Intestinal Obstruction Laila Tavazo REM Case A 50
Intestinal Obstruction Laila Tavazo, REM
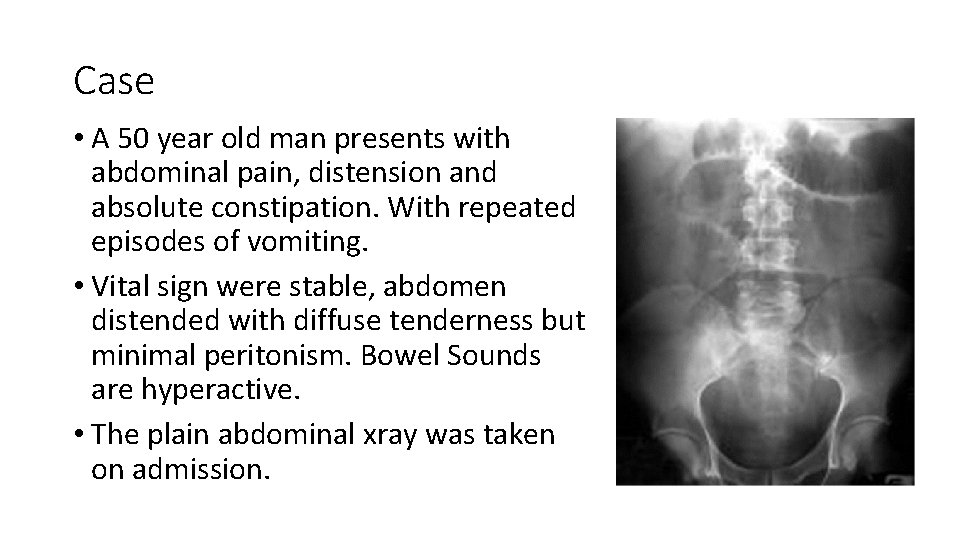
Case • A 50 year old man presents with abdominal pain, distension and absolute constipation. With repeated episodes of vomiting. • Vital sign were stable, abdomen distended with diffuse tenderness but minimal peritonism. Bowel Sounds are hyperactive. • The plain abdominal xray was taken on admission.
Definition • Lack of transit of intestinal contents is called intestinal obstruction • Intestinal obstruction is a very common problem encountered in the ED, accounting for up to 15% of all emergency admissions for abdominal pain.
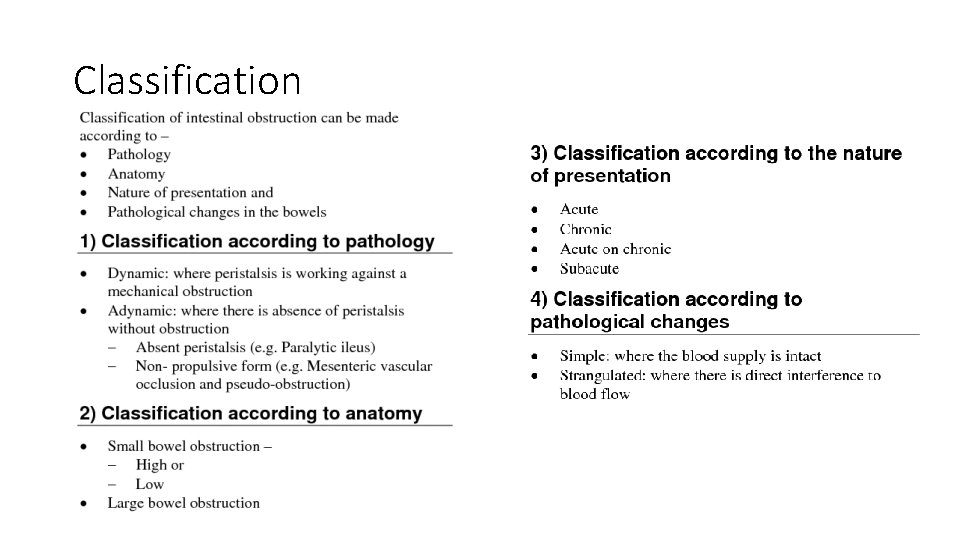
Classification
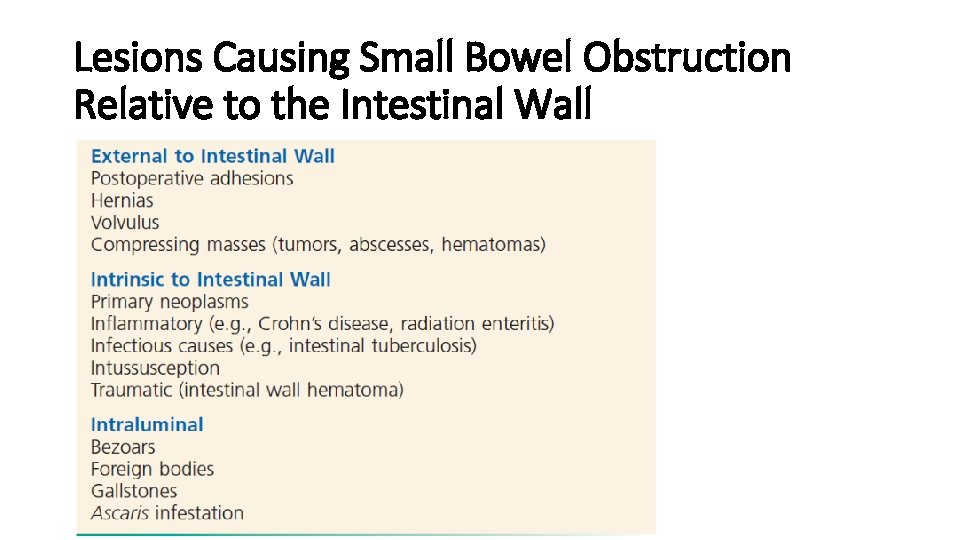
