Interprofessional Education Incorporating Clinical Pharmacy Services into Family

- Slides: 30
Interprofessional Education: Incorporating Clinical Pharmacy Services into Family Medicine Residency Training Tracy Johns, Pharm. D Elizabeth Lawrence, MD May 3, 2016
Learning Objectives On completion of this session, participants should be able to… � Assess the current level of family medicine/pharmacy interprofessional education at their residency program. � Develop concrete steps to more effectively incorporate clinical pharmacy services in their family medicine residency setting to improve both patient care and resident education. � Brainstorm methods of assessing interprofessional competencies applicable to their residency setting.
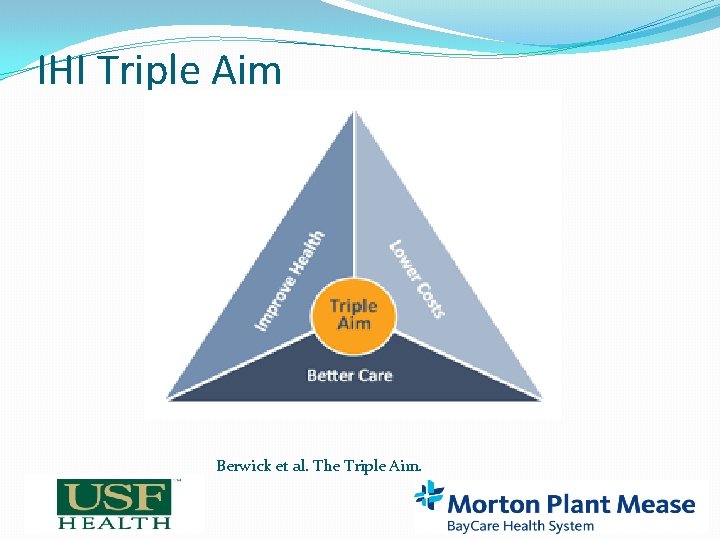
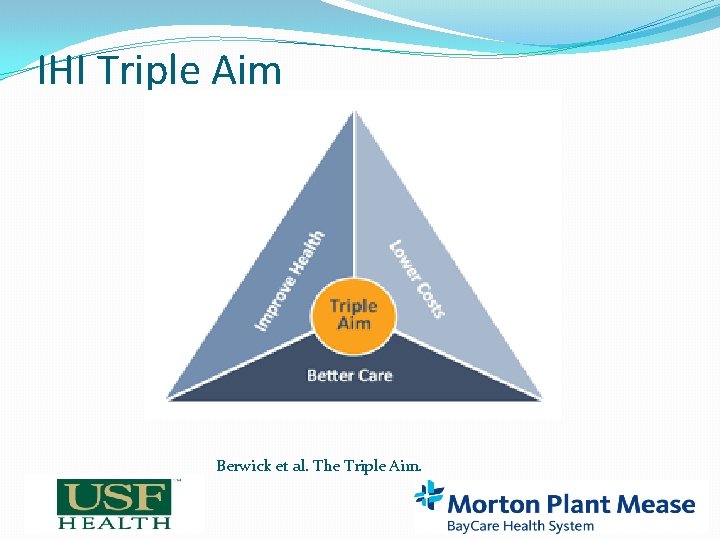
IHI Triple Aim Berwick et al. The Triple Aim.
Clinical Pharmacists in Family Medicine: Benefits �Better prescribing habits, lower cost, improved patient outcomes �Improvements in resident knowledge �Systematic approach to teaching pharmacotherapy �Promotes interprofessional education Whelan et al, Canadian Family Physician.
