Integrating Team STEPPS into Simulation and Team Debriefing
Integrating Team. STEPPS® into Simulation and Team Debriefing AHA Team Training Monthly Webinar 11/8/2017
RULES OF ENGAGEMENT • Audio for the webinar can be accessed in two ways: • Through the phone (please mute your computer speakers) • Through your computer • A Q&A session will be held at the end of the presentation • Written questions are encouraged throughout the presentation and will be answered during the Q&A session • To submit a question, type it into the Chat Area and send it at any time during the presentation

UPCOMING AHA TEAM TRAINING EVENTS • December 6 Webinar • Enhancing Patient Engagement Using Team. STEPPS® Tools • Free to register • Master Training Course in Chicago on December 14 -15 • Master Training course focused on utilizing games, scenarios and activities • Registration now open 3

TEAM TRAINING NATIONAL CONFERENCE 4
TEAM TRAINING NATIONAL CONFERENCE • Call for Proposals now open and due on December 8 • Breakout sessions and posters • Topic tracks: • Effective Teaching: Innovative Ways of Bringing Team. STEPPS to your Team • Connecting the Dots: Making Team. STEPPS a Lasting Approach • Engaging the Team: Patients, Staff, Providers, Leaders and Students • Making the Case: Assessing, Measuring and Implementing Team. STEPPS across the Continuum 5

CONTACT INFORMATION Web: www. aha. org/teamtraining Email: Team. Training@aha. org Phone: 312 -422 -2609 6
TODAY’S PRESENTERS • Jim Carlson, Ph. D, PA-C, CHSE, Vice President for Interprofessional Education and Simulation and Associate Professor at Rosalind Franklin University • William Gordon, DMin, Instructor at Rosalind Franklin University 7
