Integrated Behavioral Health Model In Primary Care From
Integrated Behavioral Health Model In Primary Care: From Collaborative Care Management for Depression to Implementation Kurt B. Angstman, MS MD; Jay D. Mitchell, MD Department of Family Medicine Kristin J. Somers, MD Department of Psychiatry and Psychology Mayo Clinic Rochester STFM December, 2011 Join the conversation! Our Twitter hashtag is #CPI 2011.
Overview • Primary care practice history • Psychiatry/psychology interactions – Co-location – Collaborative care management – Integrated Behavioral Health • Primary Care perspective • Psychiatry development of new model at Mayo Clinic Rochester
Mayo Clinic Rochester Primary Care • Employee and Community Health(ECH) – 142, 000 patients – 309 physicians, midlevels and residents • Department of Family Medicine • Division of Primary Care Internal Medicine • Division of Community and Adolescent Pediatric Medicine – Four practices • Three multispecialty (FM, P, IM) • One FM
Mayo Clinic Rochester Primary Care • Majority of patients are Olmsted county • 50%+ are employees or dependents of Mayo Clinic – As such, less Medicare, Medicaid and commercial insurance than “typical primary care practice” in Minnesota
Mayo Family Clinics • Mayo Family Clinics Northwest – 1997 – 5 miles from downtown – FM, P, IM – Psychiatry, psychology and social services offered services as visiting consultants • Saw patients referred by PCP • Rechecks and follow ups
Mayo Family Clinics • Mayo Family Clinics Northeast – Opened 2004 – 5 miles from downtown – FM, P, IM – Psychiatry, psychology and social services offered services as consultants • • Saw patients referred by PCP Rechecks and follow ups NEW: Two dedicated exam rooms and office. Increase mental health staff time initially
Co-location 1997 -2008 (NW) 2004 -2008 (NE) – Mental Health staff on site • Easier space for our patients to see the providers – No parking issues – No “new clinics”, stigma of seeing mental health provider • Scheduling problems still- booked out many months – Multiple no-shows – Patient seek other care while waiting- emergency department, etc. • Mental health staff had multiple responsibilities – Hospital service, other outpatient practices, ER – Primary care “tended” to be lower on list of priorities
Care Management 2008 -2011 • Continue co-location of mental health providers • Initiation of collaborative care management for depression (DIAMOND) with ICSI – Two care managers (RNs) onsite (1. 6 -1. 8 FTE) • Care managers are employed by primary care – Oversight by Psychiatrist- 4 hours per week • Review new patient intakes • Review patients concerns, not improving • Management by PCP
Care Management 2008 -2011 • Successful program from many points of view • Spread from 1 clinic in March 2008 to 5 by March 2010 – By September 2011 • 2, 543 patients enrolled • 1, 012 “graduated”
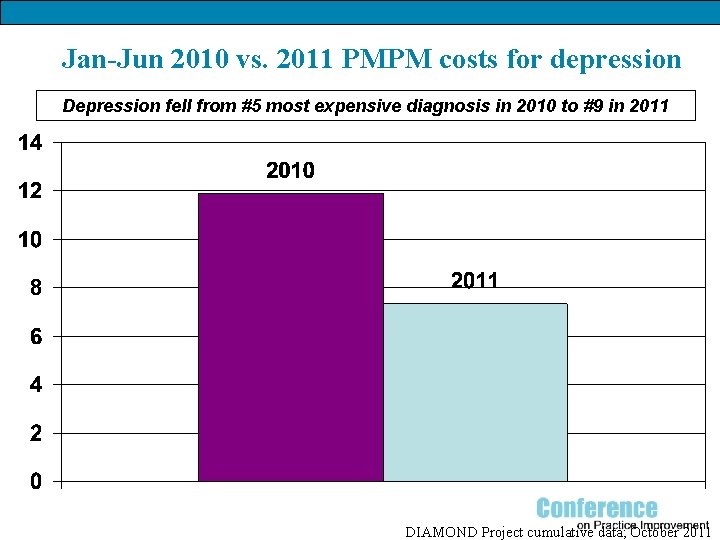
Jan-Jun 2010 vs. 2011 PMPM costs for depression Depression fell from #5 most expensive diagnosis in 2010 to #9 in 2011 DIAMOND Project cumulative data; October 2011
Care Management 2008 -2011 • #1 and #2 clinics in State of Minnesota for six and twelve month response and remission rates for depression – 2009 and 2010 – www. mnhealthscores. org • As we move forward- wish to expand on our success but not hamper our progress…
Before Integrated Behavioral Health… • A maze of options • Referrals “downtown” involved • Confusing ordering options • Delayed or no access • Potentially rescheduled if ordered incorrectly • Unclear if offered long-term follow up • High no show rate • Community referrals could be equally challenging • Fundamental issues were related to • Access (both formal and informal) • Communication/Coordination of care
DIAMOND Introduction • Introduction of DIAMOND improved services dramatically for the subset of patients that qualified • Warm hand off, “local” care at NE • Assistance with triage and consult coordination • On-site psychiatric involvement • Care recommendations on chart • Weekly availability for curbside consultations
Provider/Staff Thoughts on DIAMOND • In a qualitative study, 13 clinic staff (6 MDs, 2 NPs, 2 RNs, 1 PA, 2 CAs) All provider comments regarding DIAMOND were positive. – The Diamond Program, which I thought was a wonderful addition and extremely helpful in our patients that we could manage with depression. And, really that was going really well. – Well, without the Diamond nurses, I just really felt like I was flying by the seat of my pants. – Once Diamond started and it was a depressed person, at least I know that they’d get that ongoing regular support. – How nice it is to just get up and walk down the hall to Diamond and get someone who has the expertise.