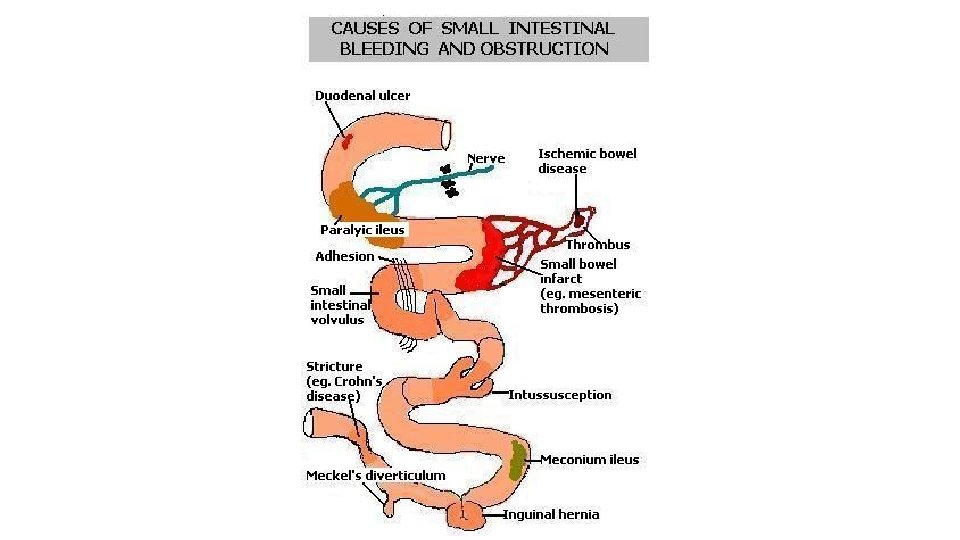
Lesions Causing Small Bowel Obstruction Relative to the Intestinal Wall
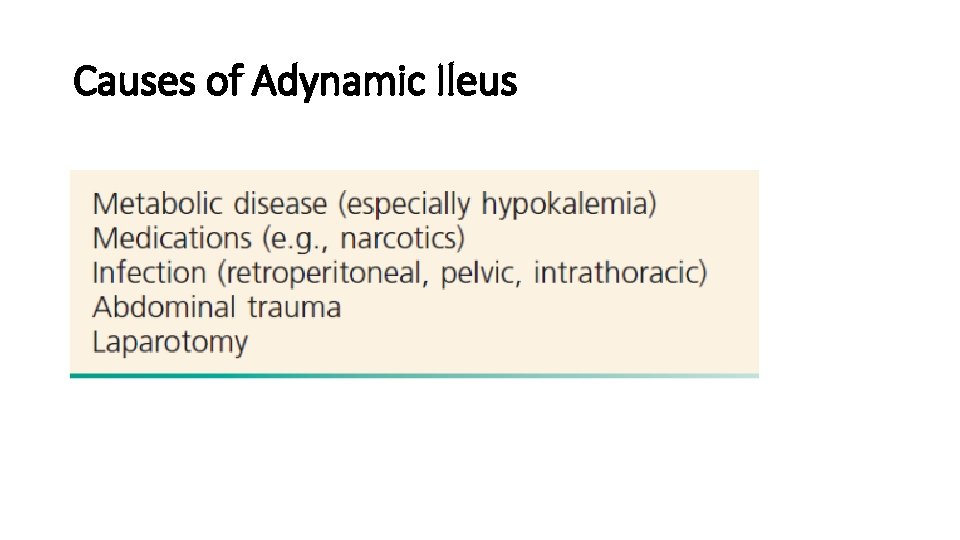
Causes of Adynamic Ileus
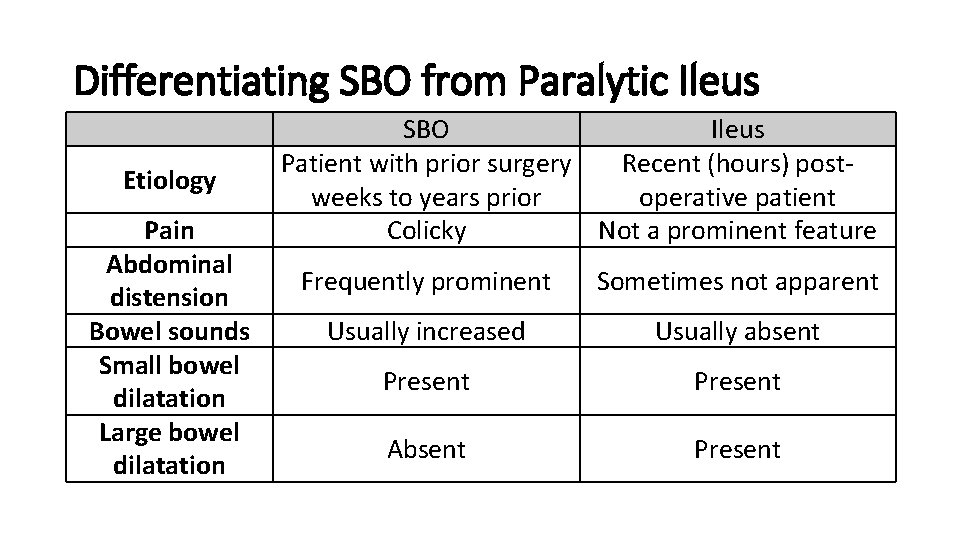
Differentiating SBO from Paralytic Ileus Etiology Pain Abdominal distension Bowel sounds Small bowel dilatation Large bowel dilatation SBO Ileus Patient with prior surgery Recent (hours) postweeks to years prior operative patient Colicky Not a prominent feature Frequently prominent Sometimes not apparent Usually increased Usually absent Present Absent Present
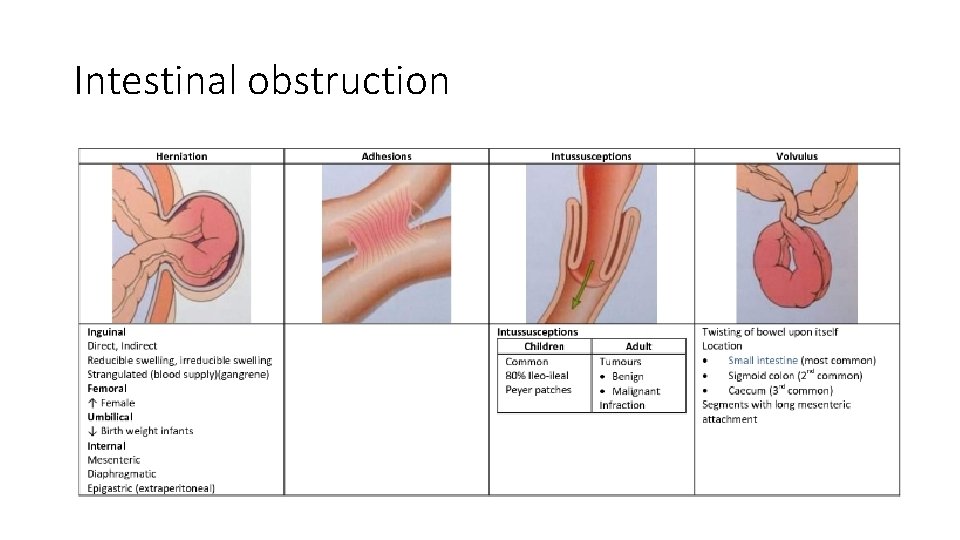
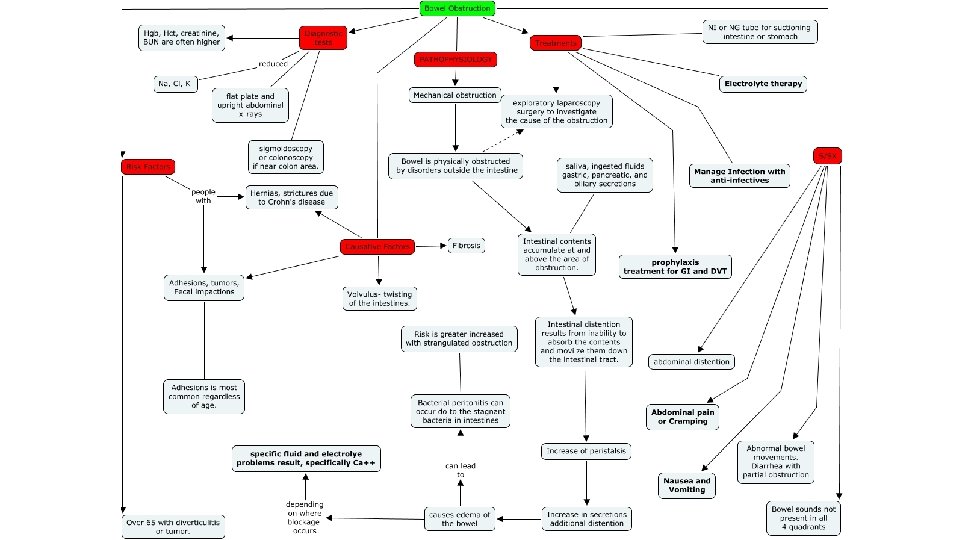
Intestinal obstruction
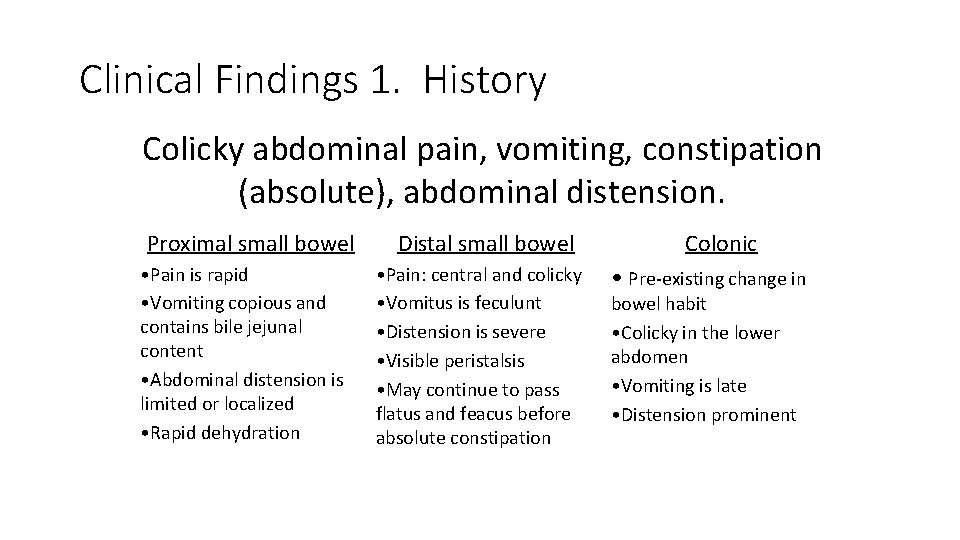
