INTEGRATED CARE MANAGEMENT AND QUALITY IMPROVEMENT Service Authorization

- Slides: 38
INTEGRATED CARE MANAGEMENT AND QUALITY IMPROVEMENT Service Authorization Process for EPSDT Personal/Attendant Care (Service Types 0090, 0098, 0091) Presented by: Ke. PRO 1
Methods of Submission Service Authorization Requests to Ke. PRO • • • Ke. PRO accepts service authorization (srv auth) requests through direct data entry (DDE), fax and phone. Submitting through DDE puts the request in the worker queue immediately; faxes are entered by the administrative staff in the order received. For direct data entry requests, providers must use Atrezzo Connect Provider Portal. For DDE submissions, service authorization checklists may be accessed on Ke. PRO’s website to assist the provider in assuring specific information is included with each request. To access Atrezzo Connect on Ke. PRO’s website, go to http: //dmas. kepro. com. 2 2
Methods of Submission Service Authorization Requests to Ke. PRO • • Please note that for Alzheimer's Assisted Living Waiver, all requests must be submitted via Ke. PRO’s Atrezzo Connect System To access Atrezzo Connect on Ke. PRO’s website, go to http: //dmas. kepro. com. • Provider registration is required to use Atrezzo Connect. • The registration process for providers happens immediately on-line • From http: //dmas. kepro. com, providers not already registered with Atrezzo Connect may click on “Register” to be prompted through the registration process. Newly registering providers will need their 10 digit National Provider Identification (NPI) number and their most recent remittance advice date for YTD 1099 amount. • The Atrezzo Connect User Guide is available at http: //dmas. kepro. com : Click on the Training tab, then the General tab. 3
Service Authorization Requests: Contact Information for Ke. PRO/ DMAS Provider Information • Providers with questions about Ke. PRO’s Atrezzo Connect Provider Portal may contact Ke. PRO by email at atrezzoissues@kepro. com. • For service authorization questions, providers may contact Ke. PRO at providerissues@kepro. com. • Ke. PRO may also be reached by phone at 1 -888 -827 -2884, or via fax at 1877 -OKBYFAX or 1 -877 -652 -9329. 4
Provider Manual/Medicaid Memorandums • DMAS publishes electronic and printable copies of its Provider Manuals and Medicaid Memoranda on the DMAS Web Portal at https: //www. virginiamedicaid. dmas. virginia. gov/wps/portal. • This link opens up a page that contains all of the various communications to providers, including Provider Manuals and Medicaid Memoranda. • The Internet is the most efficient means to receive and review current provider information. • If you do not have access to the Internet or would like a paper copy of a manual, you can order it by contacting: – Commonwealth-Martin at 1 -804 -780 -0076. A fee will be charged for the printing and mailing of the manual updates that are requested. 5
Service Authorization Information Specific to Personal Care/Attendant Care, Private Duty Nursing (PDN) Covered Services under EPSDT: • EPSDT Personal/Attendant Care-0091 • EPSDT Private Duty Nursing-0090 • EPSDT Private Duty Nursing in School (MCO)-0098 6
Service Authorization Information Specific to Personal Care/Attendant Care, PDN • Initial Requests for Services and Enrollment üInitial request for Services (EPSDT) • Change Requests üNeed to Submit Case ID or Srv Auth # and the procedure code that is in need of a chance, as well as the required justification to support. üChange requests are inclusive of requests to increase or decrease units previous authorized, or to change dates of service currently authorized. 7
