IntraAbdominal Candidiasis Candida peritonitis Paschalis Vergidis MD MSc
Intra-Abdominal Candidiasis, Candida peritonitis Paschalis Vergidis, MD, MSc Infectious Diseases Consultant Manchester University NHS Foundation Trust
Learning Objectives To understand the different forms of intra-abdominal candidiasis To discuss the risk factors for intra-abdominal candidiasis To review the management and outcomes of intra-abdominal candidiasis
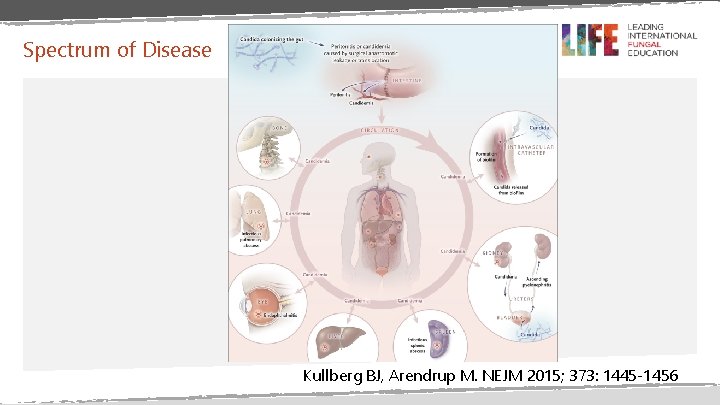
Spectrum of Disease Kullberg BJ, Arendrup M. NEJM 2015; 373: 1445 -1456

Intra-Abdominal Candidiasis • Common form of deep-seated candidiasis • Poorly studied compared to candidaemia • Accounts for ~10% of all cases of peritonitis • Bacterial co-infection is common
Classification • Primary peritonitis • No apparent breach of the GI tract • Secondary Peritonitis • Follows perforations, surgical leaks, trauma or other pathological process • Tertiary Peritonitis • Persistence or recurrence of intra-abdominal infection following treatment • Intra-Abdominal Abscess • Localized infection resulting from pathological process or breach of the GI tract • Infected Pancreatic Necrosis • Infection of the non-vitalized pancreatic tissue • Cholecystitis, cholangitis Vergidis et al. PLo. S ONE. 2016; 11(4). e 0153247
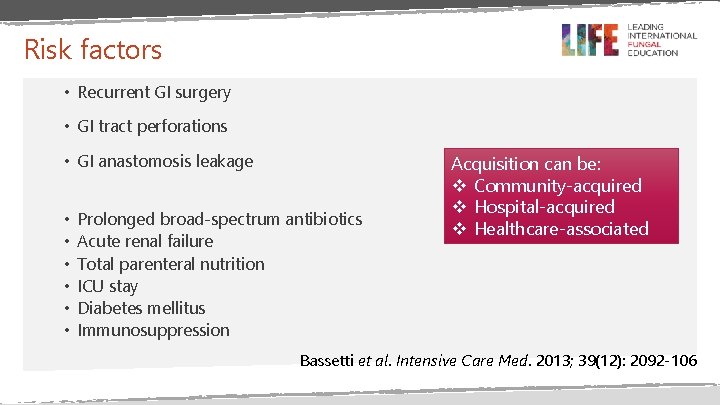
