InsulinDependent Diabetes Mellitus IDDM Anesthetic Implications and Perioperative
Insulin-Dependent Diabetes Mellitus (IDDM): Anesthetic Implications and Perioperative Management Odinakachukwu Ehie, MD Clinical Assistant Professor UCSF Benioff Children’s Hospital
Disclosures No relevant financial relationships
Learning Objectives: • Discuss diabetes mellitus and the importance for anesthesia providers to know about it • Review symptoms and diagnostic criteria for insulin-dependent diabetes • Provide guidelines in the management of insulin-dependent diabetes mellitus as well as fasting recommendations prior to surgery • Discuss the importance of a multidisciplinary approach for perioperative management • Discuss diabetic ketoacidosis and management
Overview • Diabetes mellitus - Most common metabolic disorder in pediatric patients - Increasing global incidence • Diabetes mellitus is characterized by high blood glucose levels from defects in insultin secretion and/or action • Perioperative blood glucose control can be challenging: - Physiological and metabolic stress as well as disruptions in routine - Maintain electrolyte balance and optimal hydration - Communicate with surgeons, pediatric diabetes team, and ward staff to facilitate optimal care
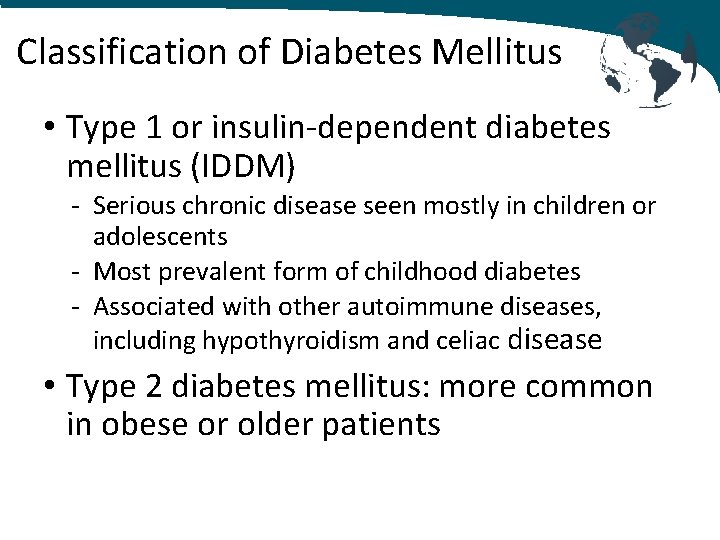
Classification of Diabetes Mellitus • Type 1 or insulin-dependent diabetes mellitus (IDDM) - Serious chronic disease seen mostly in children or adolescents - Most prevalent form of childhood diabetes - Associated with other autoimmune diseases, including hypothyroidism and celiac disease • Type 2 diabetes mellitus: more common in obese or older patients
