Integumentary System Part 2 Skin Disorders Unit 3




- Slides: 30
Integumentary System Part 2: Skin Disorders Unit 3: Integumentary System A&P Chapter 5
Skin Disorders � 1. Chronic Disorders � 2. Infectious Disorders � 3. Burns � 4. Skin Cancers
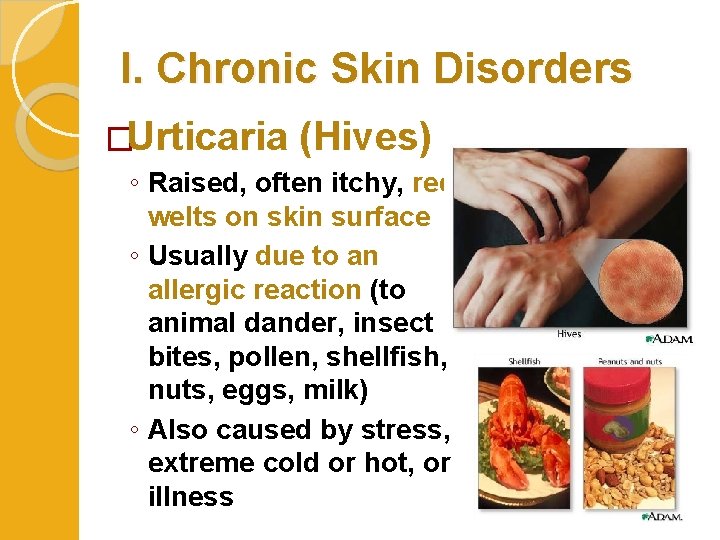
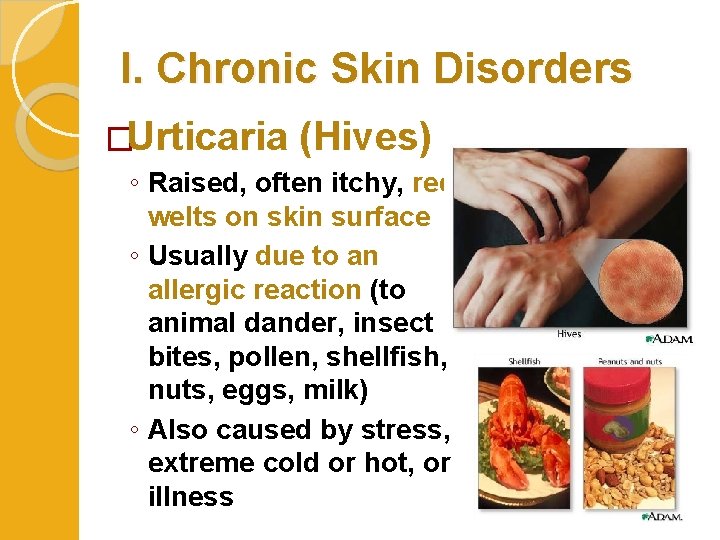
I. Chronic Skin Disorders �Urticaria (Hives) ◦ Raised, often itchy, red welts on skin surface ◦ Usually due to an allergic reaction (to animal dander, insect bites, pollen, shellfish, nuts, eggs, milk) ◦ Also caused by stress, extreme cold or hot, or illness
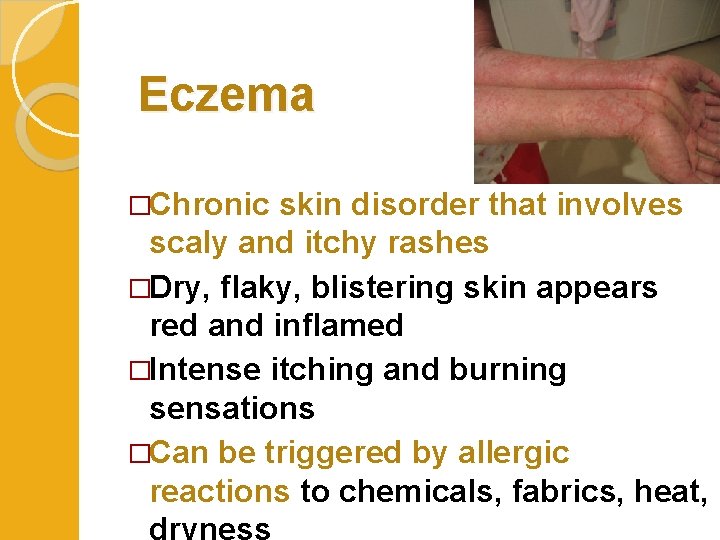
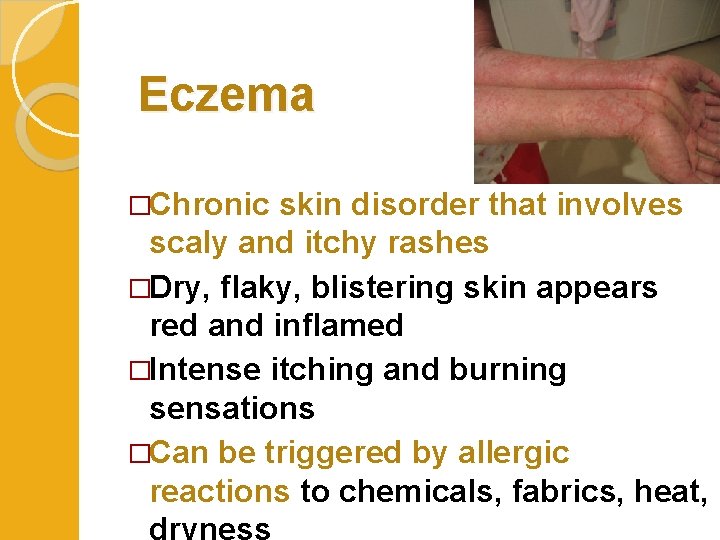
