Interpretive Skills Basic Approach to the Chest CT
Interpretive Skills Basic Approach to the Chest CT Introduction to Body Radiology Concepts
Before You Begin This module, intended for pre-clinical medical students transitioning to the clinical years, assumes familiarity with fundamental anatomy and pathology concepts. Please review our website sections: • “Anatomy” • “Radiology-Pathology” If you need to learn or review these core concepts prior to initiating this interpretive skills module If material is repeated from another module, it will be outlined as this text is so that you are aware
Objectives • Interpret the radiographic appearance of common Chest CT diagnoses • Be familiar with radiographic terminology and anatomical landmarks of the adult chest CT • Begin to develop an approach to reading the adult chest CT
General Principles
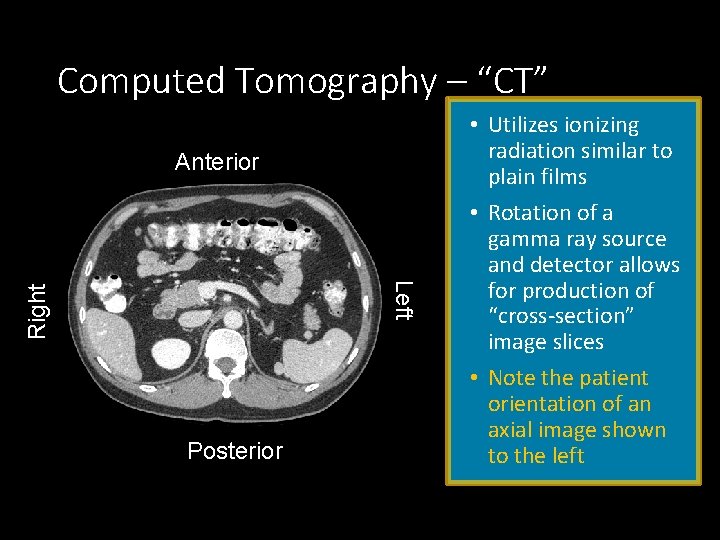
Computed Tomography – “CT” Anterior Right Left Posterior • Utilizes ionizing radiation similar to plain films • Rotation of a gamma ray source and detector allows for production of “cross-section” image slices • Note the patient orientation of an axial image shown to the left
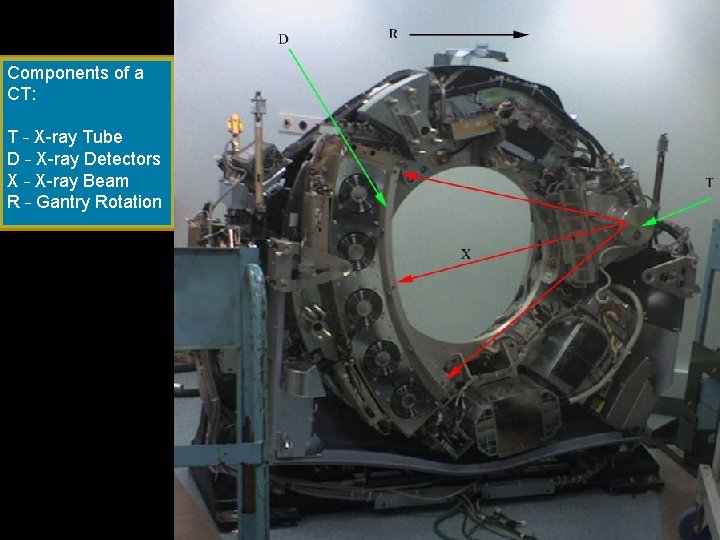
Components of a CT: T – X-ray Tube D – X-ray Detectors X – X-ray Beam R – Gantry Rotation
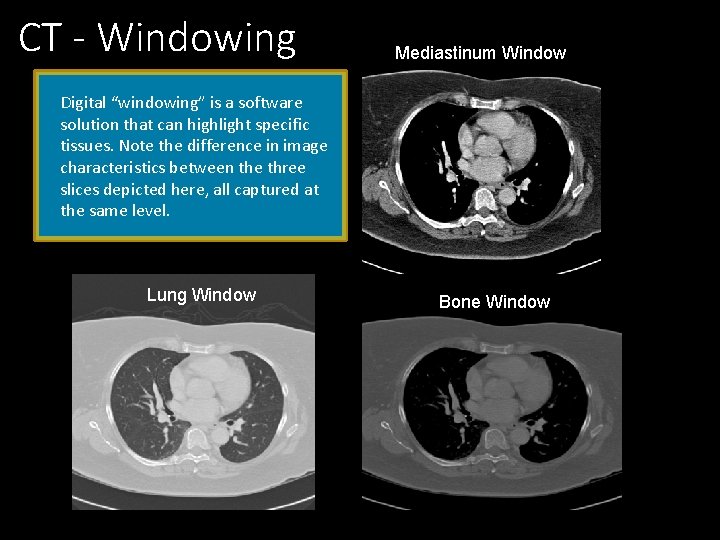
CT - Windowing Mediastinum Window Digital “windowing” is a software solution that can highlight specific tissues. Note the difference in image characteristics between the three slices depicted here, all captured at the same level. Lung Window Bone Window
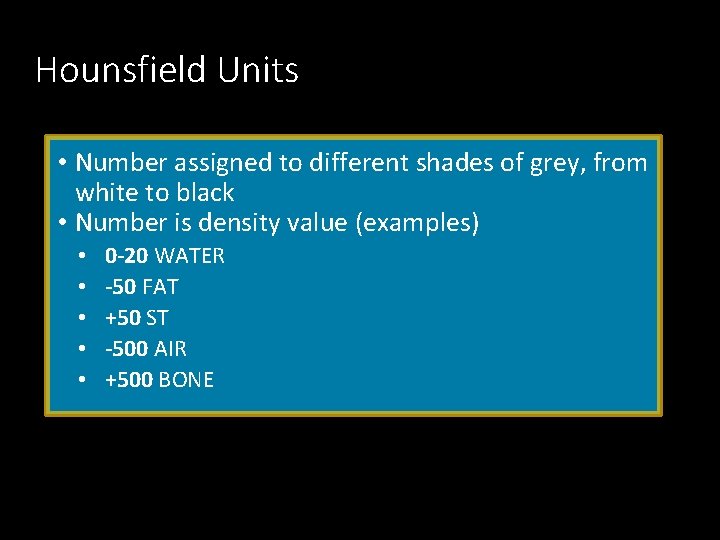
Hounsfield Units • Number assigned to different shades of grey, from white to black • Number is density value (examples) • • • 0 -20 WATER -50 FAT +50 ST -500 AIR +500 BONE
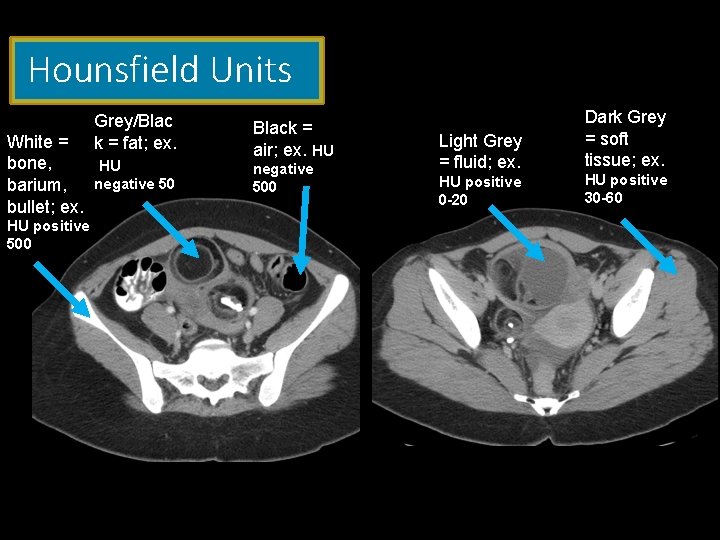
Hounsfield Units Grey/Blac k = fat; ex. White = bone, HU barium, negative 50 bullet; ex. HU positive 500 Black = air; ex. HU negative 500 Light Grey = fluid; ex. HU positive 0 -20 Dark Grey = soft tissue; ex. HU positive 30 -60
Special considerations in Chest CT Imaging Many issues unique to axial imaging • Improved spatial relations of complex overlapping anatomy (often accentuated by a patient unable to stay still) • Ability to differentiate soft tissue structures, specifically vessels (and endovascular findings!) – can generate angiograms (CTPA) • Relative increase in ionizing radiation exposure
High-resolution computed tomography (HRCT) • HRCT is a type of computed tomography (CT) with specific techniques to enhance image resolution. • All scans are “high resolution” currently • HRCT is used in the diagnosis of various health problems, though most commonly for lung disease, by assessing the lung parenchyma. • Specifically indicate special protocols when desired. • Ex. : Interstitial Lung disease (ILD) benefits from additional scans and reconstruction protocols
