INTEGRATED CARE PATHWAYS An essential toolkit in addressing

- Slides: 22
INTEGRATED CARE PATHWAYS An essential toolkit in addressing alcohol related harm Martyn Penfold Consultant in health and social care The views expressed are those of the speaker and may not necessarily reflect those of Lundbeck
Alcohol related harm is a present and growing threat to public health and to the NHS. A comprehensive and effective response is critical to the delivery of the public health framework and to the ability of the NHS to meet both its financial and population challenges.
INTEGRATED CARE PATHWAYS An essential toolkit in addressing alcohol related harm Martyn Penfold Consultant in health and social care This meeting is organised and funded by Lundbeck Ltd The views expressed are those of the speaker and may not necessarily reflect those of Lundbeck Prescribing and adverse event reporting information can be found on the last slide Date of preparation: May 2013 UK/LUK/1303/0143 d
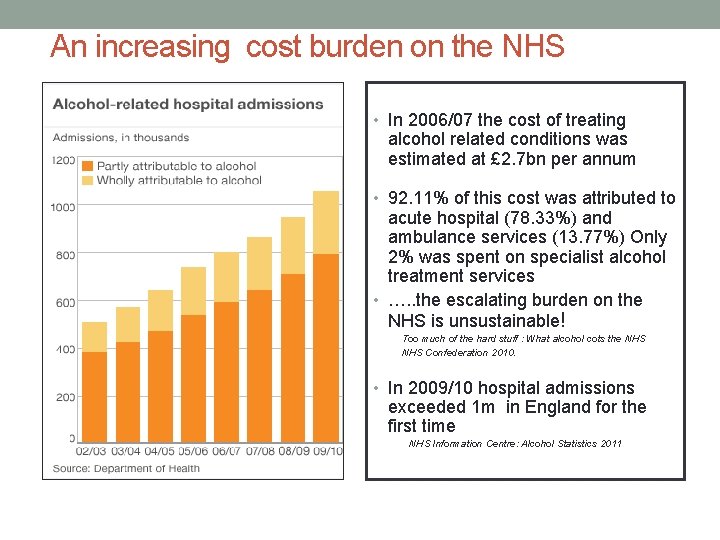
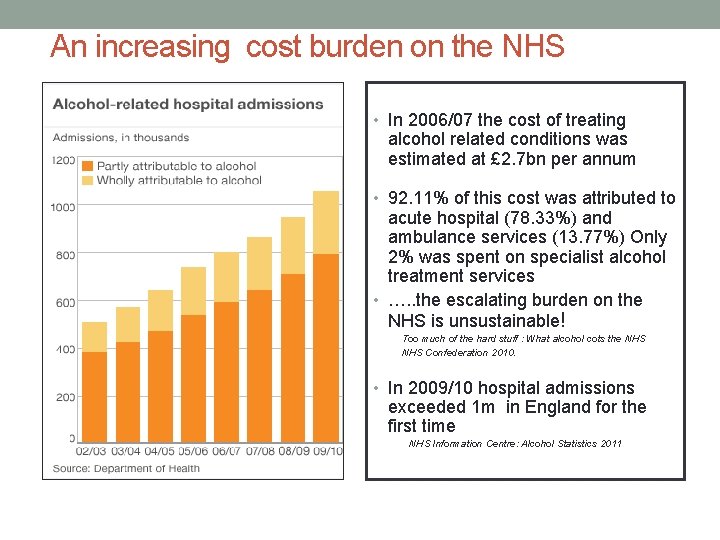
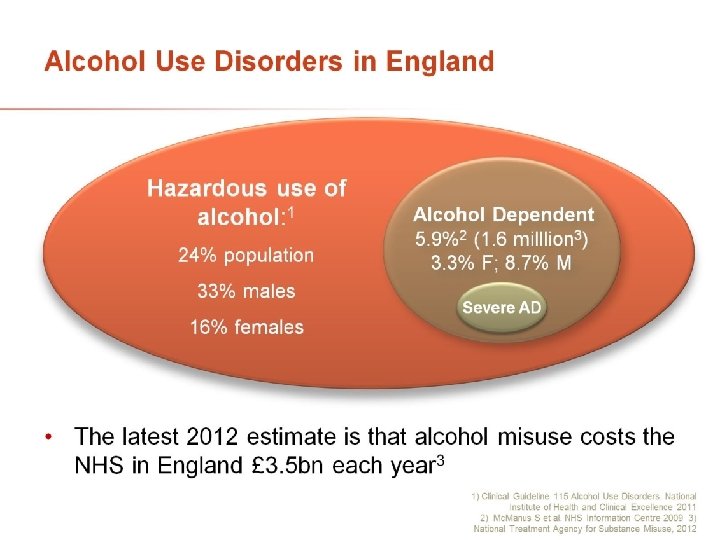