Eczema �Chronic skin disorder that involves scaly and itchy rashes �Dry, flaky, blistering skin appears red and inflamed �Intense itching and burning sensations �Can be triggered by allergic reactions to chemicals, fabrics, heat, dryness
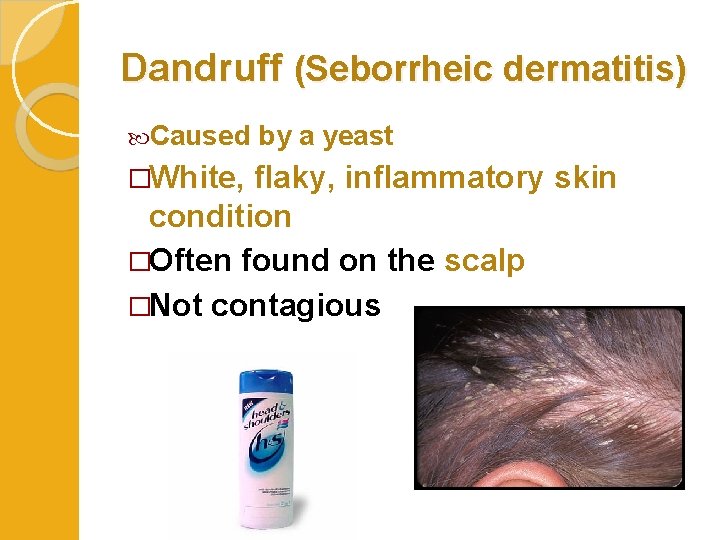
Dandruff (Seborrheic dermatitis) Caused �White, by a yeast flaky, inflammatory skin condition �Often found on the scalp �Not contagious
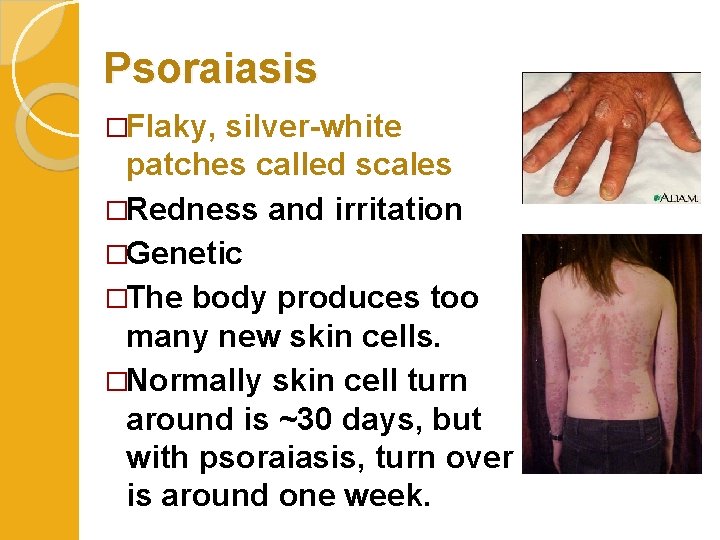
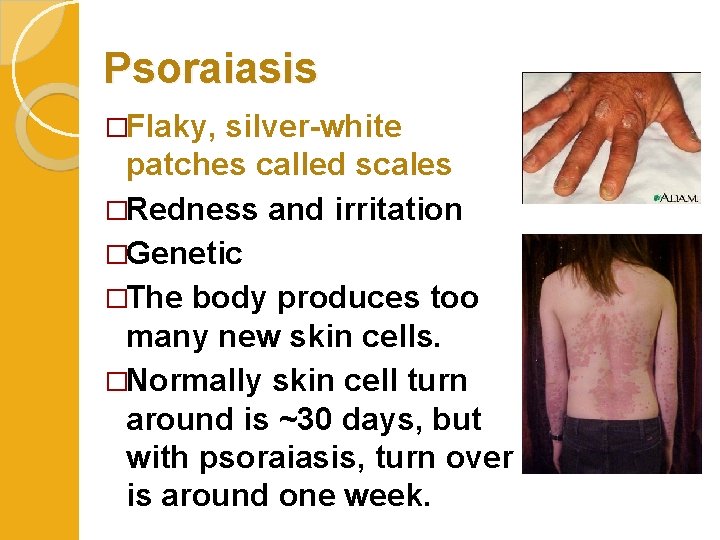
Psoraiasis �Flaky, silver-white patches called scales �Redness and irritation �Genetic �The body produces too many new skin cells. �Normally skin cell turn around is ~30 days, but with psoraiasis, turn over is around one week.
