Integumentary System RESPONSE TO ALTERED INTEGUMENTARY FUNCTION the





- Slides: 128

Integumentary System
RESPONSE TO ALTERED INTEGUMENTARY FUNCTION , the student will be able to: Unit Outcomes: Upon completion of this unit of study • Safe Effective Care Environment: • • • • 1. Identify factors that influence injury and disease prevention ( sun exposure, environmental toxins, etc. ). 2. Perform thorough dermatological assessment throughout the life span. Health Promotion and Maintenance: 3. Identify healthy behaviors by the client and family ( screening exams, limiting risk taking behaviors). Psychosocial Integrity: 4. Discuss psychosocial impact of client’s altered dermatological condition ( acne, burns, rashes, tumors). Physiologic Integrity: 5. Discuss nursing implications for medications prescribed for clients with dermatologic disorders. 6. Develop plan of care for client with impaired skin integrity. 7. Explain the eight parameters of assessing a lesion. 8. Describe common lesions and rashes utilizing proper terminology. 9. Describe pre-op and post care of clients receiving dermatological surgical procedures. 10. Select nursing diagnoses most likely to be utilized with clients with integumentary problems. 11. Discuss etiology, clinical manifestations, and interventions for viral, bacterial, fungal, and parasitic skin disorders.

Introduction: Skin in our Culture • Defining ‘beauty’ • Language • Costs
Functions: • Protective Barrier • • – Injury – Microbial Invasion – Fluid & Electrolyte Balance – Temperature control Excretion Sensation Vitamin D Identity
Topics: • Assessment • Safety and preventive measures • Nursing Implications for Pharmacologic • • • Management Nursing Implications for Nonpharmacologic Management Nursing Implications for Surgical Management Nursing Management of Clients with Alterations - Integument
KP’s • Assessment • A. Parameters of General Skin Assessment • B. Lesions • C. Cultural/Ethnic variations • D. Diagnostic Testing
Thorough History • Dx & Tx – realm of practice – Difficult due to similarities in lesions and sx • Differential dx requires clues
Assessment: Subjective Data – Past Medical History • Trauma • Surgery • Prior skin disease • Jaundice • Delayed wound healing • Allergies • Sun exposure • Radiation treatments
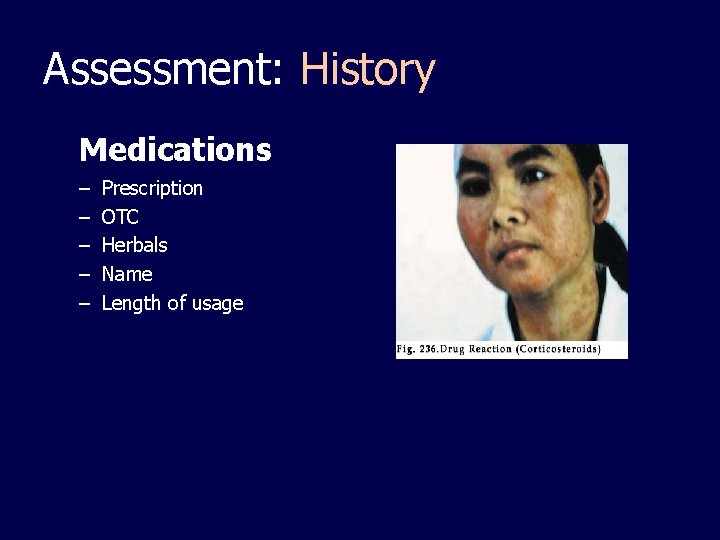
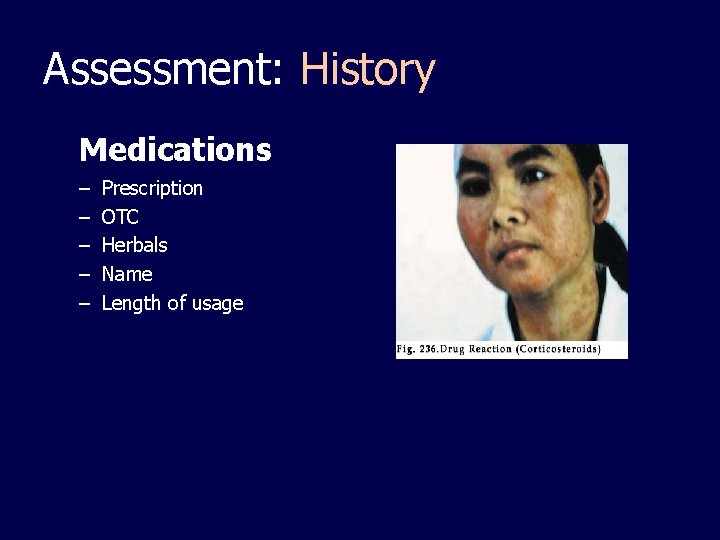
Assessment: History Medications – – – Prescription OTC Herbals Name Length of usage
Assessment: History • Surgery – Cosmetic – Biopsy • Diet • Health Practices – – – Hygiene, products Sunscreen, SPF Complementary & alternative medicine • C/O symptoms • Known exposure to • carcinogens, chemical irritants, allergens Family – Alopecia (bald) – Psoriasis – Skin cancer
Assessment: History • Changes – Skin condition – Hair condition – Nail condition – Mucous membranes
Assessment • Privacy • Carefully describe: – – – Obvious changes in color and vascularity Presence or absence of moisture Edema Skin Lesions Skin integrity • Document properly
Parameters of General Skin Assessment • color, temperature, moisture, elasticity, turgor, texture, and odor.
Assessment: Inspection • Consider Cultural and Ethnic variations – Dark skin • rates - skin cancer • Difficult to assess flushing; cyanosis; jaundice • Rashes difficult to observe • Pseudofolliculitis • Keloids • Mongolian spots
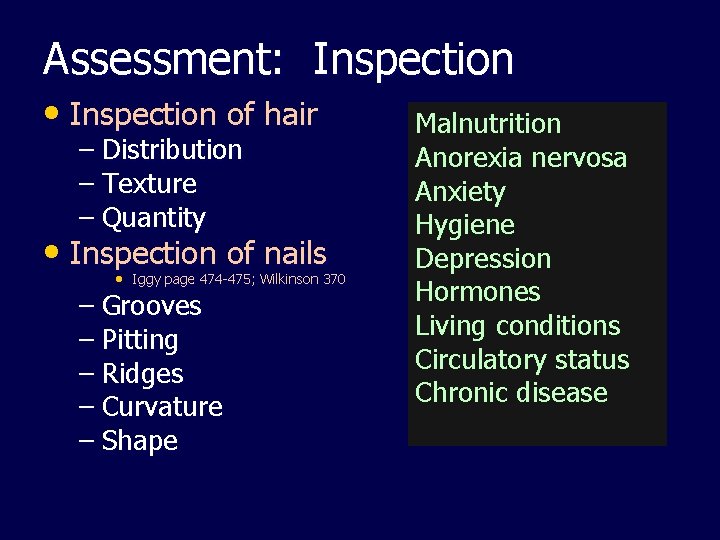
Assessment: Inspection • Inspection of hair – Distribution – Texture – Quantity • Inspection of nails • Iggy page 474 -475; Wilkinson 370 – Grooves – Pitting – Ridges – Curvature – Shape Malnutrition Anorexia nervosa Anxiety Hygiene Depression Hormones Living conditions Circulatory status Chronic disease
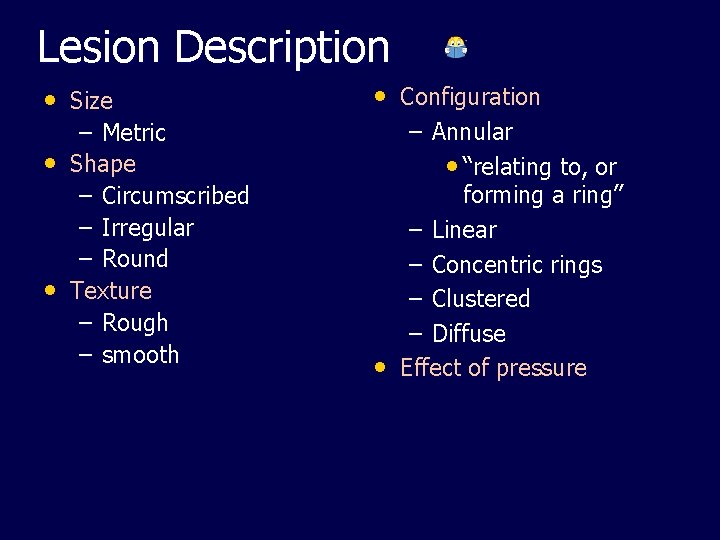
Lesion Description • Size – Metric • Shape – Circumscribed – Irregular – Round • Texture – Rough – smooth • Configuration – Annular • “relating to, or forming a ring” – Linear – Concentric rings – Clustered – Diffuse • Effect of pressure
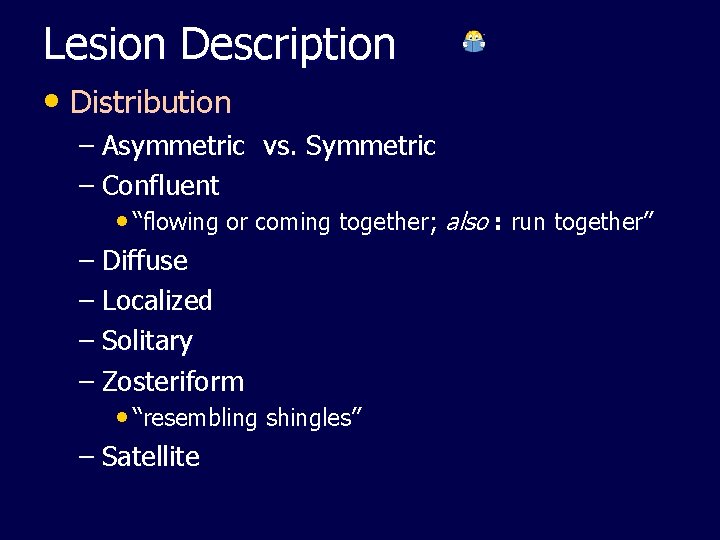
Lesion Description • Distribution – Asymmetric vs. Symmetric – Confluent • “flowing or coming together; also : run together” – Diffuse – Localized – Solitary – Zosteriform • “resembling shingles” – Satellite
