INTRA AORTIC BALLON PUMP IABP how does it
INTRA AORTIC BALLON PUMP
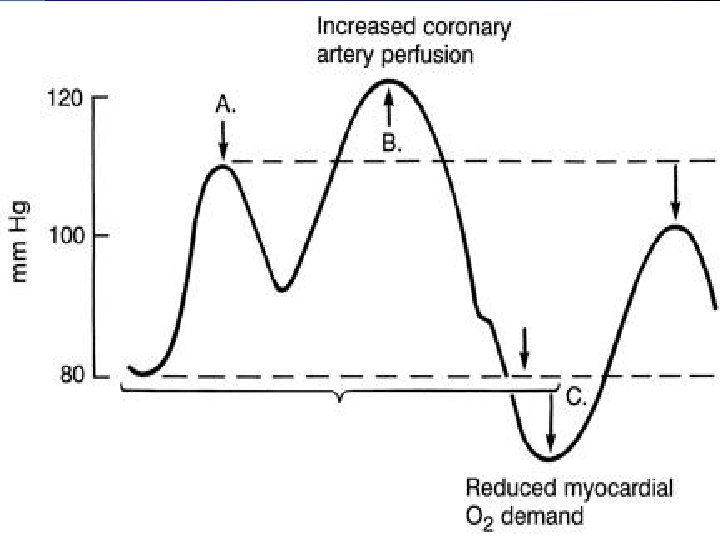
IABP- how does it work? l l l IABP does not ‘pump’ blood per se in contrast to a VAD. Requires a functioning, beating heart. IABP serves as an external source of energy to allow the sick heart to pump more efficiently. Does this via afterload reduction and diastolic augmentation. Net result is an increased DO 2, decreased MVO 2, and an increased CO.
Concepts of Counterpulsation The balloon is phasically pulsed in counterpulsation to the patient’s cardiac cycle (IABC) l IABP has no ‘inotropic’ action; does not directly increase contractility. l Primarily benefits the left ventricle, although the diastolic augmentation may improve coronary flow to both ventricals. l
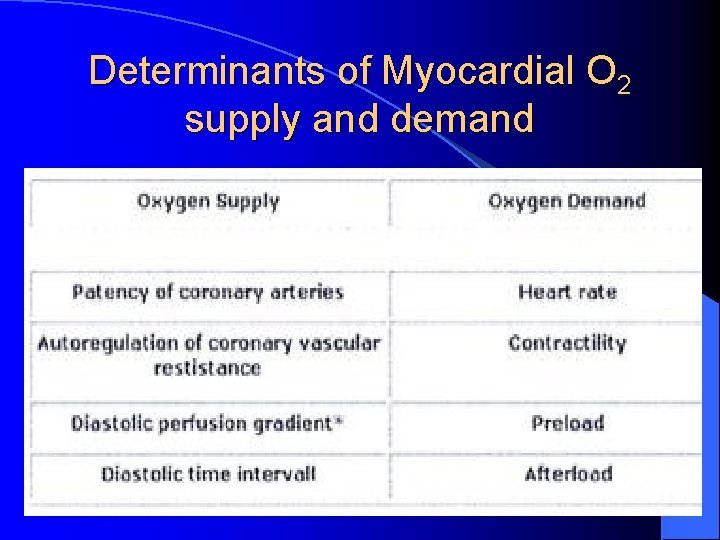
Determinants of Myocardial O 2 supply and demand

l Most Widely used temporary circulatory assist device. l Works on the principle of counter pulsations. l Poor left ventricular indices could possibly be influenced by retarding the end diastolic pressure and increasing the coronary circulation.
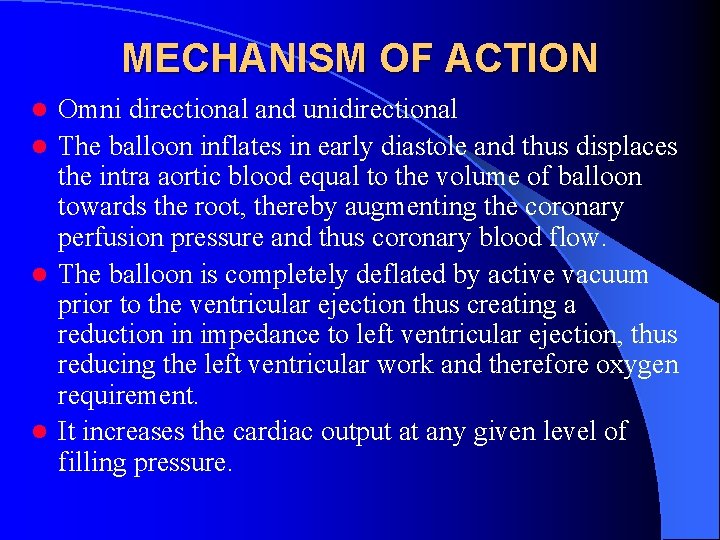
MECHANISM OF ACTION Omni directional and unidirectional l The balloon inflates in early diastole and thus displaces the intra aortic blood equal to the volume of balloon towards the root, thereby augmenting the coronary perfusion pressure and thus coronary blood flow. l The balloon is completely deflated by active vacuum prior to the ventricular ejection thus creating a reduction in impedance to left ventricular ejection, thus reducing the left ventricular work and therefore oxygen requirement. l It increases the cardiac output at any given level of filling pressure. l
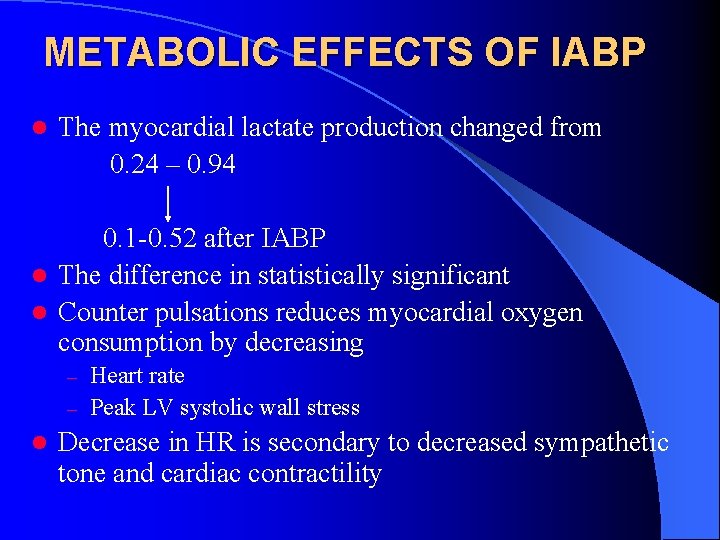
METABOLIC EFFECTS OF IABP l The myocardial lactate production changed from 0. 24 – 0. 94 0. 1 -0. 52 after IABP l The difference in statistically significant l Counter pulsations reduces myocardial oxygen consumption by decreasing Heart rate – Peak LV systolic wall stress – l Decrease in HR is secondary to decreased sympathetic tone and cardiac contractility
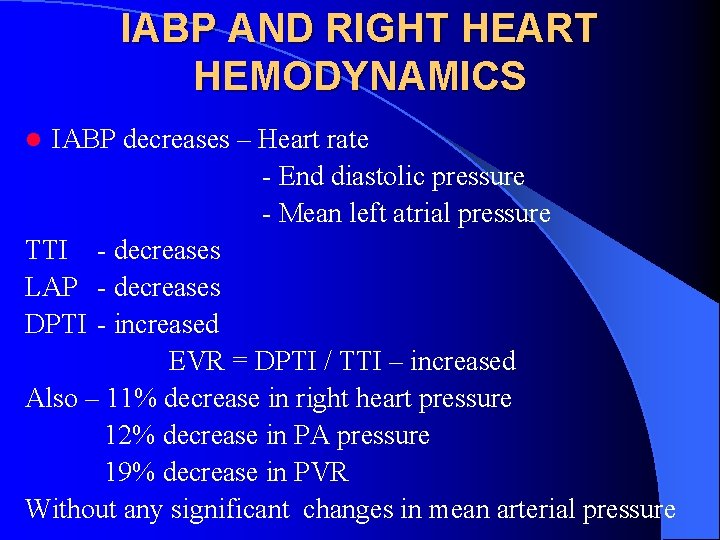
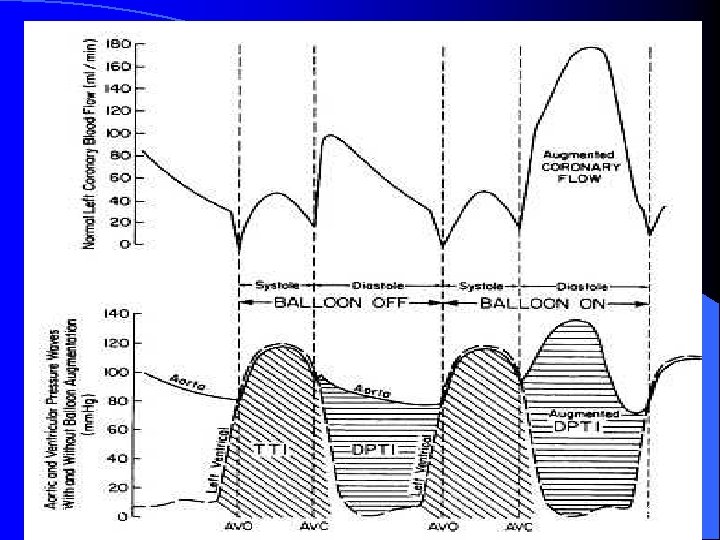
IABP AND RIGHT HEART HEMODYNAMICS IABP decreases – Heart rate - End diastolic pressure - Mean left atrial pressure TTI - decreases LAP - decreases DPTI - increased EVR = DPTI / TTI – increased Also – 11% decrease in right heart pressure 12% decrease in PA pressure 19% decrease in PVR Without any significant changes in mean arterial pressure l

ROUTES OF INSERTION l Femoral Artery – Percutaneous - Open method - Through conduit l Iliac artery l Axillary artery l Left subclavian artery l Ascending aorta and arch of aorta l Abdominal aorta (rare)
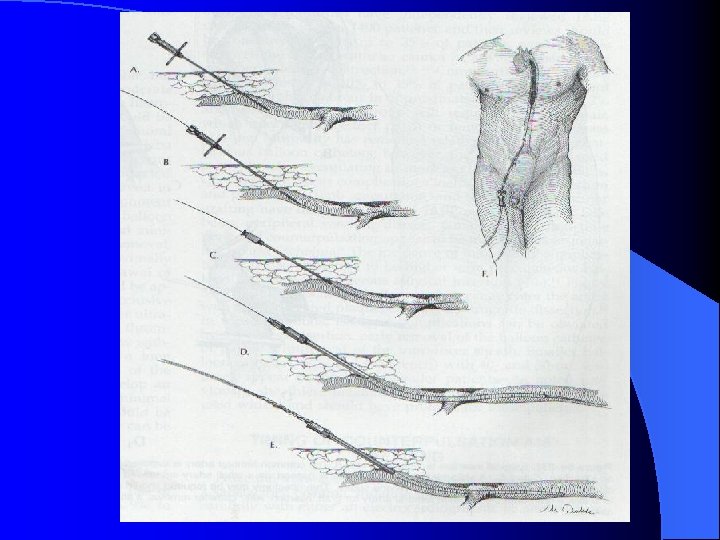
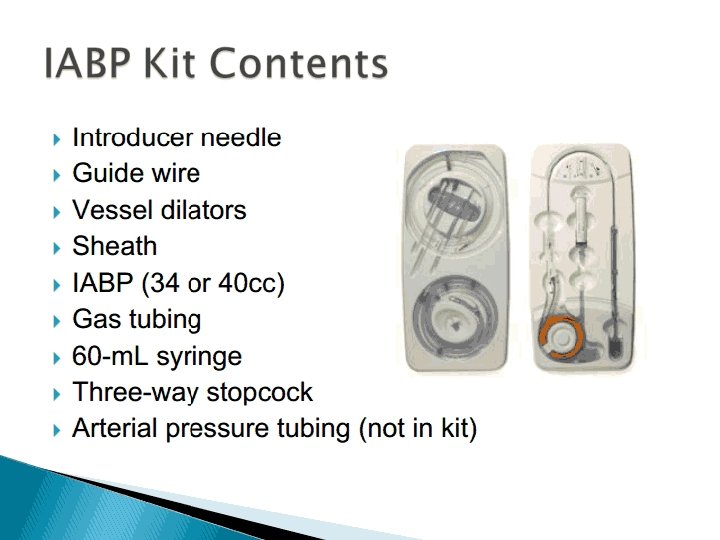
PROCEDURE l Balloon sizing l Evaluate the peripheral vasculature l Ankle brachial index l Painting and draping l Gaining access to the vessel l 16 G needle, 0. 032/0. 035/0. 038 inch J. tip Guide wire l Sheath and sheath less insertion l Balloon inserted
l Guide wire removed l Helium gas line in connected to IABP console l Central catheter attached to arterial pressure monitoring device l Balloon inflation initiated – 1: 2 augmentation l Arterial line flushed and trace detected l Inflation timing adjusted. l Balloon secured in place l Sterile dressing done l Inflation to 1: 1 augmentation
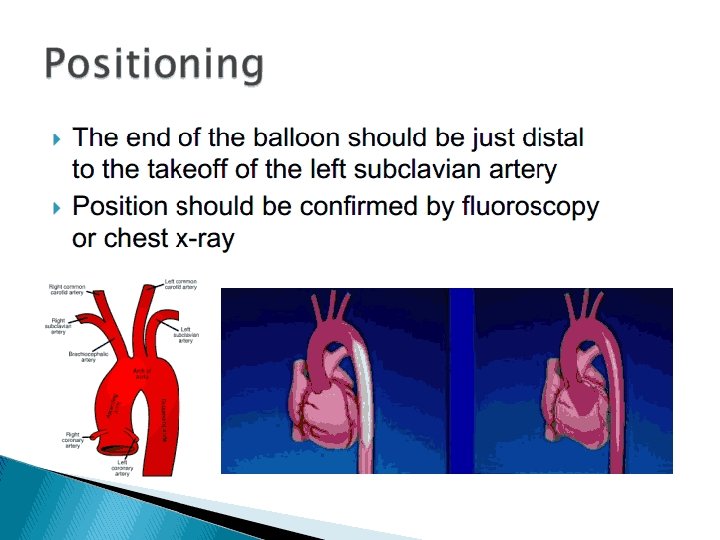
