INTEGUMENTARY SYSTEM COMPONENTS OF THE INTEGUMENTARY SYSTEM Figure

- Slides: 60
INTEGUMENTARY SYSTEM
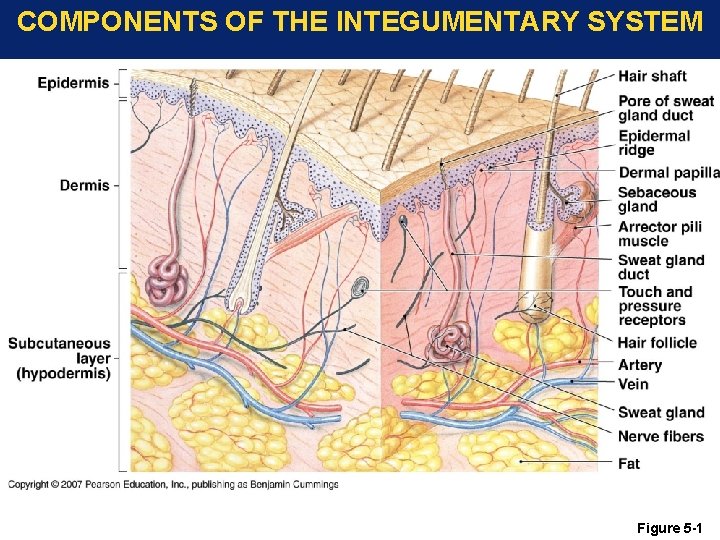
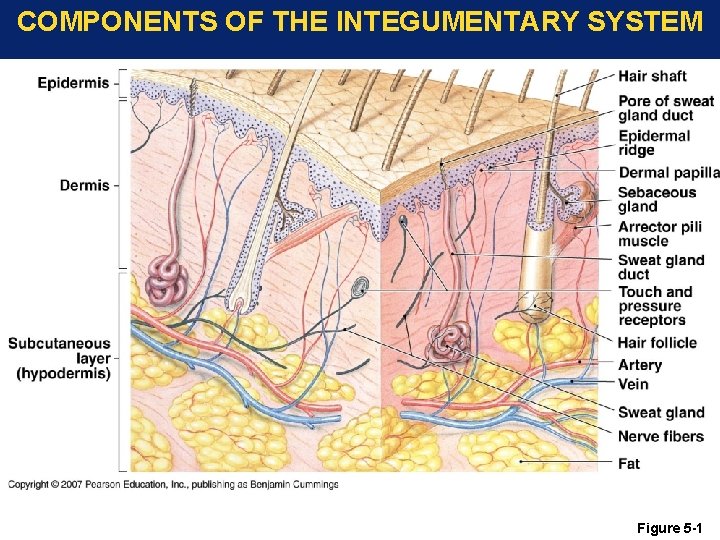
COMPONENTS OF THE INTEGUMENTARY SYSTEM Figure 5 -1
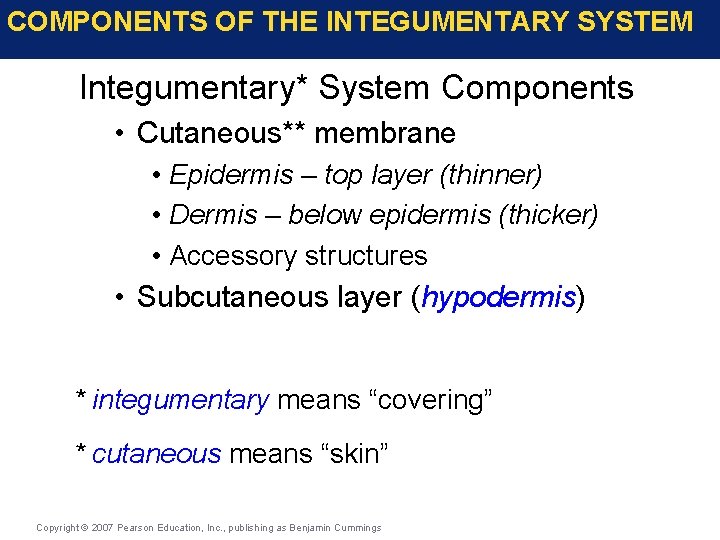
COMPONENTS OF THE INTEGUMENTARY SYSTEM Integumentary* System Components • Cutaneous** membrane • Epidermis – top layer (thinner) • Dermis – below epidermis (thicker) • Accessory structures • Subcutaneous layer (hypodermis) * integumentary means “covering” * cutaneous means “skin” Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings
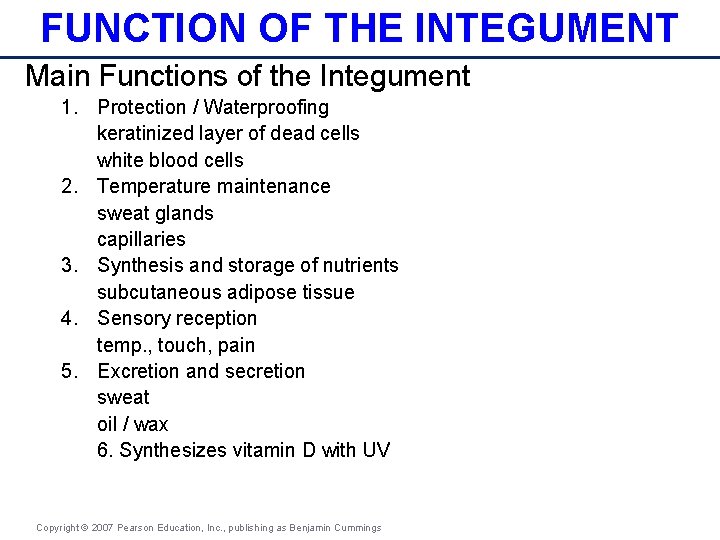
FUNCTION OF THE INTEGUMENT Main Functions of the Integument 1. Protection / Waterproofing keratinized layer of dead cells white blood cells 2. Temperature maintenance sweat glands capillaries 3. Synthesis and storage of nutrients subcutaneous adipose tissue 4. Sensory reception temp. , touch, pain 5. Excretion and secretion sweat oil / wax 6. Synthesizes vitamin D with UV Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings
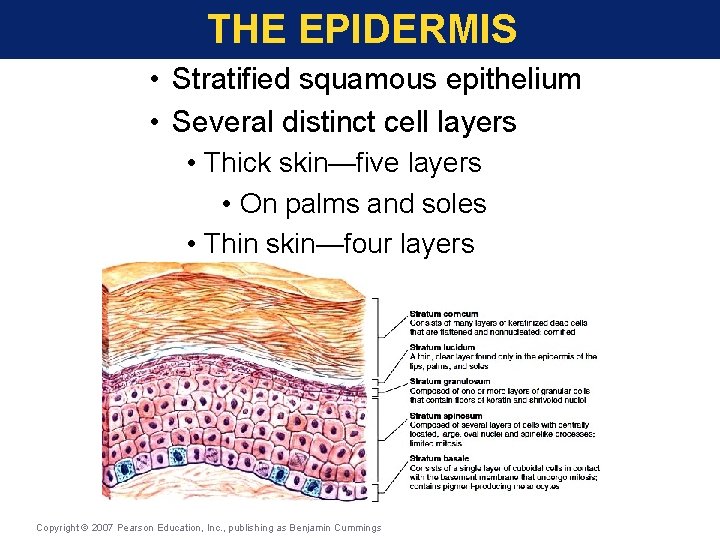
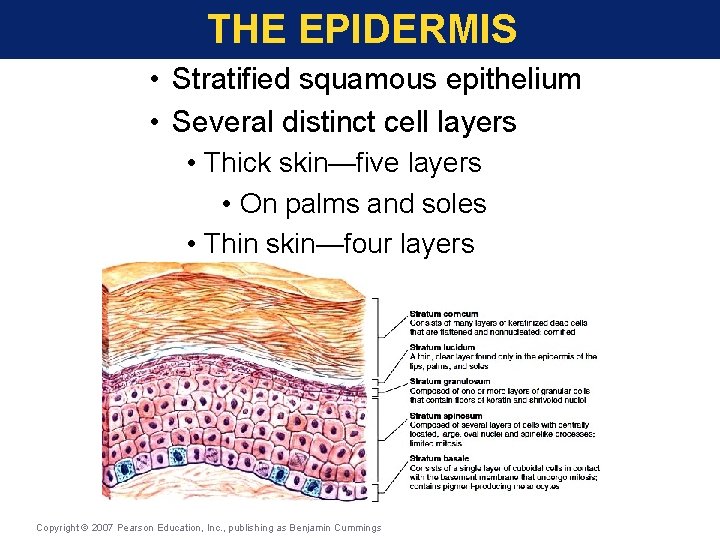
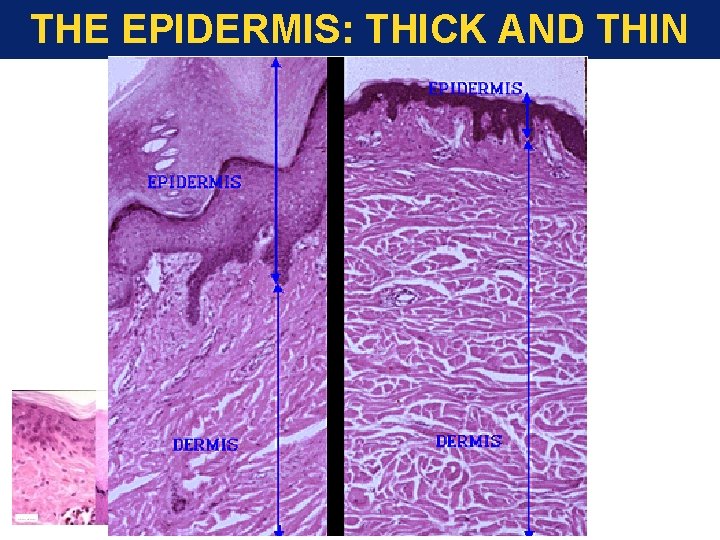
THE EPIDERMIS • Stratified squamous epithelium • Several distinct cell layers • Thick skin—five layers • On palms and soles • Thin skin—four layers • On rest of body Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings
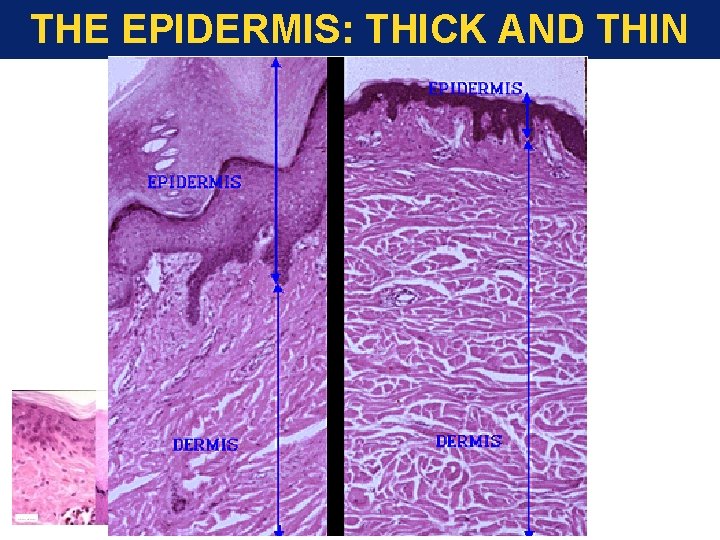
THE EPIDERMIS: THICK AND THIN SKIN
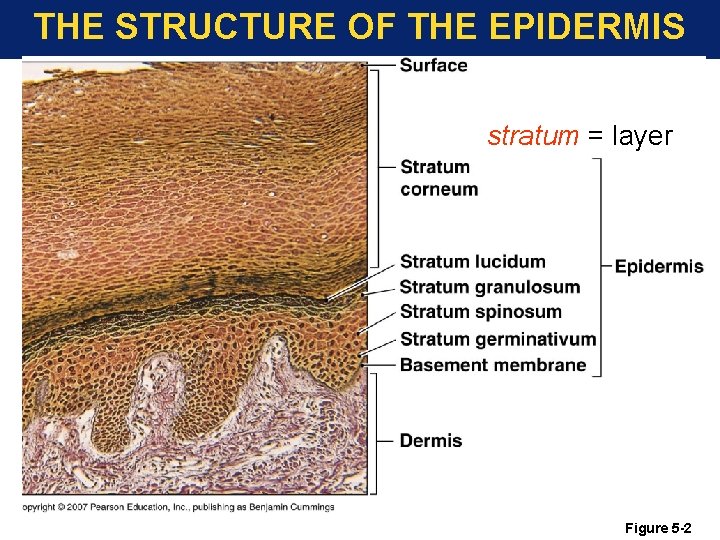
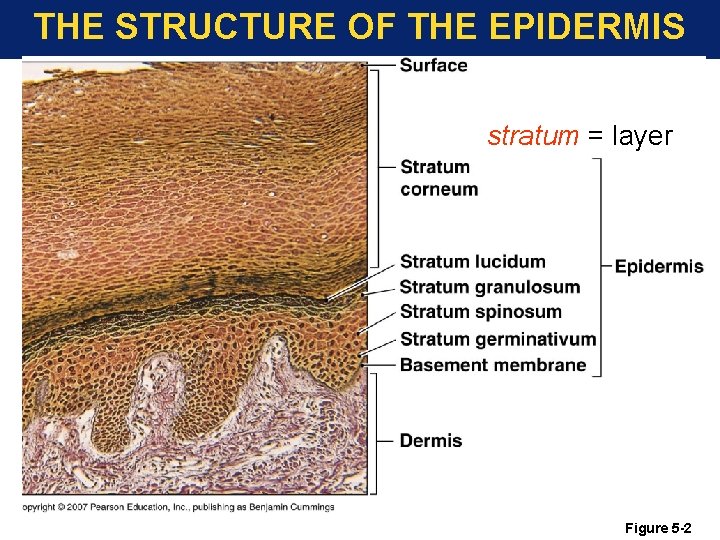
THE STRUCTURE OF THE EPIDERMIS stratum = layer Figure 5 -2
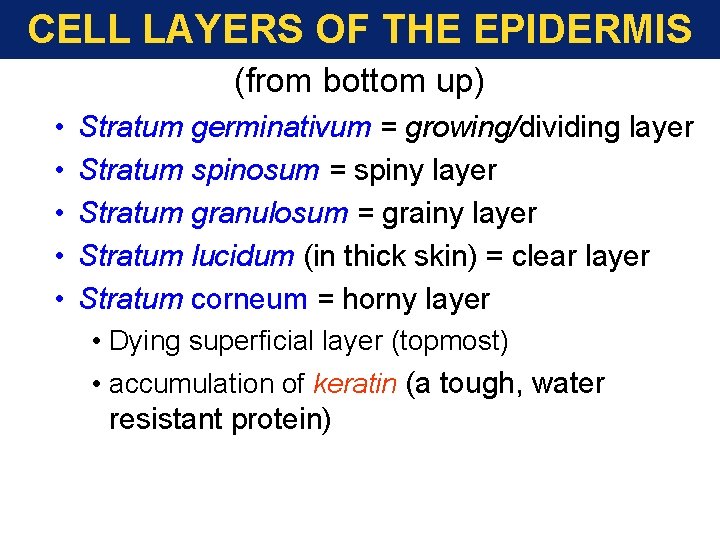
CELL LAYERS OF THE EPIDERMIS (from bottom up) • • • Stratum germinativum = growing/dividing layer Stratum spinosum = spiny layer Stratum granulosum = grainy layer Stratum lucidum (in thick skin) = clear layer Stratum corneum = horny layer • Dying superficial layer (topmost) • accumulation of keratin (a tough, water resistant protein)
CELL LAYERS OF THE EPIDERMIS • STRATUM GERMINATIVUM • Basal layer • Contain Merkel cells (found on skin that lack hair) sense touch then release chemicals. • Contain Stem cells • Mitotic cell division layer • Source of replacement cells. High mechanical stress, the cells stem cells divide more rapidly and the depth of the epidermis increases, thus a callus. • Contain Melanocytes • Synthesize melanin = brown pigment • Convert cholesterol related steroid to vitamin d
CELL LAYERS OF THE EPIDERMIS • Intermediate layers • Stratum spinosum (spiny layer) • 8 -10 layers of cells • Cells look like miniature pin cushions • Some cells still divide • Contain Langerhan cells (Immune) • May contain superficial cancer cells Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings
CELL LAYERS OF THE EPIDERMIS • Stratum granulosum (grainy layer) • 3 -5 Layers of cells • Keratin granules in cytoplasm • No cell division • Begin making large amounts of Keratin • Stratum lucidum (clear layer) • Found in thick skin • Flattened, densely packed and filled with Keratin
CELL LAYERS OF THE EPIDERMIS • Stratum corneum • 15 -30 Layers of cells • • Most superficial layer Flattened (squamous) cells Dead cells Abundant keratin • Keratinized (also, cornified) • Tough, water-resistant protein • Only maintenance is to coar surface with lipid sedretions from sebaceous and sweat glands • Water-resistant not waterproof.