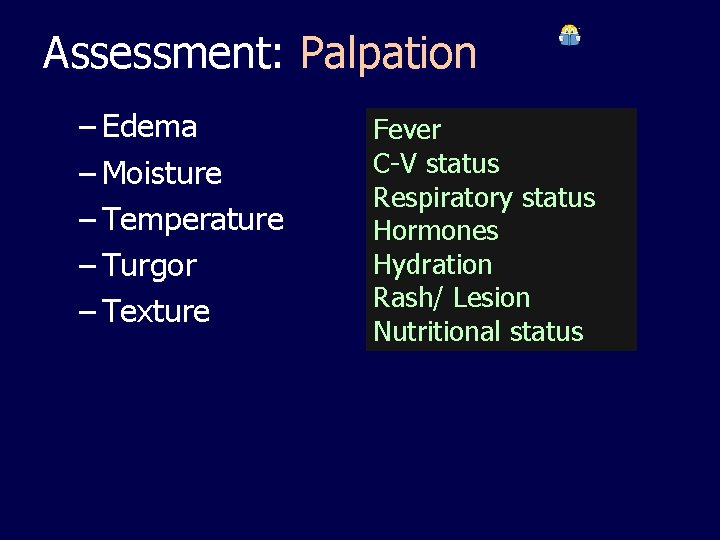
Assessment: Palpation – Edema – Moisture – Temperature – Turgor – Texture Fever C-V status Respiratory status Hormones Hydration Rash/ Lesion Nutritional status
Skin cancer - most common cancer! • Risk factors – – – – – Fair skin Blue/green eyes Blond/red hair History chronic sun exposure Family history Living near the equator Very high/low altitudes Working outdoors Age > 60 (damage is cumulative)
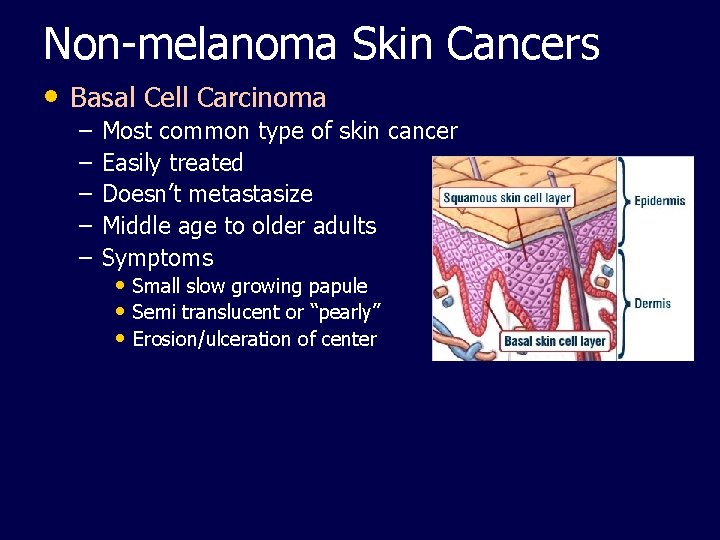
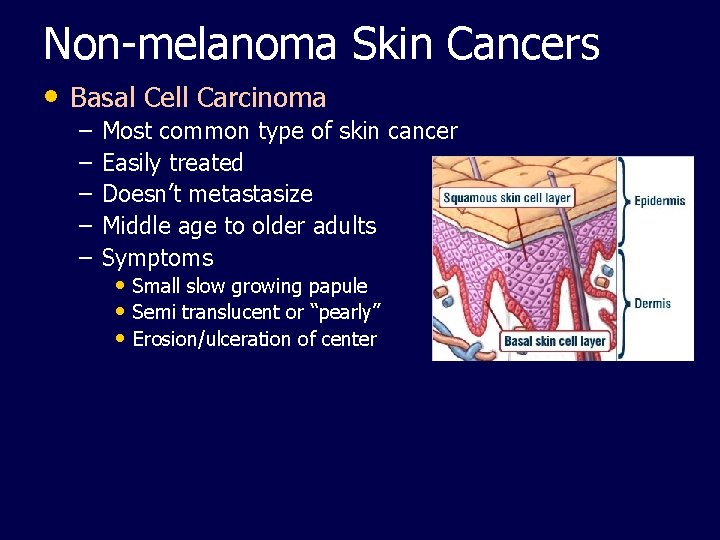
Non-melanoma Skin Cancers • Basal Cell Carcinoma – – – Most common type of skin cancer Easily treated Doesn’t metastasize Middle age to older adults Symptoms • Small slow growing papule • Semi translucent or “pearly” • Erosion/ulceration of center
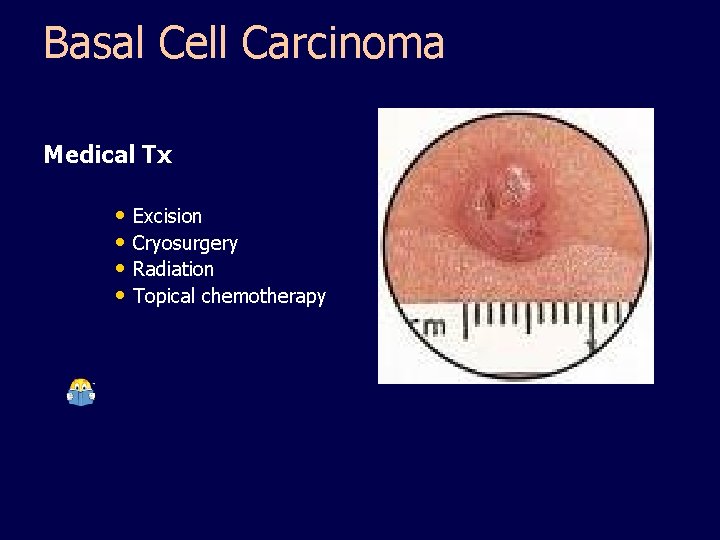
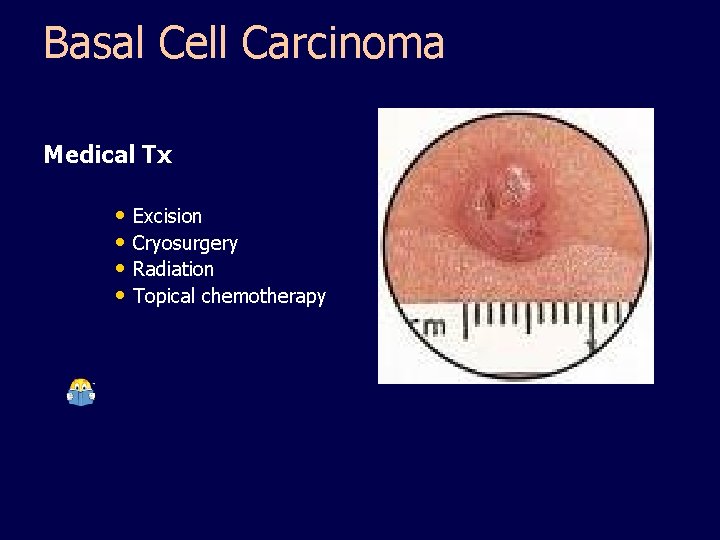
Basal Cell Carcinoma Medical Tx • Excision • Cryosurgery • Radiation • Topical chemotherapy
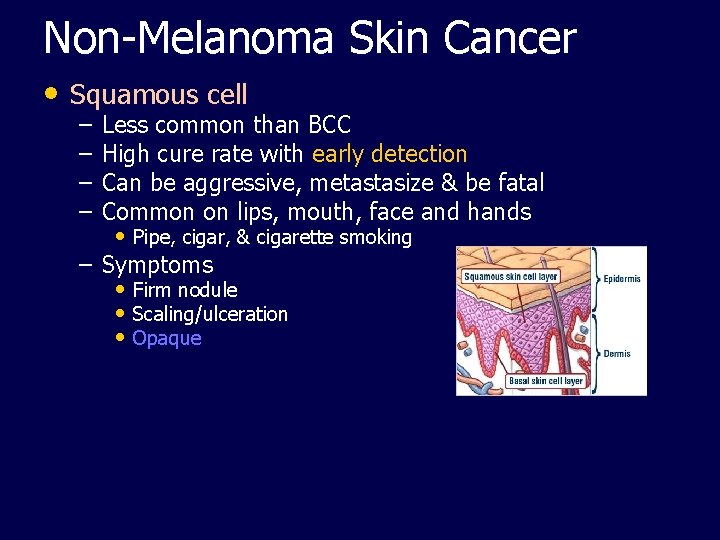
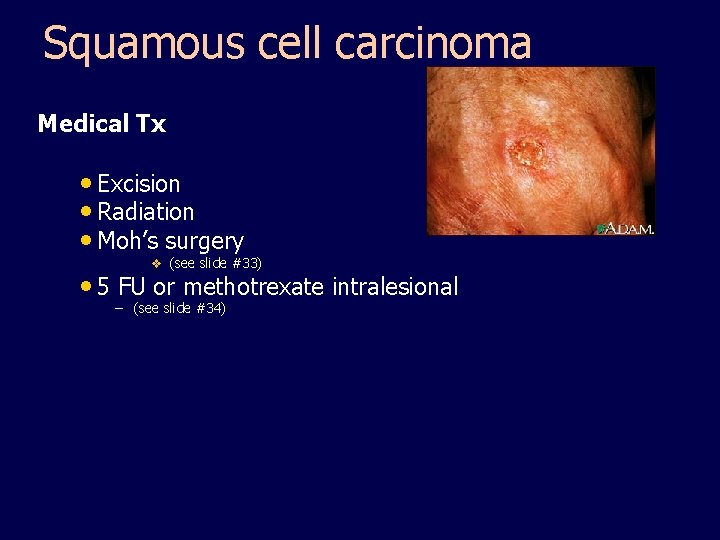
Non-Melanoma Skin Cancer • Squamous cell – – Less common than BCC High cure rate with early detection Can be aggressive, metastasize & be fatal Common on lips, mouth, face and hands • Pipe, cigar, & cigarette smoking – Symptoms • Firm nodule • Scaling/ulceration • Opaque
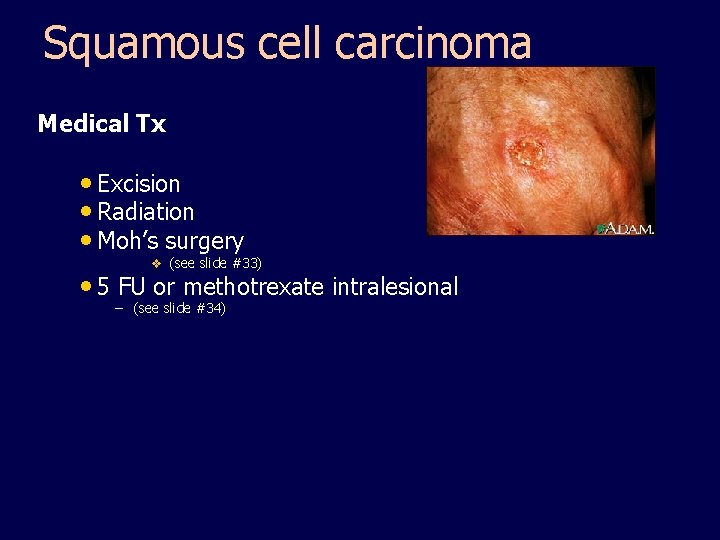
Squamous cell carcinoma Medical Tx • Excision • Radiation • Moh’s surgery v (see slide #33) • 5 FU or methotrexate intralesional – (see slide #34)
Diagnostic & Surgical Therapy • Simple Excision • Excision – Moh’s micrographic surgery • Microscopically controlled removal of lesion • Removes tissue in thin layers • Can see all margins of specimen • Preserves normal tissue • Produces smallest wound
Drug Therapy: Topical Fluorouracil (5 -FU) – Selective toxicity for sun damaged cells (cytotoxic) – Indications • Premalignant skin disease (esp. actinic keratosis) • Systemic absorption minimal It causes painful eroded area within 4 days and must use 1 -2 times daily 2 -4 weeks. Healing up to 3 weeks after med stopped Is photosensitizing - avoid sunlight during treatment Will look worse before it gets better
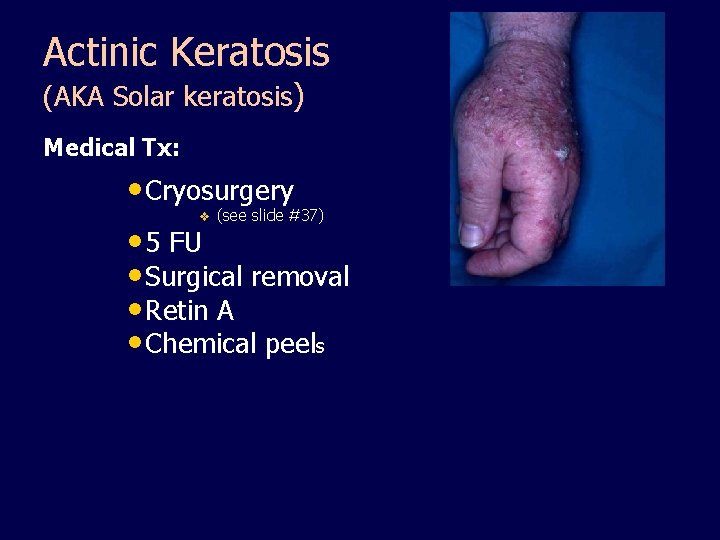
Non-Melanoma Skin Cancers • Actinic Keratosis (AKA Solar keratosis) – Most common precancerous lesion – Premalignant form of squamous cell carcinoma – Symptoms • Hyperkeratotoc papules/plaques on sun exposed areas • Varied appearance – – Irregular shape Flat Indistinct borders Overlying scale
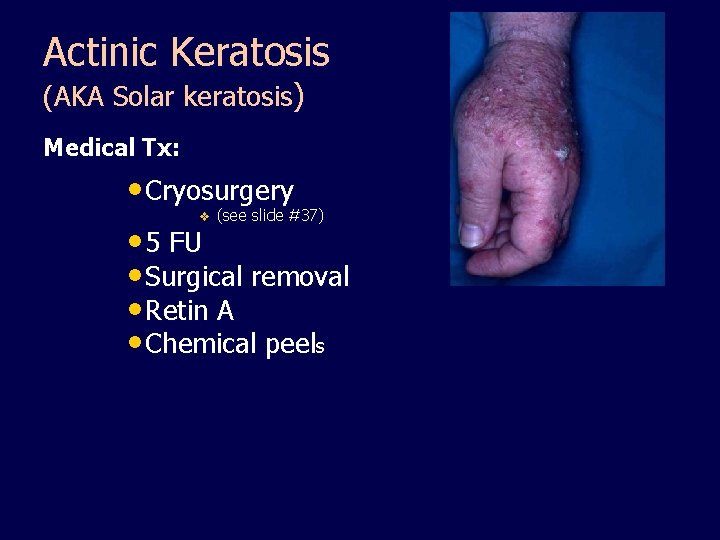
Actinic Keratosis (AKA Solar keratosis) Medical Tx: • Cryosurgery v (see slide #37) • 5 FU • Surgical removal • Retin A • Chemical peels
Cryosurgery – Subfreezing temps for surgery (liquid nitrogen) • Lesion becomes red & swollen, blisters, then scabs; falls off in 1 -3 weeks • Minimal scarring – Indications • Genital warts • Seborrheic keratosis • Actinic keratosis
Malignant Melanoma • 1/3 of all melanoma occur in existing nevi or moles – Any sudden or progressive change in size, color or shape of a mole should be checked
Malignant Melanoma • Can metastasize anywhere • Most deadly of skin cancers • Causes – – – UV radiation Skin sensitivity Genetic Hormonal Sun exposure Mutation of gene (B-RAF) 70%
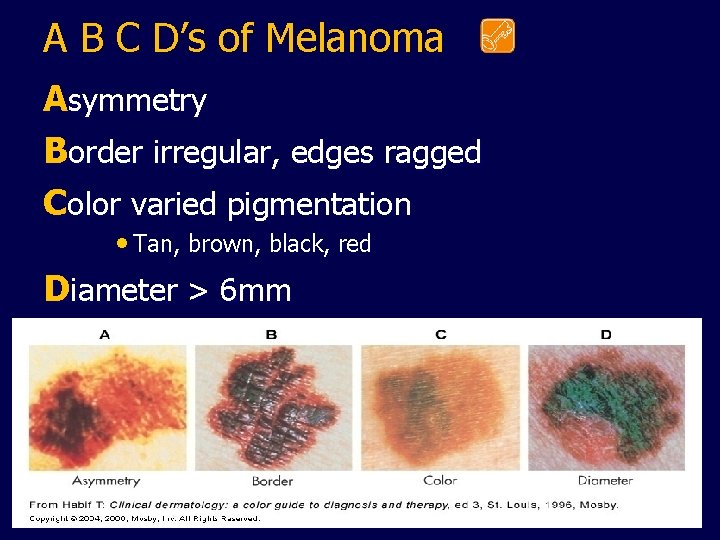
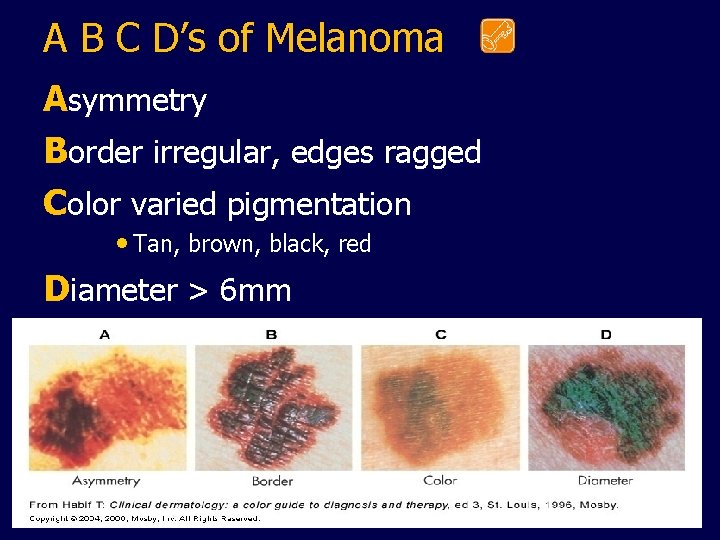
A B C D’s of Melanoma Asymmetry Border irregular, edges ragged Color varied pigmentation • Tan, brown, black, red Diameter > 6 mm
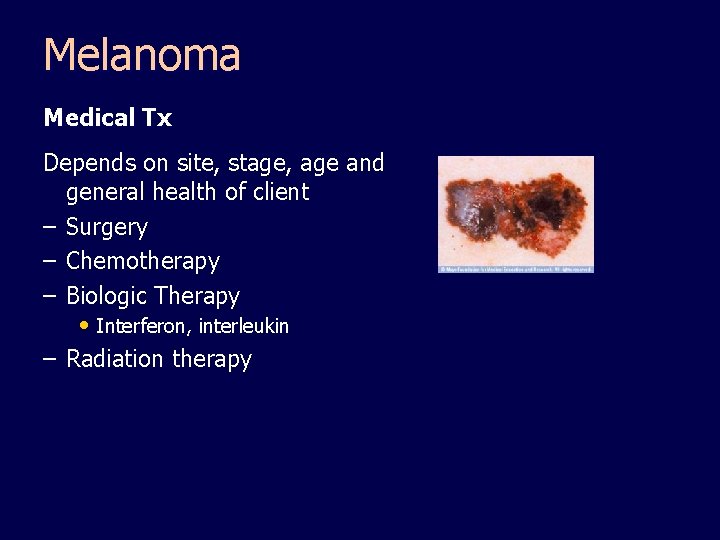
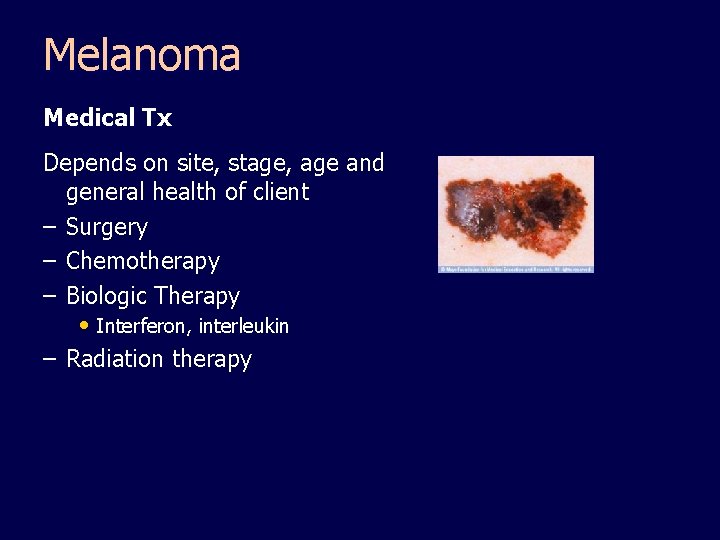
Melanoma Medical Tx Depends on site, stage, age and general health of client – Surgery – Chemotherapy – Biologic Therapy • Interferon, interleukin – Radiation therapy
Prevention/Education • Sunscreen • Limit exposure • Hat/clothes/sunglasses • Shade • Inspect skin regularly
Sunburn: Education (Protect, Protect) • Same precautions as for skin cancer. • Don’t let clouds or cool air fool you – Florida sun is damaging then too. • Get out of the sun before you turn red! • Cool skin off. Immediately! • Hydrate!