Contrast or No Contrast ? • CT plays an important role in diagnosis • • • Involved in chest wall Mediastinum Pleura Pulmonary arteries Lung parenchyma

Contrast or No Contrast ? Vascular Contrast: • Angiography (Pulmonary embolism) • Venography • Lymph node detection Vascular Contrast NOT generally required: • • • Solitary Pulmonary nodule Lung screening (low dose CT) Pulmonary parenchyma (infection, inflammation, edema) Interstitial lung disease (you want special “ILD protocol”) Pleural effusion Airway assessment
Approach to Chest CT Interpretation
Search Pattern There is no single correct approach The key is to be consistent in your approach/pattern • Identify both what is abnormal (not normally present) Yet…. • Also what is potentially missing (much harder!). Much depends on underlying anatomy – know your structures and expected relative relationships of these organs/tissues. No two patients or sequential images are identical and look the same. You must understand what causes the patterns presented.
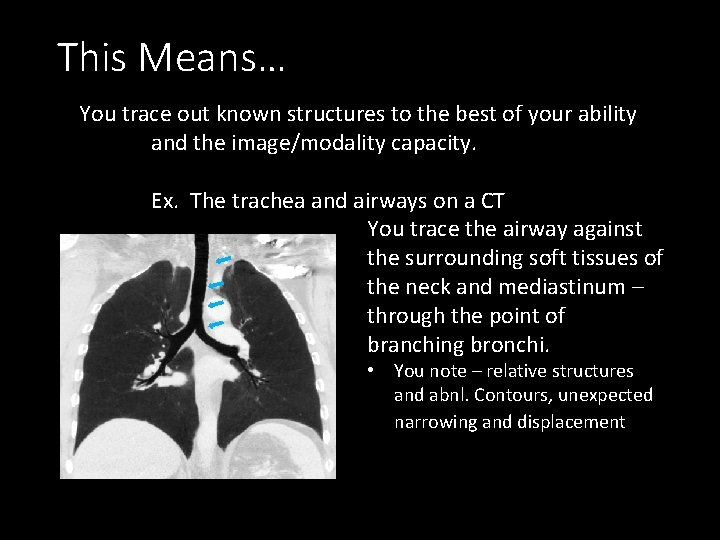
This Means… You trace out known structures to the best of your ability and the image/modality capacity. Ex. The trachea and airways on a CT You trace the airway against the surrounding soft tissues of the neck and mediastinum – through the point of branching bronchi. • You note – relative structures and abnl. Contours, unexpected narrowing and displacement
Search Pattern Lungs and Airway: • Lungs • Check for uniformity and properly tapering vessels towards fissures and peripheral margins Mediastinal structures/contour: • • Cardiac Size Check for pericardial effusion Outline major vessels (aneurysms/dissections/emboli) Check nodal stations for large lymph nodes (Abnl = >1 cm in short axis) Bones and Chest Wall: • Scan for uniformity – breaks and lytic/blastic abnormalities • Scan soft tissues and fat planes/muscles • Scan for lucent areas (gas)
Standard Radiology Report Clinical Data: This depends on information provided by the ordering physician --- Exams are optimized if this includes… • Signs/symptoms prompting the exam ordered. • Clinical Question “To be answered” Technique: A description of the exam details (often used for billing correlation). Comparison: This is a clear indication if and what prior exams were used in evaluation - particularly effective to discuss interval changes in condition. Indicates effectiveness of deployed interventions. Findings: Description of visualized findings and observations. Use of descriptors, many of which are non-specific or pathognomonic. Impression: Cohesive conclusive understanding of the findings discussed above, often with a potential differential or recommendation of what can be considered possible next steps, when the results are not explicit.