An increasing cost burden on the NHS • In 2006/07 the cost of treating alcohol related conditions was estimated at £ 2. 7 bn per annum • 92. 11% of this cost was attributed to acute hospital (78. 33%) and ambulance services (13. 77%) Only 2% was spent on specialist alcohol treatment services • …. . the escalating burden on the NHS is unsustainable! Too much of the hard stuff : What alcohol cots the NHS Confederation 2010. • In 2009/10 hospital admissions exceeded 1 m in England for the first time NHS Information Centre: Alcohol Statistics 2011
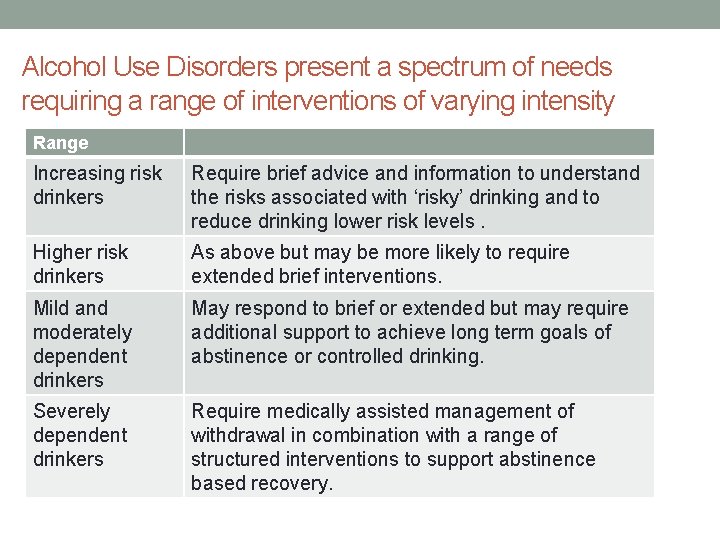
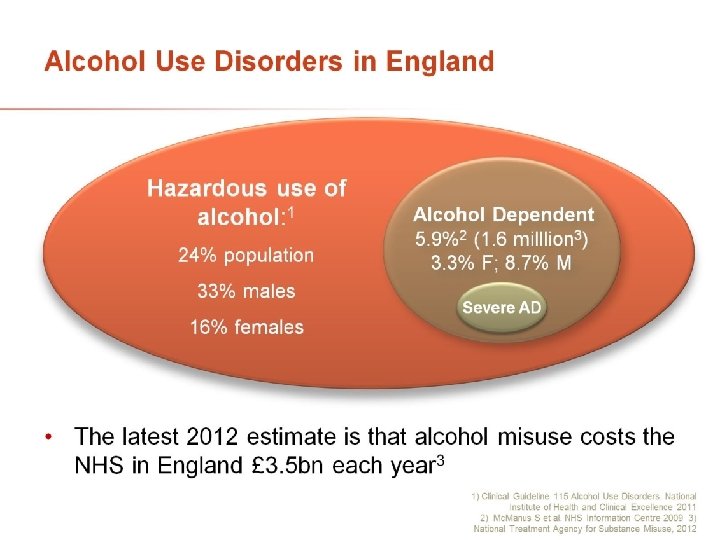
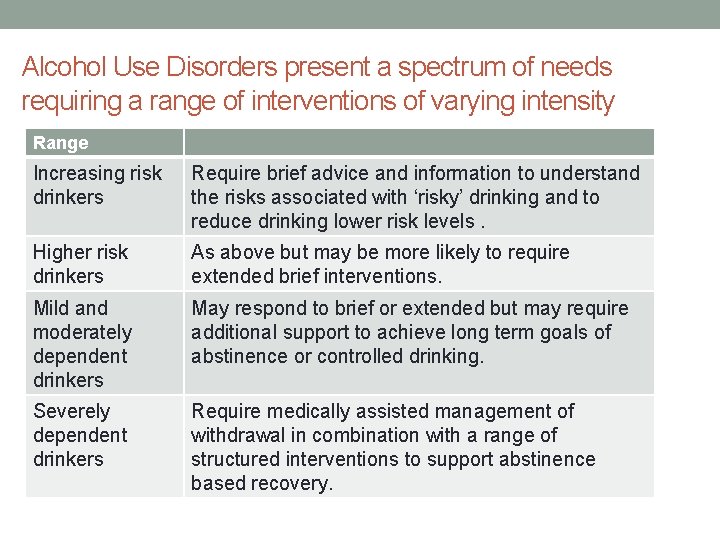
Alcohol Use Disorders present a spectrum of needs requiring a range of interventions of varying intensity Range Increasing risk drinkers Require brief advice and information to understand the risks associated with ‘risky’ drinking and to reduce drinking lower risk levels. Higher risk drinkers As above but may be more likely to require extended brief interventions. Mild and moderately dependent drinkers May respond to brief or extended but may require additional support to achieve long term goals of abstinence or controlled drinking. Severely dependent drinkers Require medically assisted management of withdrawal in combination with a range of structured interventions to support abstinence based recovery.
