Integrated Care Model Case Management Member centric One
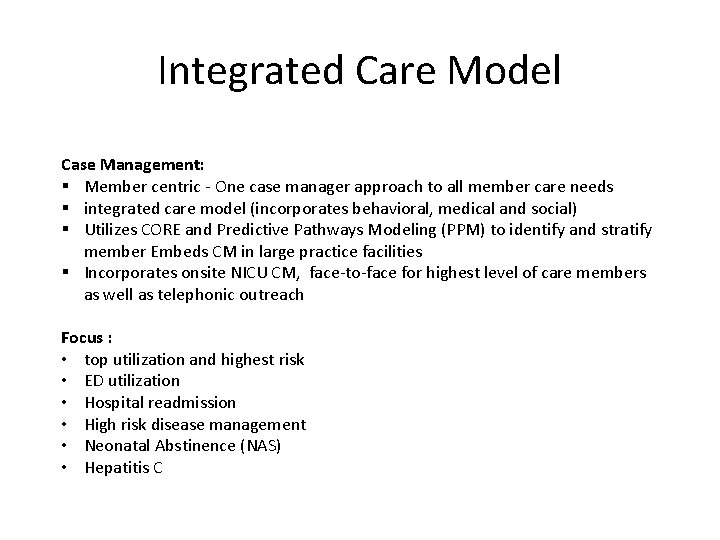
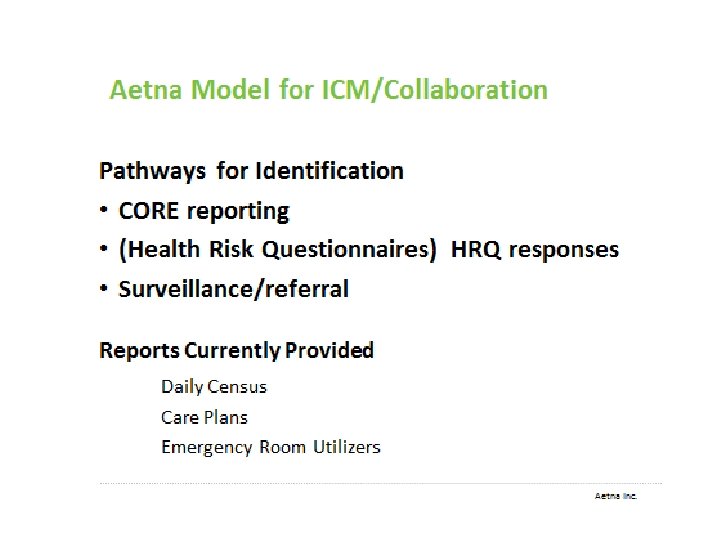
Integrated Care Model Case Management: § Member centric - One case manager approach to all member care needs § integrated care model (incorporates behavioral, medical and social) § Utilizes CORE and Predictive Pathways Modeling (PPM) to identify and stratify member Embeds CM in large practice facilities § Incorporates onsite NICU CM, face-to-face for highest level of care members as well as telephonic outreach Focus : • top utilization and highest risk • ED utilization • Hospital readmission • High risk disease management • Neonatal Abstinence (NAS) • Hepatitis C
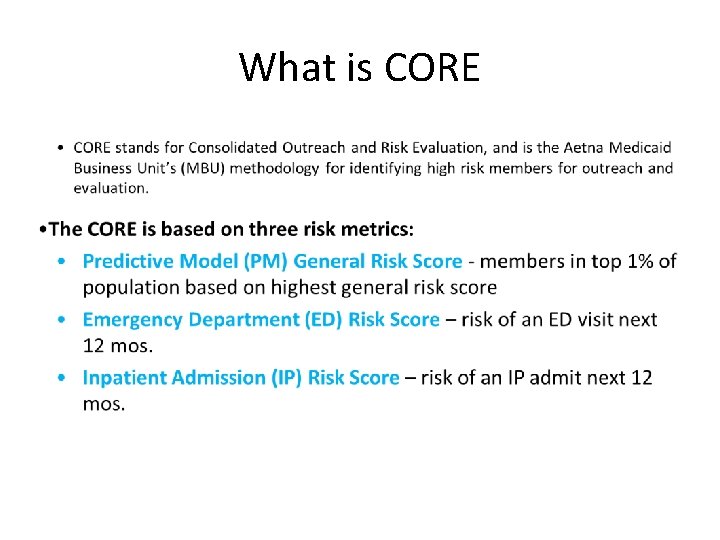
What is CORE
Care Management Shannon Jones RN, CCM Sr. Director Field Service Coordination, Kentucky Market Well. Care Health Plans Confidential and Property of Well. Care Health plans (Not for Distribution) 6
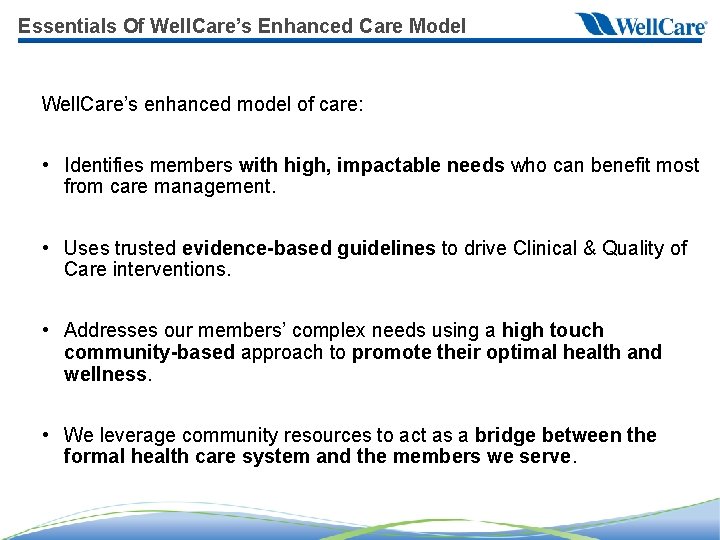