Sunburn • Superficial burn • Excessive exposure to ultraviolet rays injures dermis. • Dilated capillaries = red, tender, edema, blisters • Large area = nausea, fever
Sunburn • Redness & pain begin within a few Hours. • Intensity may increase before subsiding. • 3 -5 days to heal • Tx: cool bath; soothing lotions; topical corticosteroids; fluids
Insects/Pests/Parasites • Spiders • Fire Ants • Lice/Scabies • Mosquitoes • Scorpions • “Sand fleas”
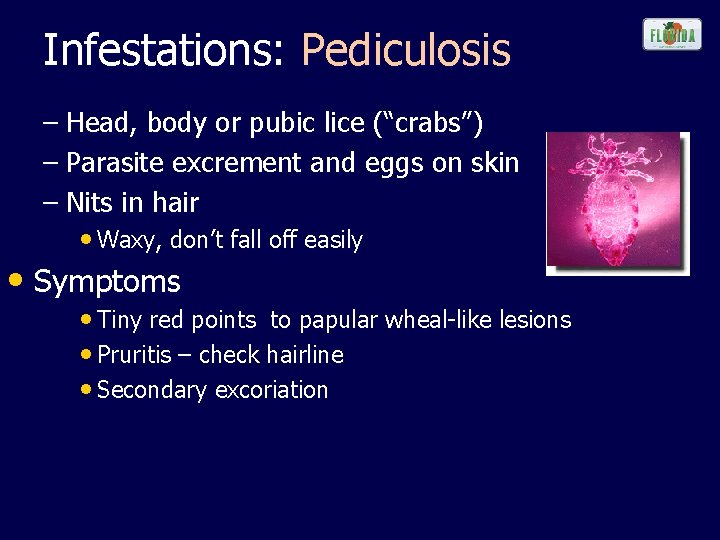
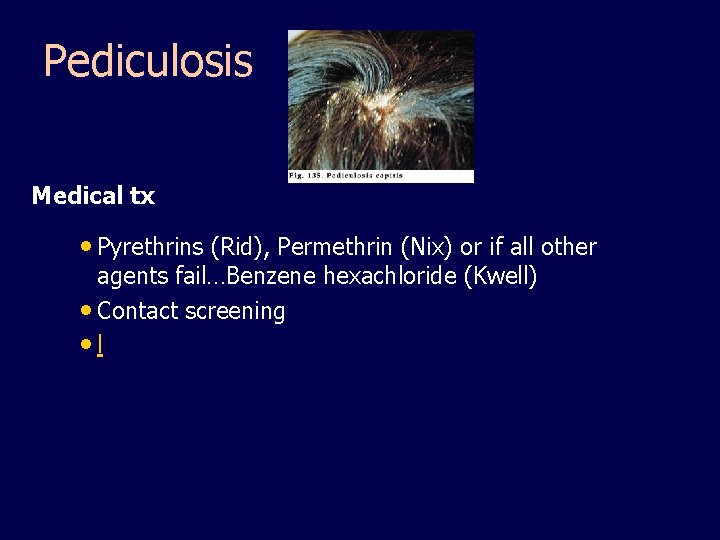
Infestations: Pediculosis – Head, body or pubic lice (“crabs”) – Parasite excrement and eggs on skin – Nits in hair • Waxy, don’t fall off easily • Symptoms • Tiny red points to papular wheal-like lesions • Pruritis – check hairline • Secondary excoriation
Pediculosis Medical tx • Pyrethrins (Rid), Permethrin (Nix) or if all other agents fail…Benzene hexachloride (Kwell) • Contact screening • l
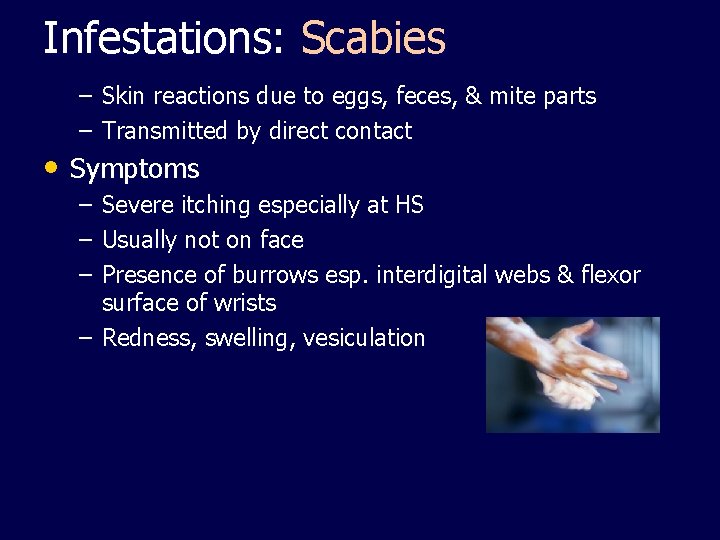
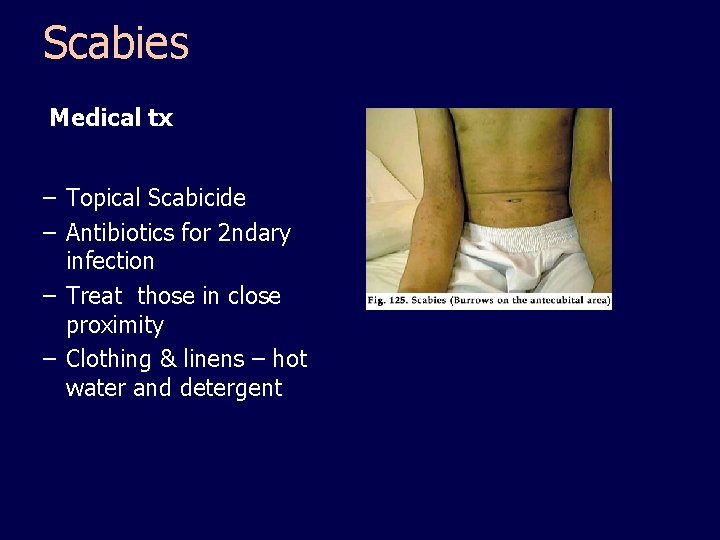
Infestations: Scabies – Skin reactions due to eggs, feces, & mite parts – Transmitted by direct contact • Symptoms – Severe itching especially at HS – Usually not on face – Presence of burrows esp. interdigital webs & flexor surface of wrists – Redness, swelling, vesiculation
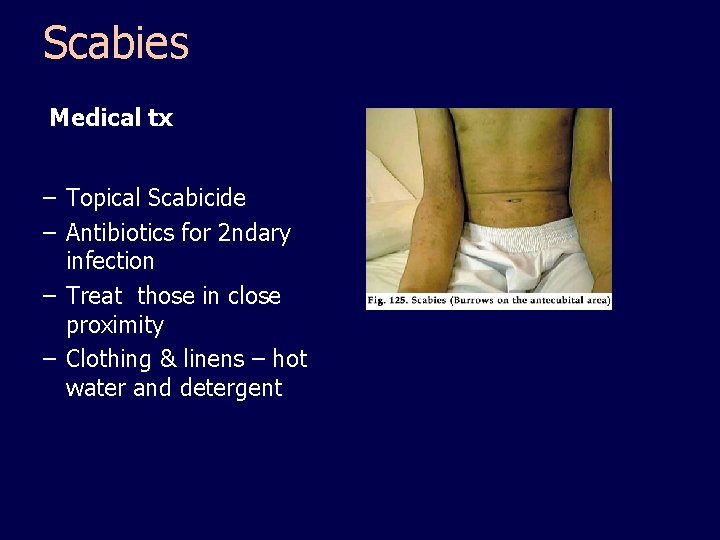
Scabies Medical tx – Topical Scabicide – Antibiotics for 2 ndary infection – Treat those in close proximity – Clothing & linens – hot water and detergent
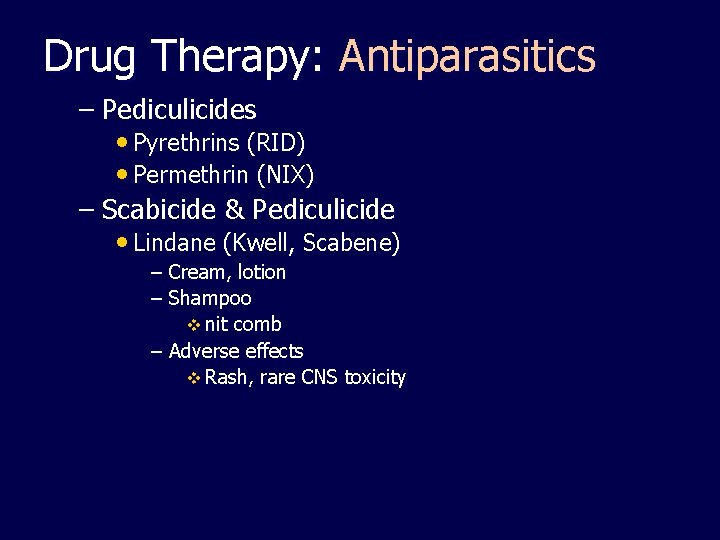
Drug Therapy: Antiparasitics – Pediculicides • Pyrethrins (RID) • Permethrin (NIX) – Scabicide & Pediculicide • Lindane (Kwell, Scabene) – Cream, lotion – Shampoo v nit comb – Adverse effects v Rash, rare CNS toxicity
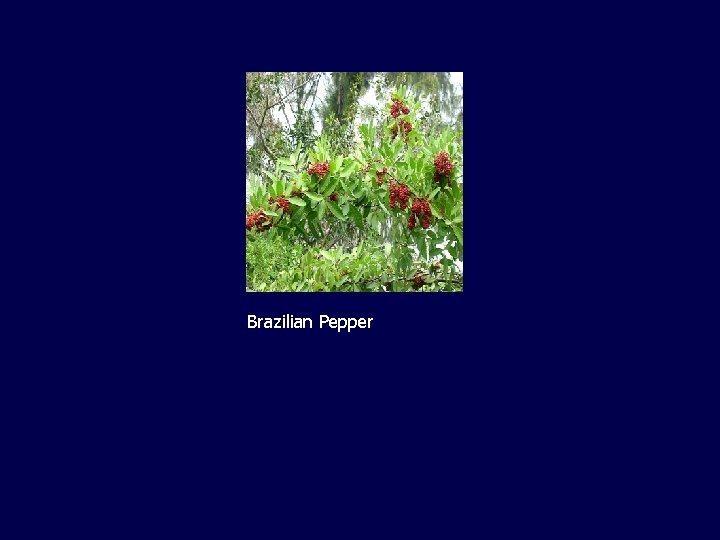
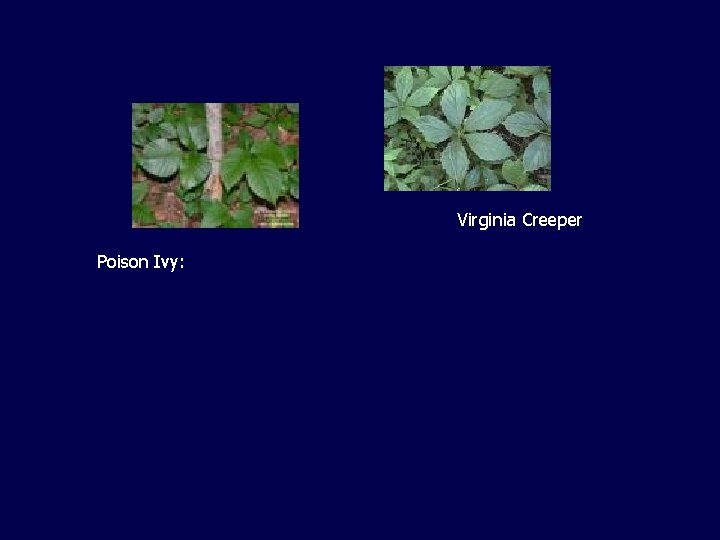
Plants in FL that irritate skin • Poinsettia, Croton • Milky sap can cause skin irritation • Oleander – Touching the plant is not dangerous, but prolonged contact can irritate the skin. • Poison Ivy , Brazilian Pepper – Touching the leaves or oil from the plant can cause an itchy rash with blisters.