IBH: The Awakening • Vision of IBH came from interested and involved providers from the department of psychiatry • IBH workgroup was created with all stakeholders represented • Assessed primary care providers thoughts and needs
Expanding from DIAMOND to IBH • Early in pilot, an IBH psychologist pursued qualitative interviews (coded for themes within and across vignettes, process of contant analysis) • Predominant themes: – Providers value on-site, coordinated care – DIAMOND is appreciated and relied upon, but not available for all patients – On-site mental health services are difficult to access with limited availability – Finding resources for patients is frustrating, confusing and with loose ends
What Providers Thought… • • • Patients were waiting a long time to be seen There wasn’t anyone to collaborate with… you had to page The [clinician] wasn’t… taking new patients People wanted to get in to psychology… couldn’t I was having difficulties getting appointments with psychiatry Having to say that they needed to wait a month was kind of frustrating • It’s a confusing process, it seemed to take a couple steps… the patient leaving without the certainty of an appointment in place
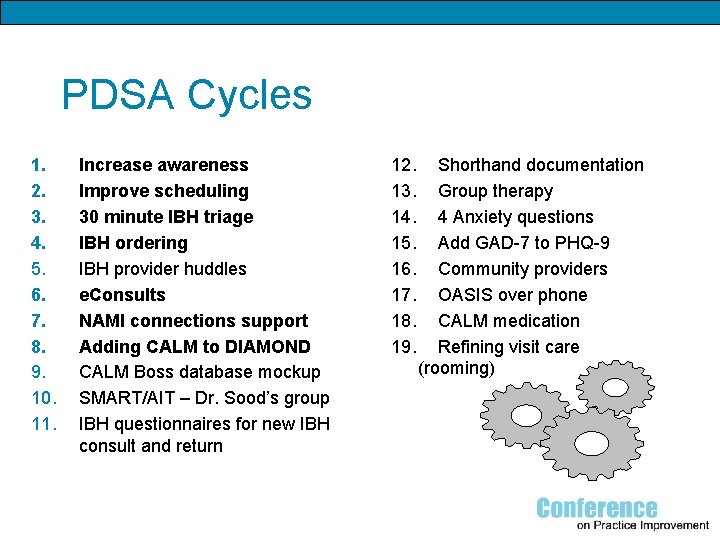
PDSA Cycles 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. Increase awareness Improve scheduling 30 minute IBH triage IBH ordering IBH provider huddles e. Consults NAMI connections support Adding CALM to DIAMOND CALM Boss database mockup SMART/AIT – Dr. Sood’s group IBH questionnaires for new IBH consult and return 12. 13. 14. 15. 16. 17. 18. 19. Shorthand documentation Group therapy 4 Anxiety questions Add GAD-7 to PHQ-9 Community providers OASIS over phone CALM medication Refining visit care (rooming)
PDSA #1 Increase Awareness • Need to introduce IBH providers to NE clinic providers/staff • Introduced at monthly meetings • Went office-to-office to meet providers individually • Postings in common areas with names and schedules • Signage outside office
PDSA #2 Improve Scheduling • Psychiatry/Psychology referrals at complicated and frustrating for providers • New system for ordering – What does the provider want? • • • Diagnosis Management Psychotherapy Social work Specialized psychiatric care – CD treatment