Clinical Findings 1. History Colicky abdominal pain, vomiting, constipation (absolute), abdominal distension. Proximal small bowel • Pain is rapid • Vomiting copious and contains bile jejunal content • Abdominal distension is limited or localized • Rapid dehydration Distal small bowel • Pain: central and colicky • Vomitus is feculunt • Distension is severe • Visible peristalsis • May continue to pass flatus and feacus before absolute constipation Colonic • Pre-existing change in bowel habit • Colicky in the lower abdomen • Vomiting is late • Distension prominent
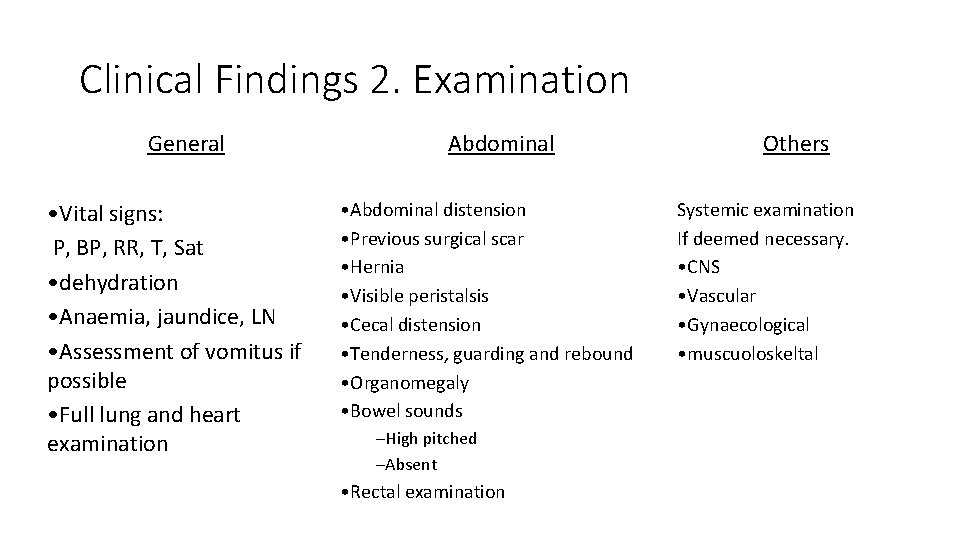
Clinical Findings 2. Examination General • Vital signs: P, BP, RR, T, Sat • dehydration • Anaemia, jaundice, LN • Assessment of vomitus if possible • Full lung and heart examination Abdominal • Abdominal distension • Previous surgical scar • Hernia • Visible peristalsis • Cecal distension • Tenderness, guarding and rebound • Organomegaly • Bowel sounds –High pitched –Absent • Rectal examination Others Systemic examination If deemed necessary. • CNS • Vascular • Gynaecological • muscuoloskeltal
Diagnostic • Lab: • CBC (leukocytosis, anemia, hematocrit, platelets) • Clotting profile • Arterial blood gasses • BUN, Crt, Na, K, Amylase, LFT and glucose • CPK, LDH, I-FABP • Optional (ESR, CRP, Hepatitis profile)
Diagnostic Plain radiographs can diagnose SBO in 50 to 60% of cases but usually cannot identify the cause of the obstruction. CT scanning is much better for determining the cause and is also very useful in identifying strangulation complicating SBO.
