Interprofessional Practice in Medical Settings Speech Language Pathology
- Slides: 16
Interprofessional Practice in Medical Settings Speech Language Pathology PRACTICUM SPRING 2020
Lecture Objectives • Interprofessional practice components and benefits • Common team members SLP's collaborate with in medical settings • Basic tips for clear communication with other care providers • Outline medical settings • Examples from specific settings • Q&A
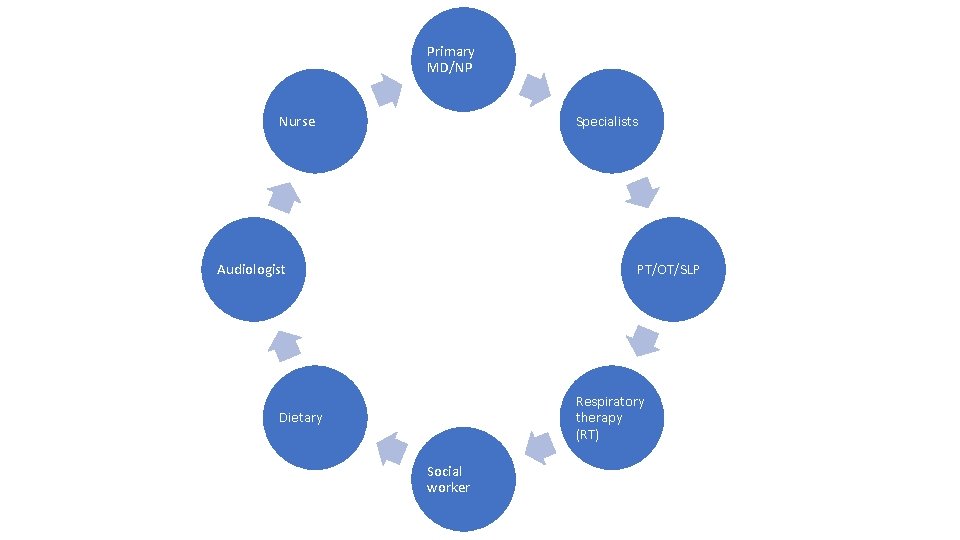
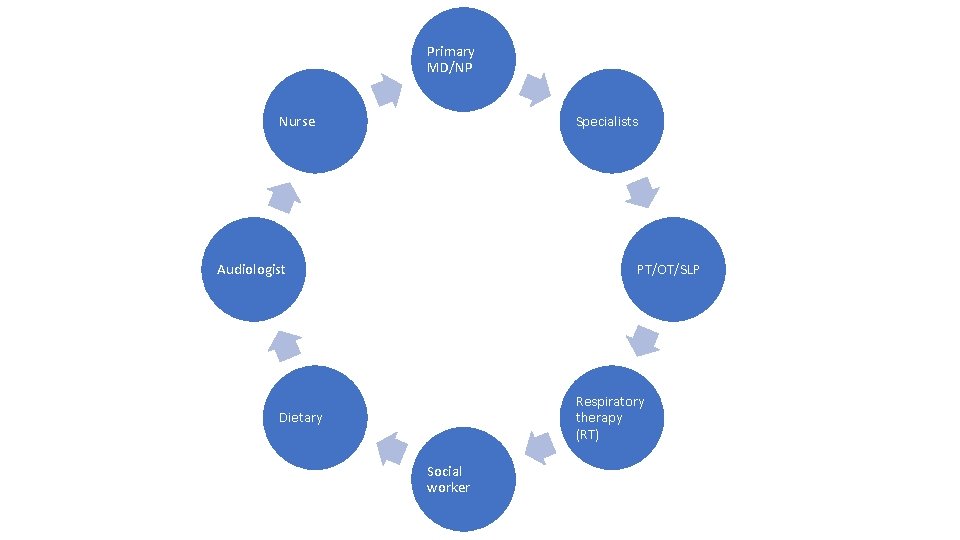
Primary MD/NP Nurse Specialists Audiologist PT/OT/SLP Respiratory therapy (RT) Dietary Social worker
Components of interdisciplinary practice: • Individuals from different disciplines coordinate care to achieve better patient outcomes • Both multidisciplinary (I. e. , containing multiple professionals with specific roles) and coordinated/collaborative • Collaboration can include shared goal setting, meetings, shared reports/documentation
Benefits of interprofessional practice • Improve outcomes • Reduce cost and errors • Improve safety • Enhance the patient experience in the health care setting • Use unique abilities of all members of the team of optimize outcomes
Basic tips for clear and effective communication • Timely written documentation! • Determine the best system for communicating with care providers in your specific facility upon arrival (e. g. , page, call, email) and when direct communication is expected (e. g. , upon completion of an evaluation, only if needing orders, etc. ) • Learn the chain of commands at your facility and within each specific team in regards to communication and collaboration (e. g. , you may be expected to communicate with a nurse practitioner, or maybe a resident physician, instead of the attending physician)
SBAR: communication tool SBAR is an evidenced based, well known communication tool used by a variety of healthcare providers to assist with communicating in a standardized fashion. • Situation: What is going on with the patient? • Background: What is the clinical background or context? • Assessment: What do I think the problem is? • Recommendation: What do I think needs to be done for the patient?