Essentials Of Well. Care’s Enhanced Care Model Well. Care’s enhanced model of care: • Identifies members with high, impactable needs who can benefit most from care management. • Uses trusted evidence-based guidelines to drive Clinical & Quality of Care interventions. • Addresses our members’ complex needs using a high touch community-based approach to promote their optimal health and wellness. • We leverage community resources to act as a bridge between the formal health care system and the members we serve.
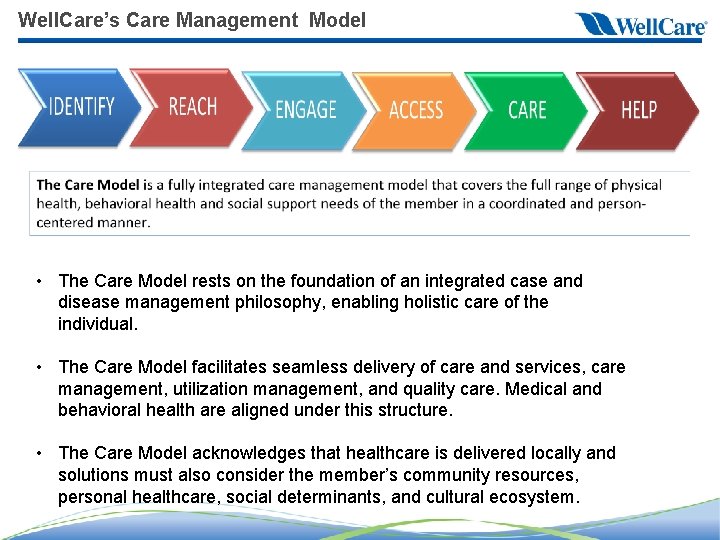
Well. Care’s Care Management Model • The Care Model rests on the foundation of an integrated case and disease management philosophy, enabling holistic care of the individual. • The Care Model facilitates seamless delivery of care and services, care management, utilization management, and quality care. Medical and behavioral health are aligned under this structure. • The Care Model acknowledges that healthcare is delivered locally and solutions must also consider the member’s community resources, personal healthcare, social determinants, and cultural ecosystem.
