Intestinal Stomas Stoma or ostomy Definition An intestinal
- Slides: 42
Intestinal Stomas
Stoma or -ostomy • Definition: • An intestinal stoma is an opening of the intestinal or urinary tract onto the abdominal wall, constructed surgically or appearing inadvertently. • The techniques of fashioning a stoma have been developed to provide – a cure or palliation for benign or malignant diseases – to provide diversion of waste until conditions are attained that permit the restoration of normal intestinal continuity
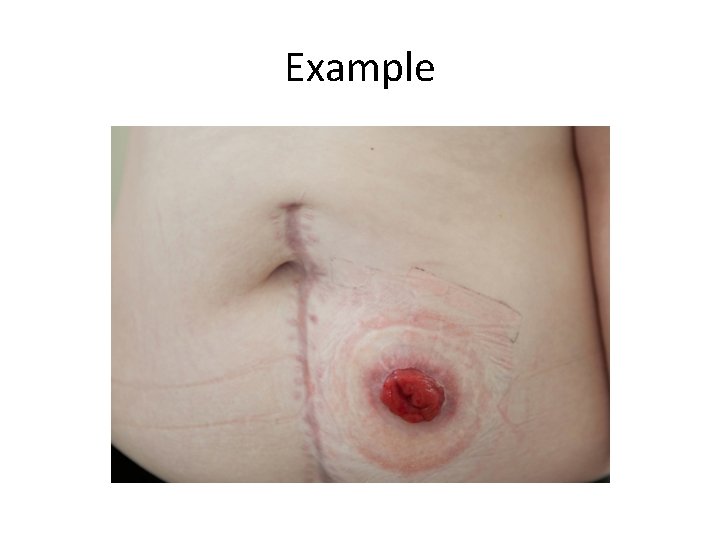
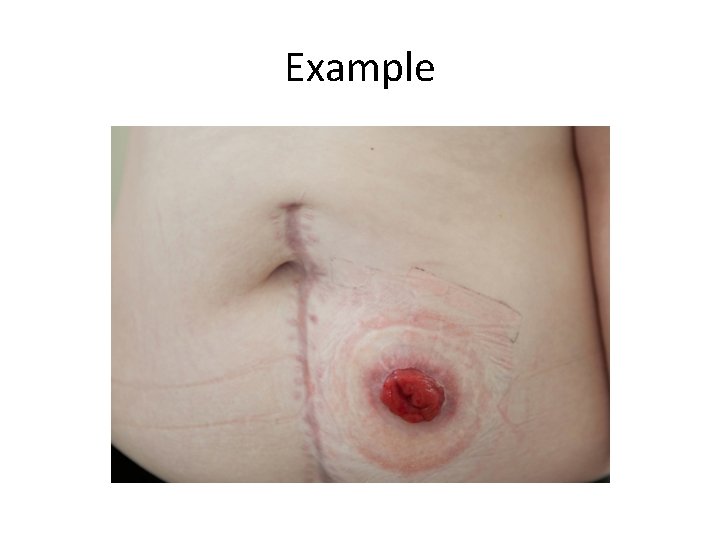
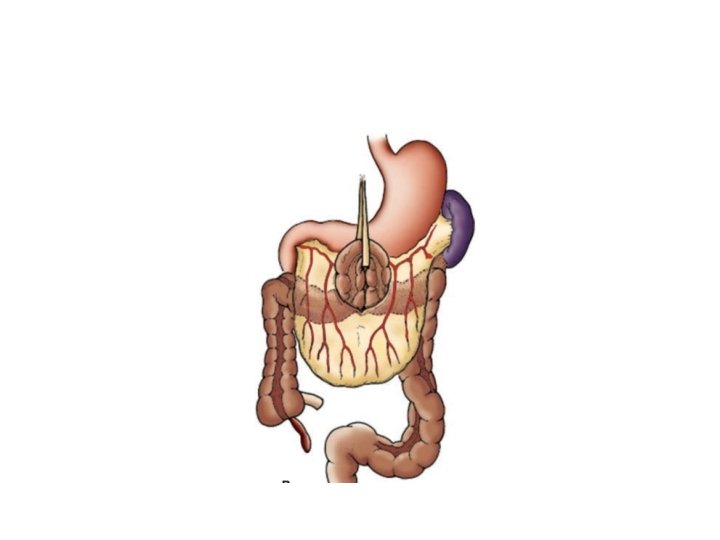
Example
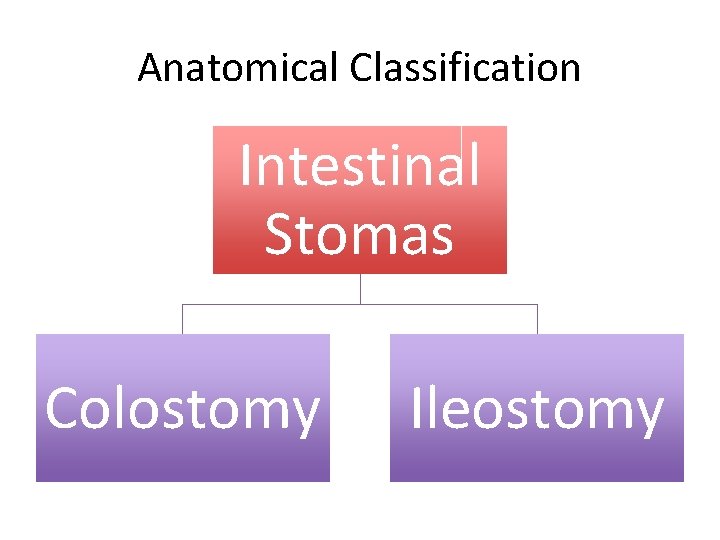
