Integrated Care Programmes Inaugural Conference Making Peoplecentred Integrated




- Slides: 38

Integrated Care Programmes: Inaugural Conference "Making People-centred Integrated Care a Reality" The Printworks, Dublin Castle, Republic of Ireland 6 th October 2015 People-centred Integrated Care Strategy – Irish Launch Hernan Montenegro, MD, MPH Coordinator Services Organization and Clinical Interventions Unit Service Delivery and Safety Department World Health Organization
Content • Global context and health system challenges • WHO policy directions • WHO strategy on integrated, people-centred health services (IPCHS) • Lessons learned on implementation of IPCHS: – Context – Content – Processes – Actors
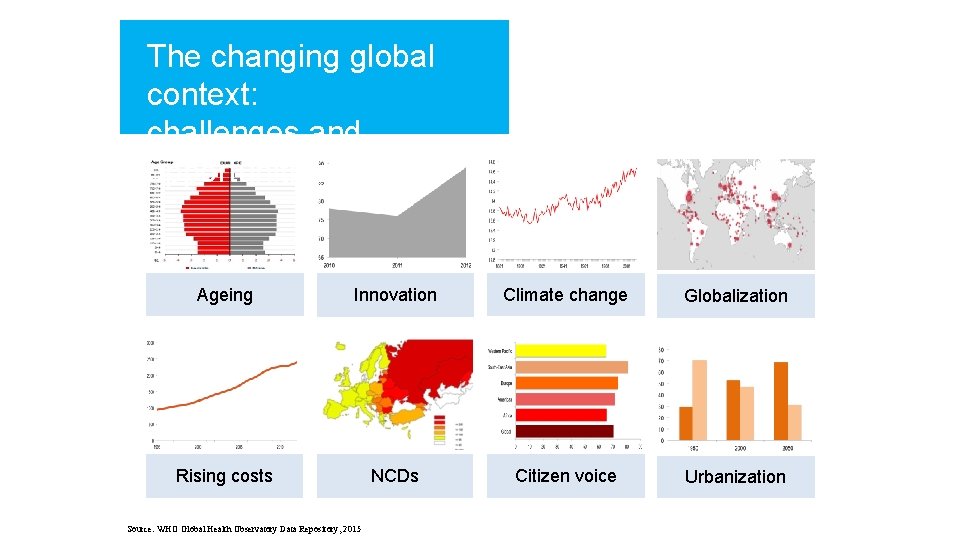
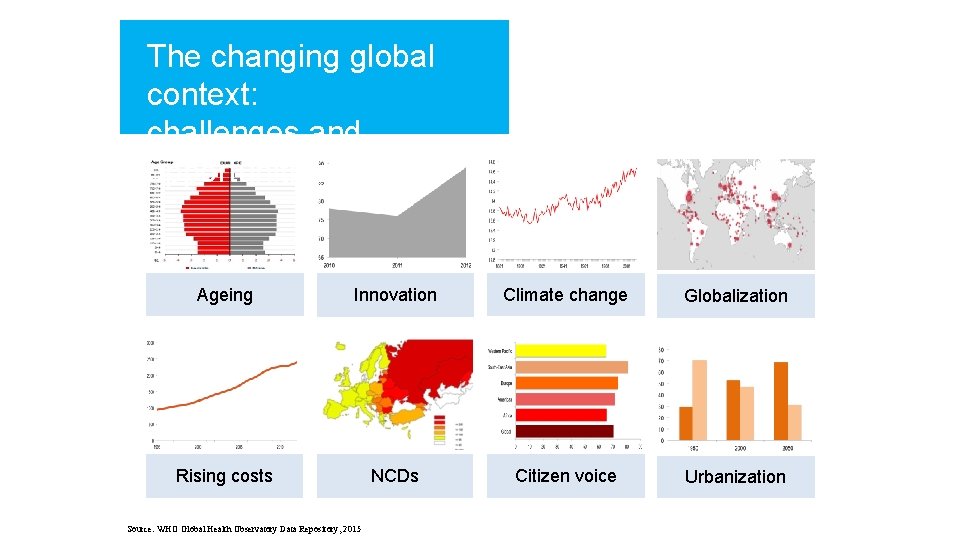
The changing global context: challenges and opportunities Ageing Innovation Climate change Globalization Rising costs NCDs Citizen voice Urbanization Source: WHO Global Health Observatory Data Repository, 2015
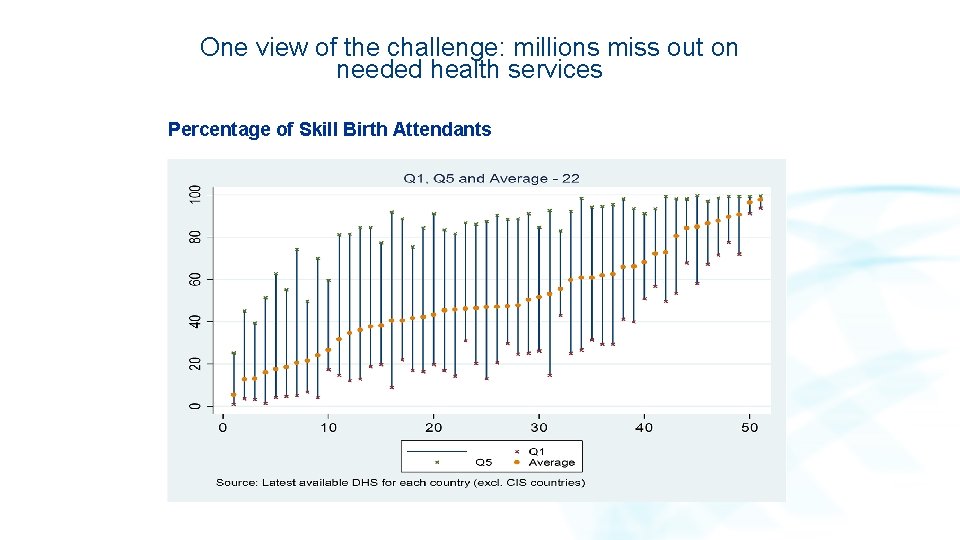
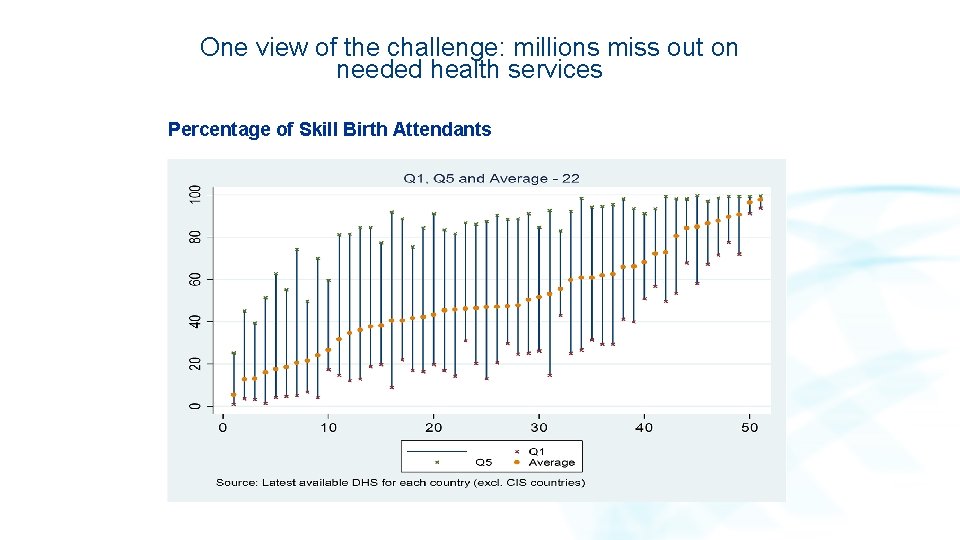
One view of the challenge: millions miss out on needed health services Percentage of Skill Birth Attendants
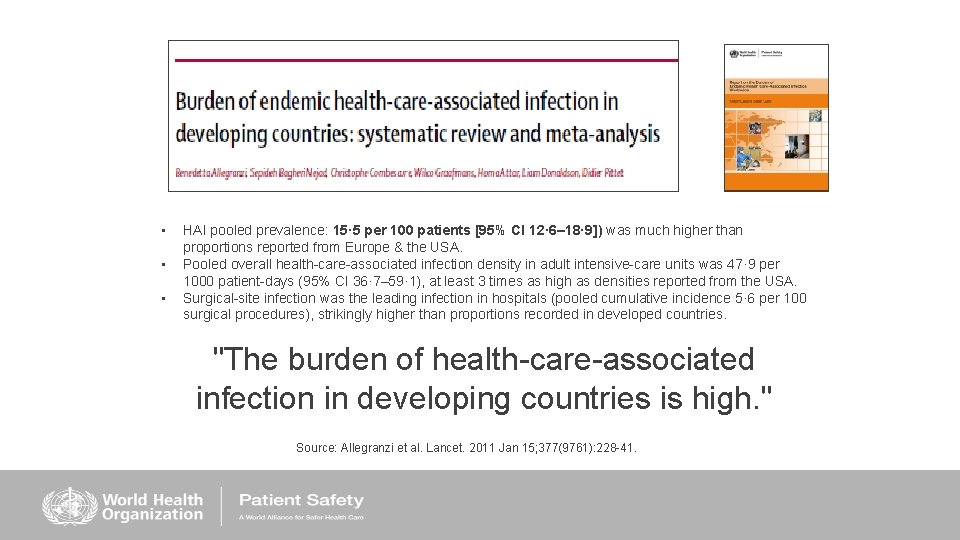
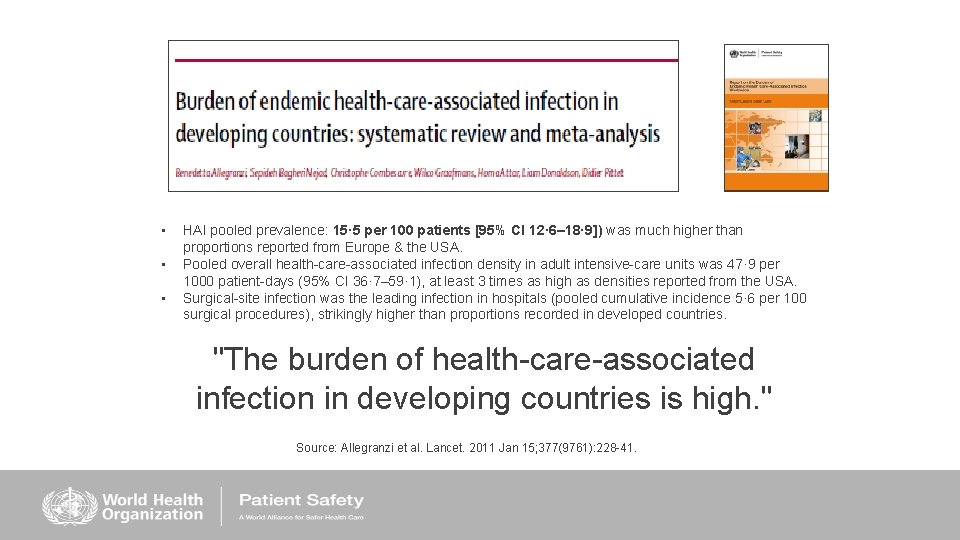
• • • HAI pooled prevalence: 15· 5 per 100 patients [95% CI 12· 6– 18· 9]) was much higher than proportions reported from Europe & the USA. Pooled overall health-care-associated infection density in adult intensive-care units was 47· 9 per 1000 patient-days (95% CI 36· 7– 59· 1), at least 3 times as high as densities reported from the USA. Surgical-site infection was the leading infection in hospitals (pooled cumulative incidence 5· 6 per 100 surgical procedures), strikingly higher than proportions recorded in developed countries. "The burden of health-care-associated infection in developing countries is high. " Source: Allegranzi et al. Lancet. 2011 Jan 15; 377(9761): 228 -41.