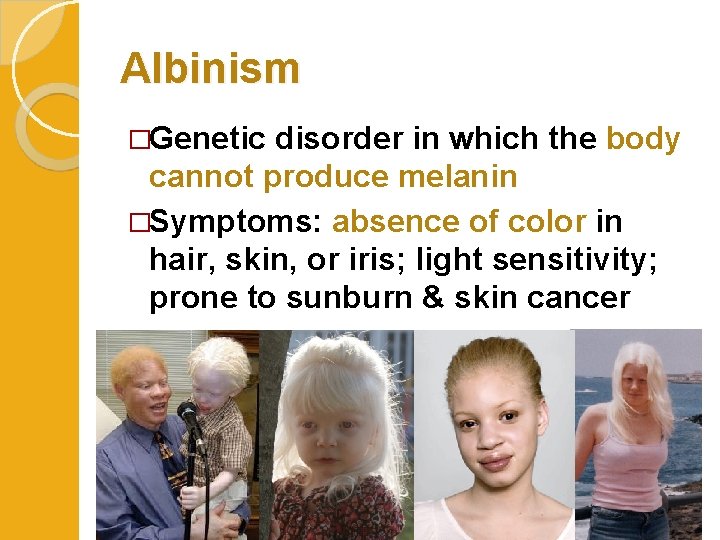
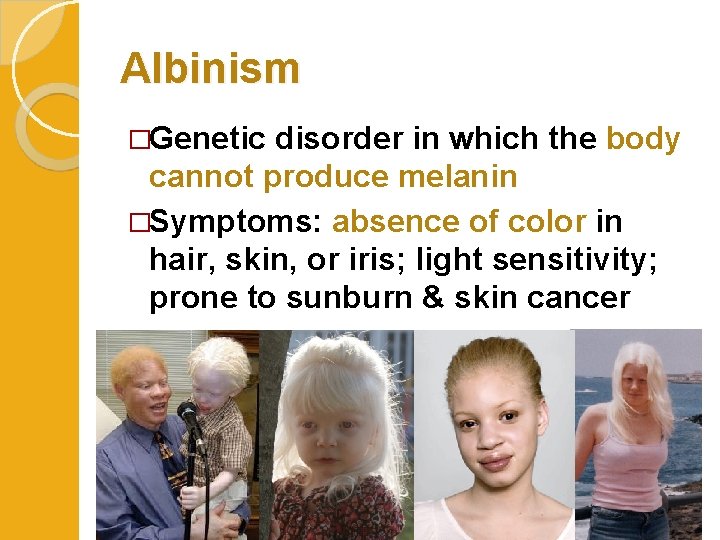
Albinism �Genetic disorder in which the body cannot produce melanin �Symptoms: absence of color in hair, skin, or iris; light sensitivity; prone to sunburn & skin cancer

II. Infectious Skin Disorders �Impetigo ◦ Bacterial infection ◦ Highly contagious ◦ Causes blisters or sores on face and hands ◦ Common among kids
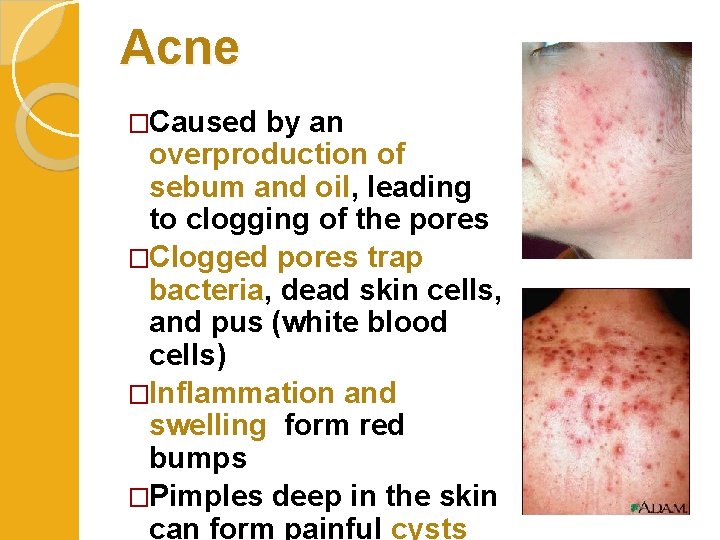
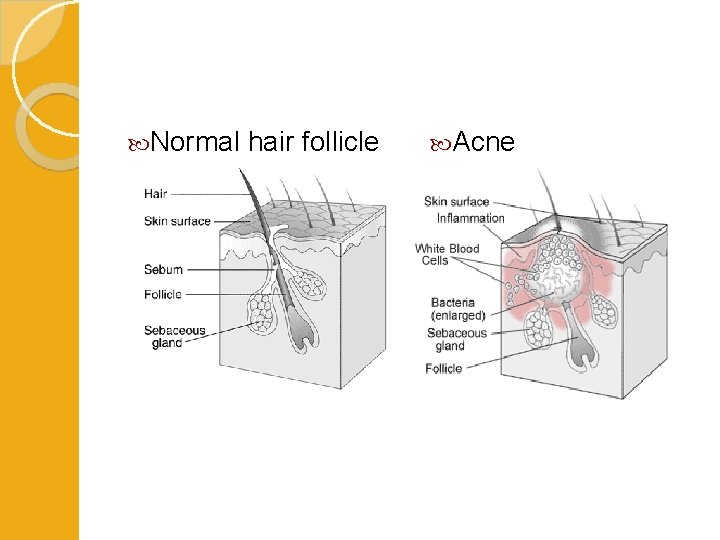
Acne �Caused by an overproduction of sebum and oil, leading to clogging of the pores �Clogged pores trap bacteria, dead skin cells, and pus (white blood cells) �Inflammation and swelling form red bumps �Pimples deep in the skin can form painful cysts
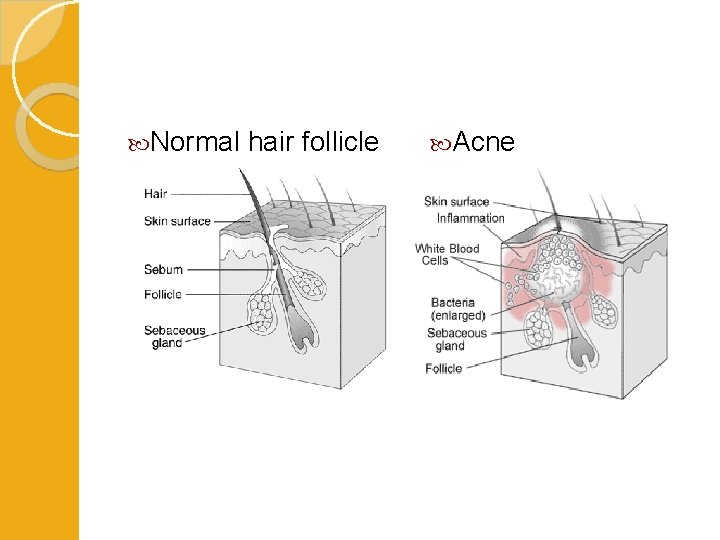
Normal hair follicle Acne