PDSA: #2 Improve Scheduling • Initially consisted of direct review and triage by involved IBH providers • Flowsheet document developed to guide schedulers • Revision of ordering buttons/options within order sets for providers
IBH: The Present Improved access Communication/Relationships Warm hand-offs Triage both within Mayo and the larger community • Improved patient experience • •

Integrated Behavioral Health (IBH) • What is it? – Behavioral health services integrated within PC clinics to serve PC patients • FM, IM, P – New division of Primary Care (ECH) and Psychiatry and Psychology • MD, Ph. D, CNS, LICSW, RN care coordinators
IBH Goals • Increase access at the point of care • Reduce stigma • Support PC providers and allied health staff • Provide more cost effective, evidencebased behavioral health services
IBH Timeline • Phase I: October 2010 -March 2011 – Establish IBH and study current mental health treatment in primary care settings • Phase II: April 2011 -September 2011 – Pilot project to integrate mental health services within a primary care clinic • Phase III- October 2011 -March 2012 – Dissemination of pilot model to other primary care sites
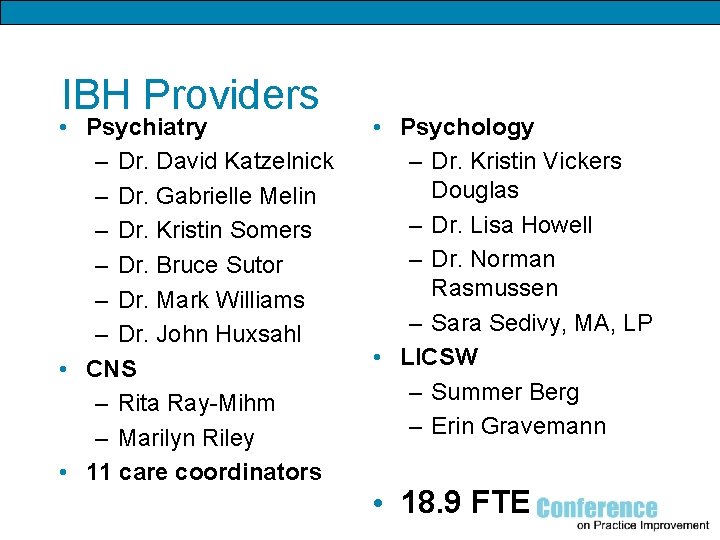
IBH Providers • Psychiatry – Dr. David Katzelnick – Dr. Gabrielle Melin – Dr. Kristin Somers – Dr. Bruce Sutor – Dr. Mark Williams – Dr. John Huxsahl • CNS – Rita Ray-Mihm – Marilyn Riley • 11 care coordinators • Psychology – Dr. Kristin Vickers Douglas – Dr. Lisa Howell – Dr. Norman Rasmussen – Sara Sedivy, MA, LP • LICSW – Summer Berg – Erin Gravemann • 18. 9 FTE
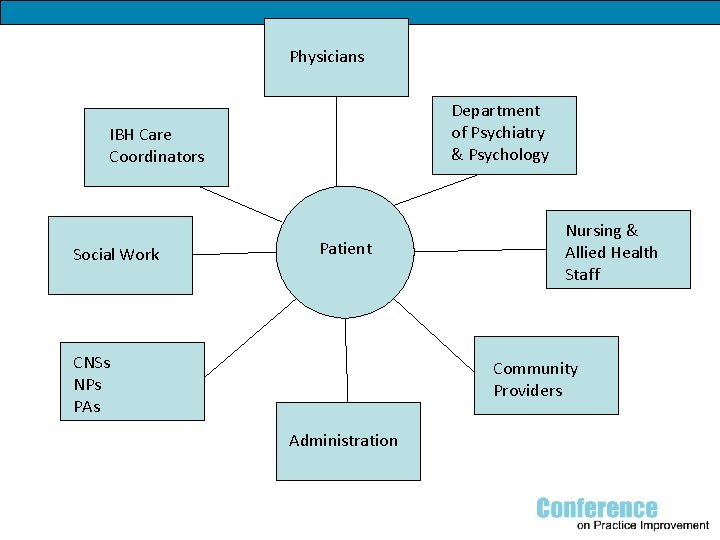
Physicians Department of Psychiatry & Psychology IBH Care Coordinators Social Work Patient CNSs NPs PAs Nursing & Allied Health Staff Community Providers Administration
30 minute LICSW triage • Patients frequently present with behavioral health concerns – PCP: limited time for treatment planning • Opportunity for collaboration with LICSW – Diagnostic clarification – Resources and referral – “Warm handoff” for brief psychotherapy
CALM - Coordinated Anxiety Learning and Management • CBT +/- pharmacotherapy for PC patients – Panic disorder – Social phobia – Generalized anxiety disorder – PTSD • RCT, effectiveness – 1004 patients; 17 PC clinics, 4 US cities • Mayo is beta site Roy-Byrne et al. JAMA. 2010 May 19; 303(19): 1921 -8.
