Integrale zorg een blijvende ontwikkeling FRITS HUYSE Psychiater
Integrale zorg een blijvende ontwikkeling FRITS HUYSE Psychiater, Consulent Integrale Zorg Afdeling Algemene Interne Geneeskunde UMCG GRONINGEN Lid council Academy of Psychosomatic Medicine USA NFZP 9 -6 -2006 Universitair Medisch Centrum Utrecht UMCG Groningen
Hoofdstuk 6 Complexe patienten Huyse Slaets de Jonge
THE FUTURE OF CONSULTATION-LIAISON PSYCHIATRY Graeme C Smith Consultation-Liaison Psychiatry Research Unit Monash University Department of Psychological Medicine Keynote speaker Anual meeting Dutch Psychiatric Association Maastricht The Netherlands 2005
CONCLUSIONS ü Patients with physical/psychiatric comorbidity and somatisation continue to be discriminated against in the public sector, despite the acknowledgement of this in the Second National Mental Health Plan ü The implication for patients is both primary and secondary; the context in which psychiatrists are training is helping perpetuate the problem ü Development of a seamless web of preadmission/post discharge functions is required if patients are to receive effective care and services are to be able to demonstrate efficacy
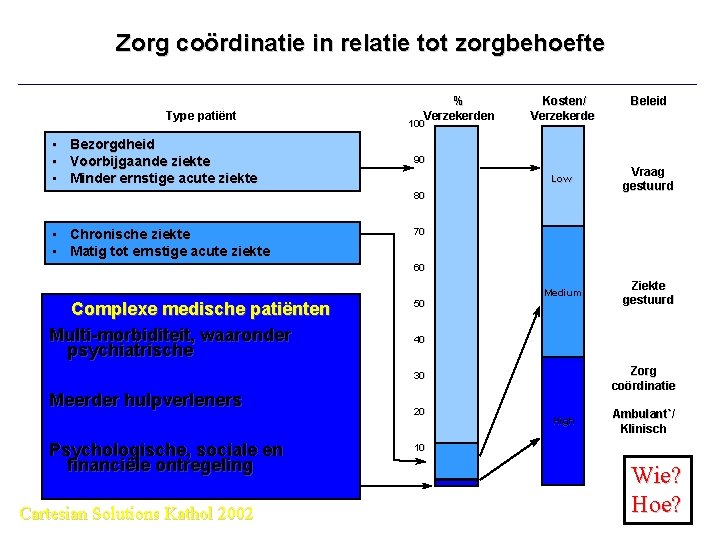
Zorg coördinatie in relatie tot zorgbehoefte Type patiënt • Bezorgdheid • Voorbijgaande ziekte • Minder ernstige acute ziekte % Verzekerden 100 Kosten/ Verzekerde 90 Low Vraag gestuurd Medium Ziekte gestuurd 80 • Chronische ziekte • Matig tot ernstige acute ziekte Beleid 70 60 Complexe medische patiënten Multi-morbiditeit, waaronder psychiatrische 50 40 Zorg coördinatie 30 Meerder hulpverleners Psychologische, sociale en financiële ontregeling Cartesian Solutions Kathol 2002 20 High Ambulant`/ Klinisch 10 Wie? Hoe?
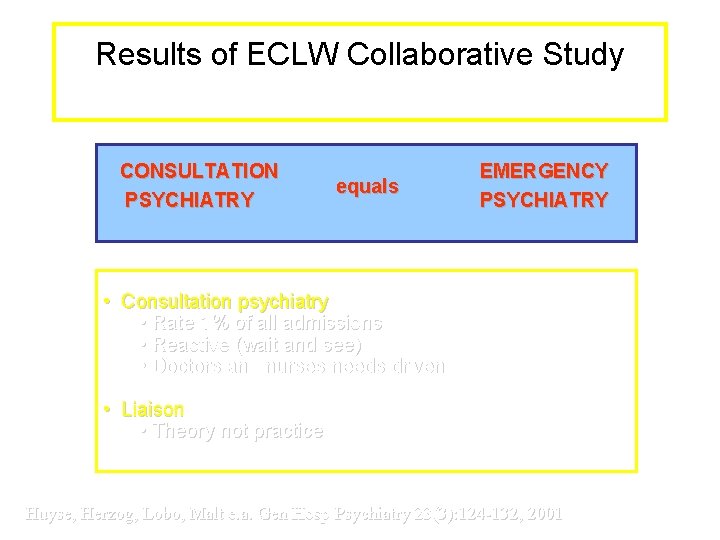
Results of ECLW Collaborative Study 14470 patients 56 hospitals 11 countries CONSULTATION PSYCHIATRY equals EMERGENCY PSYCHIATRY • Consultation psychiatry • Rate 1% of all admissions • Reactive (wait and see) • Doctors and nurses needs driven • Liaison • Theory not practice Huyse, Herzog, Lobo, Malt e. a. Gen Hosp Psychiatry 23(3): 124 -132, 2001
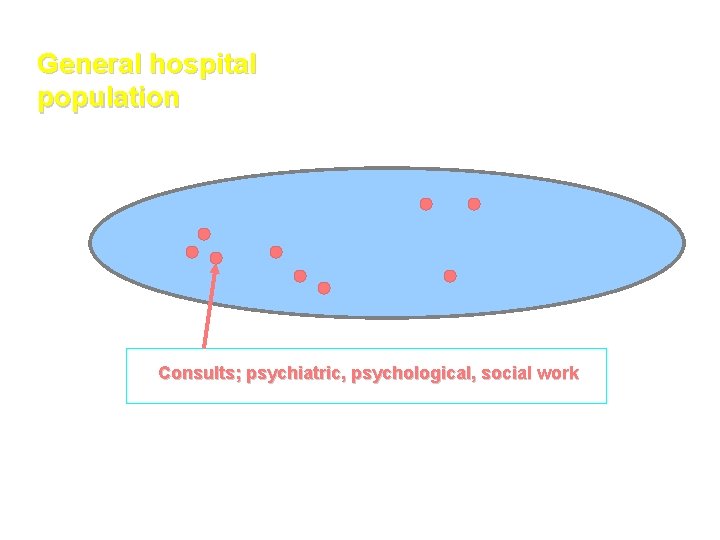
General hospital population Consults; psychiatric, psychological, social work
THE FUTURE OF CONSULTATION-LIAISON PSYCHIATRY Graeme C Smith Consultation-Liaison Psychiatry Research Unit Monash University Department of Psychological Medicine Keynote speaker Anual meeting Dutch Psychiatric Association Maastricht The Netherlands 2005
CONCLUSIONS ü Patients with physical/psychiatric comorbidity and somatisation continue to be discriminated against in the public sector, despite the acknowledgement of this in the Second National Mental Health Plan ü The implication for patients is both primary and secondary; the context in which psychiatrists are training is helping perpetuate the problem ü Development of a seamless web of preadmission/post discharge functions is required if patients are to receive effective care and services are to be able to demonstrate efficacy
THE FUTURE OF CONSULTATION-LIAISON PSYCHIATRY Graeme C Smith Consultation-Liaison Psychiatry Research Unit Monash University Department of Psychological Medicine Keynote speaker VJC NVv. P Maastricht 2005
CONCLUSIONS 1 Patients with physical/psychiatric comorbidity and somatisation continue to be discriminated against in the public sector, despite the acknowledgement of this in the Second National Mental Health Plan. Huyse NRC mei 2005: Geef psychiaters in ziekenhuizen de ruimte

“De ziekenhuispsychiatrie kan mijns inziens een belangrijke rol vervullen. In dit opzicht sluit ik mij aan bij het standpunt van de heer Huyse. De stelselwijziging in de zorg die nu plaatsvindt, is mede bedoeld om de “ontschotting” van de lichamelijke en psychische zorg te verwezenlijken. …”
CONCLUSIONS 2 The implication for patients is both primary and secondary; the context in which psychiatrists are training is helping perpetuate the problem. Huyse FJ, van der Mast RC, Boenink AD: De psychiater als medisch specialist: de psychiatrie een zorg? Tijdschrift voor Psychiatrie 44: 795 -802, 2002
CONCLUSIONS 3 Development of a seamless web of preadmission/post discharge functions is required if patients are to receive effective care and services are to be able to demonstrate efficacy. Integrated care for the complex medically ill. Editors Huyse FJ, Stiefel FC Medical clinics of North America Elsevier Juli 2006