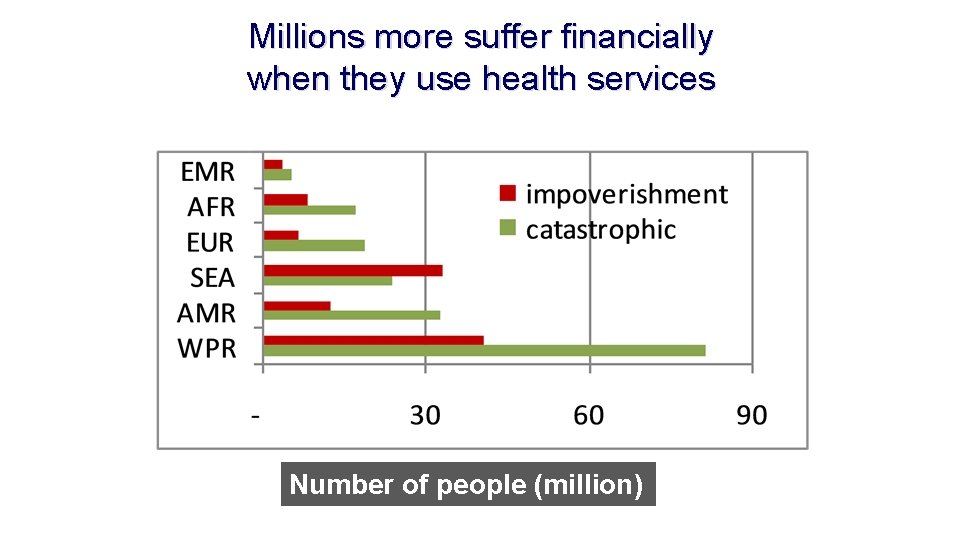
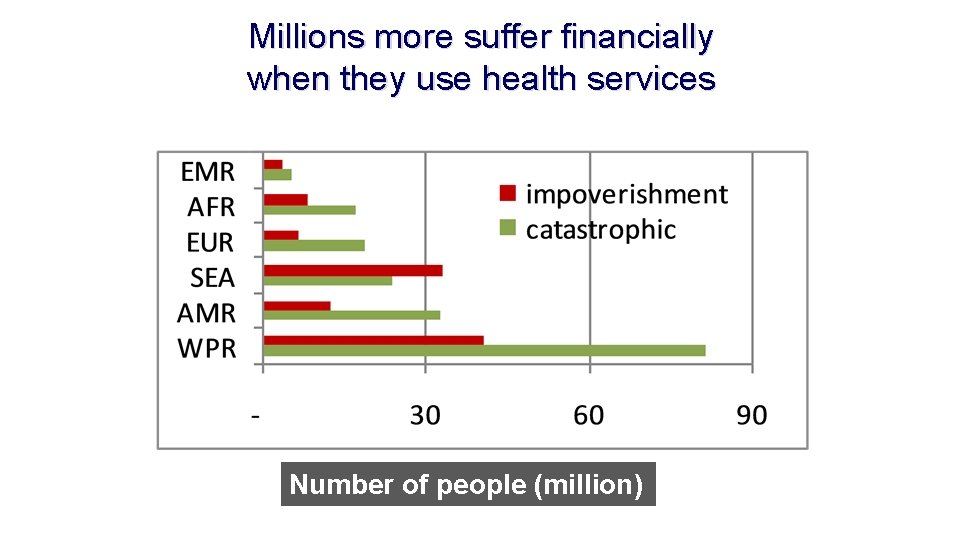
Millions more suffer financially when they use health services Number of people (million)

Model of Care: Continuity of Care Section I. 3: PHC Model of Care: Continuity of Care % 3. 1 Respondents Responses, in Percent 50 40 30 20 10 0 3. 1. 1 Never 3. 1. 2 Almost never 3. 1. 3 Sometimes 3. 1. 4 Usually 3. 1. 5 Always 3. 1. 1 Are patients seen by the same provider (doctor/ health team) whenever they consult? 3. 1. 4 Does a good referral and counterreferral system based on case complexity normally function for patients? 3. 1. 2 Is there an appointment and follow-up system, including arranging home visits by the health team? 3. 1. 5 Is there a policy that enables 3. 1. 3 Is assigning people from a geographical area to lists or registries with a ensuring that PHC facilities are regularly covered by physicians or nurses?
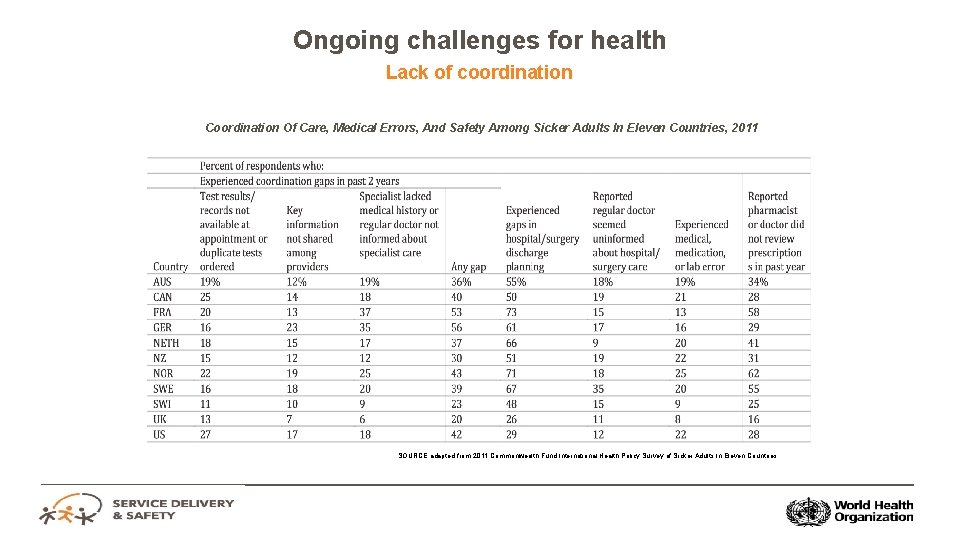
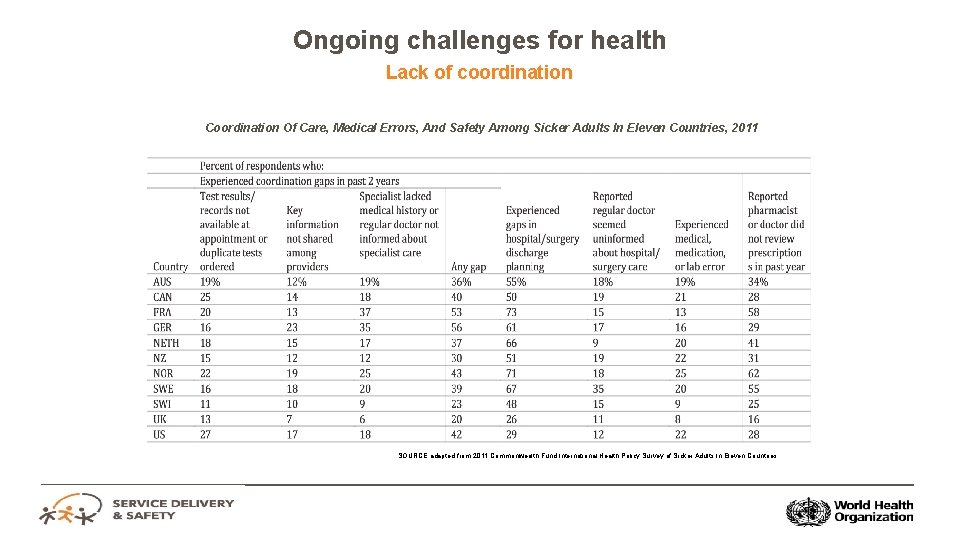
Ongoing challenges for health Lack of coordination Coordination Of Care, Medical Errors, And Safety Among Sicker Adults In Eleven Countries, 2011 SOURCE adapted from 2011 Commonwealth Fund International Health Policy Survey of Sicker Adults In Eleven Countries
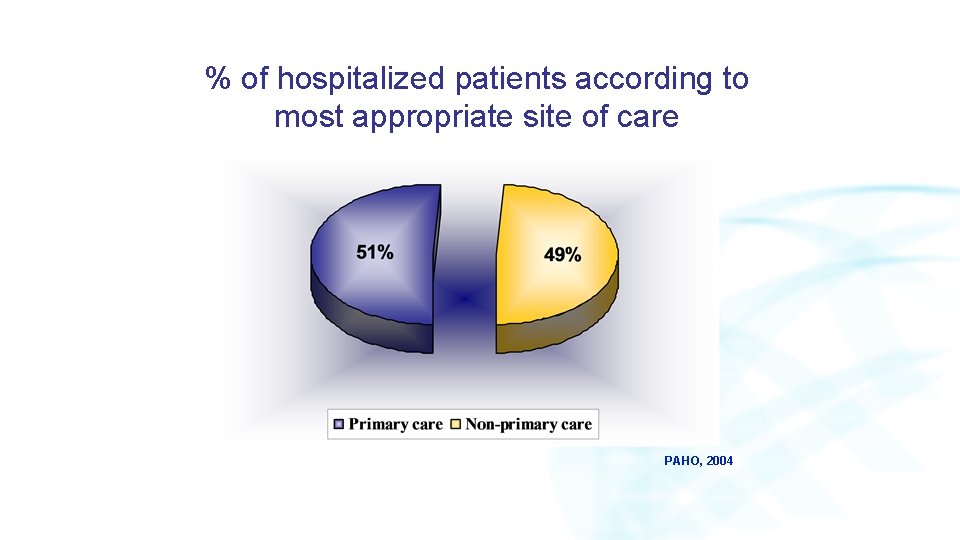
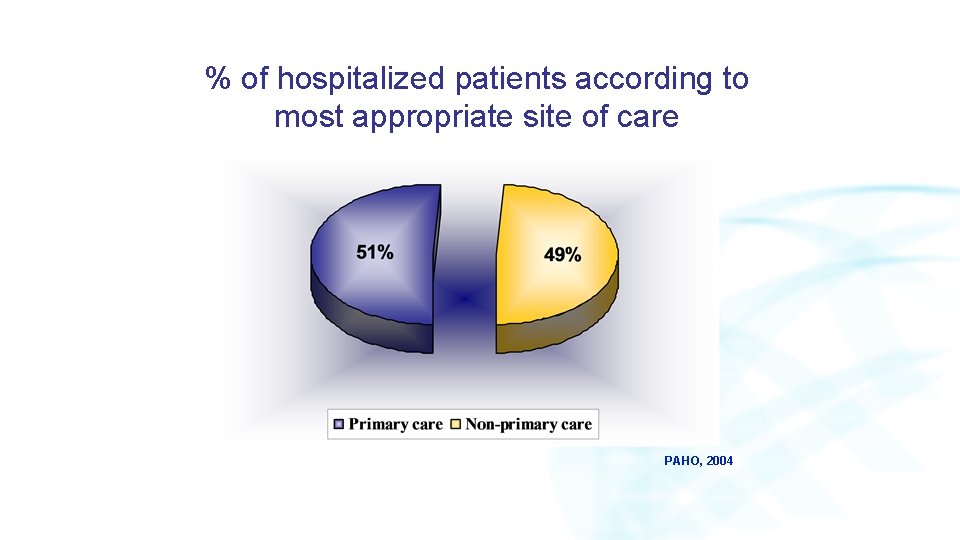
% of hospitalized patients according to most appropriate site of care PAHO, 2004
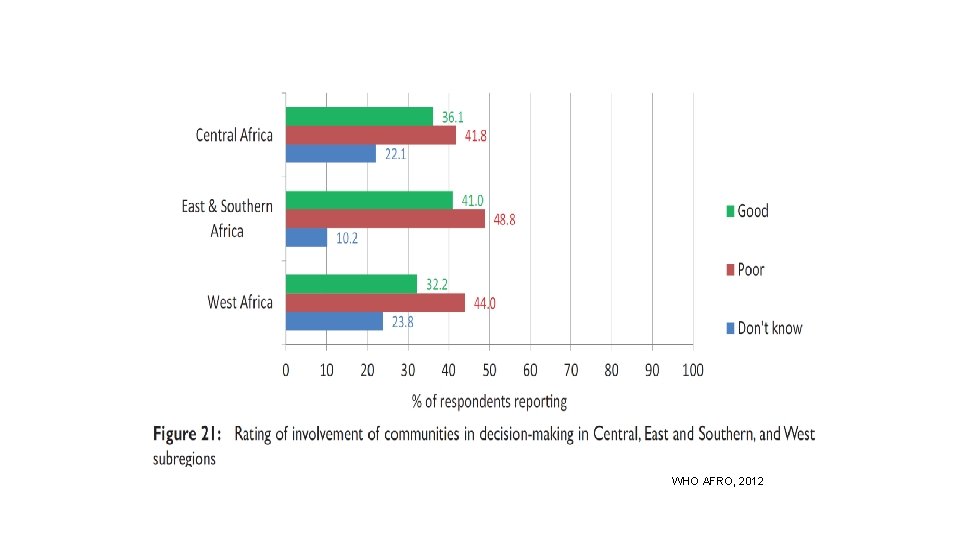
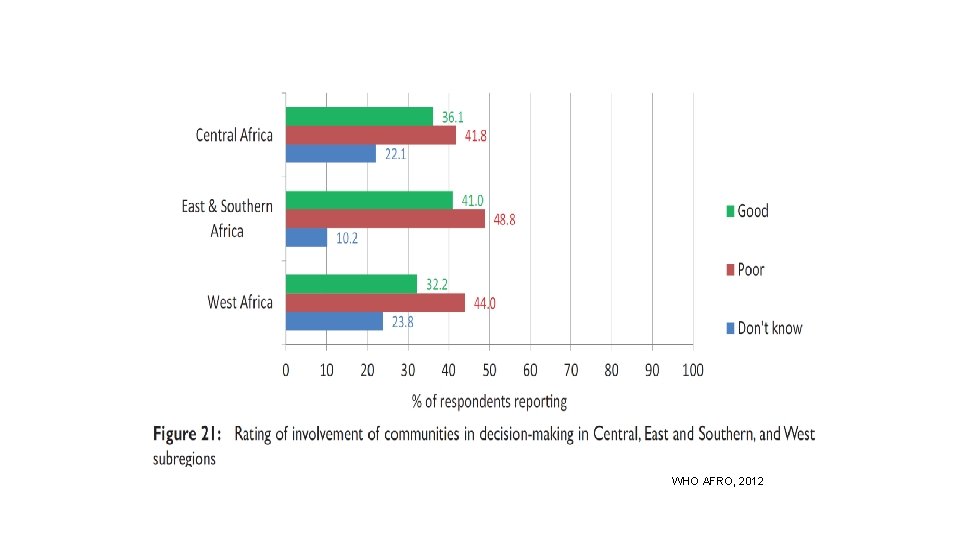
WHO AFRO, 2012
Strengthening a global commitment to people centred integrated health services delivery

Peoplecentred and integrated health services in the NUKA health system, Alaska, USA Promoting HIV/AIDS literacy in Angola Integrated health care networks in Chile Case management in Torbay, UK Integrated health care networks in Brazil Social participation in Tupiza, Bolivia Shared accountabilit y contract for population health