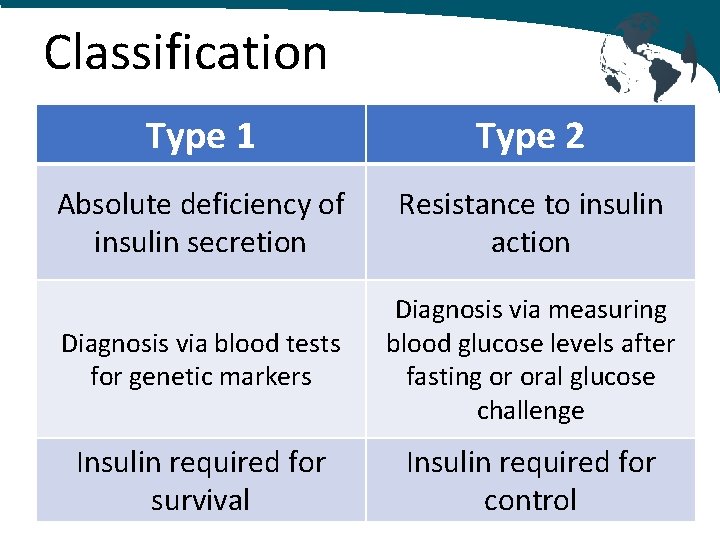
Classification Type 1 Type 2 Absolute deficiency of insulin secretion Resistance to insulin action Diagnosis via blood tests for genetic markers Diagnosis via measuring blood glucose levels after fasting or oral glucose challenge Insulin required for survival Insulin required for control

Pathophysiology of IDDM Low insulin levels Lower insulin levels Lipolysis Glycogenolysis, Proteolysis Tissue uptake of glucose is inhibited Hyperglycemia Urinary ketones, Ketonemia Acidosis
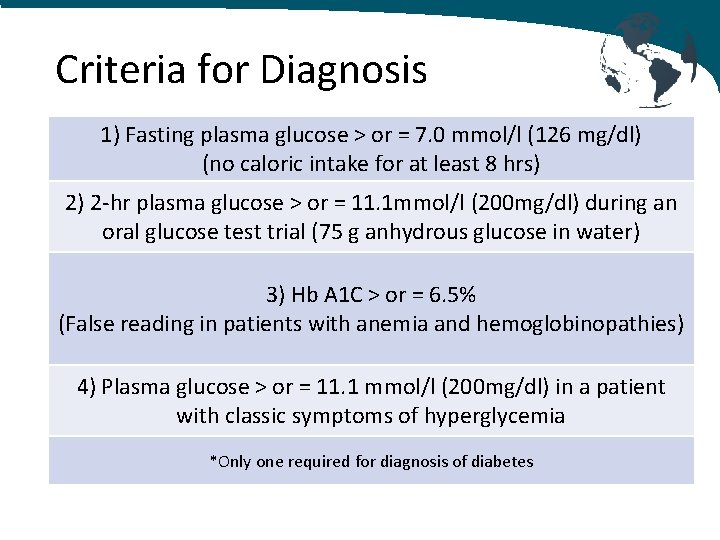
Criteria for Diagnosis 1) Fasting plasma glucose > or = 7. 0 mmol/l (126 mg/dl) (no caloric intake for at least 8 hrs) 2) 2 -hr plasma glucose > or = 11. 1 mmol/l (200 mg/dl) during an oral glucose test trial (75 g anhydrous glucose in water) 3) Hb A 1 C > or = 6. 5% (False reading in patients with anemia and hemoglobinopathies) 4) Plasma glucose > or = 11. 1 mmol/l (200 mg/dl) in a patient with classic symptoms of hyperglycemia *Only one required for diagnosis of diabetes
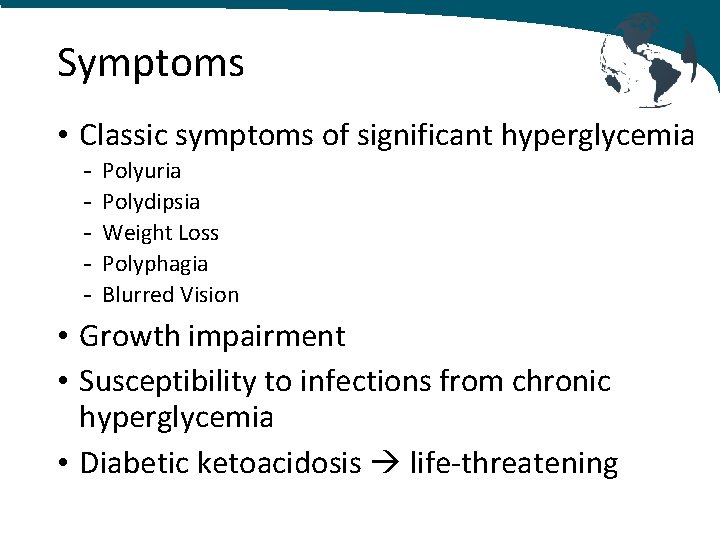
Symptoms • Classic symptoms of significant hyperglycemia - Polyuria Polydipsia Weight Loss Polyphagia Blurred Vision • Growth impairment • Susceptibility to infections from chronic hyperglycemia • Diabetic ketoacidosis life-threatening