Clinical Pharmacists in Family Medicine: Underused �Are faculty at <50% of family medicine residencies in 2016 (27% in 2002) �Top barrier: funding �Underused when available Dickerson et al. Fam Med
Interprofessional Education �Ambulatory care pharmacy residency �Optimizing interactions �Creating culture of mutual respect and learning �Building strong and functional relationships Lounsbery et al. Fam Med
FM Pharmacotherapy Curriculum �Pharmacotherapy core �Pharm. D faculty �PGY 1 pharmacy resident � 1 year position �Pharmacy students � 6 -8 week rotation �Educational opportunities �Patient care �Didactic presentations �Program development �Drug information
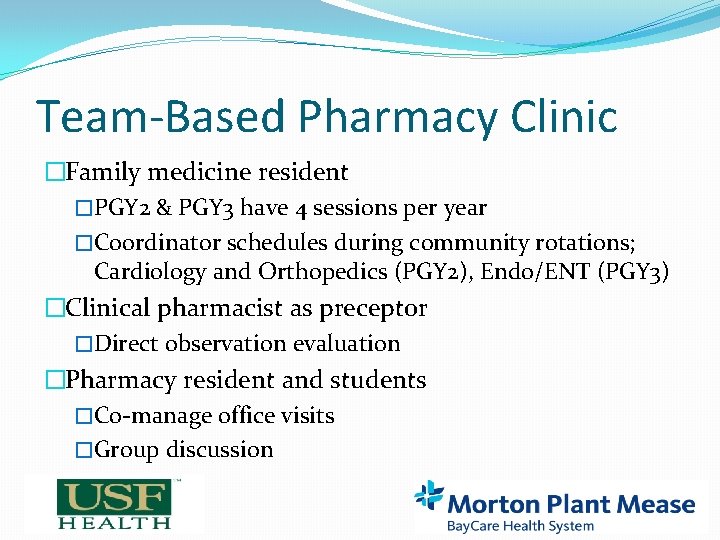
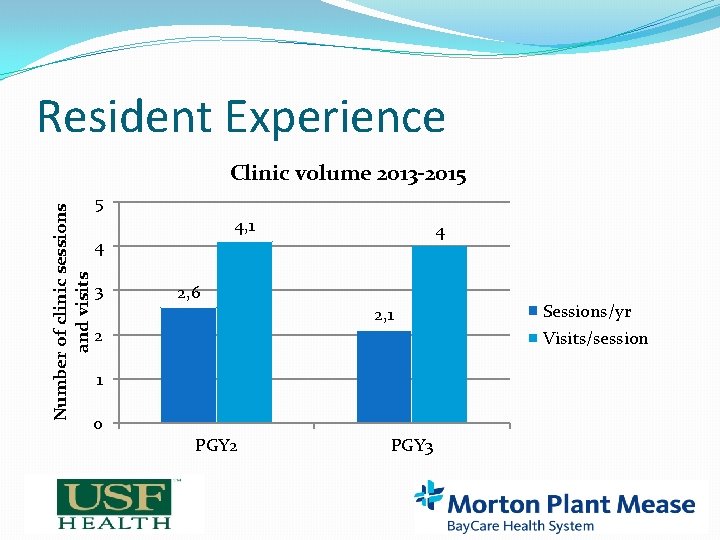
Team-Based Pharmacy Clinic �Family medicine resident �PGY 2 & PGY 3 have 4 sessions per year �Coordinator schedules during community rotations; Cardiology and Orthopedics (PGY 2), Endo/ENT (PGY 3) �Clinical pharmacist as preceptor �Direct observation evaluation �Pharmacy resident and students �Co-manage office visits �Group discussion
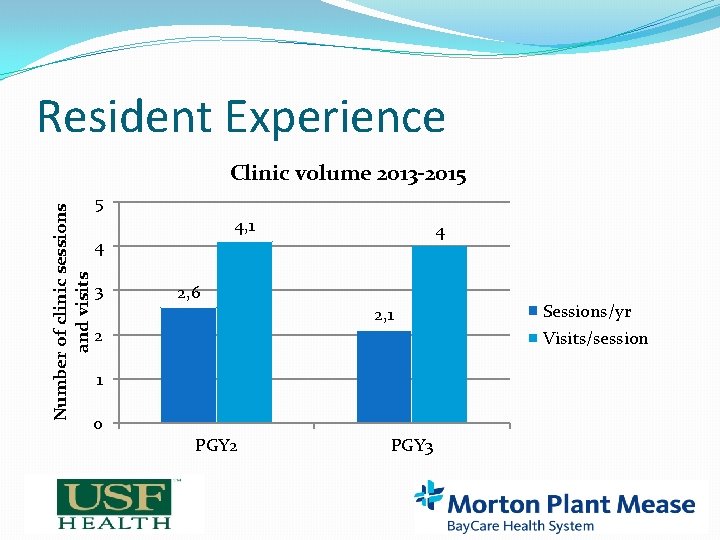
Resident Experience Number of clinic sessions and visits Clinic volume 2013 -2015 5 4, 1 4 3 4 2, 6 2, 1 2 Visits/session 1 0 Sessions/yr PGY 2 PGY 3
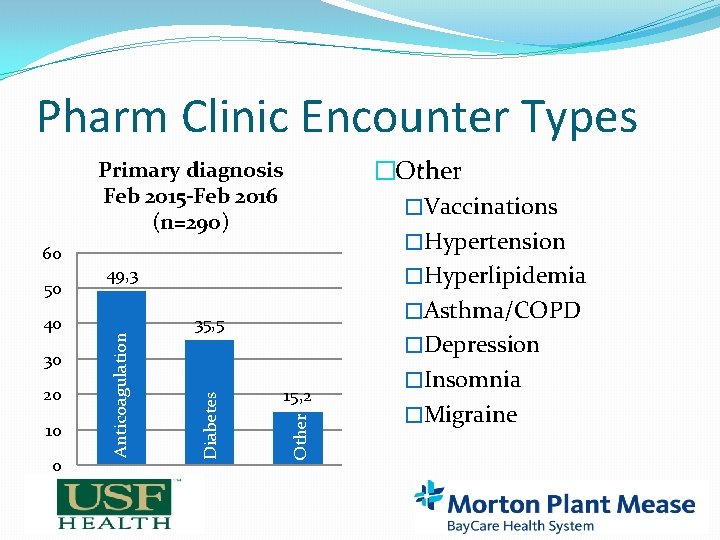
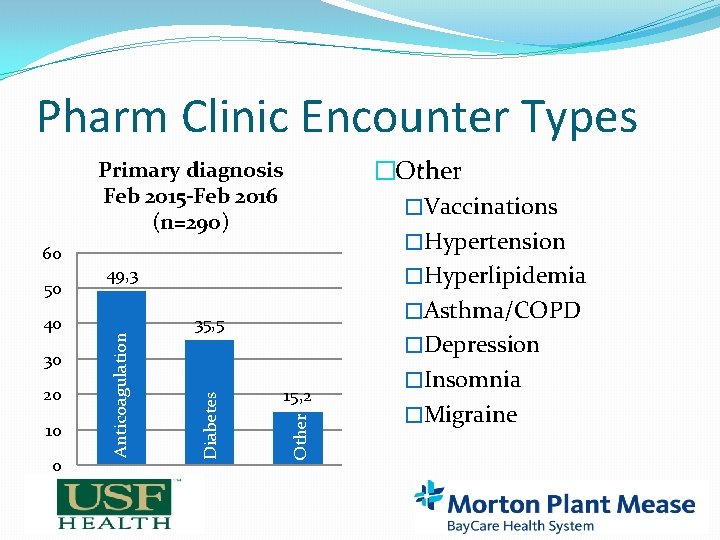