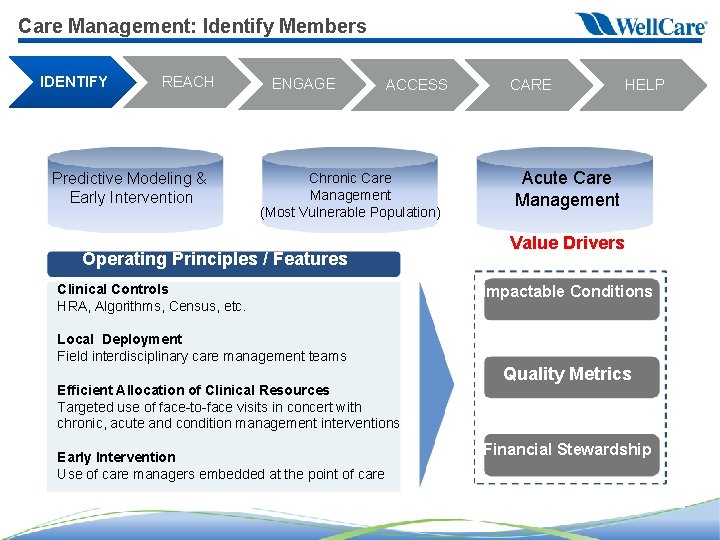
Care Management: Identify Members IDENTIFY REACH Predictive Modeling & Early Intervention ENGAGE ACCESS Chronic Care Management (Most Vulnerable Population) Operating Principles / Features Clinical Controls HRA, Algorithms, Census, etc. Local Deployment Field interdisciplinary care management teams Efficient Allocation of Clinical Resources Targeted use of face-to-face visits in concert with chronic, acute and condition management interventions Early Intervention Use of care managers embedded at the point of care CARE HELP Acute Care Management Value Drivers Impactable Conditions Quality Metrics Financial Stewardship

Engaging our Members IDENTIFY REACH ENGAGE ACCESS CARE HELP Ø Focused geographic staff assignments to synergize market expertise (CM/BH/SW/UM). Ø Discharge planning nurses provide transitional interventions and monitor length of stay at facilities with a high daily census. Ø Innovative outreach and education strategies. Ø Incentive programs for rewarding engagement in health and wellness activities.
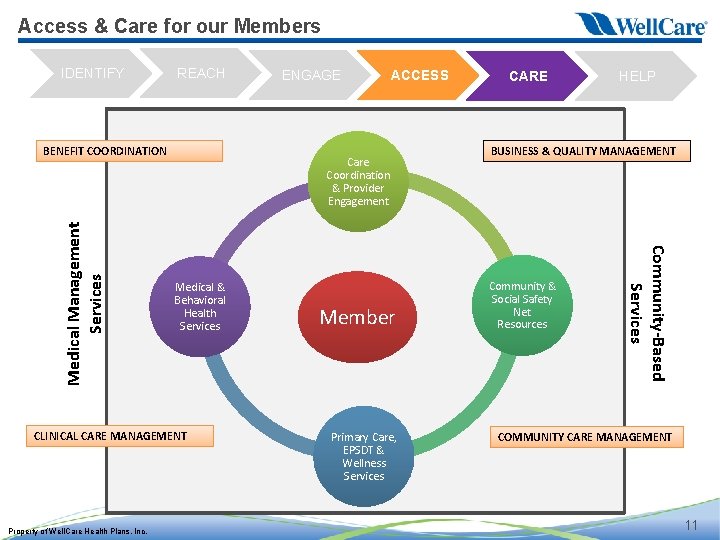
Access & Care for our Members IDENTIFY REACH Care Coordination & Provider Engagement Medical & Behavioral Health Services CLINICAL CARE MANAGEMENT Property of Well. Care Health Plans, Inc. ACCESS Member Primary Care, EPSDT & Wellness Services CARE HELP BUSINESS & QUALITY MANAGEMENT Community & Social Safety Net Resources Community-Based Services Medical Management Services BENEFIT COORDINATION ENGAGE COMMUNITY CARE MANAGEMENT 11
