Integrating the Osteopathic Structural Exam into the Physical

- Slides: 21
Integrating the Osteopathic Structural Exam into the Physical Diagnosis Practical Aubrey M. Olson, D. O. , M. S. Ed. Rebecca Moore, D. O. Danielle Cooley, D. O.
Objectives • Discuss the importance of incorporating the Osteopathic Structural exam into the general physical exam. • Describe the implementation of the Osteopathic structural exam into the general physical exam. • Examine the relevance for integrating the Osteopathic structural exam into the Physical Exam with regard to COMLEX PE and ACGME’s Osteopathic Neuromuscular Medicine Milestone Project in the unified pathway.
Background • The Osteopathic structural exam is often not included in physical examination training • Students struggle to incorporate both exams into patient care • Incorporation is critical for success in the Comlex PE
Why does this matter? As per AACOM’s Osteopathic Core Competencies for Medical Students, which sets the guidelines for Osteopathic Medical education: • Under section III Patient Care, a medical student must: – 3 a. Perform a clinically appropriate standard physical examination, including evaluation of each of the body areas (i. e. , head, neck, chest; abdomen; genitalia/groin/buttocks; back, including spine; upper and lower extremities) and organ systems (constitutional; cardiovascular; ears, nose, mouth and throat; eyes; genitourinary (female and male); hematologic/lymphatic/immunological; musculoskeletal; neurological; psychiatric; respiratory; skin). – 3 b. Perform an osteopathic structural examination and osteopathic manipulative therapy as appropriate.

Why this matters (continued) • The National Board of Medical Examiners-- Fundamental Osteopathic Medical Competency Domains: Guidelines for Osteopathic Medical Licensure and the Practice of Osteopathic Medicine • Osteopathic medical students are required to integrate all aspects of the physical exam, including the Osteopathic structural exam, into patient care • Students are at a distinct disadvantage when taught separately
Our Goal • Integrate the Osteopathic structural exam into physical diagnosis • Utilize educators from both the Osteosciences Department and the Family Medicine Departments • Interdisciplinary approach to teach the incorporated examination in both courses • Parallel teaching to help with student facilitation and integration into the incorporated exam
The Challenges • The Osteosciences and Family Medicine Departments were isolated in teaching their own courses • Didactics follow systems-based general curriculum • Courses were taught independently of each other • Limited resources: – Class size of 168 – Standardized patient laboratory with 10 examination rooms – 9 hours exam sessions for practical exams • Student performance on CSCE (Mock COMLEX PE) and COMLEX PE were not reflective of student’s ability to integrate both components into a patient encounter
How we changed the discussion • On Doctoring (physical diagnosis): – All lecturers include a slide of Osteopathic Considerations – Laboratory sessions include osteopathic structural exam considerations and treatment • OMM: table trainers discuss where the structural exam fits into the patient encounter • Physical Diagnosis Practical: rubric now includes aspects of Osteopathic Structural Exam • OMM Practical: now includes professionalism and interpersonal communications
On Doctoring Documentation and Osteopathic Structural Exam Slide: • Review of Systems • including all pertinent ROS for the body system presented • Documentation of exam finding • Normal & abnormal • Osteopathic Structural Exam • Structural exam findings • Chapman’s points
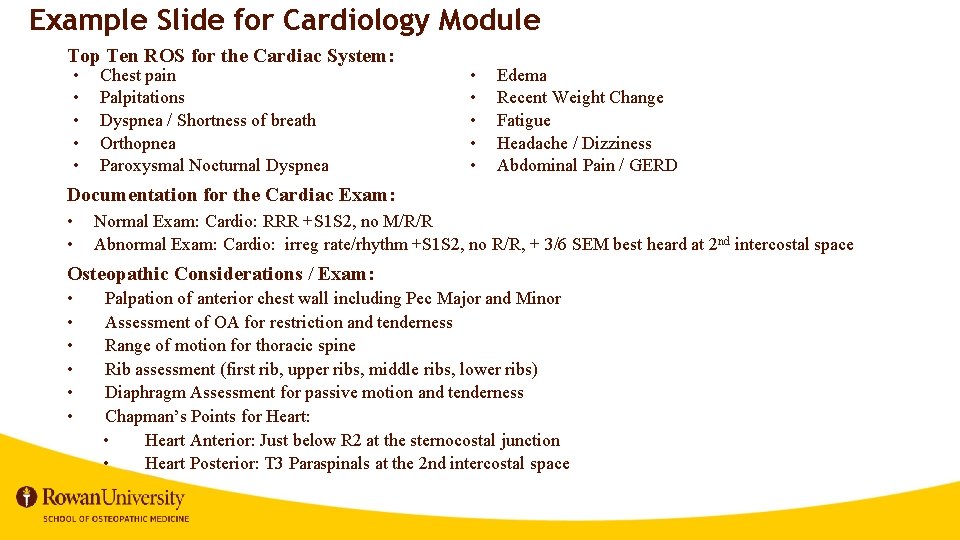
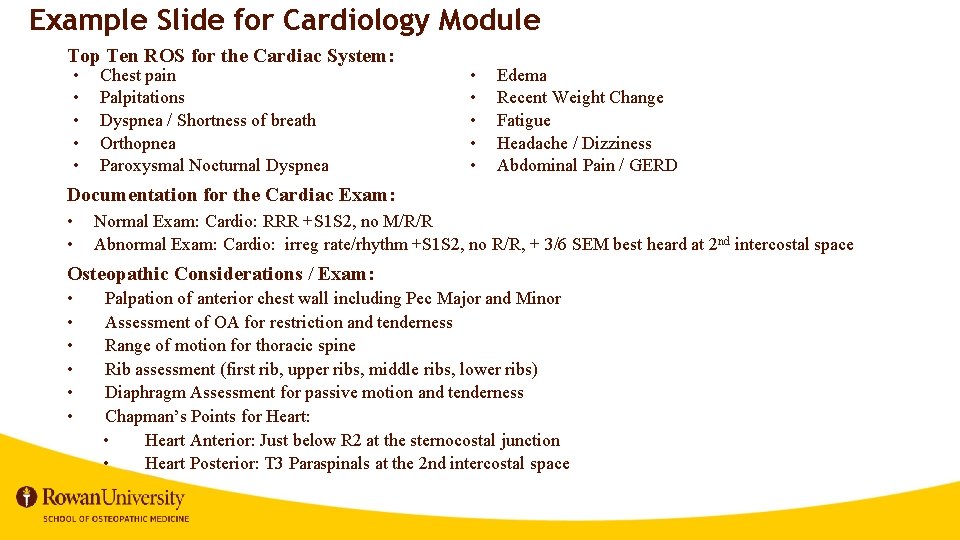
Example Slide for Cardiology Module Top Ten ROS for the Cardiac System: • • • Chest pain Palpitations Dyspnea / Shortness of breath Orthopnea Paroxysmal Nocturnal Dyspnea • • • Edema Recent Weight Change Fatigue Headache / Dizziness Abdominal Pain / GERD Documentation for the Cardiac Exam: • • Normal Exam: Cardio: RRR +S 1 S 2, no M/R/R Abnormal Exam: Cardio: irreg rate/rhythm +S 1 S 2, no R/R, + 3/6 SEM best heard at 2 nd intercostal space Osteopathic Considerations / Exam: • • • Palpation