Integration of Viral Hepatitis Prevention with STD Prevention




- Slides: 15
Integration of Viral Hepatitis Prevention with STD Prevention: What Health Professionals Should Know Presenter: Jay Todd, Training and Public Education Branch Manager Texas Department of Health Contributor: Brigette Ulin Centers for Disease Control and Prevention

Objectives • Describe the Components of Texas House Bill 1652 • Outline Activities of the Texas Department of Health to Implement HB 1652 – Professional and Public Education on Hepatitis C – Hepatitis C Seroprevalence Studies – Counseling and Testing for Hepatitis C • Discuss Lessons Learned
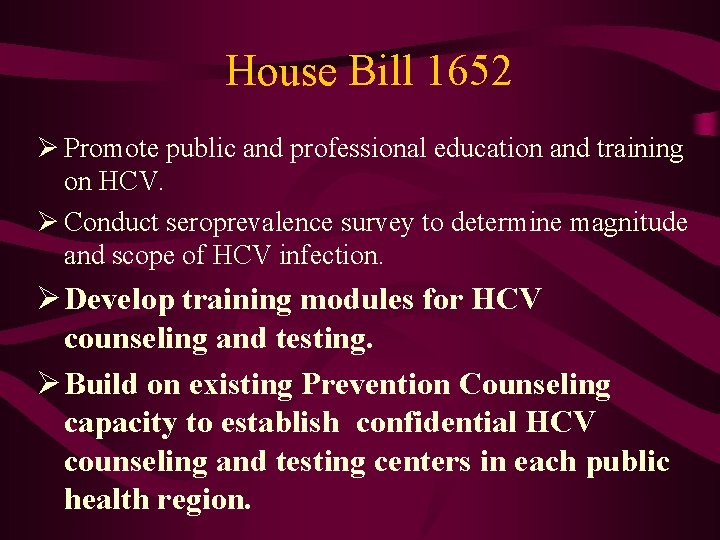
House Bill 1652 Ø Promote public and professional education and training on HCV. Ø Conduct seroprevalence survey to determine magnitude and scope of HCV infection. Ø Develop training modules for HCV counseling and testing. Ø Build on existing Prevention Counseling capacity to establish confidential HCV counseling and testing centers in each public health region.
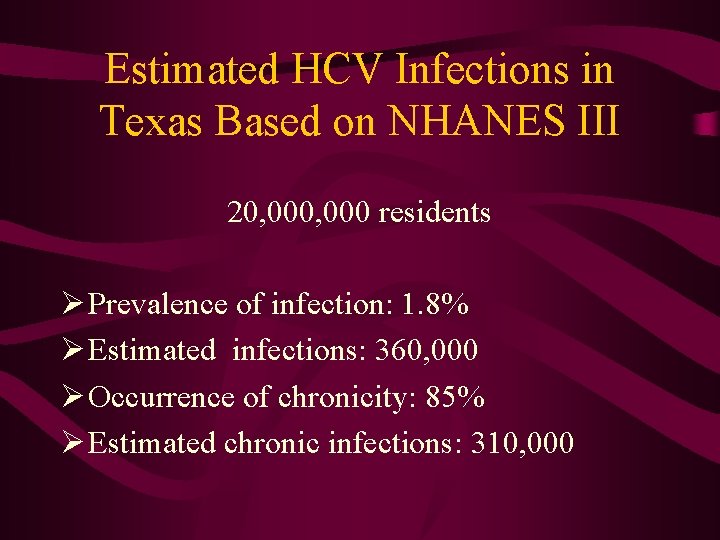
Estimated HCV Infections in Texas Based on NHANES III 20, 000 residents Ø Prevalence of infection: 1. 8% Ø Estimated infections: 360, 000 Ø Occurrence of chronicity: 85% Ø Estimated chronic infections: 310, 000
Limited Funds= Limited Counseling and Testing • Balanced four concerns – Where IDU are tested – Ability to draw blood – Some clinic presence – Easily accessible by the general public • Selected 25 sites across Texas • Created supplemental data collection form
Preparing for Counseling and Testing. What needed to be Developed? • Selecting locations/sites for HCV Counseling and Testing • Precourse materials • Training course materials • Counseling and testing guidelines – Focused intervention on IDU, medical exposures, unsafe tattoos, risky sexual behavior, sharing snorting equipment