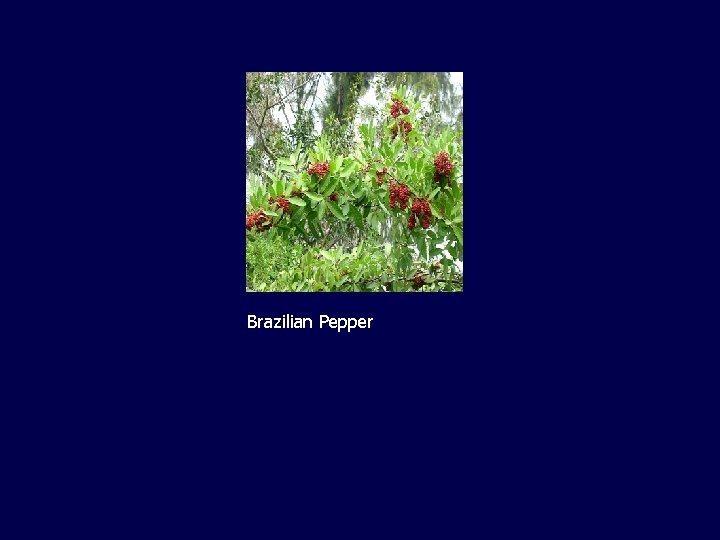
Brazilian Pepper
Virginia Creeper Poison Ivy:
Drug Therapy • Topical Corticosteroids – Anti-inflammatory, antipruritic • Low potency (hydrocortisone) – Slower acting – Can be used longer without serious side effects – Ointment most efficient – Higher potency, long term, systemic use is different tx
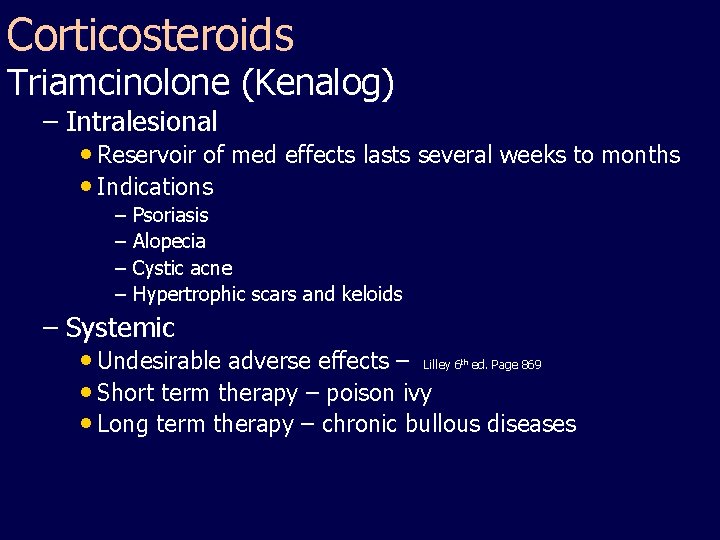
Corticosteroids Triamcinolone (Kenalog) – Intralesional • Reservoir of med effects lasts several weeks to months • Indications – Psoriasis – Alopecia – Cystic acne – Hypertrophic scars and keloids – Systemic • Undesirable adverse effects – Lilley 6 ed. Page 869 • Short term therapy – poison ivy • Long term therapy – chronic bullous diseases th
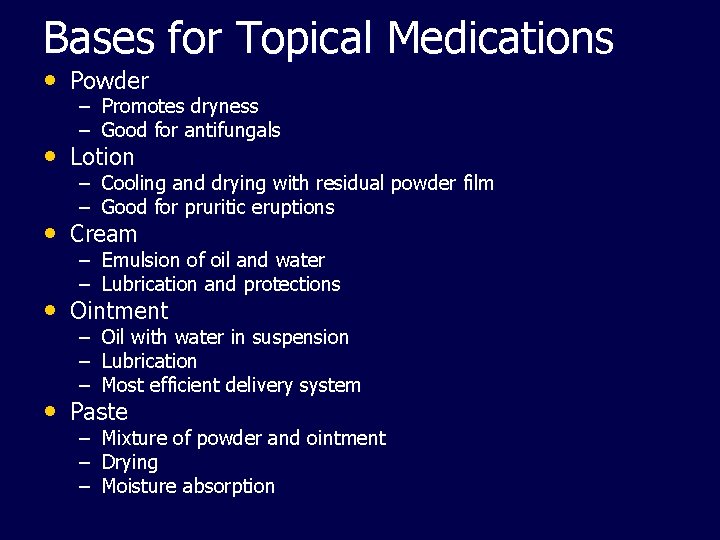
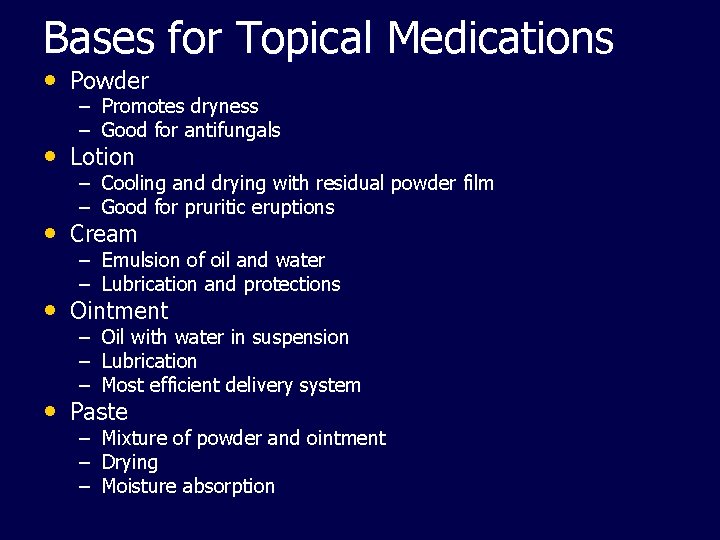
Bases for Topical Medications • Powder – Promotes dryness – Good for antifungals • Lotion – Cooling and drying with residual powder film – Good for pruritic eruptions • Cream – Emulsion of oil and water – Lubrication and protections • Ointment – – – Oil with water in suspension Lubrication Most efficient delivery system • Paste – Mixture of powder and ointment – Drying – Moisture absorption
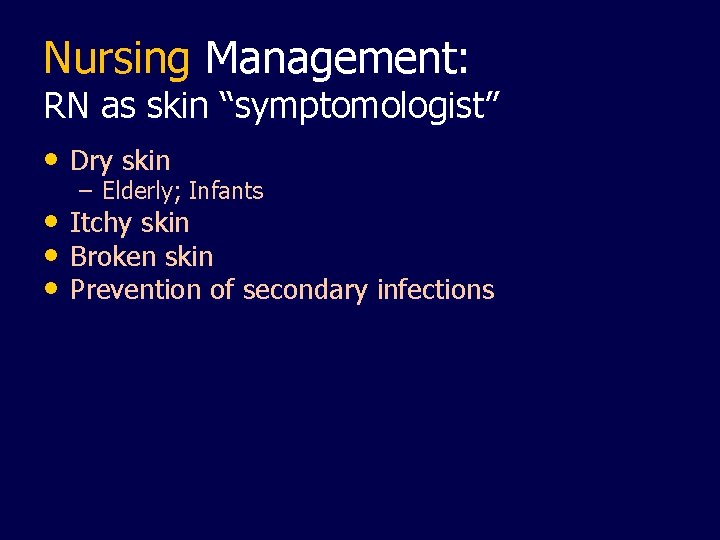
Nursing Management: RN as skin “symptomologist” • Dry skin – Elderly; Infants • Itchy skin • Broken skin • Prevention of secondary infections
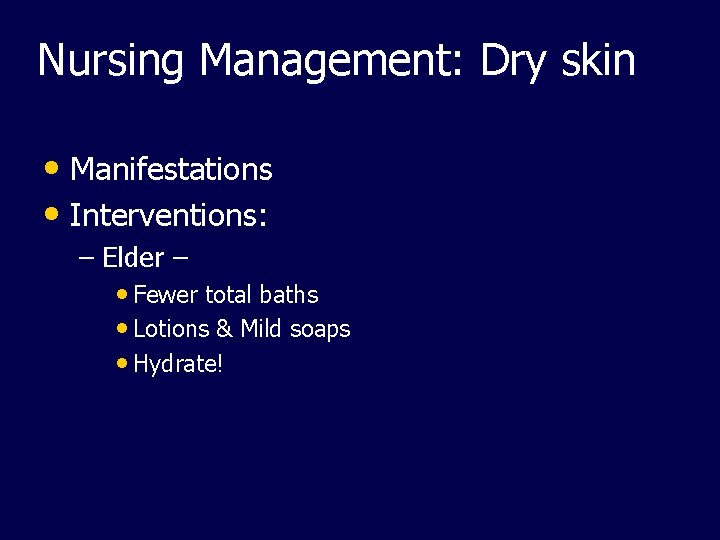
Nursing Management: Dry skin • Manifestations • Interventions: – Elder – • Fewer total baths • Lotions & Mild soaps • Hydrate!
Nursing Management: Itchy skin • Control of pruritis – – – – Keep cool No rubbing Moisturize Systemic antihistamines Wet dressing Topical steroids Menthol, Camphor, Phenol numb itch receptors Oatmeal baths
Nursing Management: itch • Baths – – – – For large body areas Has sedating and antipruritic effect Oilated oatmeal (Aveeno), potassium permangenate, sodium bicarb Temp comfortable to client Soak 15 -20 mins 3 -4 times daily Pat dry, no rubbing apply moisturizers or meds after baths
Nursing Management • Wet dressings – Indications • Skin weepy from infection/inflammation • Relieves itching • Debrides wound • Increases penetration of topical meds • Relieves discomfort • Enhances removal of scabs, crusts, and exudate
Wet dressings Procedure • Clean solution and gauze • Squeeze until not dripping • Apply to affected area, avoid normal tissue • Leave in place 10 -30 minutes 2 -4 times a day • Discontinue if skin macerates (“to soften”)
Nursing Management: Protect • Protect intact skin! – Turn at least q 2 h – Reposition frequently – Alleviate pressure – Hydration – Mechanical intervention – Rx
Nursing Management: Psychological support • Chronic skin conditions – – – Emotional stress Self concept alterations Body image changes
Nursing Interventions: Psychological support: – – – Support client Allow verbalizations of frustrations Reinforce treatment Support groups Help with camouflage
Diagnostic Testing Biopsy – – Punch Incisional Excisional Shave RN Responsibilities – – – Informed Consent Prep site Assist with procedure Apply dressing Post-op instructions Properly ID specimen
Diagnostic Testing • Cultures – Diagnose fungal, bacteria, viral infections – KOH (Potassium Hydroxide) • Fungus • Sample collection – Skin scraping – Swabbing – Meticulous labeling
Diagnostic Testing • Woods Light – Organisms fluoresce • Pseudomonas • Fungus • Vitiligo • Mineral oil slides – Infestations • Patch test – Allergen testing
Dermatological Interventions • Phototherapy – UVA & UVB (UVL) – Ultraviolet wavelengths cause erythema, desquamation, and pigmentation – Enhance with psoralem (photosensitizing) • Treatment for • Psoriasis • Atopic dermatitis • Vitiligo
Phototherapy • Adverse effects – – Basal or squamous cell Ca Burns Erythema Teach patients to avoid further sun exposure & photosensitizing drugs – Wear eye protections as psoralem absorbed by lens of eye
Dermatological Interventions • Radiation Therapy – Indications • Cutaneous malignancies – Advantages • Produces minimal damage to surrounding tissues – Adverse effects • Permanent hair loss (alopecia) to irradiated areas • Telangiectasia • Atrophy • Hyperpigmentation / depigmentation • Ulceration • BCC and SCC y.
