Internal Hernia a brief review of its clinical
Internal Hernia – a brief review of its clinical features and management Surgical Grand Round 22 nd Oct, 2011; UCH C C Chan; TMH
Hernia • Hernia: protrusion of part or whole of a viscus through an abnormal opening in the walls of its containing cavity (Bailey & Love’s 25 ) • internal: herniation confined to peritoneal cavity • external: herniation through defect in wall of abdomen or pelvis th
Internal Hernia • congenital or acquired • overall incidence < 1% (1) • 0. 6 - 5. 8% of small-bowel obstruction (SBO)(1) • incidence has been increasing (2) (1) Newsom BD, Kukora JS. Congenital and acquired internal hernias: unusual causes of small bowel obstruction. Am J Surg 1986; 152: 279– 284 (2) Higa KD, Ho T, Boone KB. Internal hernias after laparoscopic Roux-en-Y gastric bypass: Incidence, treatment and prevention. Obes Surg 2003; 13(3): 350– 4
Clinical features • symptoms & signs usually indistinguishable from band obstruction • mortality could be 50% (1) • usually diagnosed intra-op • ddx: external hernia, adhesion, intussusception, gall stone ileus (1) Mock CJ, Mock HE Jr. Strangulated internal hernia associated with trauma: Arch Surg 1958; 77: 881– 886
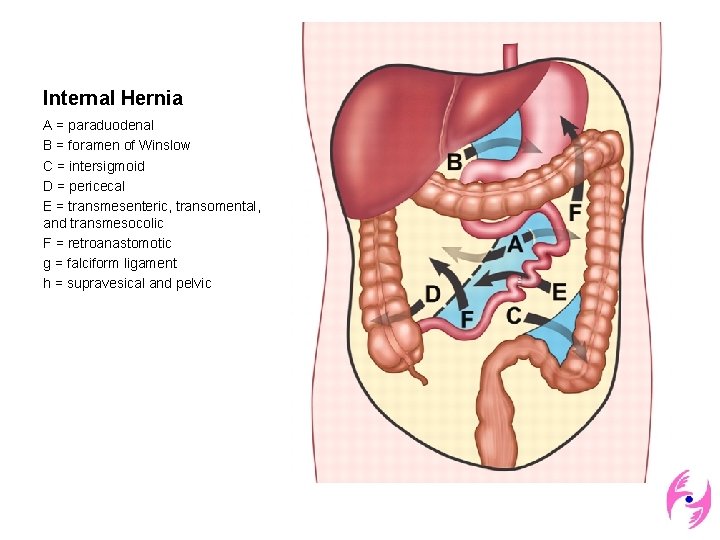
Internal Hernia A = paraduodenal B = foramen of Winslow C = intersigmoid D = pericecal E = transmesenteric, transomental, and transmesocolic F = retroanastomotic g = falciform ligament h = supravesical and pelvic