CELL LAYERS OF THE EPIDERMIS TIMING OF MOVEMENT BETWEEN LAYERS: • Stratum Basal cells take to 15 - 30 days to reach Stratum Corneum. • Cells remain in S. Corneum an additional 2 weeks before they are shed. • Replace cells of the skin once every two months
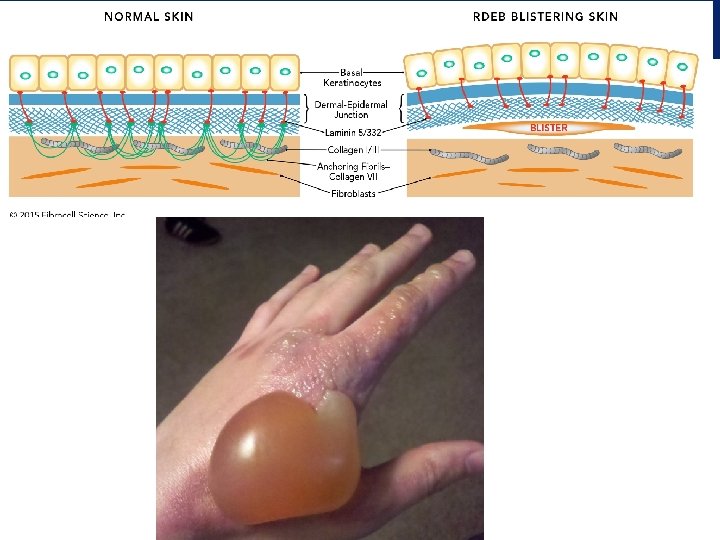
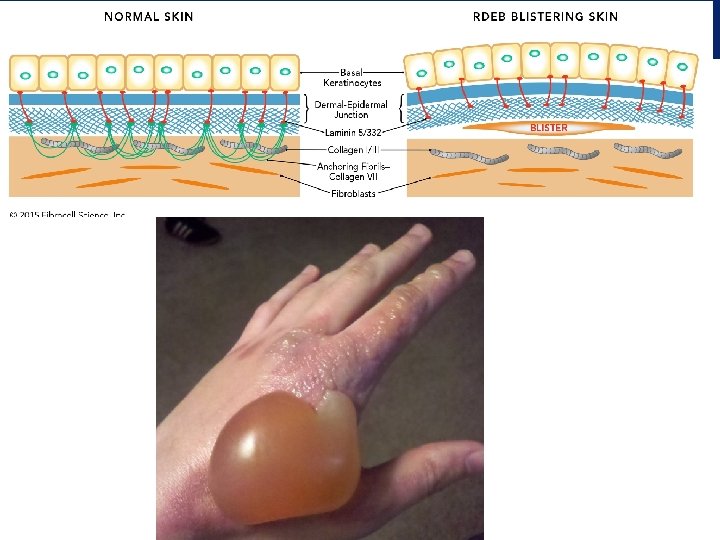
INSENSIBLE PERSPIRATION VS. SENSIBLE PERSPIRATION Insensible Perspiration: water loss from interstitial fluids slowly penetrates the stratum corneum to the surface and evaporates. 1 pint of water per day is lost through the skin Sensible Perspiration: produced by sweat glands Damage to the epidermis can speed up the water loss • Blisters • Burns
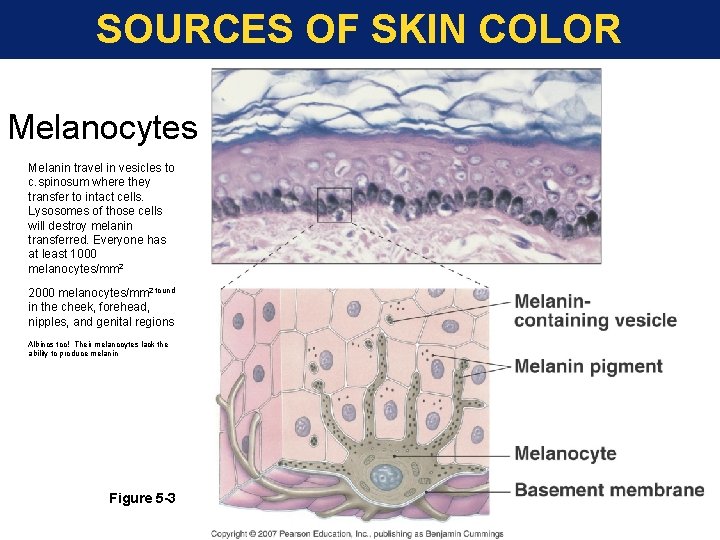
SOURCES OF SKIN COLOR • Melanocytes • make pigment, melanin • melanin provides UV protection • gives reddish-brown to brown-black color • Carotene • a pro-vitamin (gets converted to vitamin A) • contributes orange-yellow color • provided from diet • Hemoglobin • red blood pigment • carries O 2 to tissues and some CO 2 away from tissues
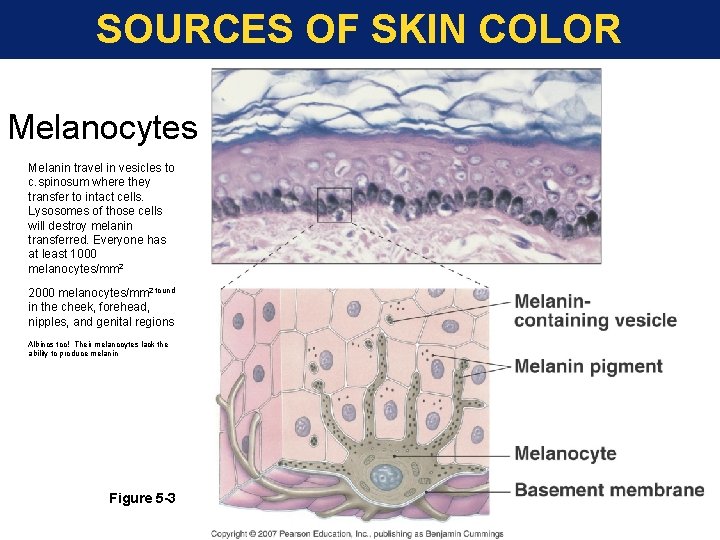
SOURCES OF SKIN COLOR Melanocytes Melanin travel in vesicles to c. spinosum where they transfer to intact cells. Lysosomes of those cells will destroy melanin transferred. Everyone has at least 1000 melanocytes/mm 2 2000 melanocytes/mm 2 found in the cheek, forehead, nipples, and genital regions Albinos too! Their melanocytes lack the ability to produce melanin Figure 5 -3
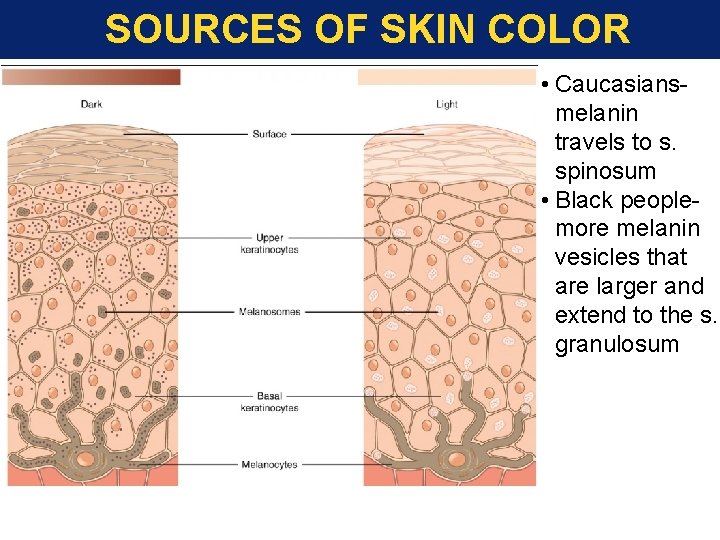
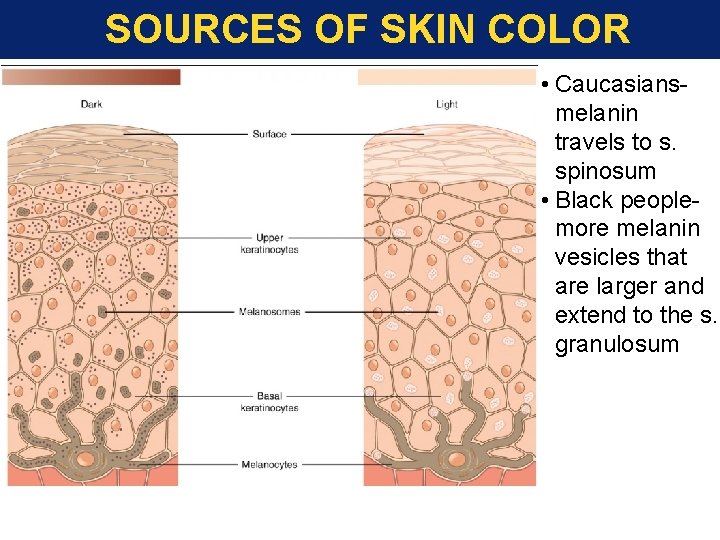
SOURCES OF SKIN COLOR • Caucasiansmelanin travels to s. spinosum • Black peoplemore melanin vesicles that are larger and extend to the s. granulosum
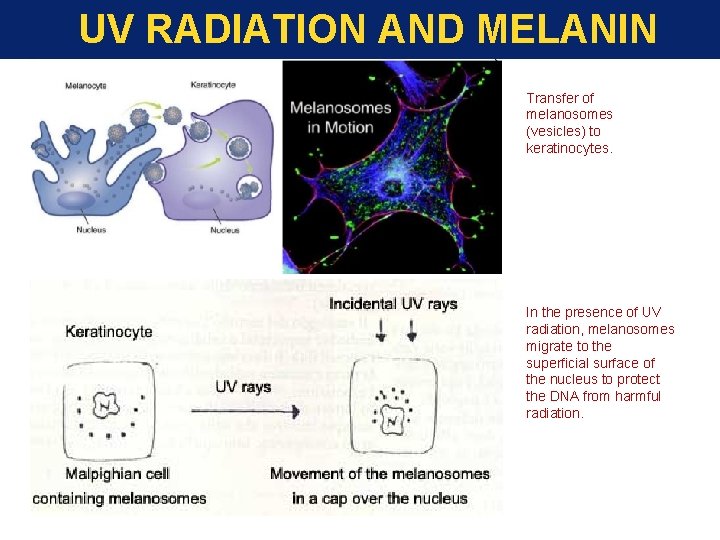
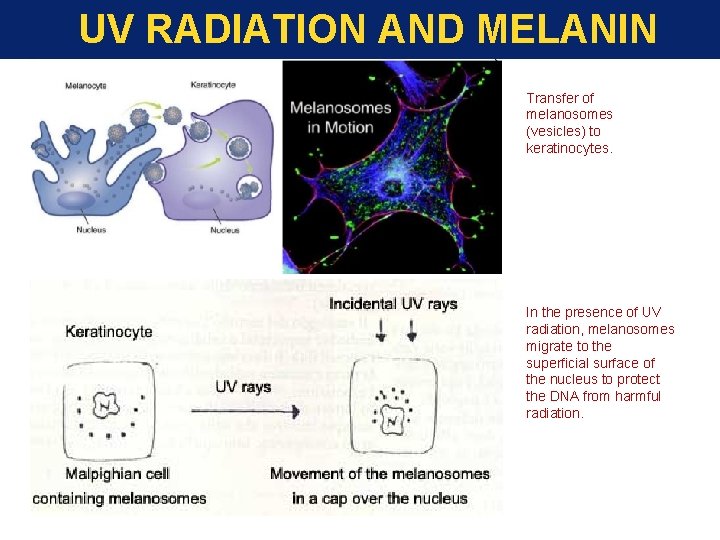
UV RADIATION AND MELANIN Transfer of melanosomes (vesicles) to keratinocytes. In the presence of UV radiation, melanosomes migrate to the superficial surface of the nucleus to protect the DNA from harmful radiation.