Type 1 diabetes (IDDM) • Autoimmune disease • IDDM must be considered in any pediatric patient who continues to urinate regularly despite clinical dehydration • Patients require insulin for normal growth and development in puberty • Normal goal of fasting blood glucose: 4 -6 mmol/L (70 -110 mg/d. L) • Types of insulin: - Prandial insulin given around meals - Basal insulin once or twice daily - Premixed insulin biphasic insulin that includes prandial and basal
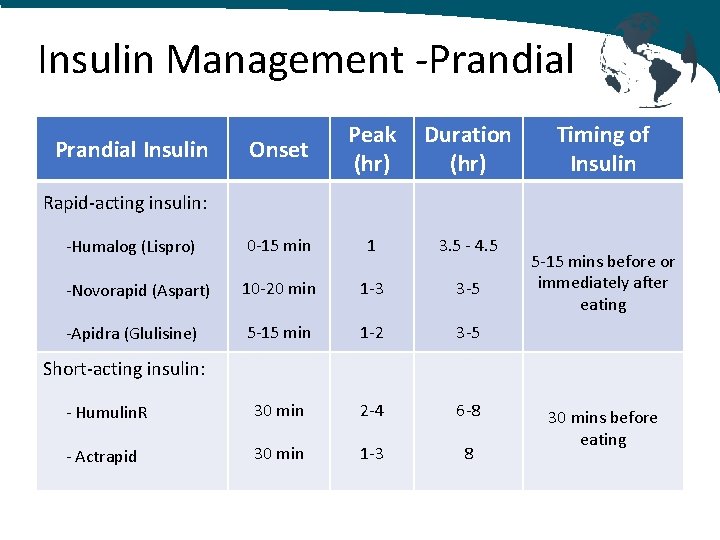
Insulin Management -Prandial Onset Peak (hr) Duration (hr) -Humalog (Lispro) 0 -15 min 1 3. 5 - 4. 5 -Novorapid (Aspart) 10 -20 min 1 -3 3 -5 -Apidra (Glulisine) 5 -15 min 1 -2 3 -5 - Humulin. R 30 min 2 -4 6 -8 - Actrapid 30 min 1 -3 8 Prandial Insulin Timing of Insulin Rapid-acting insulin: 5 -15 mins before or immediately after eating Short-acting insulin: 30 mins before eating
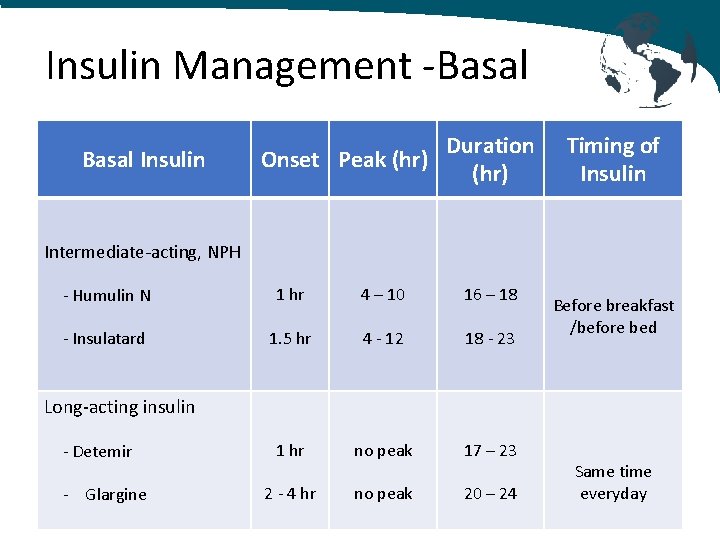
Insulin Management -Basal Insulin Onset Peak (hr) Duration (hr) Timing of Insulin Intermediate-acting, NPH - Humulin N 1 hr 4 – 10 16 – 18 - Insulatard 1. 5 hr 4 - 12 18 - 23 1 hr no peak 17 – 23 2 - 4 hr no peak 20 – 24 Before breakfast /before bed Long-acting insulin - Detemir - Glargine Same time everyday
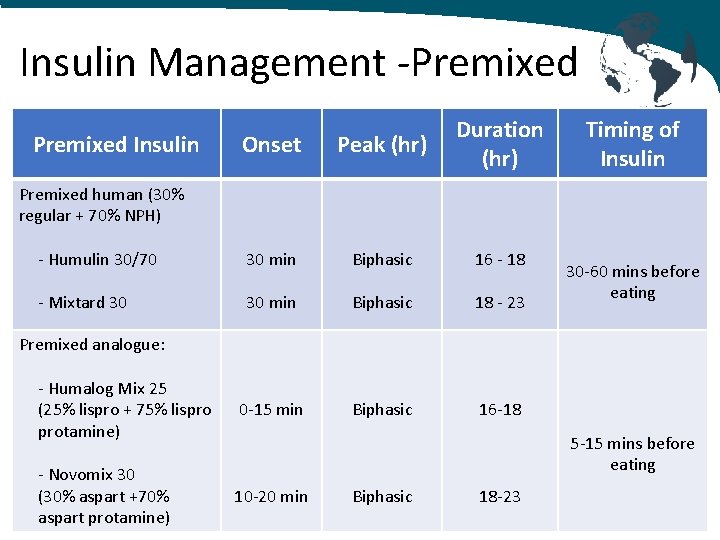
Insulin Management -Premixed Onset Peak (hr) Duration (hr) - Humulin 30/70 30 min Biphasic 16 - 18 - Mixtard 30 30 min Biphasic 18 - 23 - Humalog Mix 25 (25% lispro + 75% lispro protamine) 0 -15 min Biphasic 16 -18 - Novomix 30 (30% aspart +70% aspart protamine) 10 -20 min Premixed Insulin Timing of Insulin Premixed human (30% regular + 70% NPH) 30 -60 mins before eating Premixed analogue: 5 -15 mins before eating Biphasic 18 -23