Crossing the Quality Chasm “Quality problems occur typically not because of failure of goodwill, knowledge, effort or resources devoted to health care, but because of fundamental shortcomings in the ways care is organized” Trying harder will not work: changing systems of care will! a new HEALTH system for the 21 st century (IOM, 2001)
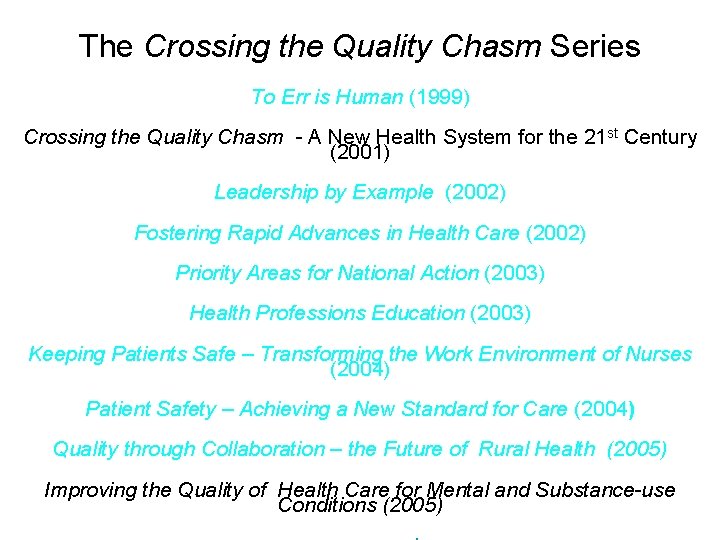
The Crossing the Quality Chasm Series To Err is Human (1999) Crossing the Quality Chasm - A New Health System for the 21 st Century (2001) Leadership by Example (2002) Fostering Rapid Advances in Health Care (2002) Priority Areas for National Action (2003) Health Professions Education (2003) Keeping Patients Safe – Transforming the Work Environment of Nurses (2004) Patient Safety – Achieving a New Standard for Care (2004) Quality through Collaboration – the Future of Rural Health (2005) Improving the Quality of Health Care for Mental and Substance-use Conditions (2005)
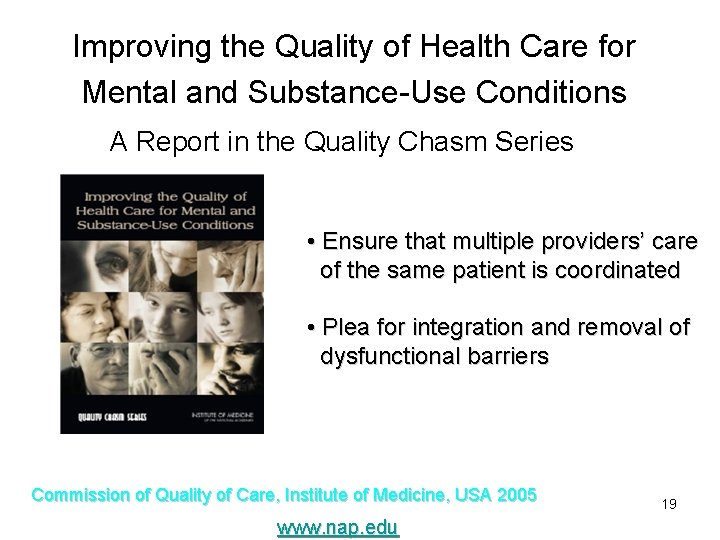
Improving the Quality of Health Care for Mental and Substance-Use Conditions A Report in the Quality Chasm Series • Ensure that multiple providers’ care of the same patient is coordinated • Plea for integration and removal of dysfunctional barriers Commission of Quality of Care, Institute of Medicine, USA 2005 www. nap. edu 19
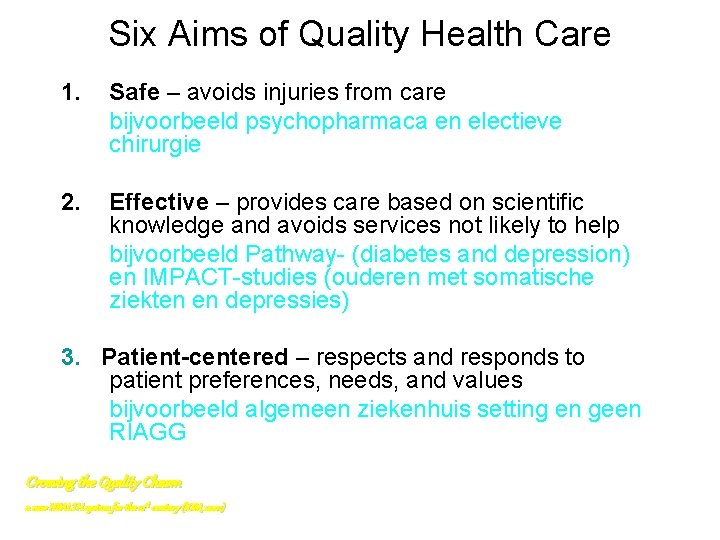
Six Aims of Quality Health Care 1. Safe – avoids injuries from care bijvoorbeeld psychopharmaca en electieve chirurgie 2. Effective – provides care based on scientific knowledge and avoids services not likely to help bijvoorbeeld Pathway- (diabetes and depression) en IMPACT-studies (ouderen met somatische ziekten en depressies) 3. Patient-centered – respects and responds to patient preferences, needs, and values bijvoorbeeld algemeen ziekenhuis setting en geen RIAGG Crossing the Quality Chasm a new HEALTH system for the 21 st century (IOM, 2001)

De berg naar Mohammed of …………
……… of de psychiatrie naar de AGZ !

Six Aims (cont. ) 4. Timely – reduces waits and sometimes harmful delays for those receiving and giving care bijvoorbeeld geïntegreerde consulten bij onbegrepen klachten poli interne UMCG; gelijktijdig consult internist en psychiater 5. Efficient – avoids waste, including waste of equipment, supplies, ideas and energy bijvoorbeeld rechtstreekse verwijzing naar collega; “snuffelconsult” 6. Equitable – care does not vary in quality due to personal characteristics (gender, ethnicity, geographic location, or socio -economic status) bijvoorbeeld psychiatrische patient heeft gelijke toegang tot somatische zorg vv Crossing the Quality Chasm a new HEALTH system for the 21 st century (IOM, 2001)
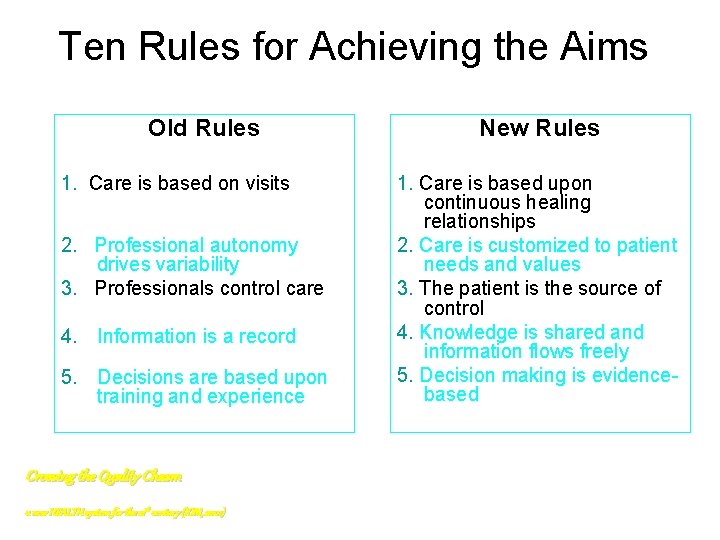
Ten Rules for Achieving the Aims Old Rules 1. Care is based on visits 2. Professional autonomy drives variability 3. Professionals control care 4. Information is a record 5. Decisions are based upon training and experience Crossing the Quality Chasm a new HEALTH system for the 21 st century (IOM, 2001) New Rules 1. Care is based upon continuous healing relationships 2. Care is customized to patient needs and values 3. The patient is the source of control 4. Knowledge is shared and information flows freely 5. Decision making is evidencebased
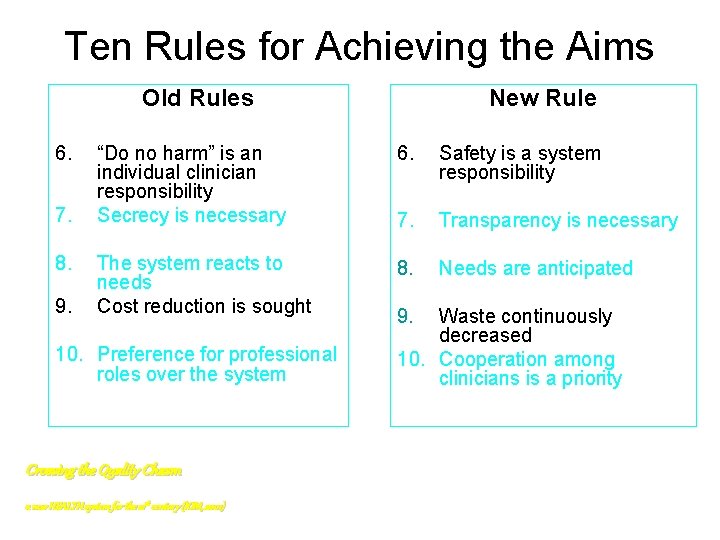
Ten Rules for Achieving the Aims Old Rules 6. 7. 8. 9. New Rule “Do no harm” is an individual clinician responsibility Secrecy is necessary 6. Safety is a system responsibility 7. Transparency is necessary The system reacts to needs Cost reduction is sought 8. Needs are anticipated 10. Preference for professional roles over the system Crossing the Quality Chasm a new HEALTH system for the 21 st century (IOM, 2001) 9. Waste continuously decreased 10. Cooperation among clinicians is a priority
Achieving Aims and Rules Requires • News ways of delivering care • Effective use of information technology (IT) • Managing the clinical knowledge, skills, and deployment of the workforce • Effective teams and coordination of care across patient conditions, services and settings • Improvements in how quality is measured • Payment methods conducive to good quality Crossing the Quality Chasm a new HEALTH system for the 21 st century (IOM, 2001)

Interdisciplinaire Opleidingen Een kans voor Interne Geneeskunde en Psychiatrie? ROB Gans Hoogleraar Interne UMCG VJC NVv. P Amsterdam, April 4, 2003 Thisbee en ….