Preliminary Site Selection • Agencies that work with IDU population • At least one site in every Public Health Region (8 regions) • Access for walk-in testing and counseling • Ability and capacity to draw blood
Development of Guidelines • Developed HCV counseling and testing guidelines to target limited resources to those at highest risk • Who to test? ØEasy call – IDU; recipients of a blood transfusion before 1992, blood products, solid organ transplants; medical exposure etc. ØDifficult call - unsafe tattoos, risky sexual behavior, sharing snorting equipment Gather data on difficult risk factors Let counselor make the difficult call

Counseling and Testing Guidelines • Developed hepatitis C counseling and testing guidelines to target limited resources to those a highest risk • Focused intervention on IDU, medical exposures, unsafe tattoos, and risky sexual behavior
Guidelines--Test persons who: • Have received clotting factor concentrates manufactured before 1987. • Ever shared needles or works. • Ever received hemodialysis (kidney dialysis). • Received a transfusion or organ transplant, before July 1992. • Health care workers who received needle stick from a contaminated sharp, or had a mucosal exposure from a HCV infected client. • Are born to HCV infected women. • Are HIV infected • Have tattoos or body piercing done in unsanitary conditions
Guidelines: Test if Resources Permit • Persons with a history of 50 or more lifetime sex partners. • Long-term sex partners of HCV-positive persons. • Sex partners of injecting drug users. • Persons reporting a history of sexually transmitted diseases. • Recipients of transplanted tissue. • Intra nasal cocaine (sharing straws) and other noninjecting illegal drug users.
Counselor Training • Developed pre-course materials on viral hepatitis and HCV specifically • Developed special 1 -day update on HCV that was delivered to staff of selected counseling and testing sites in the Fall of 2000 • Integrated discussion of HCV Counseling and Testing into current Prevention Counseling Partner Elicitation (PCPE) training for new counselors • Developed vignettes to show to integrate HCV into existing HIV counseling and testing • Materials http: //www. tdh. state. tx. us/hivstd/educate/hepc/

One-day Training • Knowledge Assessment based on two pre-course modules • Review of counseling skills and concepts • Viral hepatitis risk factors • Role plays – Transitioning to HCV risk from discussion of HIV risk – Providing positive HCV results
Number of persons tested • October 1, 2000 - September 30, 2003 – 54, 282 specimens submitted for HCV testing – 12, 933 HCV reactive EIA tests – Testing dollars were available through TDH until December 2003. Currently, no additional funding is available. Limited sites are continuing to offer HCV testing through other funding sources.
Lessons Viral hepatitis prevention messages can be integrated into existing HIV/STD prevention messages quite easily However…. • HCV counseling is resource intensive • HCV counseling staff require support – Greater number of positives – Fewer certainties about treatment and resources
 Hgado
Hgado Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention Itil wikipedia fr
Itil wikipedia fr The dynamics of viral marketing
The dynamics of viral marketing Viral inoculation in embryonated egg
Viral inoculation in embryonated egg An acute highly contagious viral disease
An acute highly contagious viral disease Vaccins à vecteur viral
Vaccins à vecteur viral Decapsidação
Decapsidação Eline's viral
Eline's viral Section 24-1 viral structure and replication
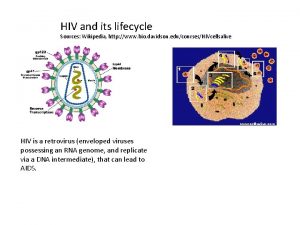
Section 24-1 viral structure and replication Virus dna
Virus dna Capsid capsomere
Capsid capsomere Csf meningitis
Csf meningitis Cultivation of viruses
Cultivation of viruses Viral life cycle
Viral life cycle Viral receptors
Viral receptors