Dermatological Interventions • Laser Therapy (CO 2, Argon) – Cuts, coagulates, & vaporizes tissue – No cumulative tissue damage • Indications – Coagulation of vascular lesions – Skin resurfacing – Removal birthmarks – BCC – Keloids – Plantar warts
Diagnostic & Surgical Therapy • Skin Scraping – Scalpel – Surface cells for microscopic inspection • Electrodesication & electrocoagulation – Electrical energy converted to heat – Destroys tissue by burning • Coagulates bleeding vessels • Curettage – Remove tissue with circular cutting edge – Small skin tumors • warts, seborrheic keratosis, BCC, SCC
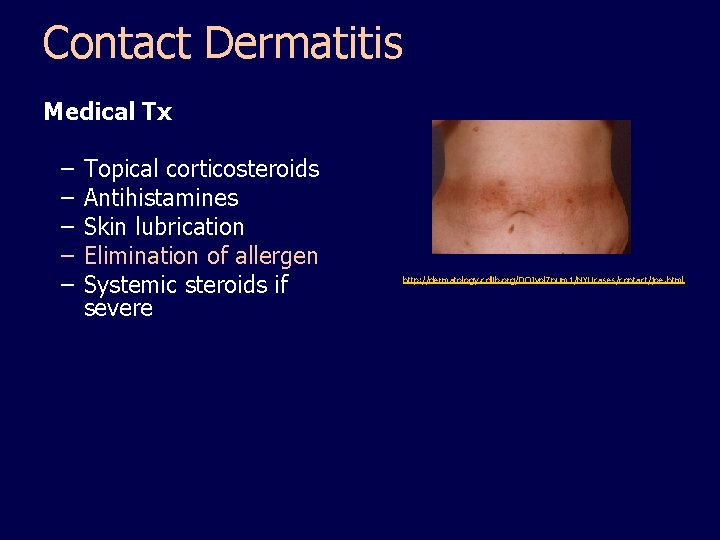
Allergic Conditions • Contact Dermatitis – Delayed hypersensitivity – Lesions 2 -7 days after antigen exposure • Manifestations – – Red, hive-like papules and plaques Sharply circumscribed Vesicles Pruritic
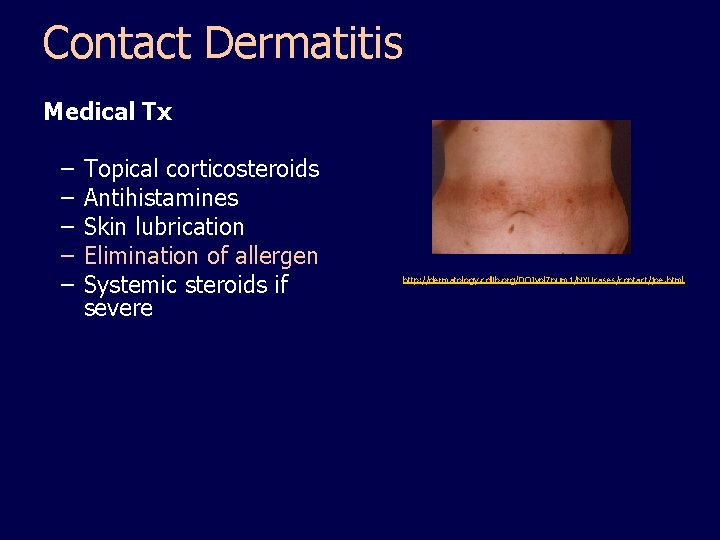
Contact Dermatitis Medical Tx – – – Topical corticosteroids Antihistamines Skin lubrication Elimination of allergen Systemic steroids if severe http: //dermatology. cdlib. org/DOJvol 7 num 1/NYUcases/contact/joe. html
Drug Therapy: Antihistamines • Compete with histamine receptor site – Oral or Topical • Cetitizine (Zyrtec) – PO tabs, syrup QD – Non-sedating • Diphenahydramine (Benadryl) – PO, IM, topical • Indications – – – Urticaria Pruritis Allergic reactions
Drug Therapy: Antihistamines • Adverse effects – – – Anticholinergic Sedation (Benadryl) Use with caution in older adults • Indications – Urticaria – Pruritis – Allergic reactions • Adverse effects – Anticholinergic – Sedation (Benadryl) – Use with caution in older adults
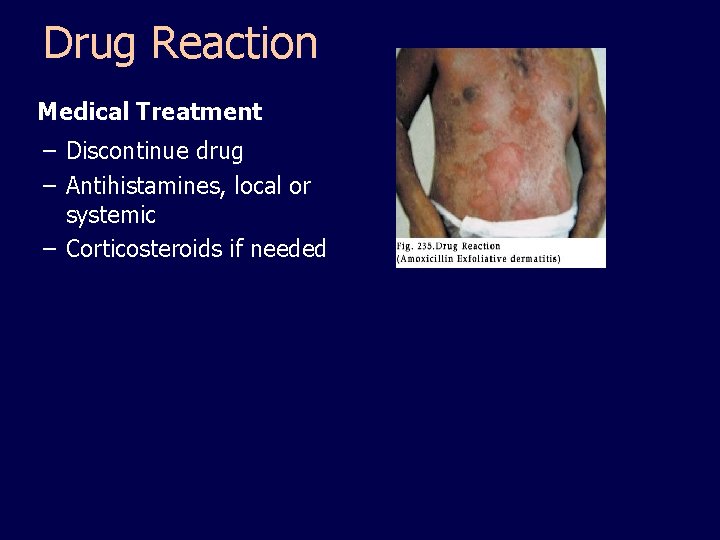
Allergic Conditions: Drug Reaction • Manifestations – – – Rash of any morphology Red, macular, papular Generalized rash with sudden onset Pruritic Can occur as late as 14 days after drug is stopped
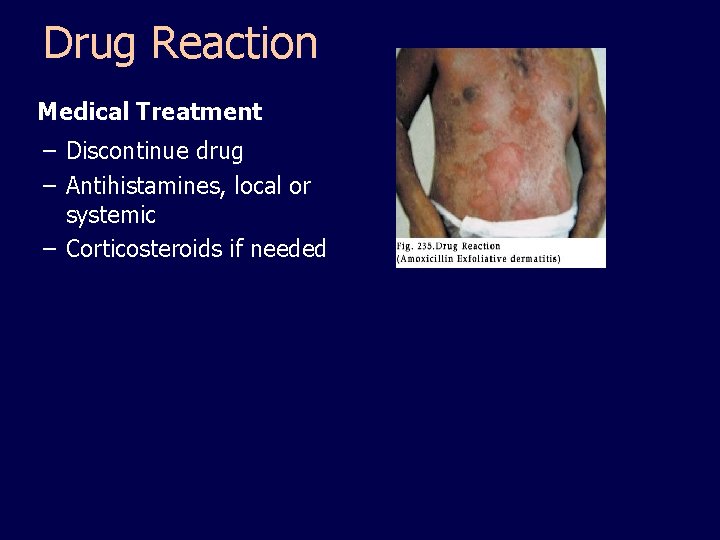
Drug Reaction Medical Treatment – Discontinue drug – Antihistamines, local or systemic – Corticosteroids if needed
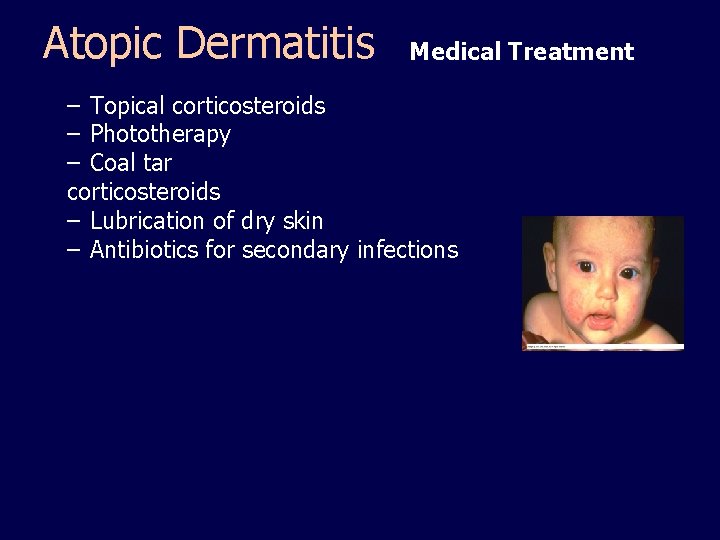
Allergic Conditions: Atopic Dermatitis – Cause unknown – Begins in infancy and declines with age • Manifestations – Scaly, red to re-brown, circumscribed lesions – Pruritic – Symmetric eruptions
Atopic Dermatitis Medical Treatment – Topical corticosteroids – Phototherapy – Coal tar corticosteroids – Lubrication of dry skin – Antibiotics for secondary infections
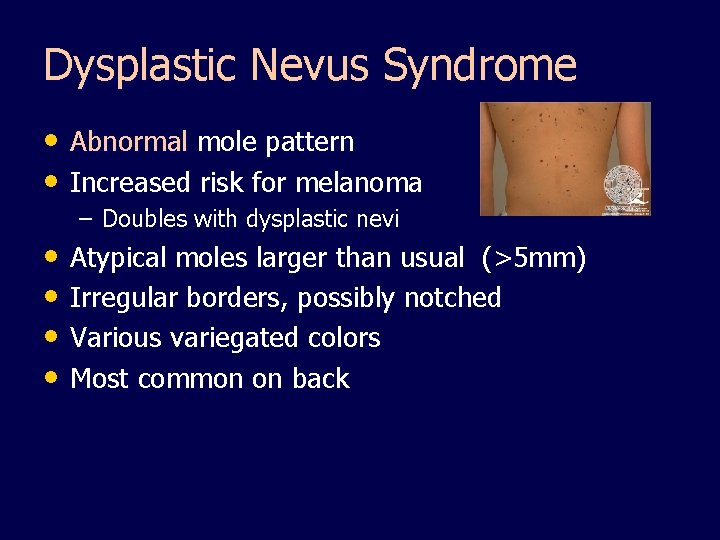
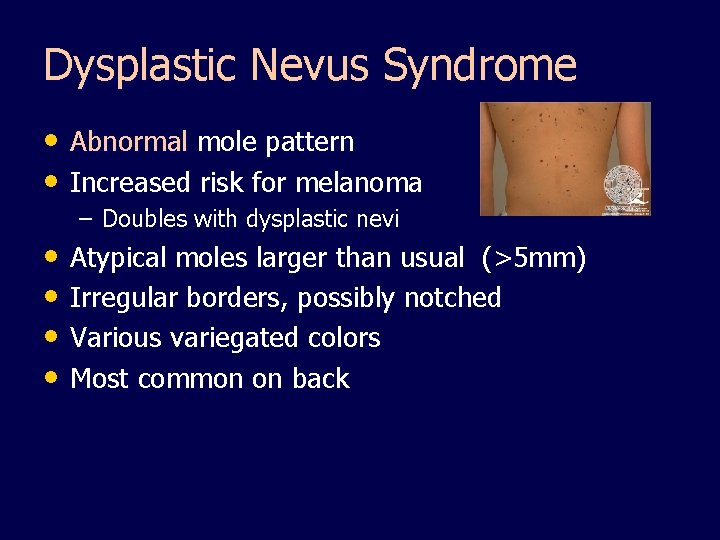
Dysplastic Nevus Syndrome • Abnormal mole pattern • Increased risk for melanoma – Doubles with dysplastic nevi • Atypical moles larger than usual (>5 mm) • Irregular borders, possibly notched • Various variegated colors • Most common on back
Infections of the skin • Risk factors – Imbalance between host and microorganism – Broken or damaged skin; Trauma – Systemic disease such as Diabetes – Moisture – Obesity – Systemic corticosteroids, antibiotics • Prevention – Proper hygiene – Good health
Infections: Herpes Simplex Virus, Type I (AKA “cold sores/fever blisters”) • Contagious • Dormant – Exacerbation • Triggers • Symptoms -- 1 st episode 3 -7 days after exposure – Painful local reaction – Vesicles on erythematous base – Fever, malaise
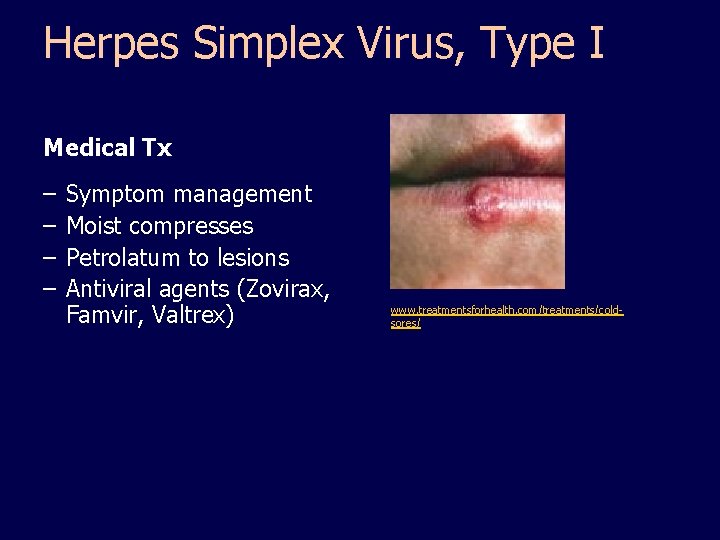
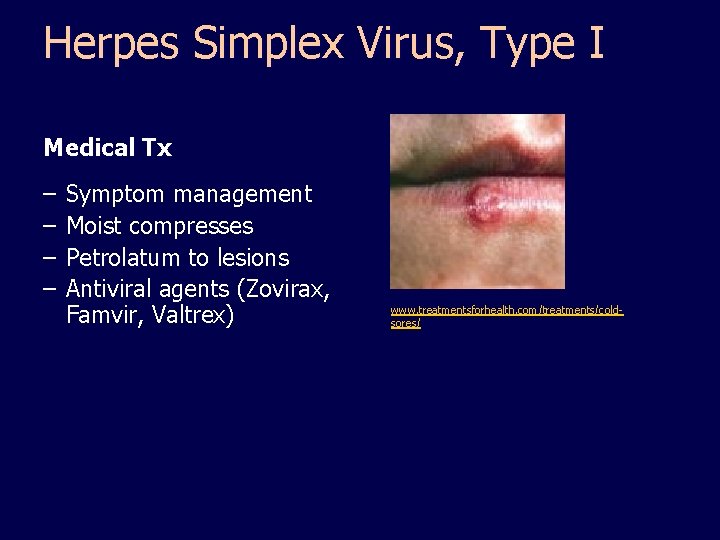
Herpes Simplex Virus, Type I Medical Tx – – Symptom management Moist compresses Petrolatum to lesions Petrolatum Antiviral agents (Zovirax, Famvir, Valtrex) www. treatmentsforhealth. com/treatments/coldsores/
Infections: Herpes Simplex Virus, Type II – Genital Iggy page 1742 -1743 “Most genital herpes is caused by HSV-2. ” (n. l. m. -n. i. h. / Medline plus) – Recurrence more common than oral • Does not mean re-infection • Symptoms – Same as Type I • Treatment – Same as Type I
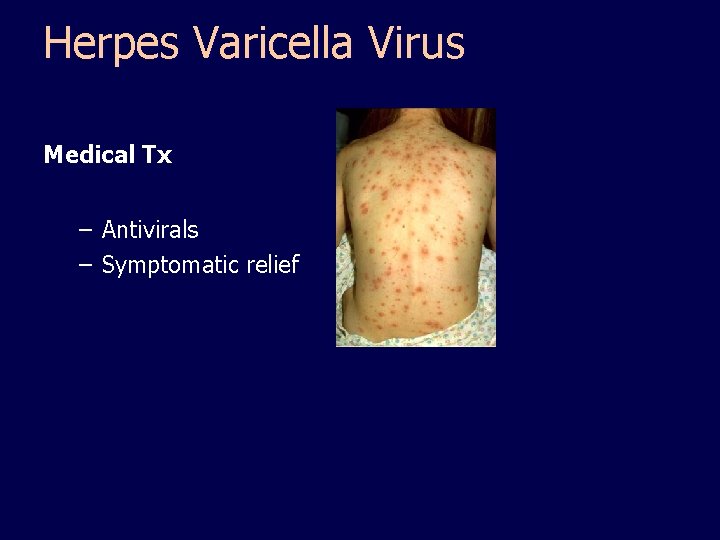
Infections: Herpes Varicella Virus (chicken pox) ** Highly contagious • No chicken pox or vaccination • Keep those w/active lesions separated until crusted • Symptoms – Vesicular lesions in successive crops • Face , scalp, spreading to trunk and extremities Protect eyes v Do not squeeze pustules or crusts v • Vesicles > pustules > crusts > scars • Postherpetic neuralgia • Self limiting in children
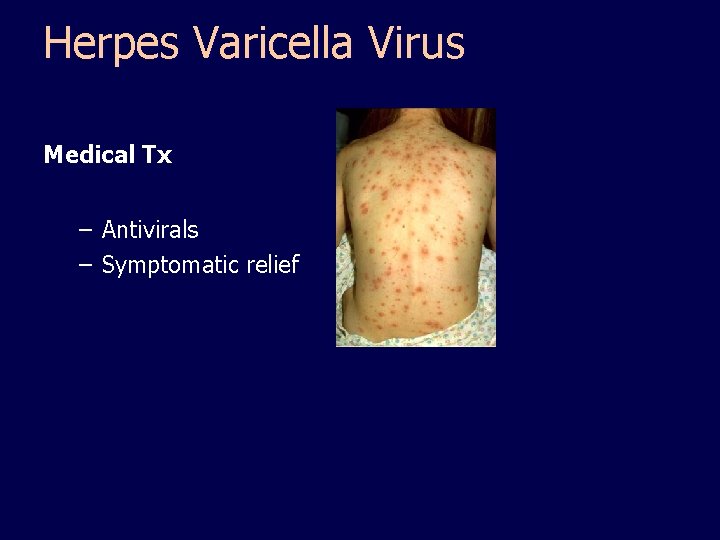
Herpes Varicella Virus Medical Tx – Antivirals – Symptomatic relief