outcomes, Kinzigtal, Germany Promoting service coordination in Lithuania Balanced Integrated scorecard to care in South promote Karelia, accountability, Finland Afghanistan What are the experiences to date? Integrating HIV/AIDS and TB in Mali Mobilizing communities to reduce maternal and neonatal deaths in Malawi Family medicine in Thailand as part of UHC Integrating traditional and complementa ry medicine in Asia Communityowned primary care networks in Mali
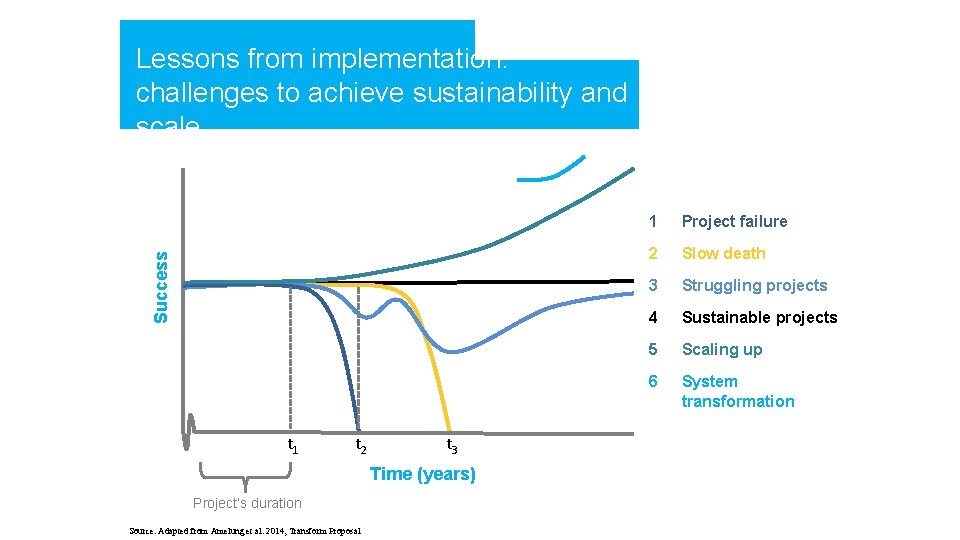
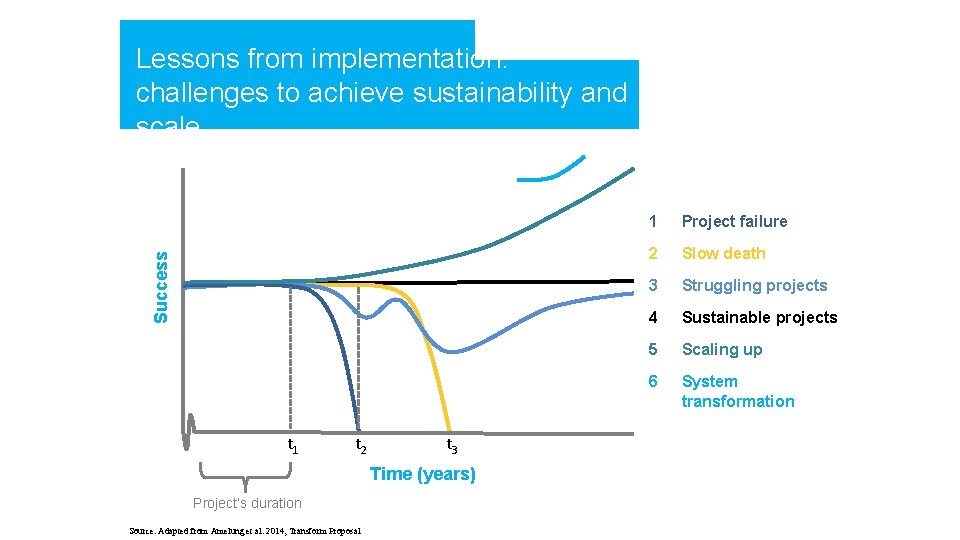
Success Lessons from implementation: challenges to achieve sustainability and scale t 1 t 2 t 3 Time (years) Project’s duration Source: Adapted from Amelung et al. 2014, Transform Proposal 1 Project failure 2 Slow death 3 Struggling projects 4 Sustainable projects 5 Scaling up 6 System transformation
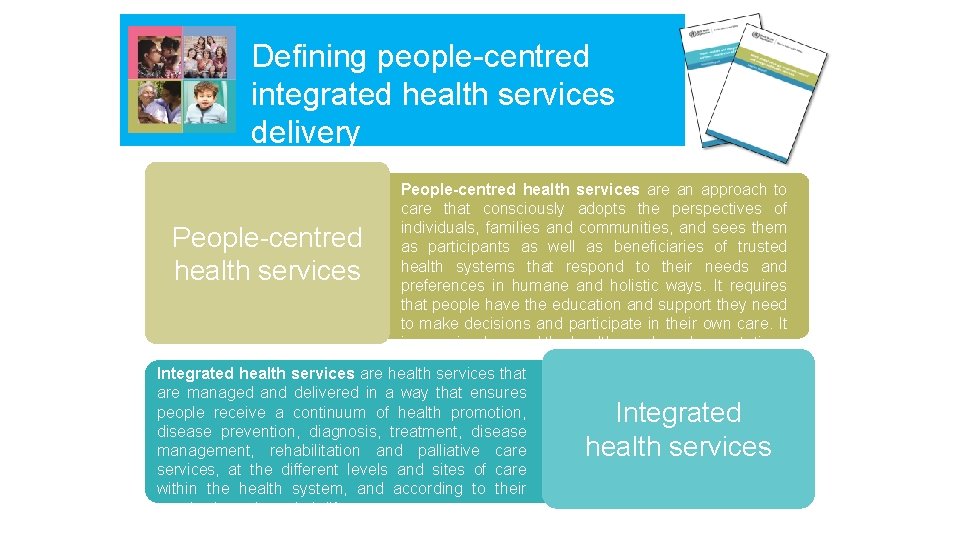
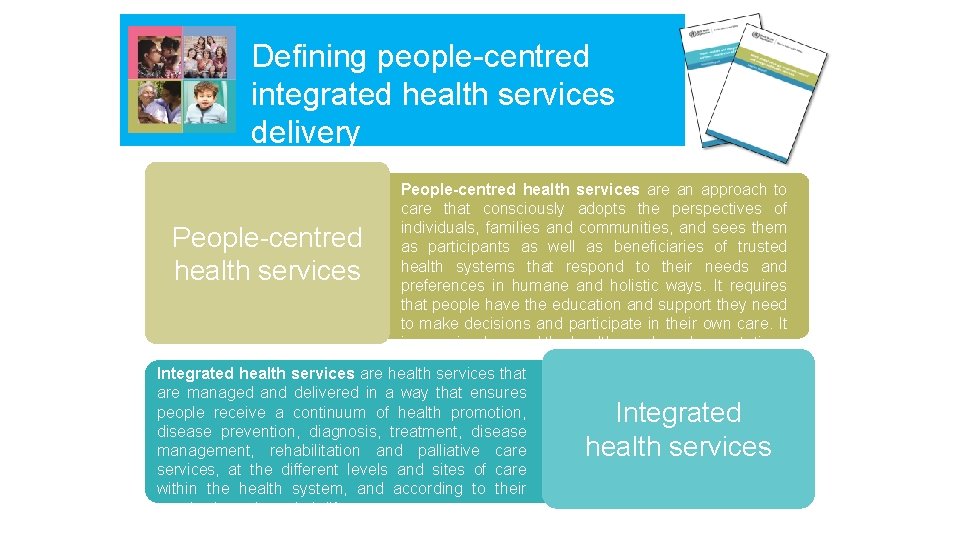
Defining people-centred integrated health services delivery People-centred health services are an approach to care that consciously adopts the perspectives of individuals, families and communities, and sees them as participants as well as beneficiaries of trusted health systems that respond to their needs and preferences in humane and holistic ways. It requires that people have the education and support they need to make decisions and participate in their own care. It is organized around the health needs and expectations of people rather than diseases. Integrated health services are health services that are managed and delivered in a way that ensures people receive a continuum of health promotion, disease prevention, diagnosis, treatment, disease management, rehabilitation and palliative care services, at the different levels and sites of care within the health system, and according to their needs, throughout their life course. People-centred health services Integrated health services