Standard Radiology Report Clinical Data: This depends information provided by the ordering physician --- Exams are optimized if this includes… • Signs/symptoms prompting the exam ordered. • Clinical Question “To be answered” Technique: A description of the exam details (often used for billing correlation). Comparison: This is a clear indication if and what prior exams were used in evaluation - particularly effective to discuss interval changes in condition. Indicates effectiveness of deployed interventions. Findings: Description of visualized findings and observations. Use of descriptors, many of which are non-specific or pathognomonic. Impression: Cohesive conclusive understanding of the findings discussed above, often with a potential differential or recommendation of what can be considered possible next steps, when the results are not explicit.
Standard Radiology Report Clinical Data: This depends information provided by the ordering physician --- Exams are optimized if this includes… • Signs/symptoms prompting the exam ordered. • Clinical Question “To be answered” Technique: A description of the exam details (often used for billing correlation). Comparison: This is a clear indication if and what prior exams were used in evaluation - particularly effective to discuss interval changes in condition. Indicates effectiveness of deployed interventions. Findings: Description of visualized findings and observations. Use of descriptors, many of which are non-specific or pathognomonic. Impression: Cohesive conclusive understanding of the findings discussed above, often with a potential differential or recommendation of what can be considered possible next steps, when the results are not explicit.
Standard Radiology Report Clinical Data: This depends information provided by the ordering physician --- Exams are optimized if this includes… • Signs/symptoms prompting the exam ordered. • Clinical Question “To be answered” Technique: A description of the exam details (often used for billing correlation). Comparison: This is a clear indication if and what prior exams were used in evaluation - particularly effective to discuss interval changes in condition. Indicates effectiveness of deployed interventions. Findings: Description of visualized findings and observations. Use of descriptors, many of which are non-specific or pathognomonic. Impression: Cohesive conclusive understanding of the findings discussed above, often with a potential differential or recommendation of what can be considered possible next steps, when the results are not explicit.
Standard Radiology Report Clinical Data: This depends information provided by the ordering physician --- Exams are optimized if this includes… • Signs/symptoms prompting the exam ordered. • Clinical Question “To be answered” Technique: A description of the exam details (often used for billing correlation). Comparison: This is a clear indication if and what prior exams were used in evaluation - particularly effective to discuss interval changes in condition. Indicates effectiveness of deployed interventions. Findings: Description of visualized findings and observations. Use of descriptors, many of which are non-specific or pathognomonic. Impression: Cohesive conclusive understanding of the findings discussed above, often with a potential differential or recommendation of what can be considered possible next steps, when the results are not explicit.
Standard Radiology Report Clinical Data: This depends information provided by the ordering physician --- Exams are optimized if this includes… • Signs/symptoms prompting the exam ordered. • Clinical Question “To be answered” Technique: A description of the exam details (often used for billing correlation). Comparison: This is a clear indication if and what prior exams were used in evaluation - particularly effective to discuss interval changes in condition. Indicates effectiveness of deployed interventions. Findings: Description of visualized findings and observations. Use of descriptors, many of which are non-specific or pathognomonic. Impression: Cohesive conclusive understanding of the findings discussed above, often with a potential differential or recommendation of what can be considered possible next steps, when the results are not explicit.
Identifying Pathology
CHEST CT - Lungs • • Pneumonia Interstitial opacity Emphysema Pulmonary Mass Pulmonary Solid Nodule Groundglass nodule (GGN) Effusion
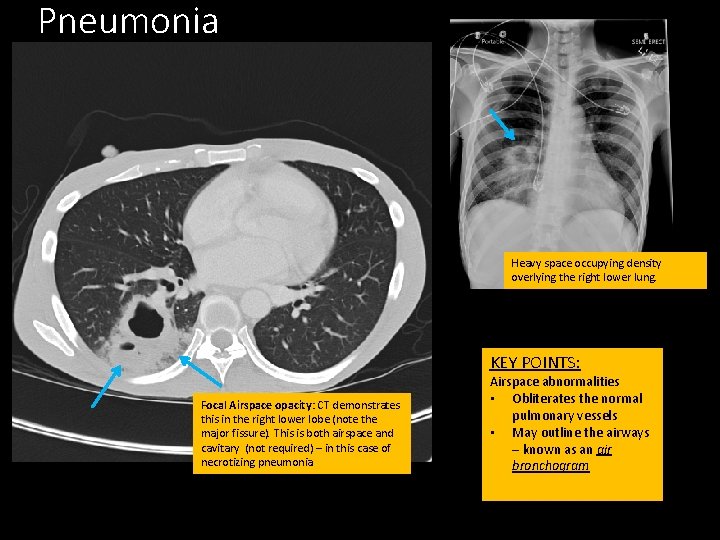
Pneumonia Heavy space occupying density overlying the right lower lung. KEY POINTS: Focal Airspace opacity: CT demonstrates this in the right lower lobe (note the major fissure). This is both airspace and cavitary (not required) – in this case of necrotizing pneumonia Airspace abnormalities • Obliterates the normal pulmonary vessels • May outline the airways – known as an air bronchogram
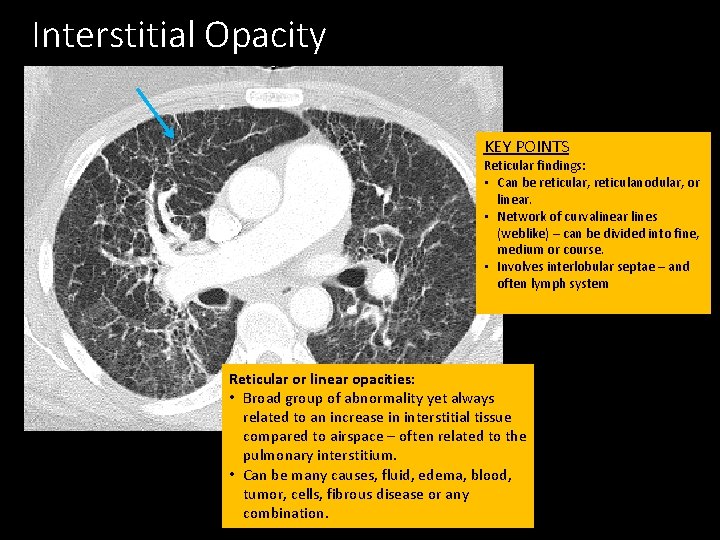
Interstitial Opacity KEY POINTS Reticular findings: • Can be reticular, reticulanodular, or linear. • Network of curvalinear lines (weblike) – can be divided into fine, medium or course. • Involves interlobular septae – and often lymph system Reticular or linear opacities: • Broad group of abnormality yet always related to an increase in interstitial tissue compared to airspace – often related to the pulmonary interstitium. • Can be many causes, fluid, edema, blood, tumor, cells, fibrous disease or any combination.