Mental health services in the general hospital 1. Emergency services a. Attempted suicide b. Acute behavioral disturbances a. Deliria b. Withdrawal 2. Integrated services a. Screening and integrated assessment b. Patient tailored multidisciplinary care (horizontal integration) and care trajectories (vertical integration)
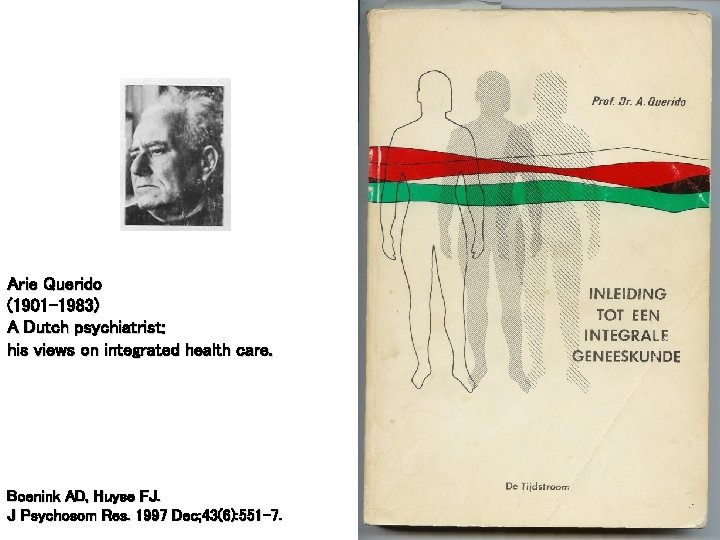
Arie Querido (1901 -1983) A Dutch psychiatrist: his views on integrated health care. Boenink AD, Huyse FJ. J Psychosom Res. 1997 Dec; 43(6): 551 -7.
Visie Querido 1935: Psychiatrie d’urgence – Naast gestichtspsychiatrie moet ambulante psychiatrie ontwikkeld worden tbv voor en nazorg – Dit is de motor achter de RIAGG vorming (70 er jaren) en zorgcircuitgedachte (negentiger jaren) geweest 1955: Integrale geneeskunde – Populatie gebaseerde studie in Weesperplein ziekenhuis waarin hij als een van de eersten aantoonde dat PScomorbiditeit leidt tot slechte uitkomsten van somatische zorg
Ontwikkeling integrale geneeskunde Querido verliet de psychiatrie en werkte uiteindelijk in de sociale geneeskunde Rooijmans, voormalig voorzitter van de NVv. P, zette de ziekenhuispsychiatrie op de kaart De huidige academische psychiatrie heeft geen visie op dit vakgebied
Ontwikkeling integrale geneeskunde Querido verliet de psychiatrie en werkte uiteindelijk in de sociale geneeskunde Rooijmans, voormalig voorzitter van de NVv. P, zette de ziekenhuispsychiatrie op de kaart De huidige academische psychiatrie heeft geen visie op dit vakgebied USA 1980: alle kernhoogleraren psychiatrie zijn psychoanalytici 1990: geen kernhoogleraar is psychoanalyticus
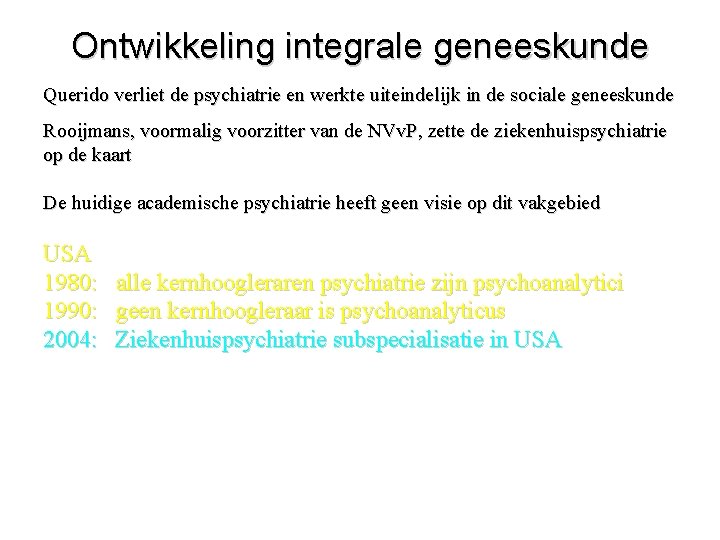
Ontwikkeling integrale geneeskunde Querido verliet de psychiatrie en werkte uiteindelijk in de sociale geneeskunde Rooijmans, voormalig voorzitter van de NVv. P, zette de ziekenhuispsychiatrie op de kaart De huidige academische psychiatrie heeft geen visie op dit vakgebied USA 1980: 1990: 2004: alle kernhoogleraren psychiatrie zijn psychoanalytici geen kernhoogleraar is psychoanalyticus Ziekenhuispsychiatrie subspecialisatie in USA
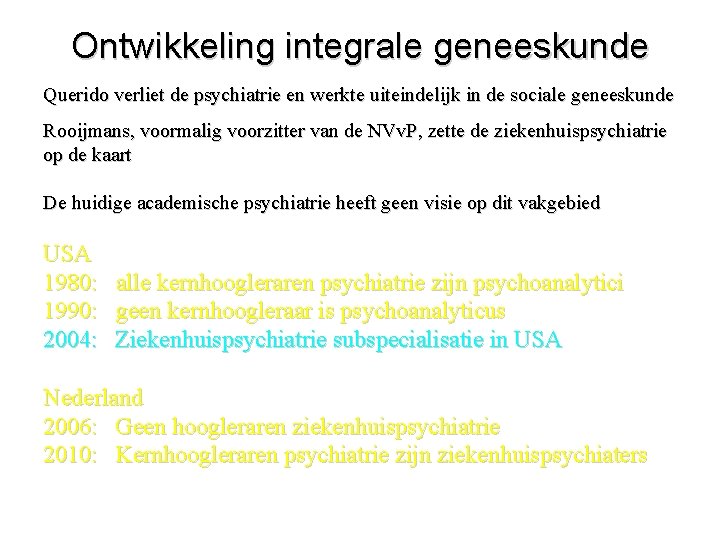
Ontwikkeling integrale geneeskunde Querido verliet de psychiatrie en werkte uiteindelijk in de sociale geneeskunde Rooijmans, voormalig voorzitter van de NVv. P, zette de ziekenhuispsychiatrie op de kaart De huidige academische psychiatrie heeft geen visie op dit vakgebied USA 1980: 1990: 2004: alle kernhoogleraren psychiatrie zijn psychoanalytici geen kernhoogleraar is psychoanalyticus Ziekenhuispsychiatrie subspecialisatie in USA Nederland 2006: Geen hoogleraren ziekenhuispsychiatrie 2010: Kernhoogleraren psychiatrie zijn ziekenhuispsychiaters