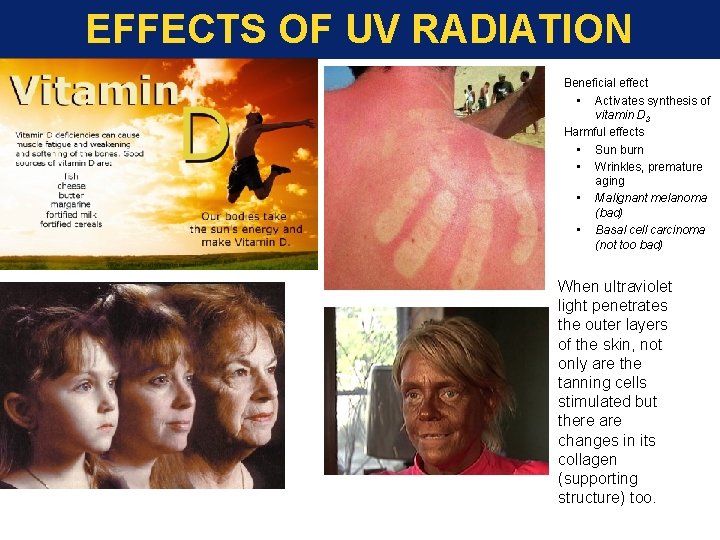
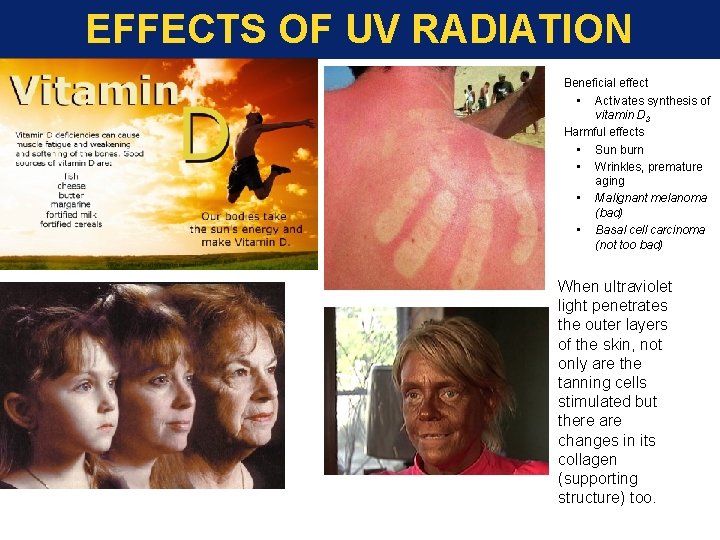
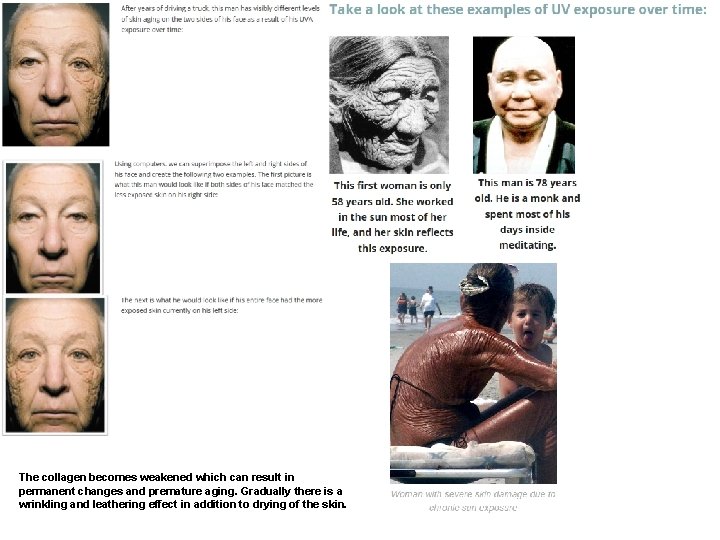
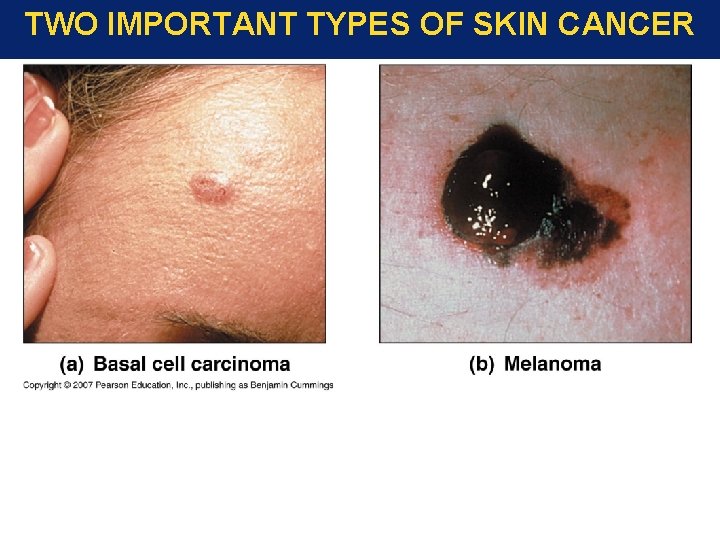
EFFECTS OF UV RADIATION • • Beneficial effect • Activates synthesis of vitamin D 3 Harmful effects • Sun burn • Wrinkles, premature aging • Malignant melanoma (bad) • Basal cell carcinoma (not too bad) When ultraviolet light penetrates the outer layers of the skin, not only are the tanning cells stimulated but there are changes in its collagen (supporting structure) too.
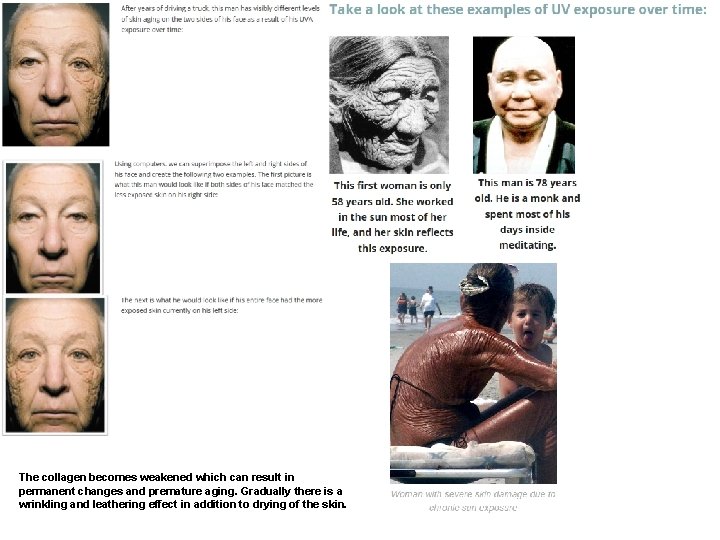
The collagen becomes weakened which can result in permanent changes and premature aging. Gradually there is a wrinkling and leathering effect in addition to drying of the skin.
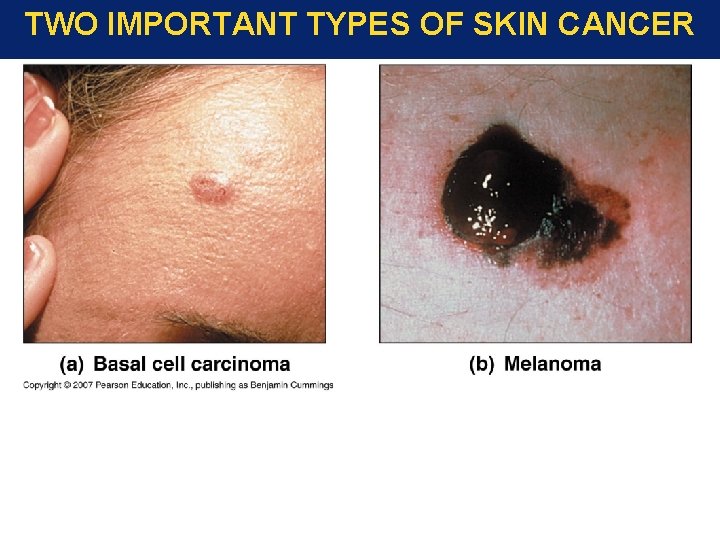
TWO IMPORTANT TYPES OF SKIN CANCER
EPIDERMIS: STRUCTURE/FUNCTION Key Note The epidermis is a multi-layered, flexible, self-repairing barrier that prevents fluid loss, provides protection from UV radiation, produces vitamin D 3, and resists damage from abrasion, chemicals, and pathogens (=disease-causers) Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings
DERMIS Strong, flexible connective tissue: your “hide” Cells: fibroblasts, macrophages, mast cells, WBCs Fiber types: collagen, elastic, reticular Rich supply of nerves and vessels Critical role in temperature regulation (the vessels) Two layers (see next slides) • Papillary – areolar connective tissue; includes dermal papillae • Reticular – “reticulum” (network) of collagen and reticular fibers
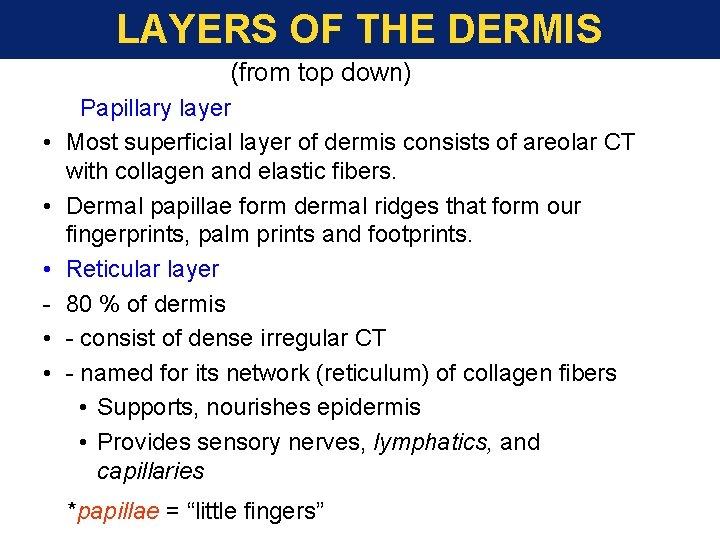
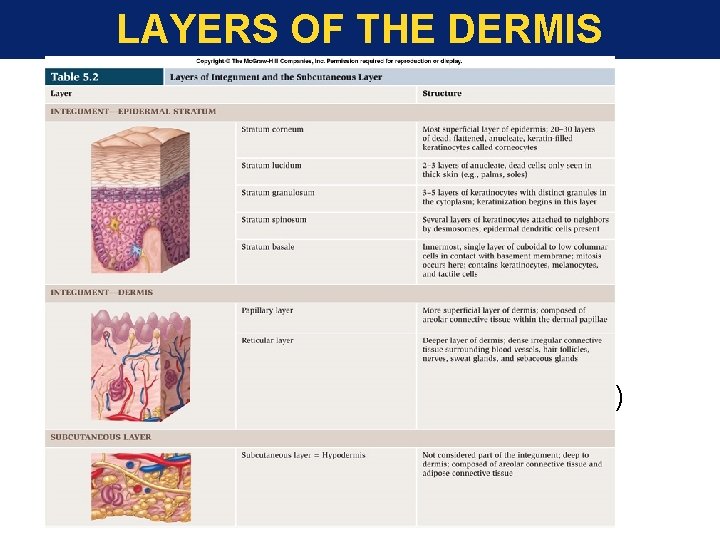
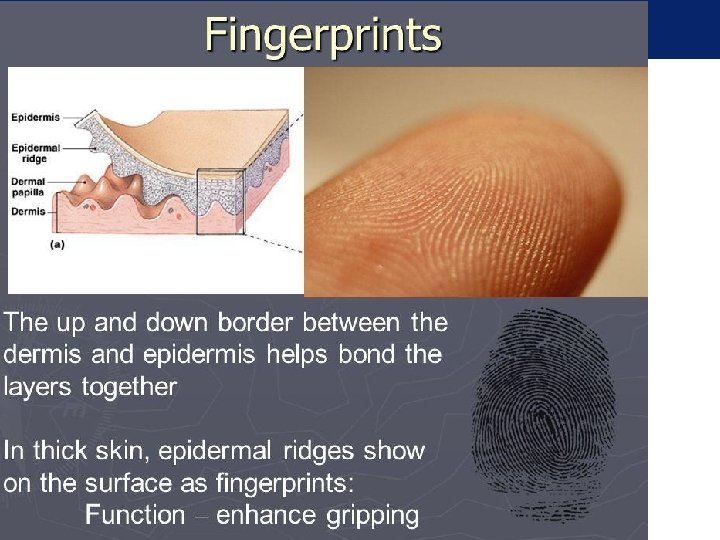
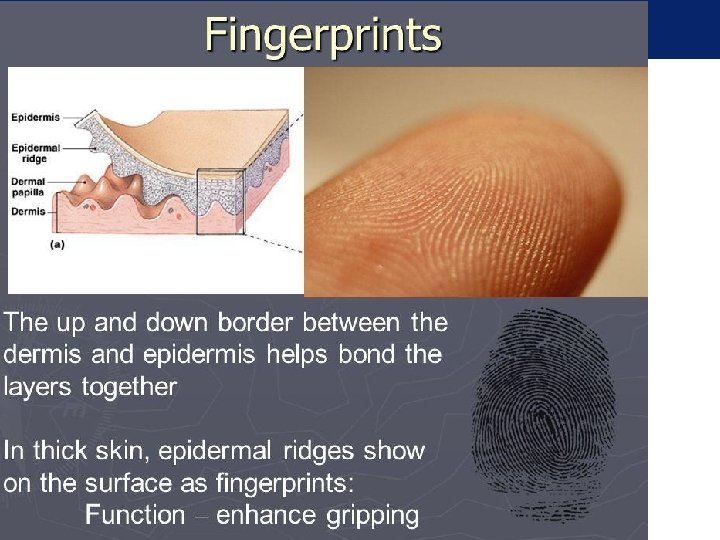
LAYERS OF THE DERMIS (from top down) • • • Papillary layer Most superficial layer of dermis consists of areolar CT with collagen and elastic fibers. Dermal papillae form dermal ridges that form our fingerprints, palm prints and footprints. Reticular layer 80 % of dermis - consist of dense irregular CT - named for its network (reticulum) of collagen fibers • Supports, nourishes epidermis • Provides sensory nerves, lymphatics, and capillaries *papillae = “little fingers”
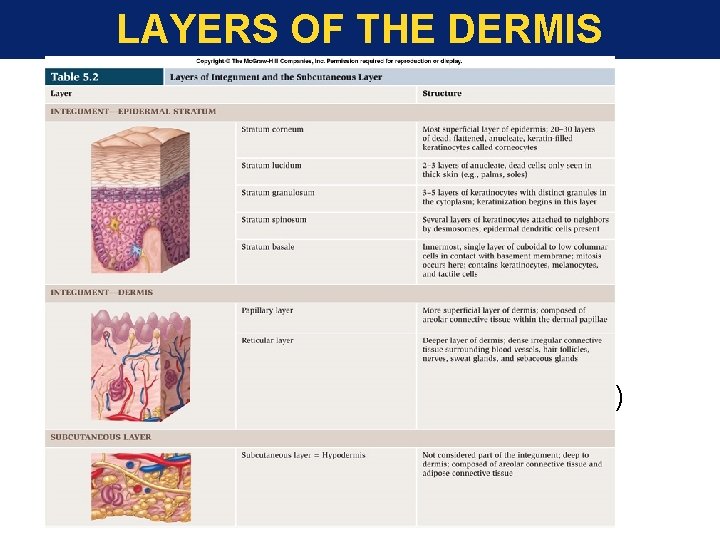
LAYERS OF THE DERMIS • Reticular layer • Tough, dense, fibrous layer • collagen fibers • limit stretch • elastin fibers • provide flexibility • blends into papillary layer (above) • blends into subcutaneous layer (below)
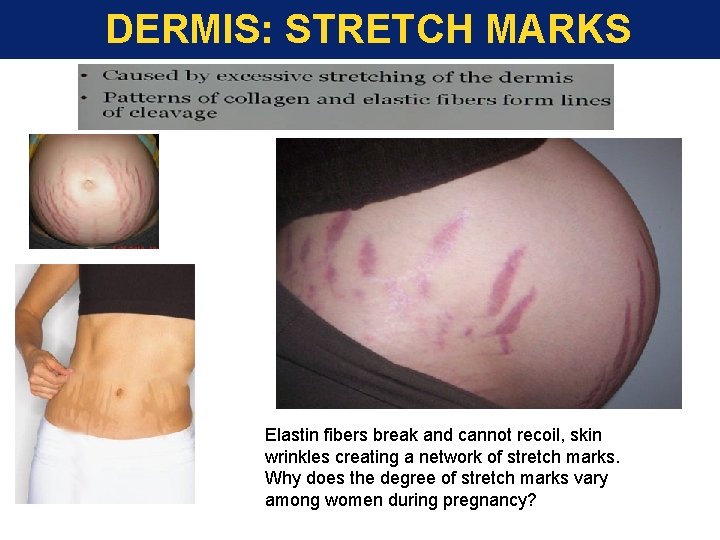
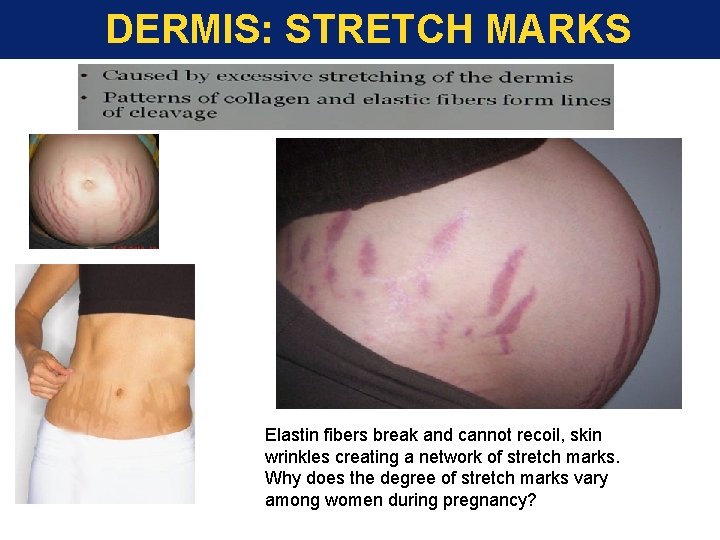
DERMIS: STRETCH MARKS Elastin fibers break and cannot recoil, skin wrinkles creating a network of stretch marks. Why does the degree of stretch marks vary among women during pregnancy?