Improved access to care for marginalized groups Reduced unplanned hospitalizations Shared decisionmaking Shift in the balance of care, allocating resources closer to needs Increased access to care Greater community influence & better relationships with care providers that build awareness and trust Increased ability to selfmanage Workforce role enhancement Reduced costs What outcomes have been achieved? Improved health literacy Reduced perinatal and neonatal mortality Increased health coverage Greater community engagement & participatory representation Better coordination of care Greater quality of care
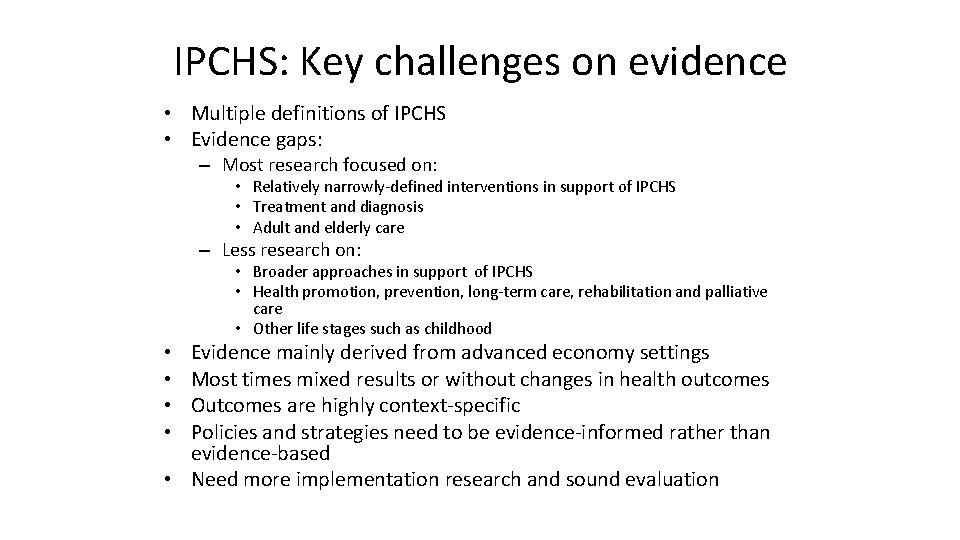
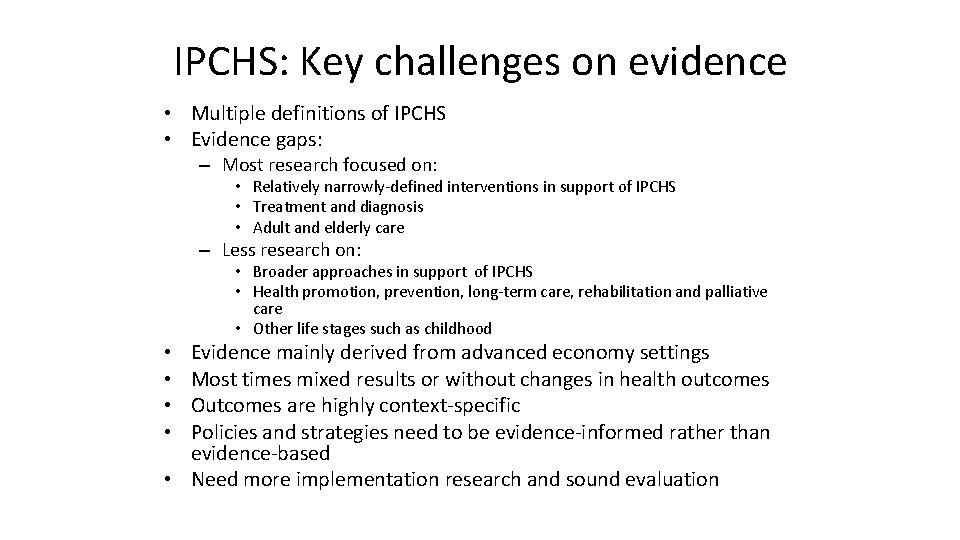
IPCHS: Key challenges on evidence • Multiple definitions of IPCHS • Evidence gaps: – Most research focused on: • Relatively narrowly-defined interventions in support of IPCHS • Treatment and diagnosis • Adult and elderly care – Less research on: • Broader approaches in support of IPCHS • Health promotion, prevention, long-term care, rehabilitation and palliative care • Other life stages such as childhood Evidence mainly derived from advanced economy settings Most times mixed results or without changes in health outcomes Outcomes are highly context-specific Policies and strategies need to be evidence-informed rather than evidence-based • Need more implementation research and sound evaluation • •
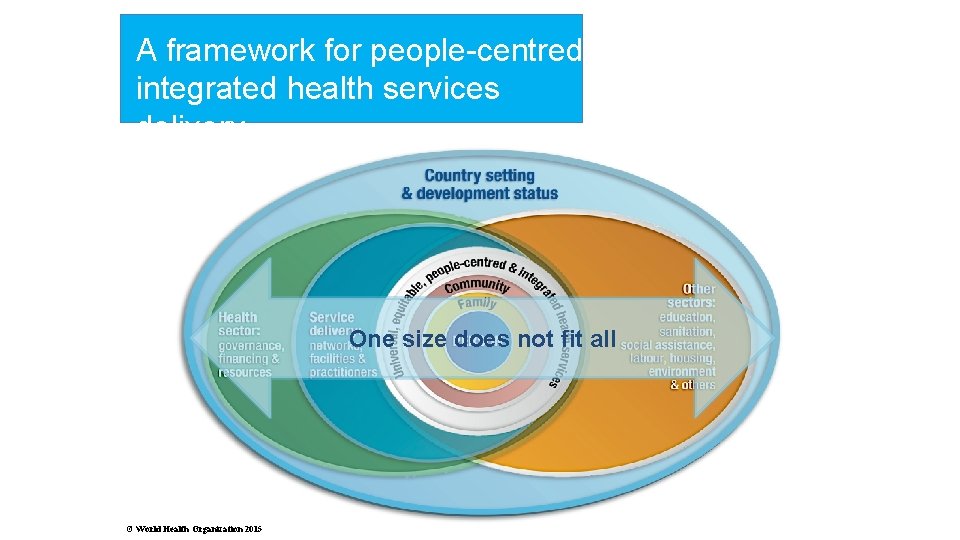
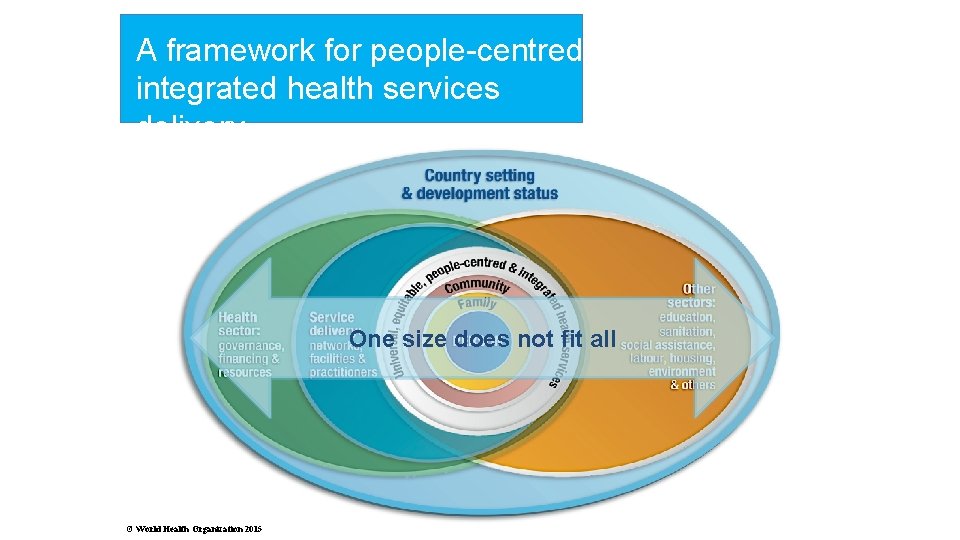
A framework for people-centred integrated health services delivery One size does not fit all © World Health Organization 2015
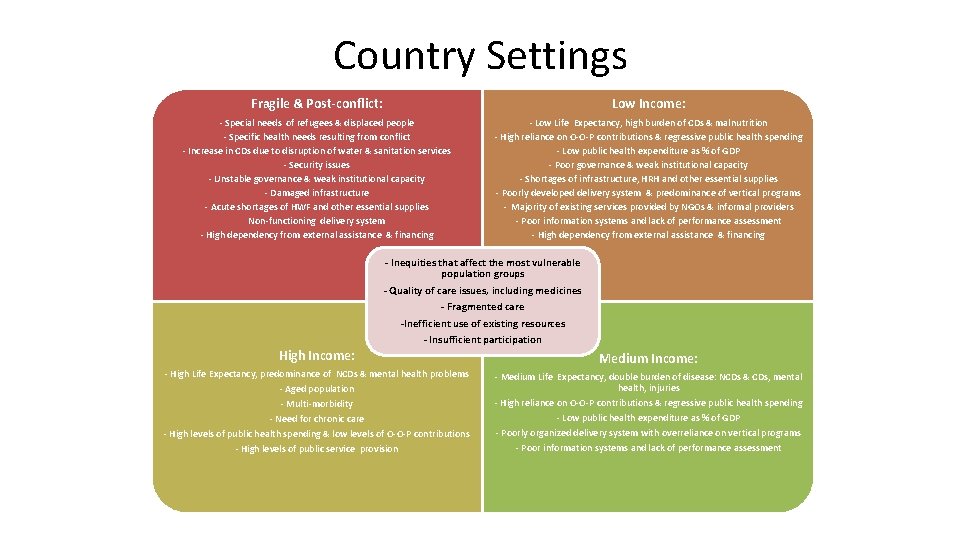
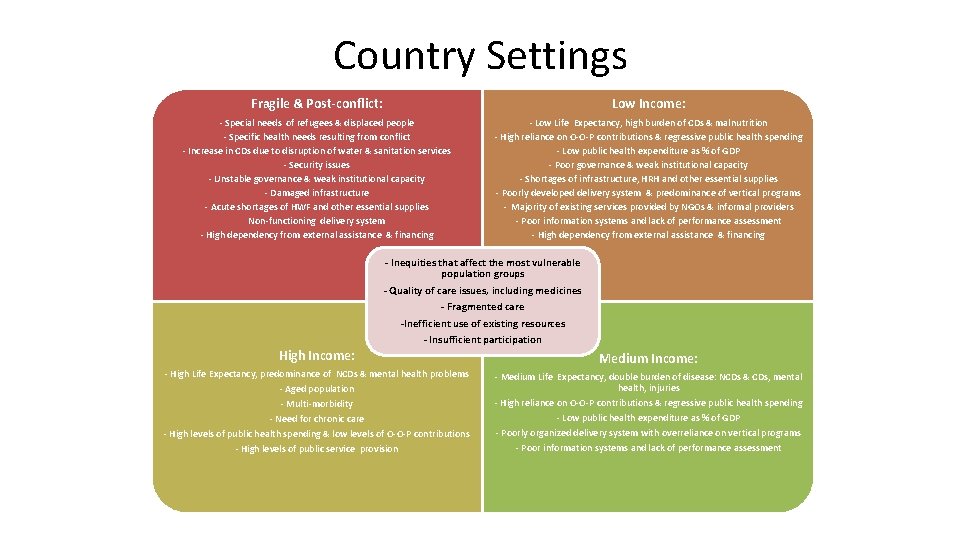