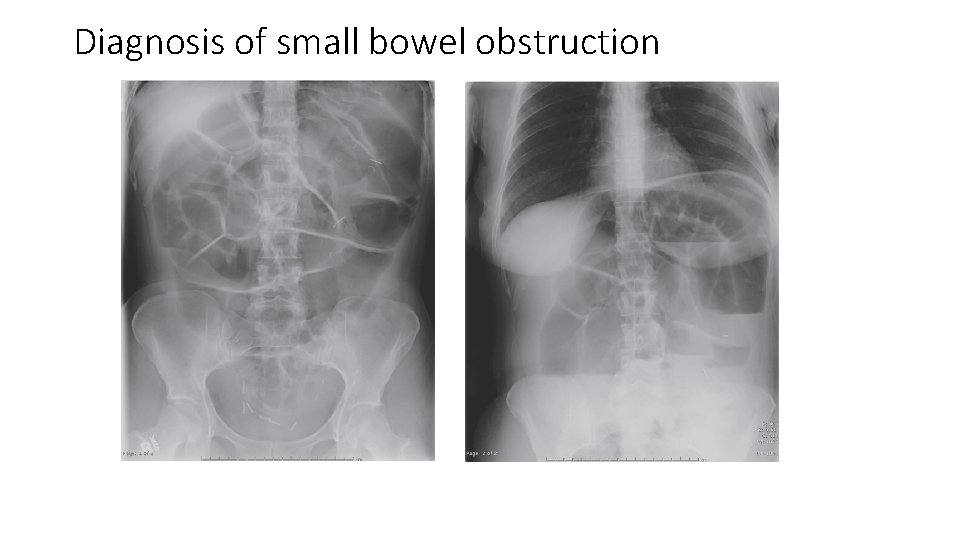
Diagnosis of small bowel obstruction
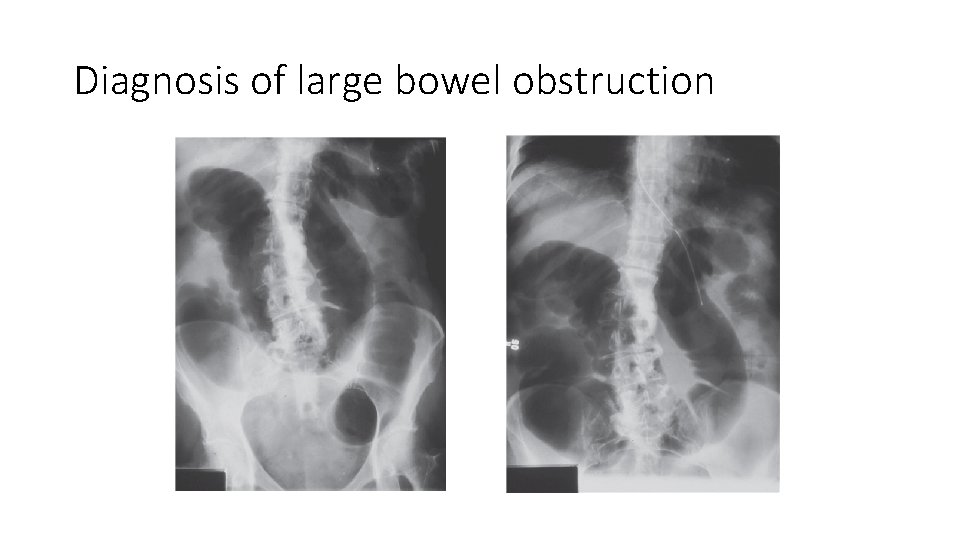
Diagnosis of large bowel obstruction
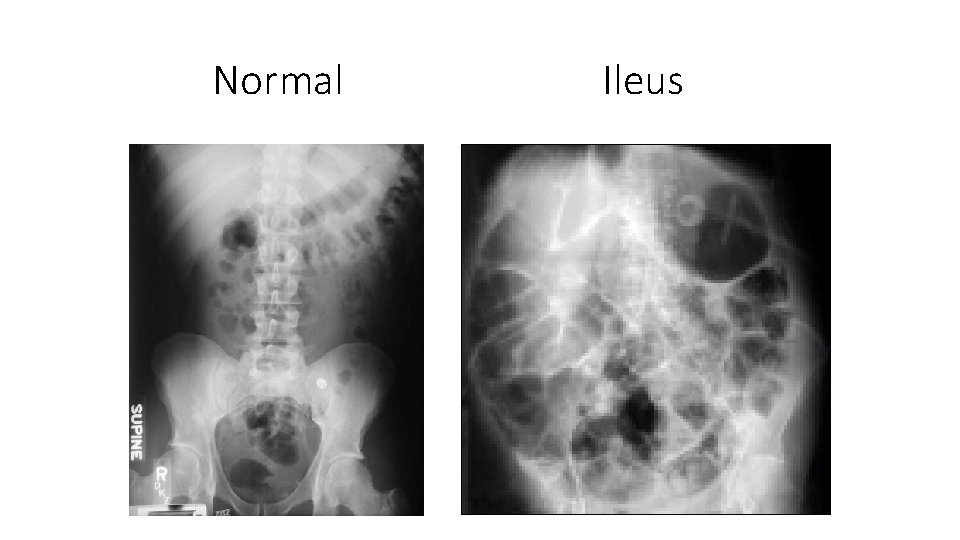
Normal Ileus
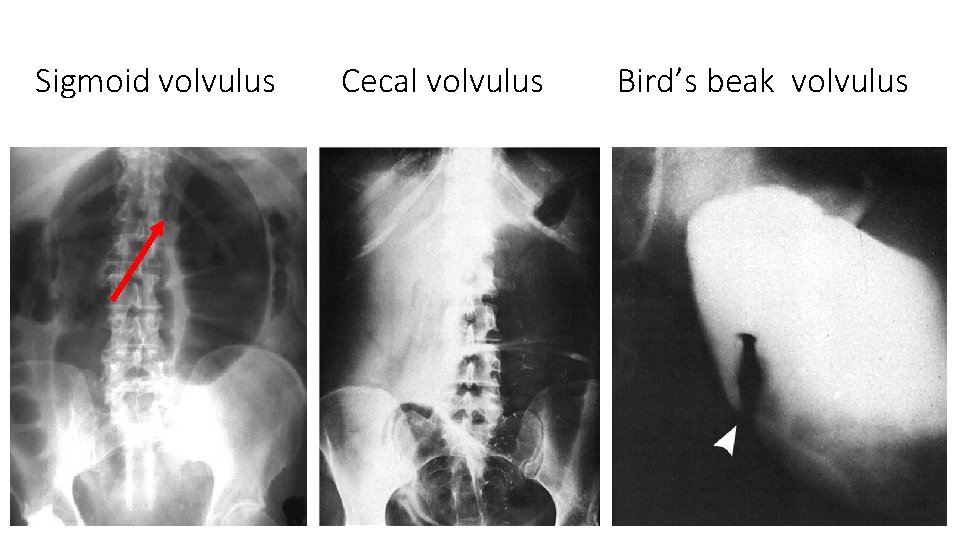
Sigmoid volvulus Cecal volvulus Bird’s beak volvulus
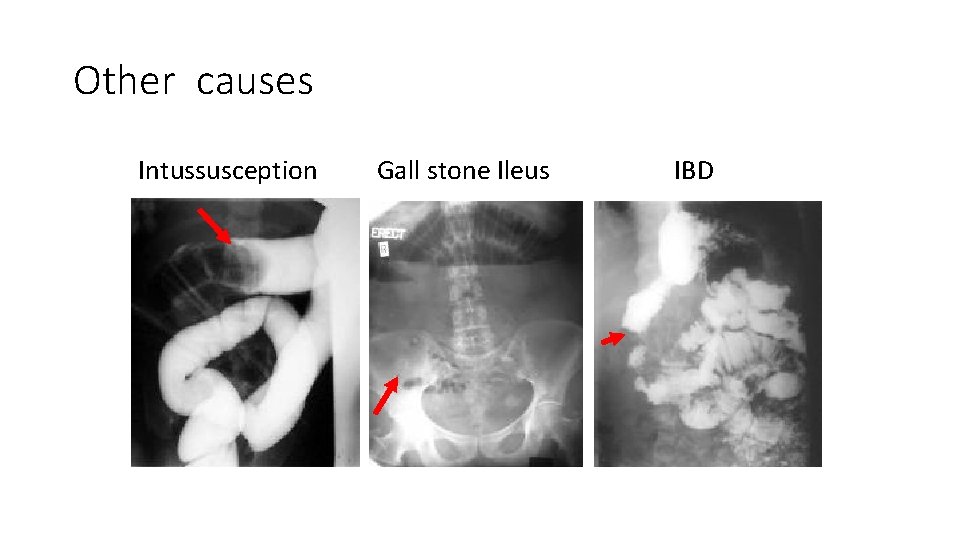
Other causes Intussusception Gall stone Ileus IBD
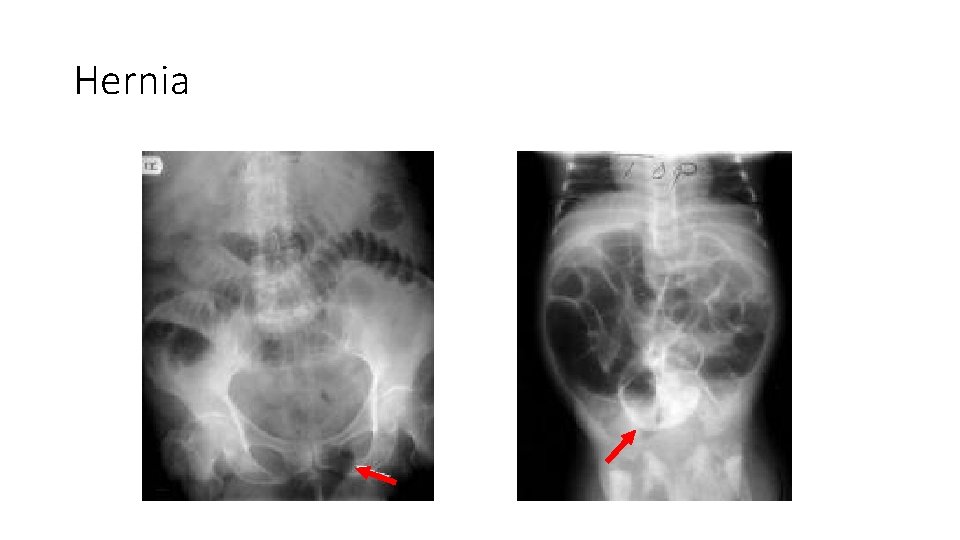