�Other causes of acne Genetics Hormonal changes due to menstrual cycles (females) or stress Greasy or oily cosmetic and hair products Certain drugs (such as steroids, testosterone, estrogen) High levels of humidity and sweating Diets high in refined sugars
Athlete’s Foot �Fungal infection �Very common on foot or other moist, warm areas of body �Fungus infects the upper layers of the skin, causing itching, cracking, and pain

Ringworm Not a worm, caused by fungus Occurs in warm, moist areas with frequent wetness (such as from sweating) and minor injuries to your skin Itchy, red, raised, scaly patches that may blister and ooze

Necrotizing Fasciitis disease” �Very rare bacterial infection �Necrosis (death) of the subcutaneous layer of skin � “Flesh-eating

MRSA (Methicillin-Resistant Staphylococcus aureus) �Staph infections are caused by bacteria �Staphylococcus bacteria normally lives on the skin with no problems �MRSA is a strain that is resistant to antibiotics and therefore very dangerous or deadly
Signs & Symptoms MRSA �People in hospitals are most likely to get MRSA �Staph skin infections start as small red bumps that resemble pimples, boils or spider bites �Quickly turn into deep, painful abscesses that must be surgically drained �Sometimes the bacteria remain in the skin, but if it penetrates into the body, it can be life-threatening
III. Skin Burns �A burn is tissue damage which destroys cell proteins and cause cell death in the affected areas �Caused by: ◦ Heat ◦ Radiation (sunlight, tanning beds) ◦ Chemicals ◦ Electricity
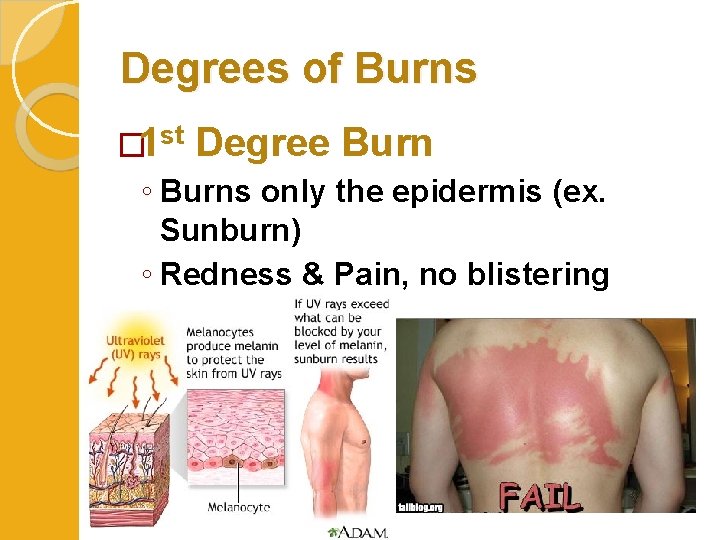
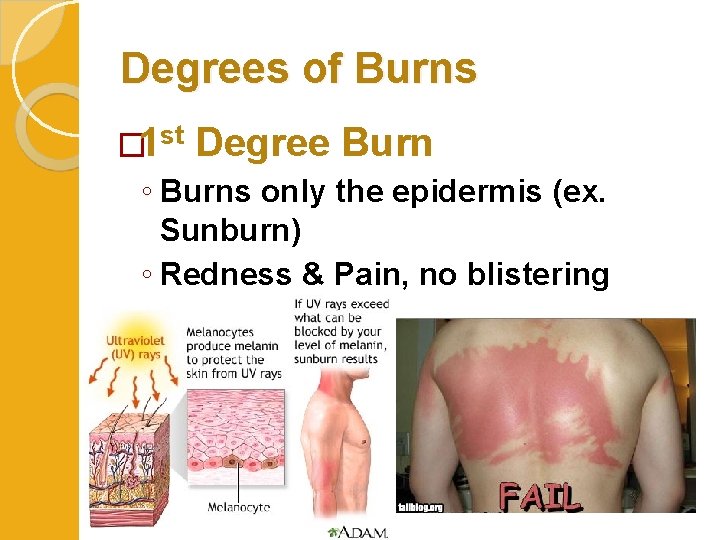
Degrees of Burns � 1 st Degree Burn ◦ Burns only the epidermis (ex. Sunburn) ◦ Redness & Pain, no blistering
Are Tanning Beds Safer? �The salons say yes, but studies show tanning beds still increase the risk of cancer
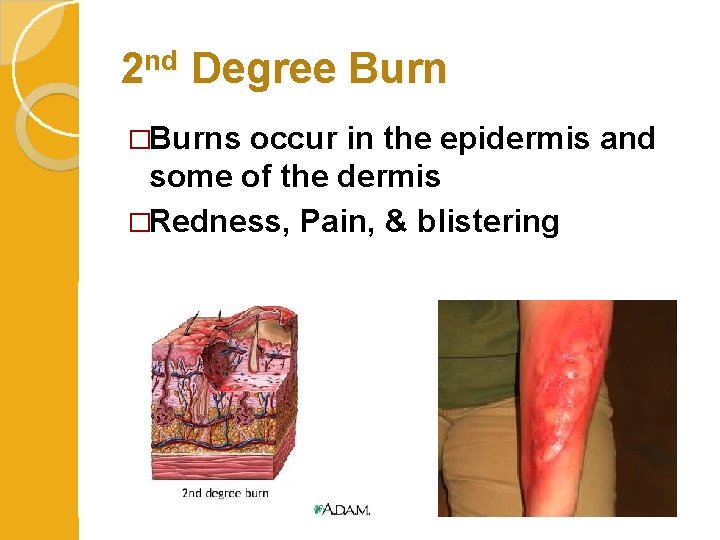
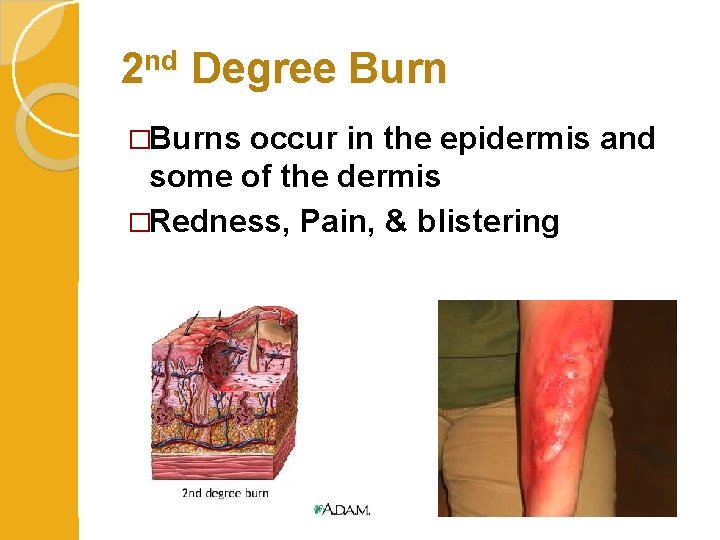