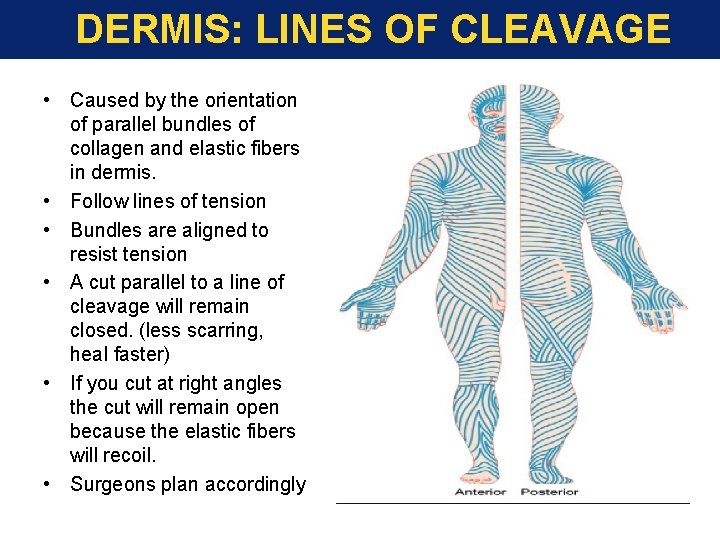
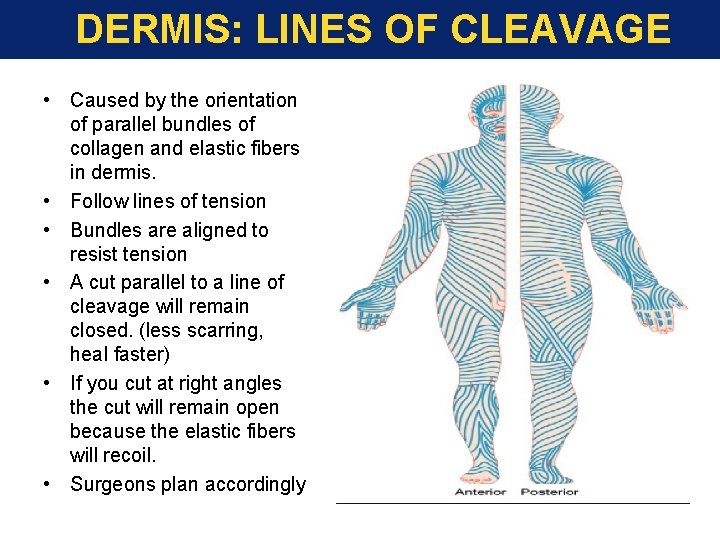
DERMIS: LINES OF CLEAVAGE • Caused by the orientation of parallel bundles of collagen and elastic fibers in dermis. • Follow lines of tension • Bundles are aligned to resist tension • A cut parallel to a line of cleavage will remain closed. (less scarring, heal faster) • If you cut at right angles the cut will remain open because the elastic fibers will recoil. • Surgeons plan accordingly
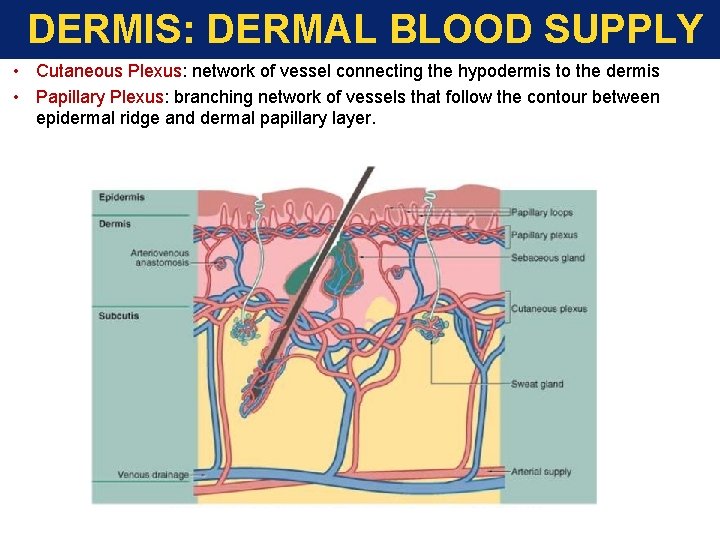
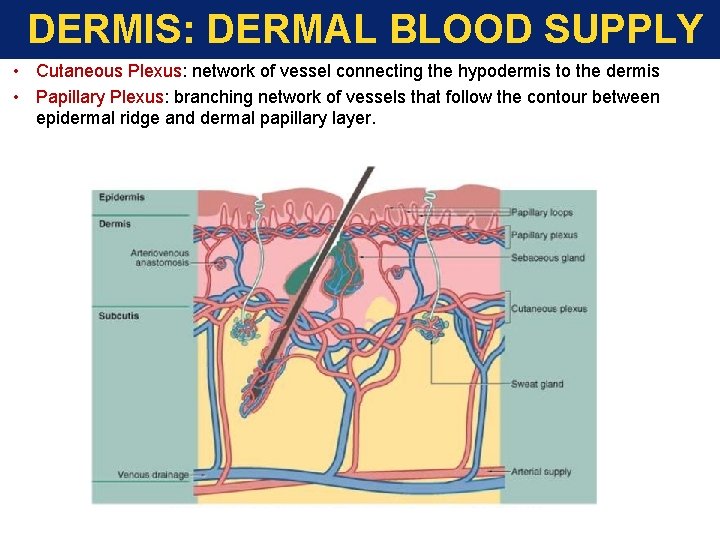
DERMIS: DERMAL BLOOD SUPPLY • Cutaneous Plexus: network of vessel connecting the hypodermis to the dermis • Papillary Plexus: branching network of vessels that follow the contour between epidermal ridge and dermal papillary layer.

DERMIS: DERMAL BLOOD SUPPLY Ulcer (bedsores)Chronic lack of circulation kills epidermal cells. Bacterial infections occur. If left untreated the dermal tissue will degenerate Necrosis- dermal tissue that has degenerated. Birthmarks: Capillary hemangioma, Cavernous hemangioma
DERMIS: STRUCTURE/FUNCTION Key Note The dermis provides mechanical strength, flexibility, and protection for underlying tissues. It is highly vascular (lots of blood vessels) and contains a variety of sensory receptors that provide information about the external environment.
THE SUBCUTANEOUS LAYER (HYPODERMIS) • Composed of loose connective tissue • Stabilizes skin position • Loosely attached to dermis above • Loosely attached to muscle below • Contains many fat cells (adipose tiss. ) • Provides thermal insulation • Cushions underlying muscle tissue. • Safely receives hypodermic needles • Also called “superficial fascia”
THE SUBCUTANEOUS LAYER (HYPODERMIS) Why are Babies Fat?