of anterior chest wall including Pec Major and Minor Assessment of OA for restriction and tenderness Range of motion for thoracic spine Rib assessment (first rib, upper ribs, middle ribs, lower ribs) Diaphragm Assessment for passive motion and tenderness Chapman’s Points for Heart: • Heart Anterior: Just below R 2 at the sternocostal junction • Heart Posterior: T 3 Paraspinals at the 2 nd intercostal space
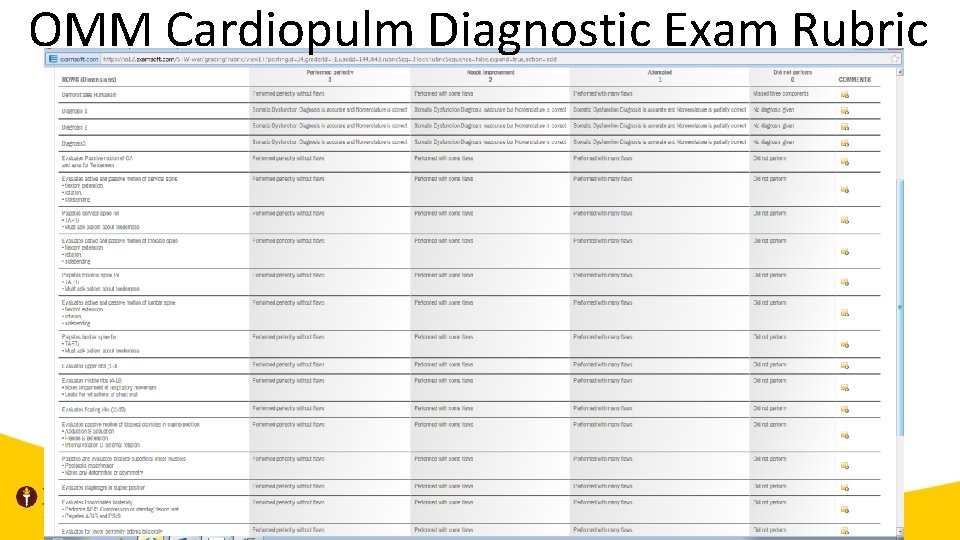
OMM Cardiopulm Diagnostic Exam Rubric
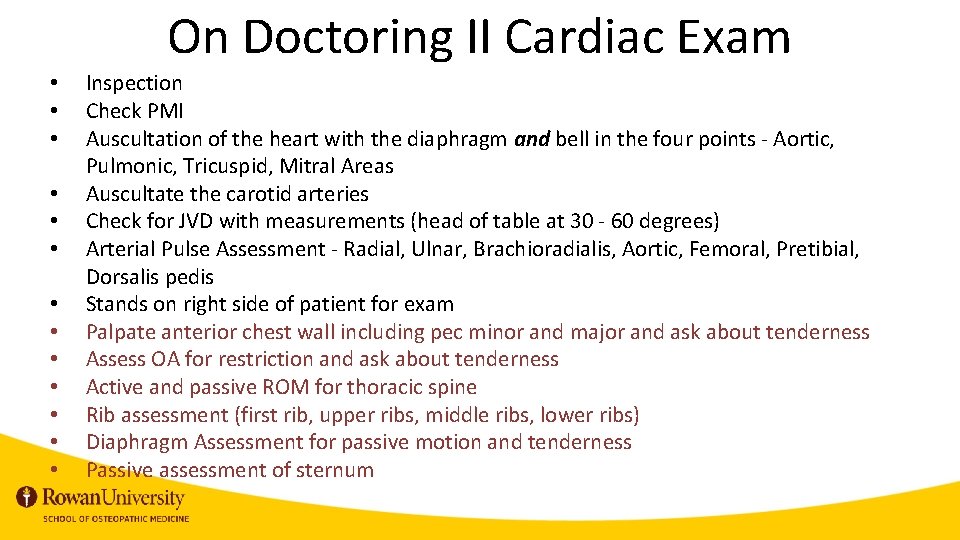
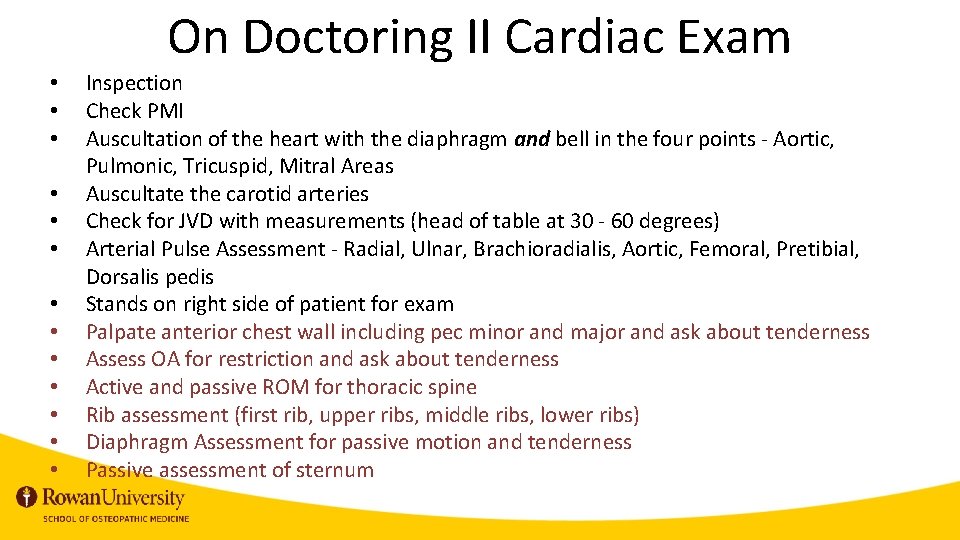
On Doctoring II Cardiac Exam • • • • Inspection Check PMI Auscultation of the heart with the diaphragm and bell in the four points - Aortic, Pulmonic, Tricuspid, Mitral Areas Auscultate the carotid arteries Check for JVD with measurements (head of table at 30 - 60 degrees) Arterial Pulse Assessment - Radial, Ulnar, Brachioradialis, Aortic, Femoral, Pretibial, Dorsalis pedis Stands on right side of patient for exam Palpate anterior chest wall including pec minor and major and ask about tenderness Assess OA for restriction and ask about tenderness Active and passive ROM for thoracic spine Rib assessment (first rib, upper ribs, middle ribs, lower ribs) Diaphragm Assessment for passive motion and tenderness Passive assessment of sternum
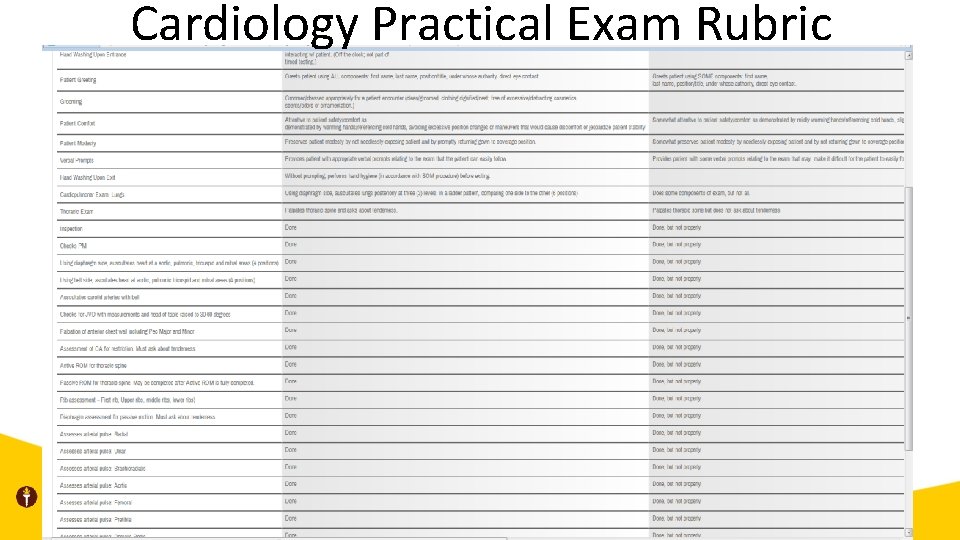
Cardiology Practical Exam Rubric
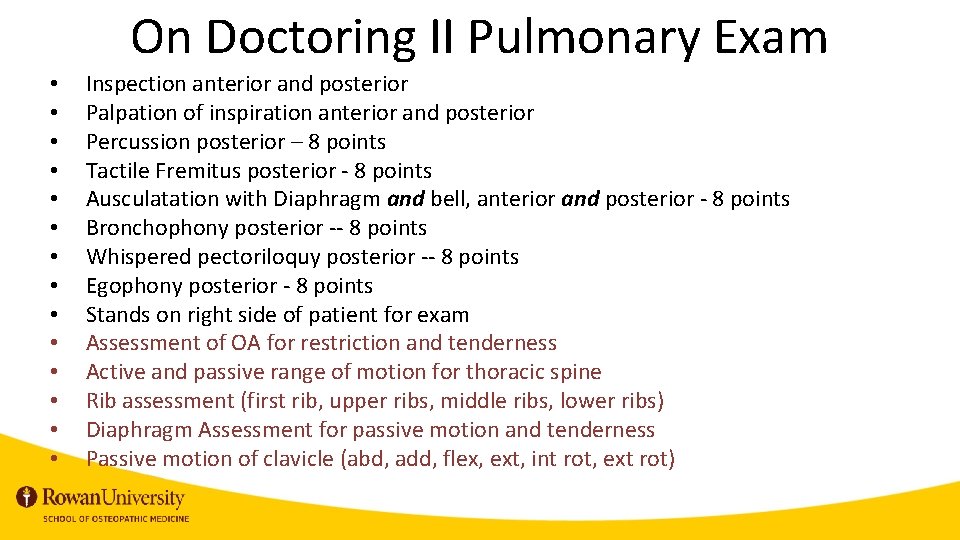