2 nd Degree Burn �Burns occur in the epidermis and some of the dermis �Redness, Pain, & blistering
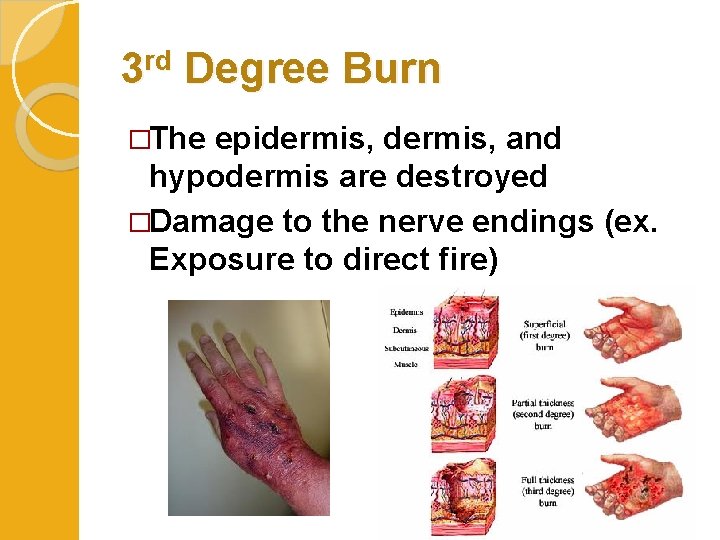
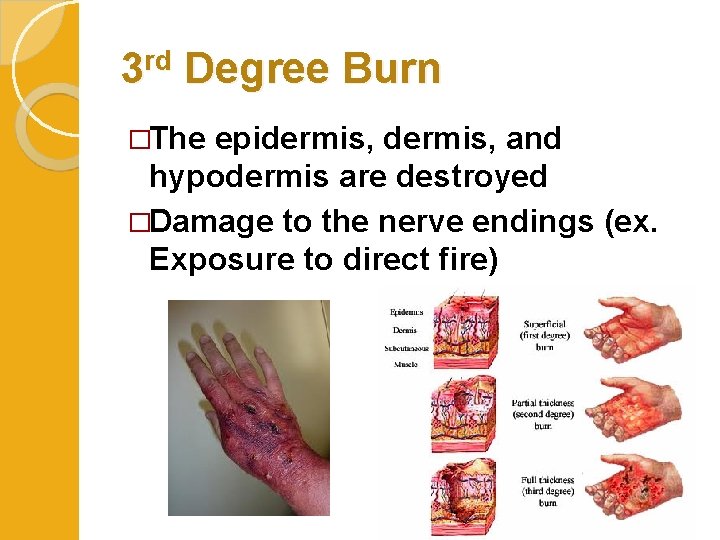
3 rd Degree Burn �The epidermis, and hypodermis are destroyed �Damage to the nerve endings (ex. Exposure to direct fire)
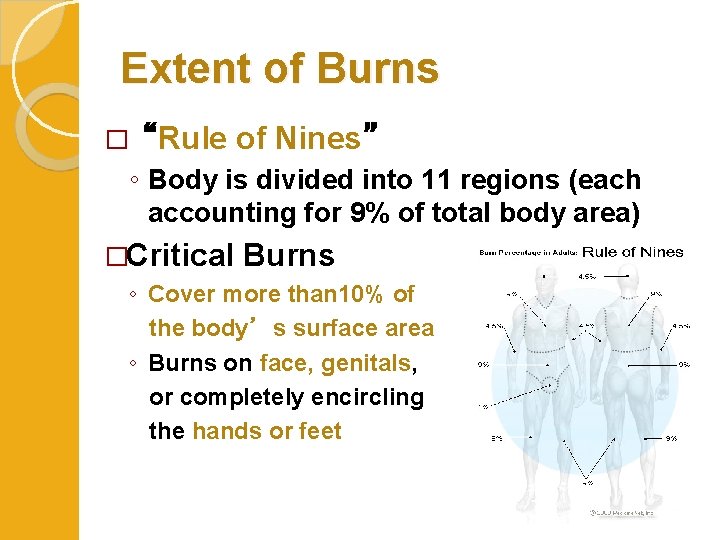
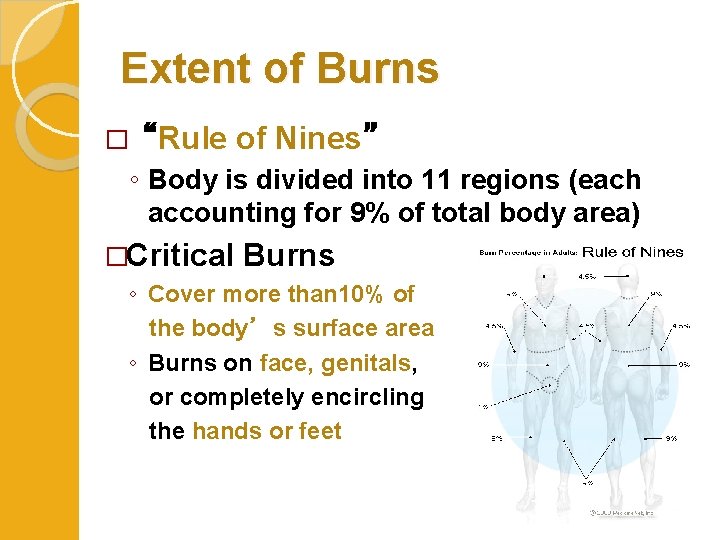
Extent of Burns �“Rule of Nines” ◦ Body is divided into 11 regions (each accounting for 9% of total body area) �Critical Burns ◦ Cover more than 10% of the body’s surface area ◦ Burns on face, genitals, or completely encircling the hands or feet
Treatment of Critical Burns �Complications: ◦ Infection, hypothermia, dehydration �Intense doses of intravenous fluids to replace electrolyte imbalance �Warm and isolated environment to reduce risk of infection �Skin graft can be done as soon as patient is stable