Pharm Clinic Encounter Types Primary diagnosis Feb 2015 -Feb 2016 (n=290) 30 20 10 0 35, 5 15, 2 Other 40 49, 3 Diabetes 50 Anticoagulation 60 �Other �Vaccinations �Hypertension �Hyperlipidemia �Asthma/COPD �Depression �Insomnia �Migraine

Longitudinal Collaborative Practice �Pharmacy residentifies high-risk patients �Prescribed inhalers/insulin �As needed pain meds/opioids �Aged 65 years and older �Taking > 5 chronic medications �Meds more than twice daily �Uncontrolled diabetes/hypertension �Chronic anticoagulation �High CV risk/statin eligible
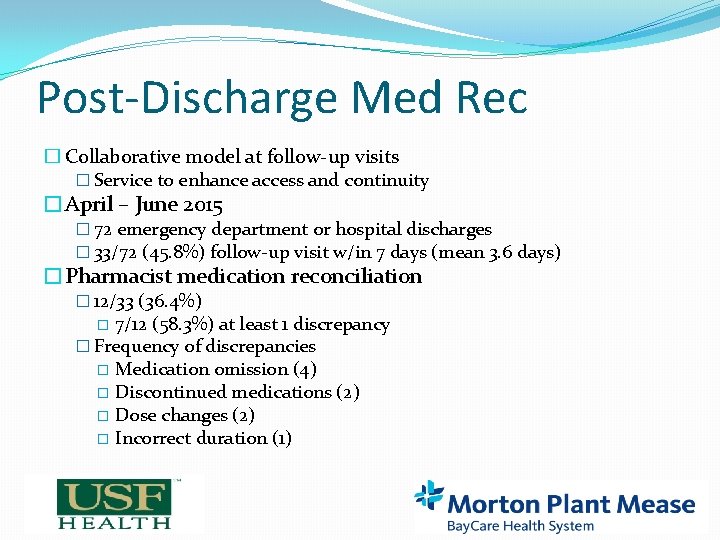
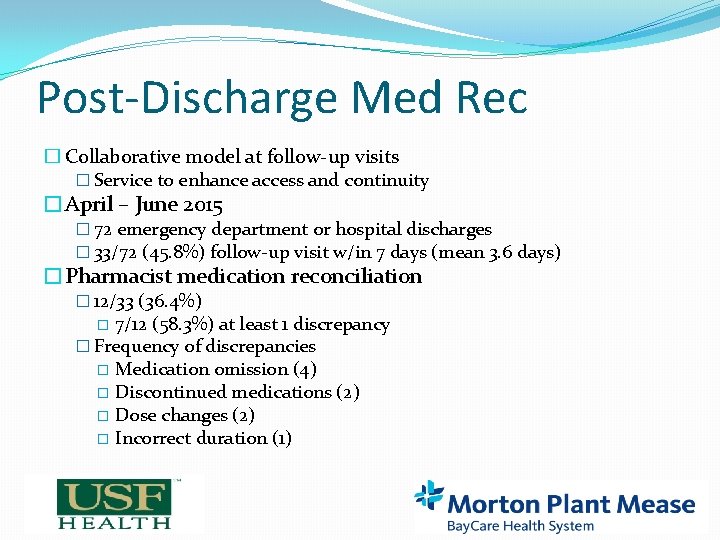
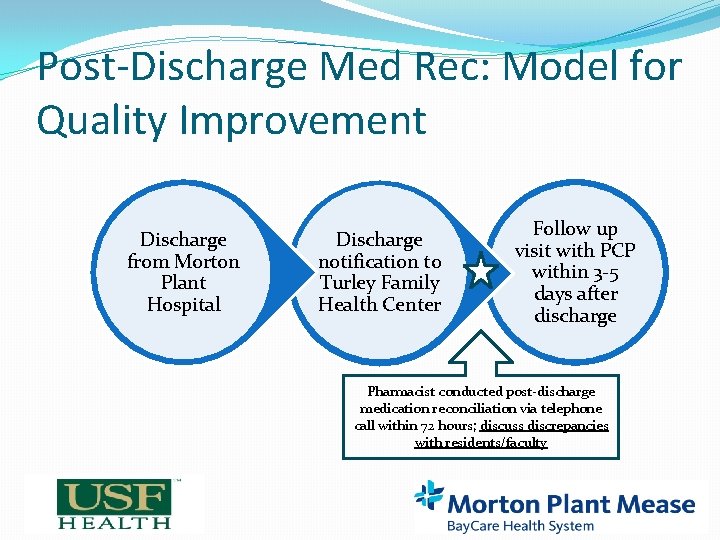
Post-Discharge Med Rec � Collaborative model at follow-up visits � Service to enhance access and continuity �April – June 2015 � 72 emergency department or hospital discharges � 33/72 (45. 8%) follow-up visit w/in 7 days (mean 3. 6 days) �Pharmacist medication reconciliation � 12/33 (36. 4%) 7/12 (58. 3%) at least 1 discrepancy � Frequency of discrepancies � Medication omission (4) � Discontinued medications (2) � Dose changes (2) � Incorrect duration (1) �
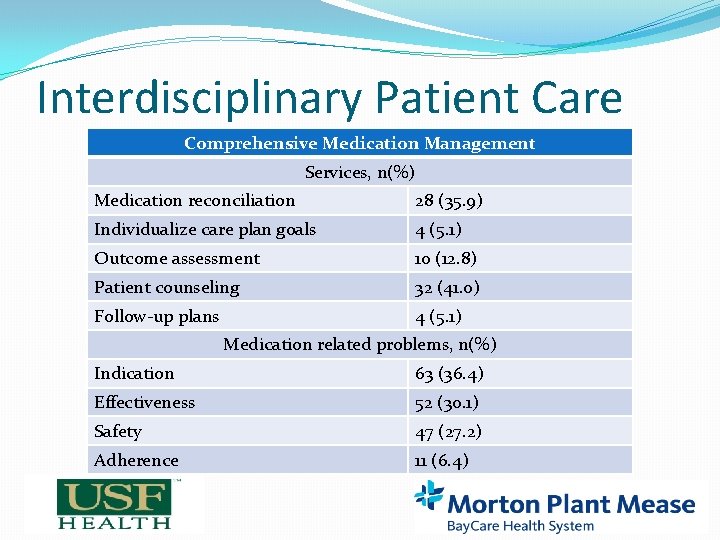
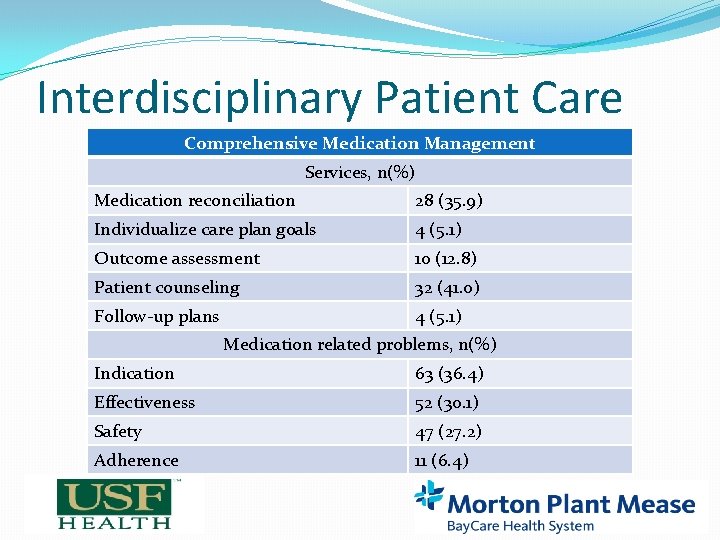