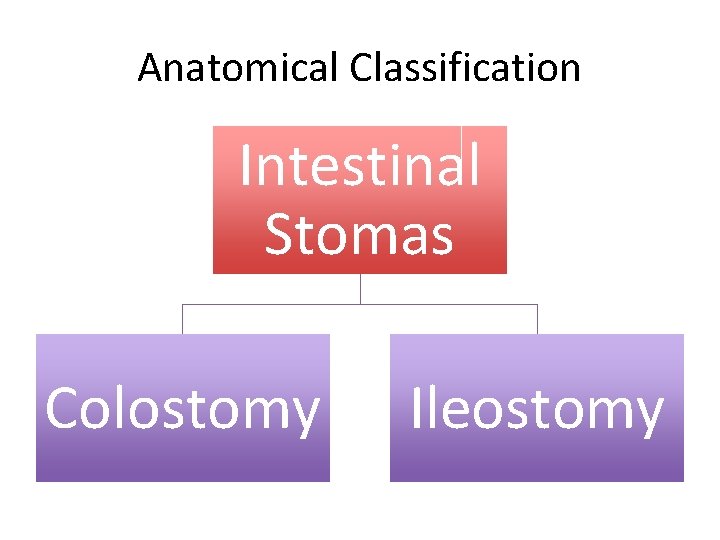
Anatomical Classification Intestinal Stomas Colostomy Ileostomy
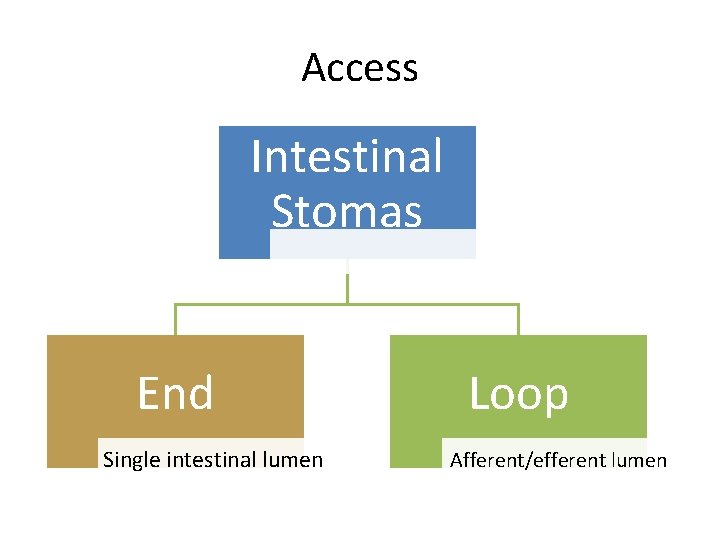
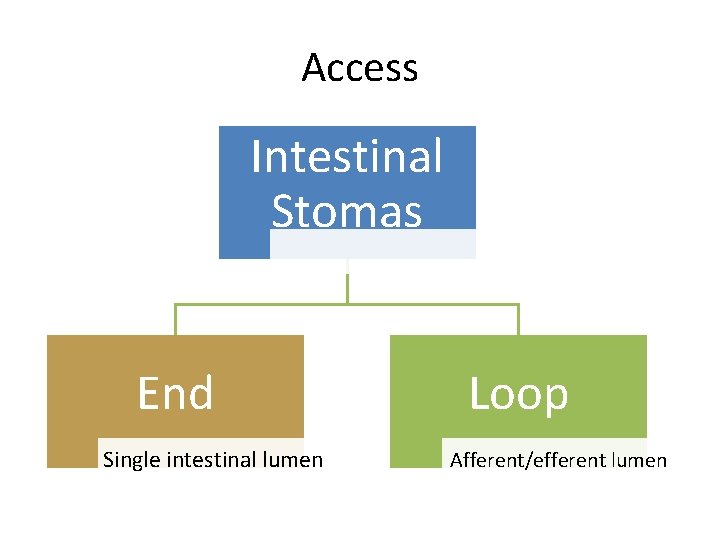
Access Intestinal Stomas End Single intestinal lumen Loop Afferent/efferent lumen
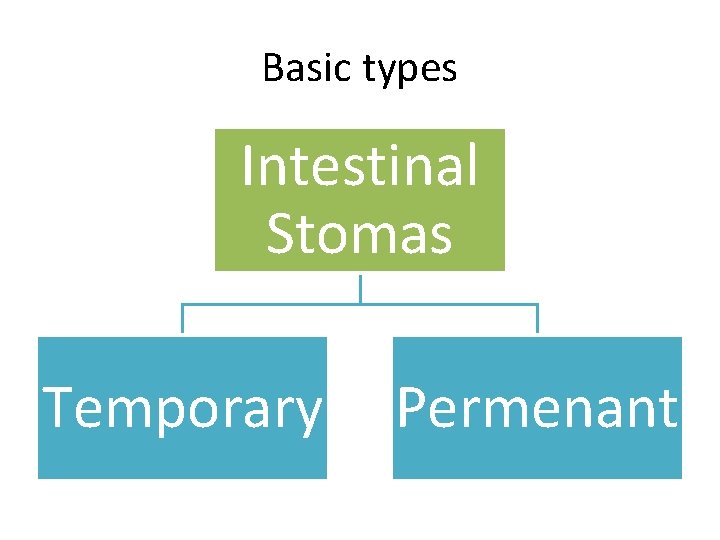
Basic types Intestinal Stomas Temporary Permenant
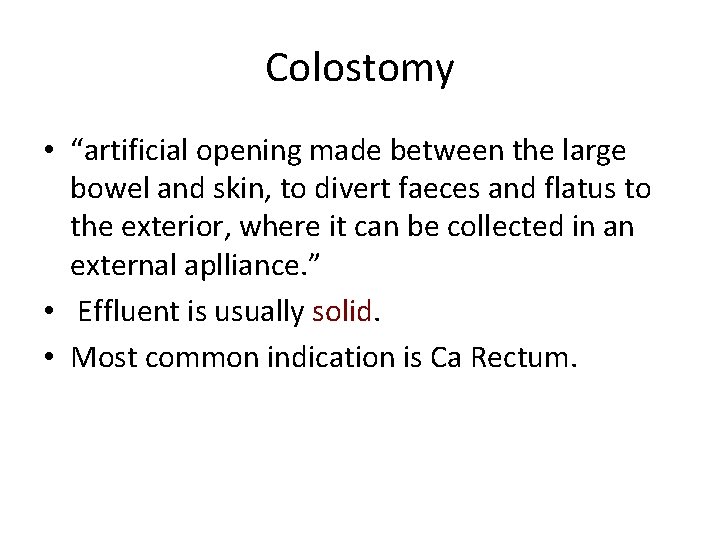
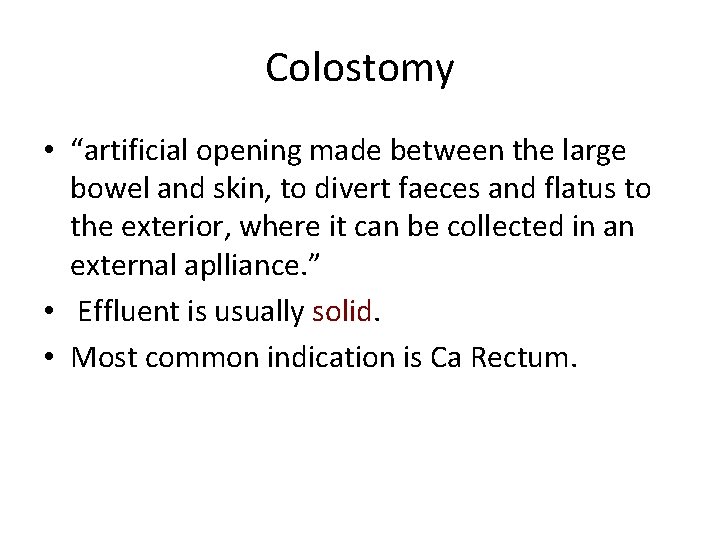
Colostomy • “artificial opening made between the large bowel and skin, to divert faeces and flatus to the exterior, where it can be collected in an external aplliance. ” • Effluent is usually solid. • Most common indication is Ca Rectum.