Service Authorization Information Specific to Personal Care/Attendant Care, PDN • Discharges üNeed to Submit Case ID or Srv Auth # and the procedure code for each service being discharged, as well as the reason for the discharge. üYou must complete a new DMAS 98, submitting the DMAS 225 is not sufficient. 8
Service Authorization Information Specific to Personal Care/Attendant Care, PDN • Completion of DMAS 98 üPage 1: Name, Age, Gender, Name of Service Provider, Service Provider ID (Must be 10 Digits), Diagnosis, Clinical or additional information in Blocks 15 & 16, Name of referring Provider (when applicable) and Referring Provider ID. ü Page 2: List type of service requested by use of the procedure code (with modifier if applicable), Hours/ units, frequency, cost (when applicable), SOC date, and End date. 9
Service Authorization Information Specific to Personal Care/Attendant Care • EPSDT Personal Care/Attendant Care 10
Service Authorization Information Specific to Personal Care/Attendant Care • Providers must submit request to the designated preauthorization contractor within 10 business days of initiating care or within 10 business days of receiving verification of Medicaid eligibility from the local DSS, unless otherwise specified in the DMAS Provider Manual. • Please note that some services can not be retro authorized and must be submitted by the SOC date requested. Refer to the specific Provider Waiver Manual for the submission requirements for each service/procedure code. 11
Service Authorization Information Specific to Personal Care/Attendant Care • EPSDT Personal/Attendant Care: 0091 – EPSDT services are available to Medicaid members under 21 years of age. Personal care may be provided exclusively through EPSDT to eligible persons who have demonstrated a medical need for personal care that is not covered under an existing Medicaid program for which the individual is enrolled. 12
Service Authorization Information Specific to Personal Care/Attendant Care • Procedure/Service Codes that Require Service Authorization: ü T 1019 (Agency Directed Personal Care) ü S 5126 (Consumer Directed Personal Care) 13
Service Authorization Information Specific to Personal Care/Attendant Care • Eligible Members include individuals who are: ü Under 21 y. o. and enrolled in Medicaid FFS, Medicaid MCO, or FAMIS Plus on dates of services requested ü Under the age of 19 y. o. and enrolled in FAMIS FFS on the dates of service requested ü Personal Care is not a covered services by FAMIS MCOs 14
Service Authorization Information Specific to Personal Care/Attendant Care Timeliness Requirements for Submission: • Providers must submit documentation to Ke. PRO within 10 business days prior to initiation of care • If request is not submitted within the required timeframe, the service must be authorized beginning with the date the information was received by Ke. PRO. 15
