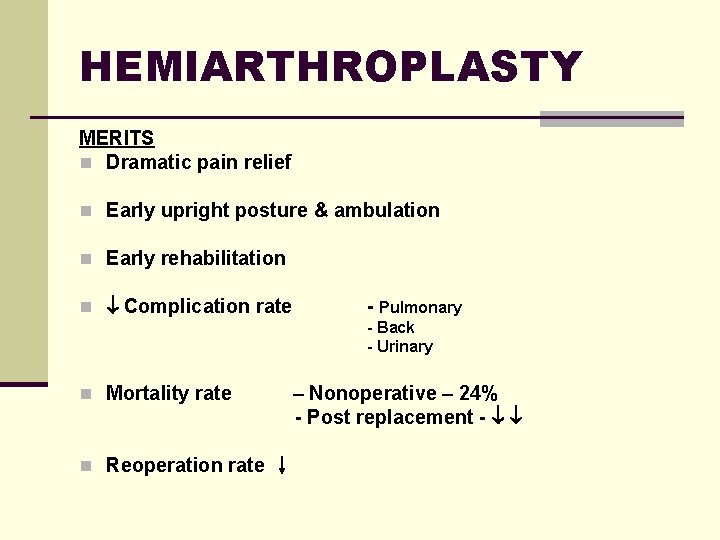
HEMIARTHROPLASTY MERITS n Dramatic pain relief n Early upright posture & ambulation n Early rehabilitation n Complication rate - Pulmonary - Back - Urinary n Mortality rate n Reoperation rate – Nonoperative – 24% - Post replacement -
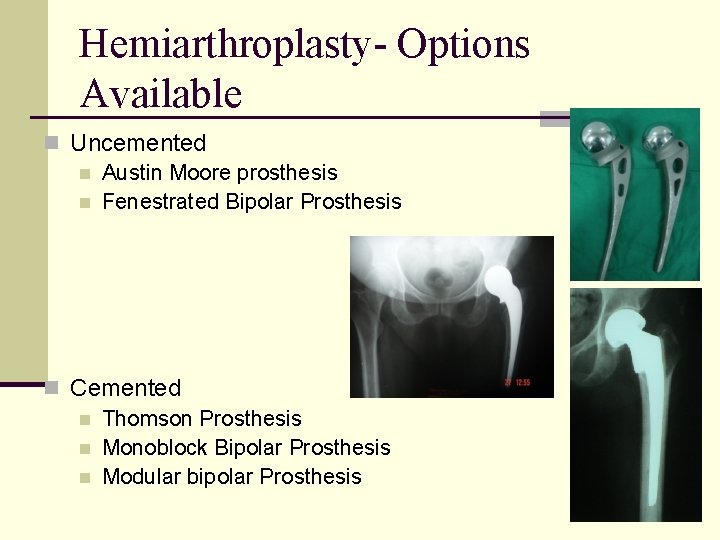
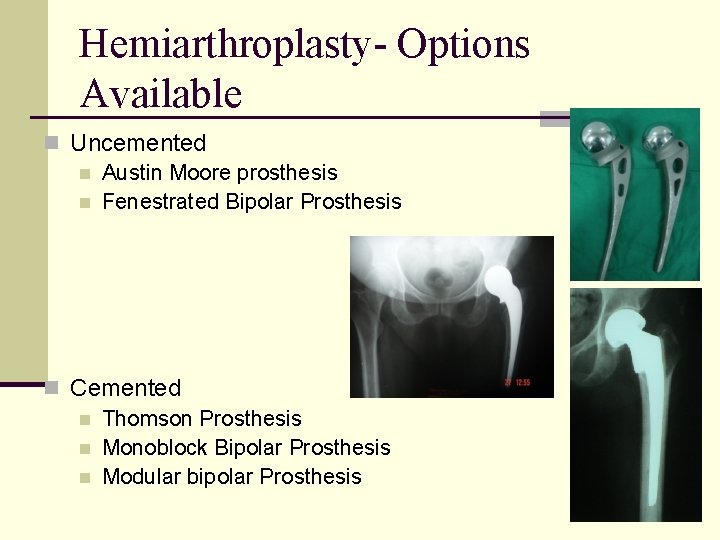
Hemiarthroplasty- Options Available n Uncemented n Austin Moore prosthesis n Fenestrated Bipolar Prosthesis n Cemented n Thomson Prosthesis n Monoblock Bipolar Prosthesis n Modular bipolar Prosthesis