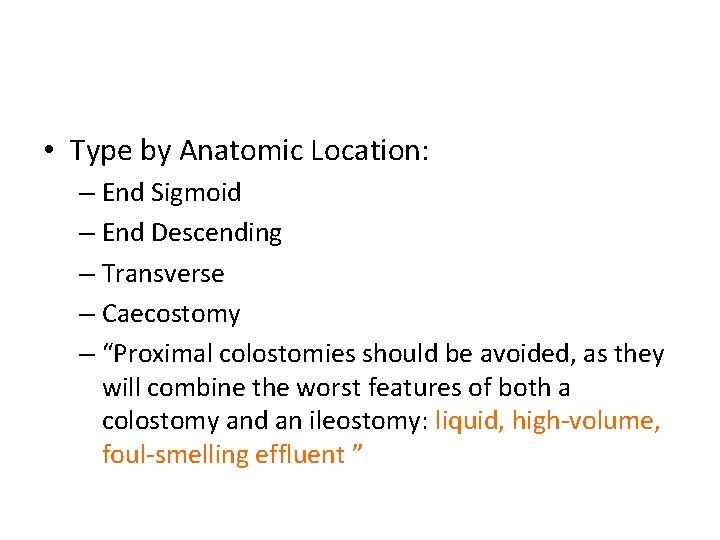
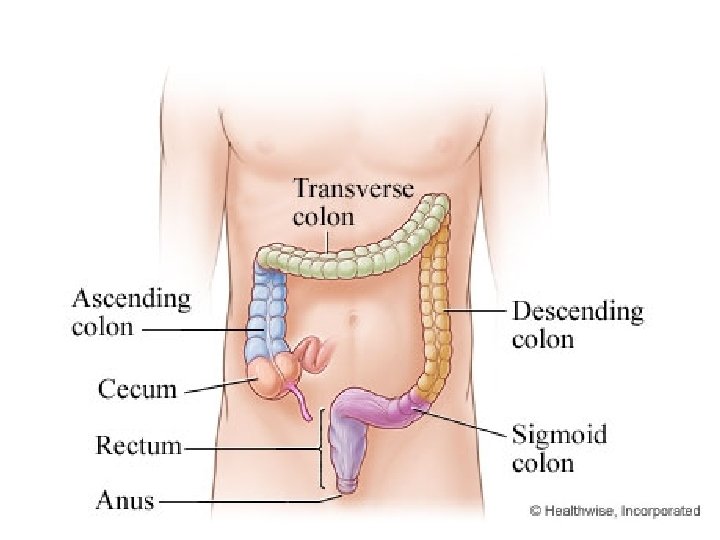
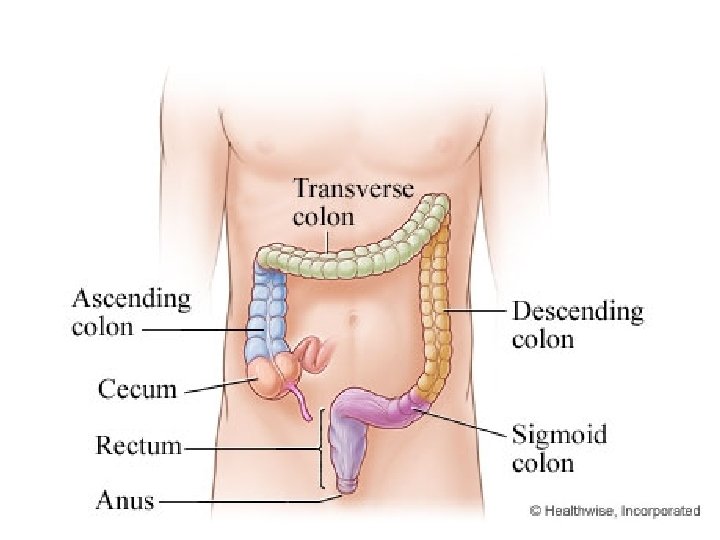
• Type by Anatomic Location: – End Sigmoid – End Descending – Transverse – Caecostomy – “Proximal colostomies should be avoided, as they will combine the worst features of both a colostomy and an ileostomy: liquid, high-volume, foul-smelling effluent ”
• Indications : Temporary Colostomy – Distal Obstruction. – Defunction a low rectal anastomosis after Anterior resection of the rectum. – Following traumatic injury to the rectum or colon. – During operative treatment of a high fistula in ano. – Fulminant Colitis (IBD). – Complicated Diverticular disease. – [Loop, Double barreled, Haartman’s procedure ]
• Indications: Permenant Colostomy: – Rectal carcinoma excision( A-P resection) ----- End colostomy – Inoperable rectal or colonic carcinoma ------ Loop colostomy
• Type by Purpose: • (1) to provide decompression of the large intestine- Decompression Colostomy • (2) to provide diversion of the feces- Diversion Colostomy
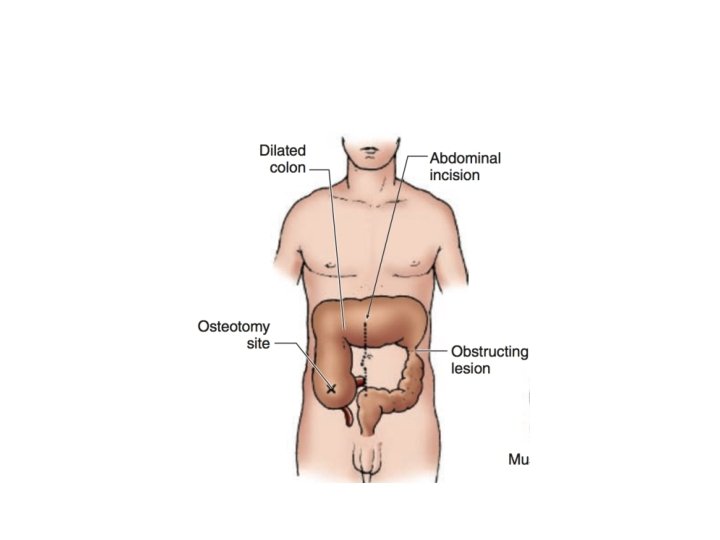
Decompression Colostomy • constructed for distal obstructing lesions: • procedure acts as a bridge to definitive operation for toxic patients with benign disease and those with malignant distal obstruction. • Indications: – dilation of the proximal colon without ischemic necrosis – severe sigmoid diverticulitis with phlegmon – selected patients with toxic megacolon.
Types : Decompression Colostomy • “blow-hole” decompressing colostomy constructed in the cecum or transverse colon. • Tube cecostomy. • Loop colostomy
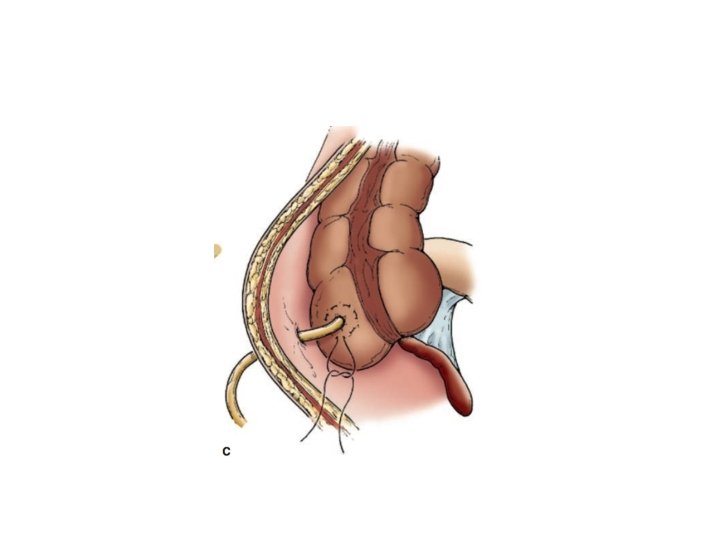
Tube Cecostomy • reserved for the severely, acutely ill patient with massive distention and impending perforation of the colon. • Usually Emergency operation. • Disadvantages: – blocked with feces, drain poorly, and sometimes leak stool adjacent to the drain. • Indicated in: – distal obstructing cancer – pseudo-obstruction syndromes seen in elderly or immuno-compromised patients.
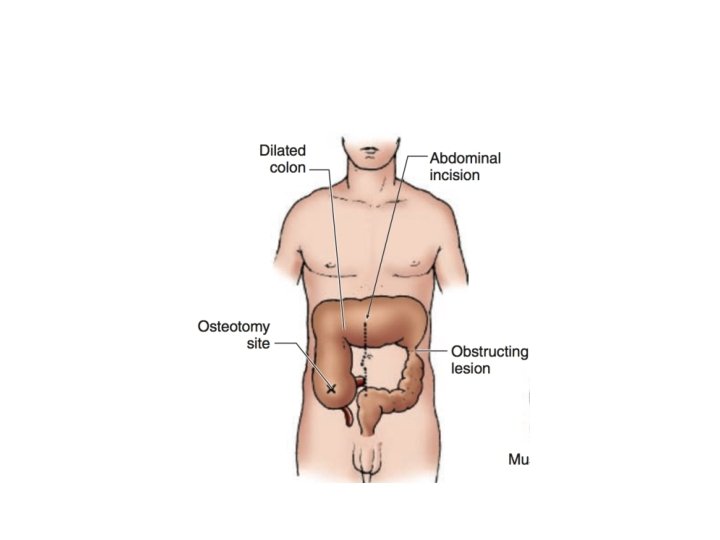
“Blow hole” Colostomy • Reserved in patients with massive distention and impending perforation of the colon.