Placement Placed percutaneously or surgically with or without a sheath via the femoral artery. l Advanced into aorta (? under flouroscopy) until the tip is about 1 cm distal to the origin of the left subclavian a. l Cathater locations more proximal than this compromise flow to the vessels of the aortic arch. l More distal locations attenuate the hemodynamic benefits of the IABP and can potentially compromise renal blood flow. l


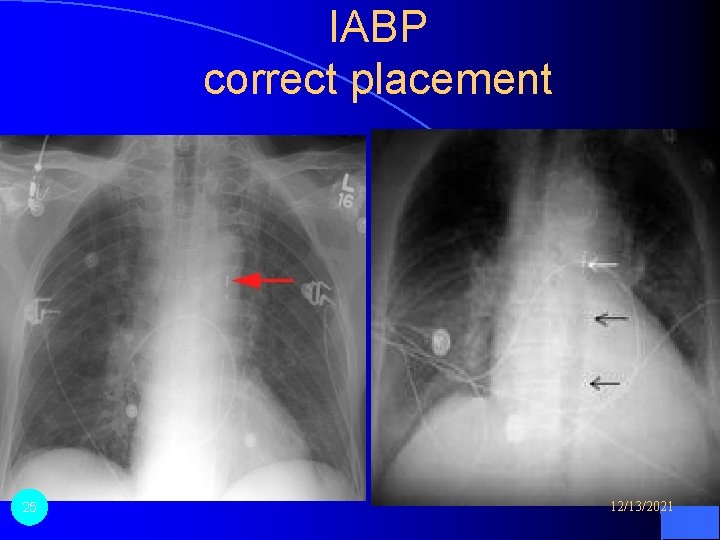
IABP correct placement 25 12/13/2021

26 12/13/2021
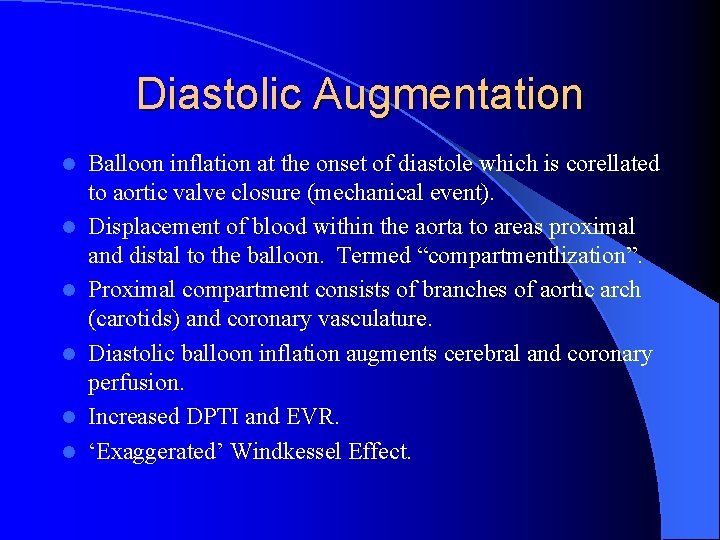
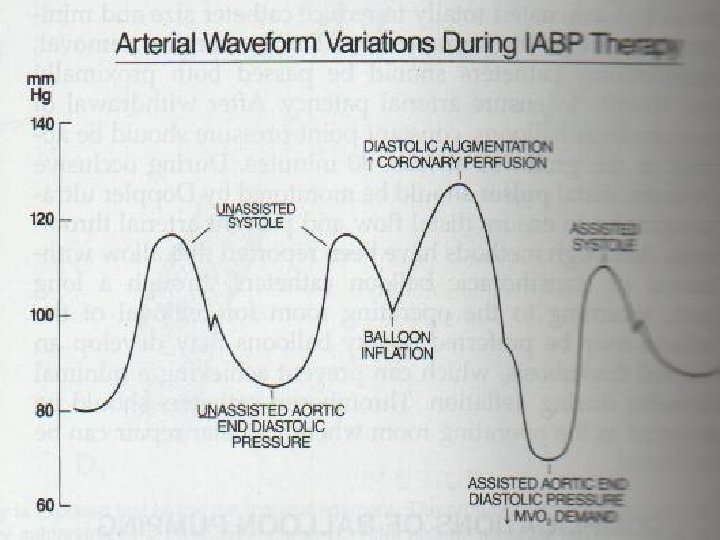
Diastolic Augmentation l l l Balloon inflation at the onset of diastole which is corellated to aortic valve closure (mechanical event). Displacement of blood within the aorta to areas proximal and distal to the balloon. Termed “compartmentlization”. Proximal compartment consists of branches of aortic arch (carotids) and coronary vasculature. Diastolic balloon inflation augments cerebral and coronary perfusion. Increased DPTI and EVR. ‘Exaggerated’ Windkessel Effect.
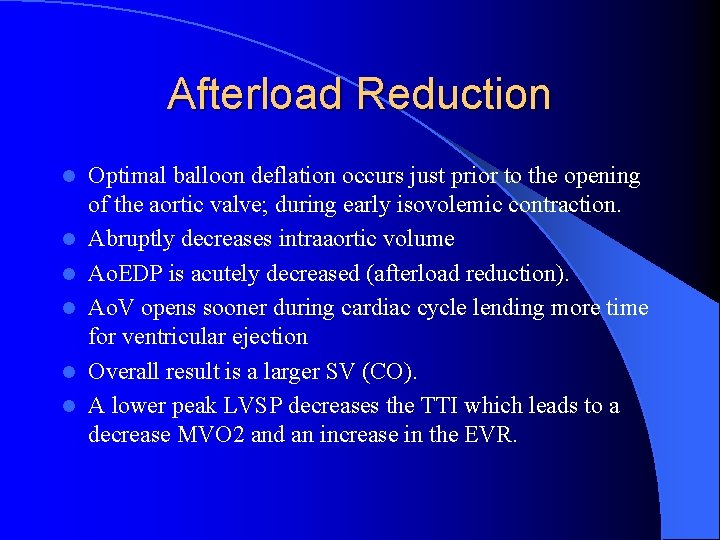
Afterload Reduction l l l Optimal balloon deflation occurs just prior to the opening of the aortic valve; during early isovolemic contraction. Abruptly decreases intraaortic volume Ao. EDP is acutely decreased (afterload reduction). Ao. V opens sooner during cardiac cycle lending more time for ventricular ejection Overall result is a larger SV (CO). A lower peak LVSP decreases the TTI which leads to a decrease MVO 2 and an increase in the EVR.
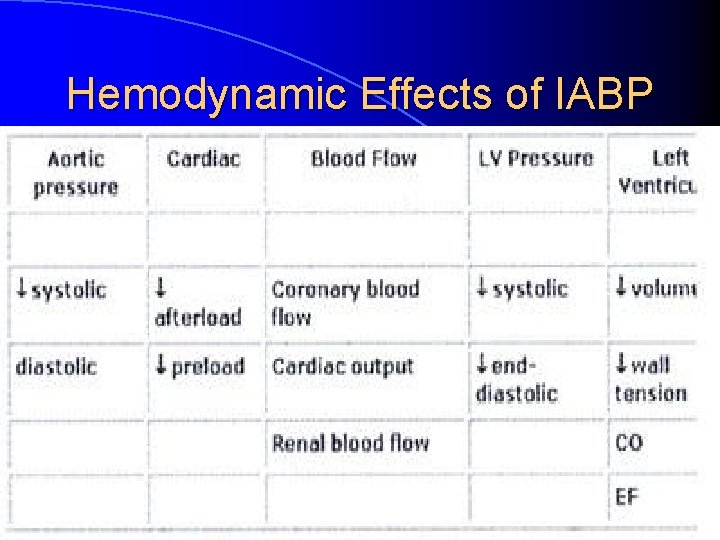
Hemodynamic Effects of IABP
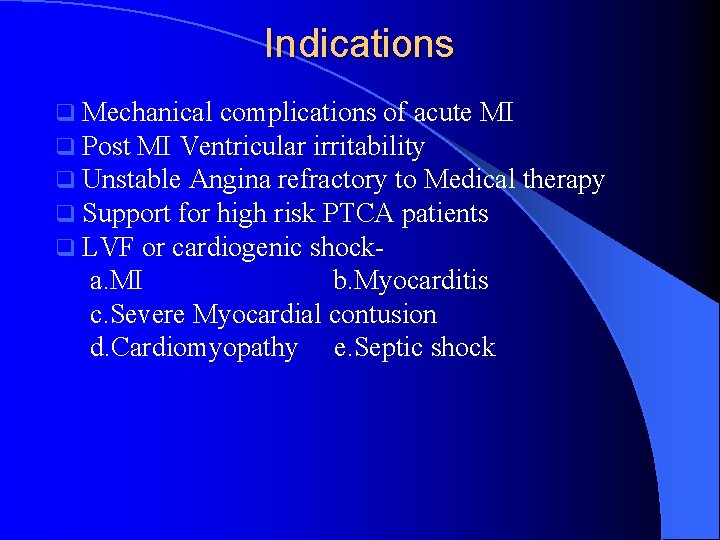
Indications q Mechanical complications of acute MI q Post MI Ventricular irritability q Unstable Angina refractory to Medical q Support for high risk PTCA patients q LVF or cardiogenic shock- a. MI b. Myocarditis c. Severe Myocardial contusion d. Cardiomyopathy e. Septic shock therapy
Indications (Contd) l Failure to wean from cardiopulmonary bypass l Low output syndrome Ø Stabilization of high risk patients undergoing GA Ø Bridge to transplant Ø Stunned Myocardium Ø Failed PTCA
Contraindications l Thoracic or abdominal aortic aneurysm l Aortic dissection l Aortic valve insufficiency l Severe pre-existing peripheral vascular disease, presence of ilio-femoral grafts. l Prosthetic aortic graft l Irreversible Brain Damage
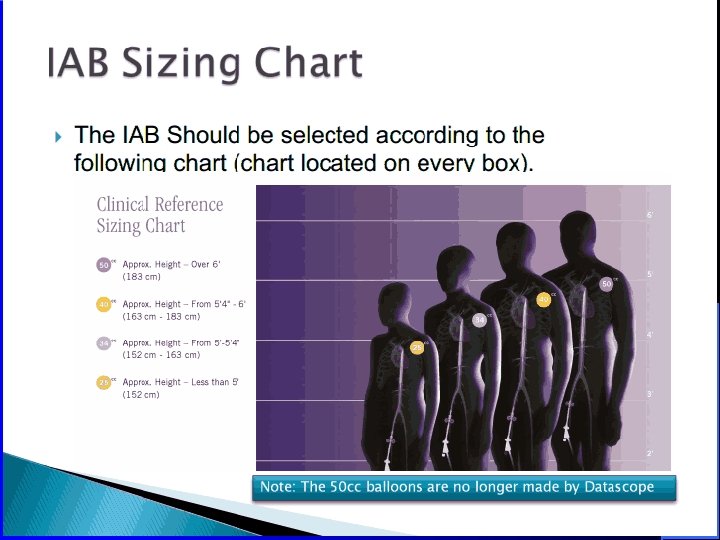
Determinants of IABP efficiency l l l Ideal balloon volume causes maximal emptying of LV without causing retrograde flow from the coronary vasculature and vessels of the aortic arch. Balloon should occlude 75 -90% of the aortic crosssectional area during inflation. CO 2 vs Helium (lower density-better rapid diffusion coeffecient) Efficiency if IABC is critically dependent on the timing of both inflation and deflation. Improper timing can worsen a patient’s condition.
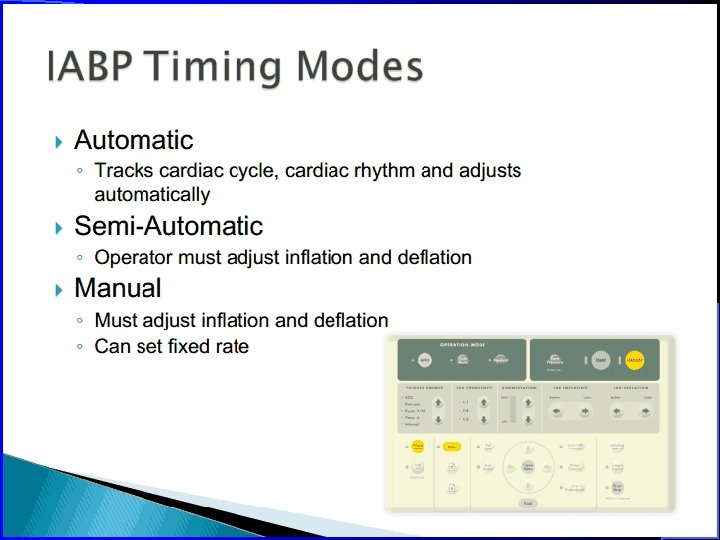
IAPB Timing l l l IABP requires a trigger to determine systole and diastole. ECG or arterial waveform. ECG directly from the patient to the pump can slave off the bedside monitor. Inflation : T-wave default - Electrical index of diastole. Deflation : occurs prior to the next QRS (during PR interval). Timing is manually fine-tuned according to the aortic pressure waveform (more representative of mechanical events). Inflation : dicrotic notch, Deflation : before next systolic upstroke
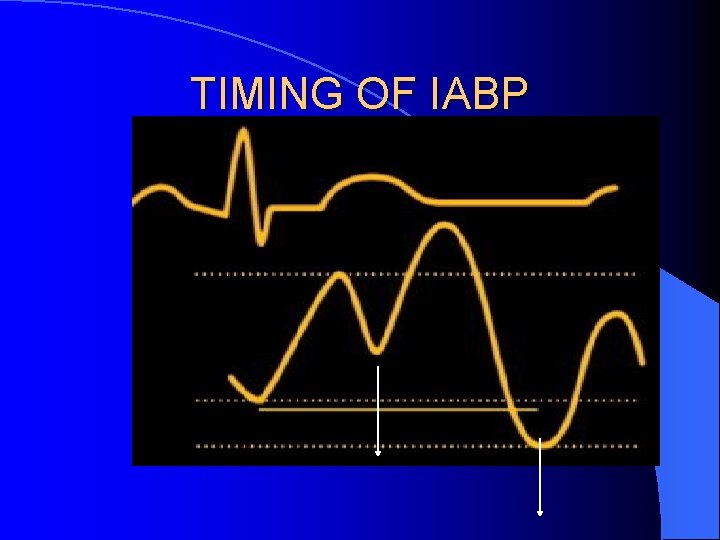
TIMING OF IABP
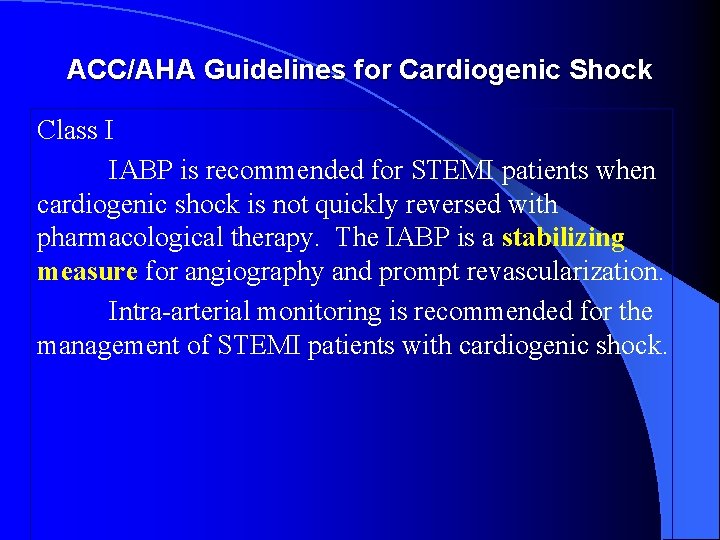
ACC/AHA Guidelines for Cardiogenic Shock Class I IABP is recommended for STEMI patients when cardiogenic shock is not quickly reversed with pharmacological therapy. The IABP is a stabilizing measure for angiography and prompt revascularization. Intra-arterial monitoring is recommended for the management of STEMI patients with cardiogenic shock.