SESSION OBJECTIVES • Describe how a health professions university or program can integrate foundational Team. STEPPS training in an interprofessional model. • Describe methods for scaffolding foundational Team. STEPPS principles into simulation-based education and assessment.
SESSION OBJECTIVES • Utilize Team. STEPPS principles and strategies as a method for debriefing and professional development in simulated encounters. • Describe outcomes related to simulation-based Team. STEPPS training and Interprofessional Education.
SESSION OVERVIEW • An overview of Rosalind Franklin University and Interprofessionalism as a core mission • Approach to IP education (Team. STEPPS , IPEC competencies, and Simulation) • Simulation design, execution, and debriefing • Challenges, opportunities, and future directions • Question and Answer
Interprofessionalism at Rosalind Franklin University of Medicine and Science
MISSION To serve the population through the interprofessional education of health and biomedical professionals and the discovery of knowledge dedicated to improving the wellness of its people. VISION To achieve national recognition as the premier interprofessional health sciences University.
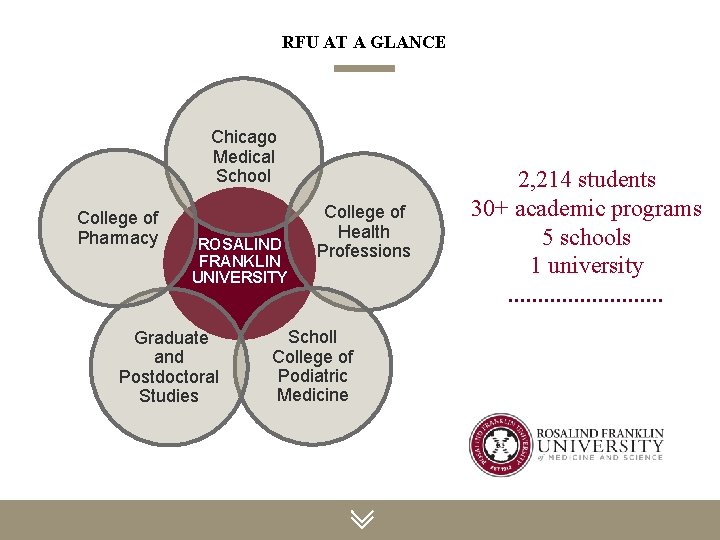
RFU AT A GLANCE Chicago Medical School College of Pharmacy ROSALIND FRANKLIN UNIVERSITY Graduate and Postdoctoral Studies College of Health Professions Scholl College of Podiatric Medicine 2, 214 students 30+ academic programs 5 schools 1 university
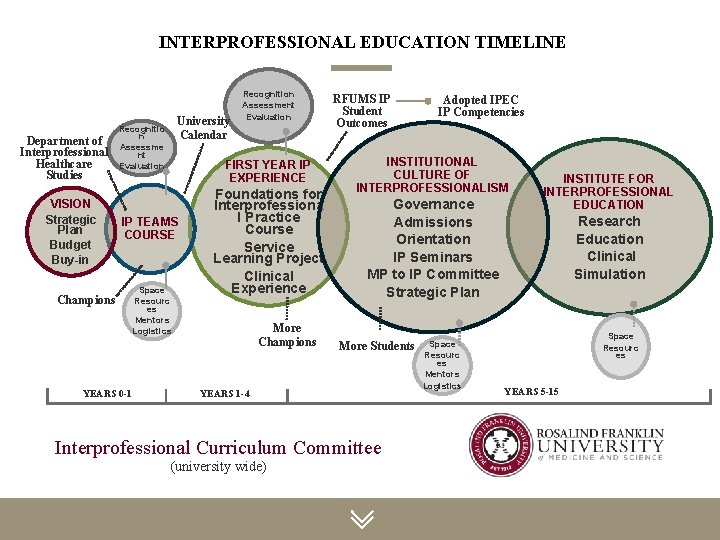