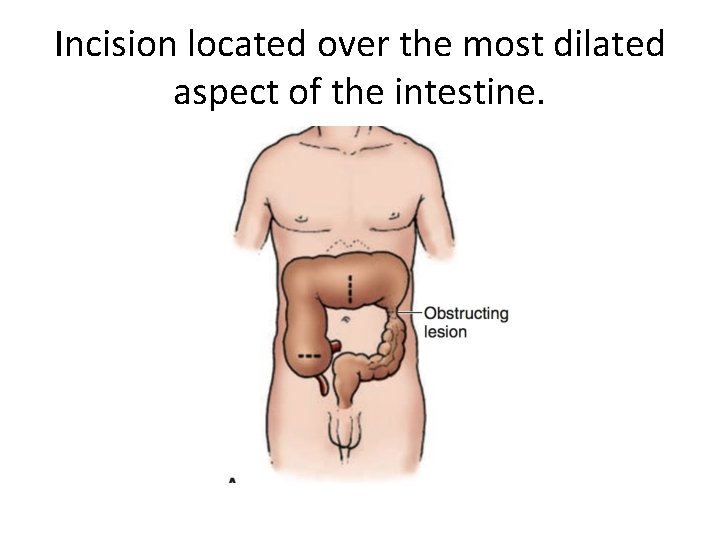
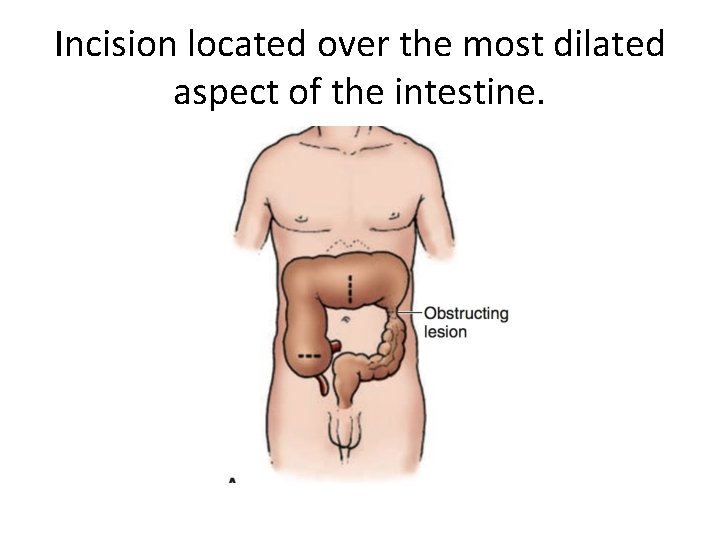
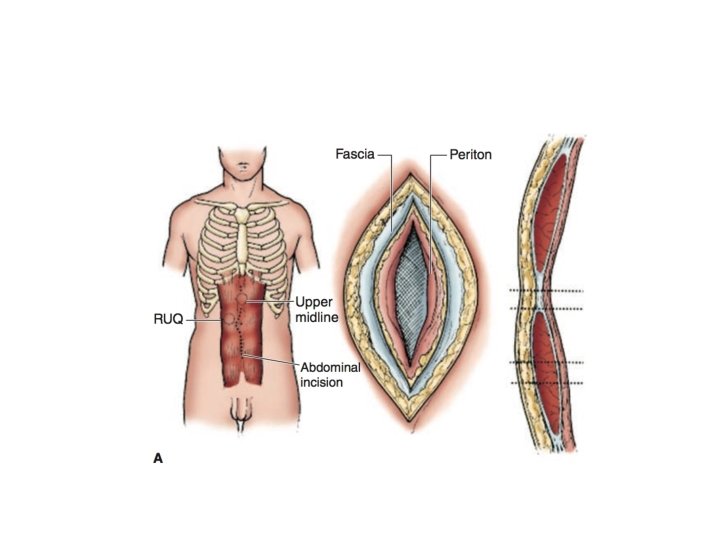
Incision located over the most dilated aspect of the intestine.
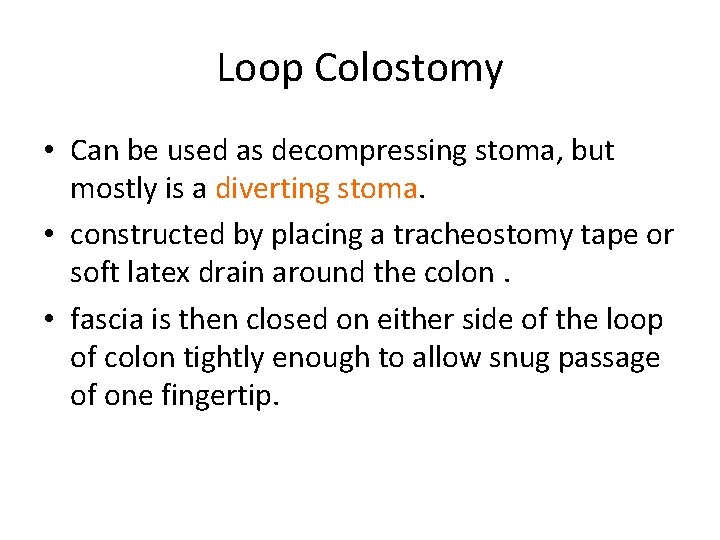
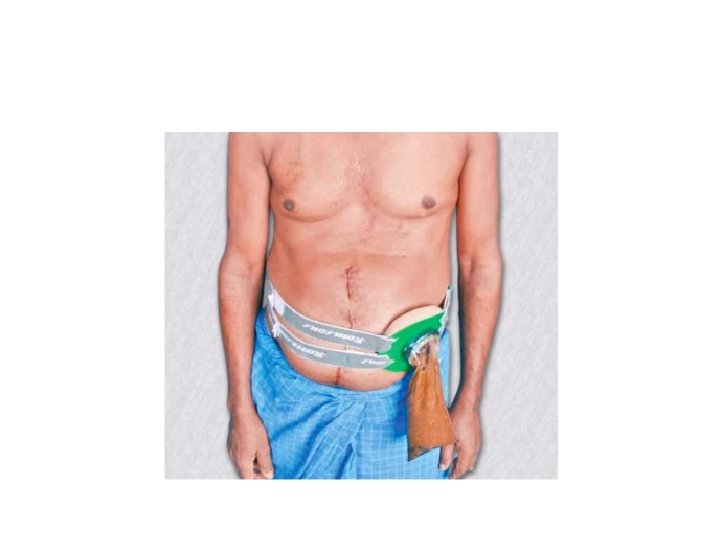
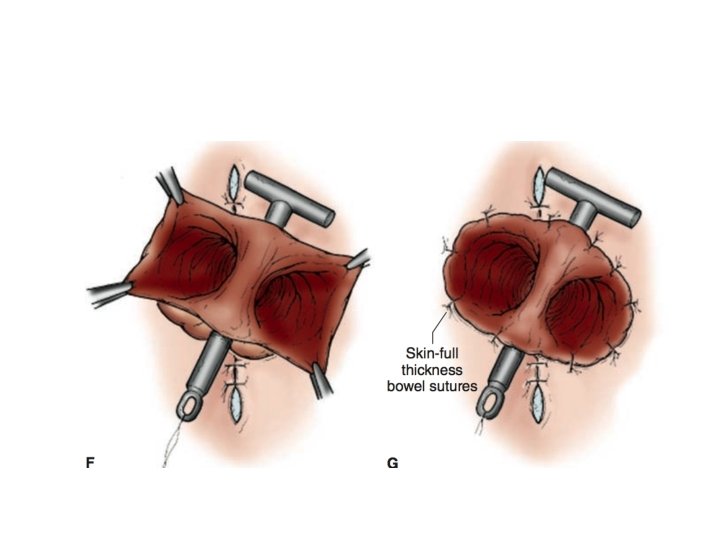
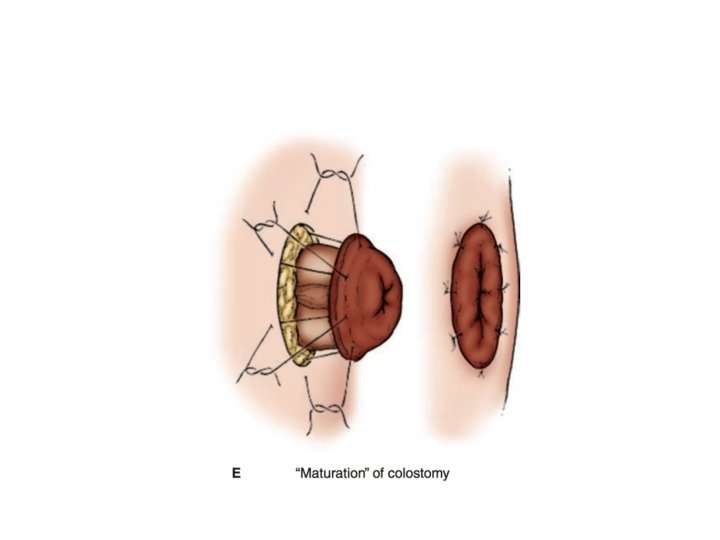
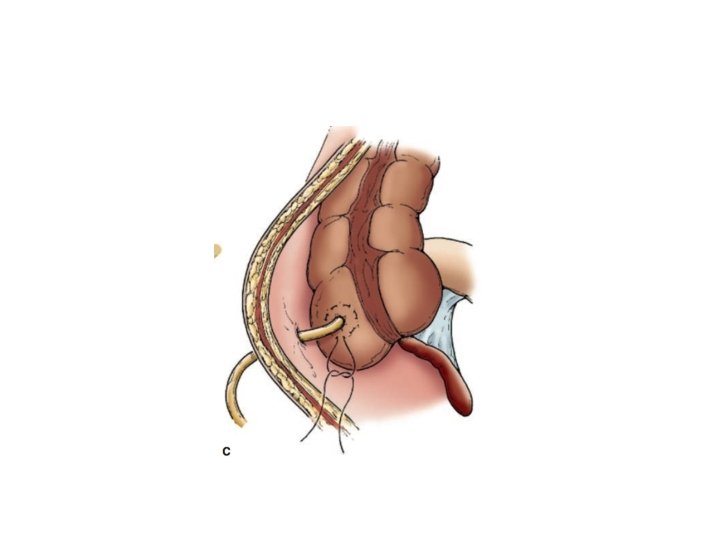
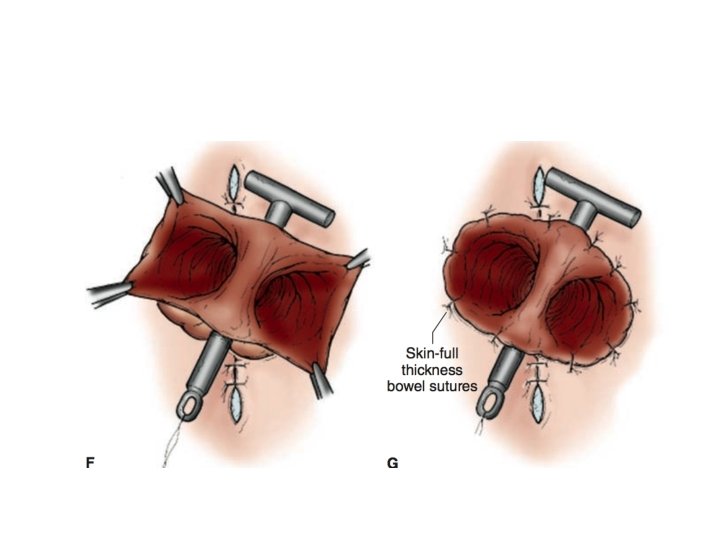
Loop Colostomy • Can be used as decompressing stoma, but mostly is a diverting stoma. • constructed by placing a tracheostomy tape or soft latex drain around the colon. • fascia is then closed on either side of the loop of colon tightly enough to allow snug passage of one fingertip.