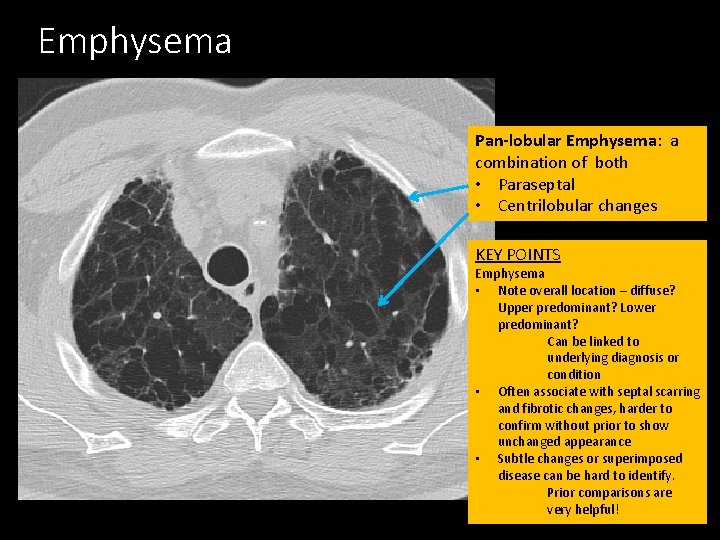
Emphysema Pan-lobular Emphysema: a combination of both • Paraseptal • Centrilobular changes KEY POINTS Emphysema • Note overall location – diffuse? Upper predominant? Lower predominant? Can be linked to underlying diagnosis or condition • Often associate with septal scarring and fibrotic changes, harder to confirm without prior to show unchanged appearance • Subtle changes or superimposed disease can be hard to identify. Prior comparisons are very helpful!
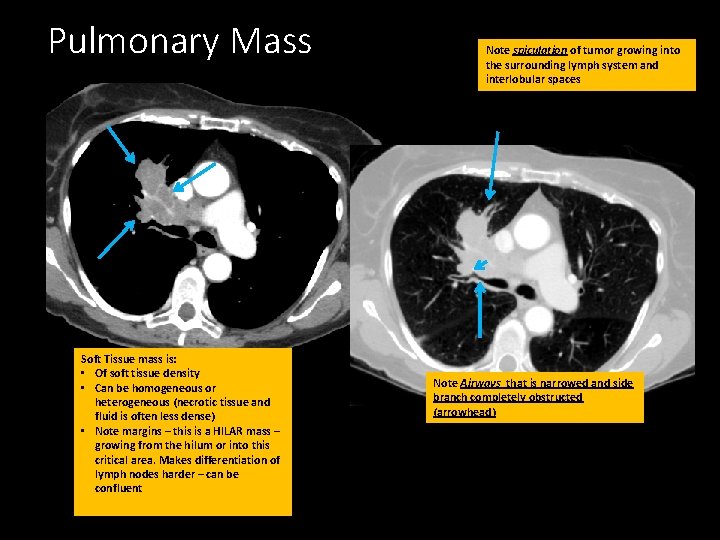
Pulmonary Mass Soft Tissue mass is: • Of soft tissue density • Can be homogeneous or heterogeneous (necrotic tissue and fluid is often less dense) • Note margins – this is a HILAR mass – growing from the hilum or into this critical area. Makes differentiation of lymph nodes harder – can be confluent Note spiculation of tumor growing into the surrounding lymph system and interlobular spaces Note Airways that is narrowed and side branch completely obstructed (arrowhead)
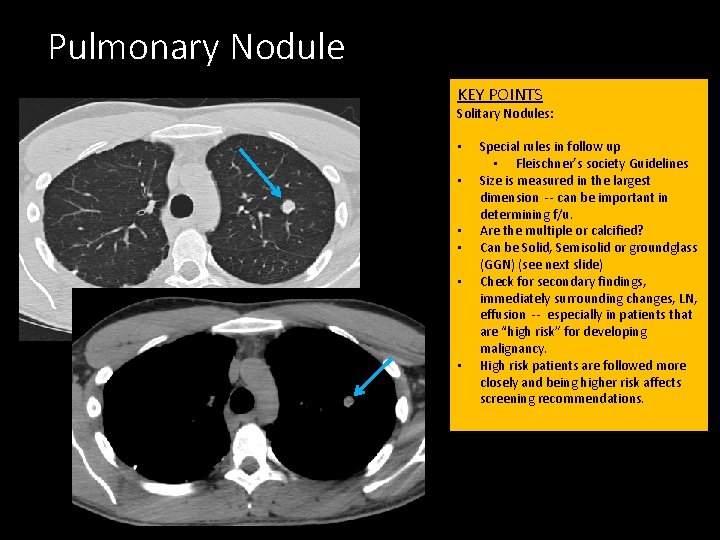
Pulmonary Nodule KEY POINTS Solitary Nodules: • • • Special rules in follow up • Fleischner’s society Guidelines Size is measured in the largest dimension -- can be important in determining f/u. Are the multiple or calcified? Can be Solid, Semisolid or groundglass (GGN) (see next slide) Check for secondary findings, immediately surrounding changes, LN, effusion -- especially in patients that are “high risk” for developing malignancy. High risk patients are followed more closely and being higher risk affects screening recommendations.