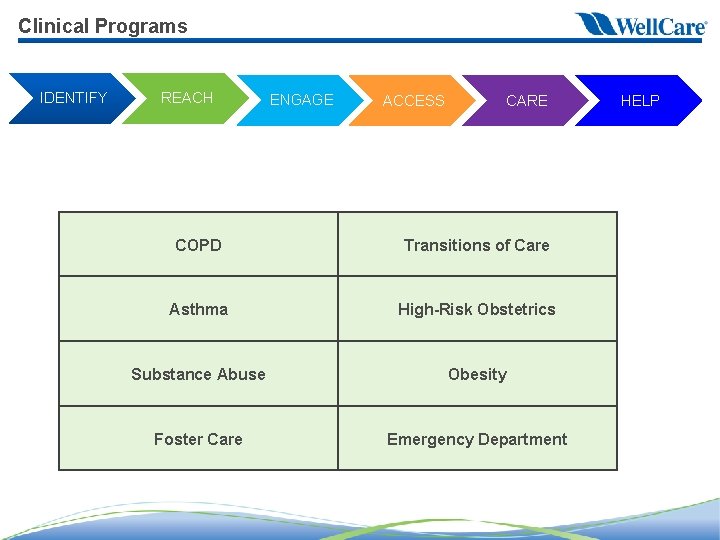
Clinical Programs IDENTIFY REACH ENGAGE ACCESS CARE COPD Transitions of Care Asthma High-Risk Obstetrics Substance Abuse Obesity Foster Care Emergency Department HELP
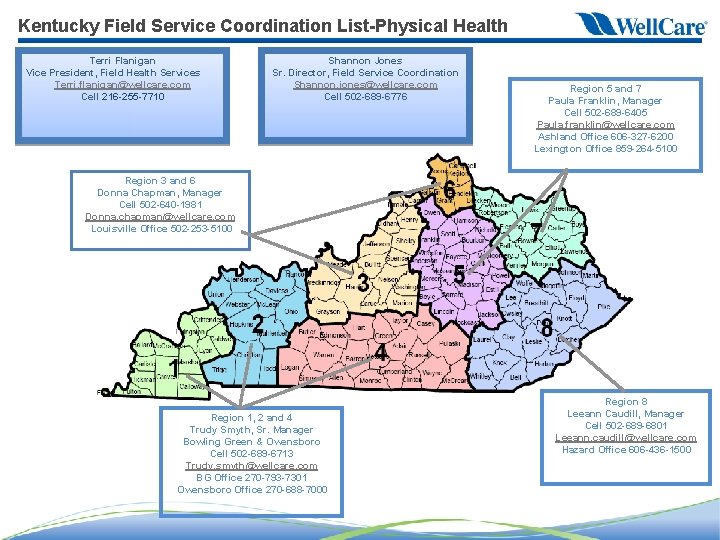
Kentucky Field Service Coordination List-Physical Health Terri Flanigan Vice President, Field Health Services Terri. flanigan@wellcare. com Cell 216 -255 -7710 Shannon Jones Sr. Director, Field Service Coordination Shannon. jones@wellcare. com Cell 502 -689 -6776 Region 5 and 7 Paula Franklin, Manager Cell 502 -689 -6405 Paula. franklin@wellcare. com Ashland Office 606 -327 -6200 Lexington Office 859 -264 -5100 Region 3 and 6 Donna Chapman, Manager Cell 502 -640 -1981 Donna. chapman@wellcare. com Louisville Office 502 -253 -5100 Region 1, 2 and 4 Trudy Smyth, Sr. Manager Bowling Green & Owensboro Cell 502 -689 -6713 Trudy. smyth@wellcare. com BG Office 270 -793 -7301 Owensboro Office 270 -688 -7000 Region 8 Leeann Caudill, Manager Cell 502 -689 -6801 Leeann. caudill@wellcare. com Hazard Office 606 -436 -1500
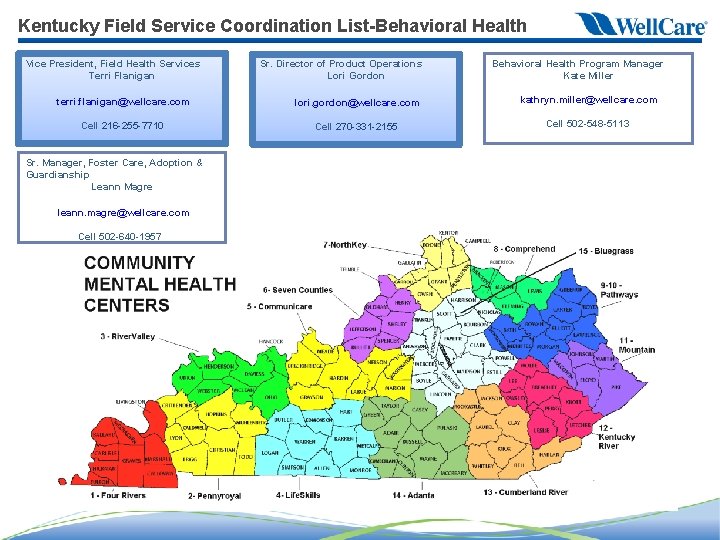
Kentucky Field Service Coordination List-Behavioral Health Vice President, Field Health Services Terri Flanigan terri. flanigan@wellcare. com Cell 216 -255 -7710 Sr. Manager, Foster Care, Adoption & Guardianship Leann Magre leann. magre@wellcare. com Cell 502 -640 -1957 Sr. Director of Product Operations Lori Gordon lori. gordon@wellcare. com Cell 270 -331 -2155 Behavioral Health Program Manager Kate Miller kathryn. miller@wellcare. com Cell 502 -548 -5113