Service Authorization Information Specific to EPSDT Personal Care/Attendant Care • Required documentation when requesting authorization: ü DMAS 98 fax form ü DMAS 7 (signed and dated by physician, physician’s assistant, or nurse practitioner) ü DMAS 7 -A from provider ü DMAS 99 Community Based Care Recipient Assessment Report ü Back-up plan documented ü Detailed Schedule of current services available to individual • NOTE****If provider is submitting in request via Atrezzo portal, the EPSDT Personal/Attendant Care Questionnaire needs to be completed, or the provider can upload all appropriate documents in lieu of the questionnaire • NOTE***If additional information is needed from the provider, the case is pended for 5 business days to allow provider time to submit additional documentation to Ke. PRO for review. 16
Service Authorization Information Specific to Personal Care/Attendant Care • In addition to medical necessity, the following criteria must be met in order for personal care services to be determined as appropriate: ü The member must have a plan of care developed by a currently enrolled personal care provider or service facilitator ü The plan of care (DMAS- 7 A) should be consistent with the findings on the EPSDT functional assessment (DMAS -7) and demonstrate the need for personal care. ü The member must have a viable back-up plan, such as a family member, neighbour, or friend who is willing and able to assist the individual on very short notice in case the personal care aide does report for work as expected. ü Individuals who do not have a viable back-up plan are not eligible for services until a backup plan as has been established. ü Individuals receiving EPSDT personal care must have a physician referral due to health conditions documented during an EPSDT medical exam 17
Service Authorization Information Specific to EPSDT Personal Care/Attendant Care • Medical Necessity üHealth conditions must cause the individual to be functionally limited in performing three or more activities of daily living (ADL) ØThese categories are bathing, dressing, transfers, ambulation, eating/feeding, toileting, and continence ØThe individual’s inability to perform an ADL cannot be exclusively due to typical limitations associated with typical attainment of developmental milestones 18
Service Authorization Information Specific to EPSDT Personal Care/Attendant Care • EPSDT Personal Care Services may be provided in a school setting if the service is not included in the member’s Individualized Education Program (IEP) and the services are deemed medically necessary • Providers must document the medical need for coverage in the school setting and document that the services is not included in the member’s IEP • EPSDT allows supervision hours when it is medically necessary for the member to receive supervision due to a health condition. • Disruptive behaviours such as aggression, self-injury, elopement/wandering, impulsivity, property destruction, etc. may require constant supervision from a personal or attendant care aide to maintain the child’s safety in addition to the hours required for ADL/IADL supports. 19
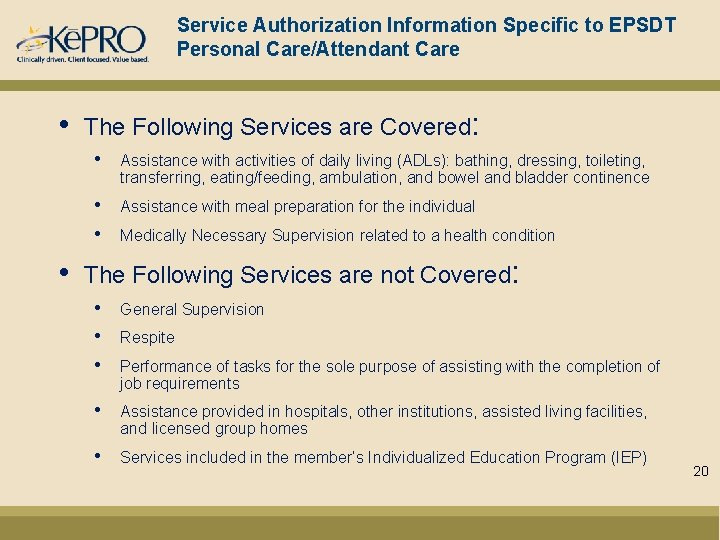
Service Authorization Information Specific to EPSDT Personal Care/Attendant Care • • The Following Services are Covered: • Assistance with activities of daily living (ADLs): bathing, dressing, toileting, transferring, eating/feeding, ambulation, and bowel and bladder continence • • Assistance with meal preparation for the individual Medically Necessary Supervision related to a health condition The Following Services are not Covered: • • • General Supervision • Assistance provided in hospitals, other institutions, assisted living facilities, and licensed group homes • Services included in the member’s Individualized Education Program (IEP) Respite Performance of tasks for the sole purpose of assisting with the completion of job requirements 20