Interdisciplinary Patient Care Comprehensive Medication Management Services, n(%) Medication reconciliation 28 (35. 9) Individualize care plan goals 4 (5. 1) Outcome assessment 10 (12. 8) Patient counseling 32 (41. 0) Follow-up plans 4 (5. 1) Medication related problems, n(%) Indication 63 (36. 4) Effectiveness 52 (30. 1) Safety 47 (27. 2) Adherence 11 (6. 4)
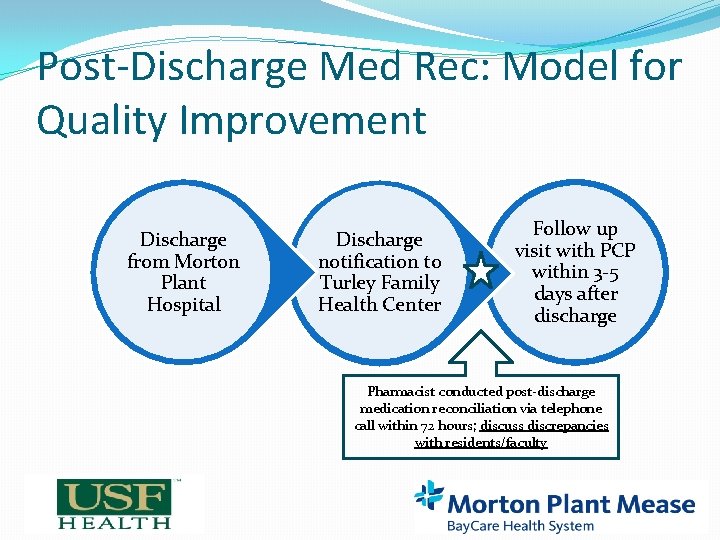
Post-Discharge Med Rec: Model for Quality Improvement Discharge from Morton Plant Hospital Discharge notification to Turley Family Health Center Follow up visit with PCP within 3 -5 days after discharge Pharmacist conducted post-discharge medication reconciliation via telephone call within 72 hours; discuss discrepancies with residents/faculty 14
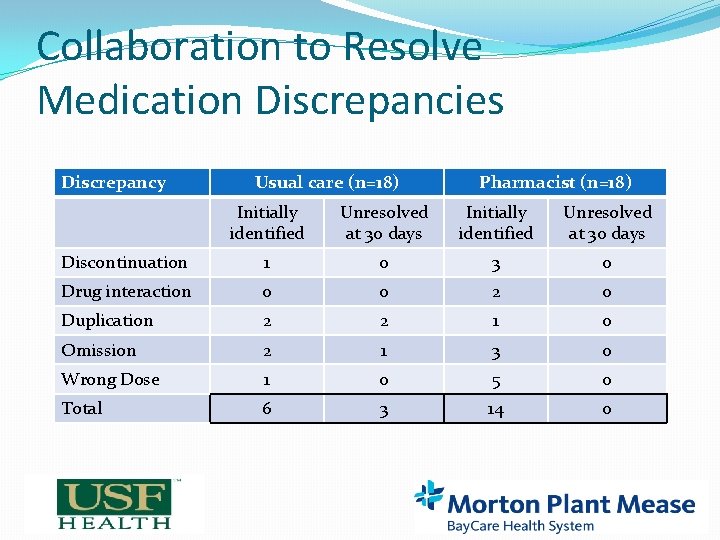
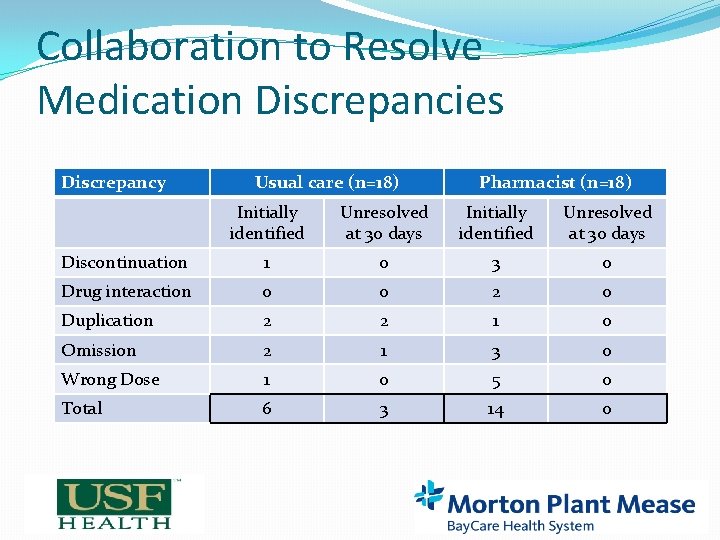
Collaboration to Resolve Medication Discrepancies Discrepancy Usual care (n=18) Pharmacist (n=18) Initially identified Unresolved at 30 days Discontinuation 1 0 3 0 Drug interaction 0 0 2 0 Duplication 2 2 1 0 Omission 2 1 3 0 Wrong Dose 1 0 5 0 Total 6 3 14 0
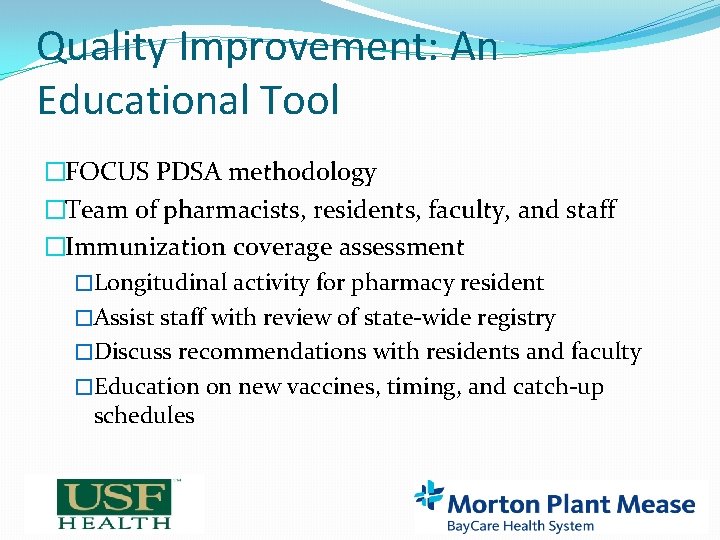
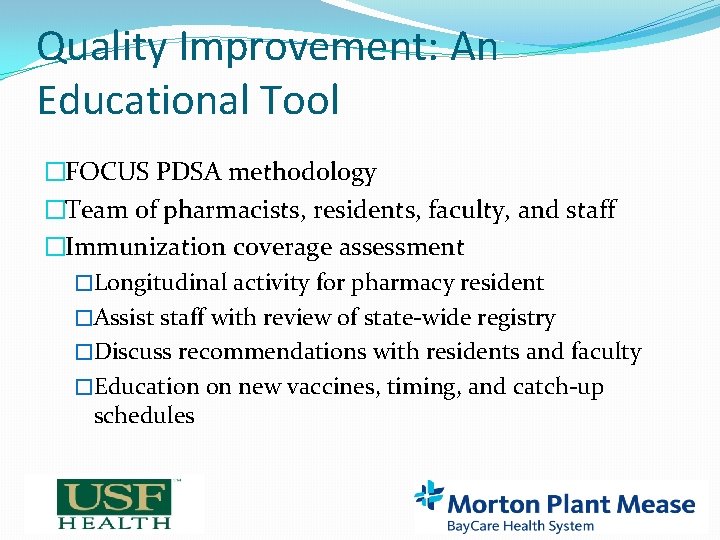