INTERPROFESSIONAL EDUCATION TIMELINE Department of Interprofessional Healthcare Studies VISION Strategic Plan Budget Buy-in University Calendar Recognitio n Assessme nt Evaluation FIRST YEAR IP EXPERIENCE IP TEAMS COURSE Champions YEARS 0 -1 Recognition Assessment Evaluation Space Resourc es Mentors Logistics Foundations for Interprofessiona l Practice Course Service Learning Project Clinical Experience More Champions RFUMS IP Student Outcomes INSTITUTIONAL CULTURE OF INTERPROFESSIONALISM Governance Admissions Orientation IP Seminars MP to IP Committee Strategic Plan More Students YEARS 1 -4 Interprofessional Curriculum Committee (university wide) Adopted IPEC IP Competencies Space Resourc es Mentors Logistics INSTITUTE FOR INTERPROFESSIONAL EDUCATION Research Education Clinical Simulation Space Resourc es YEARS 5 -15
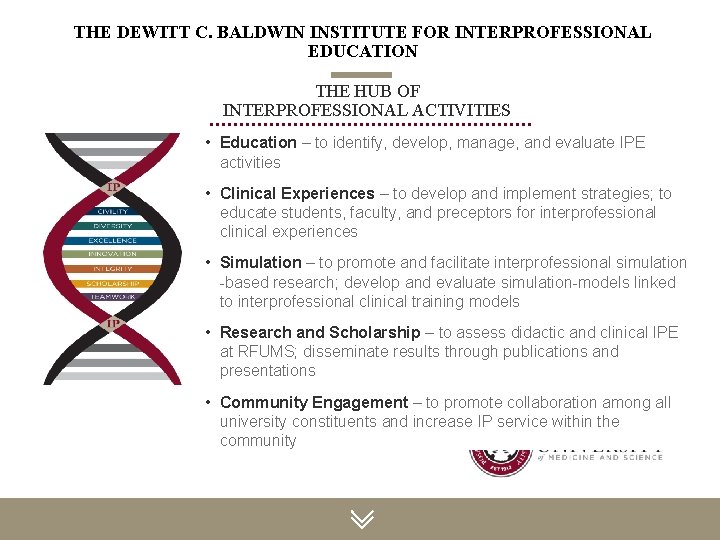
THE DEWITT C. BALDWIN INSTITUTE FOR INTERPROFESSIONAL EDUCATION THE HUB OF INTERPROFESSIONAL ACTIVITIES • Education – to identify, develop, manage, and evaluate IPE activities • Clinical Experiences – to develop and implement strategies; to educate students, faculty, and preceptors for interprofessional clinical experiences • Simulation – to promote and facilitate interprofessional simulation -based research; develop and evaluate simulation-models linked to interprofessional clinical training models • Research and Scholarship – to assess didactic and clinical IPE at RFUMS; disseminate results through publications and presentations • Community Engagement – to promote collaboration among all university constituents and increase IP service within the community