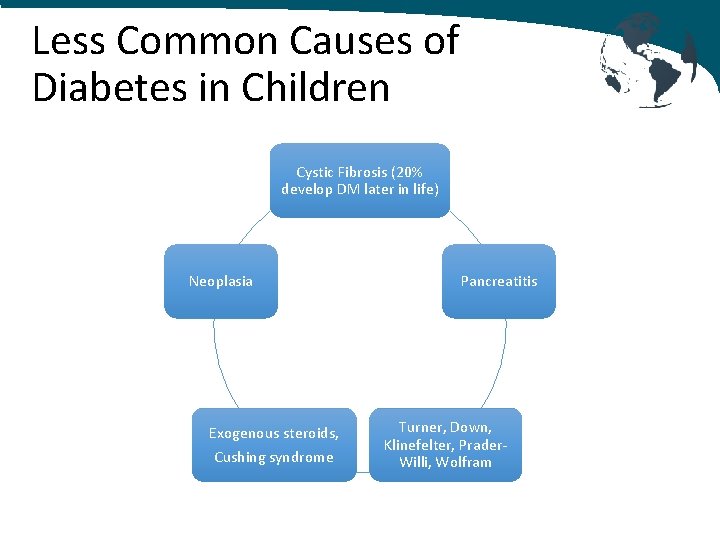
Less Common Causes of Diabetes in Children Cystic Fibrosis (20% develop DM later in life) Neoplasia Exogenous steroids, Cushing syndrome Pancreatitis Turner, Down, Klinefelter, Prader. Willi, Wolfram
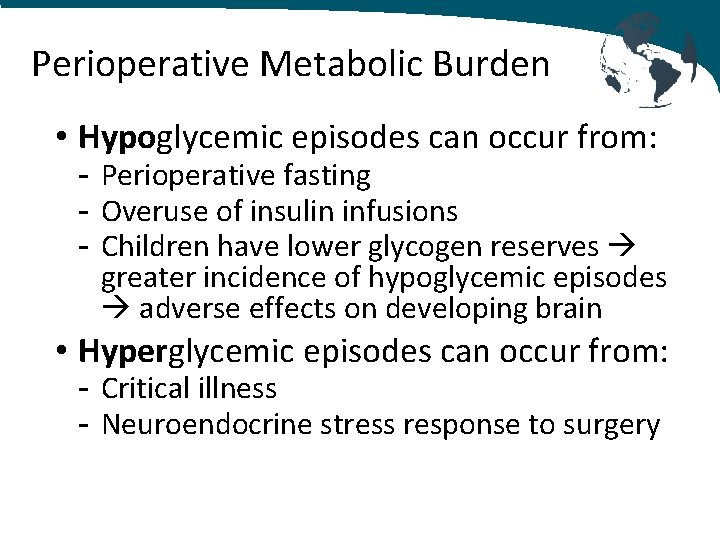
Perioperative Metabolic Burden • Hypoglycemic episodes can occur from: - Perioperative fasting - Overuse of insulin infusions - Children have lower glycogen reserves greater incidence of hypoglycemic episodes adverse effects on developing brain • Hyperglycemic episodes can occur from: - Critical illness - Neuroendocrine stress response to surgery
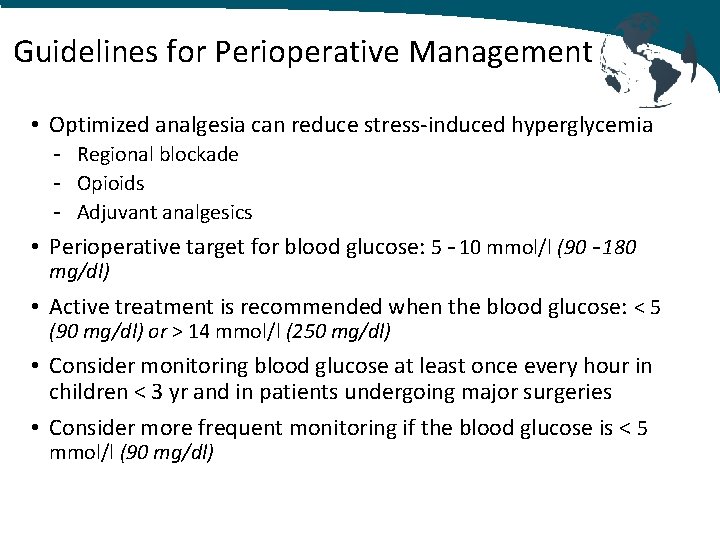
Guidelines for Perioperative Management • Optimized analgesia can reduce stress-induced hyperglycemia - Regional blockade - Opioids - Adjuvant analgesics • Perioperative target for blood glucose: 5 – 10 mmol/l (90 – 180 mg/dl) • Active treatment is recommended when the blood glucose: < 5 (90 mg/dl) or > 14 mmol/l (250 mg/dl) • Consider monitoring blood glucose at least once every hour in children < 3 yr and in patients undergoing major surgeries • Consider more frequent monitoring if the blood glucose is < 5 mmol/l (90 mg/dl)
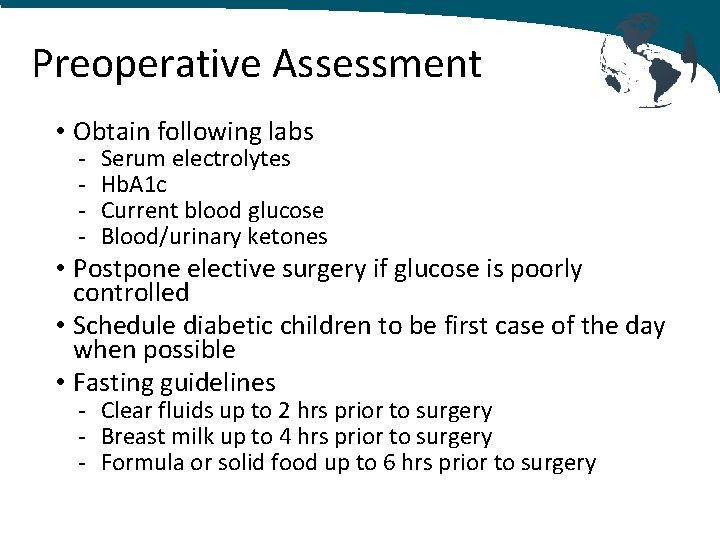