Care Coordination Your Connection to Disease and Case Management Programs Robert Beaty, RCP, RRT-ACCS, AEC, BA Team Lead, Care Coordination
What is Care Coordination?
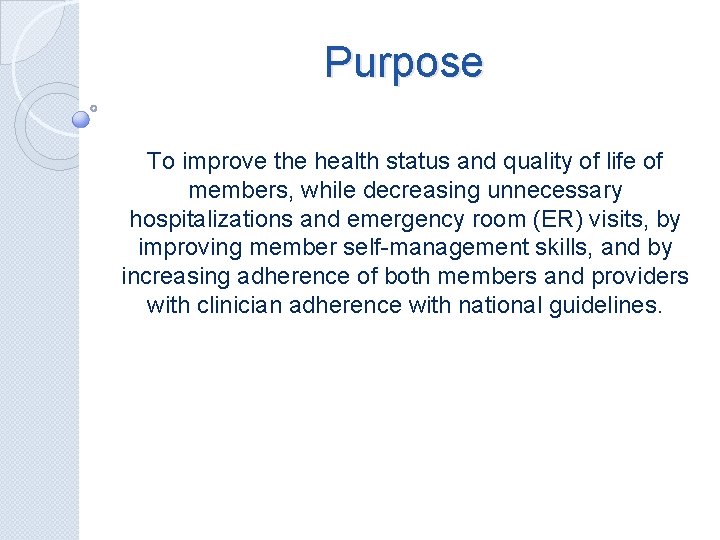
Purpose To improve the health status and quality of life of members, while decreasing unnecessary hospitalizations and emergency room (ER) visits, by improving member self-management skills, and by increasing adherence of both members and providers with clinician adherence with national guidelines.
Onsite Programs • • • ER Navigator Tiny Tots Discharge Education Team Stork Care Embedded Case Management
Programs at Passport • • • Disease Management Complex Case Management Behavioral Health Case Management Foster Care/Adoption Guardianship Liaison Mommy Steps Specialty Programs
Process �Case Manager Technician �Rapid Response Case Manager/Embedded Case Manager* �Appropriate Program �*Pregnant, Medically Fragile, etc.
Value � 2015 when compared to 2014 � 297% increase in Health Risk Assessments � 13, 003 24/7 RN hotline calls ◦ 37% increase ◦ 88% referred to Lower Level of Care ◦ 95% in agreement
How to refer to Care Coordination http: //passporthealthplan. com/wpcontent/uploads/2015/01/2 -cc-care-coordinationrequest-form. pdf • Rapid Response 1 -877 -903 -0082 • Fax 502 -585 -7997 •
- Slides: 22