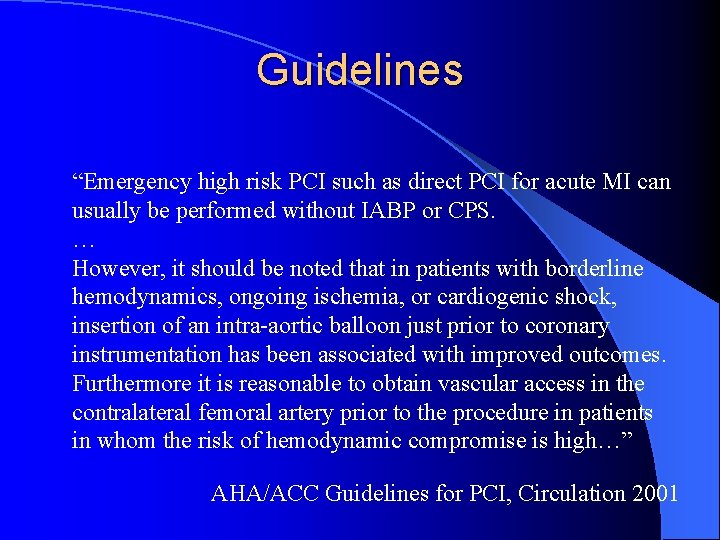
Guidelines “Emergency high risk PCI such as direct PCI for acute MI can usually be performed without IABP or CPS. … However, it should be noted that in patients with borderline hemodynamics, ongoing ischemia, or cardiogenic shock, insertion of an intra-aortic balloon just prior to coronary instrumentation has been associated with improved outcomes. Furthermore it is reasonable to obtain vascular access in the contralateral femoral artery prior to the procedure in patients in whom the risk of hemodynamic compromise is high…” AHA/ACC Guidelines for PCI, Circulation 2001
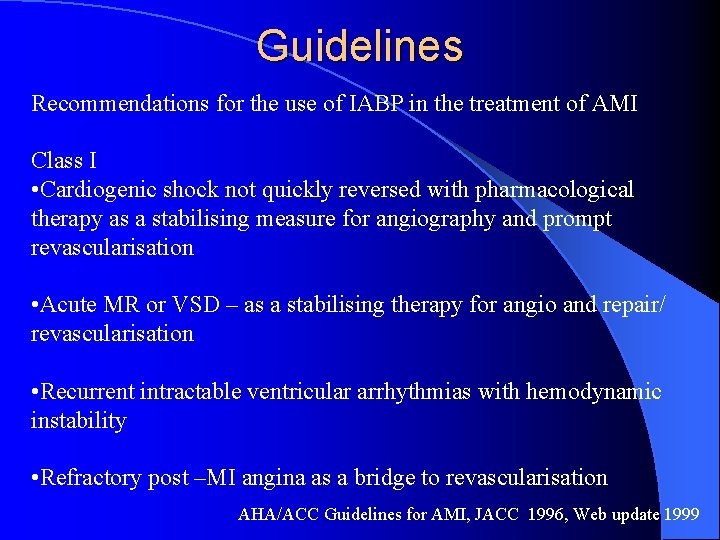
Guidelines Recommendations for the use of IABP in the treatment of AMI Class I • Cardiogenic shock not quickly reversed with pharmacological therapy as a stabilising measure for angiography and prompt revascularisation • Acute MR or VSD – as a stabilising therapy for angio and repair/ revascularisation • Recurrent intractable ventricular arrhythmias with hemodynamic instability • Refractory post –MI angina as a bridge to revascularisation AHA/ACC Guidelines for AMI, JACC 1996, Web update 1999
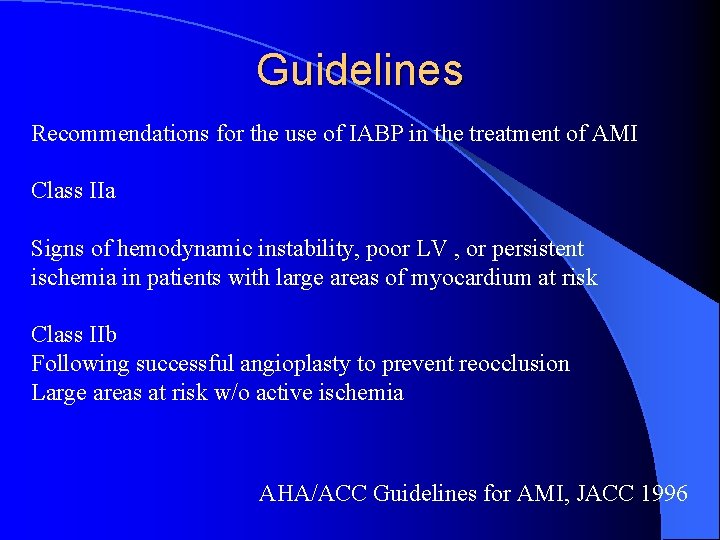
Guidelines Recommendations for the use of IABP in the treatment of AMI Class IIa Signs of hemodynamic instability, poor LV , or persistent ischemia in patients with large areas of myocardium at risk Class IIb Following successful angioplasty to prevent reocclusion Large areas at risk w/o active ischemia AHA/ACC Guidelines for AMI, JACC 1996
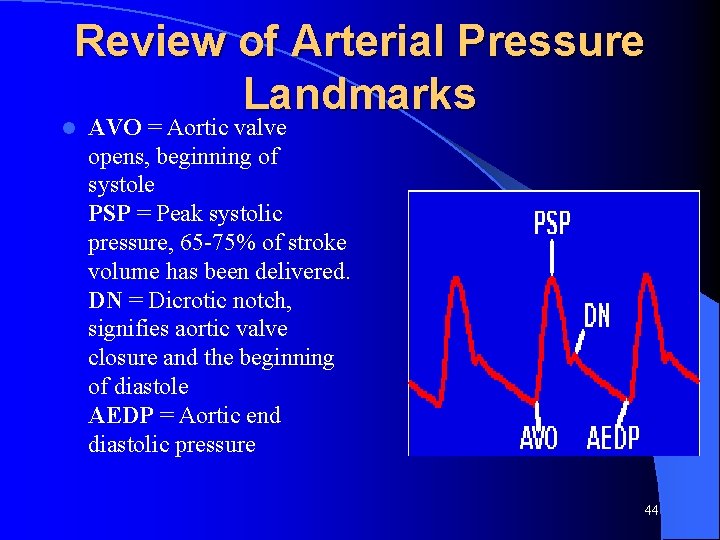
Review of Arterial Pressure Landmarks l AVO = Aortic valve opens, beginning of systole PSP = Peak systolic pressure, 65 -75% of stroke volume has been delivered. DN = Dicrotic notch, signifies aortic valve closure and the beginning of diastole AEDP = Aortic end diastolic pressure 44
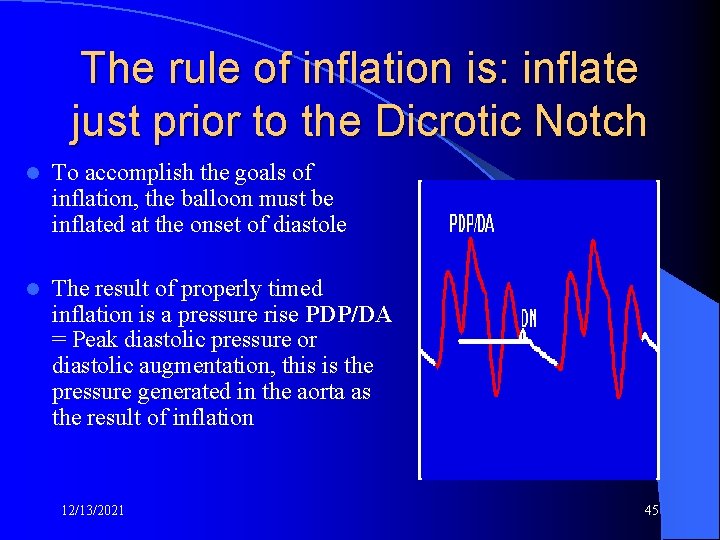
The rule of inflation is: inflate just prior to the Dicrotic Notch l To accomplish the goals of inflation, the balloon must be inflated at the onset of diastole l The result of properly timed inflation is a pressure rise PDP/DA = Peak diastolic pressure or diastolic augmentation, this is the pressure generated in the aorta as the result of inflation 12/13/2021 45
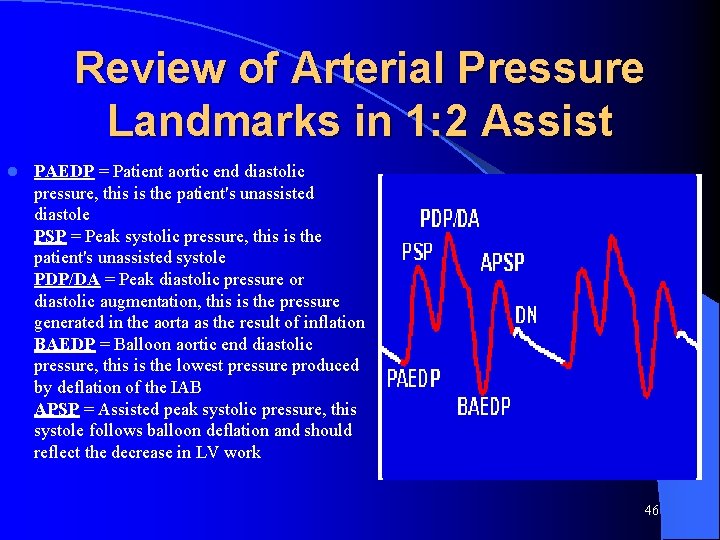
Review of Arterial Pressure Landmarks in 1: 2 Assist l PAEDP = Patient aortic end diastolic pressure, this is the patient's unassisted diastole PSP = Peak systolic pressure, this is the patient's unassisted systole PDP/DA = Peak diastolic pressure or diastolic augmentation, this is the pressure generated in the aorta as the result of inflation BAEDP = Balloon aortic end diastolic pressure, this is the lowest pressure produced by deflation of the IAB APSP = Assisted peak systolic pressure, this systole follows balloon deflation and should reflect the decrease in LV work 46
Inflation Hemodynamics l Coronary artery blood flow and pressure are increased – Increased renal and cerebral blood flow l Increased diastolic pressure increases perfusion to distal organs and tissues 12/13/2021 47
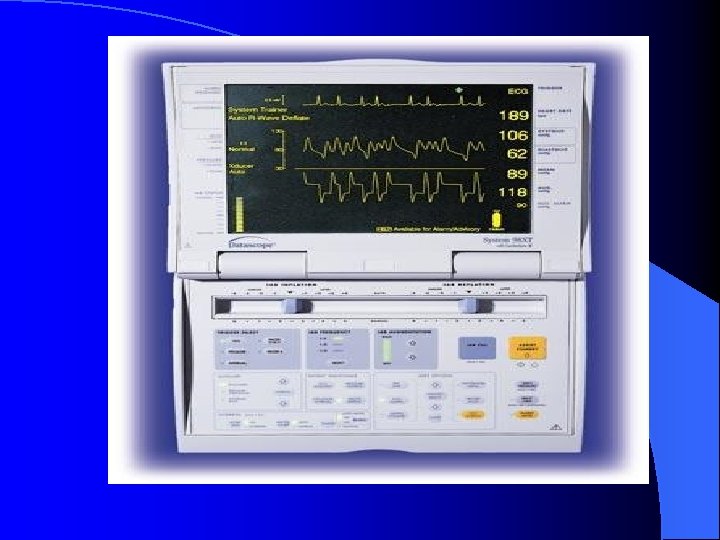
Triggering l It is necessary to establish a reliable trigger signal before balloon pumping can begin l The computer in the IAB console needs a stimulus to cycle the pneumatic system, which inflates and deflates the balloon l The trigger signal tells the computer that another cardiac cycle has begun 12/13/2021 48
Triggering l In most cases it is preferable to use the R wave of the ECG as the trigger signal l However, there are other trigger options for instances when the R wave cannot be used or is not appropriate 12/13/2021 49
Trigger Loss l The console MUST see a trigger to initiate an inflate/deflate cycle l If no trigger is seen when the clinician attempts to start pumping, no pumping will occur and an alarm will be sounded l If the trigger is lost after pumping starts, no further pumping will occur until a trigger is re-established l The pump will go to STANDBY and an alarm will be sounded 12/13/2021 50
Trigger Loss l If the current trigger is lost the clinician choose an alternate, available trigger to resume pumping l For example, if the ECG lead becomes disconnected the Arterial Pressure trigger may be selected until the ECG is re-established 12/13/2021 51
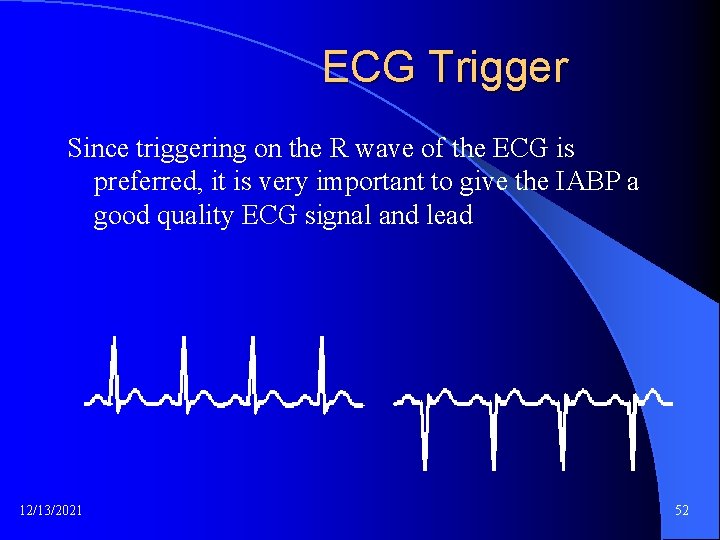
ECG Trigger Since triggering on the R wave of the ECG is preferred, it is very important to give the IABP a good quality ECG signal and lead 12/13/2021 52
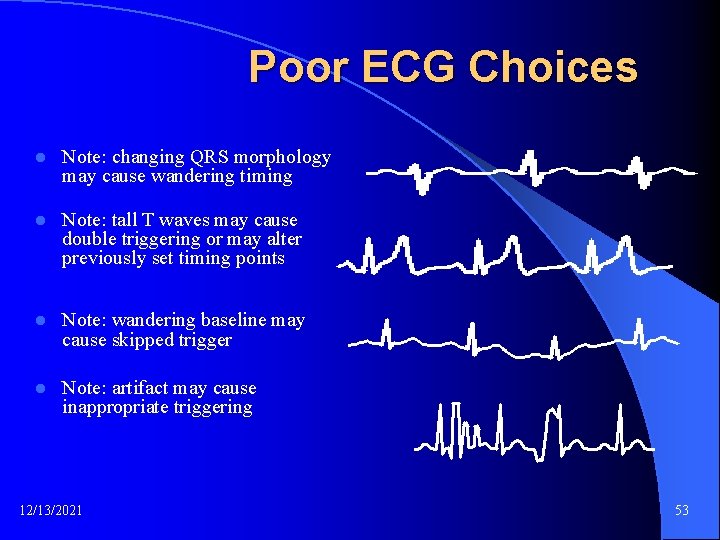
Poor ECG Choices l Note: changing QRS morphology may cause wandering timing l Note: tall T waves may cause double triggering or may alter previously set timing points l Note: wandering baseline may cause skipped trigger l Note: artifact may cause inappropriate triggering 12/13/2021 53
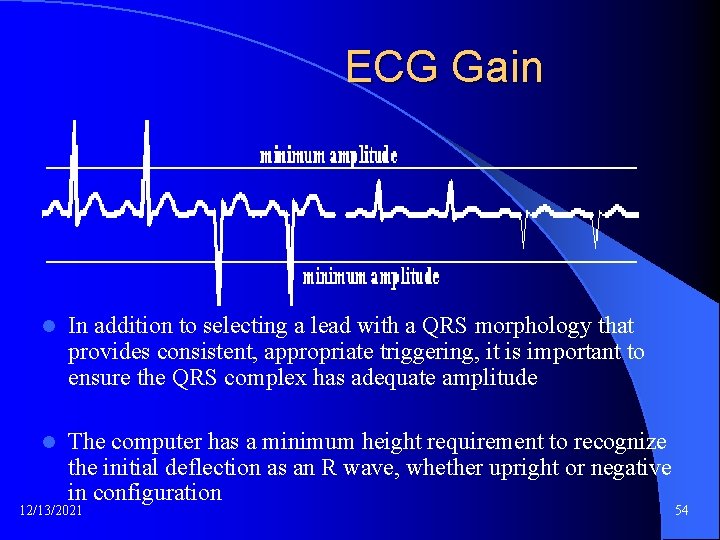
ECG Gain l In addition to selecting a lead with a QRS morphology that provides consistent, appropriate triggering, it is important to ensure the QRS complex has adequate amplitude l The computer has a minimum height requirement to recognize the initial deflection as an R wave, whether upright or negative in configuration 12/13/2021 54
Triggering on the Arterial Pressure Waveform l Arterial pressure provides another signal to the IABP to determine where the cardiac cycle begins and ends l It is used when the ECG has too much interference from patient movement or poor lead connection l There are limitations to triggering on the arterial pressure curve – Therefore AP trigger should be considered a backup trigger and not the one used as the primary trigger 12/13/2021 55
Valid Trigger Indications l Accurate Heart Rate displayed on pump l Assist marker on/under ECG in same ratio as assist ratio, e. g. if in 1: 1 there should be one assist marker per ECG complex l Flash 12/13/2021 heart symbol next to HR on screen 56
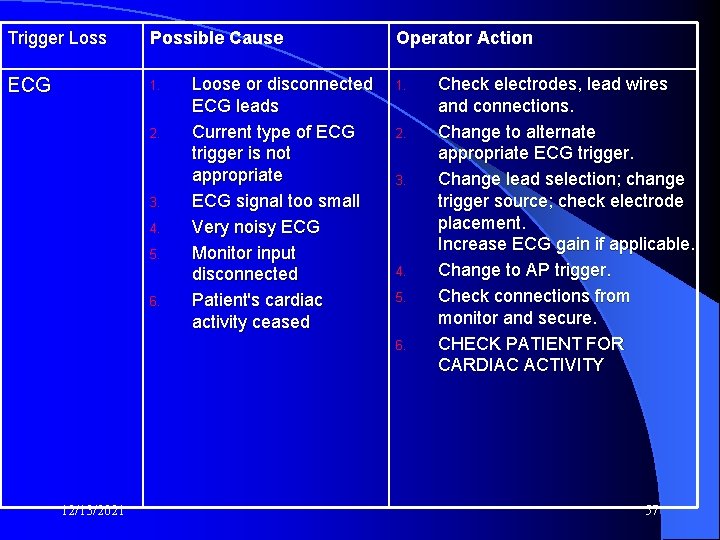
Trigger Loss Possible Cause ECG 1. 2. 3. 4. 5. 6. Loose or disconnected ECG leads Current type of ECG trigger is not appropriate ECG signal too small Very noisy ECG Monitor input disconnected Patient's cardiac activity ceased Operator Action 1. 2. 3. 4. 5. 6. 12/13/2021 Check electrodes, lead wires and connections. Change to alternate appropriate ECG trigger. Change lead selection; change trigger source; check electrode placement. Increase ECG gain if applicable. Change to AP trigger. Check connections from monitor and secure. CHECK PATIENT FOR CARDIAC ACTIVITY 57