Risk factors • Recurrent GI surgery • GI tract perforations • GI anastomosis leakage • • • Prolonged broad-spectrum antibiotics Acute renal failure Total parenteral nutrition ICU stay Diabetes mellitus Immunosuppression Acquisition can be: v Community-acquired v Hospital-acquired v Healthcare-associated Bassetti et al. Intensive Care Med. 2013; 39(12): 2092 -106

Microbiology • Candida albicans (65 -82%) • C. glabrata <20% • C. tropicalis <10% • C. parapsilosis <5% • Other non-albicans Candida spp. ~2% • Mixed Candida spp. ~5%
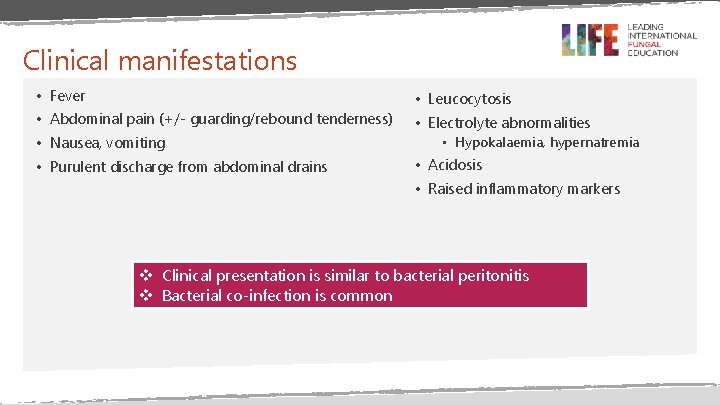
Clinical manifestations • Fever • Leucocytosis • Abdominal pain (+/- guarding/rebound tenderness) • Electrolyte abnormalities • Nausea, vomiting • Purulent discharge from abdominal drains • Hypokalaemia, hypernatremia • Acidosis • Raised inflammatory markers v Clinical presentation is similar to bacterial peritonitis v Bacterial co-infection is common
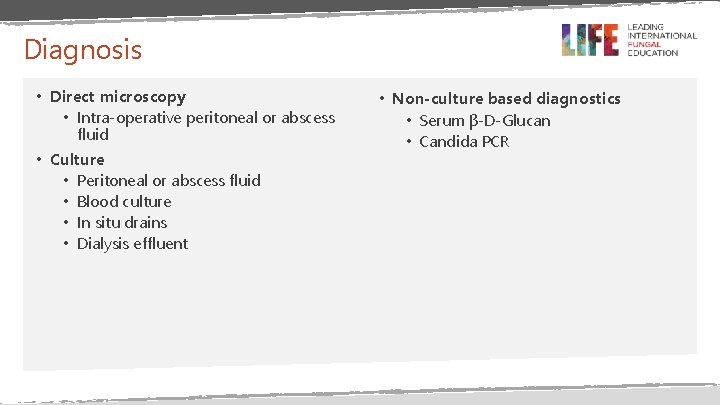
Diagnosis • Direct microscopy • Intra-operative peritoneal or abscess fluid • Culture • Peritoneal or abscess fluid • Blood culture • In situ drains • Dialysis effluent • Non-culture based diagnostics • Serum β-D-Glucan • Candida PCR
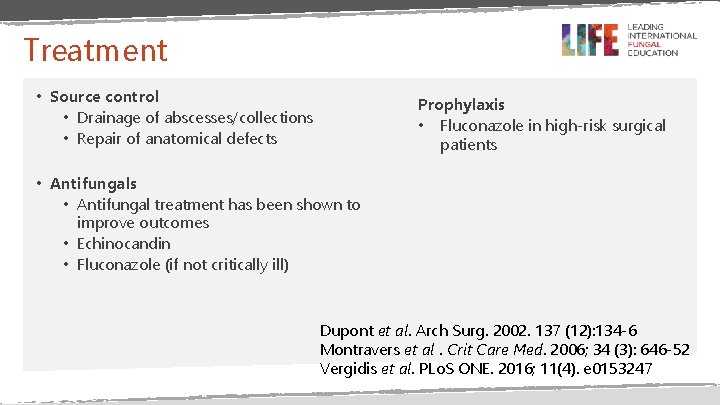
Treatment • Source control • Drainage of abscesses/collections • Repair of anatomical defects Prophylaxis • Fluconazole in high-risk surgical patients • Antifungals • Antifungal treatment has been shown to improve outcomes • Echinocandin • Fluconazole (if not critically ill) Dupont et al. Arch Surg. 2002. 137 (12): 134 -6 Montravers et al. Crit Care Med. 2006; 34 (3): 646 -52 Vergidis et al. PLo. S ONE. 2016; 11(4). e 0153247