IV. Skin Cancer �Risk Factors ◦ Age (Older people) ◦ Light-skin ◦ Excessive sun exposure ◦ Genetics (family history) ◦ Chemical exposure �When to see your doctor: ◦ If you have any of the warning signs, are older, or have a family history of skin cancer
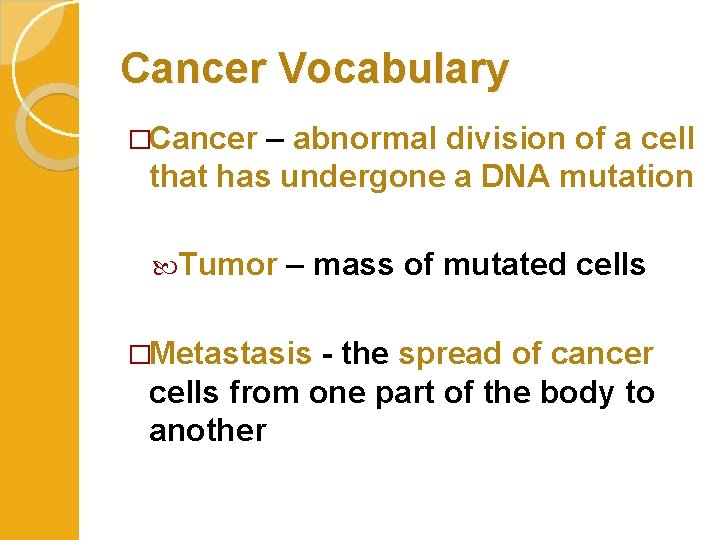
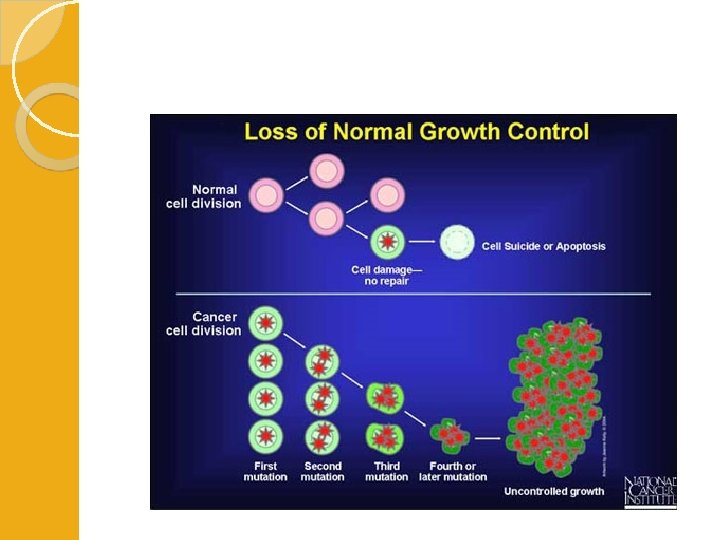
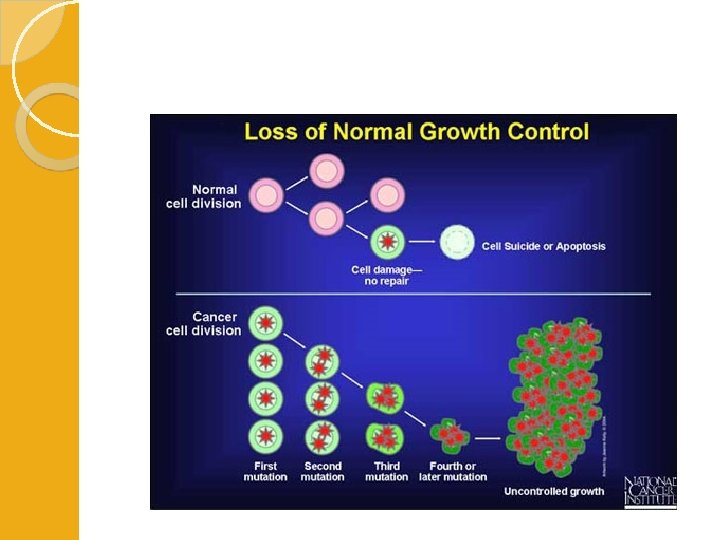
Cancer Vocabulary �Cancer – abnormal division of a cell that has undergone a DNA mutation Tumor – mass of mutated cells �Metastasis - the spread of cancer cells from one part of the body to another
�Two Categories of Skin Cancer: ◦ 1) Non-Melanoma � Includes Basal cell carcinoma and Squamous cell carcinoma ◦ 2) Melanoma
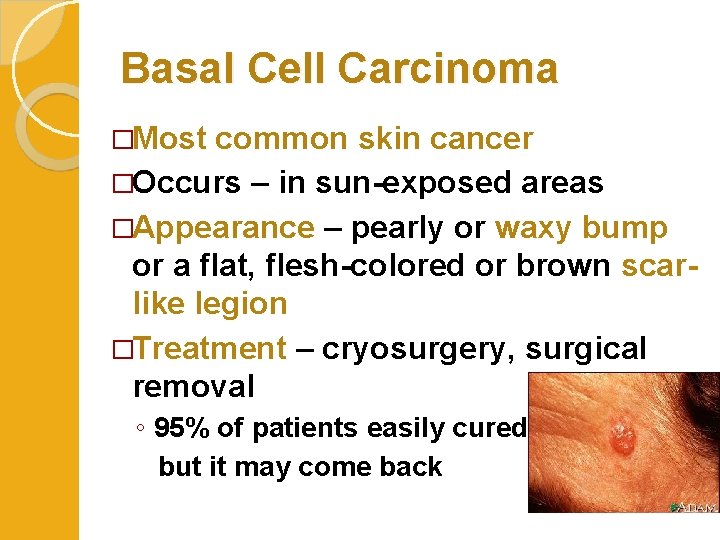
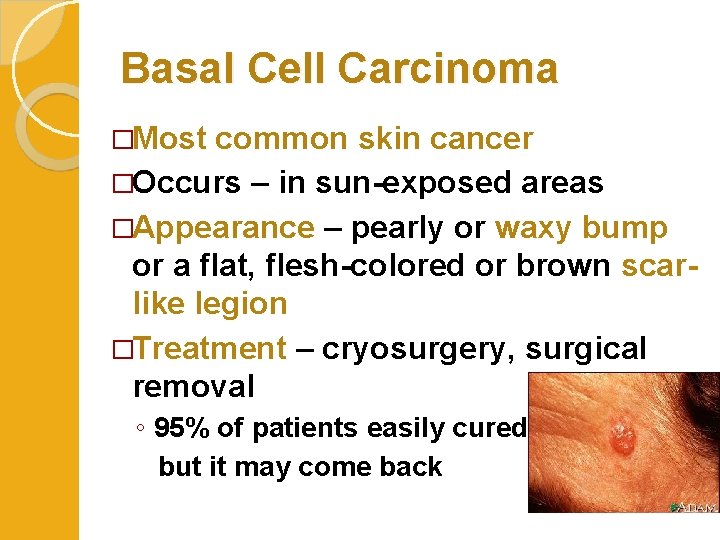
Basal Cell Carcinoma �Most common skin cancer �Occurs – in sun-exposed areas �Appearance – pearly or waxy bump or a flat, flesh-colored or brown scarlike legion �Treatment – cryosurgery, surgical removal ◦ 95% of patients easily cured, but it may come back