Quality Improvement: An Educational Tool �FOCUS PDSA methodology �Team of pharmacists, residents, faculty, and staff �Immunization coverage assessment �Longitudinal activity for pharmacy resident �Assist staff with review of state-wide registry �Discuss recommendations with residents and faculty �Education on new vaccines, timing, and catch-up schedules
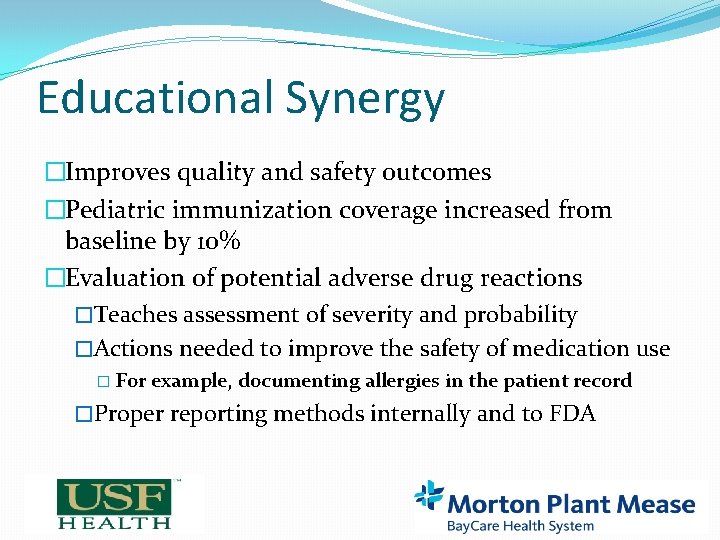
Educational Synergy �Improves quality and safety outcomes �Pediatric immunization coverage increased from baseline by 10% �Evaluation of potential adverse drug reactions �Teaches assessment of severity and probability �Actions needed to improve the safety of medication use � For example, documenting allergies in the patient record �Proper reporting methods internally and to FDA
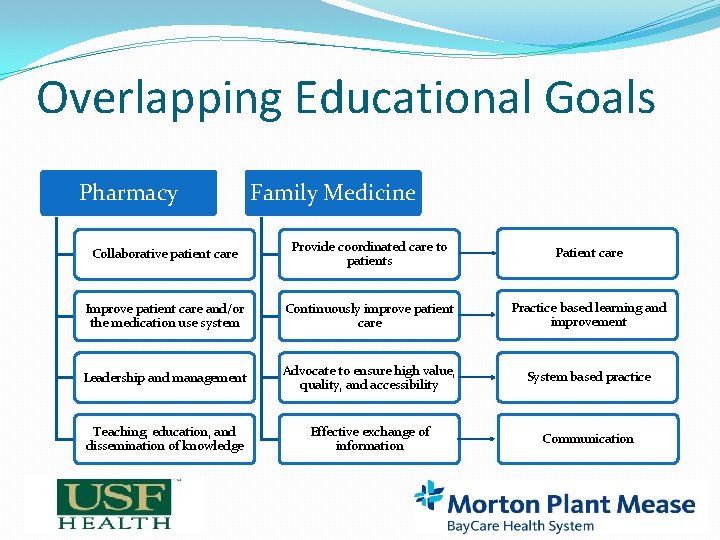
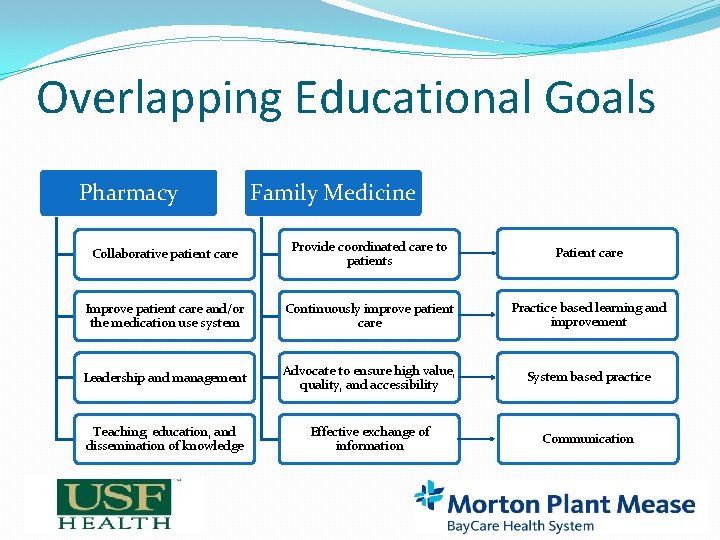
Overlapping Educational Goals Pharmacy Family Medicine Collaborative patient care Provide coordinated care to patients Patient care Improve patient care and/or the medication use system Continuously improve patient care Practice based learning and improvement Leadership and management Advocate to ensure high value, quality, and accessibility System based practice Teaching, education, and dissemination of knowledge Effective exchange of information Communication