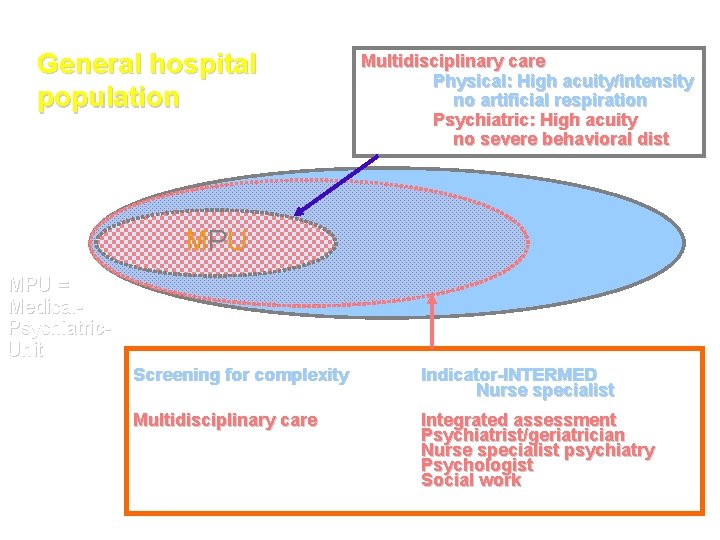
General hospital population Multidisciplinary care Physical: High acuity/intensity no artificial respiration Psychiatric: High acuity no severe behavioral dist MP U MPU = Medical. Psychiatric. Unit Screening for complexity Indicator-INTERMED Nurse specialist Multidisciplinary care Integrated assessment Psychiatrist/geriatrician Nurse specialist psychiatry Psychologist Social work
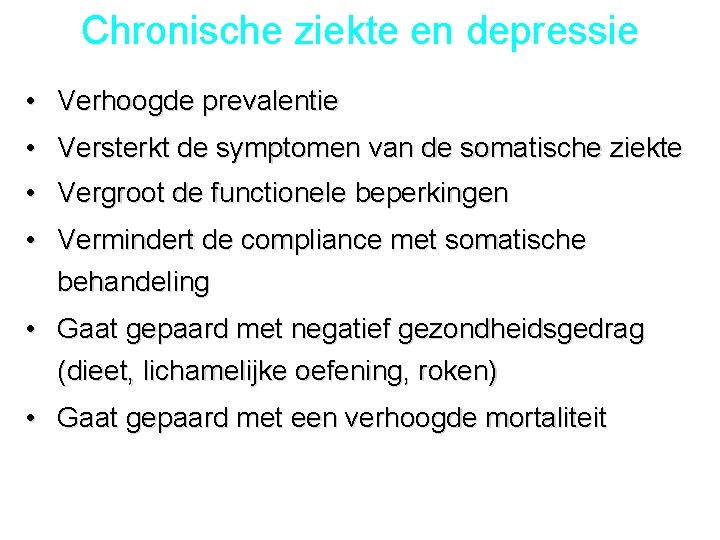
Chronische ziekte en depressie • Verhoogde prevalentie • Versterkt de symptomen van de somatische ziekte • Vergroot de functionele beperkingen • Vermindert de compliance met somatische behandeling • Gaat gepaard met negatief gezondheidsgedrag (dieet, lichamelijke oefening, roken) • Gaat gepaard met een verhoogde mortaliteit
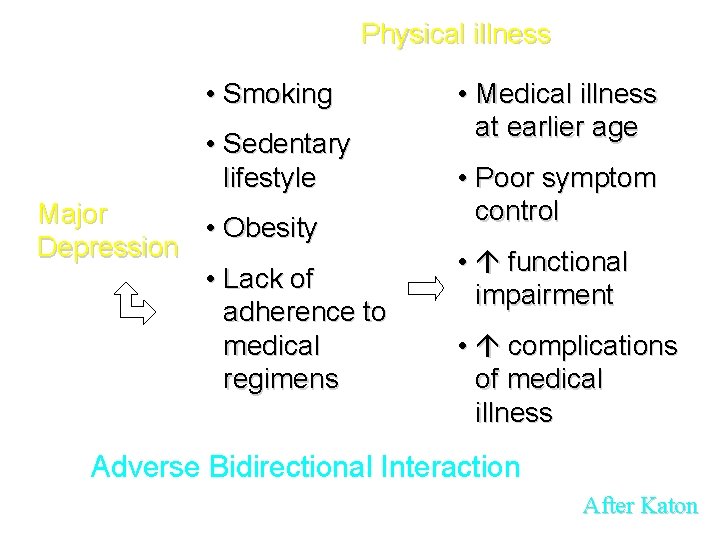
Physical illness • Smoking • Sedentary lifestyle Major • Obesity Depression • Lack of adherence to medical regimens • Medical illness at earlier age • Poor symptom control • functional impairment • complications of medical illness Adverse Bidirectional Interaction After Katon
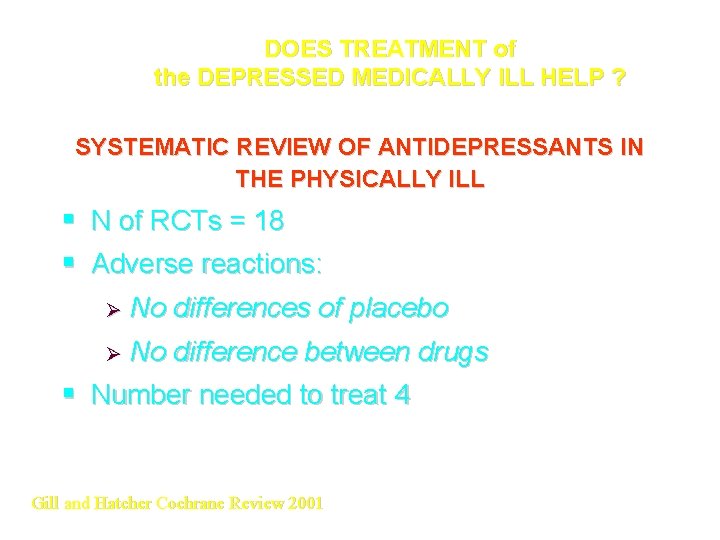
DOES TREATMENT of the DEPRESSED MEDICALLY ILL HELP ? SYSTEMATIC REVIEW OF ANTIDEPRESSANTS IN THE PHYSICALLY ILL § N of RCTs = 18 § Adverse reactions: Ø No differences of placebo Ø No difference between drugs § Number needed to treat 4 Gill and Hatcher Cochrane Review 2001
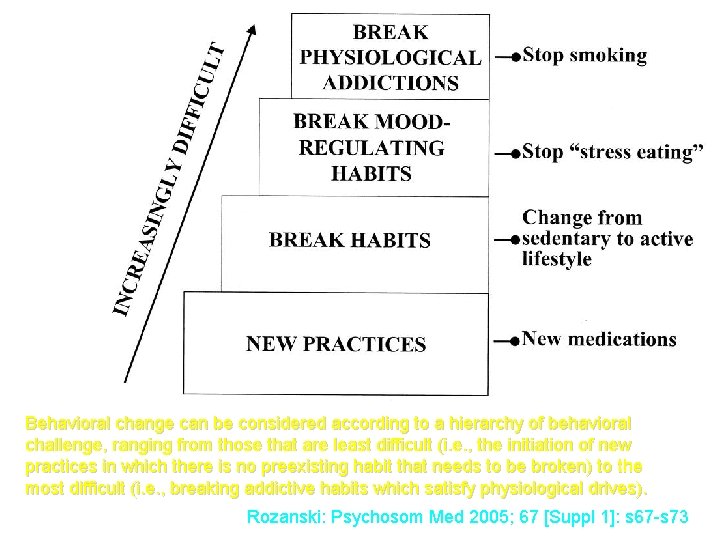
Behavioral change can be considered according to a hierarchy of behavioral challenge, ranging from those that are least difficult (i. e. , the initiation of new practices in which there is no preexisting habit that needs to be broken) to the most difficult (i. e. , breaking addictive habits which satisfy physiological drives). Rozanski: Psychosom Med 2005; 67 [Suppl 1]: s 67 -s 73

MODELLEN VOOR INTEGRALE ZORG
MODELLEN VOOR INTEGRALE ZORG • Depressie en somatische ziekte
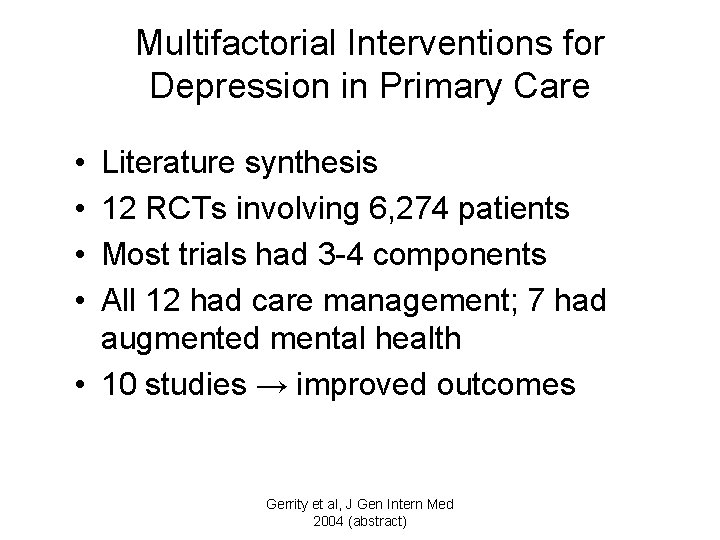
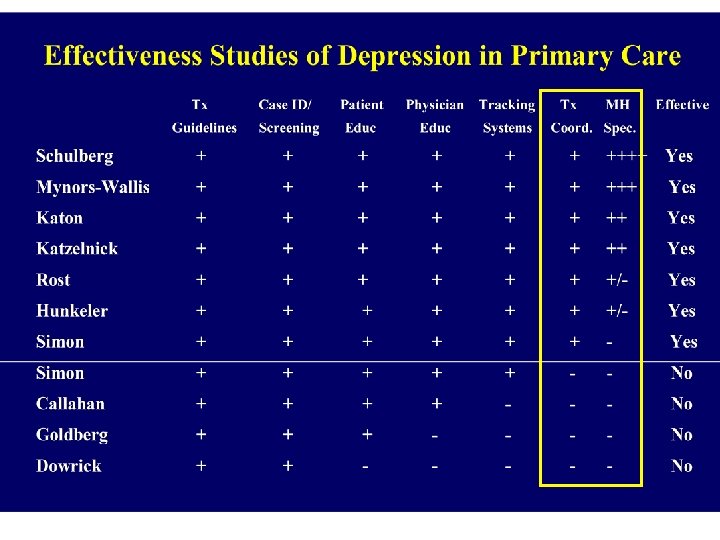
Multifactorial Interventions for Depression in Primary Care • • Literature synthesis 12 RCTs involving 6, 274 patients Most trials had 3 -4 components All 12 had care management; 7 had augmented mental health • 10 studies → improved outcomes Gerrity et al, J Gen Intern Med 2004 (abstract)
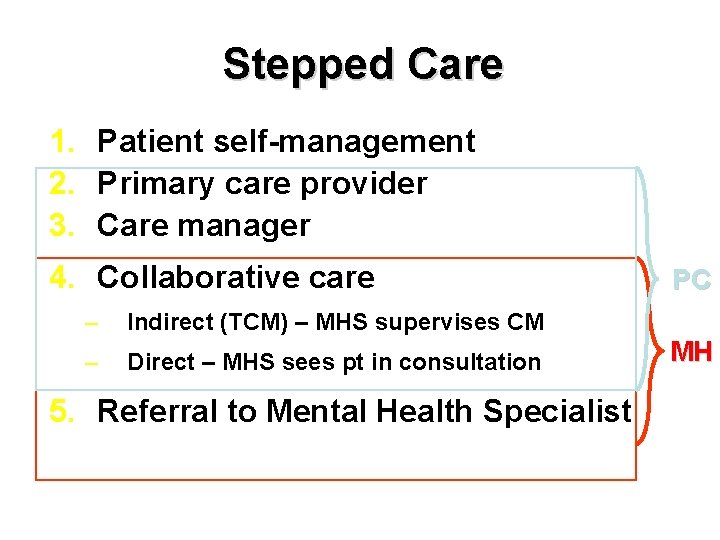
Stepped Care 1. Patient self-management 2. Primary care provider 3. Care manager 4. Collaborative care – Indirect (TCM) – MHS supervises CM – Direct – MHS sees pt in consultation 5. Referral to Mental Health Specialist PC MH