INTERPROFESSIONAL EDUCATION COMPETENCIES • Values and Ethics Work with individuals of other professions to maintain a climate of mutual respect and shared values. • Roles and Responsibilities Use the knowledge of one's own role and those of other professions to appropriately assess and address the health care needs of patients and to promote and advance the health of populations. 16
INTERPROFESSIONAL EDUCATION COMPETENCIES • Interprofessional Communication Communicate with patients, families, communities, and professionals in health and other fields in a responsive and responsible manner that supports a team approach to the promotion and maintenance of health and the prevention and treatment of disease. • Teams and Team working Apply relationship-building values and the principles of team dynamics to perform effectively in different team roles to plan, deliver, and evaluate patient/population-centered care and population health programs and policies that are safe, timely, efficient, effective, and equitable. 17
18
INTERPROFESSIONAL EDUCATION THROUGH SIMULATION AND TEAMSTEPPS
SIMULATION IN HEALTHCARE EDUCATION Simulation is a technique – not a technology – to replace or amplify real experiences with guided experiences that evoke or replicate substantial aspects of the real word in a fully interactive manner. REFERENCE Gaba DM. The future vision of simulation in healthcare. Qual Saf Health Care 2004; 13 i 2 -i 10
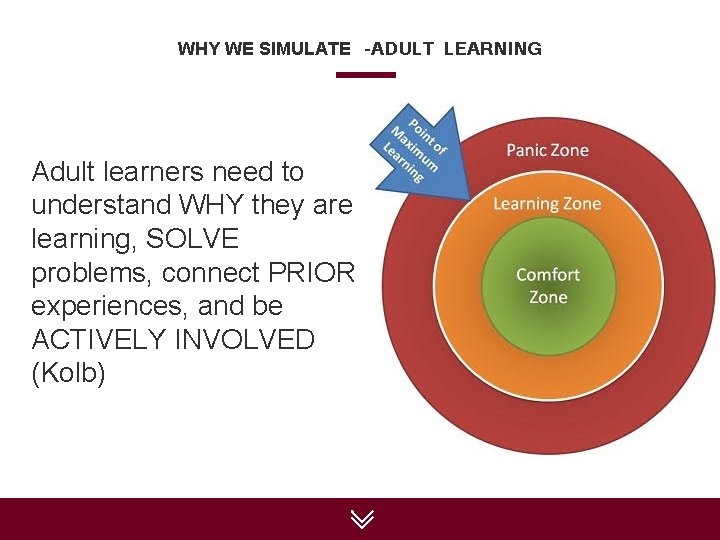
WHY WE SIMULATE –ADULT LEARNING Adult learners need to understand WHY they are learning, SOLVE problems, connect PRIOR experiences, and be ACTIVELY INVOLVED (Kolb)