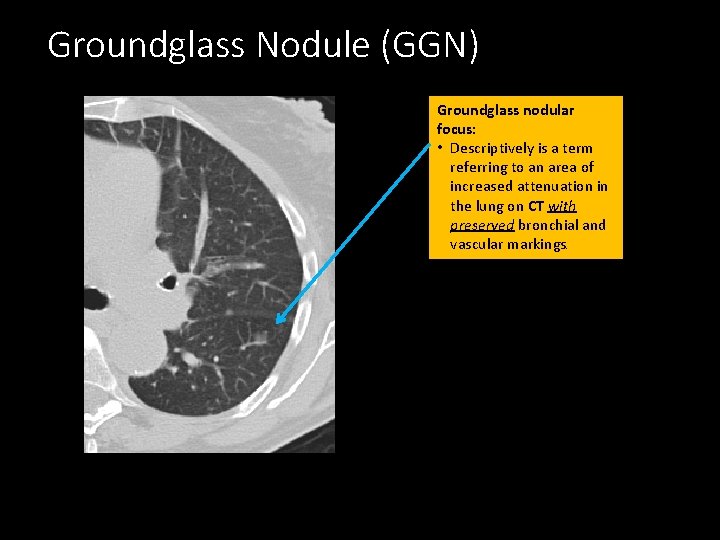
Groundglass Nodule (GGN) Groundglass nodular focus: • Descriptively is a term referring to an area of increased attenuation in the lung on CT with preserved bronchial and vascular markings.
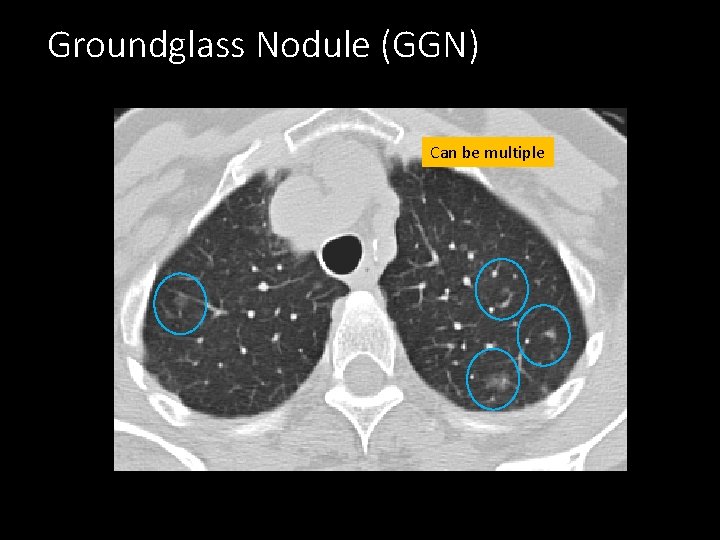
Groundglass Nodule (GGN) Can be multiple
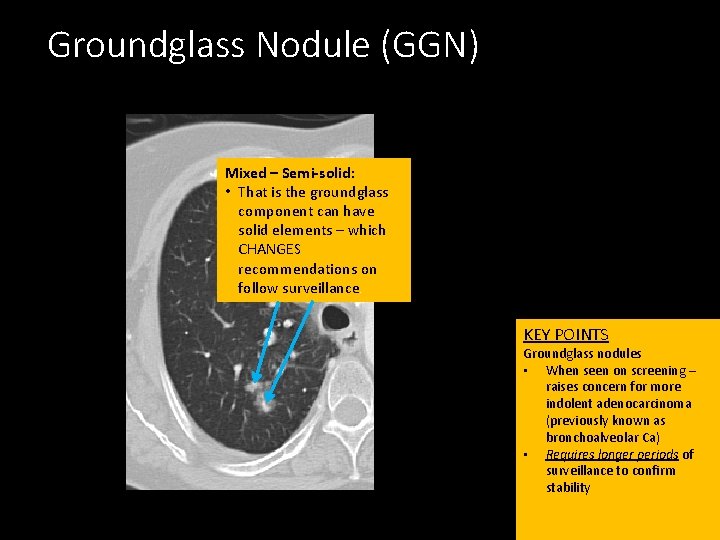
Groundglass Nodule (GGN) Mixed – Semi-solid: • That is the groundglass component can have solid elements – which CHANGES recommendations on follow surveillance. KEY POINTS Groundglass nodules • When seen on screening – raises concern for more indolent adenocarcinoma (previously known as bronchoalveolar Ca) • Requires longer periods of surveillance to confirm stability
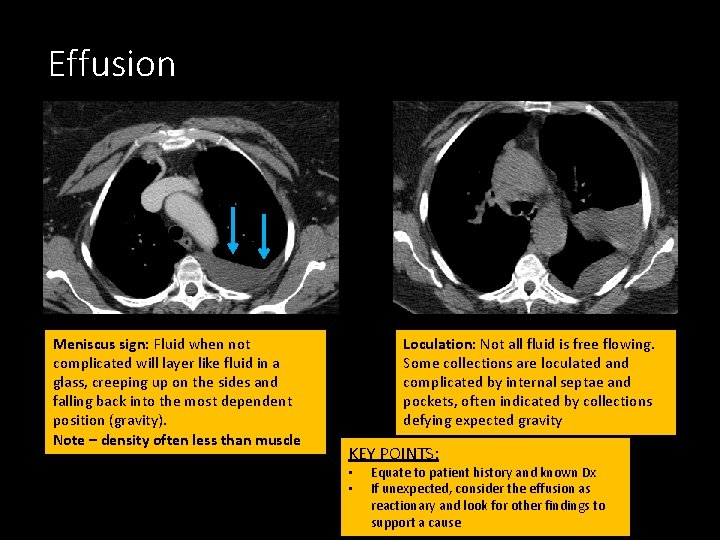
Effusion Meniscus sign: Fluid when not complicated will layer like fluid in a glass, creeping up on the sides and falling back into the most dependent position (gravity). Note – density often less than muscle Loculation: Not all fluid is free flowing. Some collections are loculated and complicated by internal septae and pockets, often indicated by collections defying expected gravity KEY POINTS: • • Equate to patient history and known Dx If unexpected, consider the effusion as reactionary and look for other findings to support a cause
Mediastinum and Cardiac: – Cardiac Size and shape – Outline major vessels (aneurysms/dissections) – Check nodal stations for large lymph nodes (>1 cm in short axis)