Country Settings Fragile & Post-conflict: Low Income: - Special needs of refugees & displaced people - Specific health needs resulting from conflict - Increase in CDs due to disruption of water & sanitation services - Security issues - Unstable governance & weak institutional capacity - Damaged infrastructure - Acute shortages of HWF and other essential supplies Non-functioning delivery system - High dependency from external assistance & financing - Low Life Expectancy, high burden of CDs & malnutrition - High reliance on O-O-P contributions & regressive public health spending - Low public health expenditure as % of GDP - Poor governance & weak institutional capacity - Shortages of infrastructure, HRH and other essential supplies - Poorly developed delivery system & predominance of vertical programs - Majority of existing services provided by NGOs & informal providers - Poor information systems and lack of performance assessment - High dependency from external assistance & financing - Inequities that affect the most vulnerable population groups - Quality of care issues, including medicines - Fragmented care High Income: -Inefficient use of existing resources - Insufficient participation - High Life Expectancy, predominance of NCDs & mental health problems - Aged population - Multi-morbidity - Need for chronic care - High levels of public health spending & low levels of O-O-P contributions - High levels of public service provision Medium Income: - Medium Life Expectancy, double burden of disease: NCDs & CDs, mental health, injuries - High reliance on O-O-P contributions & regressive public health spending - Low public health expenditure as % of GDP - Poorly organized delivery system with overreliance on vertical programs - Poor information systems and lack of performance assessment
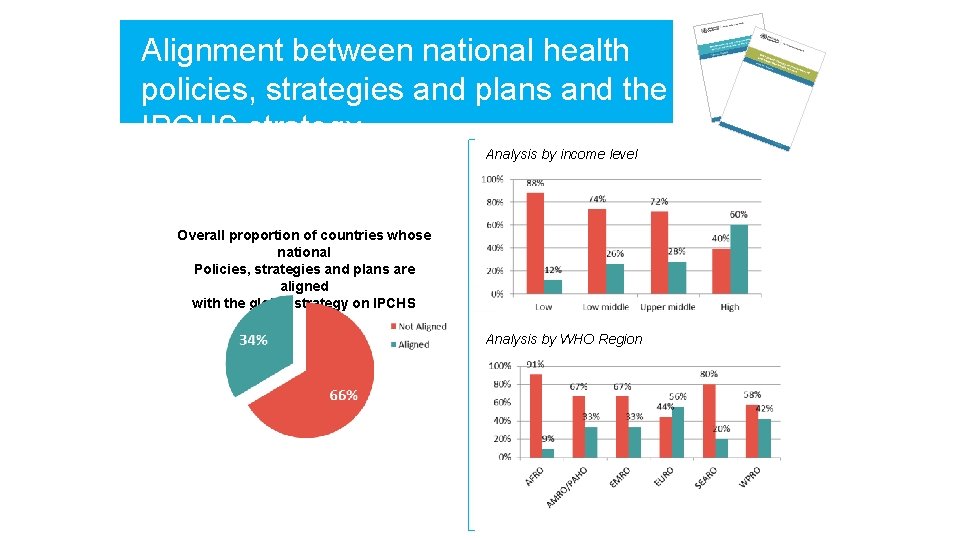
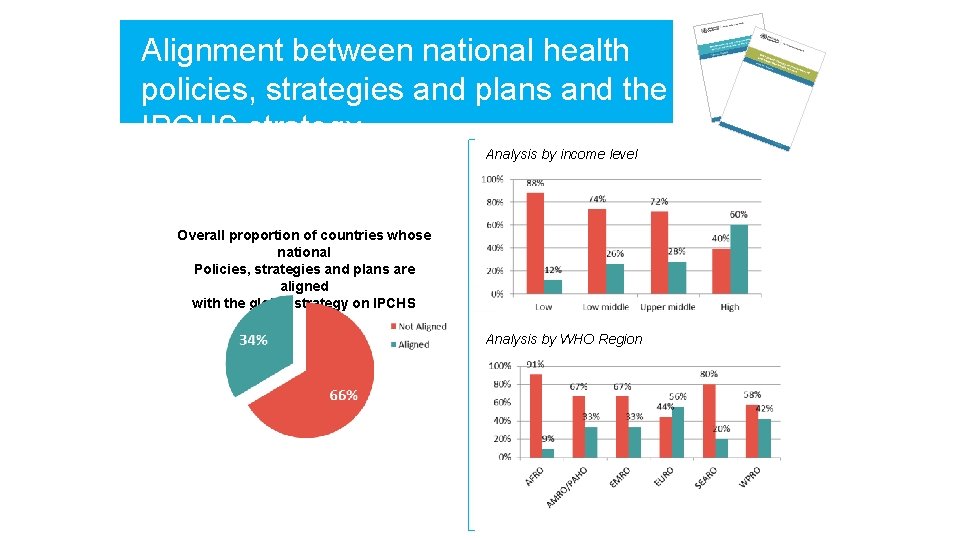
Alignment between national health policies, strategies and plans and the IPCHS strategy Analysis by income level Overall proportion of countries whose national Policies, strategies and plans are aligned with the global strategy on IPCHS Analysis by WHO Region
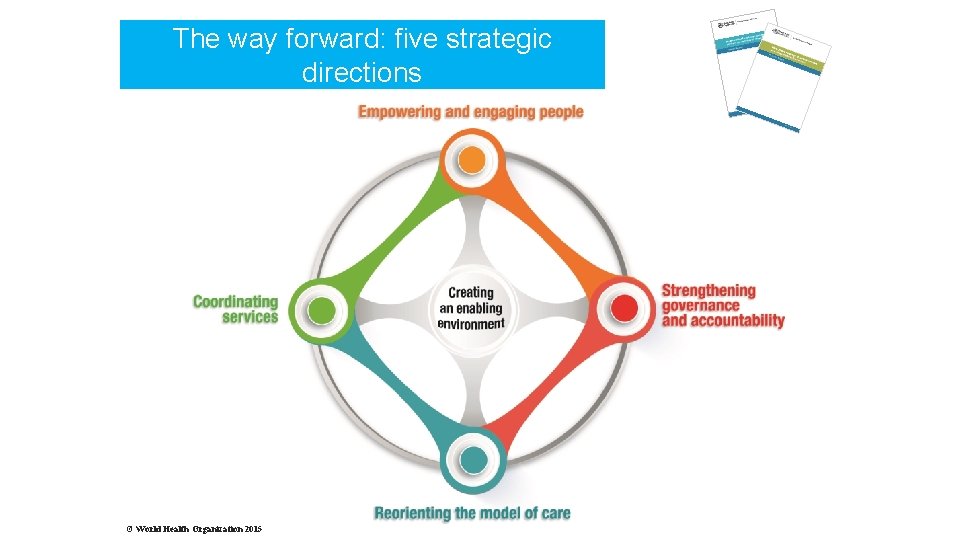