PROFESSION SPECIFIC SIMULATIONS • Allopathic Medicine • Podiatric Medicine • Physician Assistant • Pathologists’ Assistant • Physical Therapy • Pharmacy • Nurse Anesthesia • Nursing (RN) • Psychology / Clinical Counseling
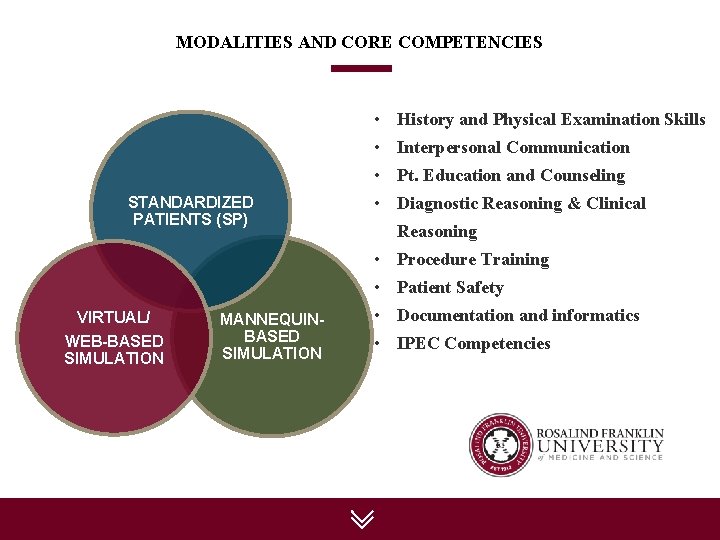
MODALITIES AND CORE COMPETENCIES • History and Physical Examination Skills • Interpersonal Communication • Pt. Education and Counseling STANDARDIZED PATIENTS (SP) • Diagnostic Reasoning & Clinical Reasoning • Procedure Training • Patient Safety VIRTUAL/ WEB-BASED SIMULATION MANNEQUINBASED SIMULATION • Documentation and informatics • IPEC Competencies
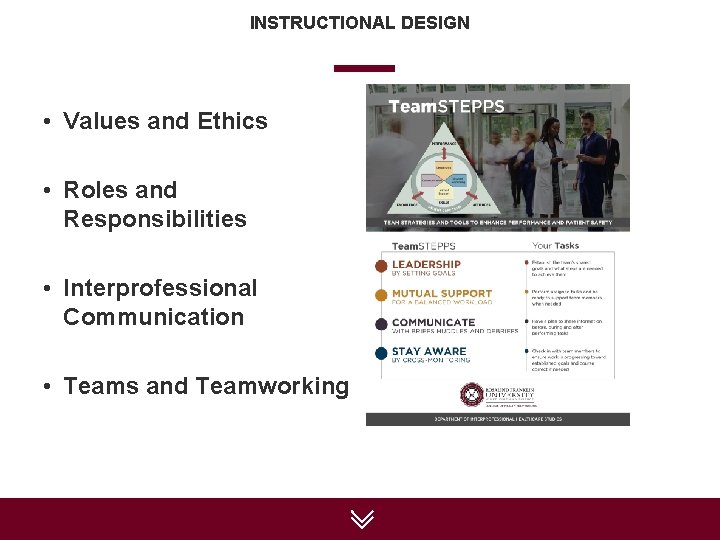
INSTRUCTIONAL DESIGN • Values and Ethics • Roles and Responsibilities • Interprofessional Communication • Teams and Teamworking 24
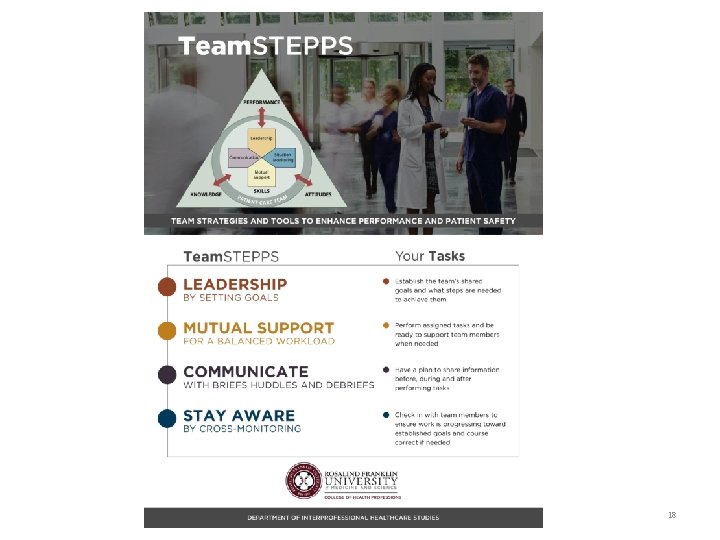
INSTRUCTIONAL DESIGN • Team. STEPPS informs – Formation of simulation objectives – Case and simulation design – Forms a foundation for effective debriefing 25
SAMPLE PROJECTS AND OUTCOMES • Team Training Workshop – M 3, PAS-2 and Pharm 4 students engaged in collaborative problem solving using Team. STEPPS principles • Patient Safety Workshop – Uniprofessional simulation engaging in handoffs and conflict resolution using Team. STEPPS principles • Diagnostic safety/ bias exercise – Interprofessional simulation engaging interprofessional communication and use of informative tools to improve diagnostic safety 26
TEAM TRAINING WORKSHOP • Clinical year activity for third year medical students, second year PA students, and fourth year pharmacy students • Designed by an Interprofessional team of faculty and simulationists 27