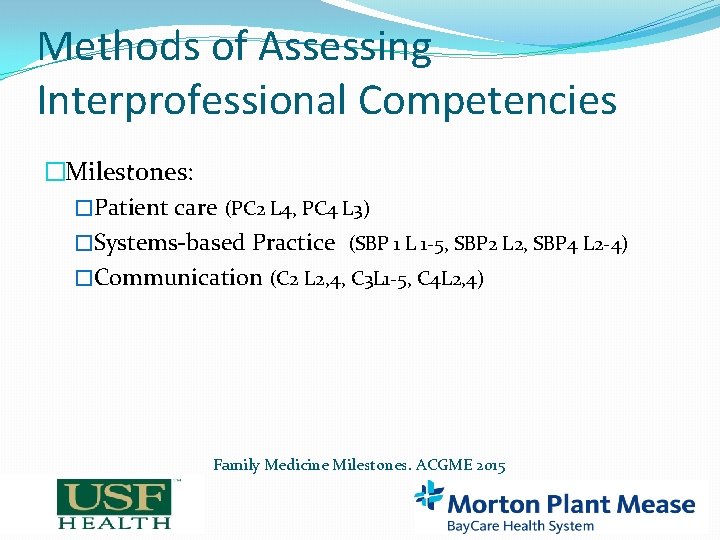
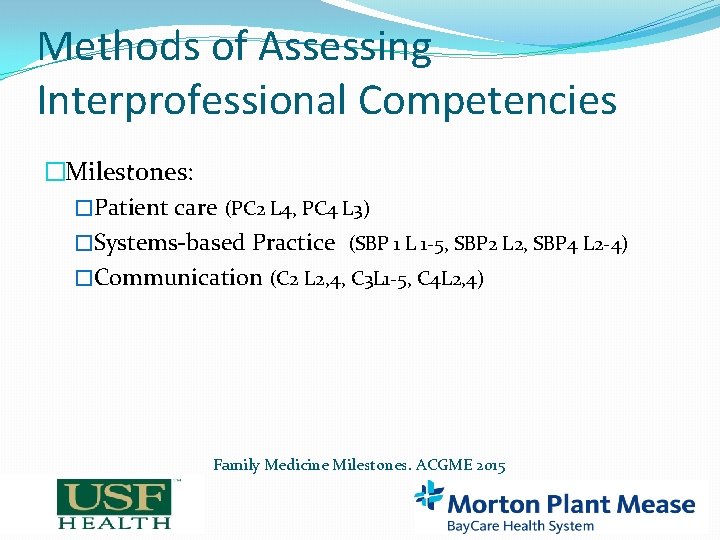
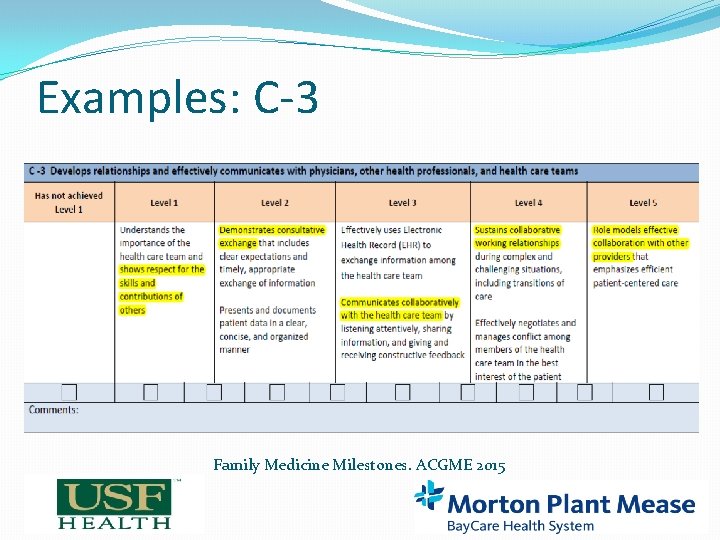
Methods of Assessing Interprofessional Competencies �Milestones: �Patient care (PC 2 L 4, PC 4 L 3) �Systems-based Practice (SBP 1 L 1 -5, SBP 2 L 2, SBP 4 L 2 -4) �Communication (C 2 L 2, 4, C 3 L 1 -5, C 4 L 2, 4) Family Medicine Milestones. ACGME 2015
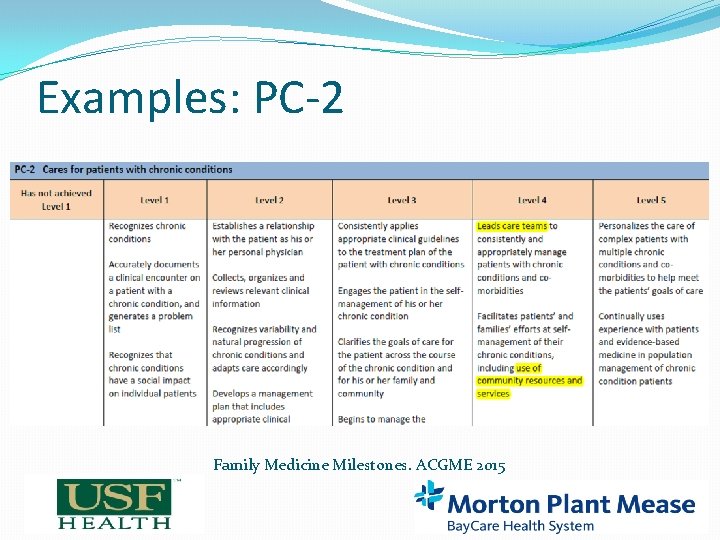
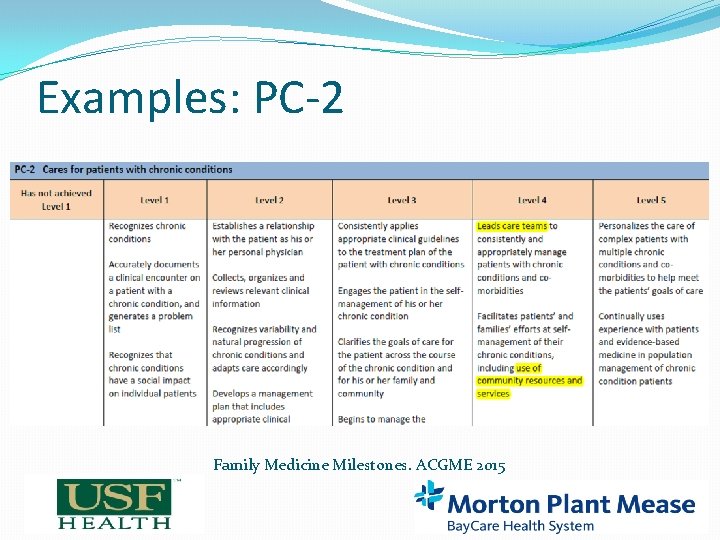
Examples: PC-2 Family Medicine Milestones. ACGME 2015
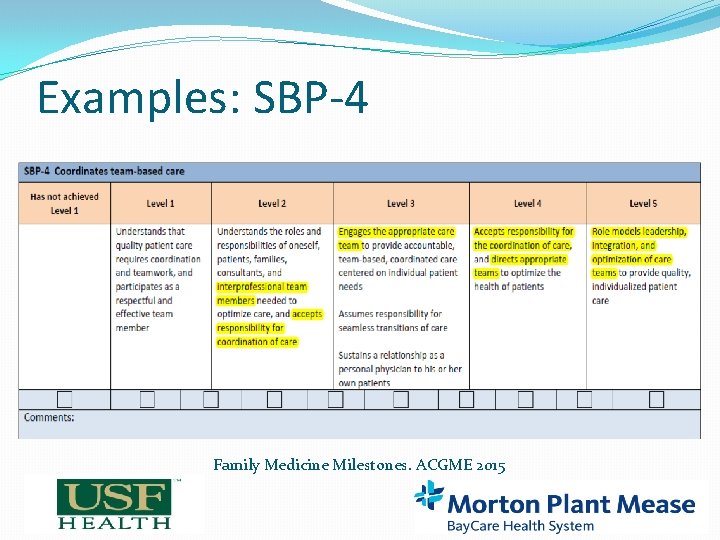
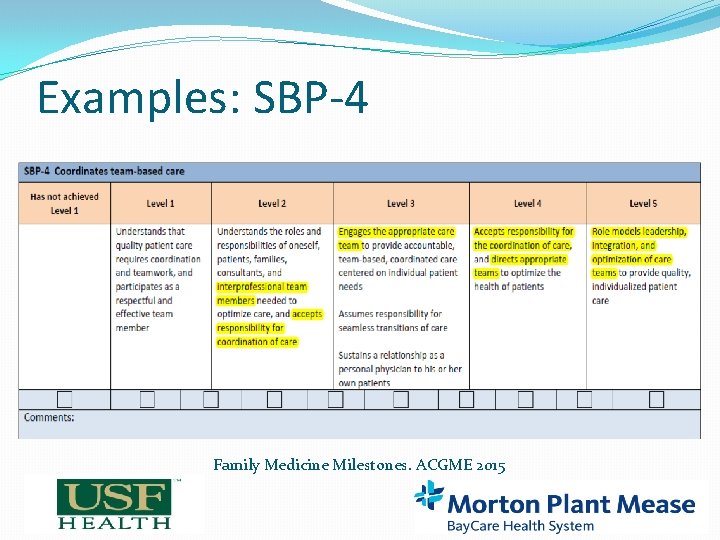
Examples: SBP-4 Family Medicine Milestones. ACGME 2015
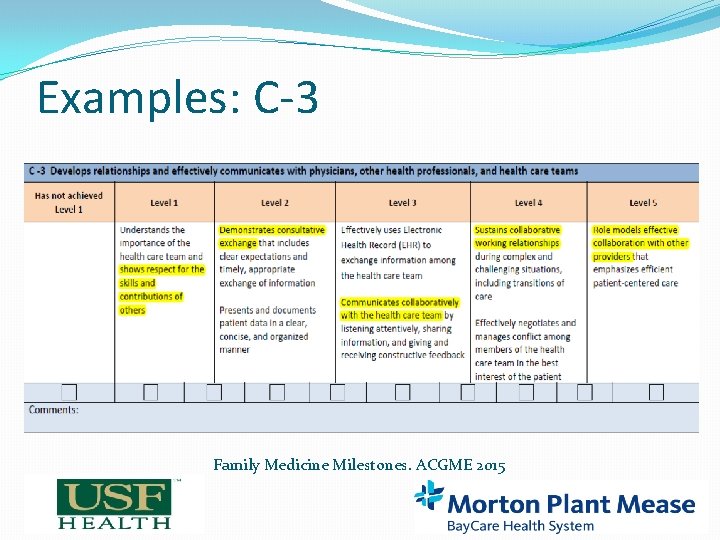
Examples: C-3 Family Medicine Milestones. ACGME 2015
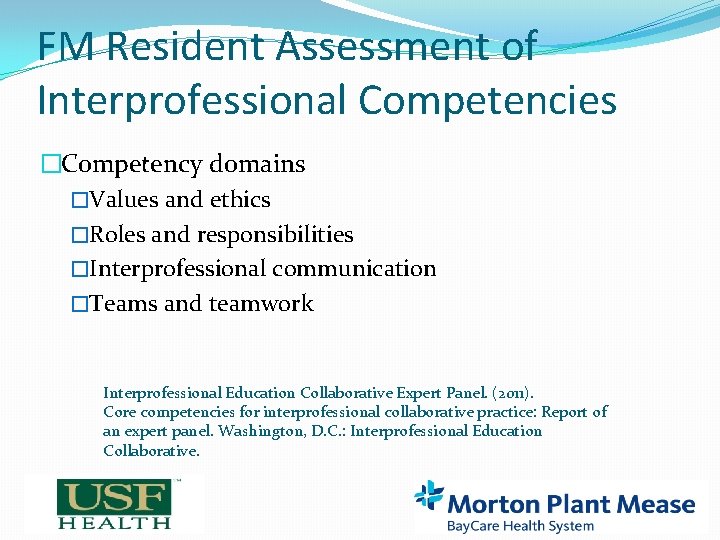
FM Resident Assessment of Interprofessional Competencies �Competency domains �Values and ethics �Roles and responsibilities �Interprofessional communication �Teams and teamwork Interprofessional Education Collaborative Expert Panel. (2011). Core competencies for interprofessional collaborative practice: Report of an expert panel. Washington, D. C. : Interprofessional Education Collaborative.
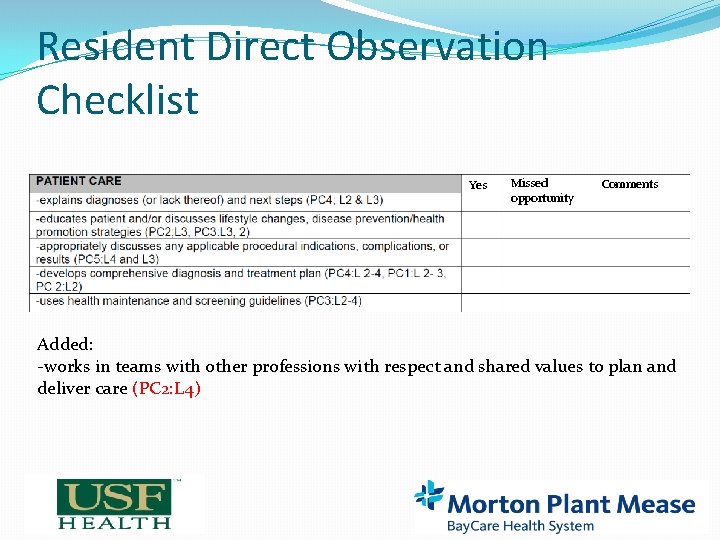
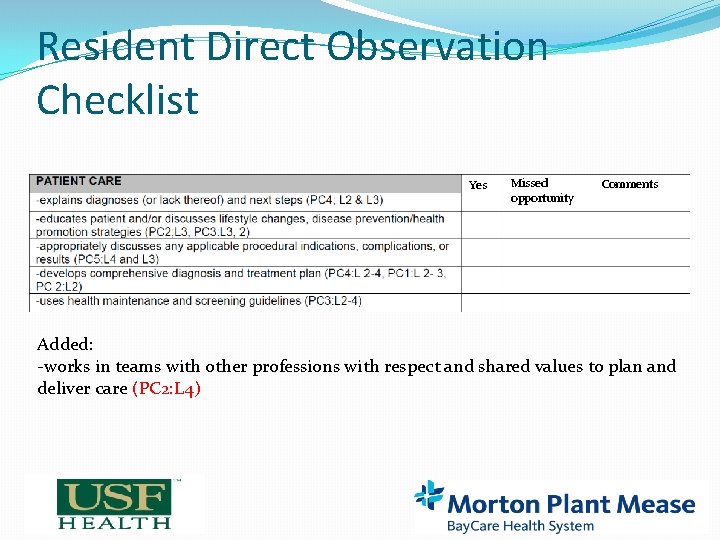