Service Authorization Information Specific to EPSDT Private Duty Nursing (PDN) 21
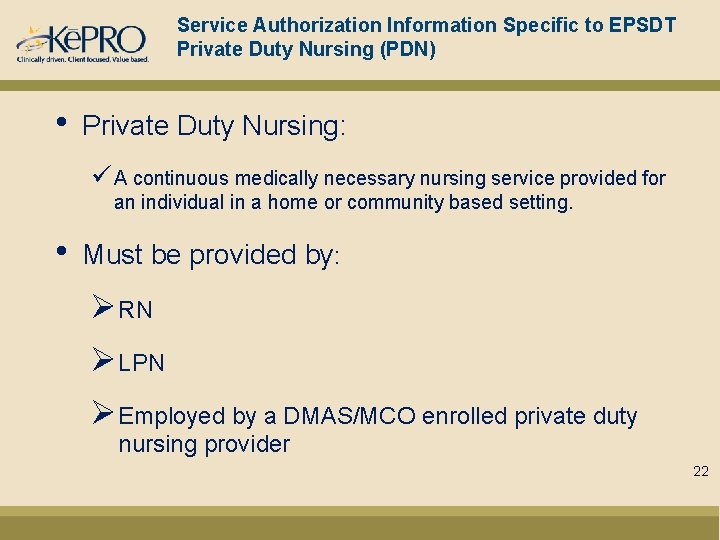
Service Authorization Information Specific to EPSDT Private Duty Nursing (PDN) • Private Duty Nursing: ü A continuous medically necessary nursing service provided for an individual in a home or community based setting. • Must be provided by: ØRN ØLPN ØEmployed by a DMAS/MCO enrolled private duty nursing provider 22
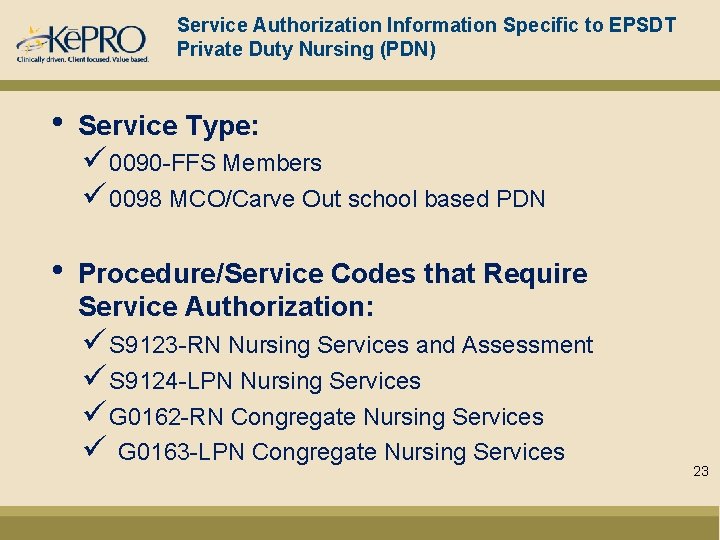
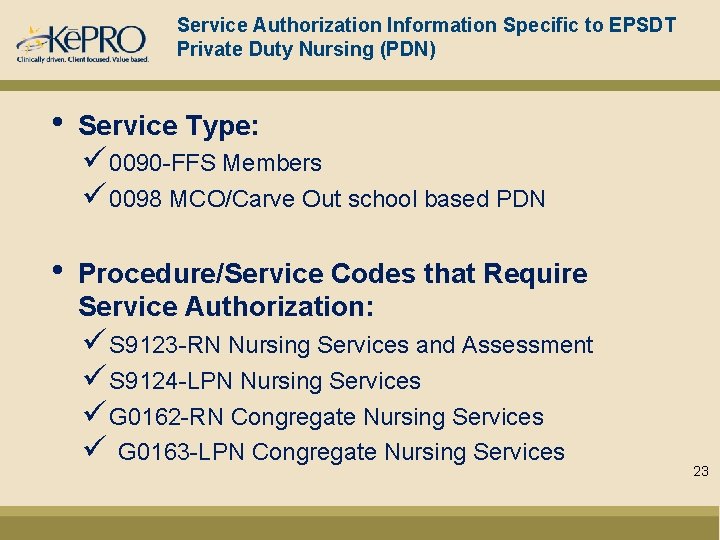
Service Authorization Information Specific to EPSDT Private Duty Nursing (PDN) • Service Type: • Procedure/Service Codes that Require Service Authorization: ü 0090 -FFS Members ü 0098 MCO/Carve Out school based PDN ü S 9123 -RN Nursing Services and Assessment ü S 9124 -LPN Nursing Services ü G 0162 -RN Congregate Nursing Services ü G 0163 -LPN Congregate Nursing Services 23
Service Authorization Information Specific to Private Duty Nursing (PDN) • Eligible Members for 0090 include individuals who are: • Under 21 y. o. and enrolled in Medicaid FFS, FAMIS, or FAMIS Plus on dates of services requested • Under the age of 19 y. o. and enrolled in FAMIS FFS on the dates of service requested • Personal Care is not a covered services by FAMIS MCOs 24
Service Authorization Information Specific to Private Duty Nursing (PDN) Timeliness Requirements for Submission: • Providers must submit documentation to the service authorization contractor prior to initiation of care • If request is not submitted prior to the start of care, the service must be authorized beginning with the date the information was received by the service authorization contractor • Continuation of service reviews are required to be submitted prior to the end of the current authorization period NOTE**If additional information is needed from the provider, the case is pended for 5 business days to allow the provider time to submit additional documentation for review 25
Service Authorization Information Specific to Private Duty Nursing (PDN) • • Private Duty Nursing ü May be used while a child is enrolled in a waiver, if that waiver does not provider PDN or does not provide congregate PDN ü PDN services are limited to the hours of skilled medical care and skilled supervision as specified in the Plan of Care (POC) and limited to the number of hours approved. Congregate Private Duty Nursing ü Provided with more than 1 individual who requires private duty nursing resides in the same home Ø Limited to a maximum ration of one PDN to two individuals who receive nursing via the Etch Waiver or EPSDT Ø When 3 or more Waiver/EPSDT individuals share a home, service staff ratios are determined by assessing the combined needs of the individuals 26
Service Authorization Information Specific to EPSDT Private Duty Nursing (PDN) • Required Documents for New Requests (0090): üDMAS 98 ü Signed DMAS 62 -signed by Physician ü Home Health Certification and Plan of Care (may use DMAS 485 or equivalent to meet documentation requirements) 27

Service Authorization Information Specific to EPSDT Private Duty Nursing (PDN) • Required Documents for New Requests (0090): üDDE - Questionnaire üSigned DMAS 62 -signed by Physician üHome Health Certification and Plan of Care (may use DMAS 485 or equivalent to meet documentation requirements) 28