SAMPLE IPEC OBJECTIVES ENGAGED • Role and Responsibilities (RR 7): Forge interdependent relationships with other professions within and outside of the health system to improve care and advance learning. • Teams and Teamwork (TT 4): Integrate the knowledge and experience of health and other professions to inform health and care decisions, while respecting patient and community values and priorities/preferences for care. 28
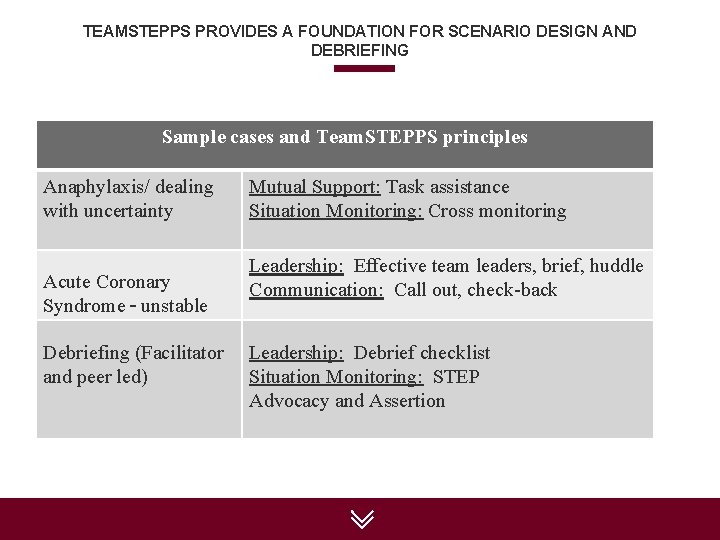
TEAMSTEPPS PROVIDES A FOUNDATION FOR SCENARIO DESIGN AND DEBRIEFING Sample cases and Team. STEPPS principles Anaphylaxis/ dealing with uncertainty Acute Coronary Syndrome – unstable Debriefing (Facilitator and peer led) Mutual Support: Task assistance Situation Monitoring: Cross monitoring Leadership: Effective team leaders, brief, huddle Communication: Call out, check-back Leadership: Debrief checklist Situation Monitoring: STEP Advocacy and Assertion 29
30
31
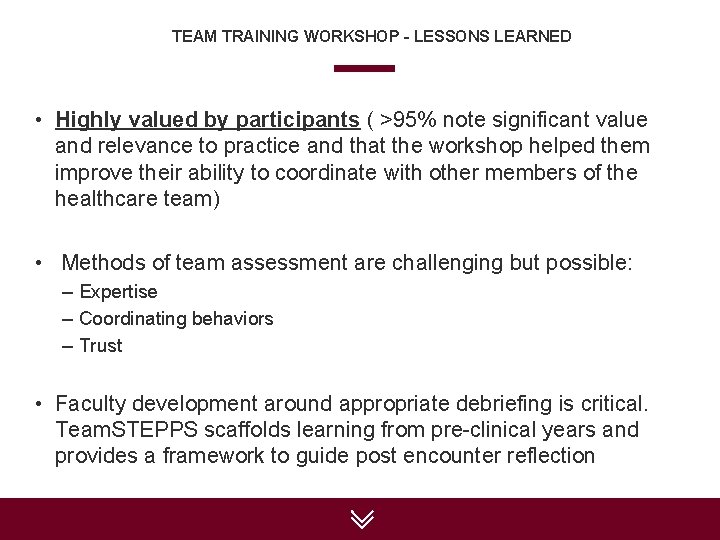
TEAM TRAINING WORKSHOP – LESSONS LEARNED • Highly valued by participants ( >95% note significant value and relevance to practice and that the workshop helped them improve their ability to coordinate with other members of the healthcare team) • Methods of team assessment are challenging but possible: – Expertise – Coordinating behaviors – Trust • Faculty development around appropriate debriefing is critical. Team. STEPPS scaffolds learning from pre-clinical years and provides a framework to guide post encounter reflection 32
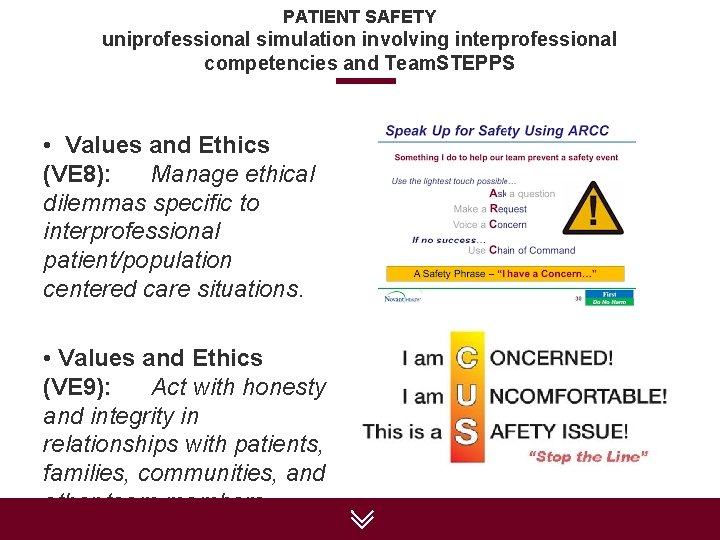