Hernia
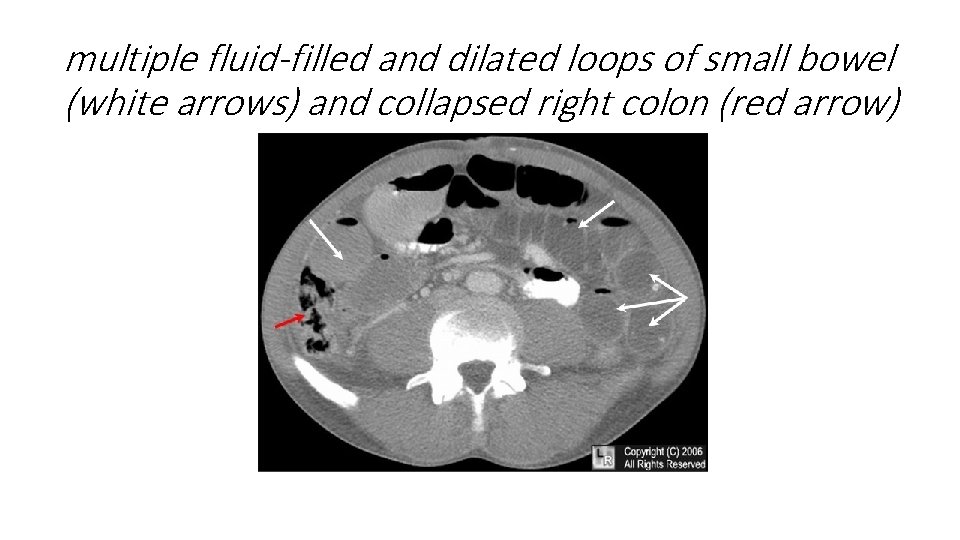
multiple fluid-filled and dilated loops of small bowel (white arrows) and collapsed right colon (red arrow)

String of pearl sign
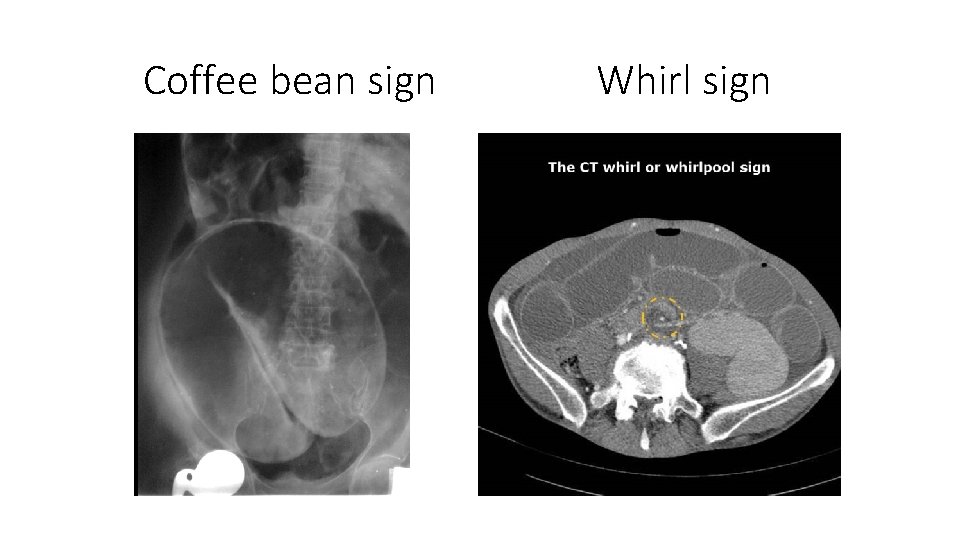
Coffee bean sign Whirl sign
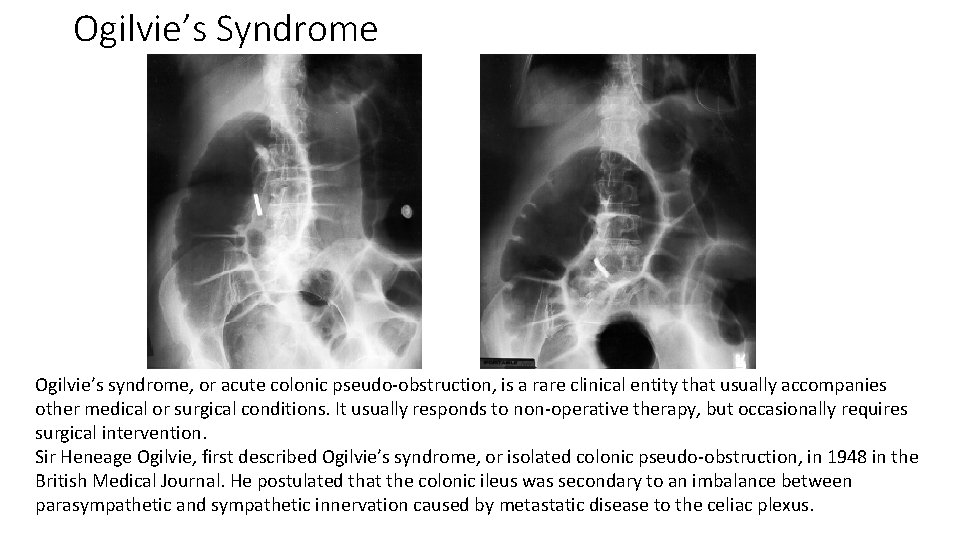
Ogilvie’s Syndrome Ogilvie’s syndrome, or acute colonic pseudo-obstruction, is a rare clinical entity that usually accompanies other medical or surgical conditions. It usually responds to non-operative therapy, but occasionally requires surgical intervention. Sir Heneage Ogilvie, first described Ogilvie’s syndrome, or isolated colonic pseudo-obstruction, in 1948 in the British Medical Journal. He postulated that the colonic ileus was secondary to an imbalance between parasympathetic and sympathetic innervation caused by metastatic disease to the celiac plexus.