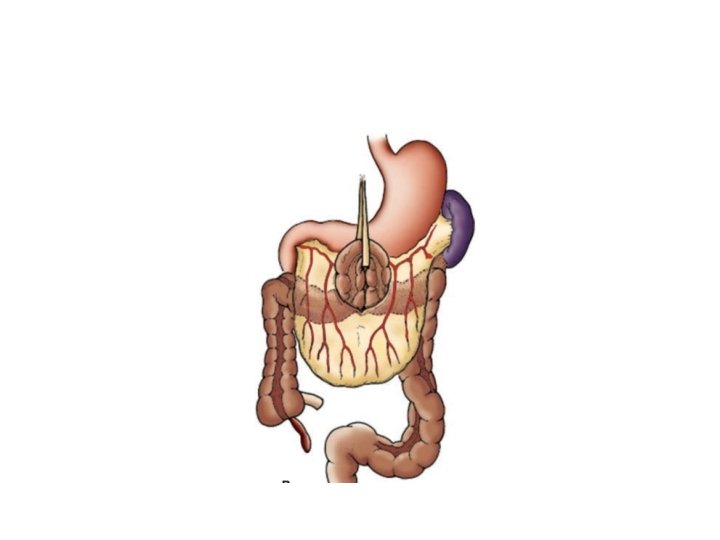
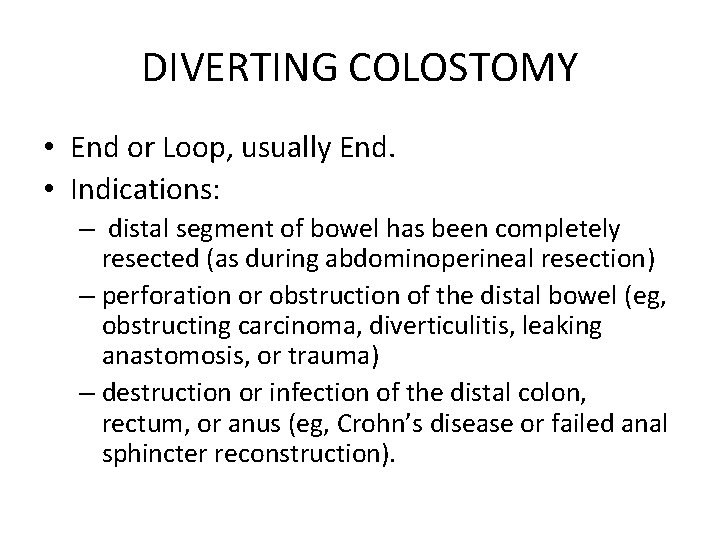
DIVERTING COLOSTOMY • End or Loop, usually End. • Indications: – distal segment of bowel has been completely resected (as during abdominoperineal resection) – perforation or obstruction of the distal bowel (eg, obstructing carcinoma, diverticulitis, leaking anastomosis, or trauma) – destruction or infection of the distal colon, rectum, or anus (eg, Crohn’s disease or failed anal sphincter reconstruction).
Complications • Generally: – Irreguarity of function – seepage of mucus and maceration of the skin because an appliance seal cannot be adequately maintained. – Gas and odour problems. – Bleeding.