Infections: Herpes Zoster (shingles) – – – Activation of varicella zoster virus Frequent occurrence in immunocompromised Potentially contagious to immunocompromised • Symptoms – – Linear patches along dermatome Grouped vesicles on erythematous base Unilateral on trunk Burning pain and neuralgia
Herpes Zoster Medical Tx – Symptomatic • Wet compresses • White petrolatum to lesions – Antiviral agents
Drug Therapy: Antivirals – Acyclovir (Zovirax) • Suppresses chicken pox, herpes simplex 1 & 2, shingles • Po, IV, topical – Valacyclovir (Valtrex) • Herpes zoster (shingles) & genital herpes – Vaccines • Varivax – Prevention of chicken pox – Given to children > 12 mo. • Zostivax – HZU vaccine for adults > 60 y/o
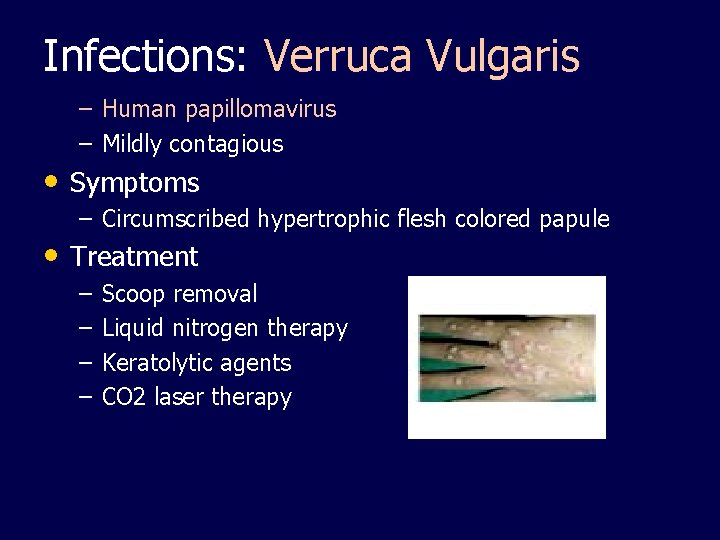
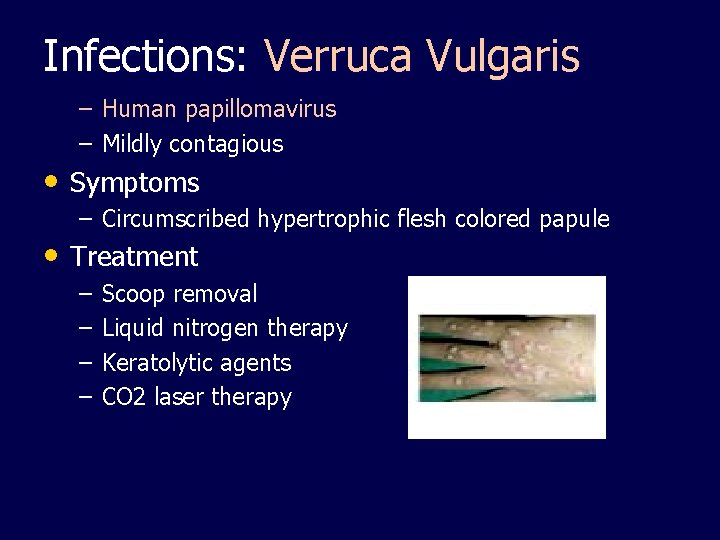
Infections: Verruca Vulgaris – Human papillomavirus – Mildly contagious • Symptoms – Circumscribed hypertrophic flesh colored papule • Treatment – – Scoop removal Liquid nitrogen therapy Keratolytic agents CO 2 laser therapy
Infections: Plantar Warts (Human papillomavirus) • Symptoms – Wart on “Plantar” surface (bottom) of foot – – Cone shaped with black dots (“seeds”)
Plantar Warts Medical Tx – – – Liquid nitrogen Frequent paring with chemical patches Duct tape? ? ?
Infections: Candidiasis (moniliasis) – Candida albicans (Fungus) – 50% are symptom free carriers – Immunocompromised >> pathogenic – Likes warm moist areas • Mouth, vagina, skin An opportunistic infection
Infections: Candidiasis – Symptoms • Mouth – White, cheesy plaque (milk curds) • Vagina – Vaginitis – Red edematous painful vaginal wall – White patches – Vaginal discharge – Pruritis – Painful urination & intercourse • Skin – Diffuse papular erythematous rash – Pinpoint satellite lesions around edges Physiologic Integrity: 5. Discuss nursing implications for medications prescribed for clients with dermatologic disorders. 6. Develop plan of care for client with impaired skin integrity.
Candidiasis Medical Tx: Anti-fungals • Nystatin – Vaginal suppository – Oral lozenge • Mycostatin powder, cream • Keep skin clean dry • Diagnosis culture Microscopic exam (KOH)
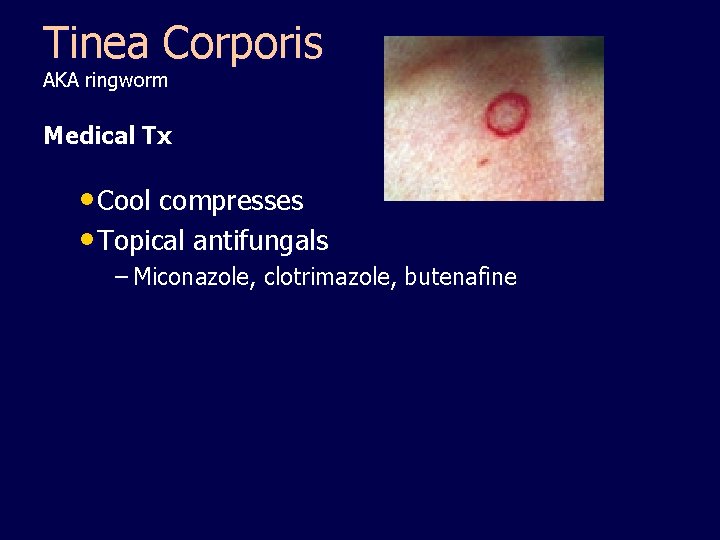
Infections: Fungal • Tinea Corporis – AKA ringworm – Symptoms • Annular • well defined margins • erythematous
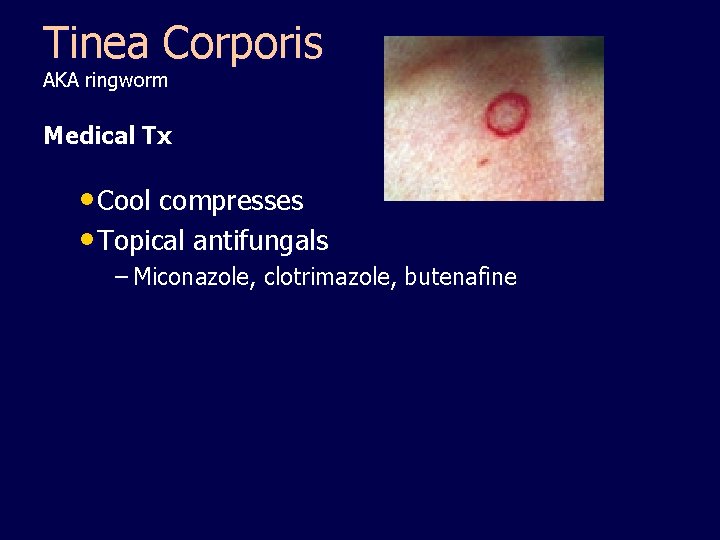
Tinea Corporis AKA ringworm Medical Tx • Cool compresses • Topical antifungals – Miconazole, clotrimazole, butenafine
Infections: Fungal • Tinea Cruris – AKA jock itch – Symptoms • Self-defined border • In groin – Treatment topical antifungal cream or solution
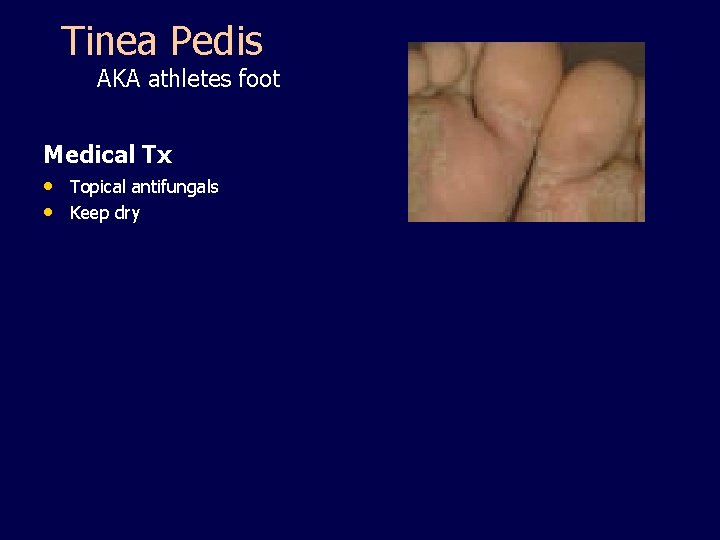
Infections: Fungal • Tinea Pedis – AKA athletes foot – Symptoms • Interdigital scaling • Erythema • Blistering • Pruritis • Pain
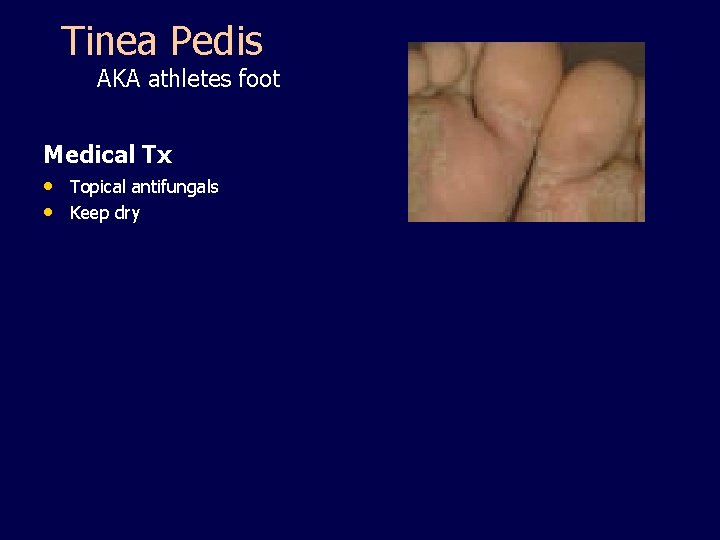
Tinea Pedis AKA athletes foot Medical Tx • Topical antifungals • Keep dry
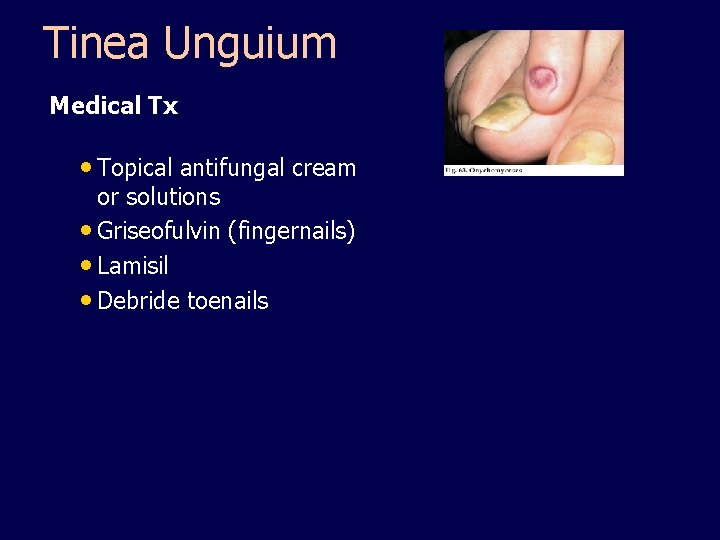
Infections: Fungal • Tinea Unguium – Symptoms • Brittle thickened nails • White/yellow discoloration
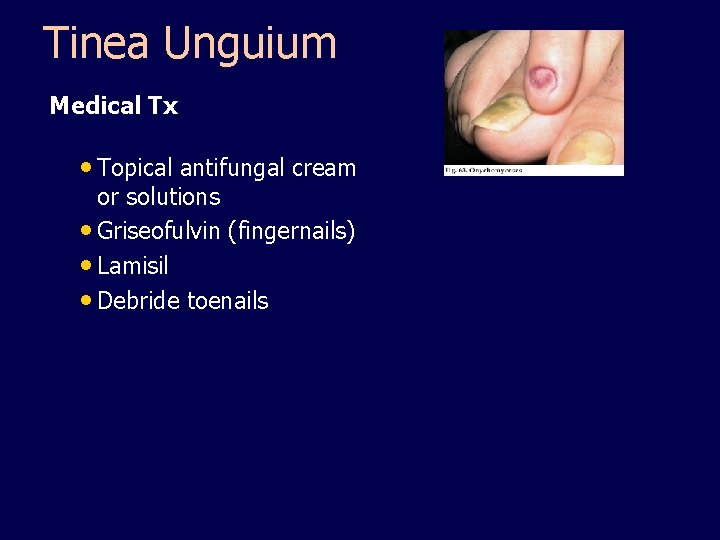
Tinea Unguium Medical Tx • Topical antifungal cream or solutions • Griseofulvin (fingernails) • Lamisil • Debride toenails

Drug Therapy: Antifungals – Clotrimazole (Mycelex, Lotrimin) • Lozenges- thrush • Cream, solution, lotion- athletes foot • Intravaginal creams, tablets – Miconazole (Monistat, Micotin) • Athletes foot • Jock itch • Ringworm • Yeast infections
Drug Therapy: Antifungals – Fluconazole (Diflucan) • PO & IV • Excellent bioavailability • Vaginal or systemic candidiasis – Ketaconazole (Nizoral) – Nystatin (Mycostatin) – Tervinafine (Lamisil) for onychomycosis – Tolnaftate (Tinactin)
Infections, Bacterial • Impetigo – Group A beta hemolytic strept or staph – Associated with poor hygiene and low socioeconomic status • Symptoms – – – Vesiculopustular lesions Thick honey colored crust Surrounded by erythema Pruritic Contagious – – – Systemic antibiotics Saline or aluminum acetate soaks Soap & water Removal of crusts Topical antibiotic cream • Treatment • Strept can cause glonerulonephritis if untreated
Infections: Bacterial • Cellulitis – – – Staph aureus or strept Can be primary or secondary infection Symptoms • Hot • Tender • Erythematous • Edematous • Diffuse borders maybe malaise and fever – Treatment • Moist heat • Immobilization • Elevation • Systemic antibiotics • Hospitalize if severe – Can progress to gangrene if untreated