Anatomic predisposition to transmesenteric hernia with biliary-enteric anastomosis a) antecolic Roux-en-Y loop b) retrocolic Roux-en-Y loop
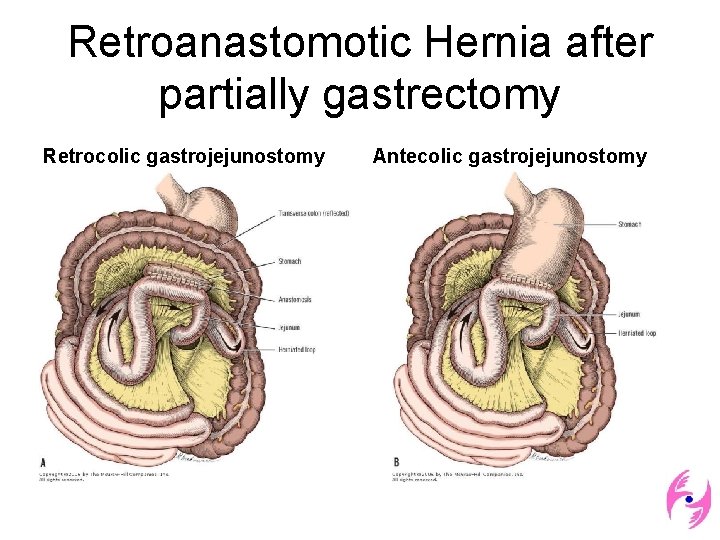
Retroanastomotic Hernia after partially gastrectomy Retrocolic gastrojejunostomy Antecolic gastrojejunostomy
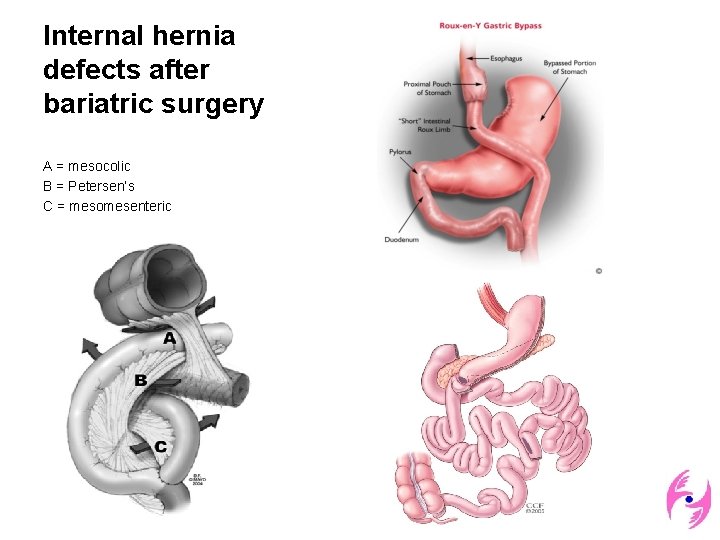
Internal hernia defects after bariatric surgery A = mesocolic B = Petersen’s C = mesomesenteric

Common symptoms • non-specific • asymptomatic • intermittent attacks of vague epigastric discomfort • colicky periumbilical pain • nausea, vomiting
Ever-changing severity • relates to duration and reducibility of hernia, presence or absence of incarceration and strangulation • may be altered by changes in posture
Imaging • • plain X ray abdomen USG abdomen barium enhanced studies / enteroclysis CT abdomen
Usual CT findings • crowded, distended bowel in abnormal location and arrangement • segmental dilatation and prolonged stasis within the herniated loops • stretched, displaced, crowded, and engorged mesenteric vessels • displacement of other bowel segments • (propensity to spontaneously reduce)
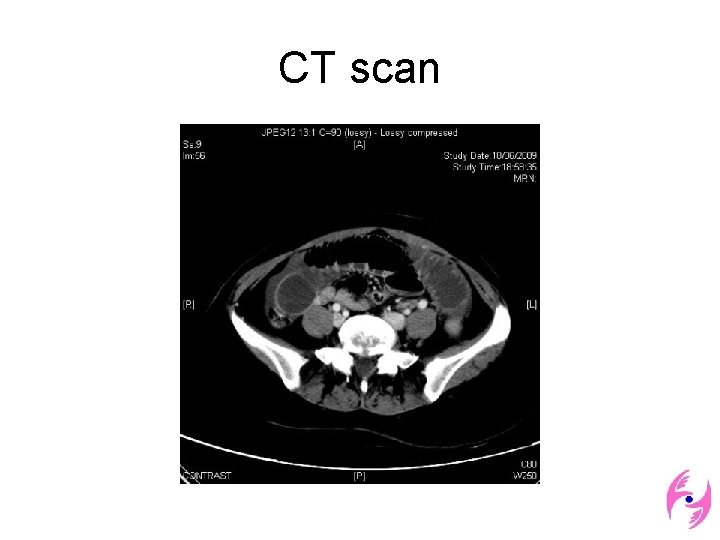
M/68 • Hx: CA splenic flexure, L hemicolectomy good recovery • readmitted Day 13 post-op for abdominal distension and pain
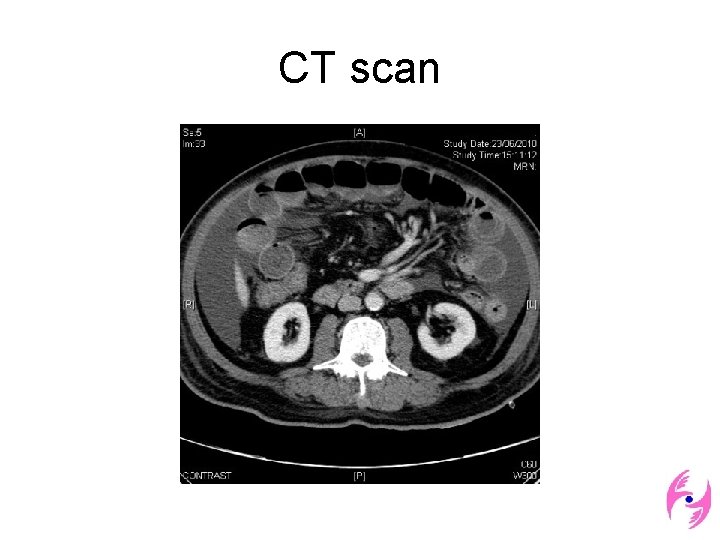
CT scan
Management • depends on stability of patient • history is important • know that it occurs, prevent it from happening • blood tests and imaging are adjunct only