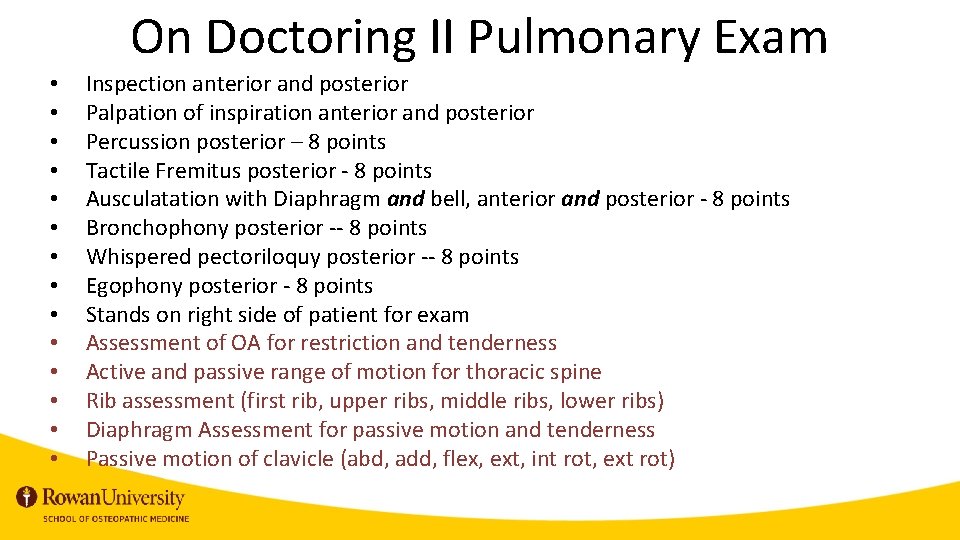
On Doctoring II Pulmonary Exam • • • • Inspection anterior and posterior Palpation of inspiration anterior and posterior Percussion posterior – 8 points Tactile Fremitus posterior - 8 points Ausculatation with Diaphragm and bell, anterior and posterior - 8 points Bronchophony posterior -- 8 points Whispered pectoriloquy posterior -- 8 points Egophony posterior - 8 points Stands on right side of patient for exam Assessment of OA for restriction and tenderness Active and passive range of motion for thoracic spine Rib assessment (first rib, upper ribs, middle ribs, lower ribs) Diaphragm Assessment for passive motion and tenderness Passive motion of clavicle (abd, add, flex, ext, int rot, ext rot)
Pulmonology Practical Exam Rubric
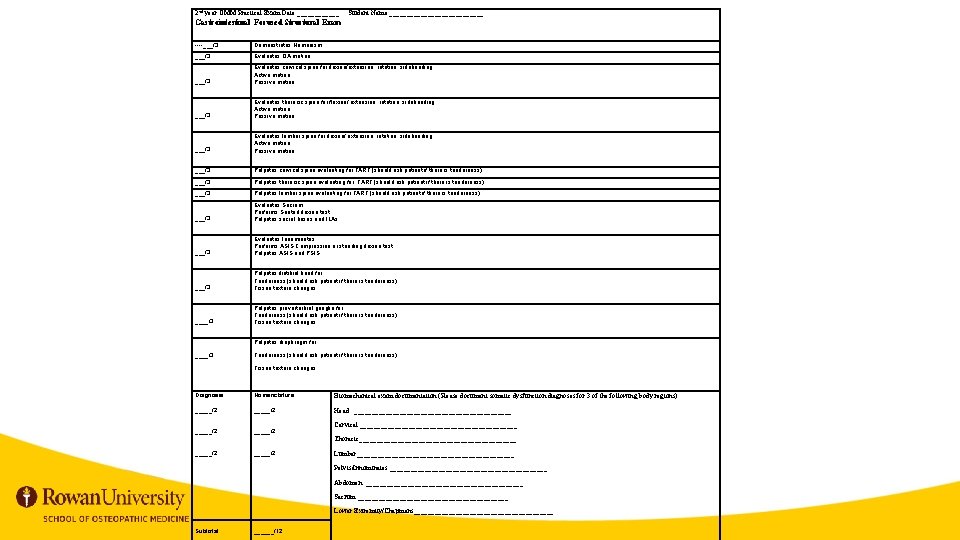
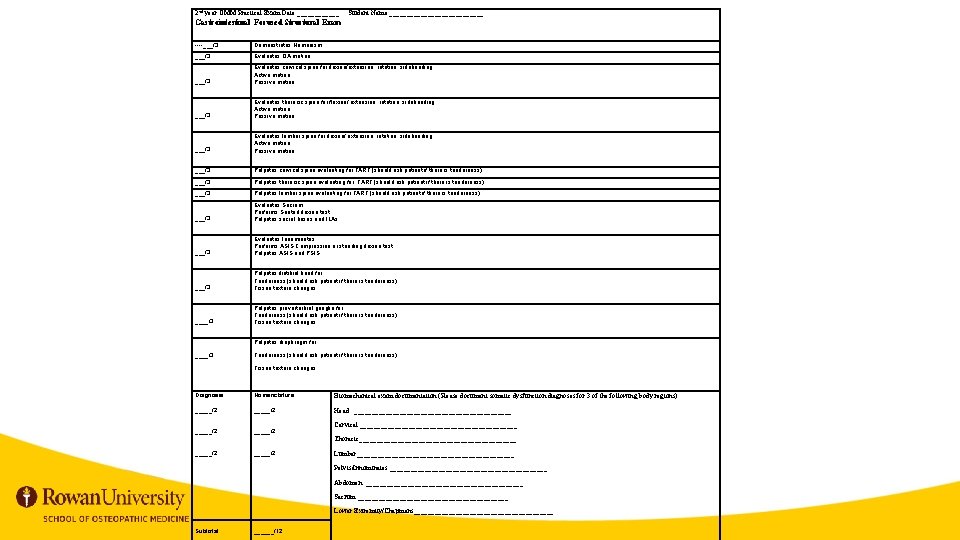
2 nd year OMM Practical Exam Date ______ Student Name ______________ Gastrointestinal Focused Structural Exam ___/3 Demonstrates Humanism ___/3 Evaluates OA motion Evaluates cervical spine for flexion/extension, rotation, sidebending. Active motion Passive motion ___/3 Evaluates thoracic spine for flexion/ extension, rotation, sidebending. Active motion Passive motion ___/3 Evaluates lumbar spine for flexion/ extension, rotation, sidebending. Active motion Passive motion ___/3 Palpates cervical spine evaluating for TART (should ask patient if