Resident Direct Observation Checklist Yes Missed opportunity Comments Added: -works in teams with other professions with respect and shared values to plan and deliver care (PC 2: L 4)
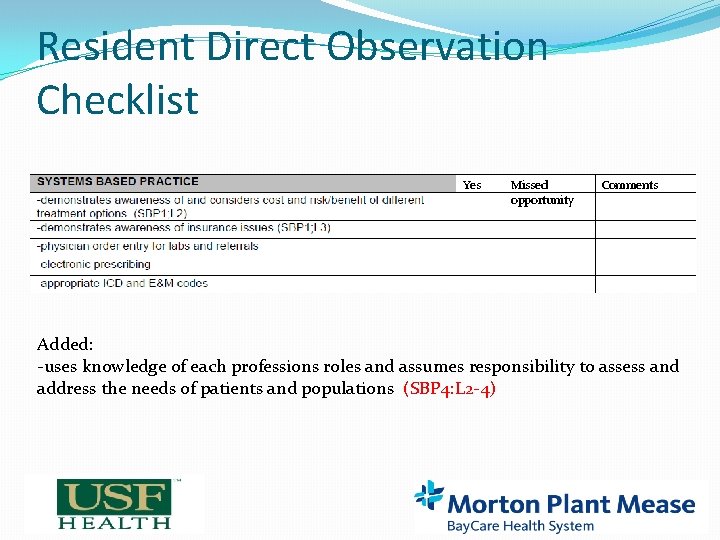
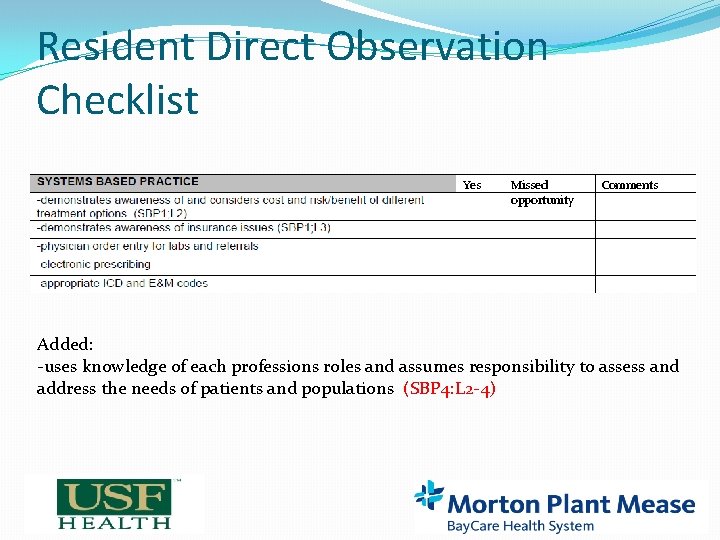
Resident Direct Observation Checklist Yes Missed opportunity Comments Added: -uses knowledge of each professions roles and assumes responsibility to assess and address the needs of patients and populations (SBP 4: L 2 -4)
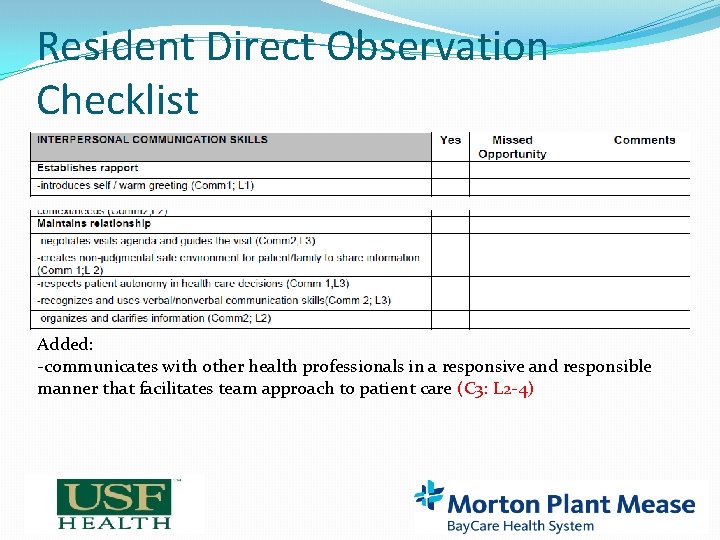
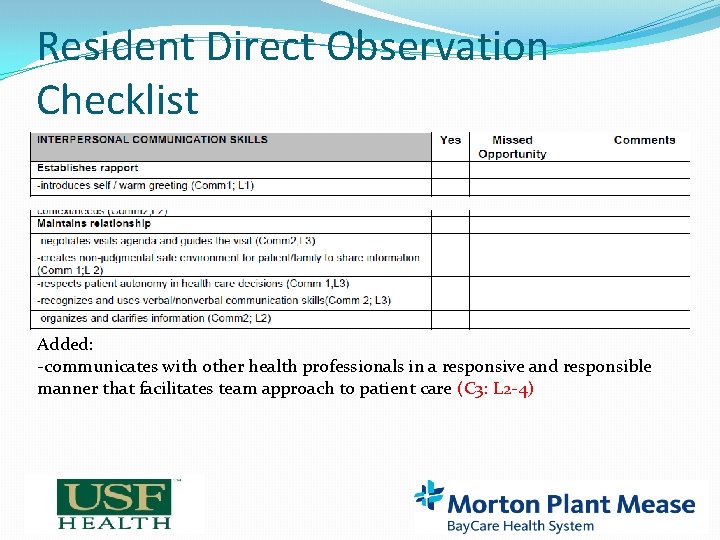
Resident Direct Observation Checklist Added: -communicates with other health professionals in a responsive and responsible manner that facilitates team approach to patient care (C 3: L 2 -4)
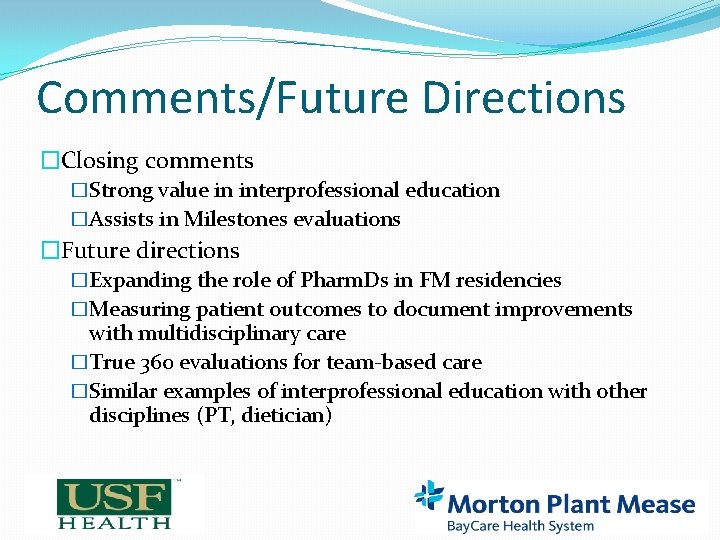
Comments/Future Directions �Closing comments �Strong value in interprofessional education �Assists in Milestones evaluations �Future directions �Expanding the role of Pharm. Ds in FM residencies �Measuring patient outcomes to document improvements with multidisciplinary care �True 360 evaluations for team-based care �Similar examples of interprofessional education with other disciplines (PT, dietician)