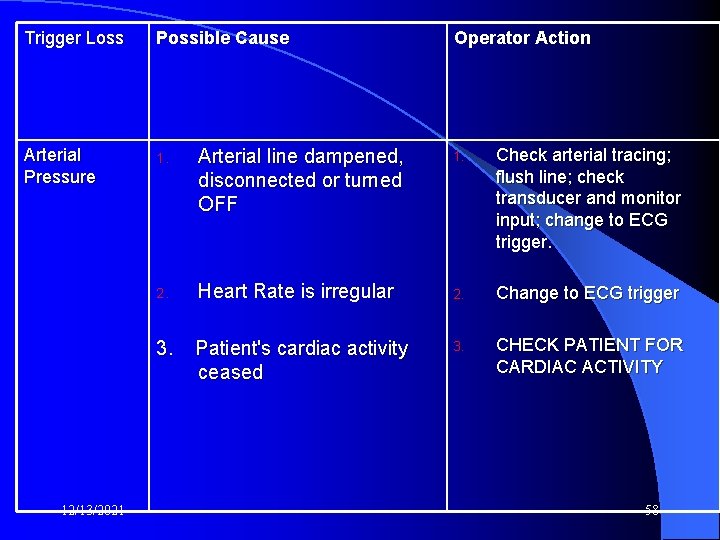
Trigger Loss Possible Cause Arterial Pressure 1. Arterial line dampened, disconnected or turned OFF 2. Heart Rate is irregular 3. Patient's cardiac activity ceased 12/13/2021 Operator Action 1. Check arterial tracing; flush line; check transducer and monitor input; change to ECG trigger. 2. Change to ECG trigger 3. CHECK PATIENT FOR CARDIAC ACTIVITY 58
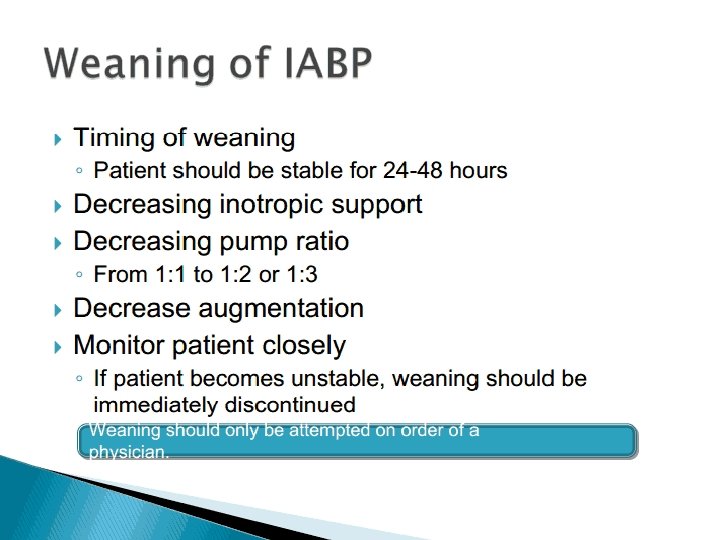
TIMING and WEANING l Balloon synchronization starts usually at a beat ratio of 1: 2. l This ratio facilitates comparison between the patient’s own ventricular beats and augmented beats to determine ideal IABP timing. l Errors in timing of the IABP may result in different waveform characteristics and a various number of physiologic effects. 12/13/2021 59
TIMING and WEANING l If the patient’s cardiac performance improves, weaning from the IABP may begin by gradually decreasing the balloon augmentation ratio (from 1: 1 to 1: 2 to 1: 4 to 1: 8) under control of hemodynamic stability. l After appropriate observation at 1: 8 counterpulsation the balloon pump is removed. 12/13/2021 60
Gas Alarms/Balloon Pressure Waveform l During a cycle of inflation/deflation, helium is rapidly moved in and out of the balloon. The environment within the balloon and the surrounding forces that affect balloon behavior all contribute to a predictable pattern of gas flow and pressure. l The Arrow International IABP consoles have in-line transducers that relay the pattern of gas pressure during the inflate/deflate cycle. l The gas pressure characteristics are converted into a waveform that is reflective of the behavior of the gas. l This transduced waveform can tell us much about the interaction of the balloon within the patient's aorta. l Thorough understanding of the balloon pressure waveform is also important for efficient troubleshooting of the console as most of the alarms are based on this gas surveillance system. 12/13/2021 61
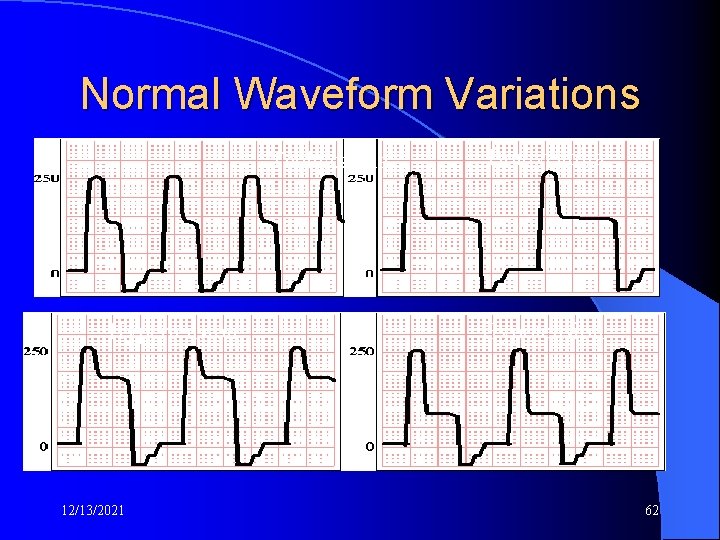
Normal Waveform Variations Tachycardia Hypertension 12/13/2021 Bradycardia Hypotension 62
12/13/2021 63
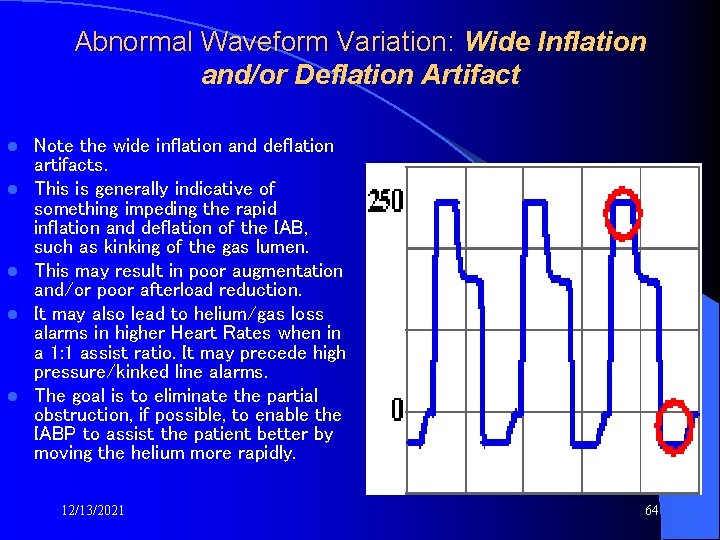
Abnormal Waveform Variation: Wide Inflation and/or Deflation Artifact l l l Note the wide inflation and deflation artifacts. This is generally indicative of something impeding the rapid inflation and deflation of the IAB, such as kinking of the gas lumen. This may result in poor augmentation and/or poor afterload reduction. It may also lead to helium/gas loss alarms in higher Heart Rates when in a 1: 1 assist ratio. It may precede high pressure/kinked line alarms. The goal is to eliminate the partial obstruction, if possible, to enable the IABP to assist the patient better by moving the helium more rapidly. 12/13/2021 64
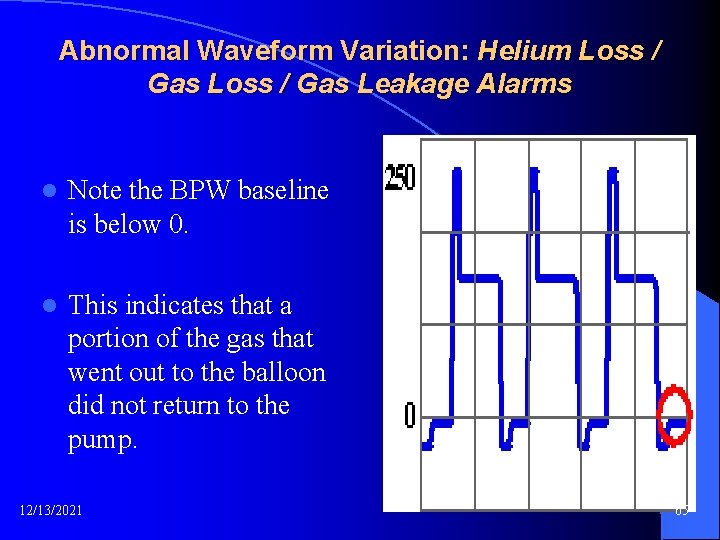
Abnormal Waveform Variation: Helium Loss / Gas Leakage Alarms l Note the BPW baseline is below 0. l This indicates that a portion of the gas that went out to the balloon did not return to the pump. 12/13/2021 65
1. Observe for blood in the gas tubing. If even a slight amount were present, it would indicate a balloon rupture. 1. 2. Do not resume pumping. Notify physician immediately and prepare for IAB removal. Check connections where gas tubing connects to IAB and to pump. 1. Secure if loose. 3. Check for kinks, as they may trap gas in the IAB. 1. If water is present in the gas tubing, remove the condensation. Pushing the helium through the water during inflation and deflation slows down gas transition. If gas transition is prolonged too much, it can create alarms. 12/13/2021 66
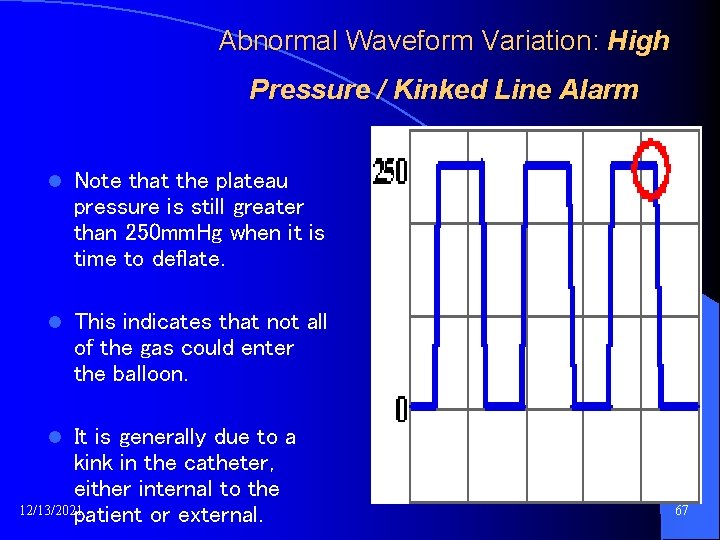
Abnormal Waveform Variation: High Pressure / Kinked Line Alarm l Note that the plateau pressure is still greater than 250 mm. Hg when it is time to deflate. l This indicates that not all of the gas could enter the balloon. It is generally due to a kink in the catheter, either internal to the 12/13/2021 patient or external. l 67
1. Reposition patient. Keep affected leg straight. Use rolled towel under hip to hyperextend hip. 2. Apply slight traction to the catheter if suspect kinking at the insertion site or in the artery. 3. Introducer sheath may be kinked which in turn is kinking the balloon. Suspect this particularly if placement of the sheath was difficult. Pull sheath back or rotate sheath a partial turn. 12/13/2021 68
1. Check placement of the balloon; it may be too high or too low. 2. IAB may be partially wrapped if alarm occurs shortly after insertion. Take steps to facilitate unwrapping (consult IAB manufacturer). 1. The balloon may be too large for the patient. Reduce the helium volume the balloon is inflated with. It is recommended to not reduce the volume below 2/3 of maximum. For example, do not decrease volume in a 40 cc IAB below 27 cc. 12/13/2021 69
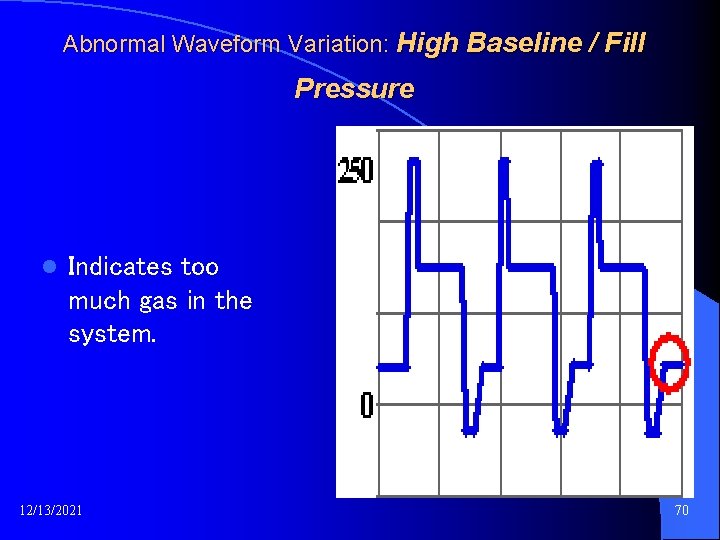
Abnormal Waveform Variation: High Baseline / Fill Pressure l Indicates too much gas in the system. 12/13/2021 70
1. Check for intermittent obstruction of gas lumen. 2. Overfill of system. 3. This condition may occur during ascent (an upward slope) in air transport since gas expands as you go up in altitude (elevation). 4. Reset the alarm and restart pumping. 5. The volume will be adjusted automatically for current barometric pressure. 6. In the Auto. CAT, ensure that the tubing to the condensation bottle (located behind the helium tank) is not kinked. 12/13/2021 71
Potential Side Effects and Complications l l l Bleeding at the insertion site Thrombocytopenia Immobility of the balloon catheter Balloon leak Infection Compartment syndrome 12/13/2021 72
IABP COMPLICATIONS �� Aortic dissection during insertion �� Reduction of platelets, RBC destruction �� Peripheral emboli �� Balloon rupture with gas embolus 73 12/13/2021 failure (balloon occlusion of renal artery) �� Renal
Complications of IABP l The following patients are at the greatest risk of developing complications associated with IABP: l Peripheral vascular disease (PVD), female, diabetic, HTN, smokers, obese, high SVR, shock 12/13/2021 74
Complications of IABP l Aortic wall dissection, rupture or local vascular injury – Care as indicated l Emboli: thrombus, plaque or air – Care as indicated 12/13/2021 75