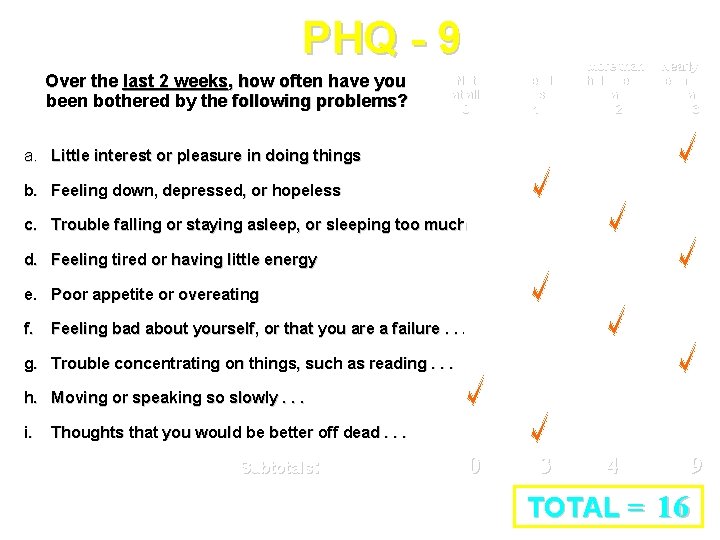
PHQ - 9 Over the last 2 weeks, how often have you been bothered by the following problems? Not at all 0 Several days 1 More than half the days 2 Nearly every day 3 a. Little interest or pleasure in doing things b. Feeling down, depressed, or hopeless c. Trouble falling or staying asleep, or sleeping too much d. Feeling tired or having little energy e. Poor appetite or overeating f. Feeling bad about yourself, or that you are a failure. . . g. Trouble concentrating on things, such as reading. . . h. Moving or speaking so slowly. . . i. Thoughts that you would be better off dead. . . Subtotals: 0 3 4 9 TOTAL = 16
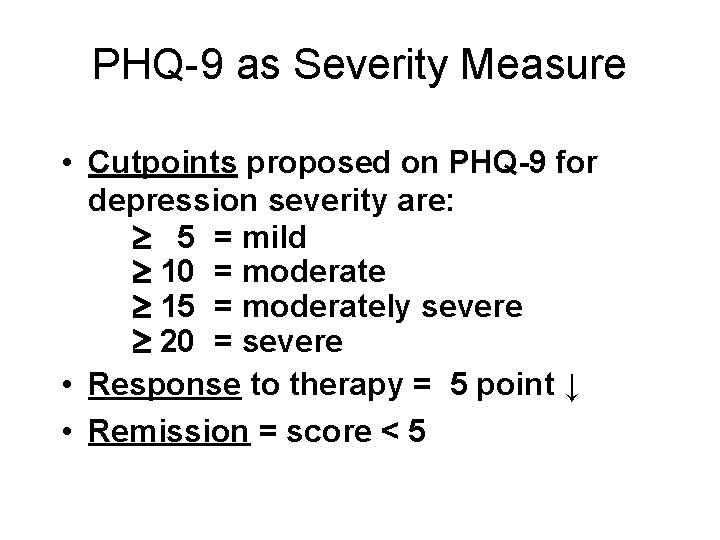
PHQ-9 as Severity Measure • Cutpoints proposed on PHQ-9 for depression severity are: 5 = mild 10 = moderate 15 = moderately severe 20 = severe • Response to therapy = 5 point ↓ • Remission = score < 5
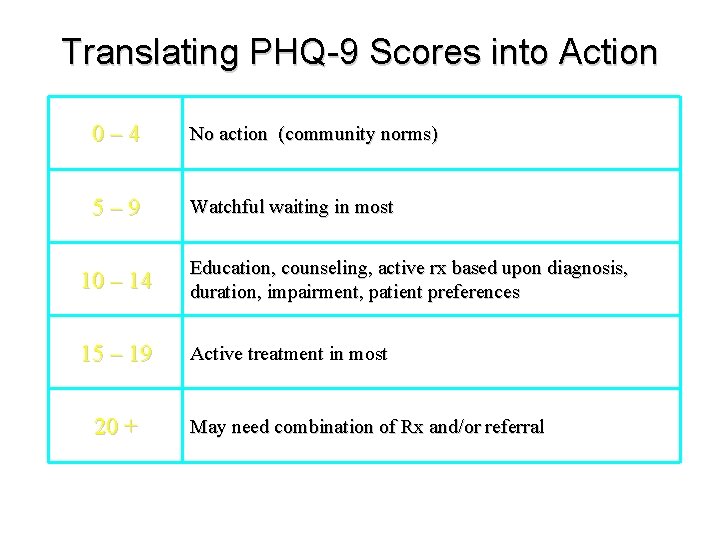
Translating PHQ-9 Scores into Action 0– 4 No action (community norms) 5– 9 Watchful waiting in most 10 – 14 Education, counseling, active rx based upon diagnosis, duration, impairment, patient preferences 15 – 19 Active treatment in most 20 + May need combination of Rx and/or referral
The Pathway Study • RCT: depressie en diabetes mellitus – Verbetert diabetes door verbeterde depressie zorg? • Intervention: stepped care Tx depression – N=329 (int: 164; CAU 165) – 9 primary care klinieken • Outcomes: – – Verbetering depressie 6 en 12 mnd Verbetering algemeen gevoel na 6 en 12 mnd Meer satisfactie met type zorg na 6 en 12 mnd HBA-1 C gelijk in interventie en controle groep Katon, Von Korff (2004) Arch Gen Psych 61: 1042 -1049
IMPACT Improving Mood – Promoting Access to Collaborative Treatment for Late-Life Depression 1801 18 8 depressive elderly (>/60 years) clinical practices healthplans Funded by John A. Hartford Foundation California Health. Care Foundation California Geriatric Education Center (via the Bureau of Health Professions, HRSA) Unutzer J, Katon W, Callahan CM ea. IMPACT. JAMA 2002; 288(22): 2835 -45
IMPACT Improving Mood – Promoting Access to Collaborative Treatment for Late-Life Depression 1801 18 8 depressive elderly (>/60 years) clinical practices healthplans Funded by John A. Hartford Foundation California Health. Care Foundation California Geriatric Education Center (via the Bureau of Health Professions, HRSA) 3. 8 chronic conditions Unutzer J, Katon W, Callahan CM ea. IMPACT. JAMA 2002; 288(22): 2835 -45
In the IMPACT study the patients had 3. 8 chronic conditions in addition to depression • e. g. cardiac • diabetes • parkinson • . .