• • • Perforation: Stoma Stricture: Necrosis: Paracolostomy Hernia: m/c complication Prolapse: m/c with transverse colostomy
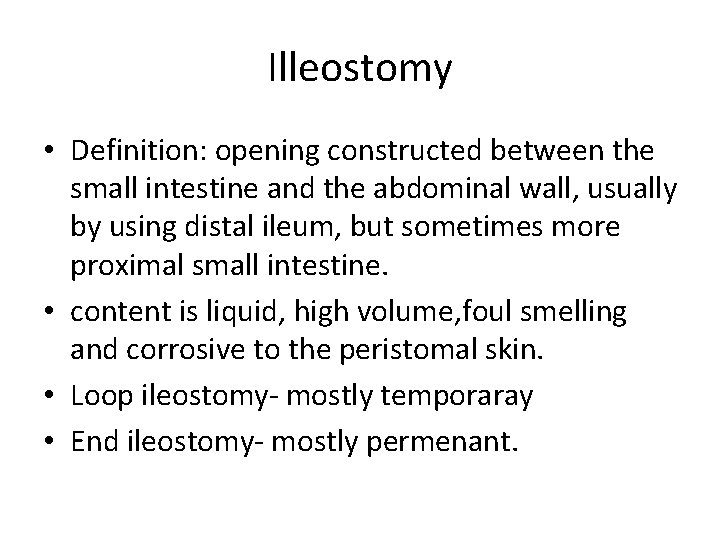
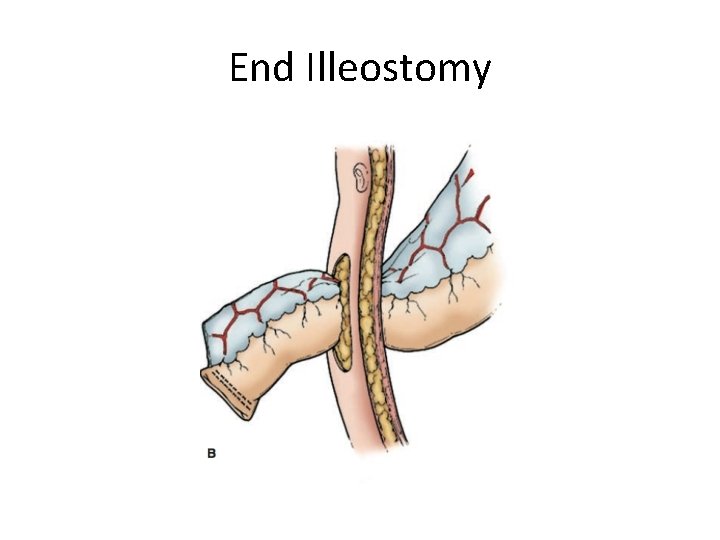
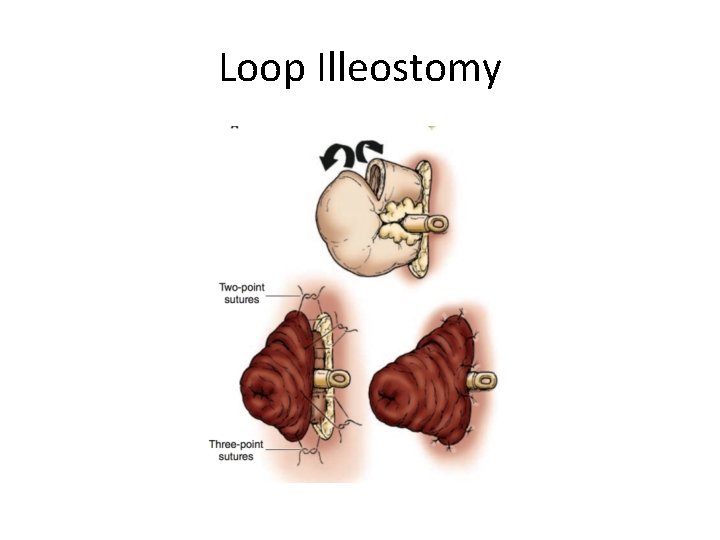
Illeostomy • Definition: opening constructed between the small intestine and the abdominal wall, usually by using distal ileum, but sometimes more proximal small intestine. • content is liquid, high volume, foul smelling and corrosive to the peristomal skin. • Loop ileostomy- mostly temporaray • End ileostomy- mostly permenant.
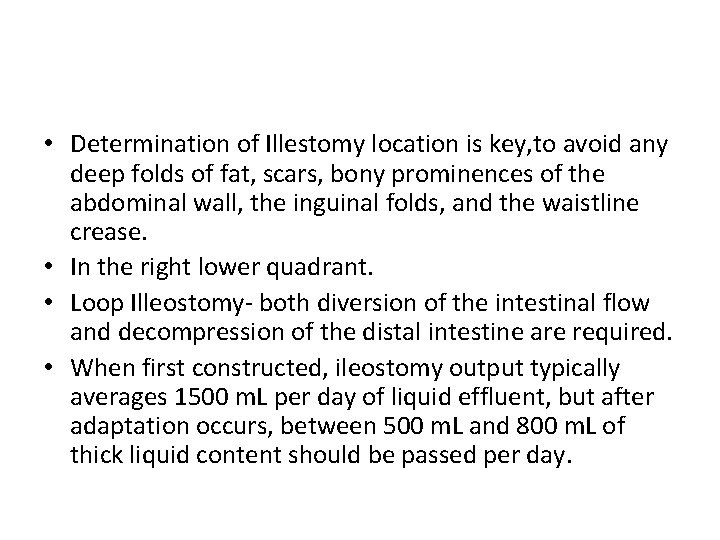
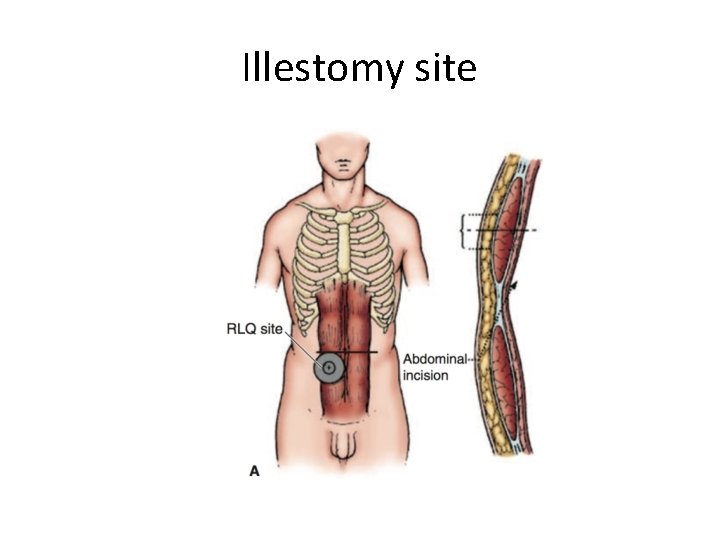
• Determination of Illestomy location is key, to avoid any deep folds of fat, scars, bony prominences of the abdominal wall, the inguinal folds, and the waistline crease. • In the right lower quadrant. • Loop Illeostomy- both diversion of the intestinal flow and decompression of the distal intestine are required. • When first constructed, ileostomy output typically averages 1500 m. L per day of liquid effluent, but after adaptation occurs, between 500 m. L and 800 m. L of thick liquid content should be passed per day.