Treatment of an air embolism is as follows l Administer 100% oxygen and intubate for significant respiratory distress or refractory hypoxemia. l Oxygen may reduce bubble size by increasing the gradient for nitrogen to move out. l Promptly place patient in Trendelenburg (head down) position and rotate toward the left lateral decubitus position. l This maneuver helps trap air in the apex of the ventricle, prevents its ejection into the pulmonary arterial system, and maintains right ventricular output. 12/13/2021 76
Complications of IABP l IABP Rupture: Helium embolus or catheter entrapment (take or catch as if in a snare or trap) – COFFEE GROUNDS seen in the drive line is a precursor to a rupture – NOTIFY RT & PHYSICIAN!!!!! – IF THERE IS A FLAGRANT (bad or offensive) RUPURE OF THE IABP CLAMP THE GAS LINE!!!!! 12/13/2021 77
Complications of IABP l Infection l Check catheter insertion site often l STRICT ASEPTIC TECHNIQUE l Restrict movement while IABP in place 12/13/2021 78
Complications of IABP l Obstruction l Malposition Too high – obstruction of left subclavian, carotids – CHECK LEFT RADIAL ARTERY PULSE – Too low – obstruction of renal and mesenteric arteries – MONITOR URINE OUTPUT – 12/13/2021 79
Complications of IABP l Compromised circulation due to catheter l Ischemia – Routine nursing care and monitoring l Compartment syndrome Rare complication seen in the LE (lupus erythematosus) , usually related to infection – 12/13/2021 Monitor calf circumference – 80
Complications of IABP l Hematologic – ALL PATIENTS Typed & Crossmatched!!! l Bleeding – REMOVE THE DRESSING!!! – PUT ON STERILE GLOVES!!! – HOLD PRESSURE!!! l Thrombocytopenia 12/13/2021 – Routine monitoring 81
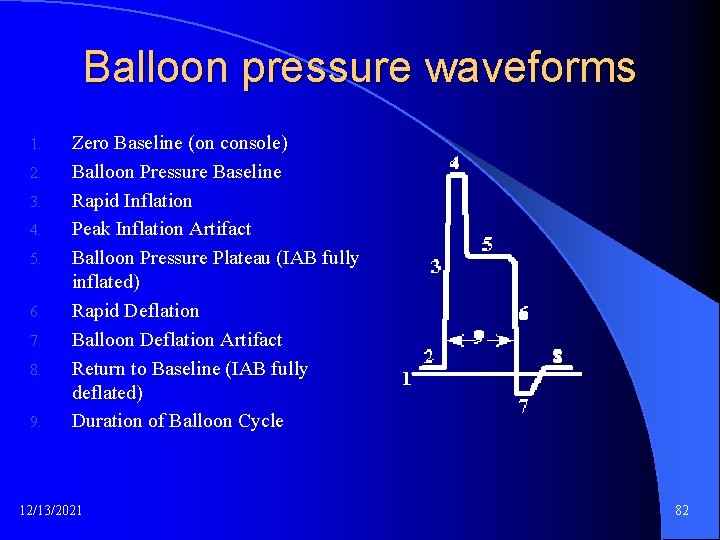
Balloon pressure waveforms 1. 2. 3. 4. 5. 6. 7. 8. 9. Zero Baseline (on console) Balloon Pressure Baseline Rapid Inflation Peak Inflation Artifact Balloon Pressure Plateau (IAB fully inflated) Rapid Deflation Balloon Deflation Artifact Return to Baseline (IAB fully deflated) Duration of Balloon Cycle 12/13/2021 82
European Journal of Cardio-thoracic Surgery 11 (1997) 1176– 1179 Case report Successful surgery for perforation of the thoracic aorta caused by the tip of an intra-aortic balloon pump Thomas Wolff *, Peter Stulz Klinik fu¨r Herz- und Thoraxchirurgie, Kantonsspital, Spitalstrasse 21, CH-4031 Basel, Switzerland We describe a case of perforation of the thoracic aorta caused by the tip of an intraaortic balloon pump. The perforation was confirmed by computed tomography (CT) scan and immediate surgical repair was successful. Vascular injury due to the insertion of an intra-aortic balloon pump is quite common but is predominantly confined to limb ischemia or injury to the femoral or iliac artery. Iatrogenic aortic perforation leading to significant bleeding is much less common and usually fatal. © 1997 Elsevier Science B. V. Keywords: Aortic injury; Intra-aortic balloon pump; Complication 12/13/2021 83
Circ J 2002; 66: 423 – 424 Perforation of the Descending Aorta by the Tip of an Intra-Aortic Balloon Pump Catheter Ryo Shiraishi, MD*; Yukio Okazaki, MD; Kozo Naito, MD; Tsuyoshi Itoh, MD Perforation of the proximal descending aorta occurred in a patient on intra-aortic balloon pump (IABP) supportafter emergency coronary intervention for acute myocardial infarction. The IABP catheter was inserted under fluoroscopic guidance into the right femoral artery without difficulty, but after 8 h on IABP support the patient went into shock with a left hemothorax. Emergency surgery was performed with cardiopulmonary bypass and a perforation of the proximal descending aorta with active bleeding was found and successfully repaired. A distorted descending aorta in which the IABP catheter was kinked, as in the aortic arch, was discovered during surgery and confirmed postoperatively with 3 -dimensional computed tomography scans, particularly in the lateral view. Not only the antero-posterior but also the lateral fluoroscopic view is recommended to prevent aortic perforation by a kinked IABP catheter. (Circ J 2002; 66: 423 – 424) 12/13/2021 84
Heart Inst J 1995; 22: 202 -3 J Thrombosis of the Abdominal Aorta Elisabeth Leude, MD et al A Rare Complication of the lntraaortic Balloon Pumping Device We describe a patient who died due to thrombosis of the abdominal aorta and its branches after placement of an intraaortic balloon pumping device. This rare complication, which occurred despite careful insertion technique, underscores the need to select balloon size as a function of the individual patient's morphology. (C omplication rates associated with the use of an intraaortic balloon pump(IABP) range from 10% to 20%. '5 Trauma-related complications are themost frequent, including dissection, perforation, and thromboembolism. We describe a patient who died of thrombosis of the abdominal aorta and itsbranches subsequent to intraaortic balloon pumping. To our knowledge, this complication has been reported only once before in the literature. 12/13/2021 85
Conclusions l . The consistent application of intra-aortic balloon pump support of patients with coronary artery disease and its complications has provided a therapeutic platform for direct surgical intervention on otherwise unstable patients with cardiac ischemia, heart failure, and shock. l This integrated approach to the treatment of patients with coronary artery disease has profoundly affected how this disease process is managed throughout the world. 12/13/2021 86
l Maintain systemic arterial pressure with fluid resuscitation and vasopressors/beta-adrenergic agents if necessary. l Consider transfer to a hyperbaric chamber. Potential benefits of this therapy include (1) compression of existing air bubbles, (2) establishment of a high diffusion gradient to speed dissolution of existing bubbles, and (3) improved oxygenation of ischemic tissues and lowered intracranial pressure. l Circulatory collapse should be addressed with CPR and consideration of more invasive procedures
GOALS OF INFLATION l Increase coronary perfusion pressure l Increase systemic perfusion pressure and peripheral oxygen supply l Increase baroreceptor response and decrease SNS stimulation – Decrease SVR – Decrease HR
Goals of Deflation l Decreases afterload – Decrease MVO 2 – Decrease assisted peak systolic pressure(APSP) – Increase cardiac output and ejection fraction (increase forward flow)
Why Inflation Works: Inflation of the IAB during diastole increases aortic volume and pressure. Why Deflation Works: IAB deflation just prior to systole creates a potential space in the aorta. This reduces aortic volume and pressure.