there is tenderness) ___/3 Palpates thoracic spine evaluating for TART (should ask patient if there is tenderness) ___/3 Palpates lumbar spine evaluating for TART (should ask patient if there is tenderness) Evaluates Sacrum Performs Seated flexion test Palpates sacral bases and ILAs ___/3 Evaluates Innominates Performs ASIS Compression or standing flexion test Palpates ASIS and PSIS Palpates iliotibial band for Tenderness (should ask patient if there is tenderness) Tissue texture changes ____/3 Palpates preverterbral ganglia for Tenderness (should ask patient if there is tenderness) Tissue texture changes Palpates diaphragm for ____/3 Tenderness (should ask patient if there is tenderness) Tissue texture changes Diagnosis _____/2 Nomenclature _____/2 Biomechanical exam documentation (Please document somatic dysfunction diagnoses for 3 of the following body regions) Head _______________________ Cervical _______________________ Thoracic_______________________ Lumbar_______________________ Pelvis/Innominates _______________________ Abdomen _______________________ Sacrum ______________________ Lower Extremity/Chapmans____________________ Subtotal ______/12
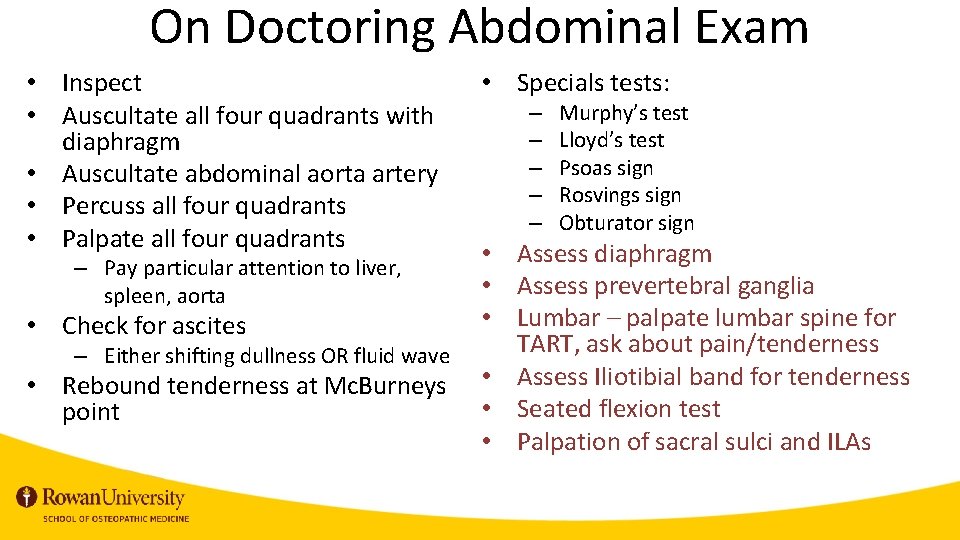
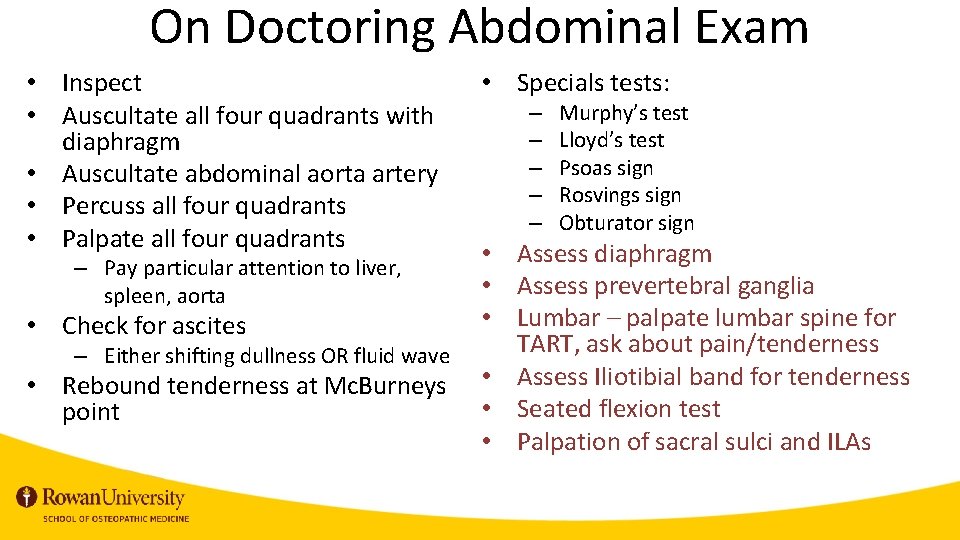