Service Authorization Information Specific to EPSDT Private Duty Nursing (PDN) • Required Documents for MCO Referral Requests: üSigned DMAS 62 -signed by Physician (a new DMAS 62 is required every 6 months) üHome Health Certification and Plan of Care (may use DMAS 485 or equivalent to meet documentation requirements) ü School Based MCO Referral (questions found on the DMAS 98 or the questionnaire) 29
Service Authorization Information Specific to EPSDT Private Duty Nursing (PDN) • Atrezzo Portal Submissions: üIf Provider is submitting Request via Atrezzo Portal, provider needs to complete EPSDT Specialized Services Questionnaire, upload DMAS 62, and submit any additional clinical 30
Service Authorization Information Specific to Private Duty Nursing (PDN) • Dual Use of EPSDT PDN: ü If a child is enrolled in a Medicaid Waiver Program, the provider must document that the waiver does not offer PDN coverage or doe not offer congregate Private Duty Nursing coverage ü If the member’s waiver offers PDN, then the EPSDT benefit is not available. ü Members may be authorized for EPSDT PDN if enrolled in the EDCD Waiver ü Members may use any of the EDCD waiver services while receiving EPSDT PDN. EPSDT is not use to authorize respite care ü Services may be approved for school based nursing supports. The hours used during the school day will count toward the number of hours allowed based on the individual’s medical need for care 31
General Information for All Service Authorization Submissions • • • Ke. PRO’s website has information related to the service authorization processes for all DMAS programs they review. Questionnaires and much more are on Ke. PRO’s website. Providers may access this information by going to http: //dmas. kepro. com. Ke. PRO will approve, deny, or pend requests. If there is insufficient medical necessity information to make a final determination, Ke. PRO will pend the request back to the provider requesting additional information. Once the case has been received and reviewed, if additional information is needed from the provider, the case is pended for 5 business days to allow the provider time to submit additional documentation to Ke. PRO for review Do not send responses to pends piecemeal since the information will be reviewed and processed upon initial receipt. If the information is not received within the time frame requested by Ke. PRO, the request will automatically be sent to a physician for a final determination. In the absence of clinical information, the request will be submitted to the supervisor for an administrative review and final determination. Providers and members are issued appeal rights through the MMIS letter generation process for any adverse determination. Instruction on how to file an appeal is included in the MMIS generated letter. 32
General Information for All Service Authorization Submissions • • There are no automatic renewals of service authorizations. Providers must submit requests for continuation of care needs, with supporting documentation, prior to the expiration of the current authorization. Providers must verify member eligibility prior to submitting the request. Authorizations will not be granted for periods of member or provider ineligibility. Requests will be rejected if required demographic information is absent. Providers should take advantage of Ke. PRO’s web based checklists/information sheets for the services(s) being requested. These sheets provide helpful information to enable providers to submit information relevant to the services being requested. Providers must submit a service authorization request under the appropriate service type. Service authorization requests cannot be bundled under one service type if the service types are different. 33