Inflation Timing: The IAB is inflated immediately upon closure of the aortic valve. Deflation Timing: The balloon must be deflated before the full onset of systole.
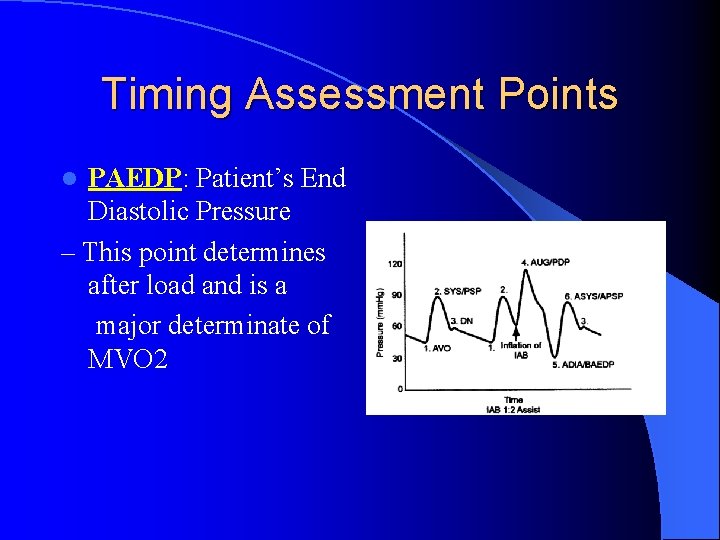
Timing Assessment Points PAEDP: Patient’s End Diastolic Pressure – This point determines after load and is a major determinate of MVO 2 l
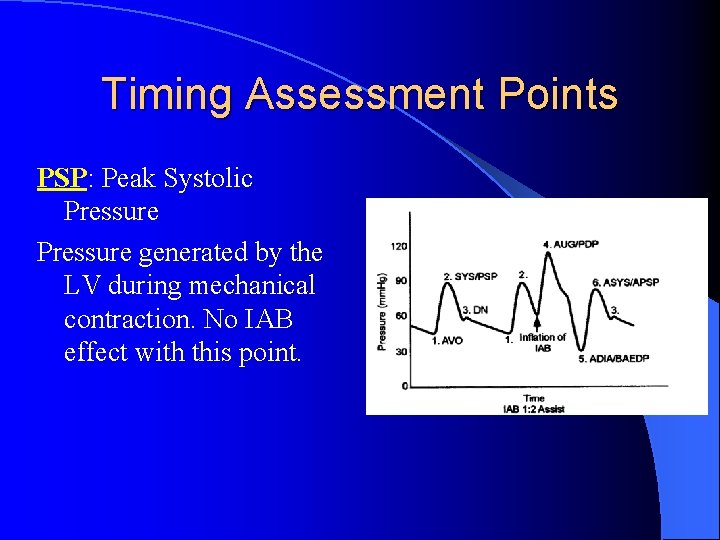
Timing Assessment Points PSP: Peak Systolic Pressure generated by the LV during mechanical contraction. No IAB effect with this point.
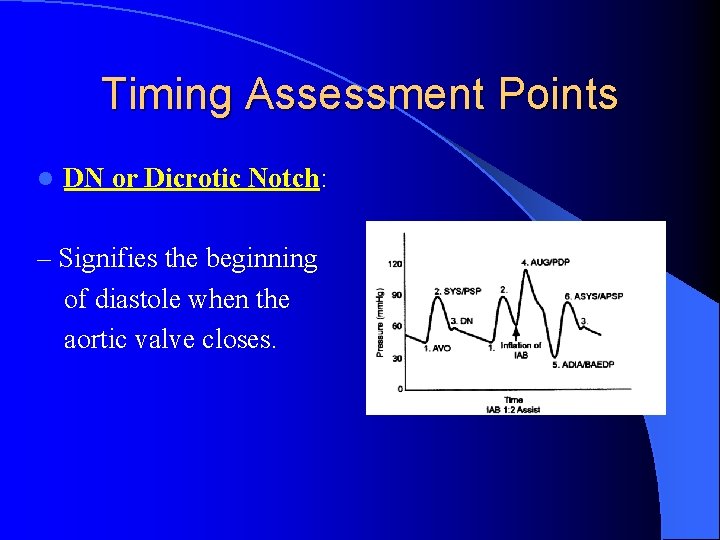
Timing Assessment Points l DN or Dicrotic Notch: – Signifies the beginning of diastole when the aortic valve closes.
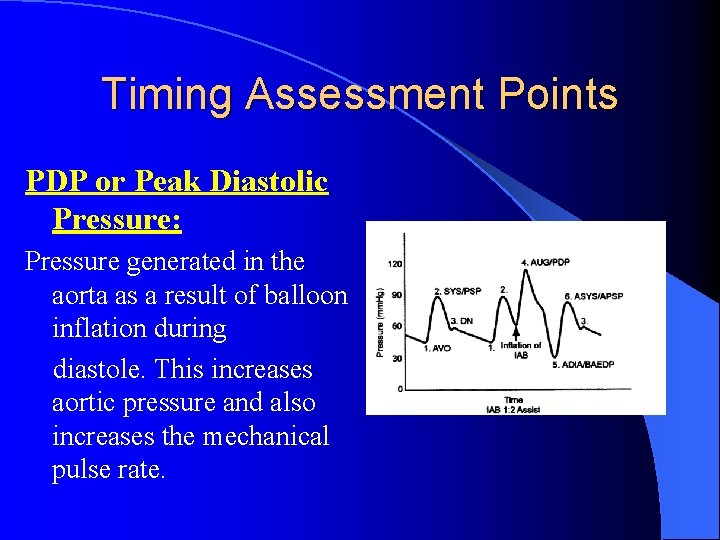
Timing Assessment Points PDP or Peak Diastolic Pressure: Pressure generated in the aorta as a result of balloon inflation during diastole. This increases aortic pressure and also increases the mechanical pulse rate.
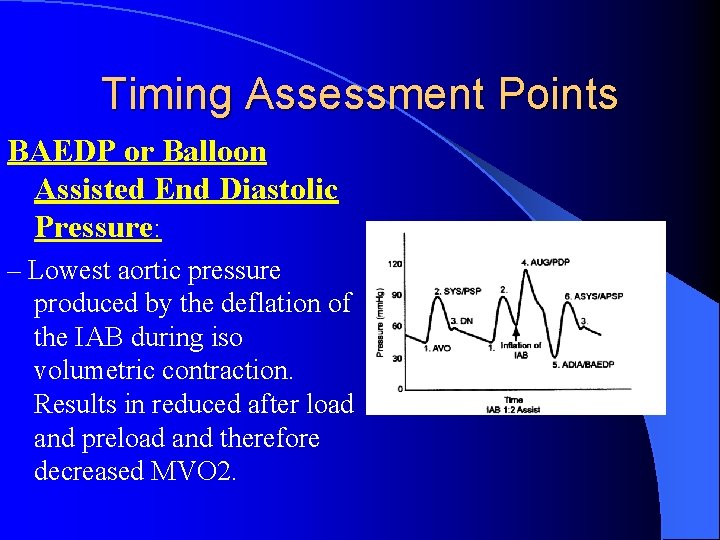
Timing Assessment Points BAEDP or Balloon Assisted End Diastolic Pressure: – Lowest aortic pressure produced by the deflation of the IAB during iso volumetric contraction. Results in reduced after load and preload and therefore decreased MVO 2.
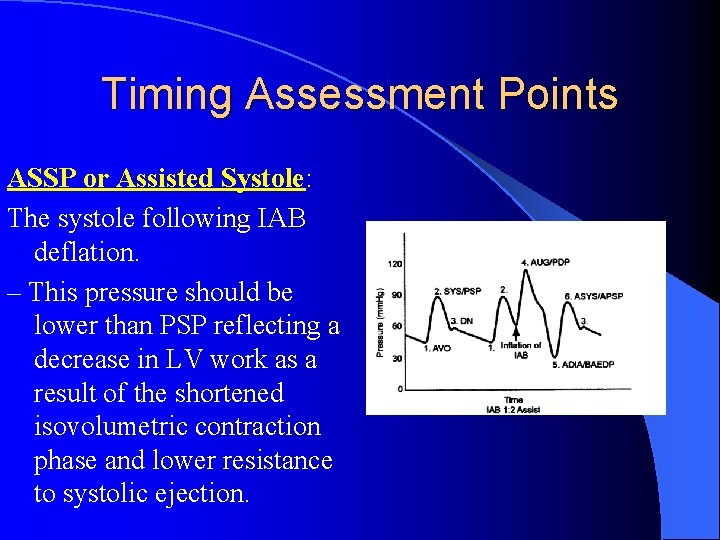
Timing Assessment Points ASSP or Assisted Systole: The systole following IAB deflation. – This pressure should be lower than PSP reflecting a decrease in LV work as a result of the shortened isovolumetric contraction phase and lower resistance to systolic ejection.