On Doctoring Abdominal Exam • Inspect • Auscultate all four quadrants with diaphragm • Auscultate abdominal aorta artery • Percuss all four quadrants • Palpate all four quadrants – Pay particular attention to liver, spleen, aorta • Check for ascites – Either shifting dullness OR fluid wave • Rebound tenderness at Mc. Burneys point • Specials tests: – – – Murphy’s test Lloyd’s test Psoas sign Rosvings sign Obturator sign • Assess diaphragm • Assess prevertebral ganglia • Lumbar – palpate lumbar spine for TART, ask about pain/tenderness • Assess Iliotibial band for tenderness • Seated flexion test • Palpation of sacral sulci and ILAs
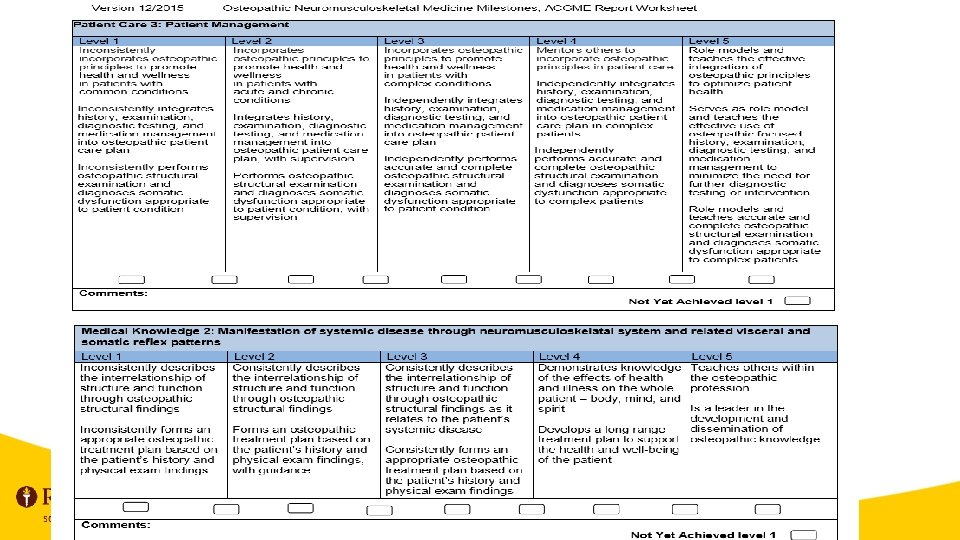
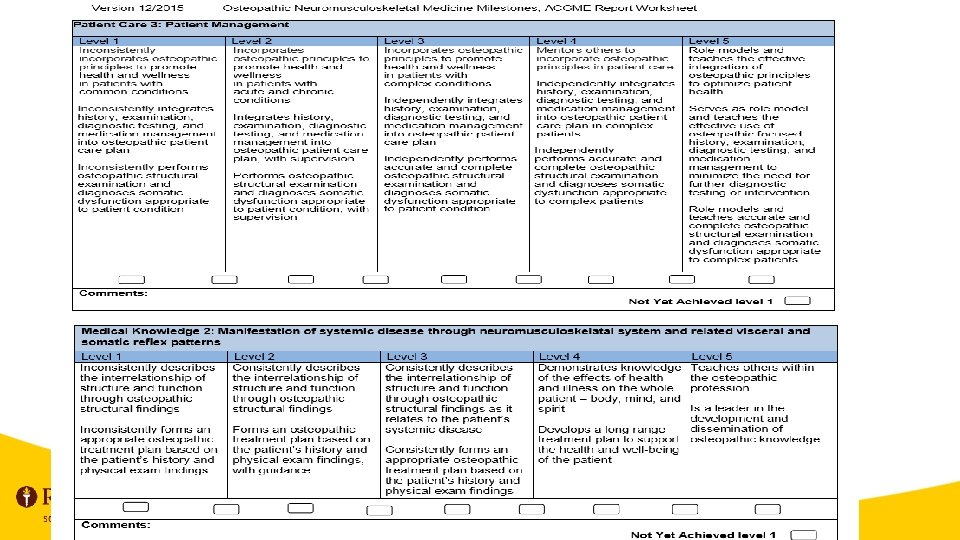
Why is this important? • Unified ACGME pathway Osteopathic Neuromuscular Medicine Milestone Project – “The Milestones provide a framework for assessment of the development of the resident in key dimensions of the elements of physician competency in a specialty or subspecialty. ” – Weights the knowledge of the interrelationship of physical diagnosis findings and osteopathic structural findings as an integral skill – These skills start in pre-clerkship years when students are first taught diagnostic skills. They are built upon in clerkship and residency.
In Conclusion • Students need to be able to integrate both skill sets for the COMLEX PE • Lack of the Osteopathic structural exam integration may result in physicians who are unsure of their Osteopathic skills • Incorporation is of both skill sets is necessary