DEVELOPING THE INTEGRATED CARE PATHWAY FOR ALCOHOL USE DISORDERS
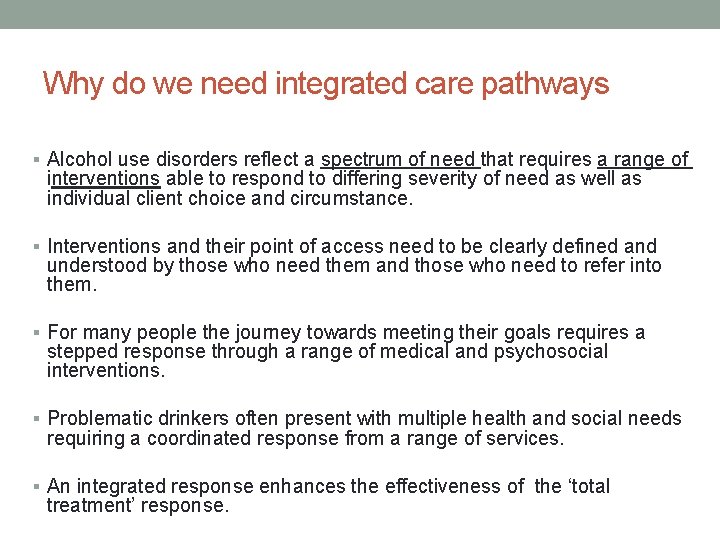
Why do we need integrated care pathways § Alcohol use disorders reflect a spectrum of need that requires a range of interventions able to respond to differing severity of need as well as individual client choice and circumstance. § Interventions and their point of access need to be clearly defined and understood by those who need them and those who need to refer into them. § For many people the journey towards meeting their goals requires a stepped response through a range of medical and psychosocial interventions. § Problematic drinkers often present with multiple health and social needs requiring a coordinated response from a range of services. § An integrated response enhances the effectiveness of the ‘total treatment’ response.
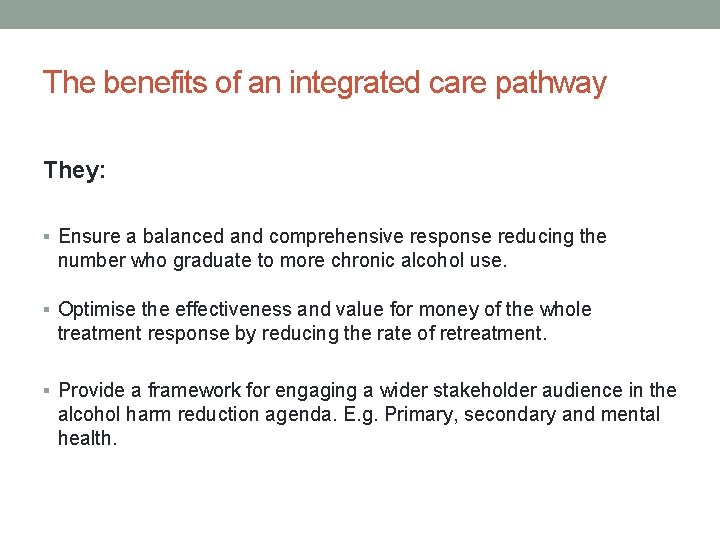
The benefits of an integrated care pathway They: § Ensure a balanced and comprehensive response reducing the number who graduate to more chronic alcohol use. § Optimise the effectiveness and value for money of the whole treatment response by reducing the rate of retreatment. § Provide a framework for engaging a wider stakeholder audience in the alcohol harm reduction agenda. E. g. Primary, secondary and mental health.