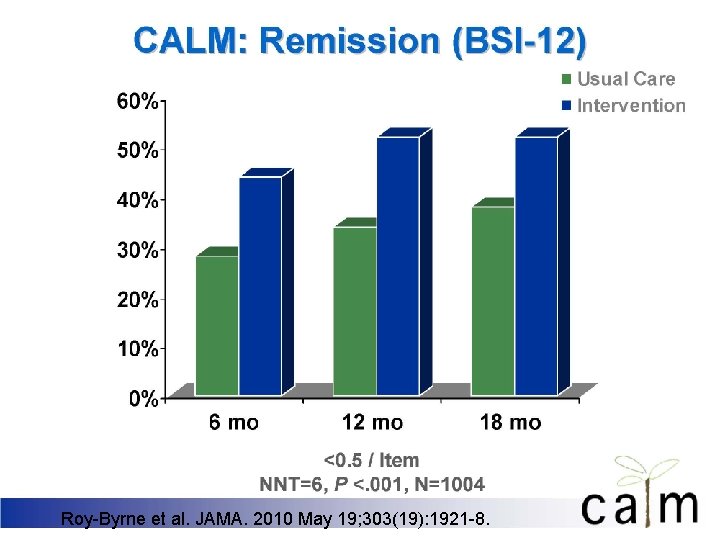
Roy-Byrne et al. JAMA. 2010 May 19; 303(19): 1921 -8.
Psychiatry e. Consults • Psychiatry e. Consults – From PCP to onsite psychiatrist – Appropriate for all visits that would not require a face to face visit – Initially at one site • Familiarity and continuity of care • In person consult available if needed • Utilize on-site resources
IBH Provider huddles • Primary care providers part of care teams – Meet weekly for 30 minutes • IBH providers meet weekly – Review patients – treatment planning – Review systems issues – Forum for brainstorming
Mayo/NAMI Connection Group • Peer-facilitated support group • Every 2 nd and 4 th Monday at NE Clinic – No appointment needed – No cost to patients – Confidential
EMERALD • Early Management and Evidence-based Recognition of Adolescents Living with Depression • Collaborative care model for managing adolescent depression • Includes a multidisciplinary team of: – – – IBH Care Coordinator (IBH CC) Primary Care Provider Child and Adolescent Psychiatrist LICSW (Psychotherapy) Other Health Care Professionals
Mental Health Integration • Evidence-based, team care aimed at improving family-centered care and quality health outcomes – Improve detection, monitoring, stratification, and management of depression and other mental health and medical conditions – Reinforce relationships with patients/families to promote self-management – Adjust treatment interventions/management to match complexity or inadequate response Reiss-Brennan et al. Group Practice Journal 2011 July-August 11 -15.
Five integration principles 1. Leadership and cultural integration – Identify and integrate ‘champions’ • Team leaders provide institutional commitment and accountability for program goals 2. Workflow integration – Train all staff from different backgrounds to use standardized tools and identified processes Reiss-Brennan et al. Group Practice Journal 2011 July-August 11 -15.
Five integration principles (con’t) 3. Information systems integration – EMR – Registry – e. Consults 4. Clinical and financial integration – Developed for depression, working on anxiety 5. Integration with the community – NAMI – Referral to community providers Reiss-Brennan et al. Group Practice Journal 2011 July-August 11 -15.
IBH: The Future • Continuing challenges • • Space EMR Staffing Chemical dependency Bipolar disorder Rollout to all of primary care at Mayo in Rochester (ECH) Rollout to the Mayo Clinic Health System sites • Serves 70 communities in Minnesota, Iowa and Wisconsin with nearly 800 physicians and 13, 000 allied health staff
Thank you! Questions? ? • angstman. kurt@mayo. edu • mitchell. jay@mayo. edu • somers. kristin@mayo. edu
- Slides: 40