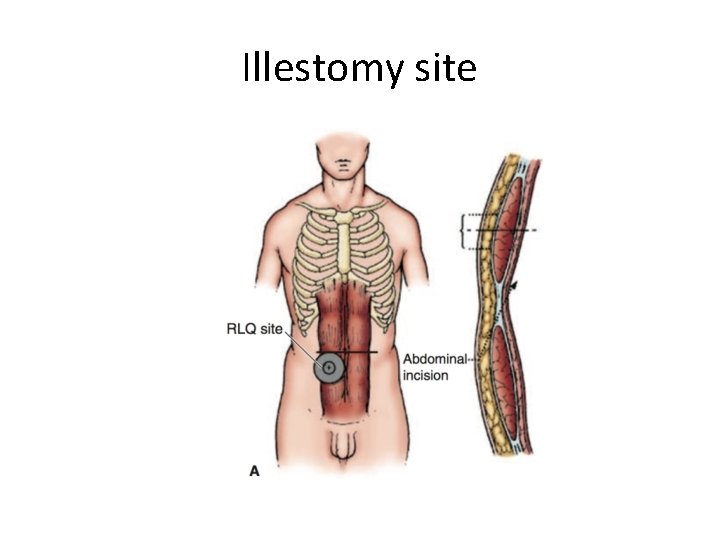
Illestomy site
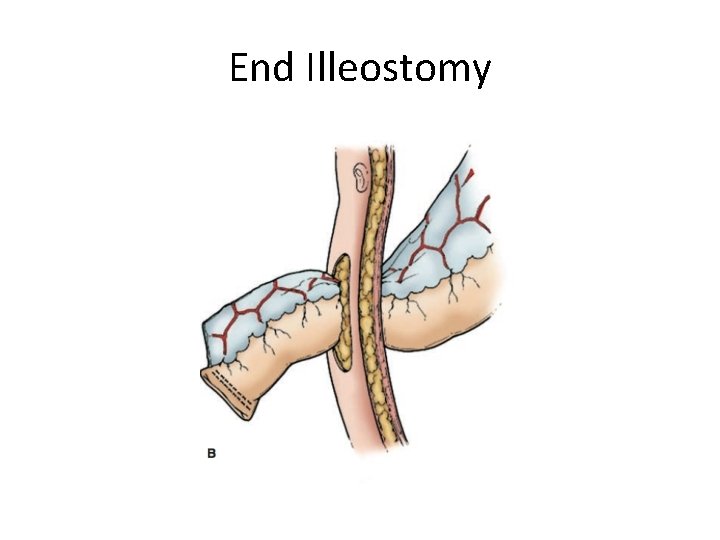
End Illeostomy
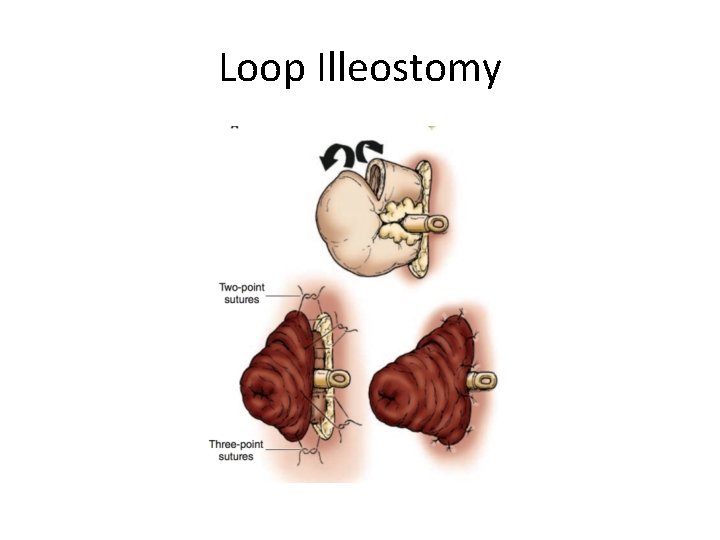
Loop Illeostomy
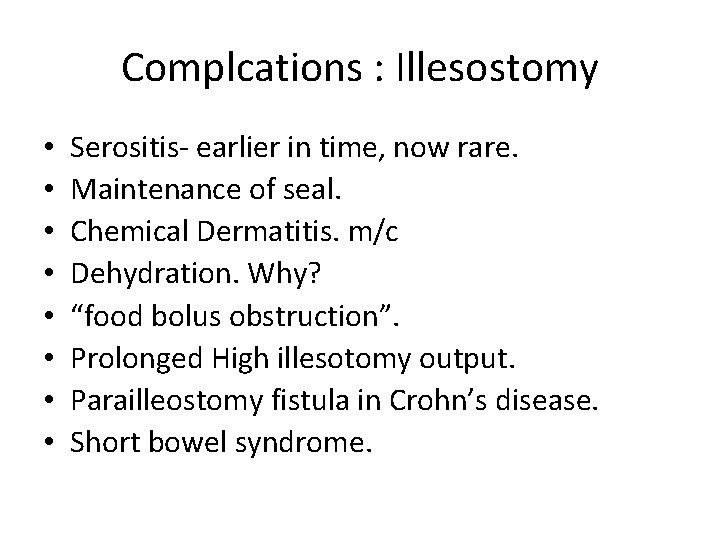
Complcations : Illesostomy • • Serositis- earlier in time, now rare. Maintenance of seal. Chemical Dermatitis. m/c Dehydration. Why? “food bolus obstruction”. Prolonged High illesotomy output. Parailleostomy fistula in Crohn’s disease. Short bowel syndrome.
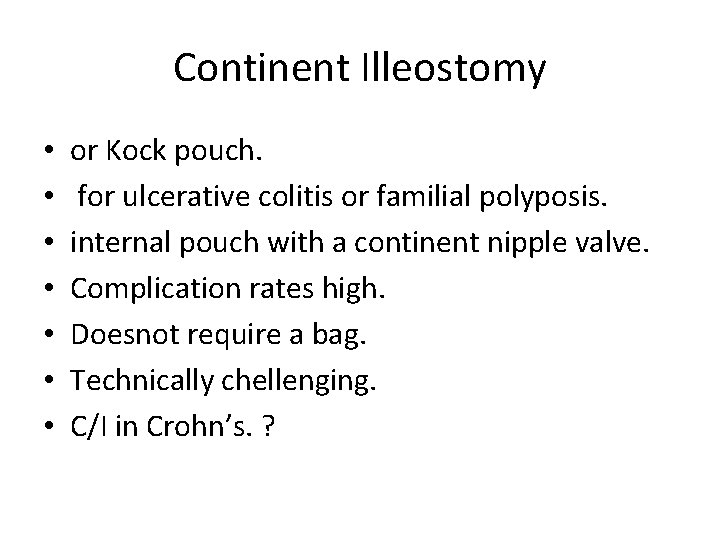
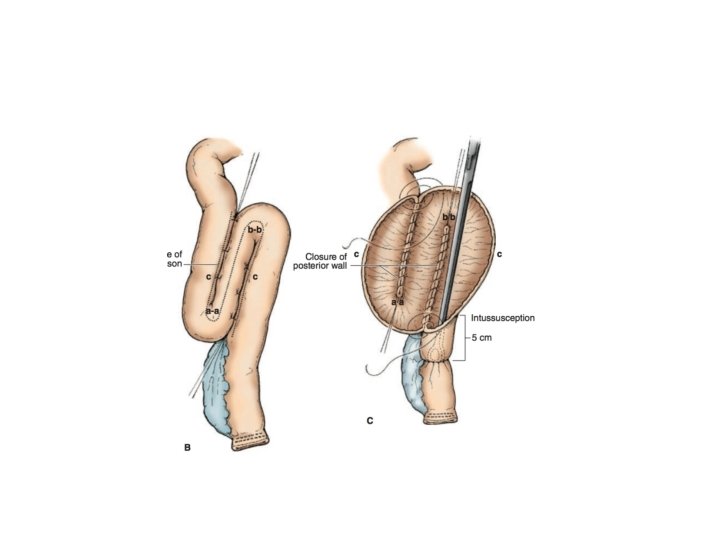
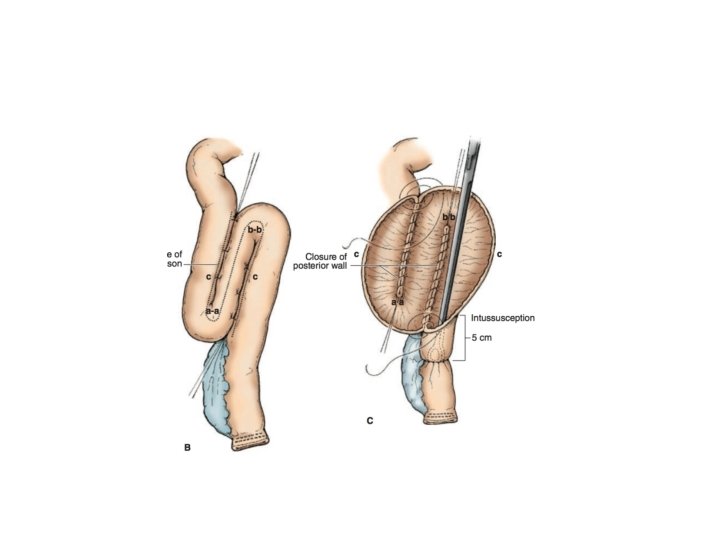
Continent Illeostomy • • or Kock pouch. for ulcerative colitis or familial polyposis. internal pouch with a continent nipple valve. Complication rates high. Doesnot require a bag. Technically chellenging. C/I in Crohn’s. ?
Enteric Fistulas • A fistula is defined as an abnormal communication between two epithelial surfaces. • Enteric Fistulas may arise from: • (1) Diseased bowel extending to surrounding epithelialized structures; • (2) Extraintestinal disease eroding into otherwise normal bowel; • (3) Surgical trauma to normal bowel including inadvertent or missed enterotomies; • (4) Anastomotic disruption following surgery for a variety of conditions. • (5)Post operative radiation is a significant factor.