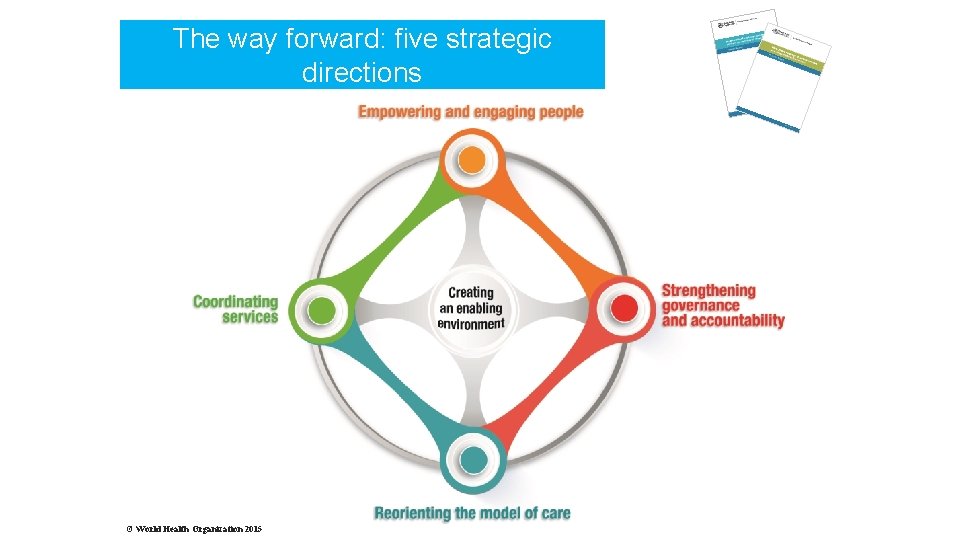
The way forward: five strategic directions © World Health Organization 2015
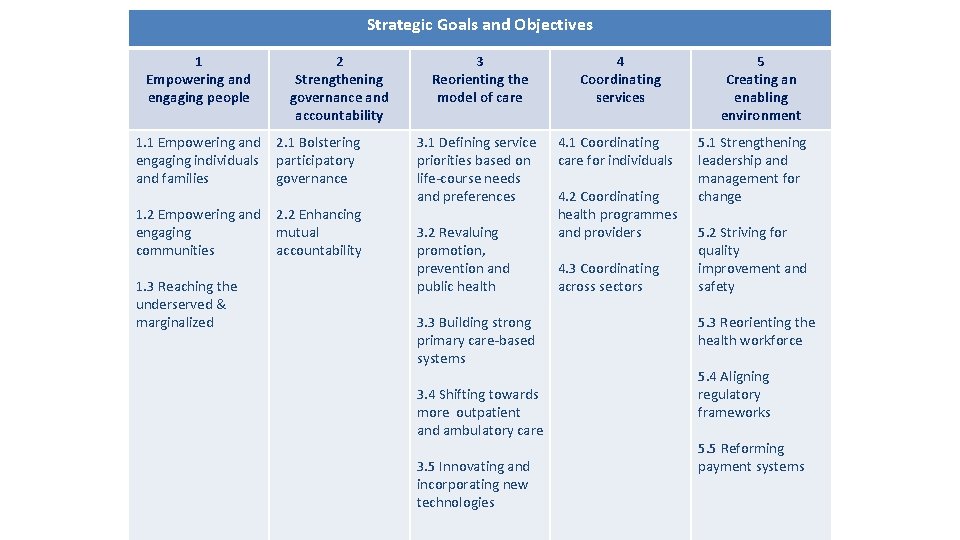
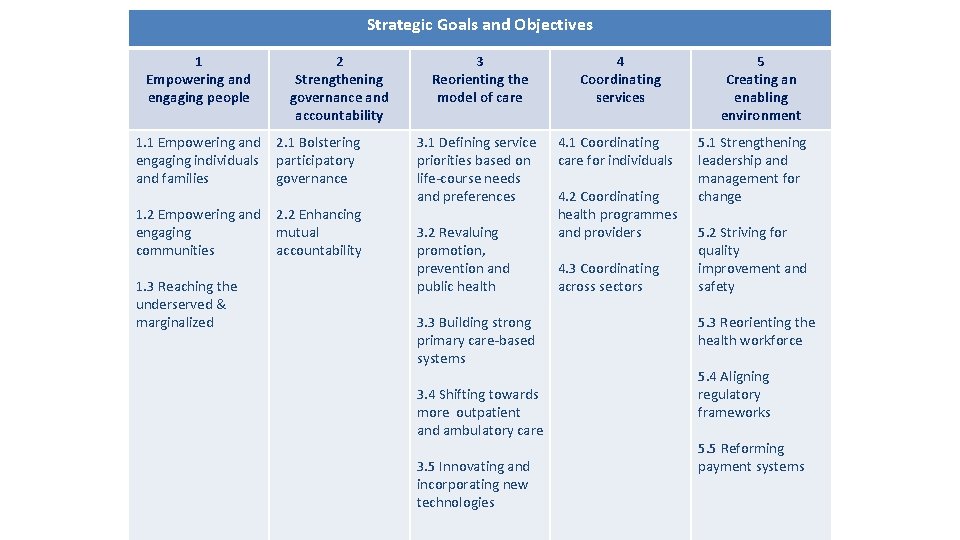
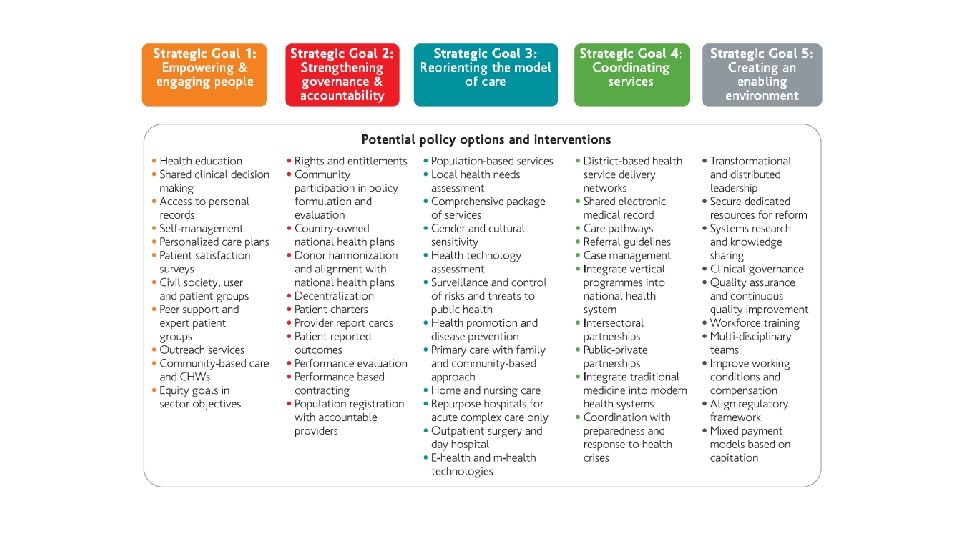
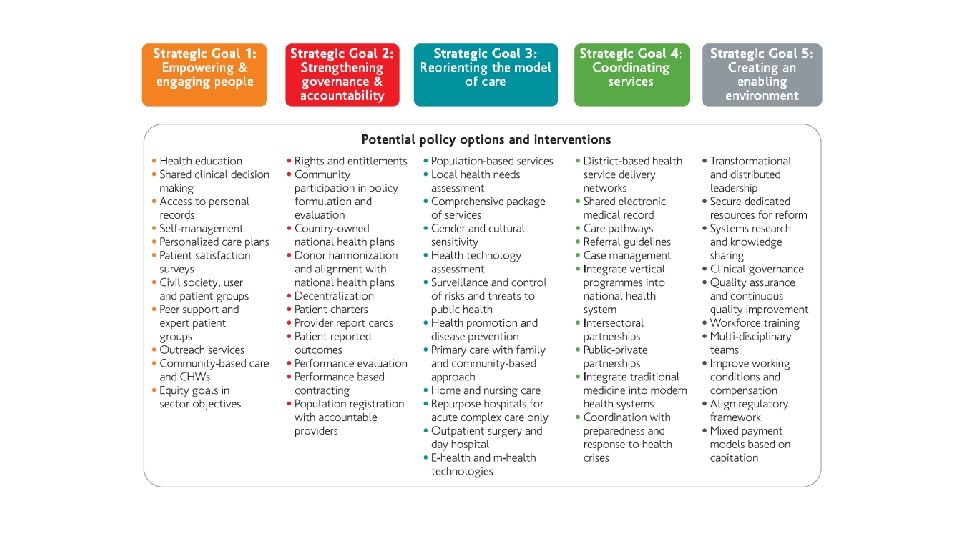
Strategic Goals and Objectives 1 Empowering and engaging people 2 Strengthening governance and accountability 1. 1 Empowering and engaging individuals and families 2. 1 Bolstering participatory governance 1. 2 Empowering and engaging communities 2. 2 Enhancing mutual accountability 1. 3 Reaching the underserved & marginalized 3 Reorienting the model of care 3. 1 Defining service priorities based on life-course needs and preferences 3. 2 Revaluing promotion, prevention and public health 3. 3 Building strong primary care-based systems 3. 4 Shifting towards more outpatient and ambulatory care 3. 5 Innovating and incorporating new technologies 4 Coordinating services 4. 1 Coordinating care for individuals 4. 2 Coordinating health programmes and providers 4. 3 Coordinating across sectors 5 Creating an enabling environment 5. 1 Strengthening leadership and management for change 5. 2 Striving for quality improvement and safety 5. 3 Reorienting the health workforce 5. 4 Aligning regulatory frameworks 5. 5 Reforming payment systems
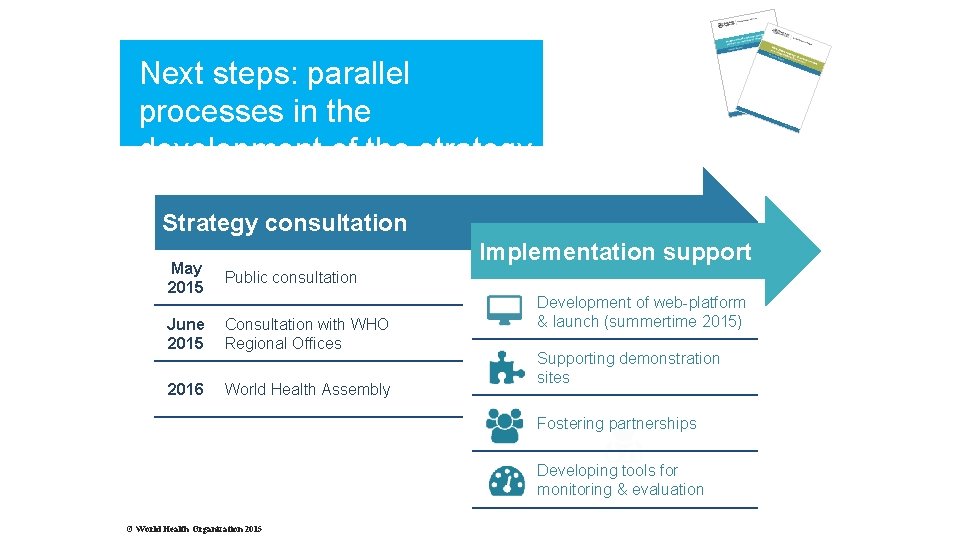
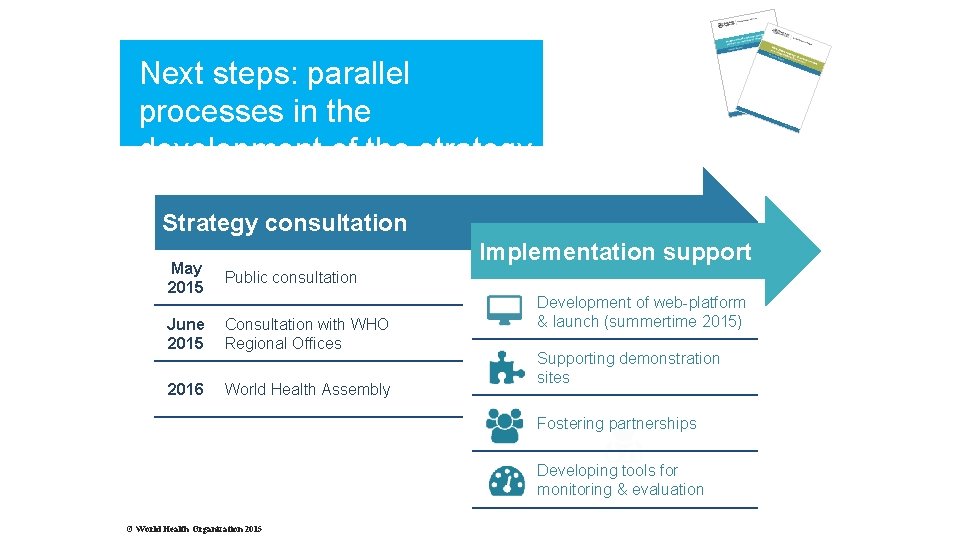
Next steps: parallel processes in the development of the strategy Strategy consultation Implementation support May 2015 Public consultation June 2015 Consultation with WHO Regional Offices 2016 World Health Assembly Development of web-platform & launch (summertime 2015) Supporting demonstration sites Fostering partnerships Developing tools for monitoring & evaluation © World Health Organization 2015
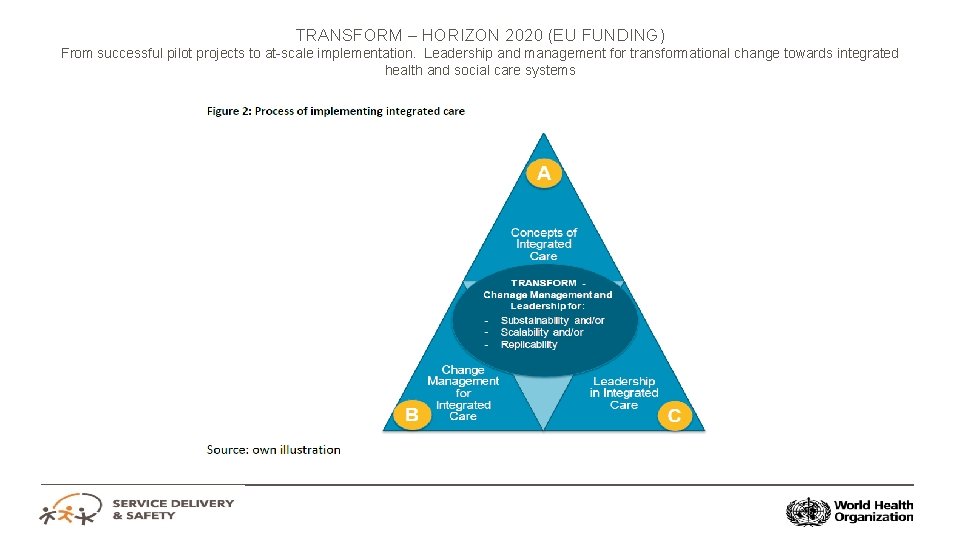
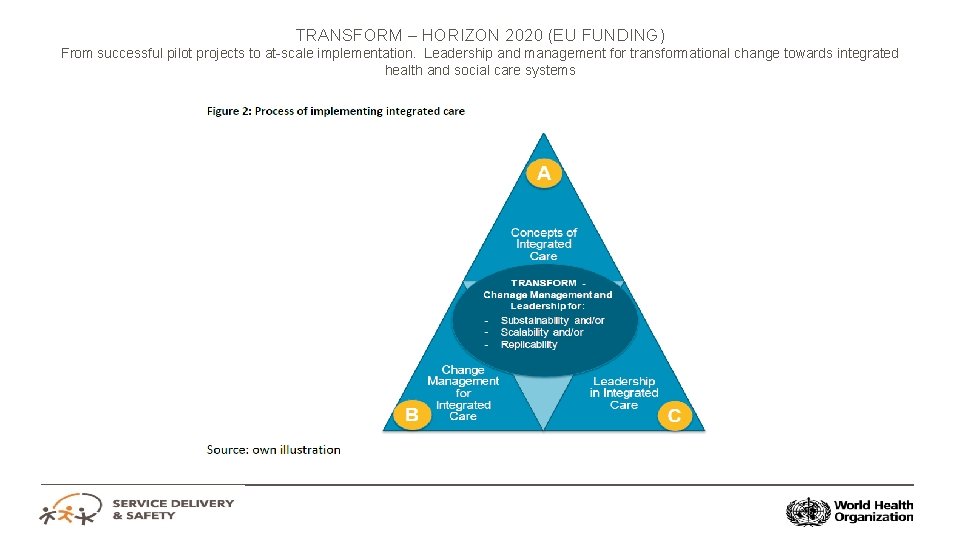