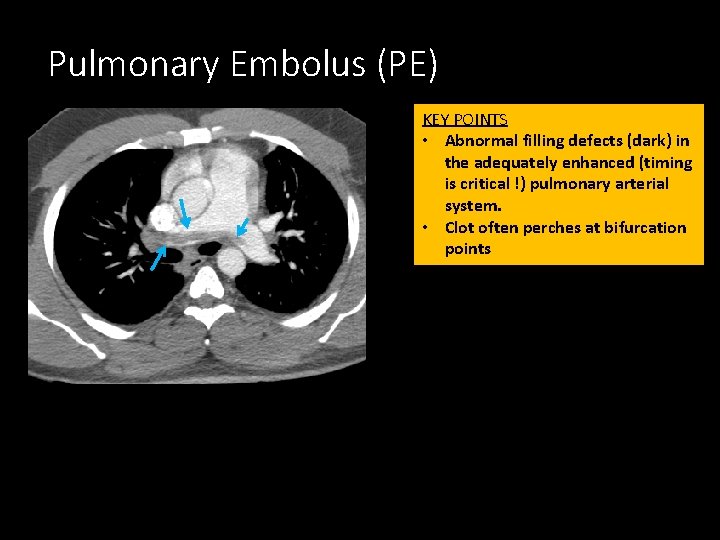
Pulmonary Embolus (PE) KEY POINTS • Abnormal filling defects (dark) in the adequately enhanced (timing is critical !) pulmonary arterial system. • Clot often perches at bifurcation points
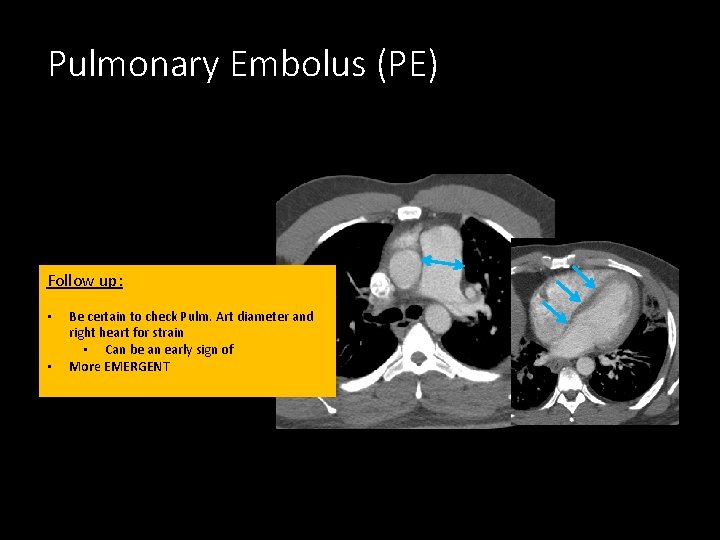
Pulmonary Embolus (PE) Follow up: • • Be certain to check Pulm. Art diameter and right heart for strain • Can be an early sign of More EMERGENT
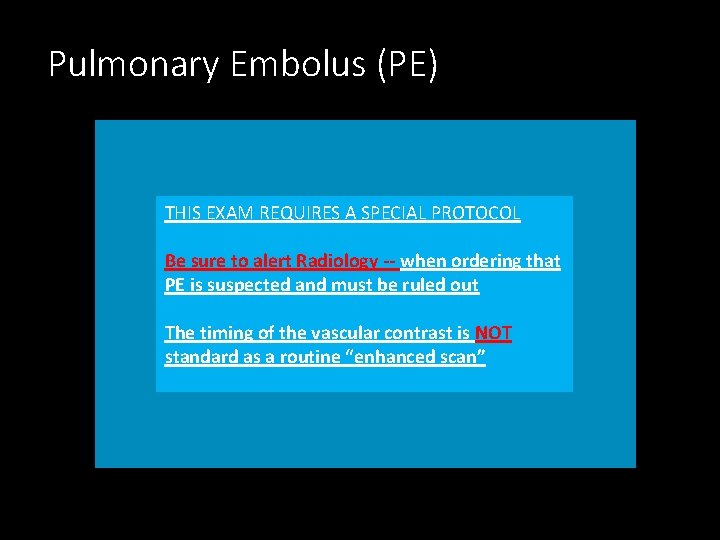
Pulmonary Embolus (PE) THIS EXAM REQUIRES A SPECIAL PROTOCOL Be sure to alert Radiology -- when ordering that PE is suspected and must be ruled out The timing of the vascular contrast is NOT standard as a routine “enhanced scan”
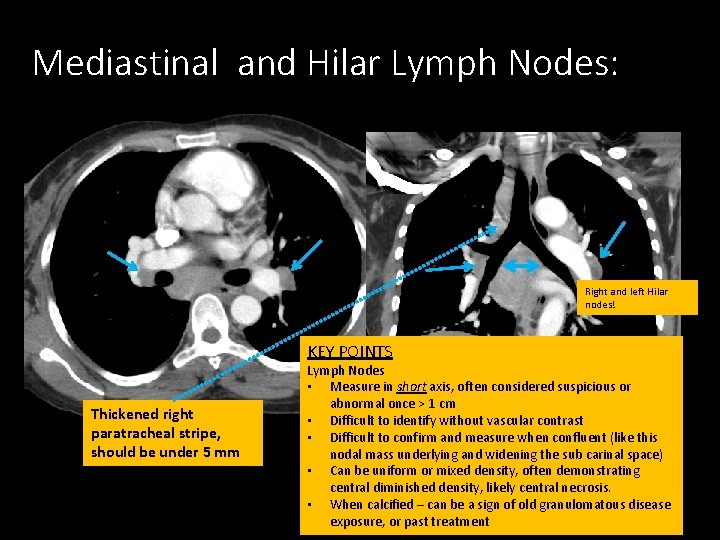
Mediastinal and Hilar Lymph Nodes: Right and left Hilar nodes! KEY POINTS Thickened right paratracheal stripe, should be under 5 mm Lymph Nodes • Measure in short axis, often considered suspicious or abnormal once > 1 cm • Difficult to identify without vascular contrast • Difficult to confirm and measure when confluent (like this nodal mass underlying and widening the sub carinal space) • Can be uniform or mixed density, often demonstrating central diminished density, likely central necrosis. • When calcified – can be a sign of old granulomatous disease exposure, or past treatment
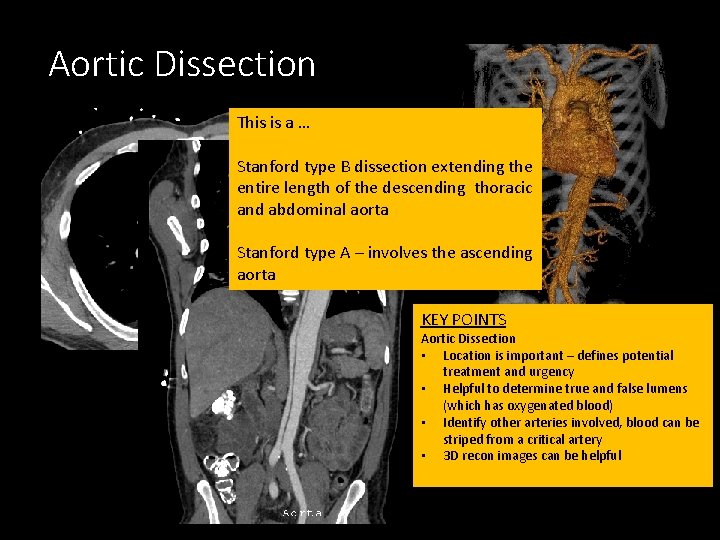