What are the key stages in developing an integrated treatment pathway for alcohol misuse? § Understanding the level and diversity of need to be met § Reviewing the impact of alcohol related on a range of services § Assessing existing responses against local needs, and reviewing them against the available evidence base for effectiveness. § Prioritise available resources § Define: - Range of interventions to be delivered - Point and criteria for access - Pathways between interventions - Quality standards and outcome measurements

Integrated Care Pathway Tool • Mr Eric Appleby - CEO Alcohol • • • Concern Prof John Ashton - Public Health Consultant Dr Steve Brinksman - GPw. SI in Substance Misuse Lead, Birmingham Mrs Diane Goslar – Service User, Expert Patient - Alcohol Dr Carsten Grimm – GPw. SI in Substance Misuse, Kirklees, Yorkshire Mr Alan Knobel - Alcohol Strategy Co-ordinator Safer Portsmouth Partnership Dr Joe Mc. Gilligan – GP Commissioning Lead, Redhill, Surrey • Dr Jane Marshall – Consultant • • • Psychiatrist in the Addictions, South London and the Maudsley NHS Foundation Trust Dr Lynn Owens – Nurse Consultant , Alcohol Services, Liverpool Mr Martyn Penfold – Drug and Alcohol Commissioner Mrs Dawn Price – Chief Pharmacist, Addaction and Director Mistura Enterprise/Informatics Ltd Ms Tracy Savage – Medicine Management, Shropshire CCG Prof Paul Wallace – National Institute of Health Research, London Dr Richard Watson – GPw. SI in Substance Misuse, Glasgow
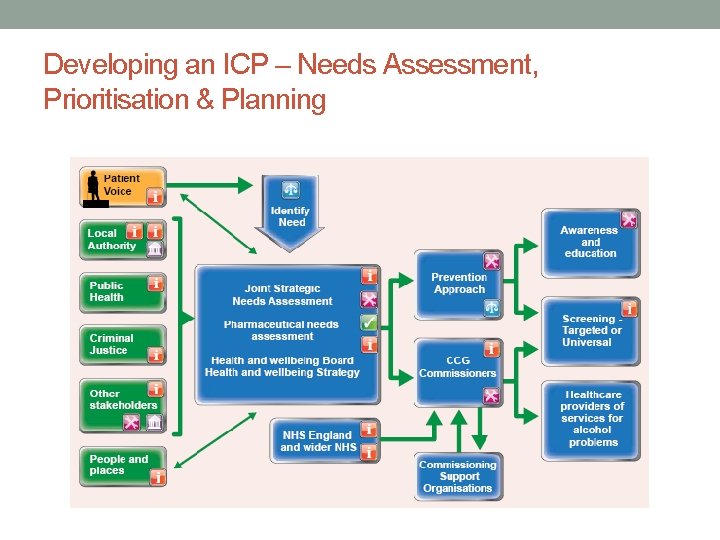
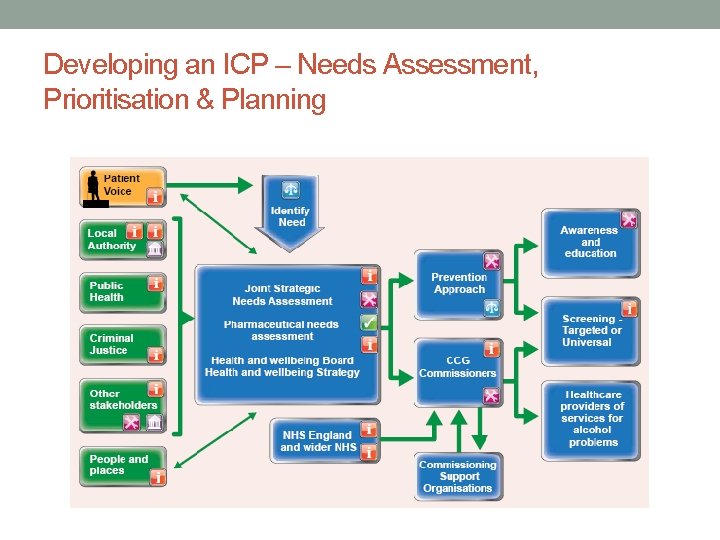
Developing an ICP – Needs Assessment, Prioritisation & Planning
WHAT ARE THE CHALLENGES OF DELIVERING AN INTEGRATED CARE PATHWAY FOR ALCOHOL USE DISORDERS?