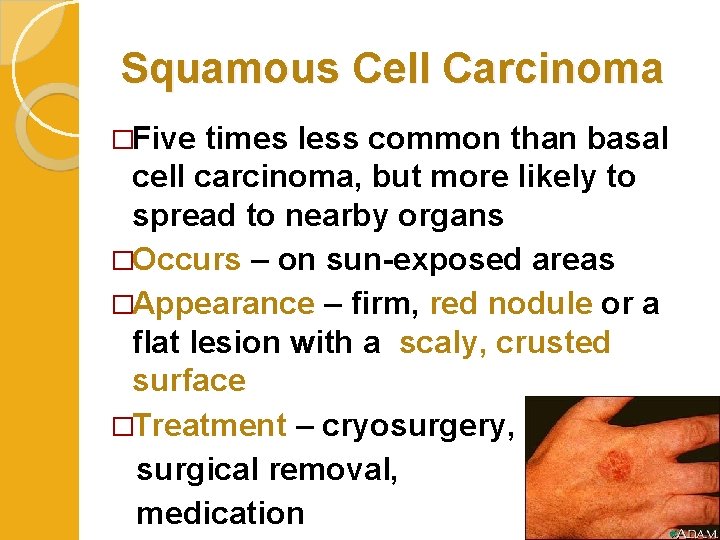
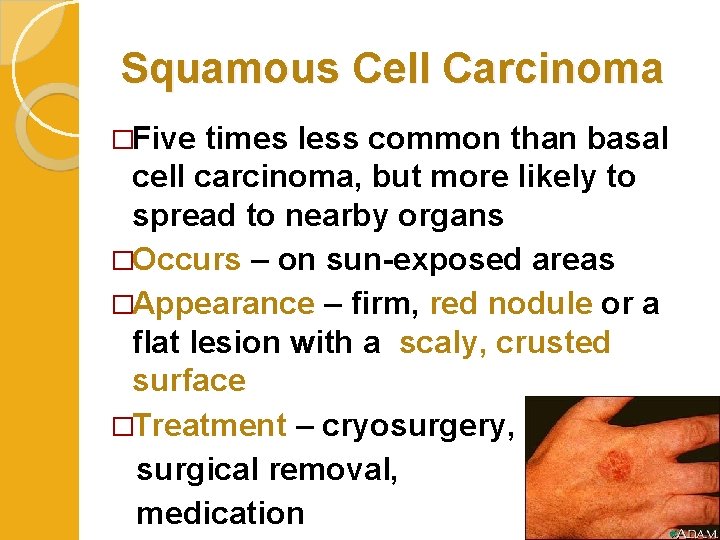
Squamous Cell Carcinoma �Five times less common than basal cell carcinoma, but more likely to spread to nearby organs �Occurs – on sun-exposed areas �Appearance – firm, red nodule or a flat lesion with a scaly, crusted surface �Treatment – cryosurgery, surgical removal, medication
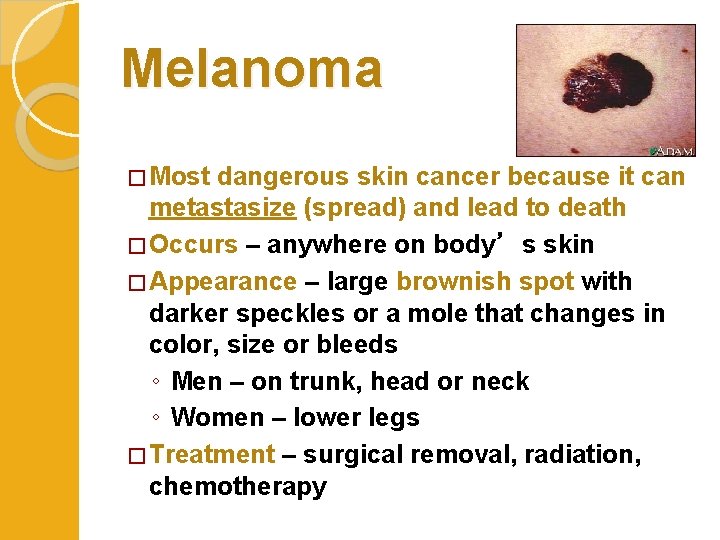
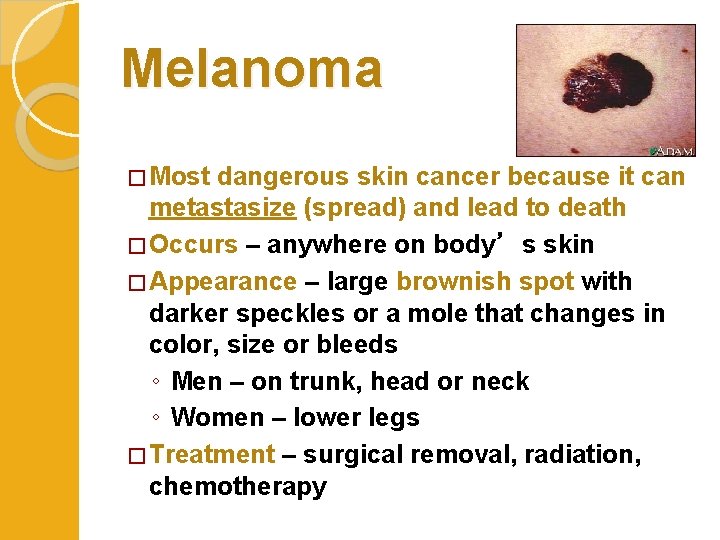
Melanoma � Most dangerous skin cancer because it can metastasize (spread) and lead to death � Occurs – anywhere on body’s skin � Appearance – large brownish spot with darker speckles or a mole that changes in color, size or bleeds ◦ Men – on trunk, head or neck ◦ Women – lower legs � Treatment – surgical removal, radiation, chemotherapy