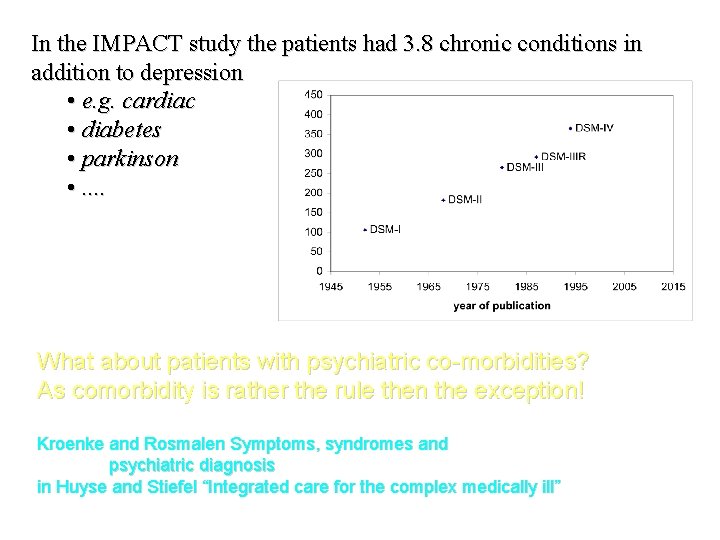
In the IMPACT study the patients had 3. 8 chronic conditions in addition to depression • e. g. cardiac • diabetes • parkinson • . . What about patients with psychiatric co-morbidities? As comorbidity is rather the rule then the exception! Kroenke and Rosmalen Symptoms, syndromes and psychiatric diagnosis in Huyse and Stiefel “Integrated care for the complex medically ill”
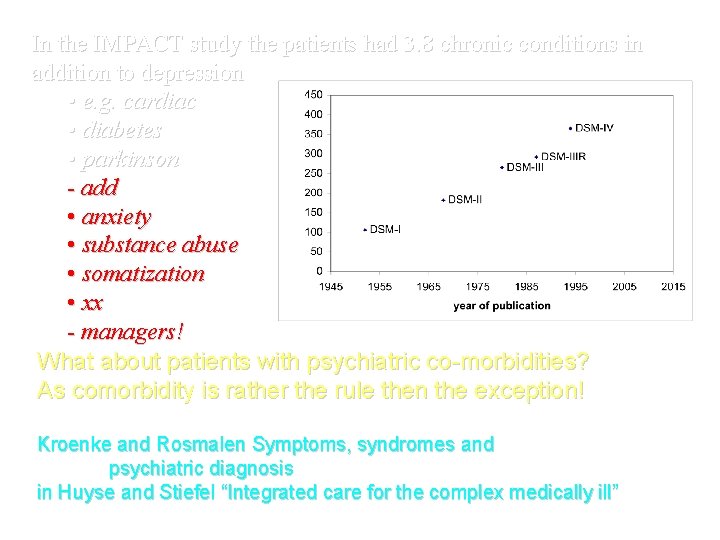
In the IMPACT study the patients had 3. 8 chronic conditions in addition to depression • e. g. cardiac • diabetes • parkinson - add • anxiety • substance abuse • somatization • xx - managers! What about patients with psychiatric co-morbidities? As comorbidity is rather the rule then the exception! Kroenke and Rosmalen Symptoms, syndromes and psychiatric diagnosis in Huyse and Stiefel “Integrated care for the complex medically ill”
Chronic Disease Focused Depression Care: New Grant • Nurse will provide depression, heart disease and diabetes case management • Behavior intervention-especially exercise, positive life activities • Optimize medication for depression, heart disease and diabetes • Supervision of nurses by psychiatrists and PCPs Katon and Unutzer
Chronic Disease Focused Depression Care: New Grant • Nurse will provide depression, heart disease and diabetes case management • Behavior intervention-especially exercise, positive life activities • Optimize medication for depression, heart disease and diabetes • Supervision of nurses by psychiatrists and PCPs Katon and Unutzer = Complexity management
MODELLEN VOOR INTEGRALE ZORG • Depressie en somatische ziekte • Ziekte specifiek
MODELLEN VOOR INTEGRALE ZORG • Depressie en somatische ziekte • Ziekte specifiek • Complexiteit
MODELLEN VOOR INTEGRALE ZORG • Depressie en somatische ziekte • Ziekte specifiek • Complexiteit • Generiek
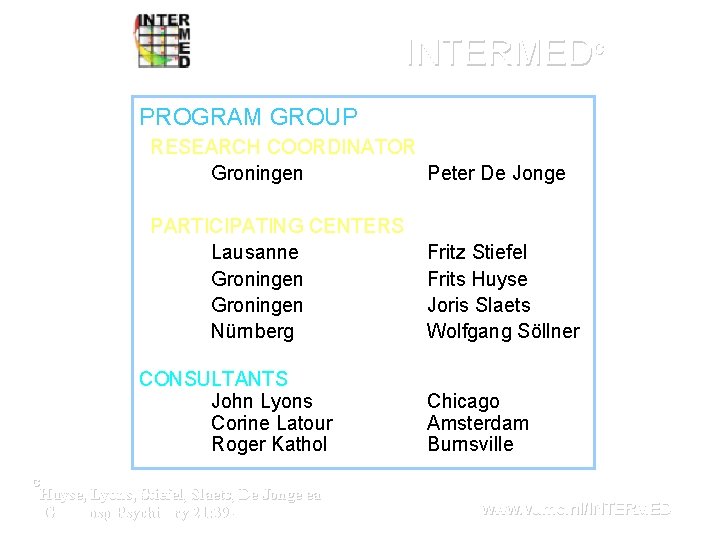
INTERMEDc PROGRAM GROUP RESEARCH COORDINATOR Groningen Peter De Jonge PARTICIPATING CENTERS Lausanne Groningen Nürnberg CONSULTANTS John Lyons Corine Latour Roger Kathol Fritz Stiefel Frits Huyse Joris Slaets Wolfgang Söllner Chicago Amsterdam Burnsville C Huyse, Lyons, Stiefel, Slaets, De Jonge ea Gen Hosp Psychiatry 21: 39 -48, 1999 www. vumc. nl/INTERMED
