Integrating Pr EP Referrals into STD Partner Services
- Slides: 1
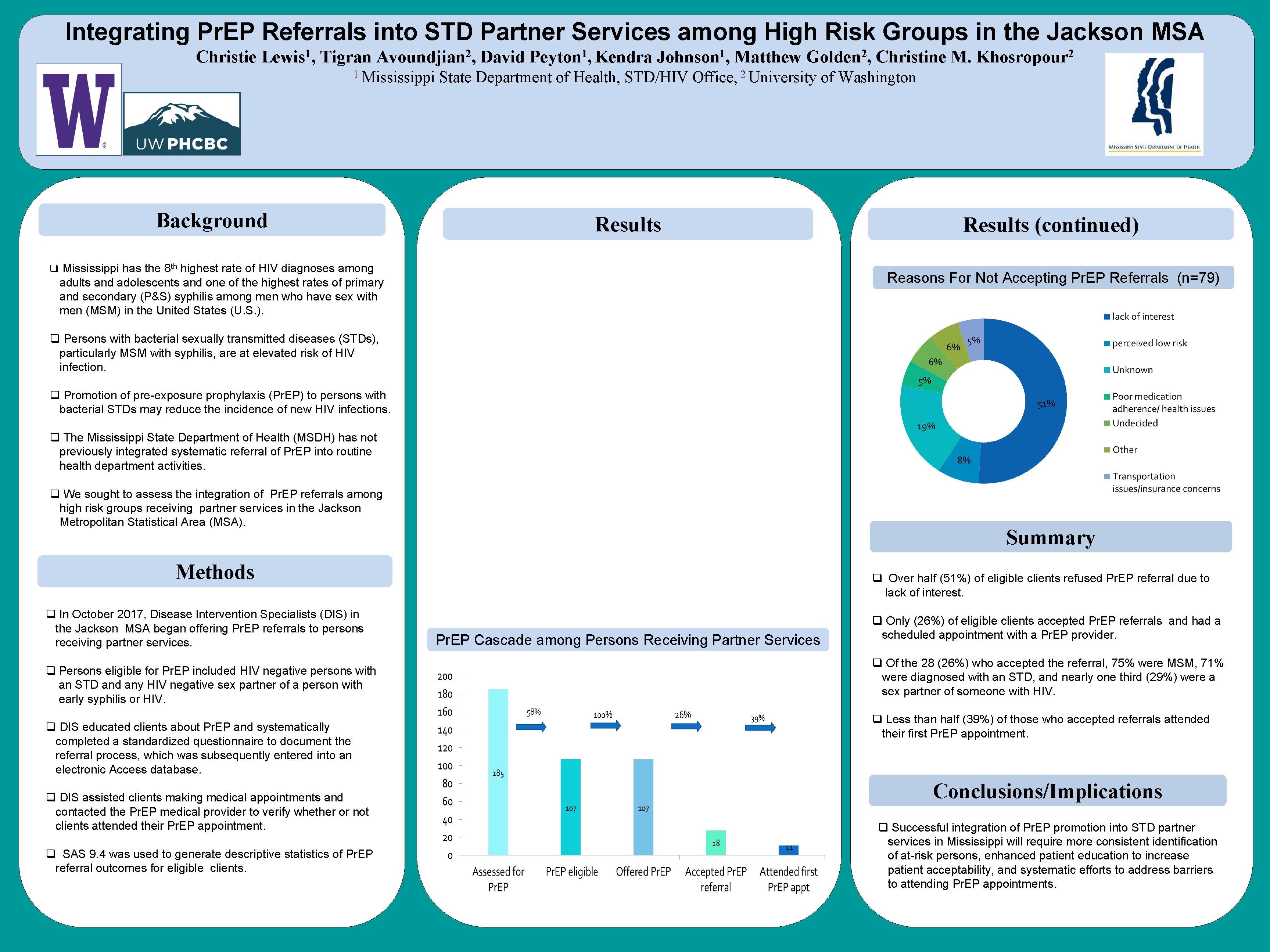
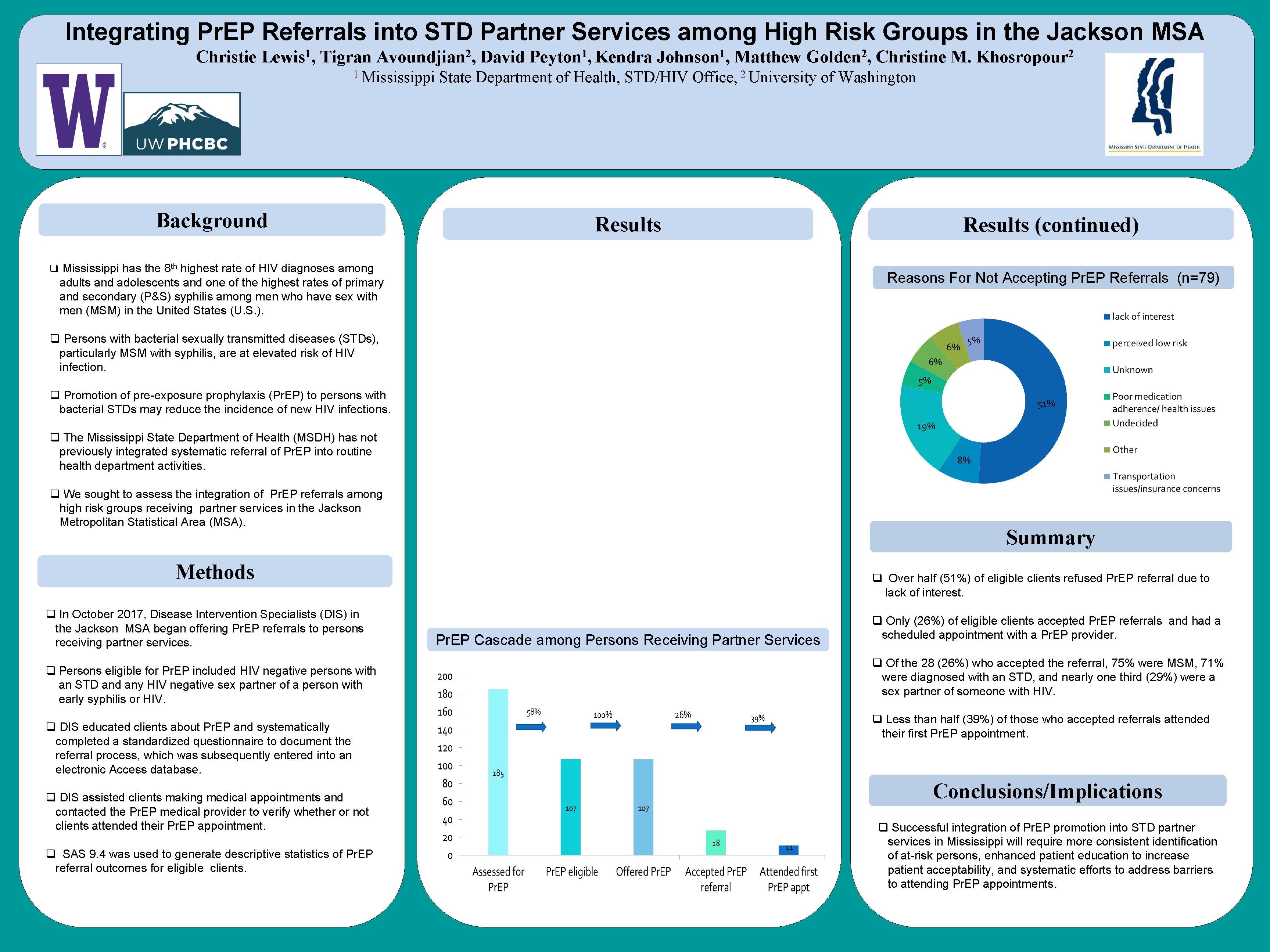
Integrating Pr. EP Referrals into STD Partner Services among High Risk Groups in the Jackson MSA Christie Lewis 1, Tigran Avoundjian 2, David Peyton 1, Kendra Johnson 1, Matthew Golden 2, Christine M. Khosropour 2 1 Mississippi Background State Department of Health, STD/HIV 2 Office, University Results q Mississippi has the 8 th highest rate of HIV diagnoses among of Washington Results (continued) Reasons For Not Accepting Pr. EP Referrals (n=79) adults and adolescents and one of the highest rates of primary and secondary (P&S) syphilis among men who have sex with men (MSM) in the United States (U. S. ). q Persons with bacterial sexually transmitted diseases (STDs), particularly MSM with syphilis, are at elevated risk of HIV infection. q Promotion of pre-exposure prophylaxis (Pr. EP) to persons with bacterial STDs may reduce the incidence of new HIV infections. q The Mississippi State Department of Health (MSDH) has not previously integrated systematic referral of Pr. EP into routine health department activities. q We sought to assess the integration of Pr. EP referrals among high risk groups receiving partner services in the Jackson Metropolitan Statistical Area (MSA). Summary Methods q In October 2017, Disease Intervention Specialists (DIS) in the Jackson MSA began offering Pr. EP referrals to persons receiving partner services. q Persons eligible for Pr. EP included HIV negative persons with an STD and any HIV negative sex partner of a person with early syphilis or HIV. q DIS educated clients about Pr. EP and systematically completed a standardized questionnaire to document the referral process, which was subsequently entered into an electronic Access database. q DIS assisted clients making medical appointments and contacted the Pr. EP medical provider to verify whether or not clients attended their Pr. EP appointment. q SAS 9. 4 was used to generate descriptive statistics of Pr. EP referral outcomes for eligible clients. q Over half (51%) of eligible clients refused Pr. EP referral due to lack of interest. Pr. EP Cascade among Persons Receiving Partner Services q Only (26%) of eligible clients accepted Pr. EP referrals and had a scheduled appointment with a Pr. EP provider. q Of the 28 (26%) who accepted the referral, 75% were MSM, 71% were diagnosed with an STD, and nearly one third (29%) were a sex partner of someone with HIV. q Less than half (39%) of those who accepted referrals attended their first Pr. EP appointment. Conclusions/Implications q Successful integration of Pr. EP promotion into STD partner services in Mississippi will require more consistent identification of at-risk persons, enhanced patient education to increase patient acceptability, and systematic efforts to address barriers to attending Pr. EP appointments.