PATIENT SAFETY uniprofessional simulation involving interprofessional competencies and Team. STEPPS • Values and Ethics (VE 8): Manage ethical dilemmas specific to interprofessional patient/population centered care situations. • Values and Ethics (VE 9): Act with honesty and integrity in relationships with patients, families, communities, and other team members. 33
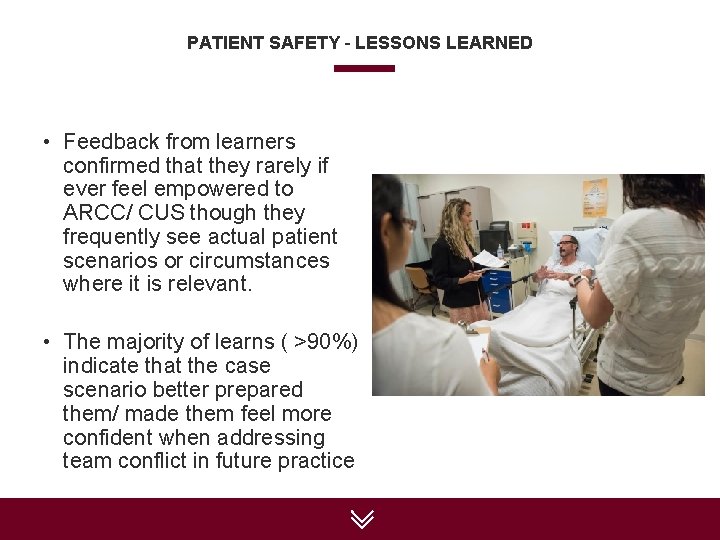
PATIENT SAFETY – LESSONS LEARNED • Feedback from learners confirmed that they rarely if ever feel empowered to ARCC/ CUS though they frequently see actual patient scenarios or circumstances where it is relevant. • The majority of learns ( >90%) indicate that the case scenario better prepared them/ made them feel more confident when addressing team conflict in future practice 34
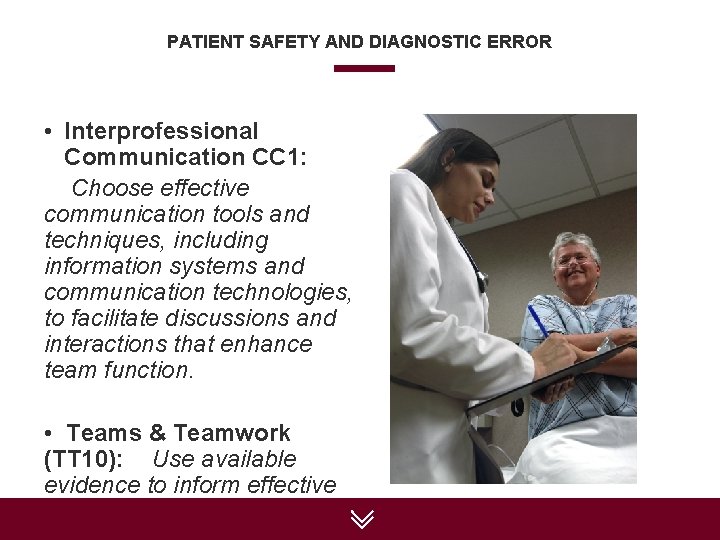
PATIENT SAFETY AND DIAGNOSTIC ERROR • Interprofessional Communication CC 1: Choose effective communication tools and techniques, including information systems and communication technologies, to facilitate discussions and interactions that enhance team function. • Teams & Teamwork (TT 10): Use available evidence to inform effective teamwork and team-based 35
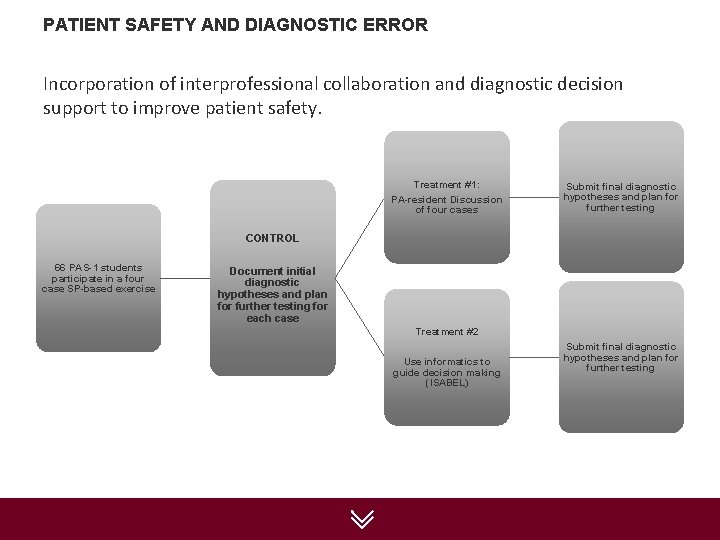
PATIENT SAFETY AND DIAGNOSTIC ERROR Incorporation of interprofessional collaboration and diagnostic decision support to improve patient safety. Treatment #1: PA-resident Discussion of four cases Submit final diagnostic hypotheses and plan for further testing CONTROL 66 PAS-1 students participate in a four case SP-based exercise Document initial diagnostic hypotheses and plan for further testing for each case Treatment #2 Use informatics to guide decision making (ISABEL) Submit final diagnostic hypotheses and plan for further testing 36