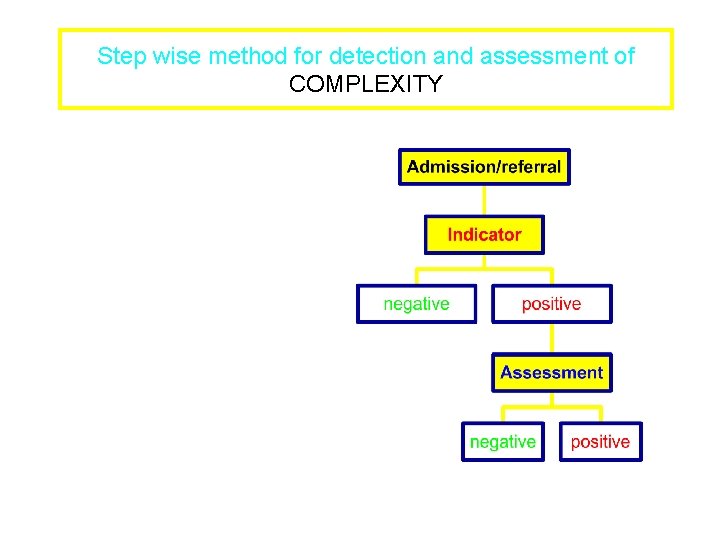
Step wise method for detection and assessment of COMPLEXITY
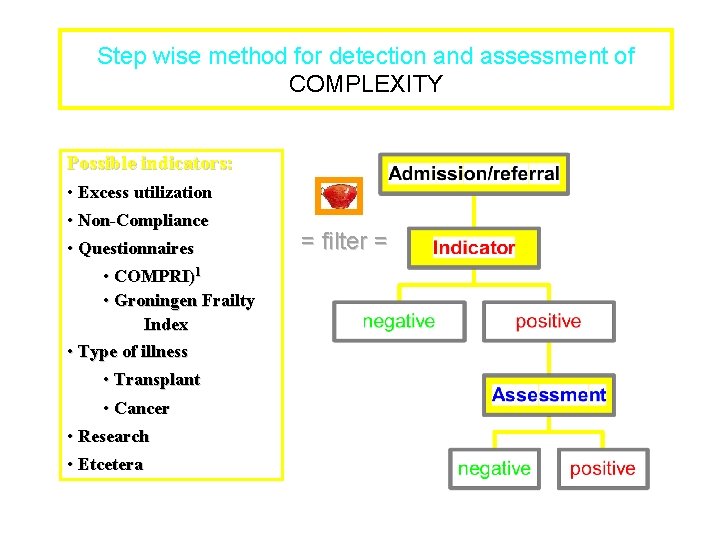
Step wise method for detection and assessment of COMPLEXITY Possible indicators: • Excess utilization • Non-Compliance • Questionnaires • COMPRI)1 • Groningen Frailty Index • Type of illness • Transplant • Cancer • Research • Etcetera = filter =
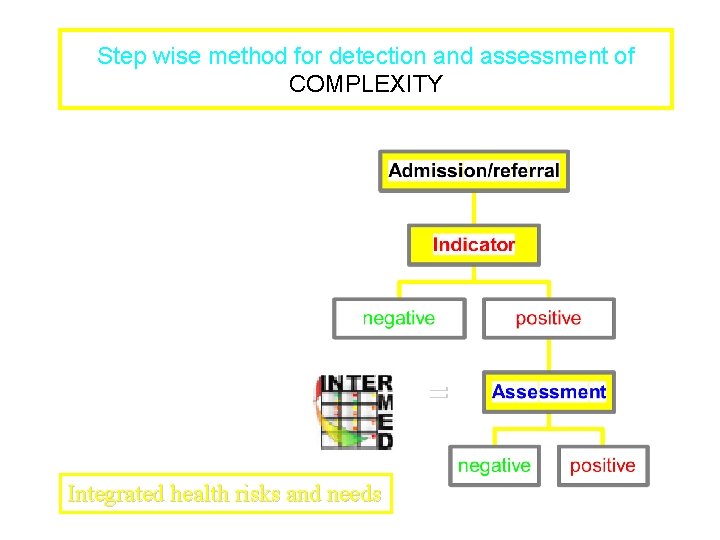
Step wise method for detection and assessment of COMPLEXITY = Integrated health risks and needs

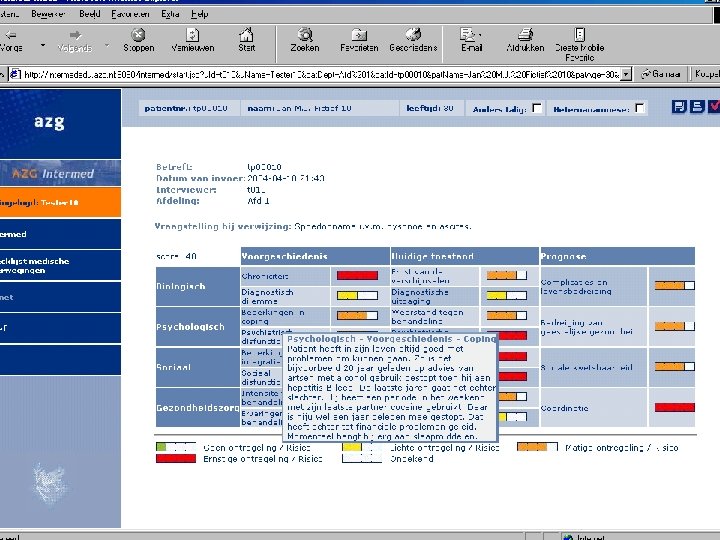

Intervention studies Pre/post internal medicine IP (NL) – Reduction of LOS in elderly (16 -> 11 days) – Improvement in psychological functioning RCT prevention readmission post discharge (NL) – No effects; restricted funding and lack of cooperation/integration
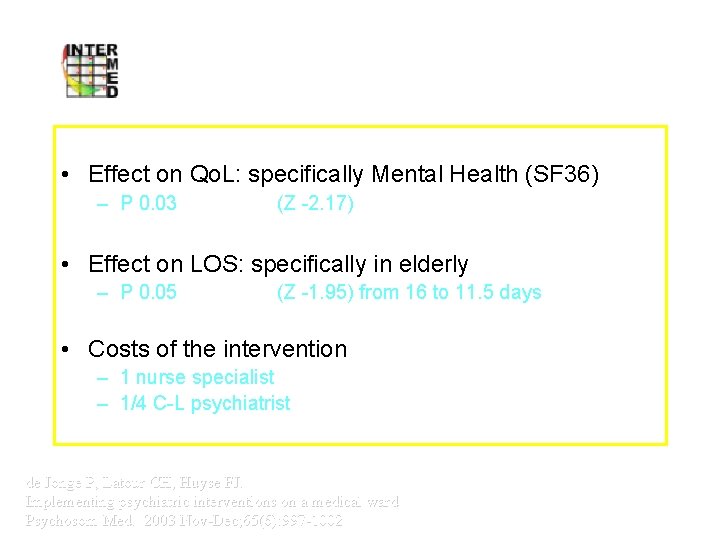
Intervention Study Internal Medicine Vumc • Effect on Qo. L: specifically Mental Health (SF 36) – P 0. 03 (Z -2. 17) • Effect on LOS: specifically in elderly – P 0. 05 (Z -1. 95) from 16 to 11. 5 days • Costs of the intervention – 1 nurse specialist – 1/4 C-L psychiatrist de Jonge P, Latour CH, Huyse FJ. Implementing psychiatric interventions on a medical ward Psychosom Med. 2003 Nov-Dec; 65(6): 997 -1002
Intervention studies Pre/post internal medicine IP (NL) – Reduction of LOS in elderly (16 -> 11 days) – Improvement in psychological functioning RCT prevention readmission post discharge (NL) – No effects; restricted funding and lack of cooperation/integration RCT depression and DM or Rheuma – In analysis; positive effects on most outcomes (SU)
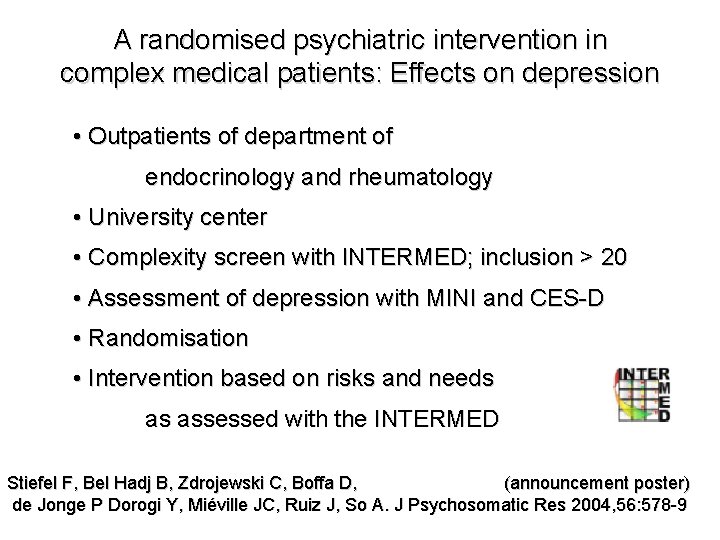
A randomised psychiatric intervention in complex medical patients: Effects on depression • Outpatients of department of endocrinology and rheumatology • University center • Complexity screen with INTERMED; inclusion > 20 • Assessment of depression with MINI and CES-D • Randomisation • Intervention based on risks and needs as assessed with the INTERMED Stiefel F, Bel Hadj B, Zdrojewski C, Boffa D, (announcement poster) de Jonge P Dorogi Y, Miéville JC, Ruiz J, So A. J Psychosomatic Res 2004, 56: 578 -9