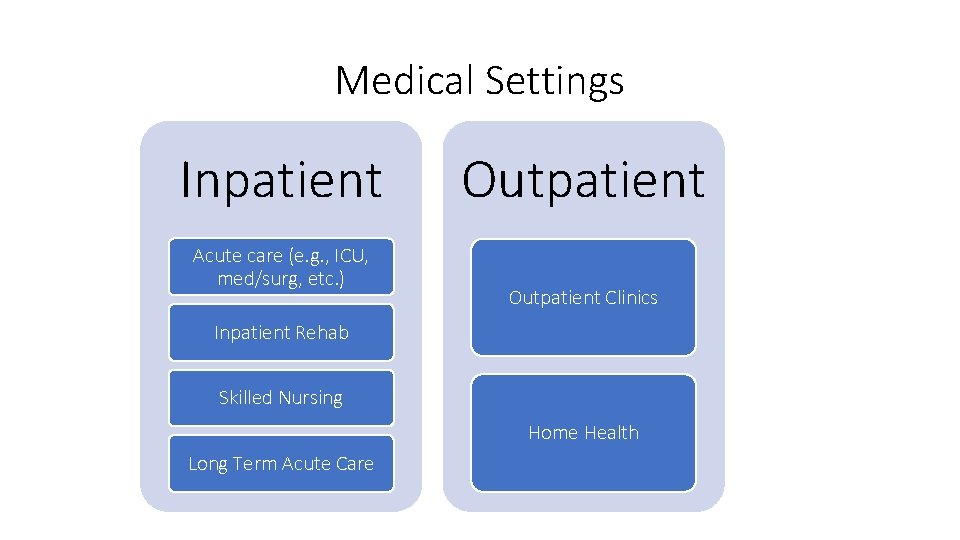
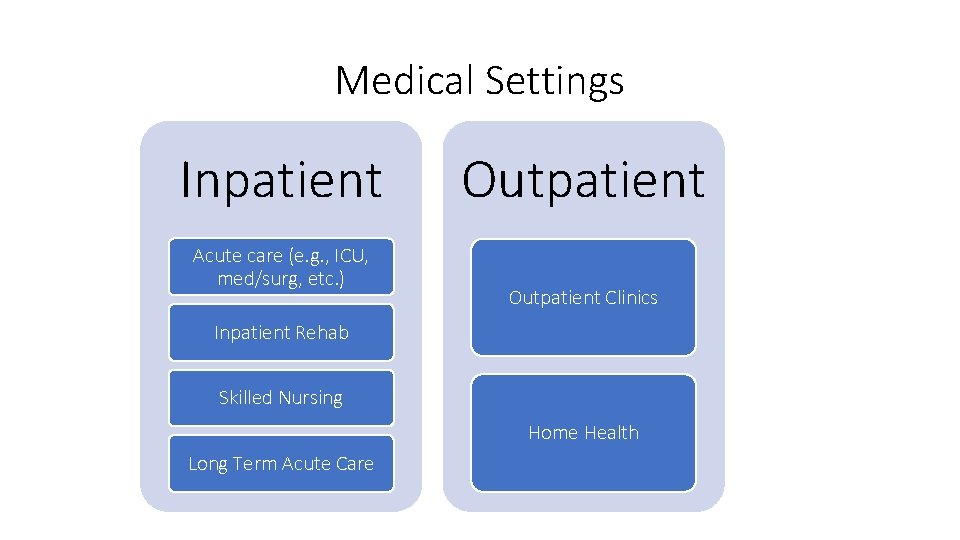
Medical Settings Inpatient Acute care (e. g. , ICU, med/surg, etc. ) Outpatient Clinics Inpatient Rehab Skilled Nursing Home Health Long Term Acute Care
Acute Care • What: Patients admitted to hospital likely with acute medical issues • Who: MD (intensivist, hospitalist); nurse; RT; PT/OT; social worker; specialists (GI, neurology, radiologist, ENT) • How: • SLP will communicate with medical team in passing, at bedside, or via telephone call or page • Interactions with MD will be brief (clear, concise, simple language) • Consult with RN prior to entering room and upon completion of evaluations • Why: • Assist MD with making appropriate referrals (e. g. , GI, ENT) • Assist with safe & timely discharge (e. g. , recommendations for safety at home, determine need for ongoing SLP involvement at next level of care)
Acute: Example Dysphagia services • 42 y/o male admitted for respiratory failure secondary to suspected aspiration pneumonia. MD (hospitalist) consulted SLP for a bedside swallow evaluation. Patient is NPO. • SLP calls RN: receives verbal OK to proceed with PO trials. • SLP recommends a modified barium swallow study (MBSS) due to inconsistent coughing with PO trials at bedside. Sends text page to MD who concurs and places orders • SLP, radiologist, and radiologist technician complete MBSS. Found silent aspiration after the swallow due to observed retrograde flow • SLP pages MD (hospitalist) to discuss results and recommend GI consult • SLP & MD (hospitalist & GI) meet with patient (often separately) to help patient make informed decision and to potentially improve QOL and patient safety
IPR/IRF (Inpatient Rehab/Inpatient Rehab Floor) • What: Intensive rehabilitation while still technically 'inpatient' • Who: MD, PCP, nursing staff (both day and night nurses!), PT, OT, Social Work, Case Coordinator, Kitchen Staff • How: • Interdisciplinary rounds- work with the entire team to discuss patient progress/make recommendations • Hallway chats, discussions with MD and nursing • Co-treats- work with PT/OT/RT in areas that cover both fields (e. g. , feeding) • Communication with MD, direct vs. indirect • Why: Medicare guidelines, ensuring appropriate recommendations for discharge date and further rehab
Skilled Nursing Facility (SNF) • What: Short term rehabilitation (sometimes with long term care) likely after hospital stay when patient isn't ready to return home yet due to medications/IV's or rehabilitation needs. • Who: Building administrator, house MD (typically on site 1 -2 x/week), nursing staff (4 or 5 levels), Director of Rehab, PT/OT/ST, dietary staff, social work, activities coordinator • How: • • Therapy team meetings and discharge planning Weekly IDT (Interdisciplinary Team) meetings Co-treat with PT/OT as appropriate Communication with nursing staff, dietary staff, activities staff and house MD as needed • Why: Medicare and Insurance guidelines largely drive reimbursement and qualification of stay. Stay must be justified by skill of nursing and/or therapy