References � Whelan AM, Burge F, Munroe K. Pharmacy services in family medicine residencies. Survey of clinics associated with Canadian residency programs. Canadian Family Physician. 1994; 40: 468 -471. � Dickerson L, Denham AM, Lynch T. The State of Clinical Pharmacy Practice in Family Practice Residency Programs. Fam Med 2002; 34(9): 653 -657. � Lounsbery JL, Moon J, Humphrey A, Prasad <. Optimizing Physician Use of Clinical Pharmacy Services. Fam Med 2012; 45(1): 33 -37. � Dolovich L, Pottie K, Kaczorowski J, et al. Integrating family medicine and pharmacy to advance primary care therapeutics. Clin Pharmacol Ther 2008; 83(6): 913 -7.
References � Donald M. Berwick, Thomas W. Nolan, John Whittington. The triple aim: care, health, and cost. Health Aff (Millwood) 2008. May. Jun; 27(3): 759– 769. � Jarrett JB, Lounsbery JL, D’Amico F et al. Clinical Pharmacists as Educators in Family Medicine Residency Programs: A CERA Study of Program Directors. Fam Med 2016; 48(3): 180 -186. � Family Medicine Milestones. ACGME 2015. � Interprofessional Education Collaborative Expert Panel. (2011). Core competencies for interprofessional collaborative practice. Report of an expert panel. Washington, D. C. : Interprofessional Education Collaborative.
Questions? Comments?