TRANSFORM – HORIZON 2020 (EU FUNDING) From successful pilot projects to at-scale implementation. Leadership and management for transformational change towards integrated health and social care systems
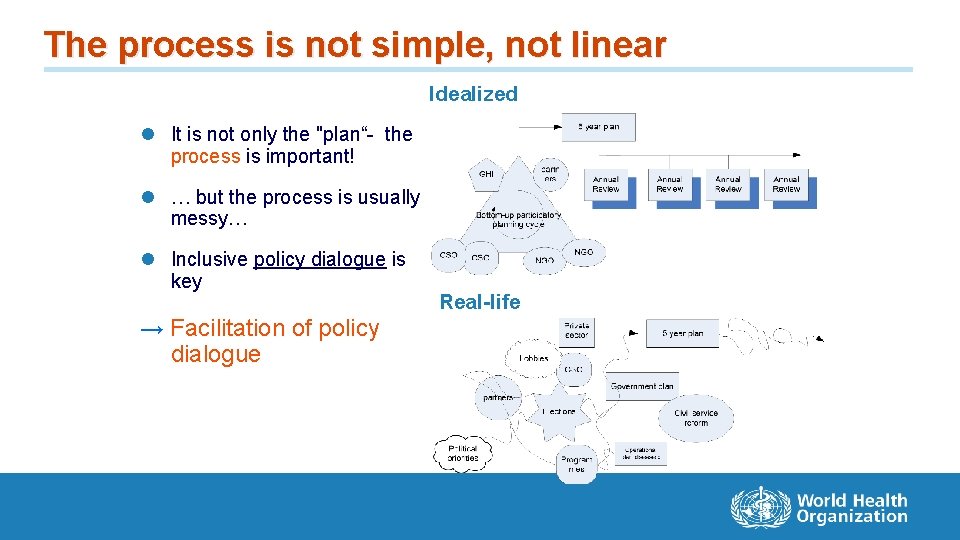
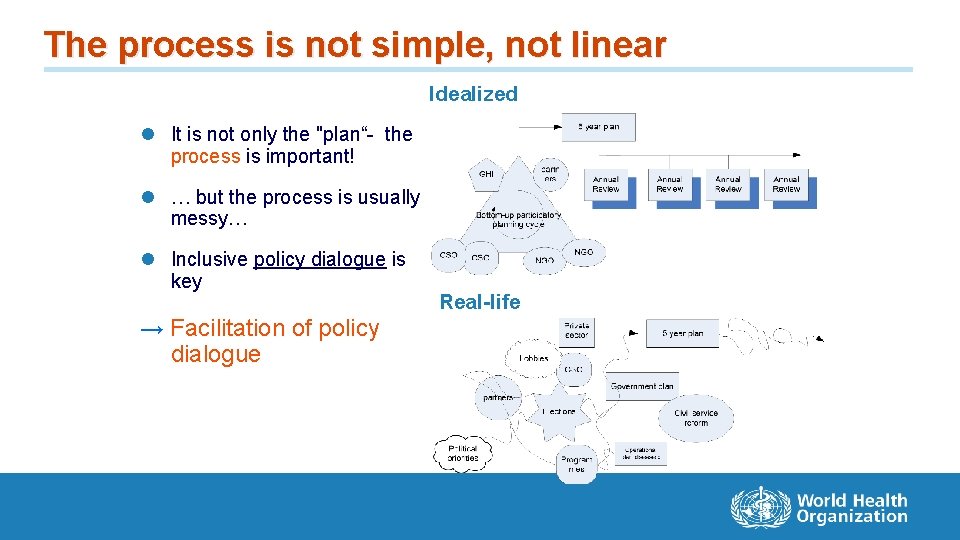
The process is not simple, not linear Idealized l It is not only the "plan“- the process is important! l … but the process is usually messy… l Inclusive policy dialogue is key → Facilitation of policy dialogue Real-life
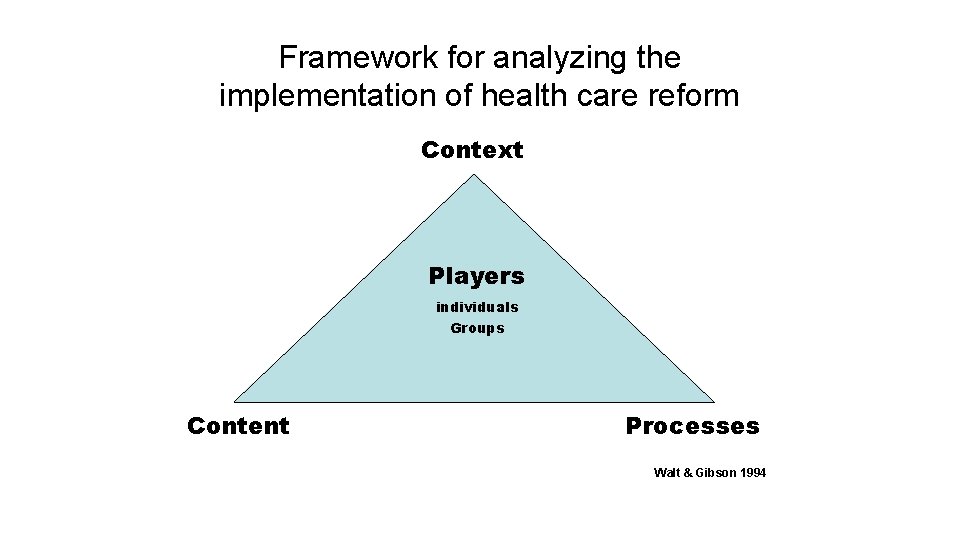
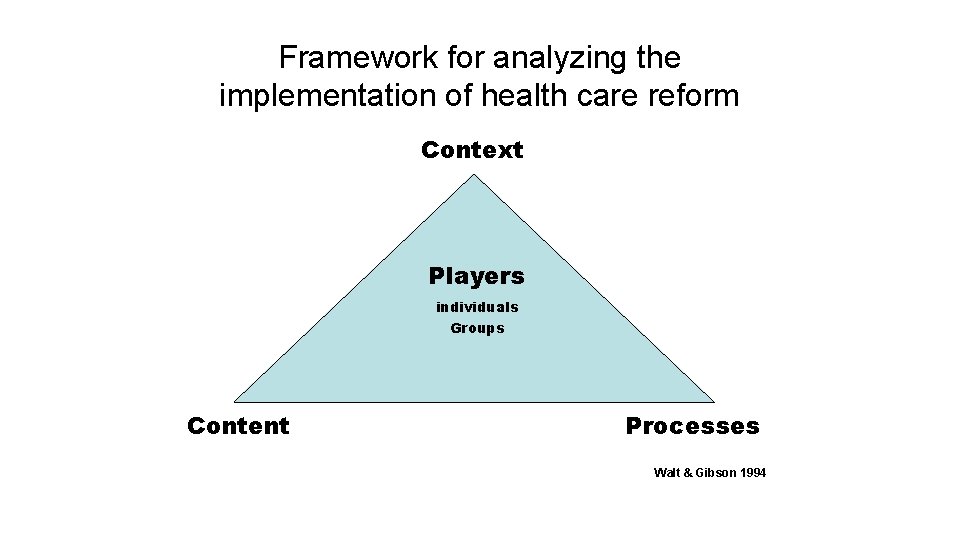
Framework for analyzing the implementation of health care reform Context Players individuals Groups Content Processes Walt & Gibson 1994
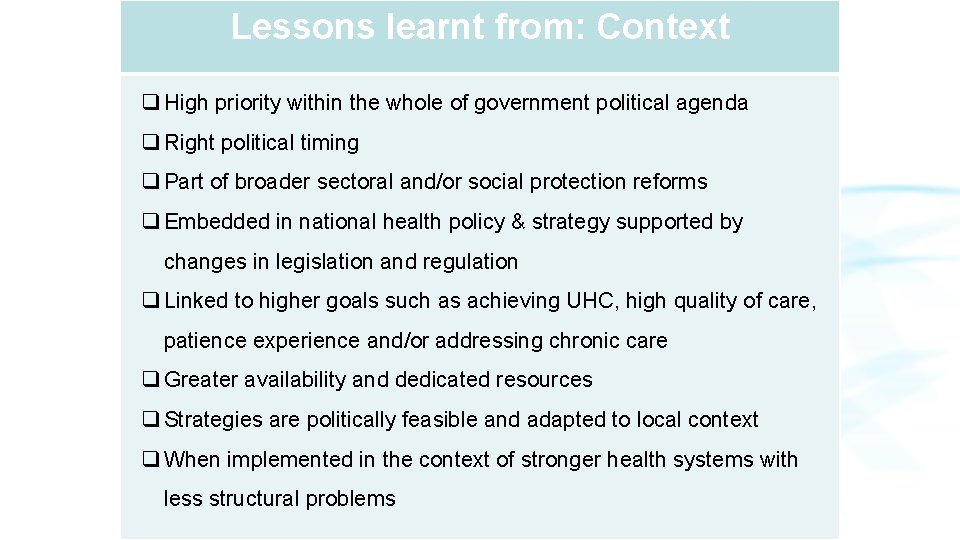
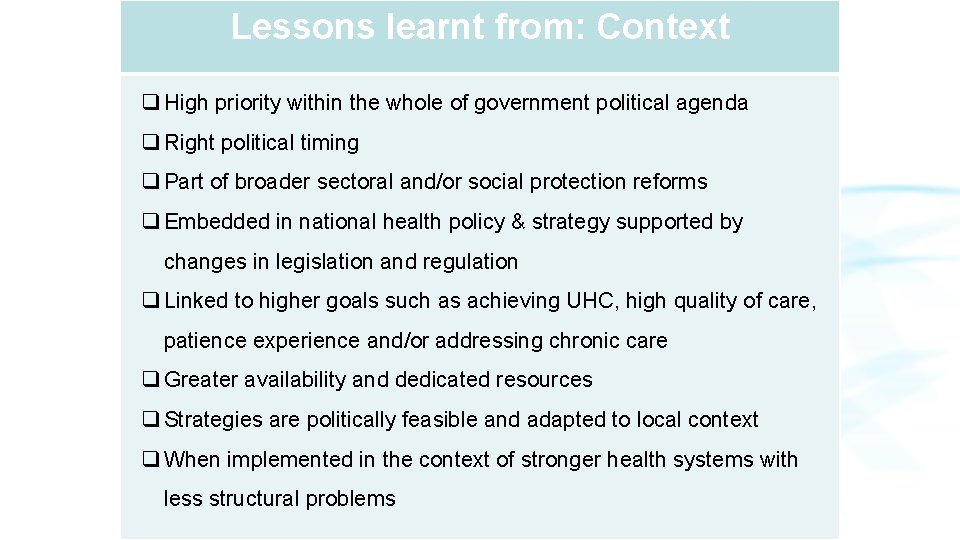
Lessons learnt from: Context q High priority within the whole of government political agenda q Right political timing q Part of broader sectoral and/or social protection reforms q Embedded in national health policy & strategy supported by changes in legislation and regulation q Linked to higher goals such as achieving UHC, high quality of care, patience experience and/or addressing chronic care q Greater availability and dedicated resources q Strategies are politically feasible and adapted to local context q When implemented in the context of stronger health systems with less structural problems
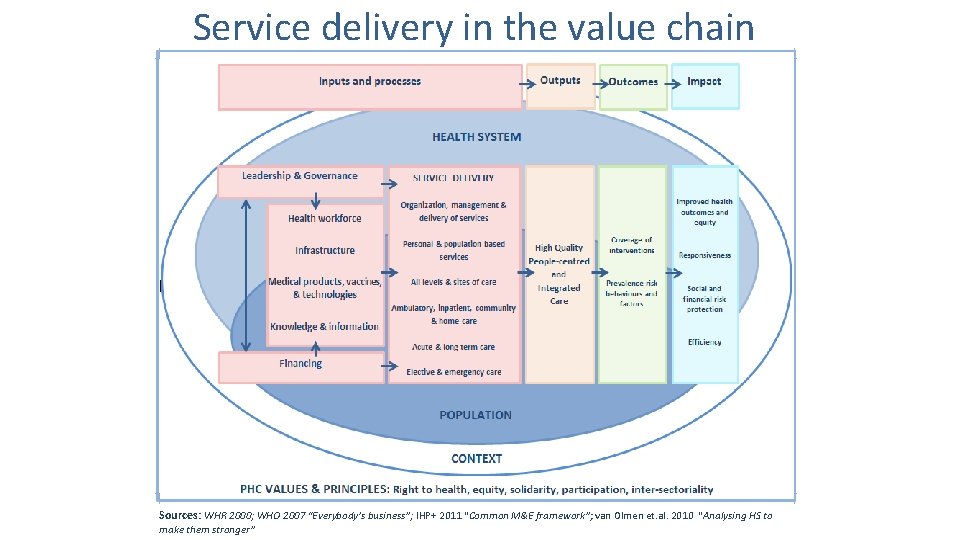
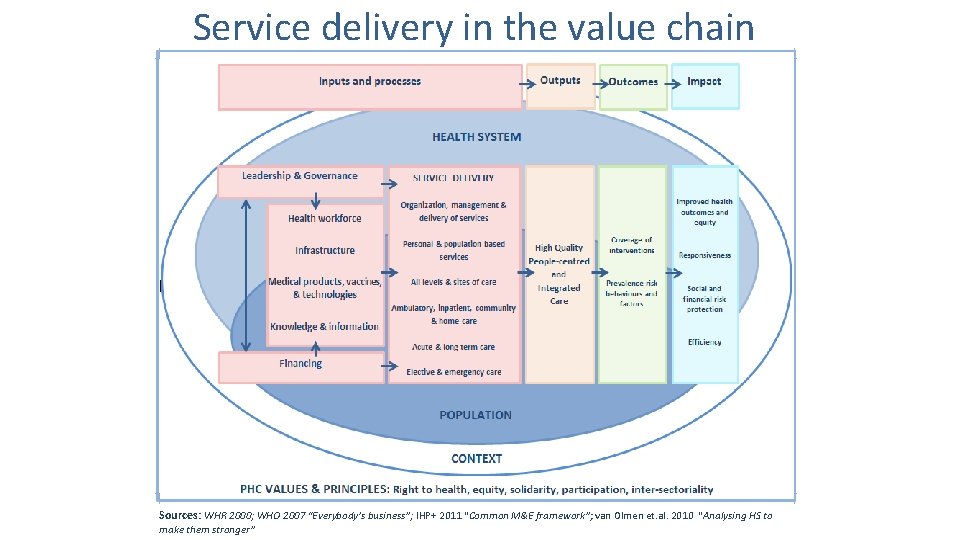
Service delivery in the value chain Sources: WHR 2000; WHO 2007 “Everybody’s business”; IHP+ 2011 “Common M&E framework”; van Olmen et. al. 2010 “Analysing HS to make them stronger”
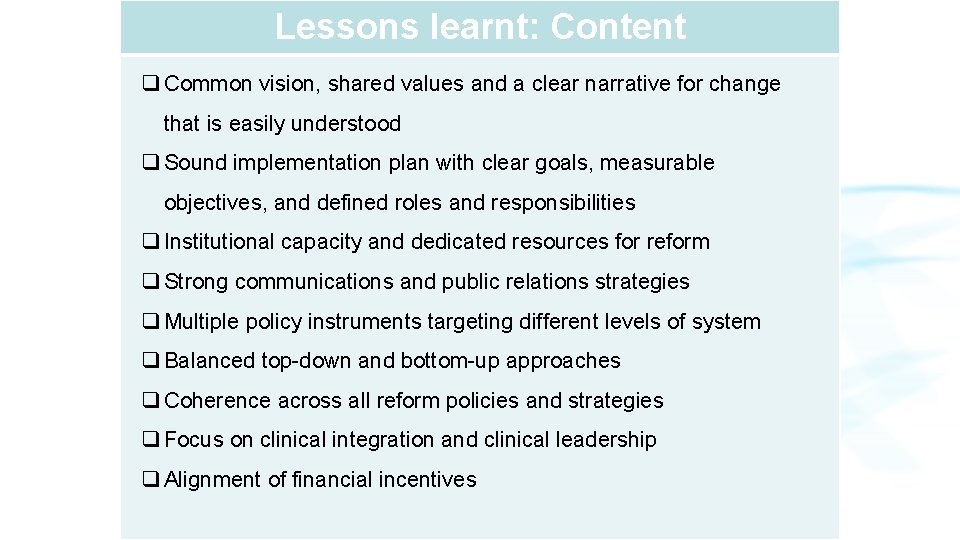
Lessons learnt: Content q Common vision, shared values and a clear narrative for change that is easily understood q Sound implementation plan with clear goals, measurable objectives, and defined roles and responsibilities q Institutional capacity and dedicated resources for reform q Strong communications