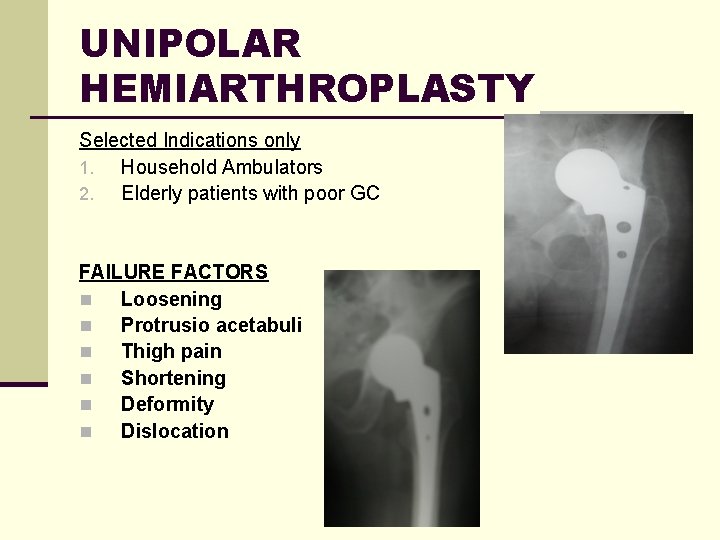
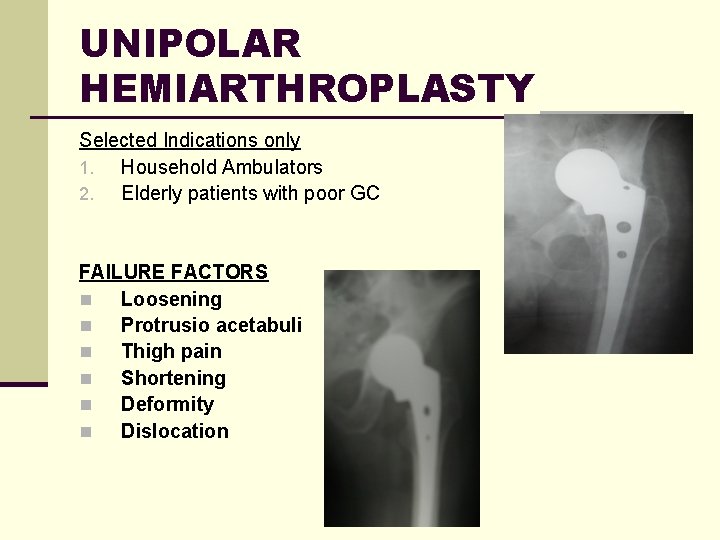
UNIPOLAR HEMIARTHROPLASTY Selected Indications only 1. Household Ambulators 2. Elderly patients with poor GC FAILURE FACTORS n Loosening n Protrusio acetabuli n Thigh pain n Shortening n Deformity n Dislocation
Bipolar Hip Arthroplasty n Less pain n Increased range of motion n Minimal erosion and protrusion
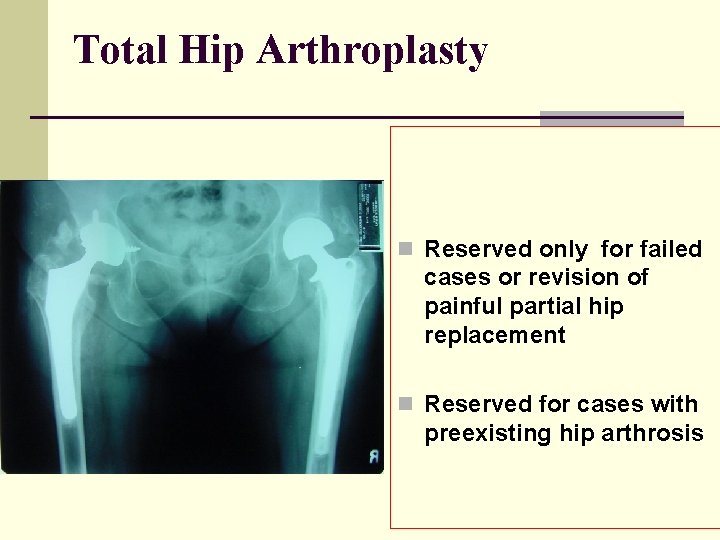
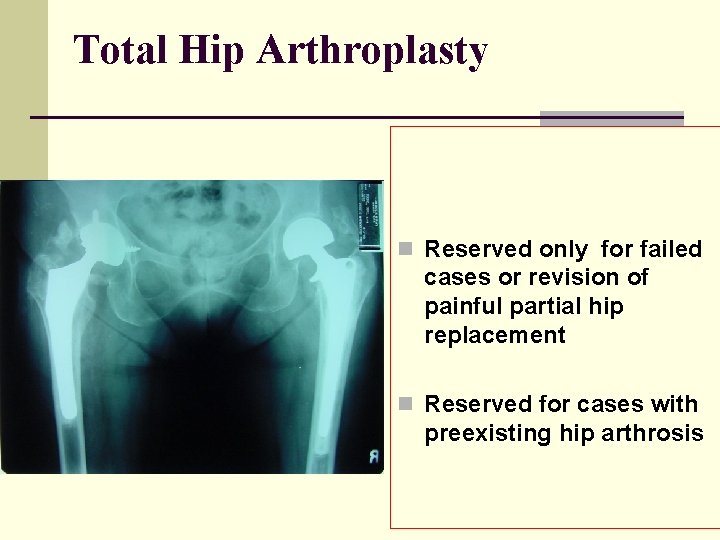