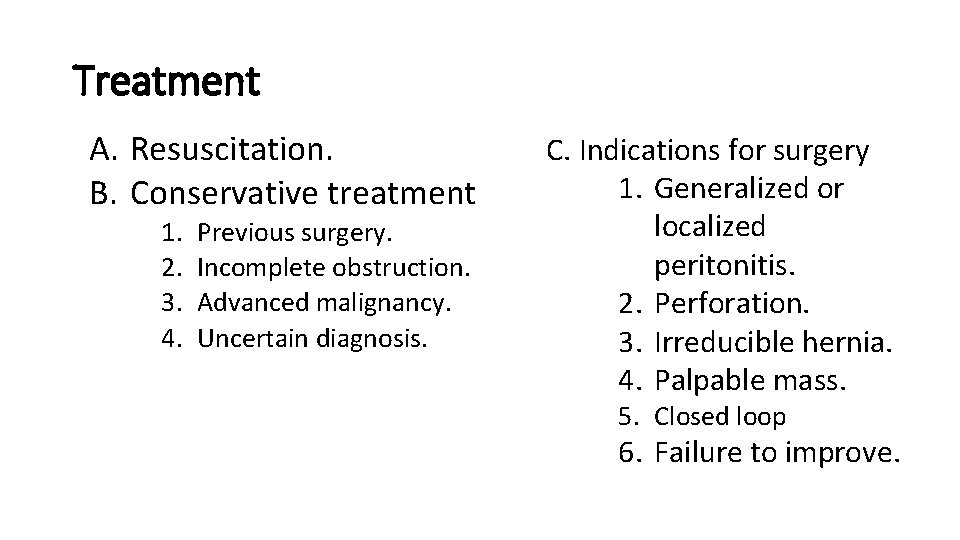
Treatment A. Resuscitation. B. Conservative treatment 1. 2. 3. 4. Previous surgery. Incomplete obstruction. Advanced malignancy. Uncertain diagnosis. C. Indications for surgery 1. Generalized or localized peritonitis. 2. Perforation. 3. Irreducible hernia. 4. Palpable mass. 5. Closed loop 6. Failure to improve.
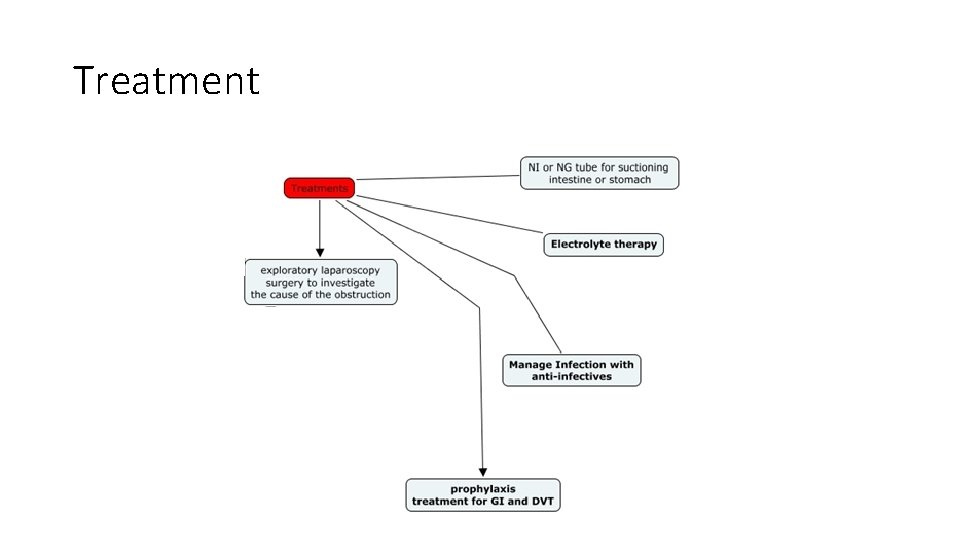
Treatment
Thank you for your attention
- Slides: 27