Management • prompt surgical intervention: assessment of bowel viability, reduction and closure of all internal hernia defects • hernial ring should not be incised liberally • reduction of the hernia may be accomplished by enterostomy, followed by closure of the ring
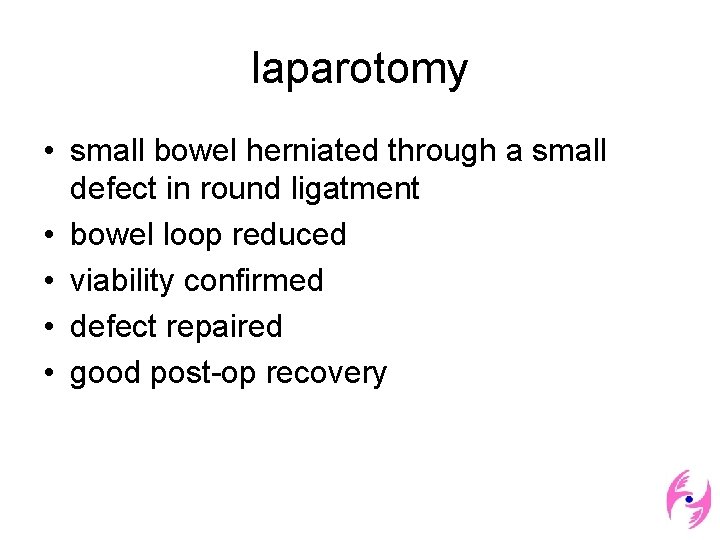
F/44 • acute LUQ pain with vomiting BO daily no UTI, gyn symptoms • afebrile vitals stable abdomen - LUQ tenderness, no mass
• CXR - no free gas AXR - no dilated bowel • Hb: 8. 2, L/RFT: normal
CT scan
laparotomy • small bowel herniated through a small defect in round ligatment • bowel loop reduced • viability confirmed • defect repaired • good post-op recovery
M/67 • RIIH with mesh repair done • generalized severe abdominal pain for 1 day • fever with tachycardia, BP stable tenderness & guarding at right side of abdomen • ANC: 17 Hb, R/LFT, amylase: normal CXR: no free gas
Emergency laparotomy • herniation of a segment of terminal ileum into a defect in mesosigmoid with gangrenous changes • limited right hemicolectomy done • post-op ICU care and smooth recovery
TMH data July 07’ to July 11’ • • 17 internal hernia diagnosed and operated female to male: 4(23. 5%) to 13(76. 5%) age: 22 to 83, mean: 58. 3 previous surgery: 70. 6%
Types of internal hernia • transmesenteric type: 10 (58. 8%) hernia neck was congenital fibrous band: 3 (17. 6%) paraduodenal: 1 (5. 88%) intersigmoid: 1 (5. 88%) round ligament: 1 (5. 88%) retroanastomotic: 1 (5. 88%)
Clinical features • non-specific • X-ray may not show I/O • all end up in surgery