and public relations strategies q Multiple policy instruments targeting different levels of system q Balanced top-down and bottom-up approaches q Coherence across all reform policies and strategies q Focus on clinical integration and clinical leadership q Alignment of financial incentives
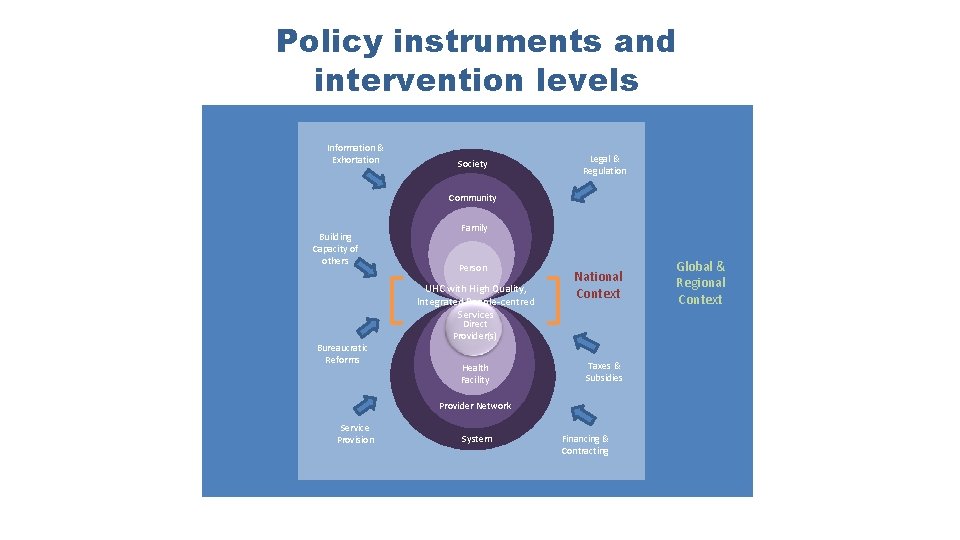
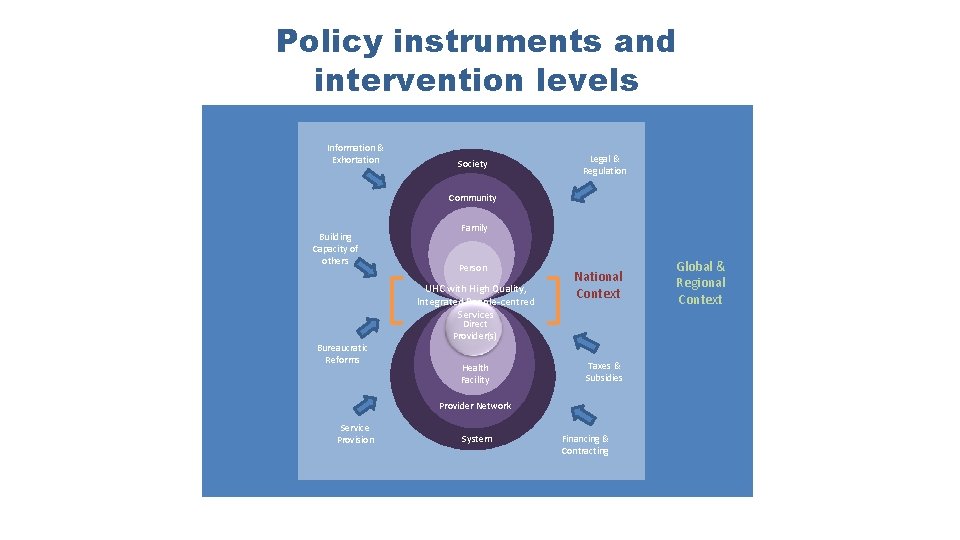
Policy instruments and intervention levels Information & Exhortation Society Legal & Regulation Community Building Capacity of others Family Person UHC with High Quality, Integrated People-centred Services Bureaucratic Reforms National Context Direct Provider(s) Health Facility Taxes & Subsidies Provider Network Service Provision System Financing & Contracting Global & Regional Context
Lessons learnt: Processes q Processes are complex, difficult and long-term q Sustained political will, leadership and policy direction over time q Build from existing structures and strengths q Different speeds depending on political context: "big-bang" versus gradual, incremental q Experiment and test innovative approaches, allow for failure q Take advantage of low hanging fruits and demonstrate early gains through measurable results q Use demonstration sites and spread knowledge gains
Lessons learnt: Actors q Patients, users, and service providers should be involved in all stages of reform q Support from the public and strategic alliances q Quality interpersonal and inter-institutional relations, including: willingness to change, trust, credibility, appreciation, and sense of belonging q Close gap between policy makers, managers, providers and users through spaces for open dialogue and exchanges
CONTACT INFORMATION Services Delivery and Safety Department World Health Organization Avenue Appia 20 CH-1211, Geneva 27 Switzerland For more information on health services delivery visit http: //www. who. int/servicedeliverysafety/areas/p eople-centred-care/en/