Preoperative Assessment • Obtain following labs - Serum electrolytes Hb. A 1 c Current blood glucose Blood/urinary ketones • Postpone elective surgery if glucose is poorly controlled • Schedule diabetic children to be first case of the day when possible • Fasting guidelines - Clear fluids up to 2 hrs prior to surgery - Breast milk up to 4 hrs prior to surgery - Formula or solid food up to 6 hrs prior to surgery
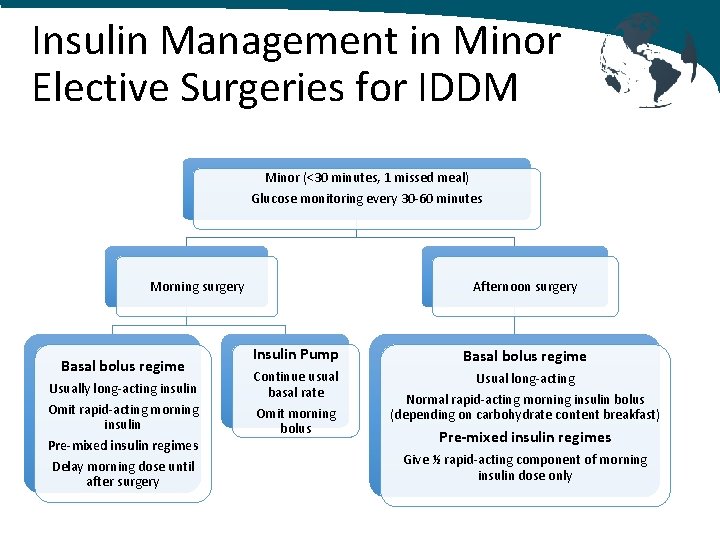
Insulin Management in Minor Elective Surgeries for IDDM Minor (<30 minutes, 1 missed meal) Glucose monitoring every 30 -60 minutes Morning surgery Basal bolus regime Usually long-acting insulin Omit rapid-acting morning insulin Pre-mixed insulin regimes Delay morning dose until after surgery Afternoon surgery Insulin Pump Basal bolus regime Continue usual basal rate Usual long-acting Omit morning bolus Normal rapid-acting morning insulin bolus (depending on carbohydrate content breakfast) Pre-mixed insulin regimes Give ½ rapid-acting component of morning insulin dose only
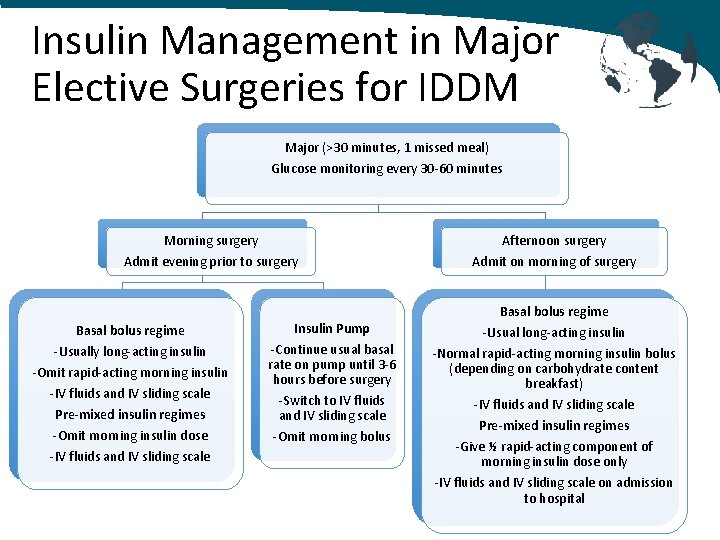
Insulin Management in Major Elective Surgeries for IDDM Major (>30 minutes, 1 missed meal) Glucose monitoring every 30 -60 minutes Morning surgery Afternoon surgery Admit evening prior to surgery Admit on morning of surgery Basal bolus regime -Usually long-acting insulin -Omit rapid-acting morning insulin -IV fluids and IV sliding scale Pre-mixed insulin regimes -Omit morning insulin dose -IV fluids and IV sliding scale Insulin Pump -Continue usual basal rate on pump until 