SKIN ACCESSORIES 1. Hair: (pilus/pili) derived from keratin 2. Glands: sebaceous and sweat (sudoriferous glands). 3. Nails: are produced from keratin
HAIR AND HAIR FOLLICLES Functions of hair • Warmth – less in man than other mammals • Sense light touch of the skin (Root Hair Plexus) • Protection – scalp from UV and blows to head • Prevent foreign particles from entering (nasal, ears, lashes) Parts • Root imbedded in skin • Shaft projecting above skin surface Make up of hair – hard keratin. Three concentric layers • Medulla (core) • Cortex (surrounds medulla) • Cuticle (single layers, overlapping)
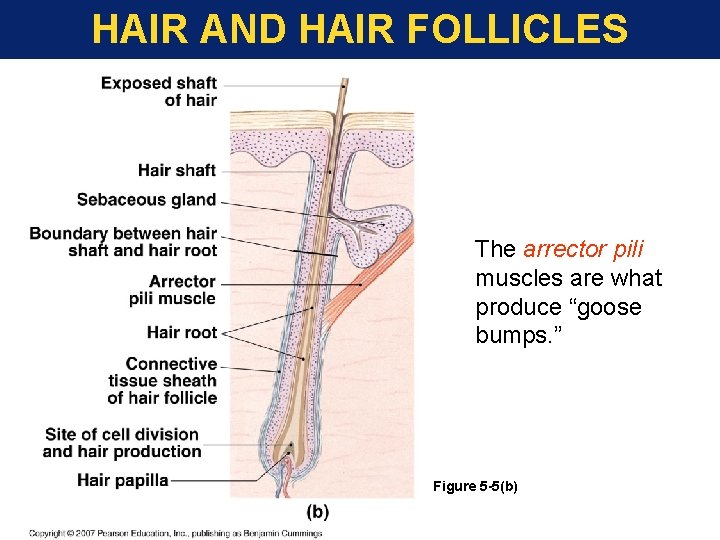
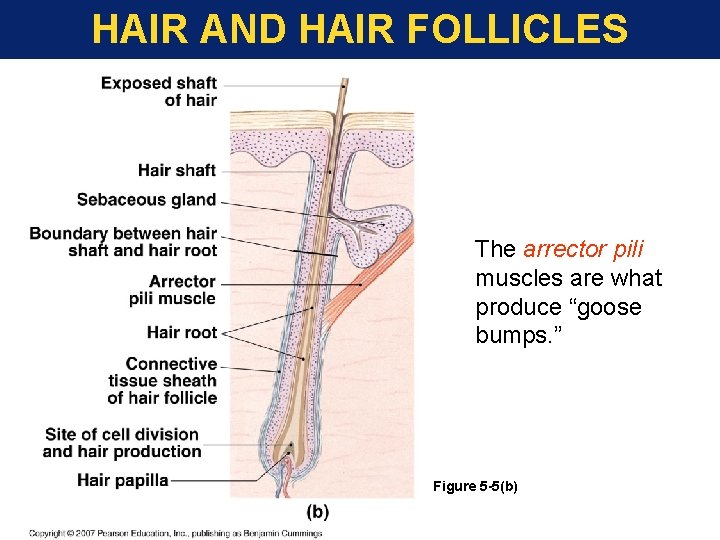
HAIR AND HAIR FOLLICLES The arrector pili muscles are what produce “goose bumps. ” Figure 5 -5(b)
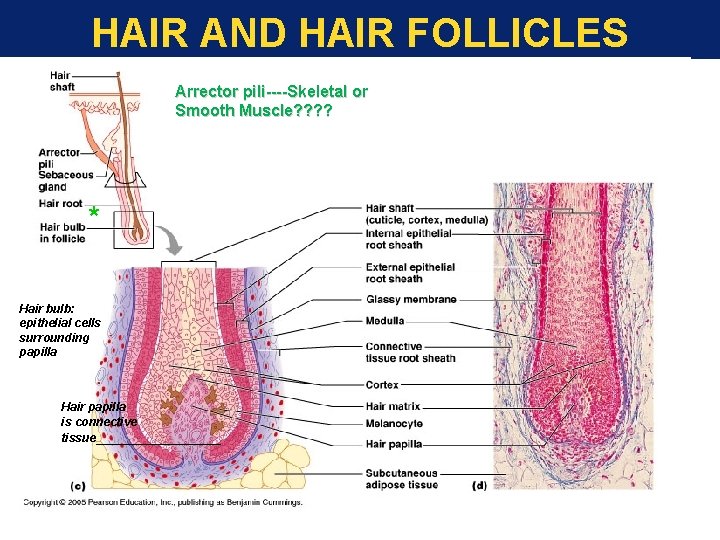
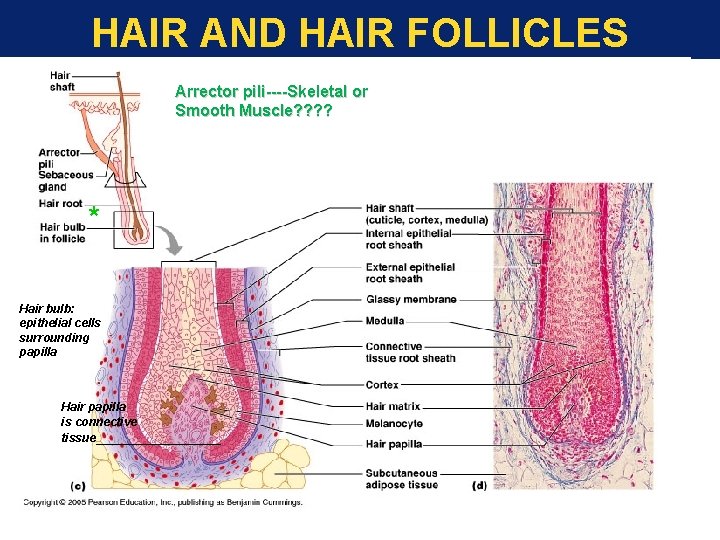
HAIR AND HAIR FOLLICLES Arrector pili----Skeletal or Smooth Muscle? ? * Hair bulb: epithelial cells surrounding papilla Hair papilla is connective tissue________
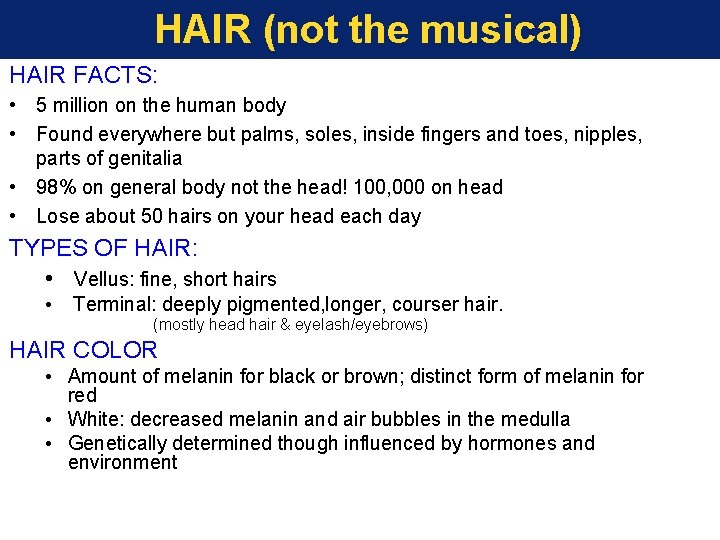
HAIR (not the musical) HAIR FACTS: • 5 million on the human body • Found everywhere but palms, soles, inside fingers and toes, nipples, parts of genitalia • 98% on general body not the head! 100, 000 on head • Lose about 50 hairs on your head each day TYPES OF HAIR: • Vellus: fine, short hairs • Terminal: deeply pigmented, longer, courser hair. (mostly head hair & eyelash/eyebrows) HAIR COLOR • Amount of melanin for black or brown; distinct form of melanin for red • White: decreased melanin and air bubbles in the medulla • Genetically determined though influenced by hormones and environment
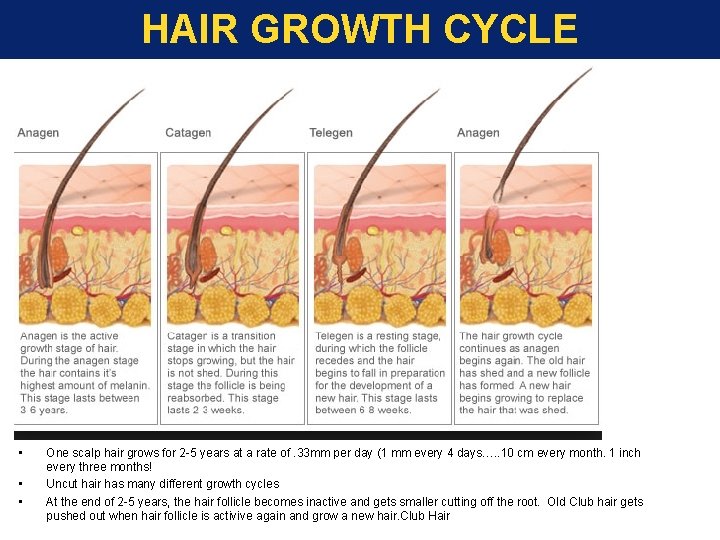
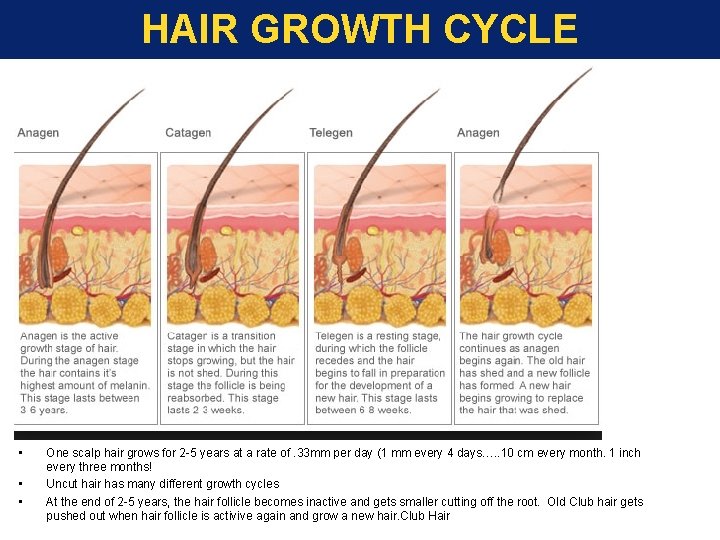
HAIR GROWTH CYCLE • • • One scalp hair grows for 2 -5 years at a rate of. 33 mm per day (1 mm every 4 days…. . 10 cm every month. 1 inch every three months! Uncut hair has many different growth cycles At the end of 2 -5 years, the hair follicle becomes inactive and gets smaller cutting off the root. Old Club hair gets pushed out when hair follicle is activive again and grow a new hair. Club Hair
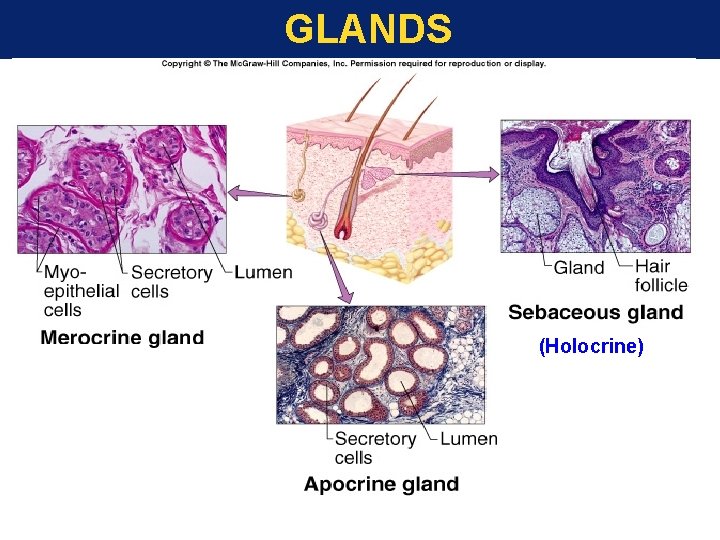
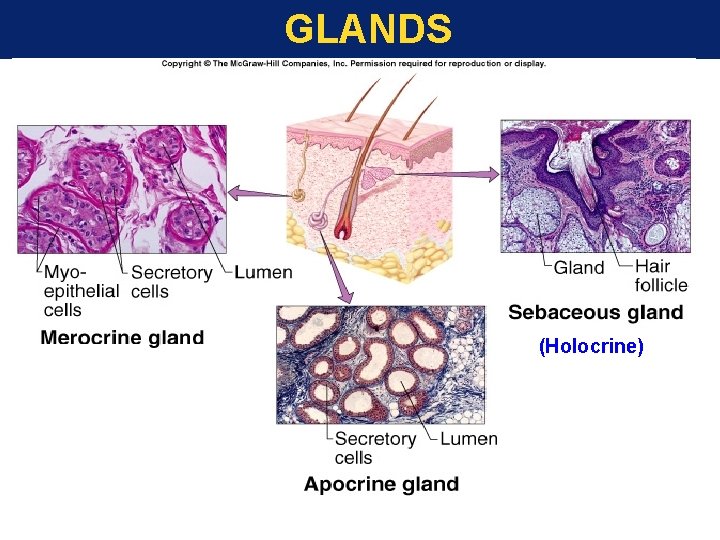
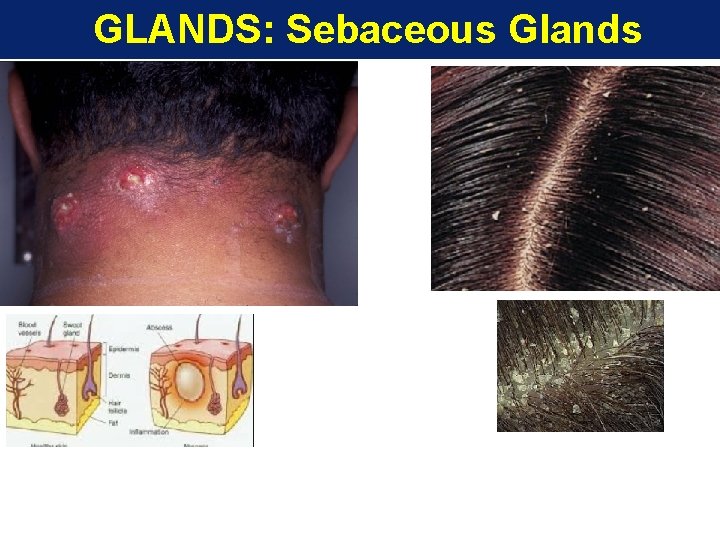
GLANDS (Holocrine)
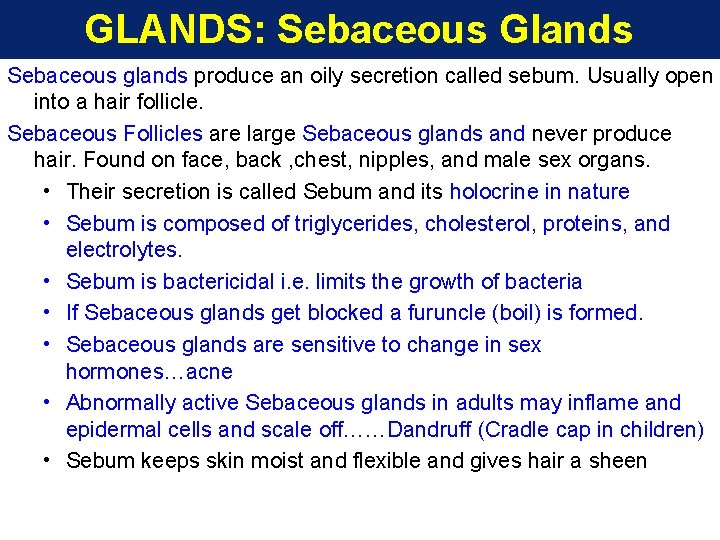
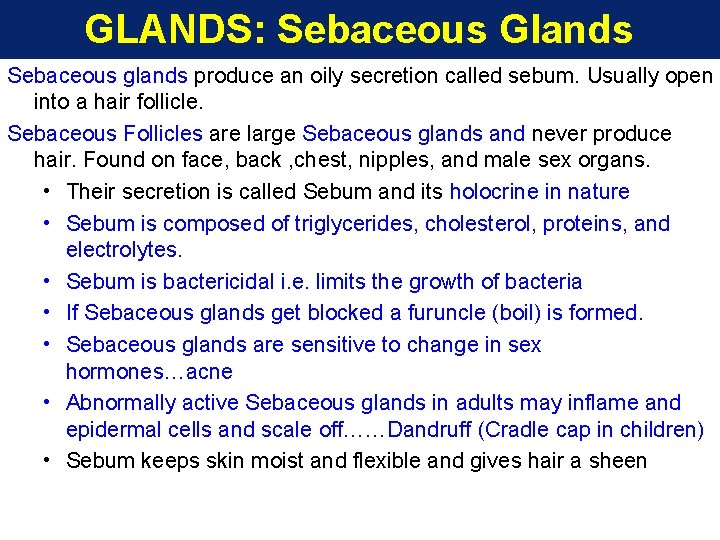