References • • • ACGME. The Osteopathic Neuromusculoskeletal Medicine Milestone Project. The Accreditation Council for Graduate Medical Education. December, 2015. Accessed via the internet at: https: //www. acgme. org/Portals/0/PDFs/Milestones/Osteopathic. Neuromusculoskeletal. Medicnie. Milestones. pdf AACOM. Osteopathic Core Competencies for Medical Students. American Association of Colleges of Osteopathic Medicine. August, 2012. Accessed via the internet at: https: //www. aacom. org/docs/defaultsource/core-competencies/corecompetencyreport 2012. pdf? sfvrsn=4 NBOME. Fundamental Osteopathic Medical Competency Domains: Guidelines for Osteopathic Medical Licensure and the Practice of Osteopathic Medicine. National Board of Osteopathic Medical Examiners. June, 2011. Accessed via the internet at: https: //www. nbome. org/docs/NBOME%20 Fundamental%20 Osteopathic%20 Medical%20 Competencies. pdf Brian F. Degenhardt, DO. “Osteopathic Manipulative Medicine: Optimizing Patient-focused Health Care. ” The Advisor, Vol. 21, #1 (Dec 2000) Amy W. Johnson, DO; Jay H. Shubrook, Jr, DO. “Role of Osteopathic Structural Diagnosis and Osteopathic Manipulative Treatment for Diabetes Mellitus and Its Complications. ” The Journal of the American Osteopathic Association, November 2013, Vol. 113, 829 -836. doi: 10. 7556/jaoa. 2013. 058 A special thank you to Brittany Lipsett, Kathleen Maguire, Sima Bennett, and Kathy Roderique, for their invaluable help in this endeavor.