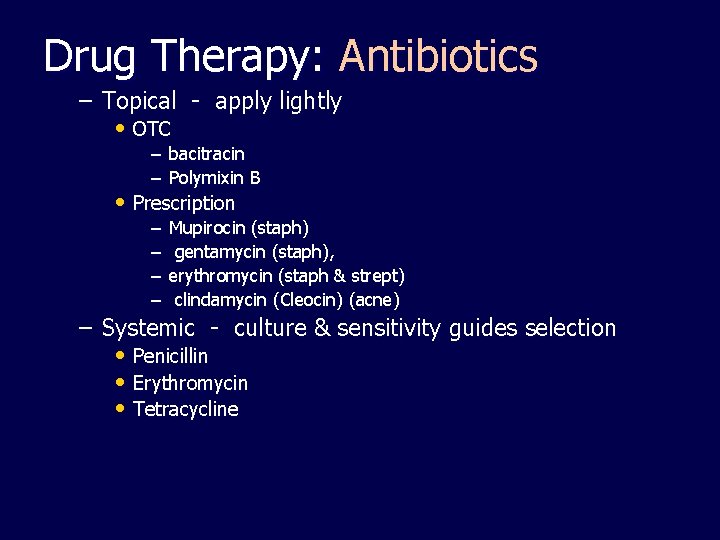
Drug Therapy: Antibiotics – Topical - apply lightly • OTC – bacitracin – Polymixin B • Prescription – – Mupirocin (staph) gentamycin (staph), erythromycin (staph & strept) clindamycin (Cleocin) (acne) – Systemic - culture & sensitivity guides selection • Penicillin • Erythromycin • Tetracycline
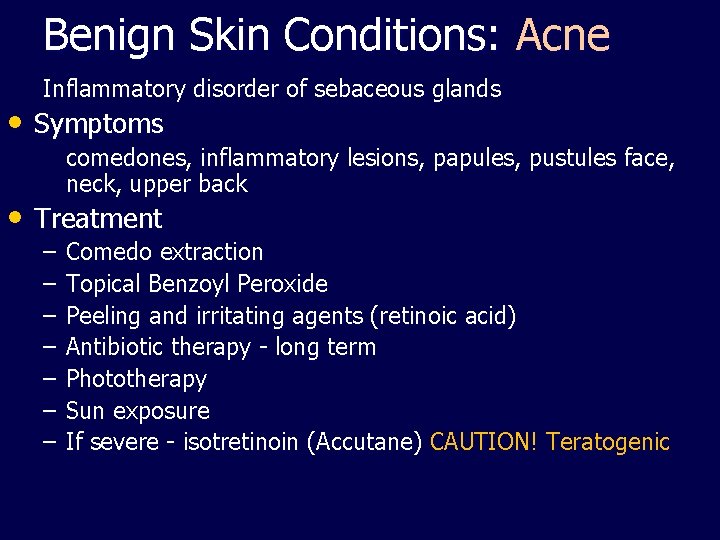
Benign Skin Conditions: Acne Inflammatory disorder of sebaceous glands • Symptoms comedones, inflammatory lesions, papules, pustules face, neck, upper back • Treatment – – – – Comedo extraction Topical Benzoyl Peroxide Peeling and irritating agents (retinoic acid) Antibiotic therapy - long term Phototherapy Sun exposure If severe - isotretinoin (Accutane) CAUTION! Teratogenic
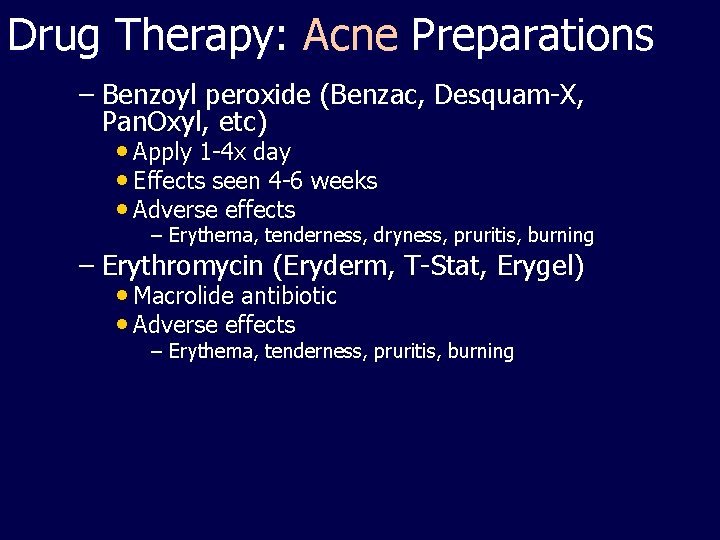
Drug Therapy: Acne Preparations – Benzoyl peroxide (Benzac, Desquam-X, Pan. Oxyl, etc) • Apply 1 -4 x day • Effects seen 4 -6 weeks • Adverse effects – Erythema, tenderness, dryness, pruritis, burning – Erythromycin (Eryderm, T-Stat, Erygel) • Macrolide antibiotic • Adverse effects – Erythema, tenderness, pruritis, burning
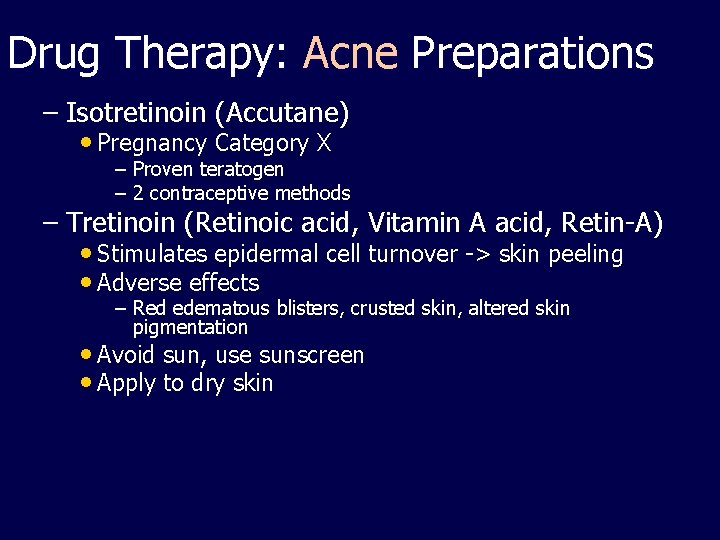
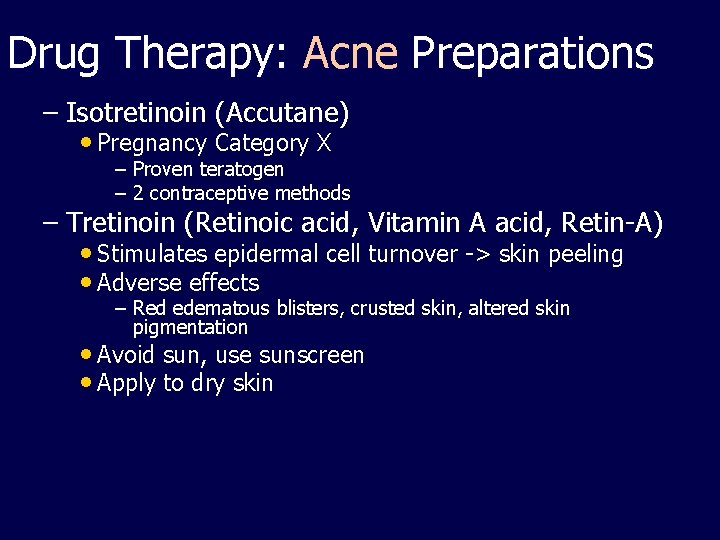
Drug Therapy: Acne Preparations – Isotretinoin (Accutane) • Pregnancy Category X – Proven teratogen – 2 contraceptive methods – Tretinoin (Retinoic acid, Vitamin A acid, Retin-A) • Stimulates epidermal cell turnover -> skin peeling • Adverse effects – Red edematous blisters, crusted skin, altered skin pigmentation • Avoid sun, use sunscreen • Apply to dry skin
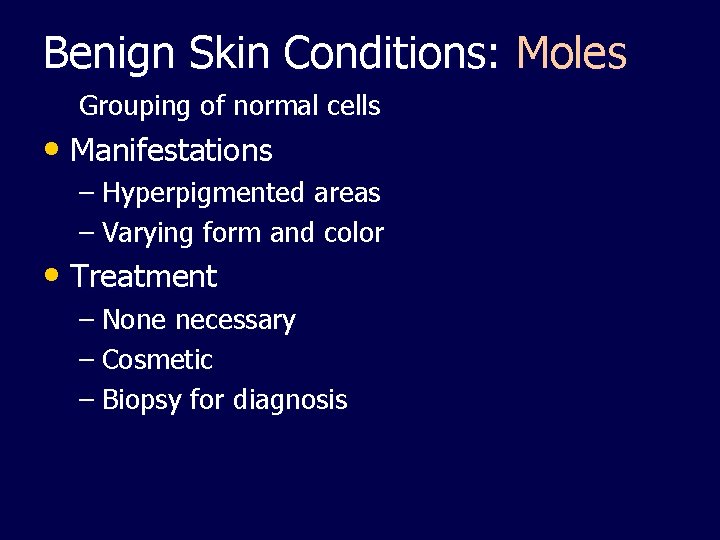
Benign Skin Conditions: Moles Grouping of normal cells • Manifestations – Hyperpigmented areas – Varying form and color • Treatment – None necessary – Cosmetic – Biopsy for diagnosis
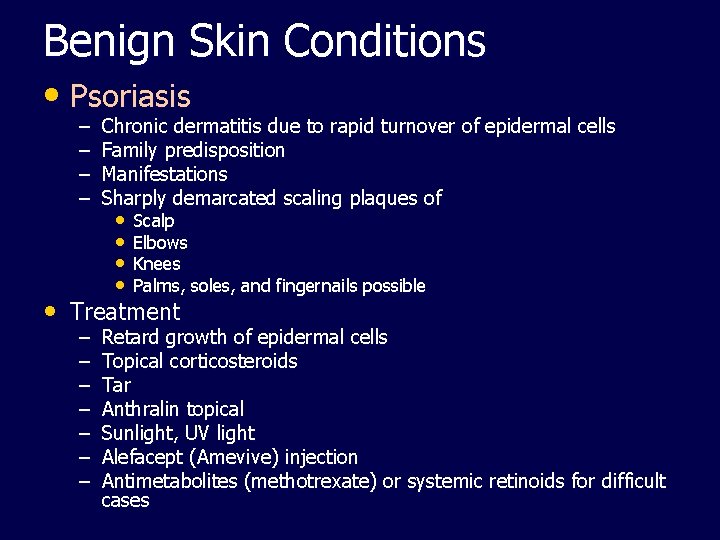
Benign Skin Conditions • Psoriasis – – Chronic dermatitis due to rapid turnover of epidermal cells Family predisposition Manifestations Sharply demarcated scaling plaques of • • Scalp Elbows Knees Palms, soles, and fingernails possible • Treatment – – – – Retard growth of epidermal cells Topical corticosteroids Tar Anthralin topical Sunlight, UV light Alefacept (Amevive) injection Antimetabolites (methotrexate) or systemic retinoids for difficult cases
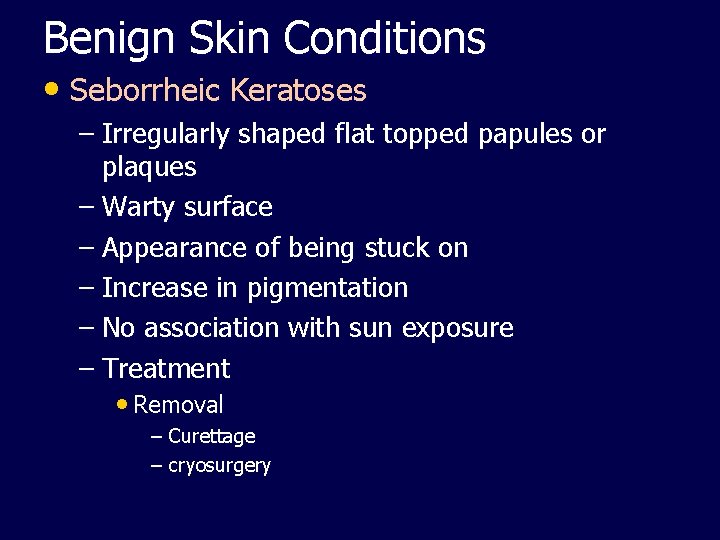
Benign Skin Conditions • Seborrheic Keratoses – Irregularly shaped flat topped papules or plaques – Warty surface – Appearance of being stuck on – Increase in pigmentation – No association with sun exposure – Treatment • Removal – Curettage – cryosurgery
Benign Skin Conditions: Lipoma Encapsulated tumor of adipose tissue Most common 40 -60 years of age • Manifestations – Rubbery, compressible, round mass – Variable in size – Most common on trunk, back of neck, forearms • Treatment – Biopsy – Excision if indicated
Benign Skin Conditions: Vitiligo – – Unknown cause Genetic connection Complete absence of melanocytes Non-contagious • Manifestations – Complete loss of pigment – Variation in size an location – Symmetric and permanent • Treatment – Exposure to UVA and psoralens – Depigmentation of pigmented skin in extensive disease – Cosmetics and stains
Benign Skin Conditions: Lentigo • (see fig. 26 -7, Iggy page 465) – AKA liver spots – Increased number of melanocytes – Related to aging and sun exposure • Manifestations – Hyperpigmented brown to black flat lesion – Usually in sun exposed areas • Treatment – Liquid nitrogen • Possible reoccurrence in 1 -2 years – Cosmetics
Primary Lesions • Macule (freckles, petecchia, measles) – Flat – Change in color – < 1 cm • Papule (wart, mole) – elevated, – Solid – <1 cm • Vesicle (chicken pox, herpes zoster, 2 nd burns) – Elevated – Fluid filled – <1 cm
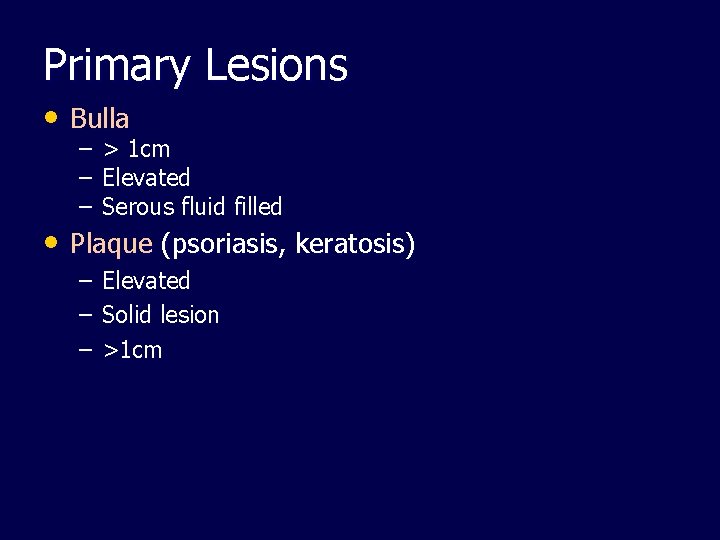
Primary Lesions • Bulla – > 1 cm – Elevated – Serous fluid filled • Plaque (psoriasis, keratosis) – – – Elevated Solid lesion >1 cm
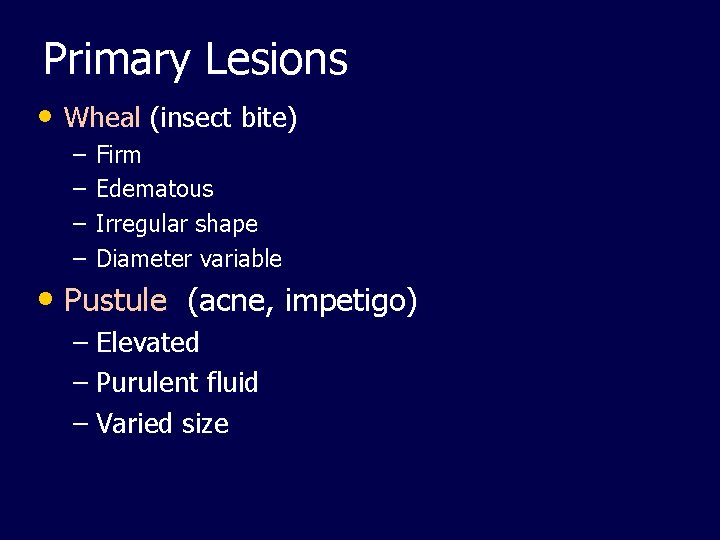
Primary Lesions • Wheal (insect bite) – – Firm Edematous Irregular shape Diameter variable • Pustule (acne, impetigo) – Elevated – Purulent fluid – Varied size
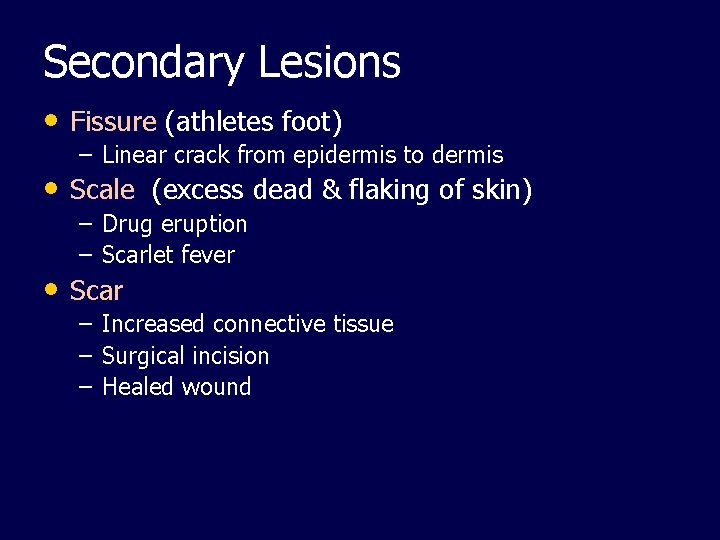