Aortic Dissection This is a … Stanford type B dissection extending the entire length of the descending thoracic and abdominal aorta Stanford type A – involves the ascending aorta KEY POINTS Aortic Dissection • Location is important – defines potential treatment and urgency • Helpful to determine true and false lumens (which has oxygenated blood) • Identify other arteries involved, blood can be striped from a critical artery • 3 D recon images can be helpful
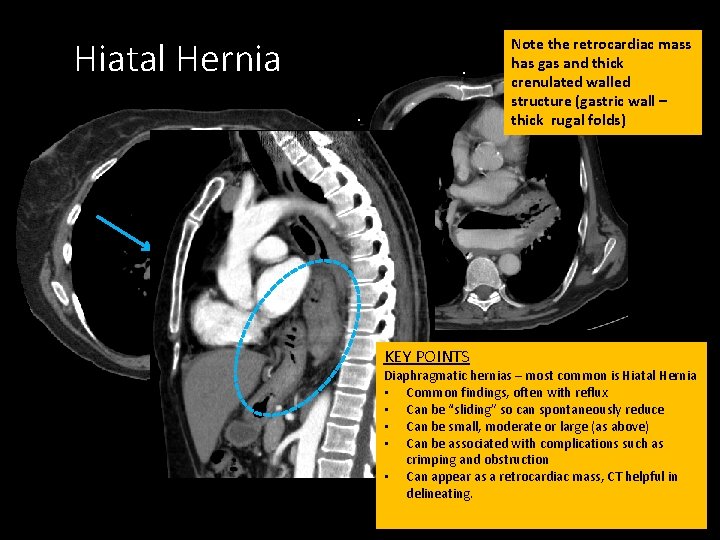
Hiatal Hernia Note the retrocardiac mass has gas and thick crenulated walled structure (gastric wall – thick rugal folds) KEY POINTS Diaphragmatic hernias – most common is Hiatal Hernia • Common findings, often with reflux • Can be “sliding” so can spontaneously reduce • Can be small, moderate or large (as above) • Can be associated with complications such as crimping and obstruction • Can appear as a retrocardiac mass, CT helpful in delineating.
Bones/Chest wall: – Scan for uniformity – breaks and lytic/blastic abnormalities – Scan soft tissues and fat planes/muscles – Scan for lucent areas (gas)
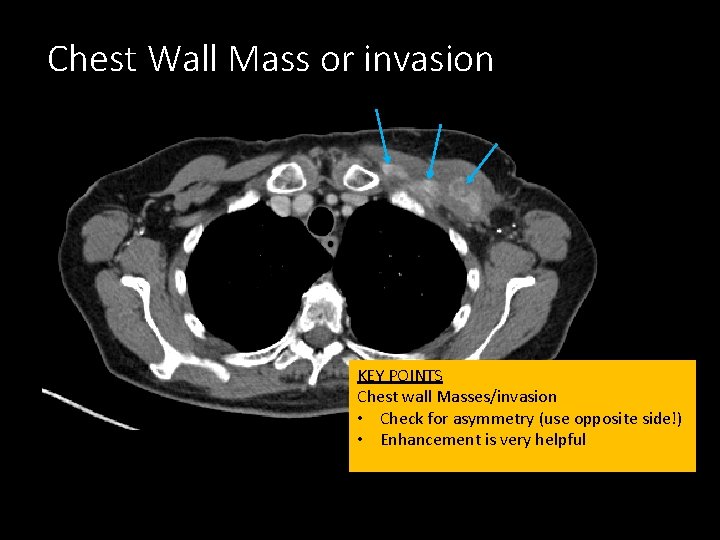
Chest Wall Mass or invasion KEY POINTS Chest wall Masses/invasion • Check for asymmetry (use opposite side!) • Enhancement is very helpful
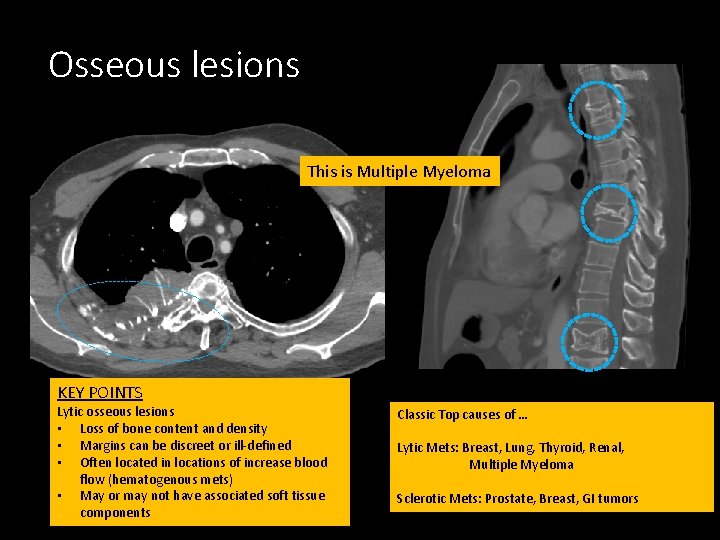