3 -6 hours before surgery -Switch to IV fluids and IV sliding scale -Omit morning bolus Basal bolus regime -Usual long-acting insulin -Normal rapid-acting morning insulin bolus (depending on carbohydrate content breakfast) -IV fluids and IV sliding scale Pre-mixed insulin regimes -Give ½ rapid-acting component of morning insulin dose only -IV fluids and IV sliding scale on admission to hospital
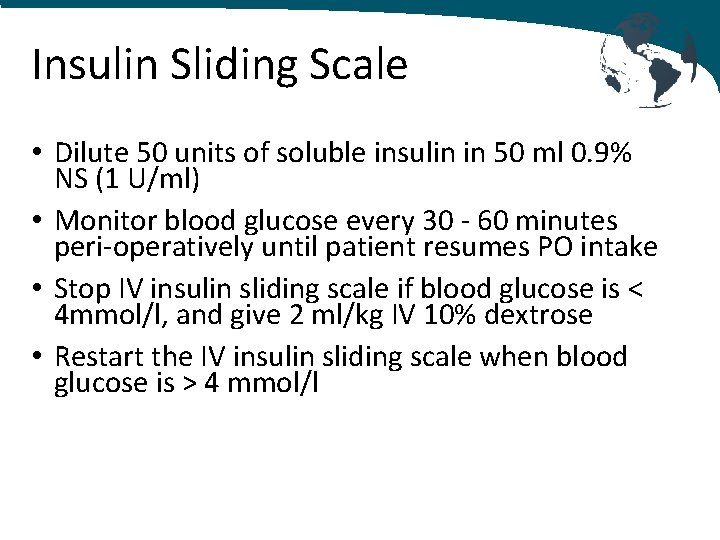
Insulin Sliding Scale • Dilute 50 units of soluble insulin in 50 ml 0. 9% NS (1 U/ml) • Monitor blood glucose every 30 - 60 minutes peri-operatively until patient resumes PO intake • Stop IV insulin sliding scale if blood glucose is < 4 mmol/l, and give 2 ml/kg IV 10% dextrose • Restart the IV insulin sliding scale when blood glucose is > 4 mmol/l
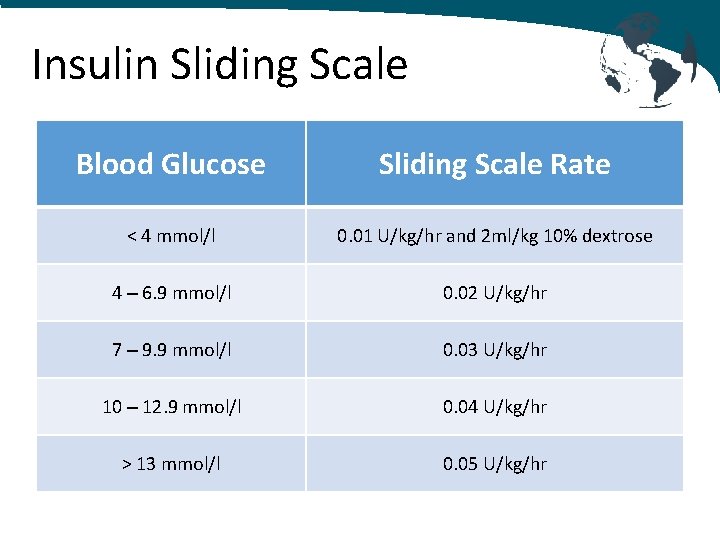
Insulin Sliding Scale Blood Glucose Sliding Scale Rate < 4 mmol/l 0. 01 U/kg/hr and 2 ml/kg 10% dextrose 4 – 6. 9 mmol/l 0. 02 U/kg/hr 7 – 9. 9 mmol/l 0. 03 U/kg/hr 10 – 12. 9 mmol/l 0. 04 U/kg/hr > 13 mmol/l 0. 05 U/kg/hr
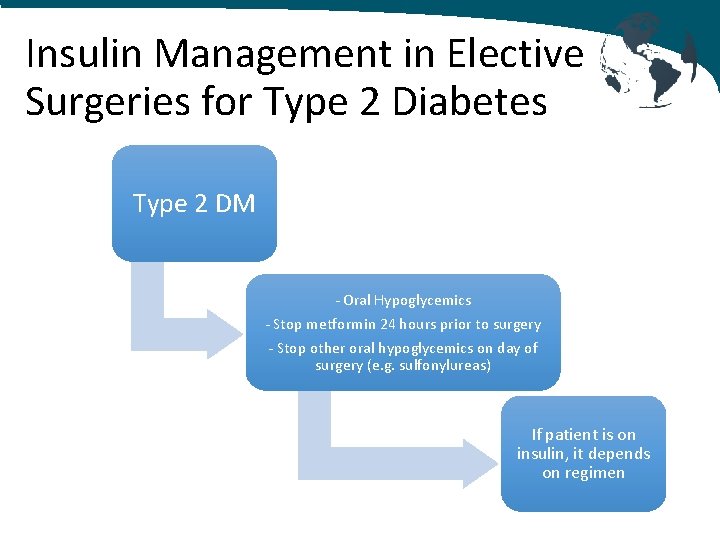
Insulin Management in Elective Surgeries for Type 2 Diabetes Type 2 DM - Oral Hypoglycemics - Stop metformin 24 hours prior to surgery - Stop other oral hypoglycemics on day of surgery (e. g. sulfonylureas) If patient is on insulin, it depends on regimen
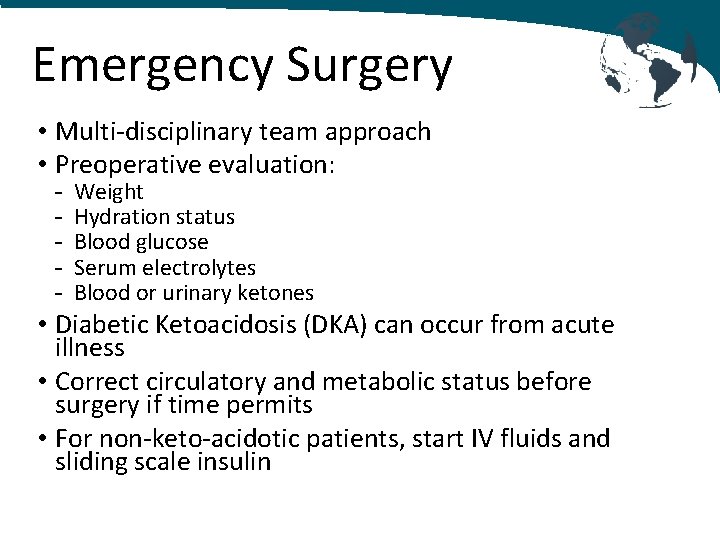