GLANDS: Sebaceous Glands Sebaceous glands produce an oily secretion called sebum. Usually open into a hair follicle. Sebaceous Follicles are large Sebaceous glands and never produce hair. Found on face, back , chest, nipples, and male sex organs. • Their secretion is called Sebum and its holocrine in nature • Sebum is composed of triglycerides, cholesterol, proteins, and electrolytes. • Sebum is bactericidal i. e. limits the growth of bacteria • If Sebaceous glands get blocked a furuncle (boil) is formed. • Sebaceous glands are sensitive to change in sex hormones…acne • Abnormally active Sebaceous glands in adults may inflame and epidermal cells and scale off……Dandruff (Cradle cap in children) • Sebum keeps skin moist and flexible and gives hair a sheen
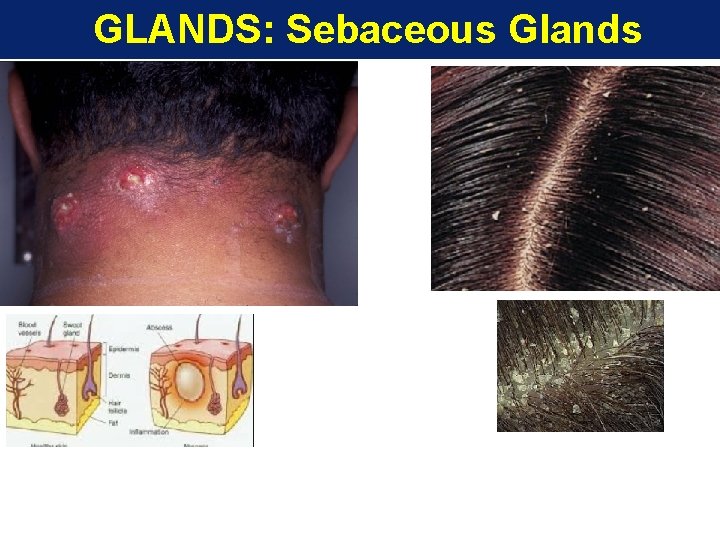
GLANDS: Sebaceous Glands
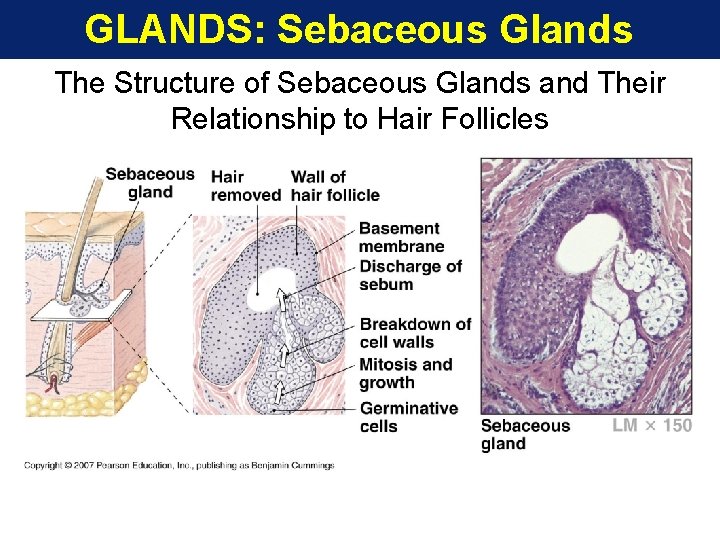
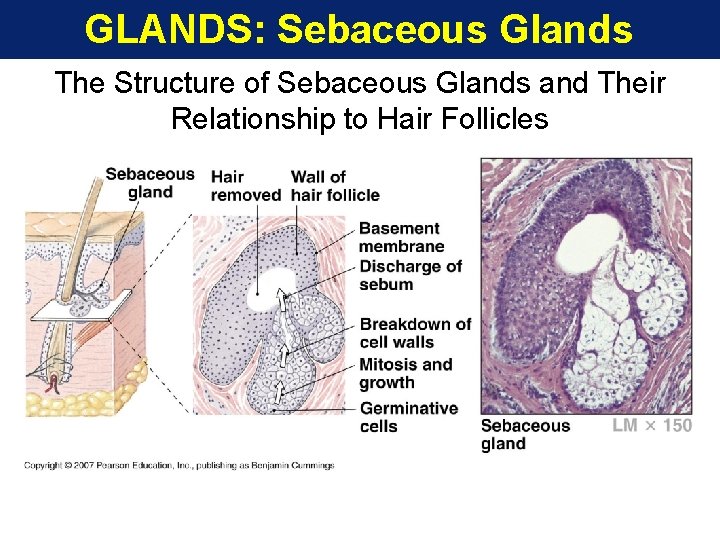
GLANDS: Sebaceous Glands The Structure of Sebaceous Glands and Their Relationship to Hair Follicles
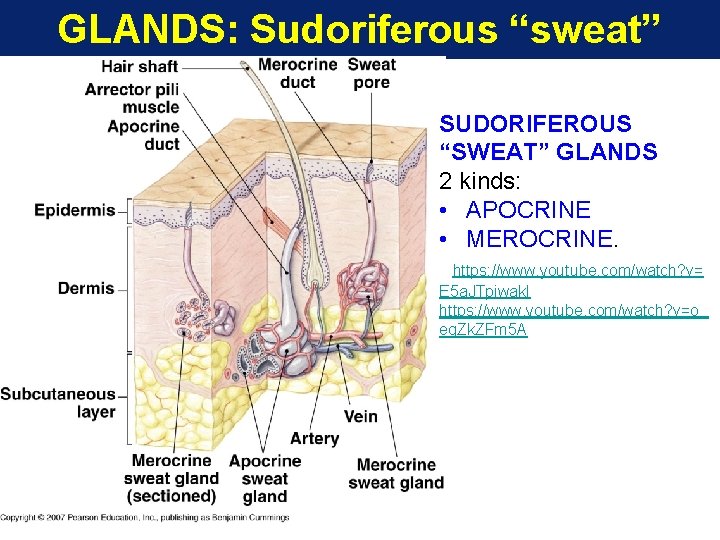
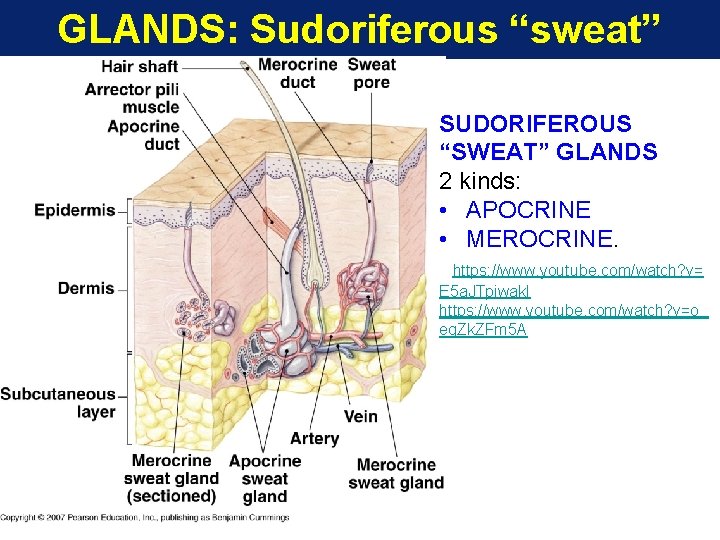
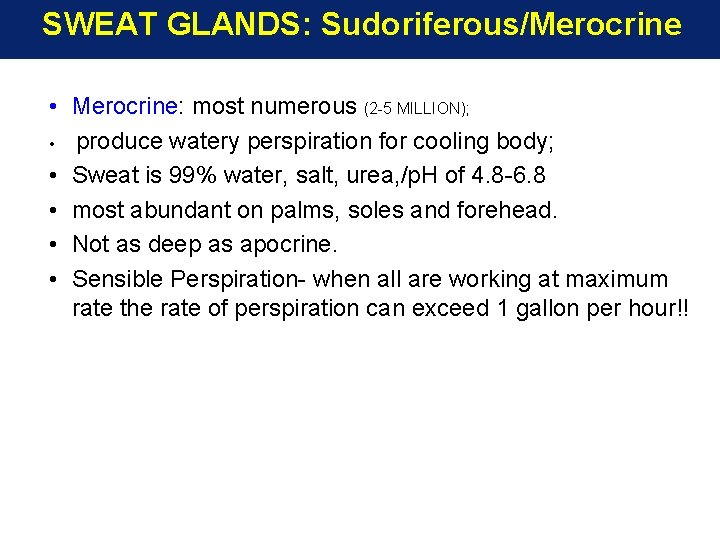
GLANDS: Sudoriferous “sweat” glands SUDORIFEROUS “SWEAT” GLANDS 2 kinds: • APOCRINE • MEROCRINE. https: //www. youtube. com/watch? v= E 5 a. JTpiwak. I https: //www. youtube. com/watch? v=o_ eq. Zk. ZFm 5 A Figure 5 -7
SWEAT GLANDS: Sudoriferous/Merocrine • Merocrine: most numerous (2 -5 MILLION); • produce watery perspiration for cooling body; • Sweat is 99% water, salt, urea, /p. H of 4. 8 -6. 8 • most abundant on palms, soles and forehead. • Not as deep as apocrine. • Sensible Perspiration- when all are working at maximum rate the rate of perspiration can exceed 1 gallon per hour!!
SWEAT GLANDS: Sudoriferous/Apocrine Sudoriferous “sweat” glands – are of 2 kinds; apocrine and merocrine Apocrine: • Present in groin, axilla, anal, areola, and beard regions; • Ducts open into hair follicle; • Sweat is thicker milkier due to fatty acids. • Nutrient rich for bacteria. • Strong odor is due to bacterial decay. • Scent glands that respond to stress and sexual stimulation • Become fully functional at puberty. • Open into hair follicles
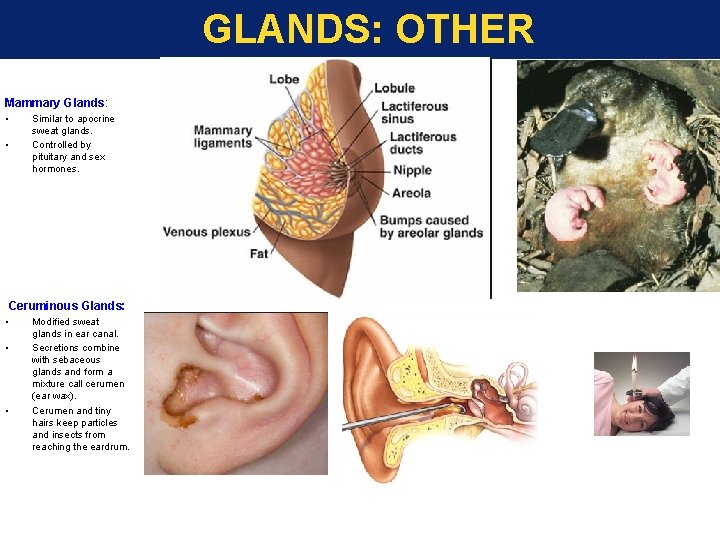
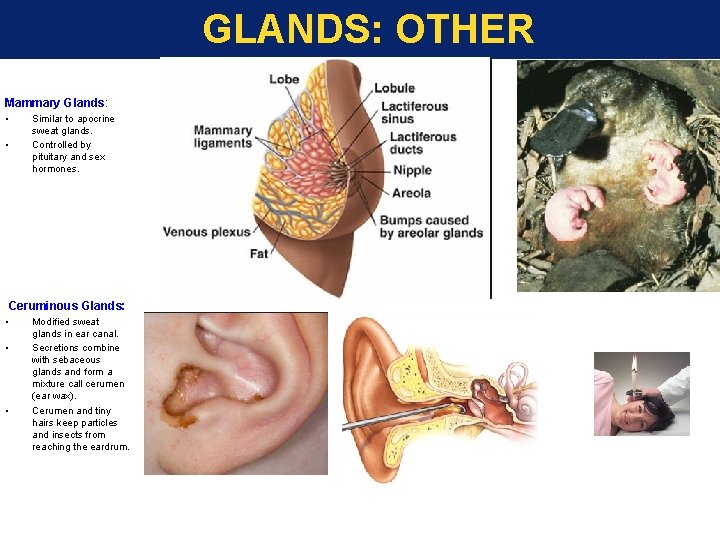
GLANDS: OTHER Mammary Glands: • • Similar to apocrine sweat glands. Controlled by pituitary and sex hormones. Ceruminous Glands: • • • Modified sweat glands in ear canal. Secretions combine with sebaceous glands and form a mixture call cerumen (ear wax). Cerumen and tiny hairs keep particles and insects from reaching the eardrum.
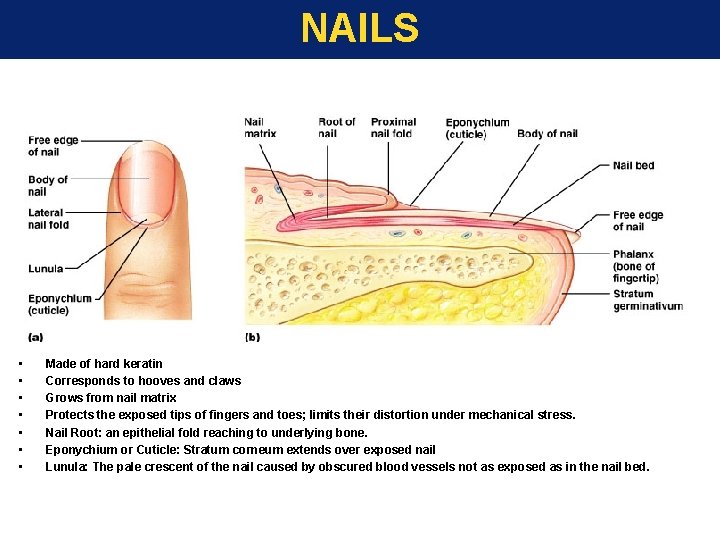
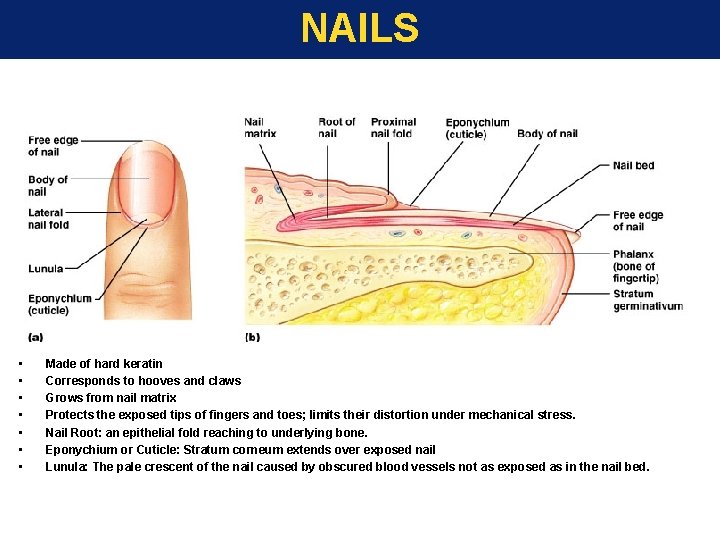
NAILS • • Made of hard keratin Corresponds to hooves and claws Grows from nail matrix Protects the exposed tips of fingers and toes; limits their distortion under mechanical stress. Nail Root: an epithelial fold reaching to underlying bone. Eponychium or Cuticle: Stratum corneum extends over exposed nail Lunula: The pale crescent of the nail caused by obscured blood vessels not as exposed as in the nail bed.