Secondary Lesions • Fissure (athletes foot) – Linear crack from epidermis to dermis • Scale (excess dead & flaking of skin) – – Drug eruption Scarlet fever – – – Increased connective tissue Surgical incision Healed wound • Scar
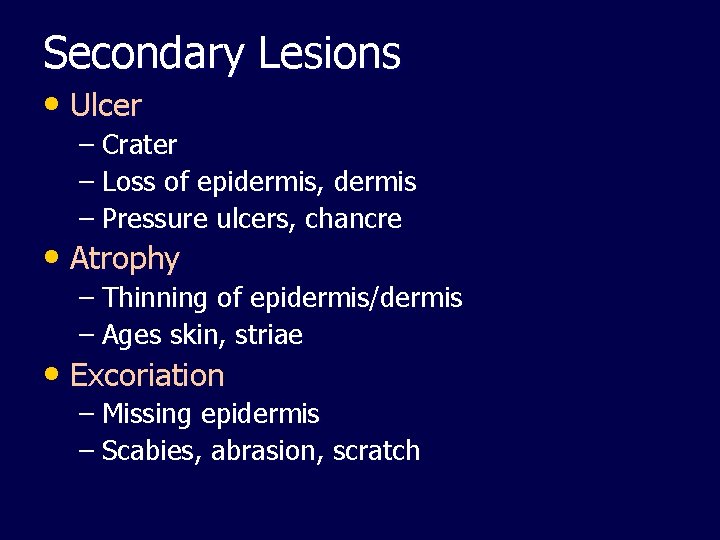
Secondary Lesions • Ulcer – Crater – Loss of epidermis, dermis – Pressure ulcers, chancre • Atrophy – Thinning of epidermis/dermis – Ages skin, striae • Excoriation – Missing epidermis – Scabies, abrasion, scratch

References: • Chickenpox in Pregnancy. (2009). March of Dimes Foundation. Retrieved 9/25/09 from • • • http: //www. marchofdimes. com/professionals/14332_1185. asp Common Poisonous Plants of Florida (Florida Poison Information Center/Tampa) @ http: //www. poisoncentertampa. org/poisonous-plants. aspx Culbert, D. (April 14, 2005). Florida scorpions. UF/IFAS Okeechobee County Extension Service. Retrieved 6/17/09 from http: //okeechobee. ifas. ufl. edu/News%20 columns/Florida. Scorpions. htm Groch, J. (August 23, 2006). Guidelines for Preventing Pressure Ulcers Seen as Suboptimal. Med. Page Today. Retrieved 6/12/09 from http: //www. medpagetoday. com/Dermatology/General. Dermatology/3982
References: • Hembree, D. (July 21, 2008) 10 Poisonous Plants in Florida and Safety Precautions @ • • • http: //www. associatedcontent. com/article/875395/10_poisonous_plants_in_florida_and_pg 2. html? cat=11 “Herpes simplex” (May, 2009). Medline Plus Medical Encyclopedia. Retrieved 6/15/09 from http: //www. nlm. nih. gov/MEDLINEPLUS/ency/article/001324. htm Lilly, L. L. , Harrington, S, & Snyder, J. (2005) Pharmacology and the Nursing Process. (4 th ed. ) Mosby Elsevier. St. Louis, MS. Medical Dictionary (2009) Merrium – Webster Inc. Retrieved 6/15/09 from http: //www. nlm. nih. gov/medlineplus/mplusdictionary. html
References: • The Medical News. Brain eating amoeba in lake kills sixth victim. (October 2007). Retrieved 6/16/09 from • • http: //www. news-medical. net/news/2007/10/07/30863. aspx The US Market for Skin Care Products. (May, 2005). Retrieved 6/12/09 from http: //www. mindbranch. com/Skincare-Products-R 567 -0199/ Scorpion Sting Treatments. (2008). Orkin. Retrieved 6/17/09 from http: //www. orkin. com/other/scorpions/scorpion -sting-treatments

Burns • Thermal burns – Flame, flash, scald • Chemical burns – Necrotizing substances • Acids • Alkali – Cleaning agents, drain cleaners, lye • Electrical burns – Intense heat from electrical current The Following Content – Burns – will be covered in future classes! Save this information for future use.
Classification: Depth of Burn See page 522 in Iggy text • ABA by depth of destruction – Partial thickness burn • Epidermis and dermis involved – Full thickness burn • “burns reach through the entire dermis and sometimes into the subcutaneous fat. ” (Iggy, page 522) • Possibly involves muscles, tendons, and bones • *Skin cannot heal on its own.
Classification: Extent of Burn • Total Body Surface Area (TBSF) – (Iggy page 531) • Berkow method – http: //www. umobile. edu/main/notes/Burn. pdf • Rule of 9’s – (Iggy page 531)
Classification: Location of Burns • Severity related to location • Complication risks related to location • Face, neck, chest – Respiratory complications • Hands, feet, joints, and eyes – Compromise ADLs • Circumferential burns of extremities – Circulatory compromise
Emergent Care • A, B, C’s • Fluid Therapy • Wound Care • Pain management • Prevention of infection
Burns What happens….
Complications of Emergent Phase • Cardiovascular – Arrhythmias – Hypovolemic shock – Impaired circulation • Respiratory – Upper airway burns – Inhalation injuries • Urinary – Acute tubular necrosis
Acute Phase • Fluid therapy – Lactated Ringers per Parkland (Baxter) formula • Wound care – Topical silvadene, sulfamylon, bacitracin, or bactroban – PREVENT INFECTION • Excision and grafting – Remove necrotic tissue – Apply split thickness auto graft skin • Porcine skin, cadaver skin, clients own skin, skin culture • Nutritional therapy – Increased fluids, proteins, vitamins A, C, E. – Zinc, iron, folate • Physical therapy – Prevent contractures • Physical and psychological comfort
Drug Therapy: Antibiotics • Silver Sulfadiazine (Slivadene) – Burn treatment – QD or BID – “frosting” – Adverse effects • Pain • Itching • Burning
Rehabilitation Phase • Prevent and minimize contractures and scarring! • Cosmetic / reconstructive therapy • Psychological support if needed