Total Hip Arthroplasty n Reserved only for failed cases or revision of painful partial hip replacement n Reserved for cases with preexisting hip arthrosis
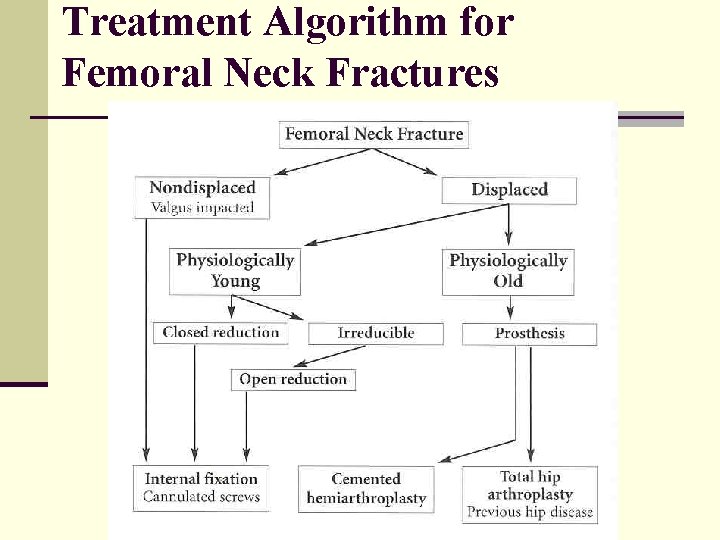
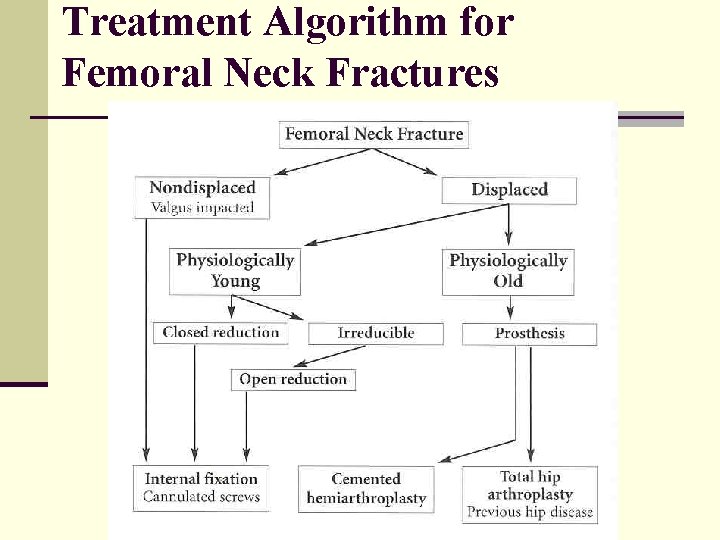
Treatment Algorithm for Femoral Neck Fractures
Can the ‘Problem’ fracture be considered ‘Solved’? n Making the right decision about the right treatment in the right patient is still very surgeon dependent n The time since fracture type of fracture age of the patient ALL MAKE A DIFFERENCE TO THE ULTIMATE OUTCOME
THE DEBATE ABOUT THE BEST TREATMENT STILL GOES ON…. .