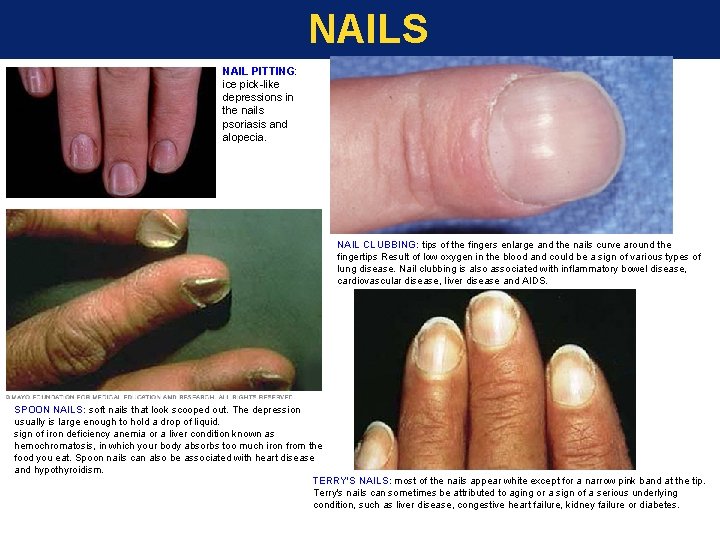
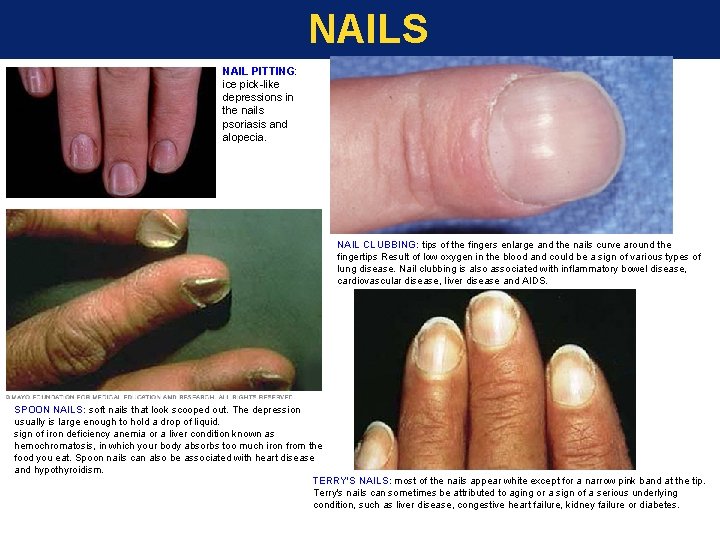
NAILS NAIL PITTING: ice pick-like depressions in the nails psoriasis and alopecia. NAIL CLUBBING: tips of the fingers enlarge and the nails curve around the fingertips Result of low oxygen in the blood and could be a sign of various types of lung disease. Nail clubbing is also associated with inflammatory bowel disease, cardiovascular disease, liver disease and AIDS. SPOON NAILS: soft nails that look scooped out. The depression usually is large enough to hold a drop of liquid. sign of iron deficiency anemia or a liver condition known as hemochromatosis, in which your body absorbs too much iron from the food you eat. Spoon nails can also be associated with heart disease and hypothyroidism. TERRY'S NAILS: most of the nails appear white except for a narrow pink band at the tip. Terry's nails can sometimes be attributed to aging or a sign of a serious underlying condition, such as liver disease, congestive heart failure, kidney failure or diabetes.
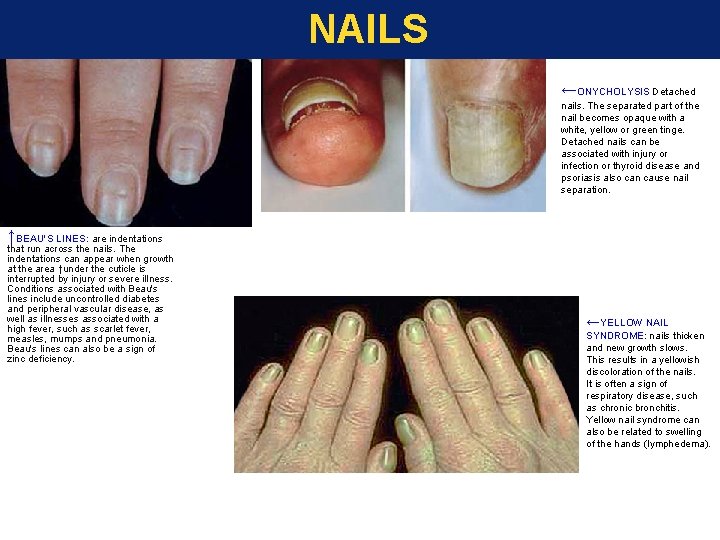
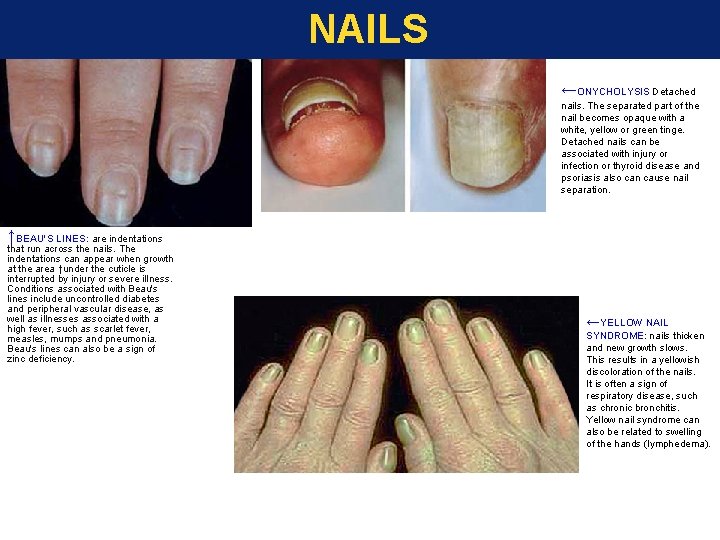
NAILS ←ONYCHOLYSIS Detached nails. The separated part of the nail becomes opaque with a white, yellow or green tinge. Detached nails can be associated with injury or infection or thyroid disease and psoriasis also can cause nail separation. ↑BEAU'S LINES: are indentations that run across the nails. The indentations can appear when growth at the area ↑under the cuticle is interrupted by injury or severe illness. Conditions associated with Beau's lines include uncontrolled diabetes and peripheral vascular disease, as well as illnesses associated with a high fever, such as scarlet fever, measles, mumps and pneumonia. Beau's lines can also be a sign of zinc deficiency. ←YELLOW NAIL SYNDROME: nails thicken and new growth slows. This results in a yellowish discoloration of the nails. It is often a sign of respiratory disease, such as chronic bronchitis. Yellow nail syndrome can also be related to swelling of the hands (lymphedema).
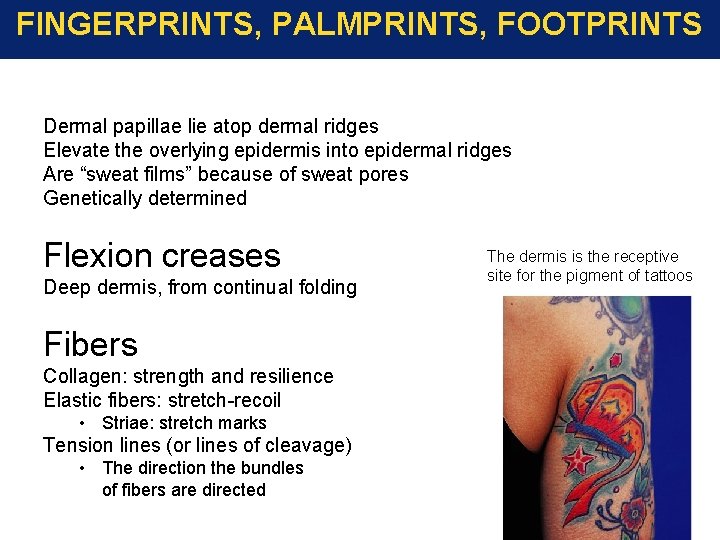
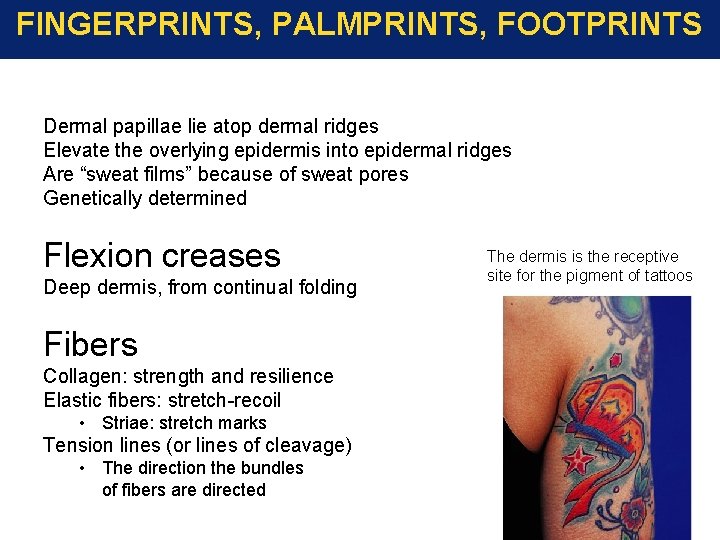
FINGERPRINTS, PALMPRINTS, FOOTPRINTS Dermal papillae lie atop dermal ridges Elevate the overlying epidermis into epidermal ridges Are “sweat films” because of sweat pores Genetically determined Flexion creases Deep dermis, from continual folding Fibers Collagen: strength and resilience Elastic fibers: stretch-recoil • Striae: stretch marks Tension lines (or lines of cleavage) • The direction the bundles of fibers are directed The dermis is the receptive site for the pigment of tattoos
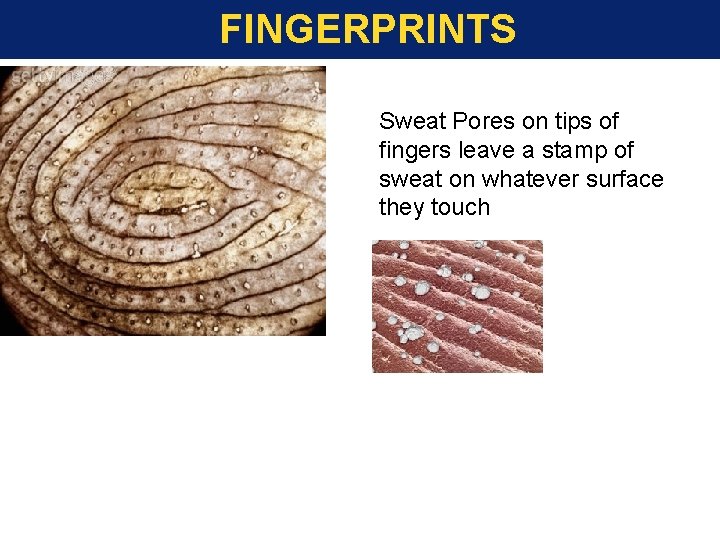
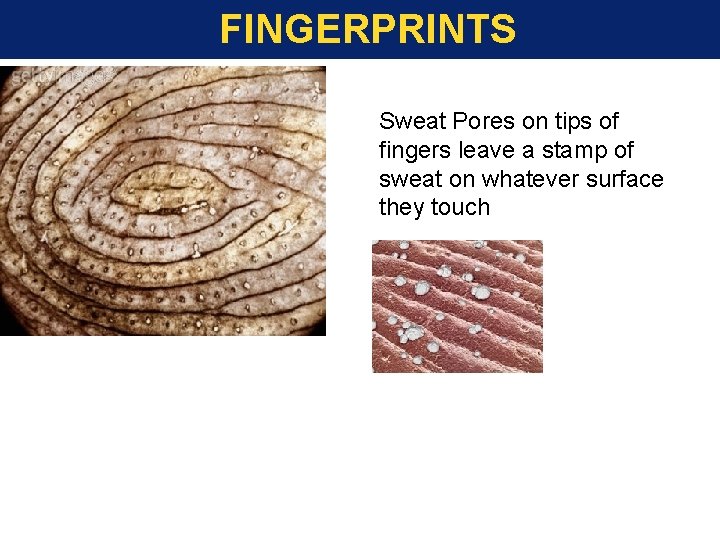
FINGERPRINTS Sweat Pores on tips of fingers leave a stamp of sweat on whatever surface they touch
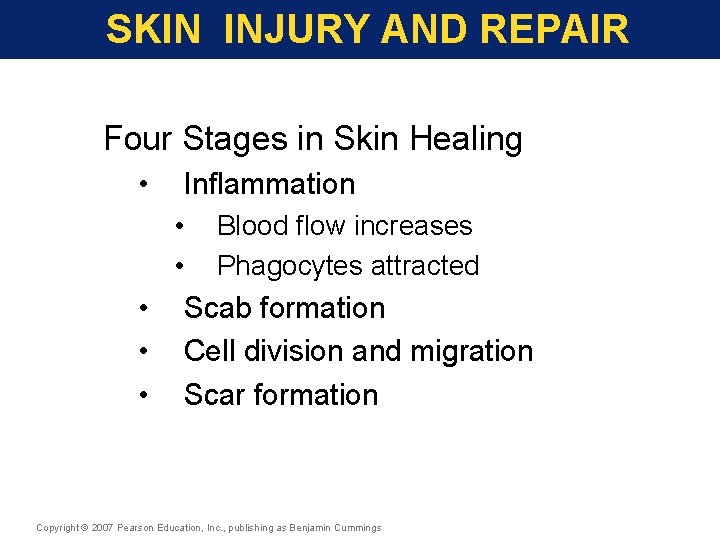
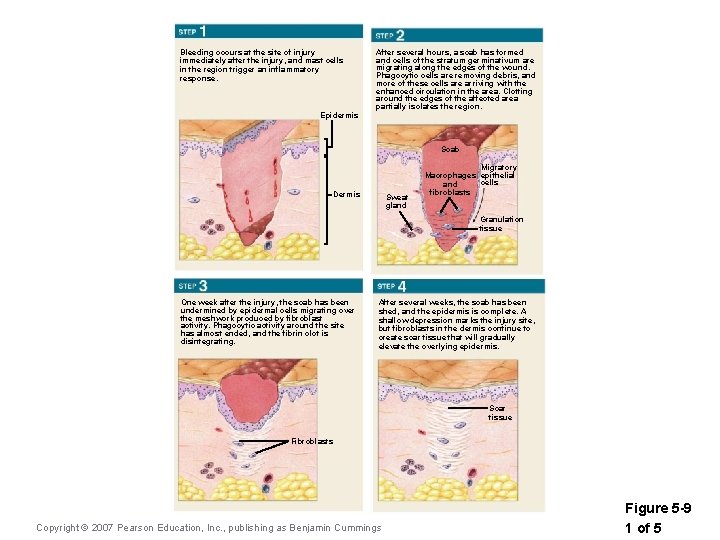
SKIN INJURY AND REPAIR Four Stages in Skin Healing • Inflammation • • • Blood flow increases Phagocytes attracted Scab formation Cell division and migration Scar formation Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings
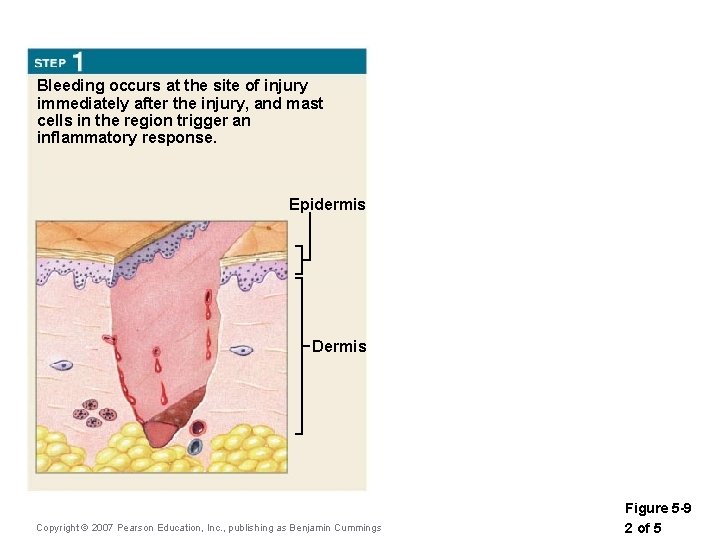
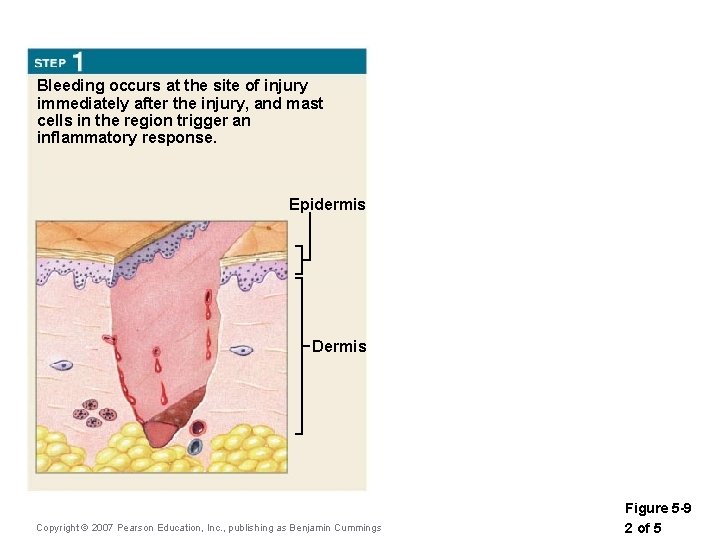