Emergency Surgery • Multi-disciplinary team approach • Preoperative evaluation: - Weight Hydration status Blood glucose Serum electrolytes Blood or urinary ketones • Diabetic Ketoacidosis (DKA) can occur from acute illness • Correct circulatory and metabolic status before surgery if time permits • For non-keto-acidotic patients, start IV fluids and sliding scale insulin
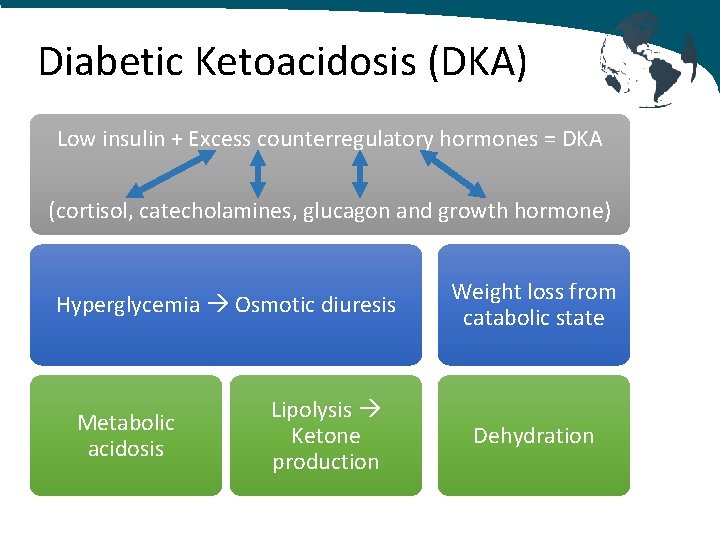
Diabetic Ketoacidosis (DKA) Low insulin + Excess counterregulatory hormones = DKA (cortisol, catecholamines, glucagon and growth hormone) Hyperglycemia Osmotic diuresis Metabolic acidosis Lipolysis Ketone production Weight loss from catabolic state Dehydration
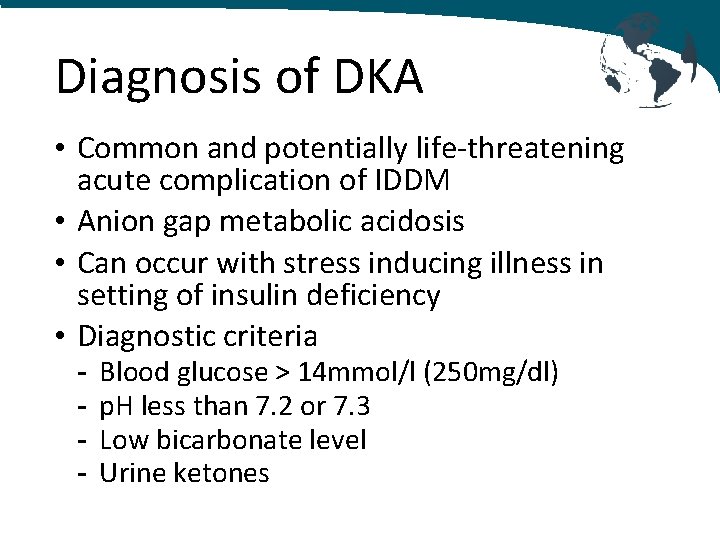
Diagnosis of DKA • Common and potentially life-threatening acute complication of IDDM • Anion gap metabolic acidosis • Can occur with stress inducing illness in setting of insulin deficiency • Diagnostic criteria - Blood glucose > 14 mmol/l (250 mg/dl) p. H less than 7. 2 or 7. 3 Low bicarbonate level Urine ketones
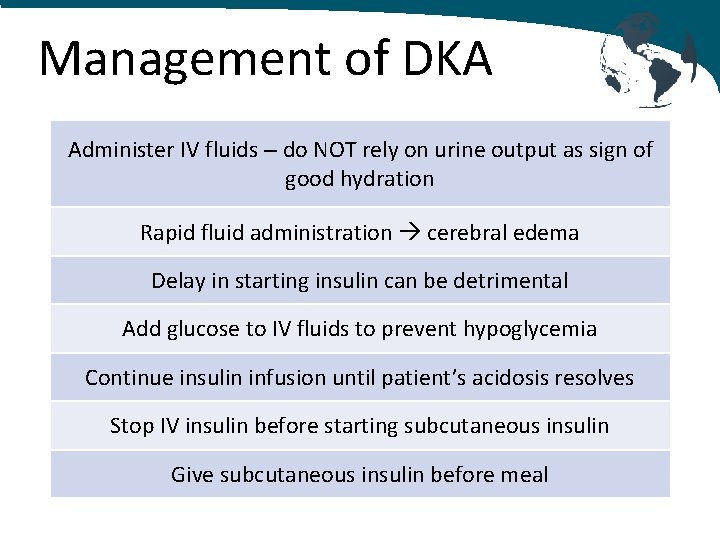
Management of DKA Administer IV fluids – do NOT rely on urine output as sign of good hydration Rapid fluid administration cerebral edema Delay in starting insulin can be detrimental Add glucose to IV fluids to prevent hypoglycemia Continue insulin infusion until patient’s acidosis resolves Stop IV insulin before starting subcutaneous insulin Give subcutaneous insulin before meal