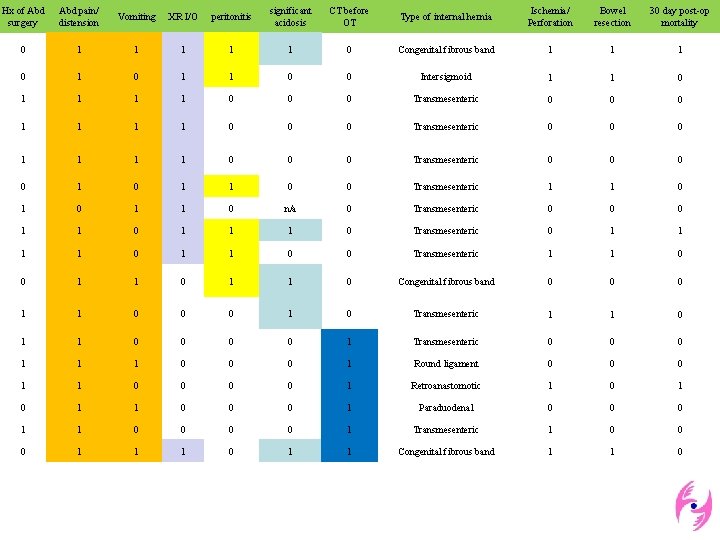
Hx of Abd surgery Abd pain/ distension Vomiting XR I/O peritonitis significant acidosis CT before OT Type of internal hernia Ischemia/ Perforation Bowel resection 30 day post-op mortality 0 1 1 1 0 Congenital fibrous band 1 1 1 0 0 Intersigmoid 1 1 0 1 1 1 1 0 0 0 Transmesenteric 0 0 0 1 1 0 0 0 Transmesenteric 0 0 1 0 1 1 0 0 Transmesenteric 1 1 0 n/a 0 Transmesenteric 0 0 0 1 1 1 0 Transmesenteric 0 1 1 0 0 Transmesenteric 1 1 0 0 1 1 0 Congenital fibrous band 0 0 0 1 1 0 0 0 1 0 Transmesenteric 1 1 0 0 0 0 1 Transmesenteric 0 0 0 1 1 1 0 0 0 1 Round ligament 0 0 0 1 1 0 0 1 Retroanastomotic 1 0 1 1 0 0 0 1 Paraduodenal 0 0 0 1 1 0 0 1 Transmesenteric 1 0 0 0 1 1 1 0 1 1 Congenital fibrous band 1 1 0
• pre-op CT: 6/17 (33. 3%) • • • comparing CT group to non-CT group: 0% vs 63. 6% peritonitis 17% vs 36% significant acidosis (p=0. 58%)(*) 16. 7% vs 54. 5% bowel resection (P=0. 22)(*) 16. 7% vs 18. 2% mortality (P=0. 49)(*) *Fisher’s Exact Test
Lesson to learn • know it occurs • CT might be valuable if the patient is not in distress clinically, having no clues from baseline Ix and might be expected to operate on +ve imaging results • laparoscopic repair possible (1) B Palmar, R Palmar. Laparoscopic management of left paraduodenal hernia. J Minimal Access Surgery: 2010; 6: 122 -24
Thank You Special thanks to Dr C C Cheung for inspiration and guidance & Dr K K Li for data framework
- Slides: 29