Classification • Etiologically: – Spontaneous – Post op …m/c • Physilogical: – High output >500 ml/day – Moderate output 200 -500 ml/day – Low output <200 ml/day
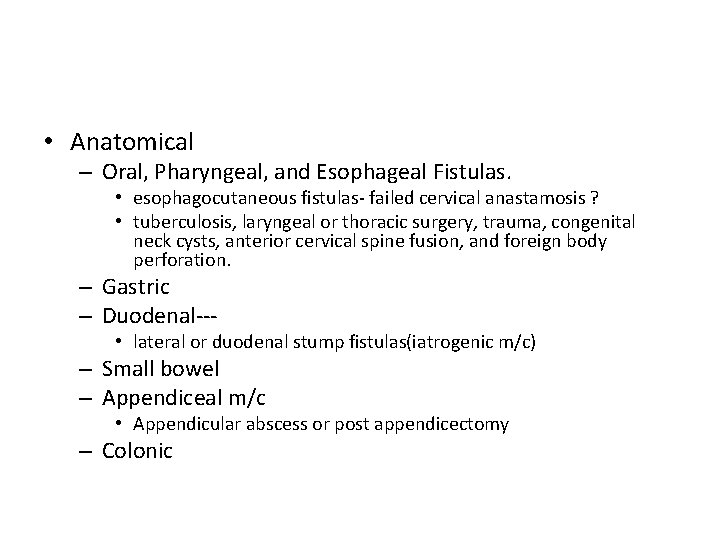
• Anatomical – Oral, Pharyngeal, and Esophageal Fistulas. • esophagocutaneous fistulas- failed cervical anastamosis ? • tuberculosis, laryngeal or thoracic surgery, trauma, congenital neck cysts, anterior cervical spine fusion, and foreign body perforation. – Gastric – Duodenal--- • lateral or duodenal stump fistulas(iatrogenic m/c) – Small bowel – Appendiceal m/c • Appendicular abscess or post appendicectomy – Colonic
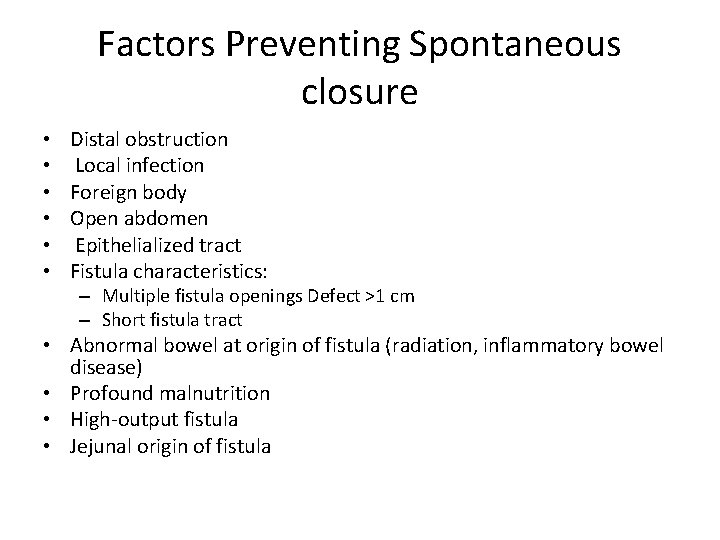
Factors Preventing Spontaneous closure • • • Distal obstruction Local infection Foreign body Open abdomen Epithelialized tract Fistula characteristics: – Multiple fistula openings Defect >1 cm – Short fistula tract • Abnormal bowel at origin of fistula (radiation, inflammatory bowel disease) • Profound malnutrition • High-output fistula • Jejunal origin of fistula
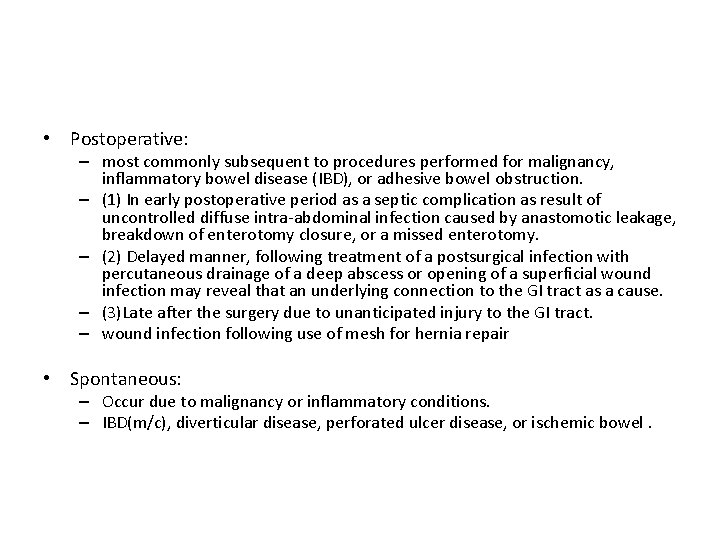
• Postoperative: – most commonly subsequent to procedures performed for malignancy, inflammatory bowel disease (IBD), or adhesive bowel obstruction. – (1) In early postoperative period as a septic complication as result of uncontrolled diffuse intra-abdominal infection caused by anastomotic leakage, breakdown of enterotomy closure, or a missed enterotomy. – (2) Delayed manner, following treatment of a postsurgical infection with percutaneous drainage of a deep abscess or opening of a superficial wound infection may reveal that an underlying connection to the GI tract as a cause. – (3)Late after the surgery due to unanticipated injury to the GI tract. – wound infection following use of mesh for hernia repair • Spontaneous: – Occur due to malignancy or inflammatory conditions. – IBD(m/c), diverticular disease, perforated ulcer disease, or ischemic bowel.
 Diverting loop ileostomy
Diverting loop ileostomy Rn division 1
Rn division 1 Ileostomy sample menu
Ileostomy sample menu Stoma definition
Stoma definition Hematology word surgery
Hematology word surgery Oxia medical term
Oxia medical term Gramineae tipi stoma
Gramineae tipi stoma Nursing interventions for endoscopy complications
Nursing interventions for endoscopy complications Protocol stomazorg vilans
Protocol stomazorg vilans Dışkıyı katılaştıran besinler
Dışkıyı katılaştıran besinler Retractie stoma
Retractie stoma Granugel pasta
Granugel pasta Kseromorf
Kseromorf Binnenste buitenste bil quadrant
Binnenste buitenste bil quadrant Guard cell
Guard cell Stoma function
Stoma function Leaf structure
Leaf structure Pyelostomi nedir
Pyelostomi nedir Explain the function of leaf
Explain the function of leaf Change language to english
Change language to english Devierend ileostoma
Devierend ileostoma Ccmc ear nose and throat
Ccmc ear nose and throat Palisadno tkivo
Palisadno tkivo Stoma
Stoma Stoma care procedure
Stoma care procedure Tracheostomy care
Tracheostomy care Dope mnemonic emt
Dope mnemonic emt Chapter 10 airway management
Chapter 10 airway management Abcd-stoma®
Abcd-stoma® Nazogastrik sonda çeşitleri
Nazogastrik sonda çeşitleri Ishrana preko sonde
Ishrana preko sonde Keratan rentas arteri
Keratan rentas arteri Intestinal glands
Intestinal glands Giardia cyst and trophozoite
Giardia cyst and trophozoite Meconium ileus
Meconium ileus Layers of the intestinal wall
Layers of the intestinal wall Datos de obstrucción intestinal
Datos de obstrucción intestinal Git organs
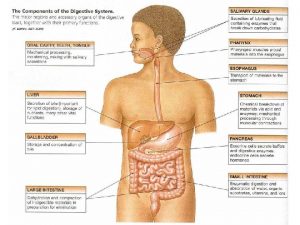
Git organs Protein absorption
Protein absorption Eradikationsbehandling
Eradikationsbehandling Antidiarreicos
Antidiarreicos Identificação
Identificação Infecção intestinal
Infecção intestinal