Osseous lesions This is Multiple Myeloma KEY POINTS Lytic osseous lesions • Loss of bone content and density • Margins can be discreet or ill-defined • Often located in locations of increase blood flow (hematogenous mets) • May or may not have associated soft tissue components Classic Top causes of … Lytic Mets: Breast, Lung, Thyroid, Renal, Multiple Myeloma Sclerotic Mets: Prostate, Breast, GI tumors
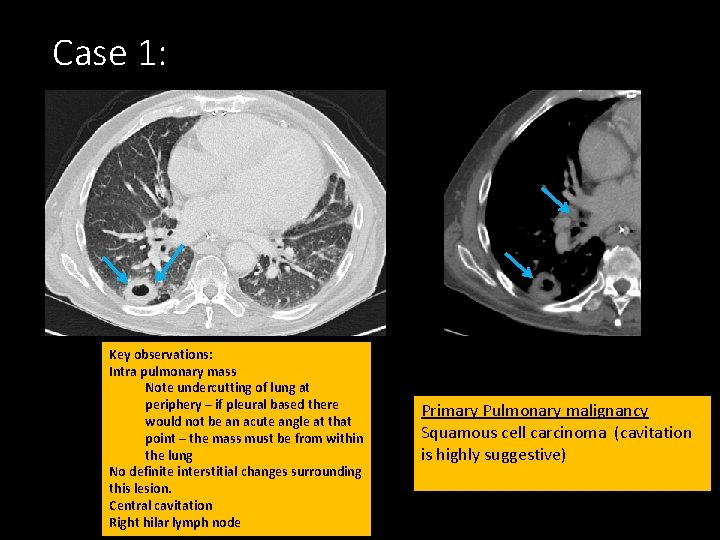
Case 1: Key observations: Intra pulmonary mass Note undercutting of lung at periphery – if pleural based there would not be an acute angle at that point – the mass must be from within the lung No definite interstitial changes surrounding this lesion. Central cavitation Right hilar lymph node Primary Pulmonary malignancy Squamous cell carcinoma (cavitation is highly suggestive)
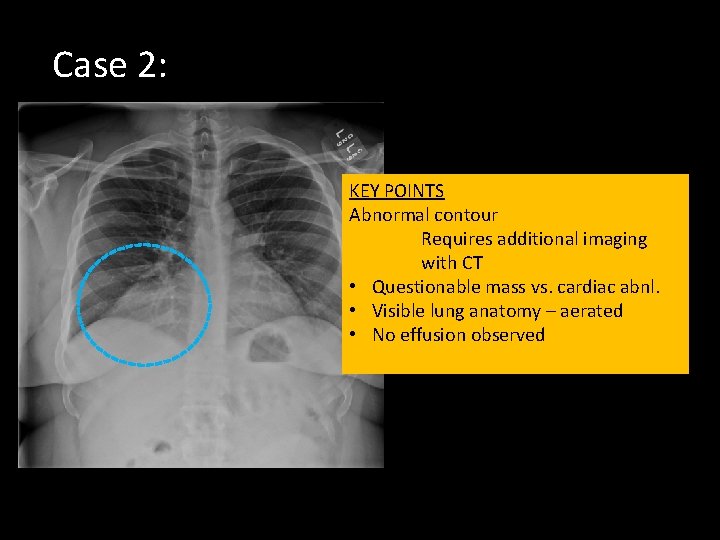
Case 2: KEY POINTS Abnormal contour Requires additional imaging with CT • Questionable mass vs. cardiac abnl. • Visible lung anatomy – aerated • No effusion observed
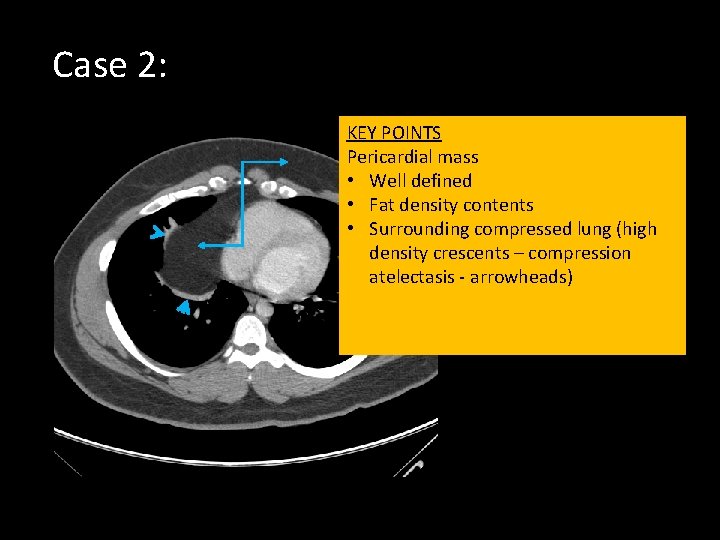
Case 2: KEY POINTS Pericardial mass • Well defined • Fat density contents • Surrounding compressed lung (high density crescents – compression atelectasis - arrowheads)
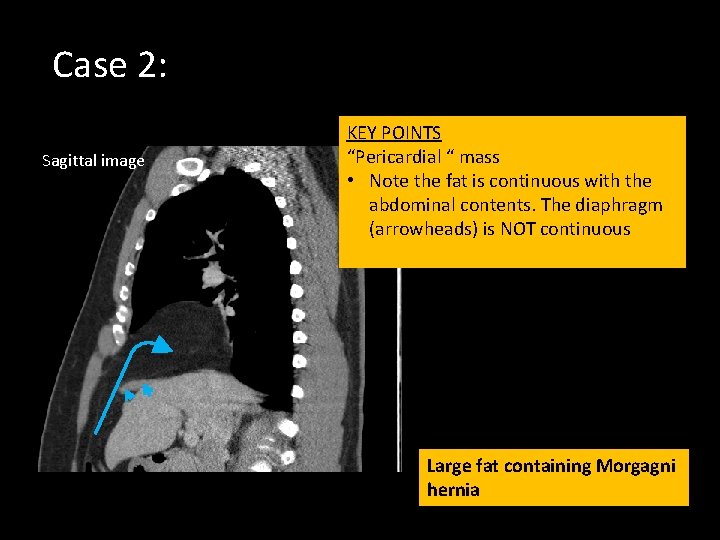
Case 2: Sagittal image KEY POINTS “Pericardial “ mass • Note the fat is continuous with the abdominal contents. The diaphragm (arrowheads) is NOT continuous Large fat containing Morgagni hernia
END
- Slides: 49