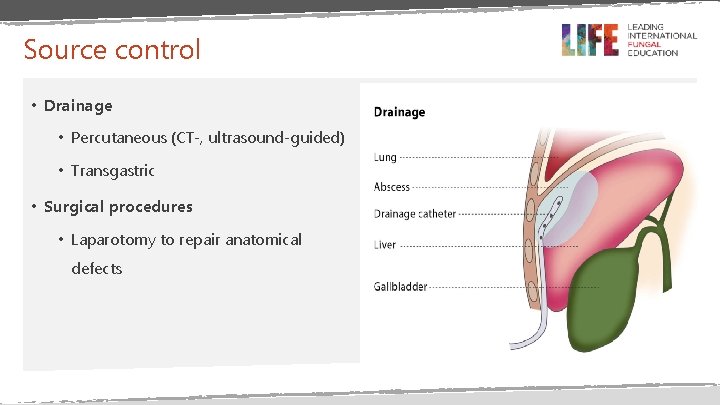
Source control • Drainage • Percutaneous (CT-, ultrasound-guided) • Transgastric • Surgical procedures • Laparotomy to repair anatomical defects
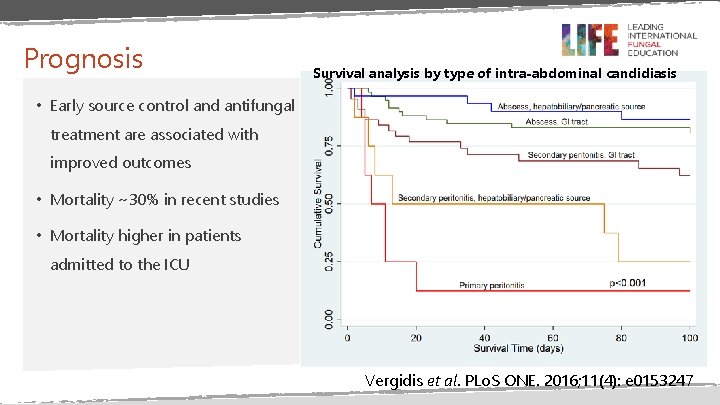
Prognosis Survival analysis by type of intra-abdominal candidiasis • Early source control and antifungal treatment are associated with improved outcomes • Mortality ~30% in recent studies • Mortality higher in patients admitted to the ICU Vergidis et al. PLo. S ONE. 2016; 11(4): e 0153247
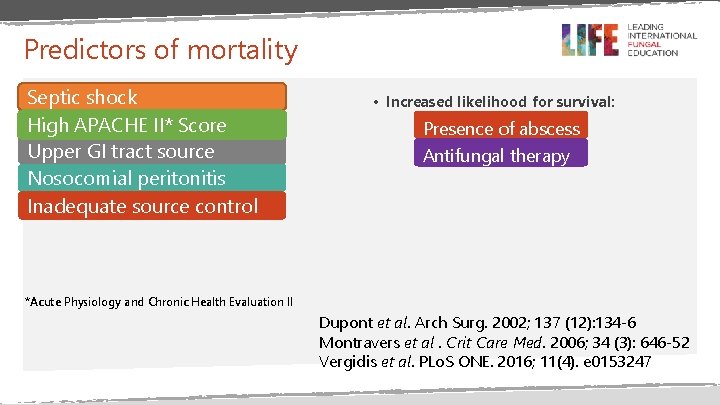
Predictors of mortality Septic shock High APACHE II* Score Upper GI tract source Nosocomial peritonitis Inadequate source control • Increased likelihood for survival: Presence of abscess Antifungal therapy *Acute Physiology and Chronic Health Evaluation II Dupont et al. Arch Surg. 2002; 137 (12): 134 -6 Montravers et al. Crit Care Med. 2006; 34 (3): 646 -52 Vergidis et al. PLo. S ONE. 2016; 11(4). e 0153247
Summary Intra-abdominal candidiasis is as common as Candida bloodstream infections Mortality rates are comparable to that of candidaemia Early source control and antifungal treatment are associated with improved outcomes
END
- Slides: 15