Augmented Diastolic Pressure (Peak Diastolic Pressure) l Caused by increased pressure (volume) in aorta during diastole l PDP should be > than PSP l The amount of augmentation will be affected by the timing of balloon inflation Maximal augmentation: Balloon inflation 40 msec prior to dicrotic notch
High Augmentation Risks of increased augmentation (or PDP) are l mechanical l In low cardiac output states the benefits l outweigh the risks l High augmentation post cardiac surgery – Benefits: Maintenance of coronary graft patency – Risks: Bleeding and disruption of suture sites – Use of vasodilators – Lower placement l
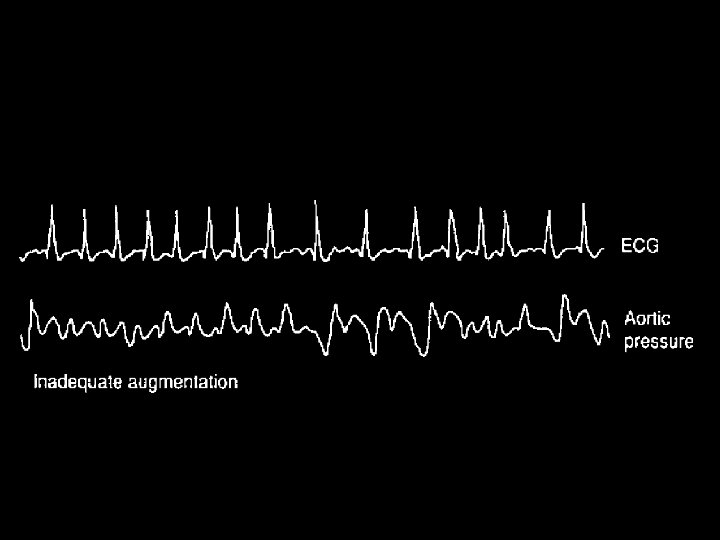
Low Augmentation l Weaning states l Low volume or output states
Early Inflation: Prior to Closure of Aortic Valve l Increased aortic pressure: regurgitation of blood into the LV l Rise in aortic pressure will prematurely close the aortic valve: decrease LV emptying l Rise in LVEDP with no change in systemic pressure
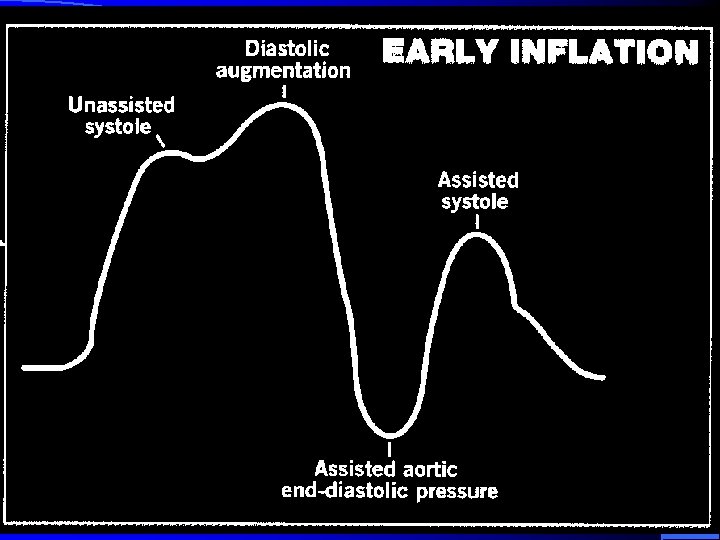
Early Inflation: Prior to Closure of Aortic Valve Increased ESV / ESP l Increased work and oxygen requirements l Increased Preload l Significantly impaired l Increased MVO 2 LV function l Increased Stroke Work l Decreased cardiac output and systemic l Decreased SV perfusion l Decreased CO l
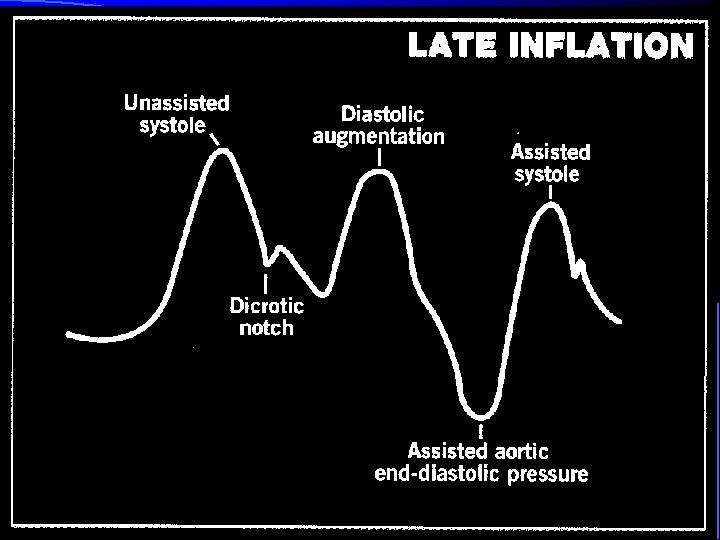
Late Inflation: After Closure of Aortic Valve l PDP (augmentation) is decreased -Systolic volume has run off to peripheral circulation l PDP (augmentation) is less than optimal -Decreased perfusion pressure and volume to coronary arteries
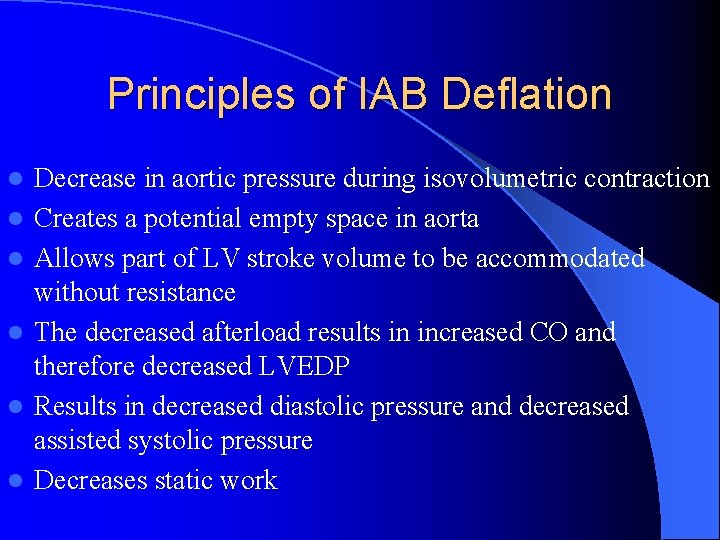
Principles of IAB Deflation l l l Decrease in aortic pressure during isovolumetric contraction Creates a potential empty space in aorta Allows part of LV stroke volume to be accommodated without resistance The decreased afterload results in increased CO and therefore decreased LVEDP Results in decreased diastolic pressure and decreased assisted systolic pressure Decreases static work
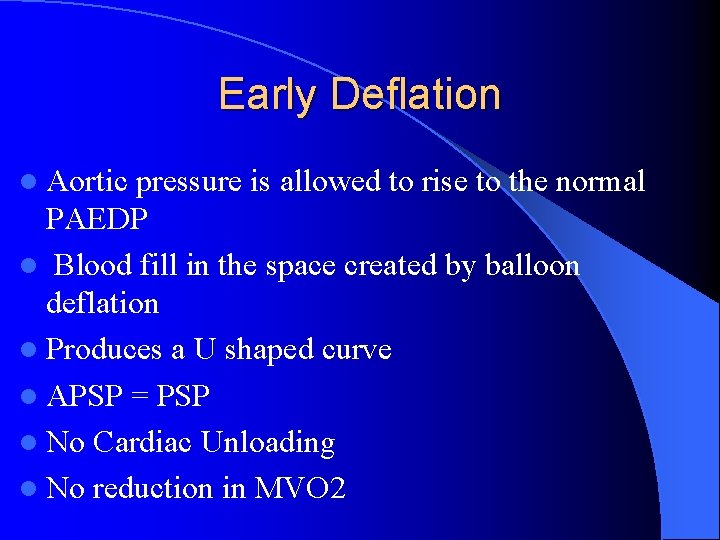
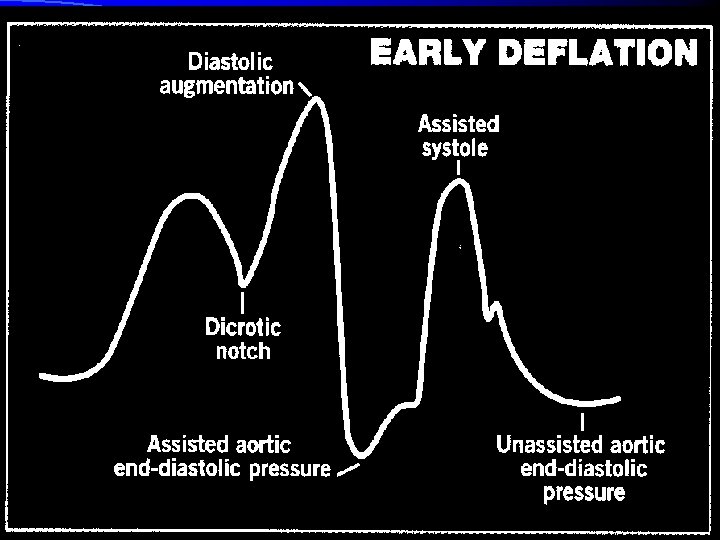
Early Deflation l Aortic pressure is allowed to rise to the normal PAEDP l Blood fill in the space created by balloon deflation l Produces a U shaped curve l APSP = PSP l No Cardiac Unloading l No reduction in MVO 2
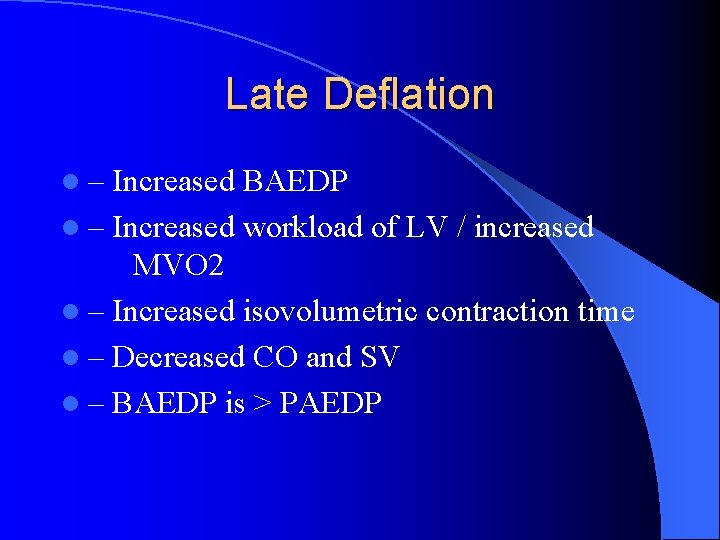
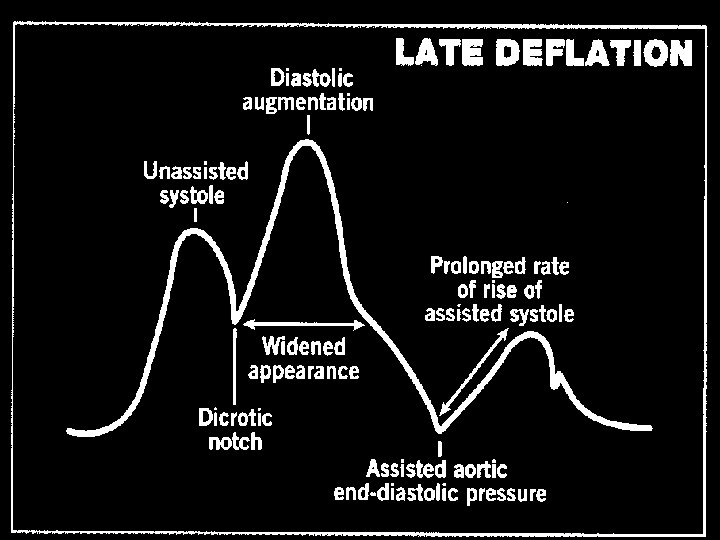
Late Deflation l– Increased BAEDP l – Increased workload of LV / increased MVO 2 l – Increased isovolumetric contraction time l – Decreased CO and SV l – BAEDP is > PAEDP
Trouble Shooting
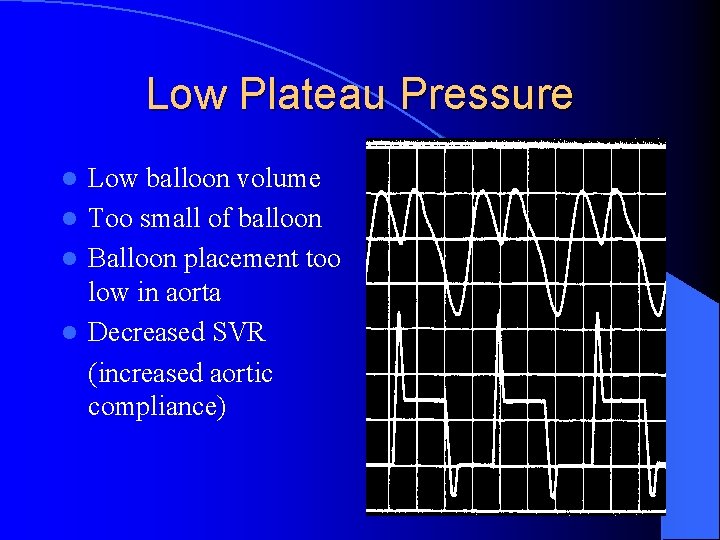
Low Plateau Pressure Low balloon volume l Too small of balloon l Balloon placement too low in aorta l Decreased SVR (increased aortic compliance) l
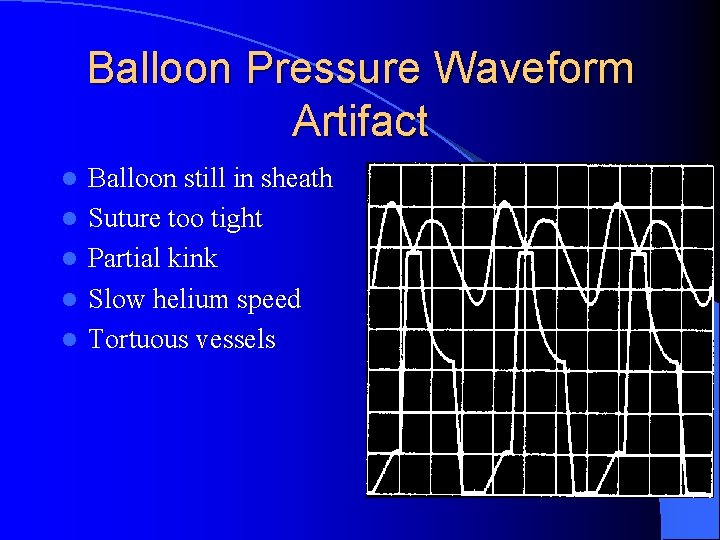
Balloon Pressure Waveform Artifact l l l Balloon still in sheath Suture too tight Partial kink Slow helium speed Tortuous vessels
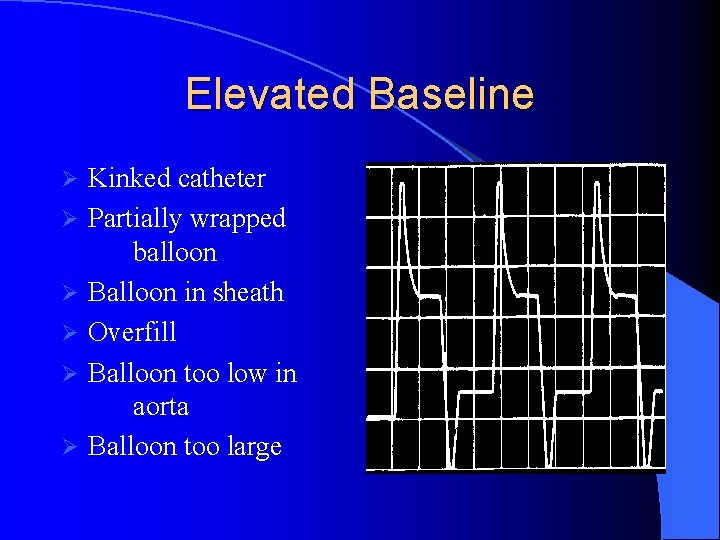
Elevated Baseline Ø Ø Ø Kinked catheter Partially wrapped balloon Balloon in sheath Overfill Balloon too low in aorta Balloon too large
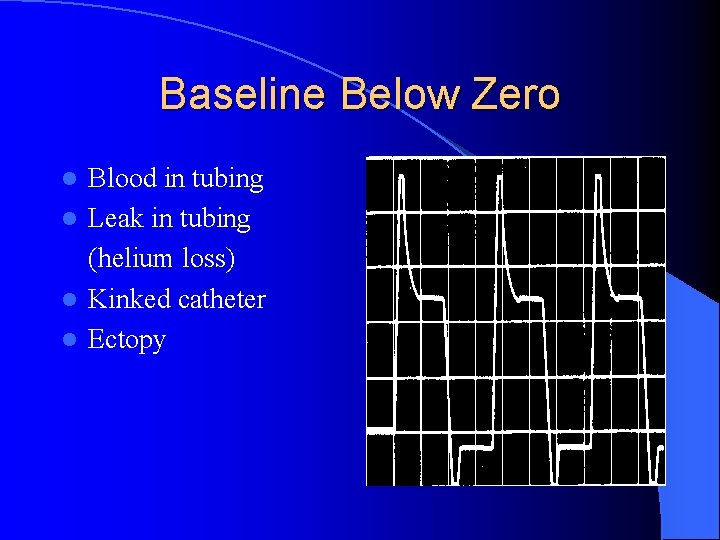
Baseline Below Zero Blood in tubing l Leak in tubing (helium loss) l Kinked catheter l Ectopy l
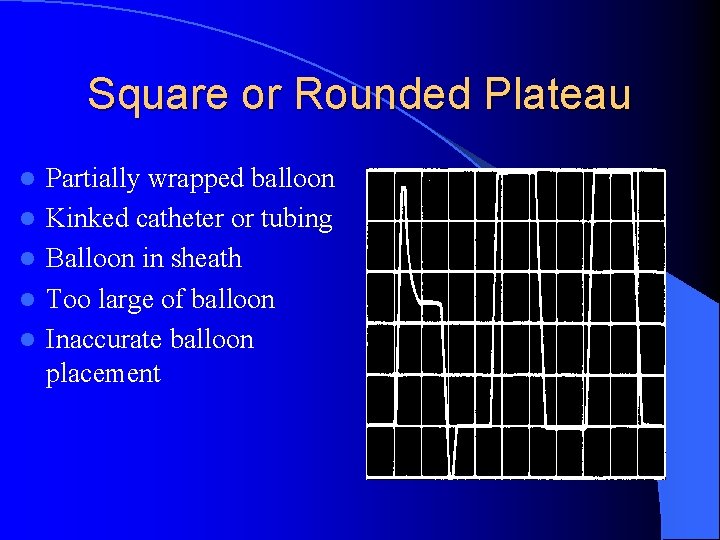
Square or Rounded Plateau l l l Partially wrapped balloon Kinked catheter or tubing Balloon in sheath Too large of balloon Inaccurate balloon placement
Discussion of Key Nursing Considerations l l l l Pressure assessment for optimization of therapy Balloon mobility Left radial pulse assessment Urine output Distal pulse assessment Groin care Platelets Other complications
ADVANTAGES OF BALLOON COUNTER PULSATIONS l Circulatory assistance can be maintained for prolonged periods without clinically significant hemolysis. l Single arterial puncture is required. l Coronary blood flow augmented in hypotensive state. l Dormant inter coronary beds are opened. l Early institution of IABP decreases the size of potential MI after coronary occlusion.