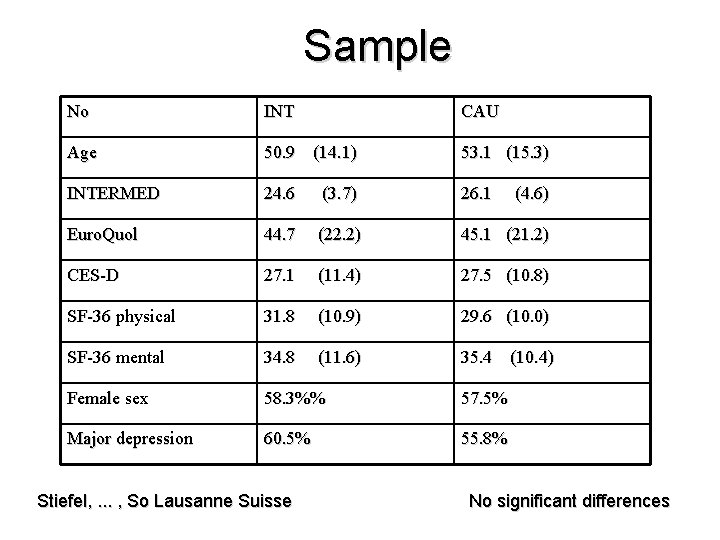
Sample No INT CAU Age 50. 9 (14. 1) 53. 1 (15. 3) INTERMED 24. 6 (3. 7) 26. 1 Euro. Quol 44. 7 (22. 2) 45. 1 (21. 2) CES-D 27. 1 (11. 4) 27. 5 (10. 8) SF-36 physical 31. 8 (10. 9) 29. 6 (10. 0) SF-36 mental 34. 8 (11. 6) 35. 4 (10. 4) Female sex 58. 3%% 57. 5% Major depression 60. 5% 55. 8% Stiefel, . . . , So Lausanne Suisse (4. 6) No significant differences
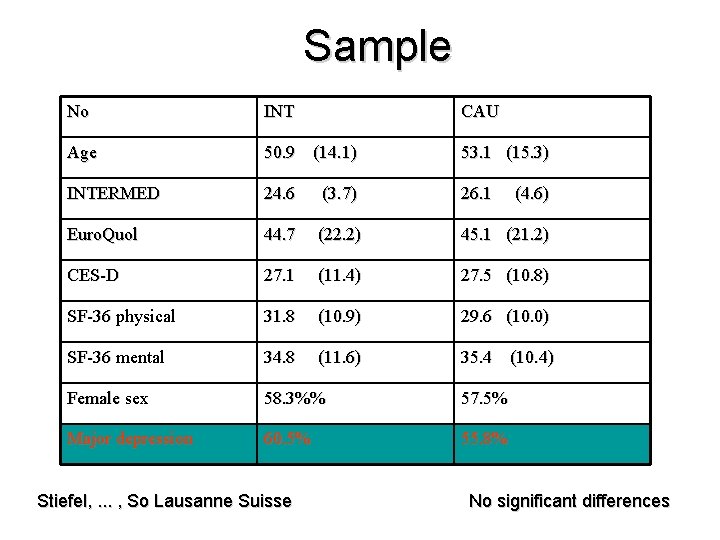
Sample No INT CAU Age 50. 9 (14. 1) 53. 1 (15. 3) INTERMED 24. 6 (3. 7) 26. 1 Euro. Quol 44. 7 (22. 2) 45. 1 (21. 2) CES-D 27. 1 (11. 4) 27. 5 (10. 8) SF-36 physical 31. 8 (10. 9) 29. 6 (10. 0) SF-36 mental 34. 8 (11. 6) 35. 4 (10. 4) Female sex 58. 3%% 57. 5% Major depression 60. 5% 55. 8% Stiefel, . . . , So Lausanne Suisse (4. 6) No significant differences
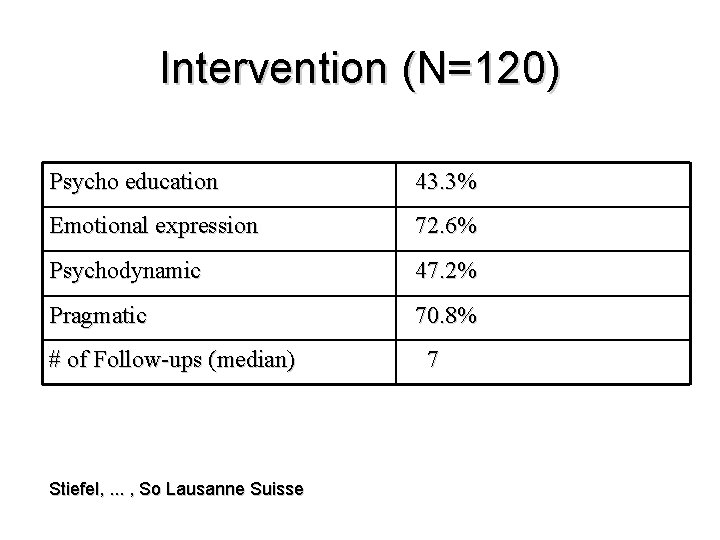
Intervention (N=120) Psycho education 43. 3% Emotional expression 72. 6% Psychodynamic 47. 2% Pragmatic 70. 8% # of Follow-ups (median) Stiefel, . . . , So Lausanne Suisse 7
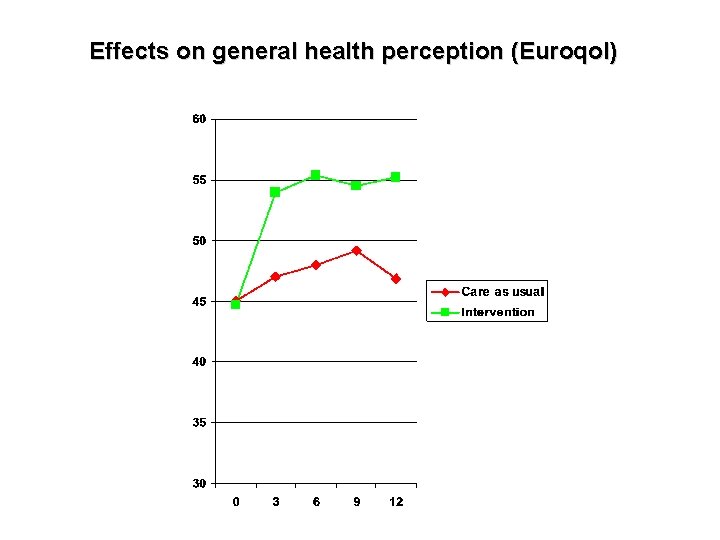
Effects on general health perception (Euroqol)
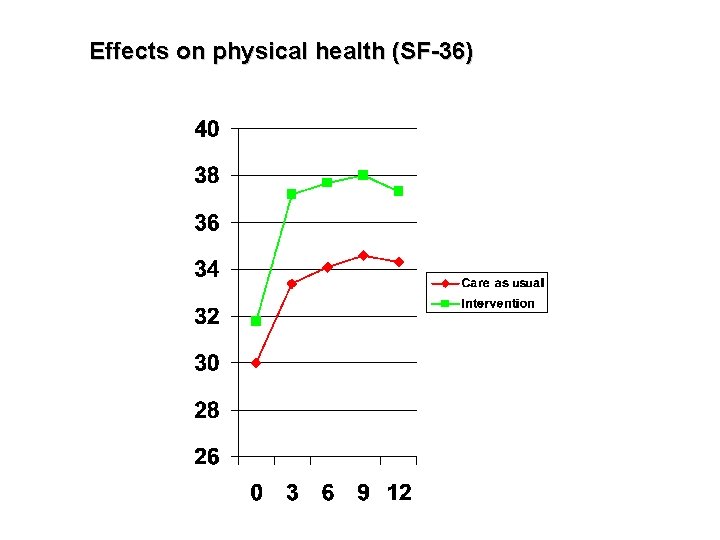
Effects on physical health (SF-36)
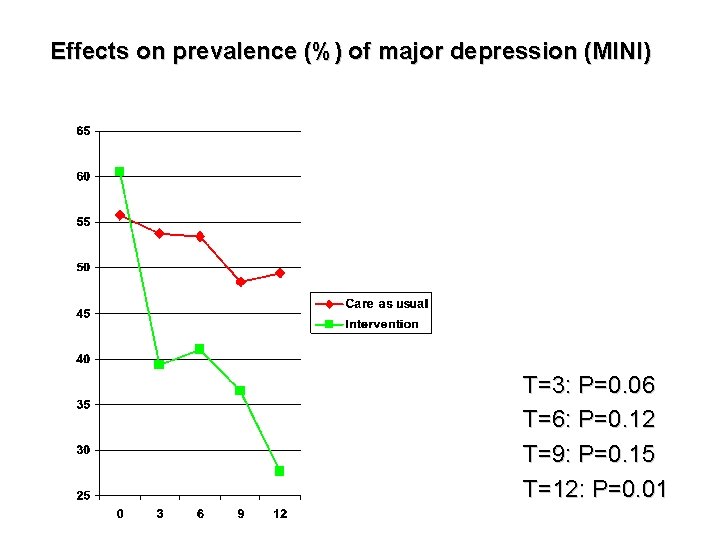
Effects on prevalence (%) of major depression (MINI) T=3: P=0. 06 T=6: P=0. 12 T=9: P=0. 15 T=12: P=0. 01
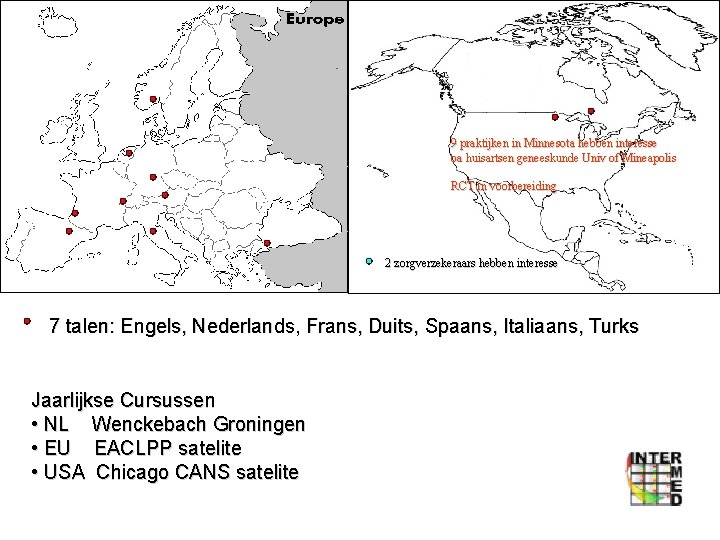
9 praktijken in Minnesota hebben interesse oa huisartsen geneeskunde Univ of Mineapolis RCT in voorbereiding 2 zorgverzekeraars hebben interesse 7 talen: Engels, Nederlands, Frans, Duits, Spaans, Italiaans, Turks Jaarlijkse Cursussen • NL Wenckebach Groningen • EU EACLPP satelite • USA Chicago CANS satelite
Developments Several studies on their way and in preparation – Transplant. MC outcome prediction study Europe – MC RCT in oncology Germany – Preassessment in elective surgery Groningen – RCT depression and rheuma/diabetes Minneapolis USA – RCT Functional neurologic complaints – Touchscreen module for patient self assessment INTERMEDFoundation INTERMED BV • webbased training • webbased clinical support AMC NL Groningen January 2006 Beginning 2007


Staatsecretaris voor Integrale zorg
Na regen komt zonneschijn!
- Slides: 84