Bleeding occurs at the site of injury immediately after the injury, and mast cells in the region trigger an inflammatory response. Epidermis Dermis Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 5 -9 2 of 5
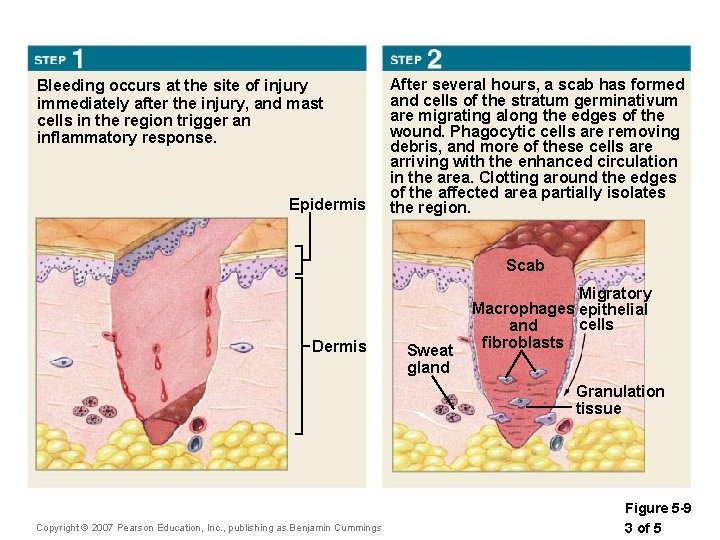
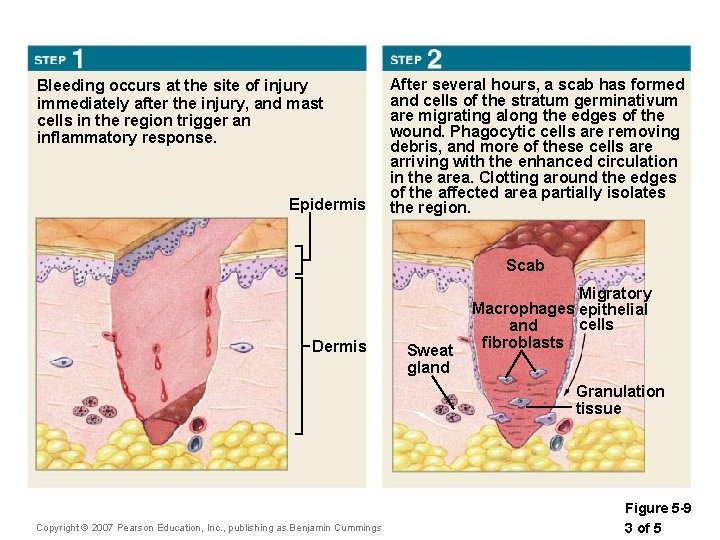
Bleeding occurs at the site of injury immediately after the injury, and mast cells in the region trigger an inflammatory response. Epidermis After several hours, a scab has formed and cells of the stratum germinativum are migrating along the edges of the wound. Phagocytic cells are removing debris, and more of these cells are arriving with the enhanced circulation in the area. Clotting around the edges of the affected area partially isolates the region. Scab Dermis Sweat gland Migratory Macrophages epithelial cells and fibroblasts Granulation tissue Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 5 -9 3 of 5
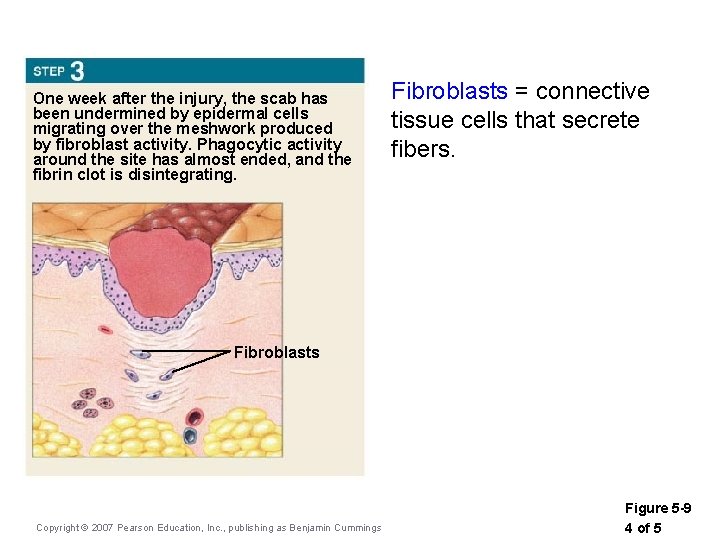
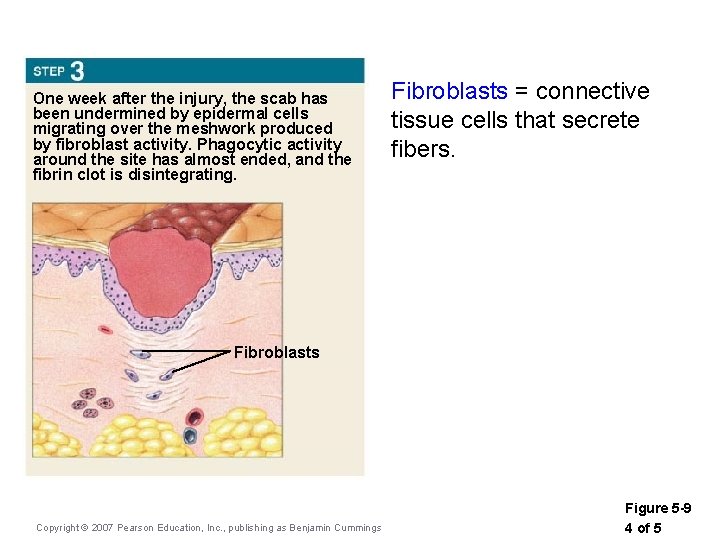
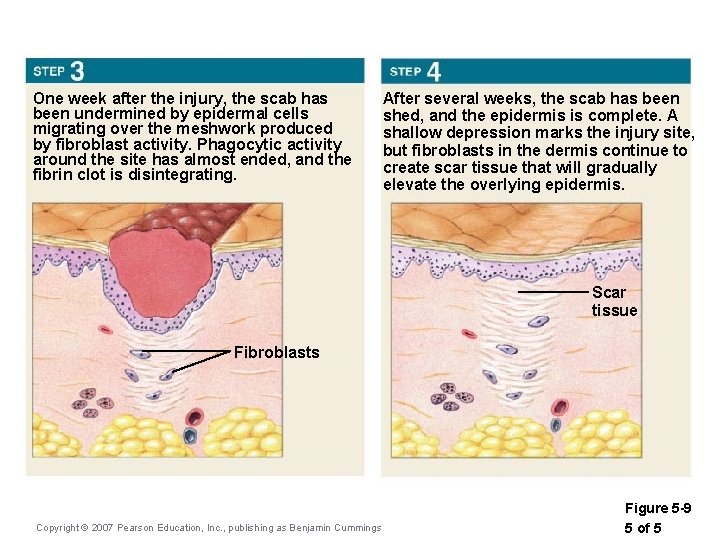
One week after the injury, the scab has been undermined by epidermal cells migrating over the meshwork produced by fibroblast activity. Phagocytic activity around the site has almost ended, and the fibrin clot is disintegrating. Fibroblasts = connective tissue cells that secrete fibers. Fibroblasts Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 5 -9 4 of 5
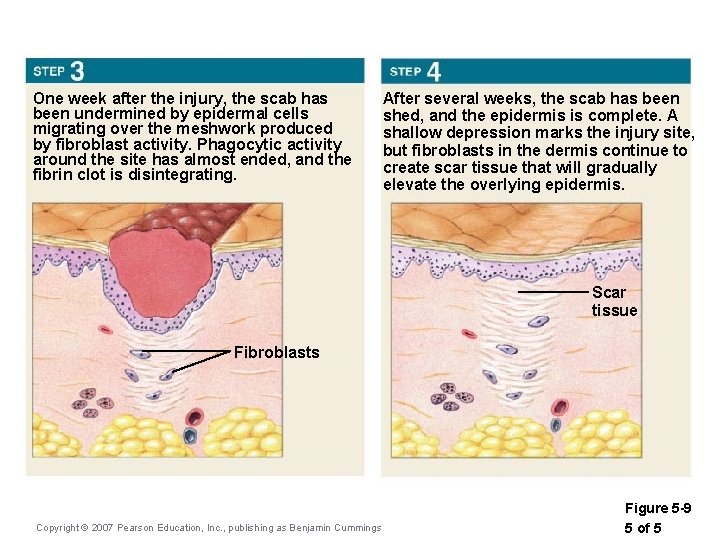
One week after the injury, the scab has been undermined by epidermal cells migrating over the meshwork produced by fibroblast activity. Phagocytic activity around the site has almost ended, and the fibrin clot is disintegrating. After several weeks, the scab has been shed, and the epidermis is complete. A shallow depression marks the injury site, but fibroblasts in the dermis continue to create scar tissue that will gradually elevate the overlying epidermis. Scar tissue Fibroblasts Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 5 -9 5 of 5
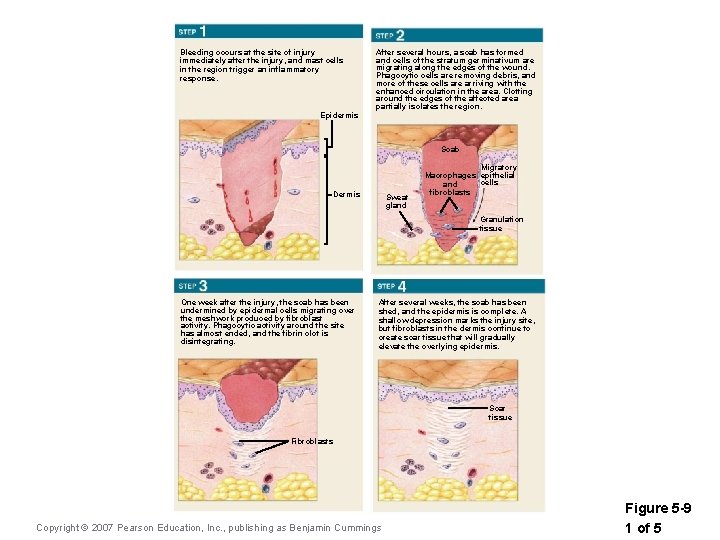
Bleeding occurs at the site of injury immediately after the injury, and mast cells in the region trigger an inflammatory response. After several hours, a scab has formed and cells of the stratum germinativum are migrating along the edges of the wound. Phagocytic cells are removing debris, and more of these cells are arriving with the enhanced circulation in the area. Clotting around the edges of the affected area partially isolates the region. Epidermis Scab Dermis Sweat gland Migratory Macrophages epithelial cells and fibroblasts Granulation tissue One week after the injury, the scab has been undermined by epidermal cells migrating over the meshwork produced by fibroblast activity. Phagocytic activity around the site has almost ended, and the fibrin clot is disintegrating. After several weeks, the scab has been shed, and the epidermis is complete. A shallow depression marks the injury site, but fibroblasts in the dermis continue to create scar tissue that will gradually elevate the overlying epidermis. Scar tissue Fibroblasts Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 5 -9 1 of 5
BOZEMAN : //www. youtube. com/watch? v=z 5 Vn. OS 9 Ke 3 g