OUTCOMES • PA students that coordinated with the resident did not improve accuracy and were overconfident in their decisions. • PA students that used a self-directed support system (ISABEL) significantly improved accuracy and were more appropriately calibrated in terms of confidence. • Video analysis of PA-Resident discussions revealed communication behaviors that promoted anchoring and confirmation bias. 37
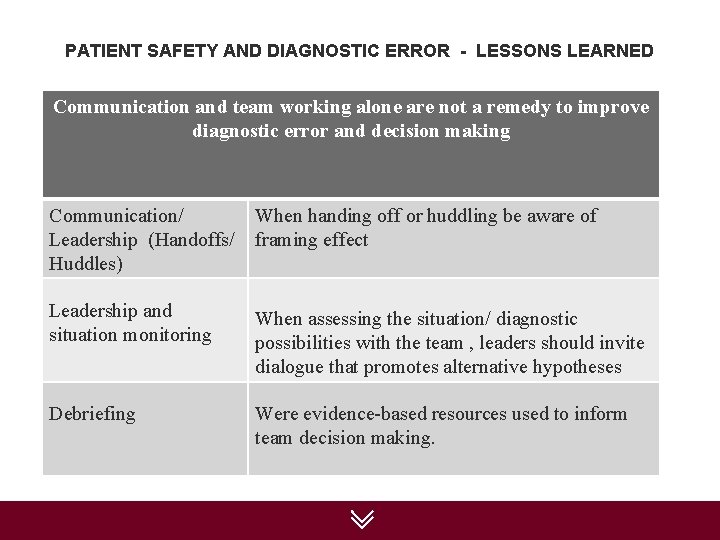
PATIENT SAFETY AND DIAGNOSTIC ERROR - LESSONS LEARNED Communication and team working alone are not a remedy to improve diagnostic error and decision making Communication/ Leadership (Handoffs/ Huddles) When handing off or huddling be aware of framing effect Leadership and situation monitoring When assessing the situation/ diagnostic possibilities with the team , leaders should invite dialogue that promotes alternative hypotheses Debriefing Were evidence-based resources used to inform team decision making. 38
MEANINGFUL INTERPROFESSIONAL SIMULATION THE VIRTUAL HOSPITAL 39
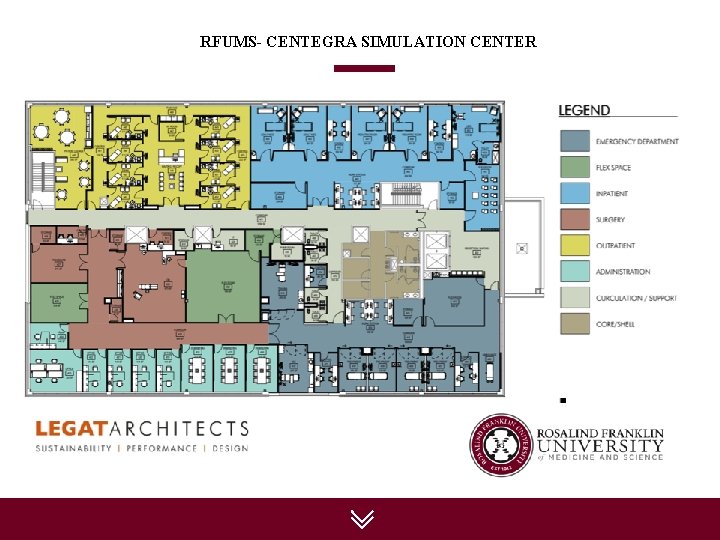
RFUMS- CENTEGRA SIMULATION CENTER
EMERGENCY DEPARTMENT

EMERGENCY DEPARTMENT

AMBULATORY CARE / OUTPATIENT
INPATIENT UNIT
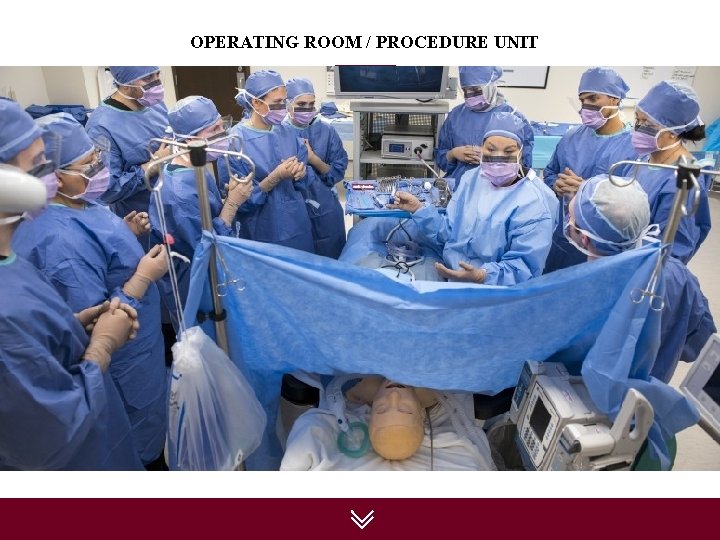
OPERATING ROOM / PROCEDURE UNIT
QUESTIONS? • If you enjoyed this webinar and wish to attend a Master Training Course, click here or visit www. aha. org/teamtraining to learn more about our December 14 -15 in Chicago led by Bill Gordon and his team. • Stay in touch! Email teamtraining@aha. org or visit www. aha. org/teamtraining 48
- Slides: 48