INDICATIONS OF IABP CARDIOGENIC SHOCK : l Mean arterial pressure < 60 mm. Hg l Systolic arterial pressure < 90 mm. Hg l CI < 2. 0 L/min /M 2 l Urine output <20 -30 ml /hr l Wedge pressure > 18 mm. Hg l Such patients have poor prognosis with high mortality. l Not responding to medical management indication of IABP. l 75% patients have hemodynamic improvement.
UNSTABLE ANGINA : l Pre infarction unstable angina - Worse prognosis - Due to circulatory support it lessens the ischemic injury during the period of induction and prior to CPB l Post infarction unstable angina - Suggestive of viable but threatened myocardium - Predictive of early re-infarction and death. - 6 months mortality – 72% - IABP stabilizes the patient prior to revascularization.
l Study by Bardet for such patients Total 21 patient of post infarction unstable angina kept on IABP 4 – inoperable – 2 deaths – 6 months 17 – operated - 1 death 14 – pain free – 28 months follow up
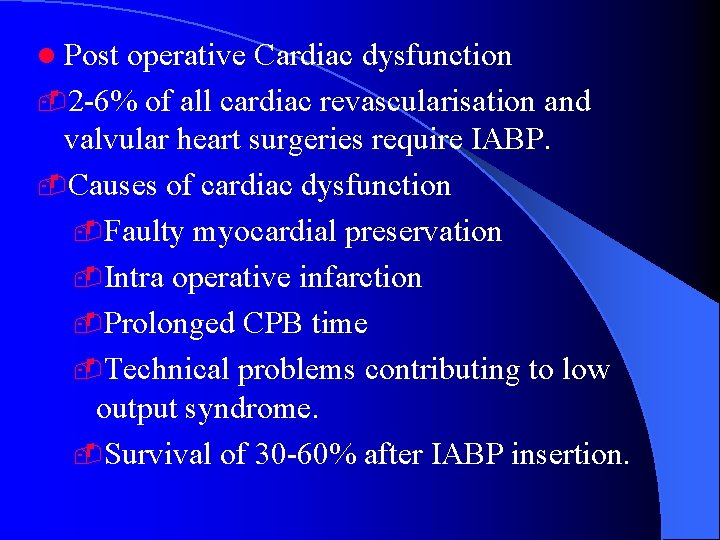
l Post operative Cardiac dysfunction -2 -6% of all cardiac revascularisation and valvular heart surgeries require IABP. -Causes of cardiac dysfunction -Faulty myocardial preservation -Intra operative infarction -Prolonged CPB time -Technical problems contributing to low output syndrome. -Survival of 30 -60% after IABP insertion.
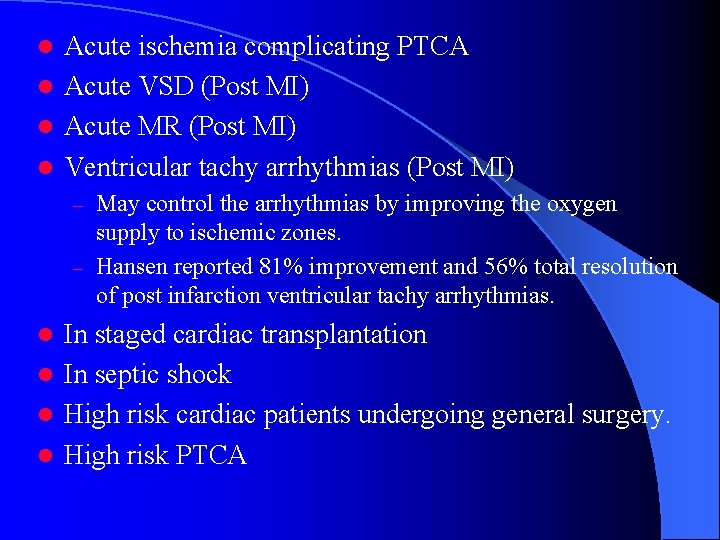
Acute ischemia complicating PTCA l Acute VSD (Post MI) l Acute MR (Post MI) l Ventricular tachy arrhythmias (Post MI) l May control the arrhythmias by improving the oxygen supply to ischemic zones. – Hansen reported 81% improvement and 56% total resolution of post infarction ventricular tachy arrhythmias. – In staged cardiac transplantation l In septic shock l High risk cardiac patients undergoing general surgery. l High risk PTCA l
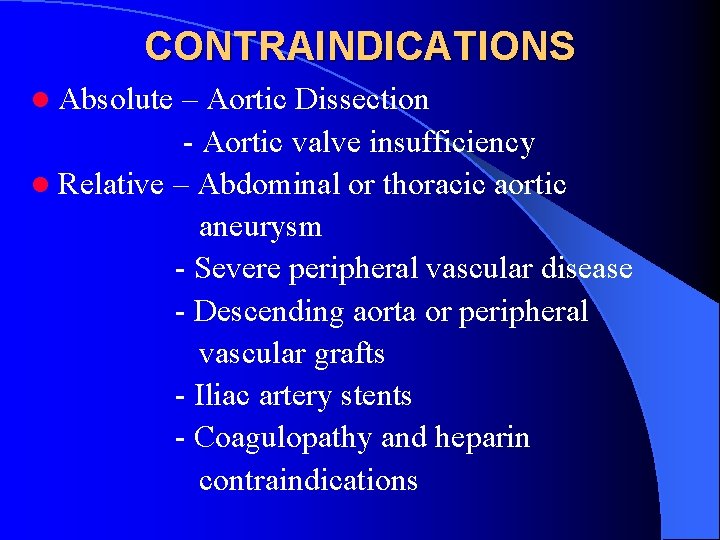
CONTRAINDICATIONS l Absolute – Aortic Dissection - Aortic valve insufficiency l Relative – Abdominal or thoracic aortic aneurysm - Severe peripheral vascular disease - Descending aorta or peripheral vascular grafts - Iliac artery stents - Coagulopathy and heparin contraindications
MONITORING A IABP PATIENT l X-ray to verify the catheter position l IV heparin to maintain ACT > 150 l Daily hemoglobin and platelet counts to monitor hemolysis and thrombocytopenia
CARE OF THE PATIENT l Supine position l Assessed leg should be secured l Prophylactic antibiotics l Blood samples should not be obtained from central lumen of IABP for the risk of clotting the lumen
TRIGGERING l Surface electrocardiogram l Arterial pressure wave form l Paced rhythm l Internal asynchronous mode
TIMING l Inflation – On the down slope of systolic wave form just before the dicrotic notch. l Deflation – Prior to the onset of next systolic waveform
l Early Inflation – Increase after load - Increase LV stress - Increase myocardial O 2 demand - Decreased stroke volume l Late Inflation – Diminished diastolic pressure augmentation - Sub optimal coronary perfusion
l Early Deflation – Sub optimal augmentation - Sub optimal after load reduction. - Sub optimal coronary perfusion l Late Deflation – Impaired left ventricular emptying - Increased after load and pre load - Increased myocardial O 2 consumption l Arrhythmias – 1: 2 augmentation
IN CASE OF TROUBLE l Check for loose connections l Balloon rupture – blood in tube l Poor augmentation Adjust timing – Change trigger mode – Evaluate the inflation with deflation under fluoroscopy – Inject dye to rule out false lumen –
IABP Evidence A randomized comparison of intraaortic balloon pumping after primary coronary angioplasty in high risk patients with acute MI treated Van ‘t Hoft 1999, Eur Heart J
SHOCK Result IABP vs. no IABP mortality after adjustement for revascularisation p=0. 313 Use of IABP with or without thrombolysis improves survival in pts with cardiogenic shock because of the higher rate of attempted revascularisation in the IABP group Sanborn et al. J Am Coll Cardiol 2000; 36: 1123
COMPLICATIONS l Risk factors - Age - Female sex - Pre existing PVD - H/0 smoking - Catheter size
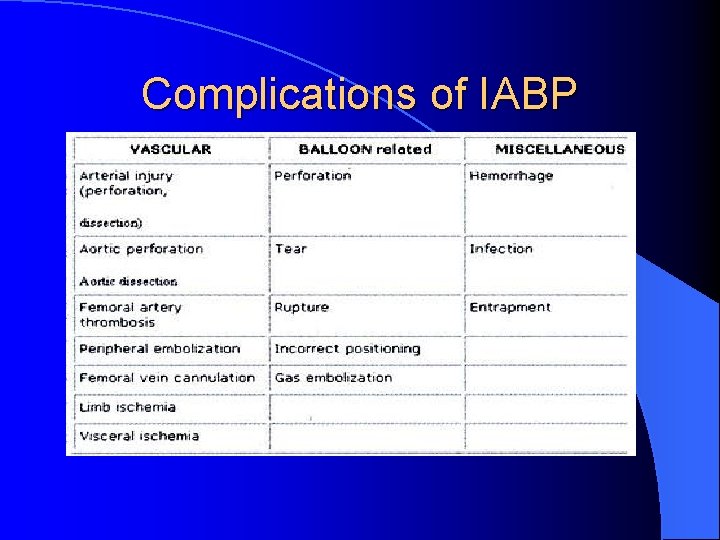
Complications of IABP
VASCULAR COMPLICATIONS l Ischemia - Removal of catheter / sheath - Embolectomy - Bypass - Rarely Amputation l Bleeding - 1 -5% hematoma formation - Requires blood transfusion - Direct repair of vessel - Pseudo aneurysm
BALLOON RUPTURE l Considered when blood in tubing l Due to surface damage against the calcific arterial plaques l Helium gas embolism. l Rupture may cause entrapment BALLOON ENTRAPMENT - Thrombolysis - Surgical removal
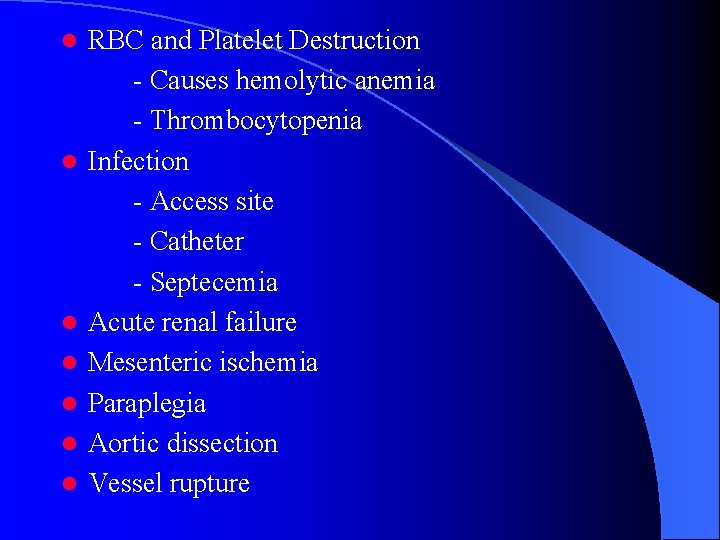
l l l l RBC and Platelet Destruction - Causes hemolytic anemia - Thrombocytopenia Infection - Access site - Catheter - Septecemia Acute renal failure Mesenteric ischemia Paraplegia Aortic dissection Vessel rupture
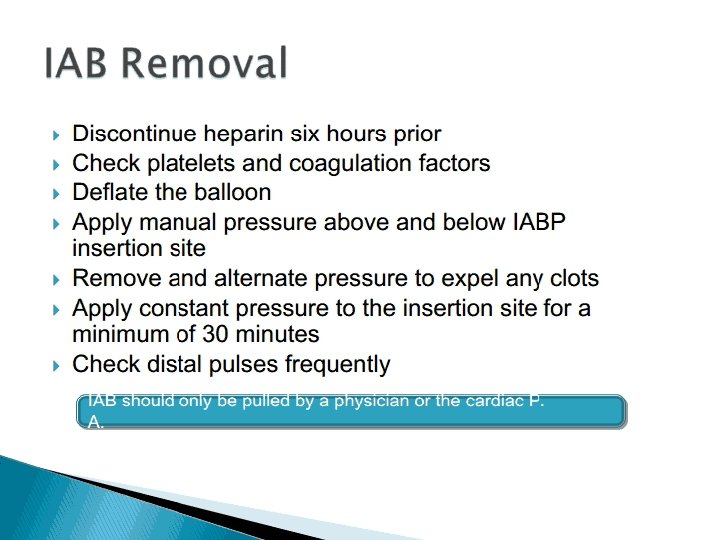
REMOVAL OF IABP l Weaning l Withdrawal l Percutaneous – manual removal l Open – Surgical removal with hemostasis

- Slides: 142