Out of State Providers • Out of State Providers: – Out of state providers must be enrolled with Virginia Medicaid in order to submit a request for out of state services to the Contractor. If the provider is not enrolled as a participating provider with Virginia Medicaid, the provider is still encouraged to submit the request to the Contractor, as timeliness of the request will be considered in the review process starting November 1, 2012. These providers will not have a NPI number but may submit a request to the Contractor. • • The Contractor will advise out of state providers that they may enroll with Virginia Medicaid by going to: https: //www. virginiamedicaid. dmas. virginia. gov/wps/myportal/Provider. Enrol lment. (At the toolbar at the top of the page, click on Provider Services and then Provider Enrollment in the drop down box. It may take up to 10 business days to become a Virginia participating provider. ) 34
VIRGINIA MEDICAID WEB PORTAL • • • DMAS offers a web-based Internet option to access information regarding Medicaid or FAMIS member eligibility, claims status, check status, service limits, service authorizations, and electronic copies of remittance advices. Providers must register through the Virginia Medicaid Web Portal in order to access this information. The Virginia Medicaid Web Portal can be accessed by going to: www. virginiamedicaid. dmas. virginia. gov. If you have any questions regarding the Virginia Medicaid Web Portal, please contact the Xerox State Healthcare Web Portal Support Helpdesk, toll free, at 1 -866 -352 -0496 from 8: 00 a. m. to 5: 00 p. m. Monday through Friday, except holidays. The Medi. Call audio response system provides similar information and can be accessed by calling 1 -800 -884 -9730 or 1 -800 -772 -9996. Both options are available at no cost to the provider. Providers may also access service authorization information including status via Ke. PRO’s Provider Portal at http: //dmas. kepro. com. 35
ELIGIBILITY VENDORS: How to check for Member Eligibility • • • DMAS has contracts with the following eligibility verification vendors offering internet real-time, batch and/or integrated platforms. Eligibility details such as eligibility status, third party liability, and service limits for many service types and procedures are available. Contact information for each of the vendors is listed below: – Passport Health Communications, Inc. • www. passporthealth. com, sales@passporthealth. com • Telephone: 1 (888) 661 -5657 – SIEMENS Medical Solutions – Health Services • Foundation Enterprise Systems/HDX • www. hdx. com • Telephone: 1 (610) 219 -2322 – Emdeon • www. emdeon. com • Telephone: 1 (877) 363 -3666 36
DMAS Helpline Information • The “HELPLINE” is available to answer questions Monday through Friday from 8: 00 a. m. to 5: 00 p. m. , except on holidays. • The “HELPLINE” numbers are: – 1 -804 -786 -6273 – 1 -800 -552 -8627 Richmond area and out-of-state long distance All other areas (in-state, toll-free long distance) • Please remember that the “HELPLINE” is for provider use only. • Please have your Medicaid Provider Identification Number available when you call. 37
INTEGRATED CARE MANAGEMENT AND QUALITY IMPROVEMENT Questions? ? ? 38