What are the challenges of delivering a effective response in the context of austerity § Meeting a level of demand that has consistently outstripped our ability to respond, and which continues to rise, within the context of a public sector austerity program. § Delivering within the context of new NHS commissioning frameworks. § Promoting the value of alcohol harm reduction interventions to key provider partners. § Redefining the concept of ‘treatment’ beyond the tight confines of abstinence based interventions to reflect more client focused outcomes. § Developing more client-centred response to more complex ‘hard to engage’ drinkers.
How can we overcome some of these challenges? § Develop more Integrated Care Pathways for alcohol use disorders § Broaden the partnership for delivery, starting with those areas where alcohol is a common presenting issue e. g. primary and secondary care, mental health services: Making every contact count § Increase capacity in the system through novel channels e. g. Community pharmacy or online IBA: Any qualified provider § Engage suppliers such as Industry - potential partnership working opportunities to secure investment and develop services in a tough financial climate: Any willing and appropriate partner § Review our approach to the treatment of alcohol use disorders to better client choice and the growing range of options available:
ENHANCING TREATMENT CAPACITY FOR ALCOHOL USE DISORDERS IN PRIMARY CARE A case study
What patients and GP’s told us § A significant amount of primary treatment (detox) episodes taking place in general practice. § A high rate of relapse (>3 months) due to lack of access to psychosocial support and relapse prescribing. § Many GP’s reluctantly treat ‘AUD’s due to long waits for community alcohol team and resistance by some clients to be referred on. § Many moderately alcohol dependent clients waited 12 weeks+ only to be told they were not a priority. § Patients and GP’s wanted quicker access to a more comprehensive treatment response and a greater choice of treatment setting.
Fresh Start: A GP led alcohol clinic
Developing the primary care response to Alcohol Use Disorders Fresh Start: §GP led clinic for mild – moderately alcohol dependent adults §Supported by a full time equivalent nurse prescriber §Self, GP or agency referral §Offering planned withdrawal within pre-agreed treatment plan §Daily attendance, breathalysing, dispensing §Access to onsite counselling and group support (controlled drinking or abstinence) including evening sessions §Relapse prescribing offered §Follow up at three months
Fresh Start Outcomes/benefits § A 40% reduction in waiting times for the community alcohol team § Increased client and GP choice § An additional 150 -200 treatment places p. a. § Streamlined referral and fast access (7 days) § 98% treatment completion rate § Positive re-engagement rates on relapse § 58% sustained treatment gains at 3 and 6 months § Measured improvements in both liver and mental health Further developments: § 3 clinics; in each borough locality § Each clinic expanded to include 2 x weekly IBA clinics § Locality based family/carer support groups planned (2013) § Reviewing primary care referral to inpatient unit
On a broader level: • DOH guideline is that 15 -20% of in need dependent drinkers should be accessing treatment each year. • There is significant ‘treatment in a range of Tier 1 settings: • Primary care: (estimated ) 300 -400 episodes • Secondary care (estimated) 500 • Mental health: unmeasured although up to 40% of Sec 136 admissions involve alcohol • Pathways between T 1 services and community alcohol services were undefined and often ineffective • In most cases the and lack of outcomes were poor or undefined and lacked a care planned approach. • Integrated care pathways need to start at the point where the need presents and treatment starts!
In summary: • Alcohol related harm presents a significant challenge to public health and services • Without a more comprehensive and sustained response the alcohol related burden will continue to rise on an annual basis • An integrated treatment response is the best starting point in terms of optimising the impact of existing commissioned capacity • A sustainable response to alcohol related harm requires the engagement of a wider stakeholder audience • We need to be more creative in our response in those who cannot or will not engage in structured abstinence based interventions
THANK YOU FOR LISTENING