SNF: Example Dysphagia Services • Patient was admitted to SNF with orders for altered diet texture and thickened liquids • If patient was not admitted to SNF with orders for ST interventions, ST/nursing requests order from house doctor to evaluate and treat the patient as indicated. • Once order is received, evaluation can be completed to determine if patient would benefit from interventions to upgrade to a less restrictive diet • Plan of treatment is established and initiated, typically patients are seen 5 days a week for ~30 -60 minutes per day. • ST consults with DOR for treatment plan, nursing staff for precautions/recommendations and dietary staff for recommendations/trials.
OP (Outpatient Therapy) • What: Patients are living at home (or assisted living facilities) and come into the clinic for tx (just like HEDCO!) • Who: PCP (or referring doctor), PT, OT, AAC/tech representatives, insurance companies, Family Members • How: Calling appropriate provider via phone, most often speaking to the doc's nurse, faxing, try try again to get in contact with the right person to get the referral because you are likely the only care provider for your patient at this point. • Why: Reassessing patient progress with dysphagia therapy, making recommendations for further care (need that referral!)
OP: Example • Your patient is now dischagred from the SNF and has been sent home on thickened liquid and a regular diet. You receive a referral from the patient's PCP requesting dysphagia therapy to ensure patient is on safest/least restrictive diet. • Depending on your facility, you may call the patient directly or have the schedulers contact the patient to set up initial intake appointment. • Due to the patient's insurance coverage, he is only covered for one (1) session. . . • Establish need/frequency/duration and write report to be sent to the PCP and to the insurance company. • Following 6 weeks of swallowing therapy 3 x/week, recommend additional MBSS by contacting PCP directly for referral. • Contact the facility that completed the MBSS (if it is not within your system, provide an ROI). Coordinate with the patient to discuss results/recommendations
Resources • Dingley C, Daugherty K, Derieg MK, et al. Improving Patient Safety Through Provider Communication Strategy Enhancements. In: Henriksen K, Battles JB, Keyes MA, et al. , editors. Advances in Patient Safety: New Directions and Alternative Approaches (Vol. 3: Performance and Tools). Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Aug. Available from: https: //www. ncbi. nlm. nih. gov/books/NBK 43663/ • Johnson, A. (2016, August). Interprofessional Education and Interprofessional Practice in Communication Sciences and Disorders: An Introduction and Case. Based Examples of Implementation in Education and Health Care Settings. Retrieved April 8, 2020, from https: //www. asha. org/uploaded. Files/IPE-IPPReader-e. Book. pdf • Shahid, S. , Thomas, S. Situation, Background, Assessment, Recommendation (SBAR) Communication Tool for Handoff in Health Care – A Narrative Review. Saf Health 4, 7 (2018). https: //doi. org/10. 1186/s 40886 -018 -0073 -1