Conclusions: • DM is the most prevalent metabolic disorder in pediatric patients • Insulin-dependent diabetes mellitus requires close perioperative blood glucose monitoring • Multidisciplinary team approach is optimal • Resume normal oral intake and diabetes management as soon as possible postoperatively • DKA treatment involves insulin, IV fluid and electrolyte replacement (carefully monitor potassium) • Challenges in LMICs include adequate refrigeration for insulin and availability of glucose monitors
References: 1. 2. 3. 4. 5. 6. 7. 8. Tjen, C. , Wilkinson, K. Perioperative care of children and young people with diabetes. British Journal of Anaesthesia. 2016; 16(4): 124 -129. Lewis, H. Perioperative management of infants and children with diabetes. WFSA Anaesthesia Tutorial of the Week. (Tutorial 402). 16 April 2019. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetic Care. 2010; 33: S 62 -S 69. Plotnick, L. Insulin-dependent Diabetes Mellitus. Pediatrics in Review. 1994; 15: 137 -148. Fasting recommendations for patients with insulin-dependent diabetes. Medscape. Feb 15, 2017 Suzuki, et al. Glycemic control indicator levels at diagnosis of neonatal diabetes mellitus: Comparison with other types of insulin-dependent diabetes mellitus. Pediatric Diabetes. 2017; 18: 767 -771. Zanaria, H. , et al. Practical guide to insulin therapy in type 2 diabetes. Guidebook from Malaysian Ministry of Health. 2011. Lanzinger, S. , et al. Comparing clinical characteristics of pediatric patients with pancreatic diabetes to patients with type 1 diabetes: A matched case-control study. Pediatric Diabetes. 2019; 20: 955 -963.
- Slides: 28