Insulin Therapy In Type 1 DM H Delshad




- Slides: 79

Insulin Therapy In Type 1 DM H. Delshad M. D Endocrinologist Research Institute For Endocrine Sciences
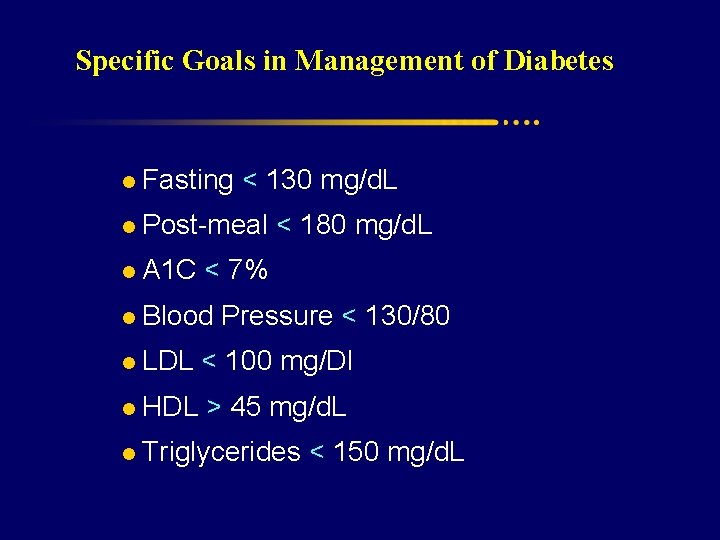
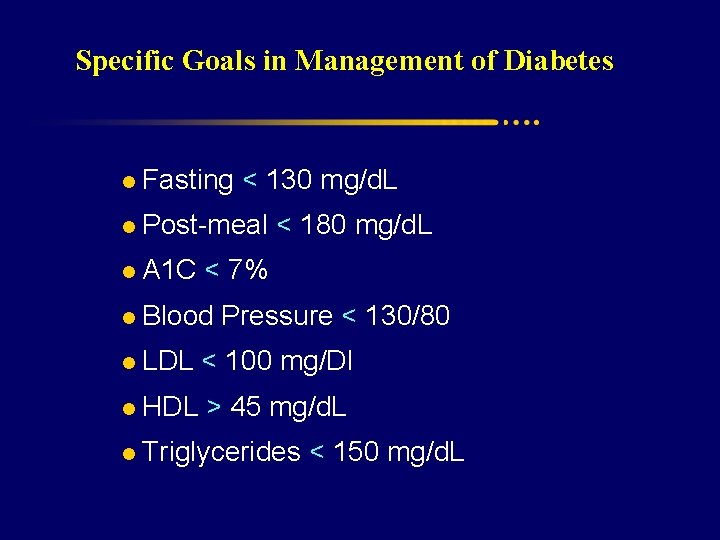
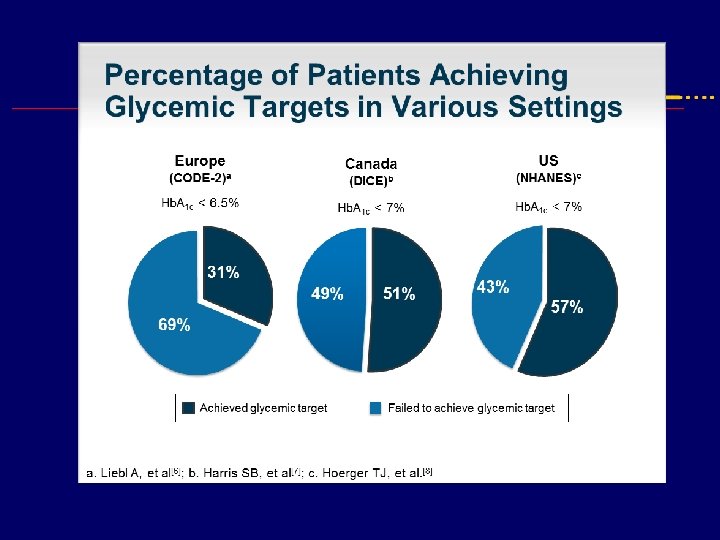
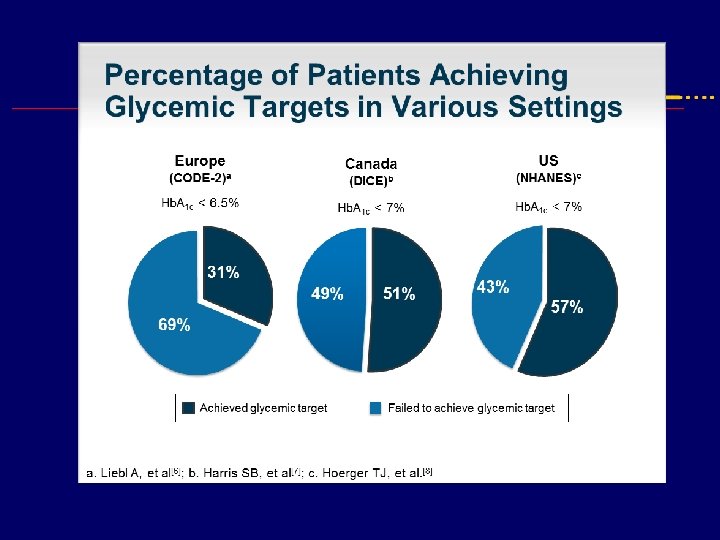
Specific Goals in Management of Diabetes l Fasting < 130 mg/d. L l Post-meal < 180 mg/d. L l A 1 C < 7% l Blood Pressure < 130/80 l LDL < 100 mg/Dl l HDL > 45 mg/d. L l Triglycerides < 150 mg/d. L
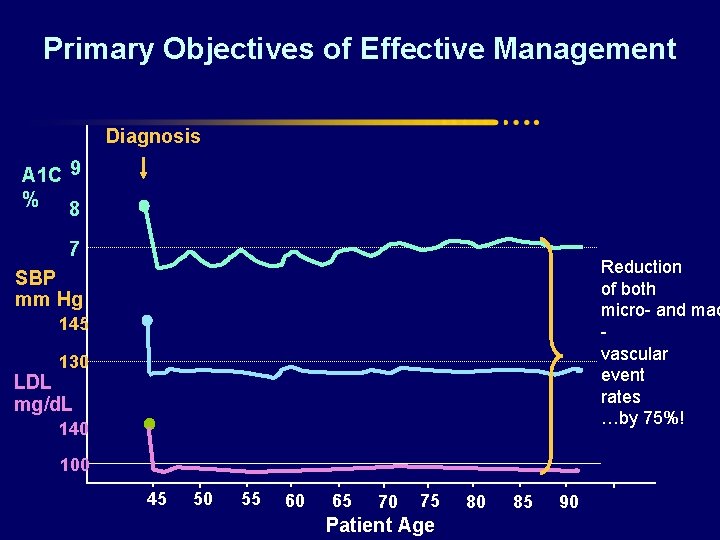
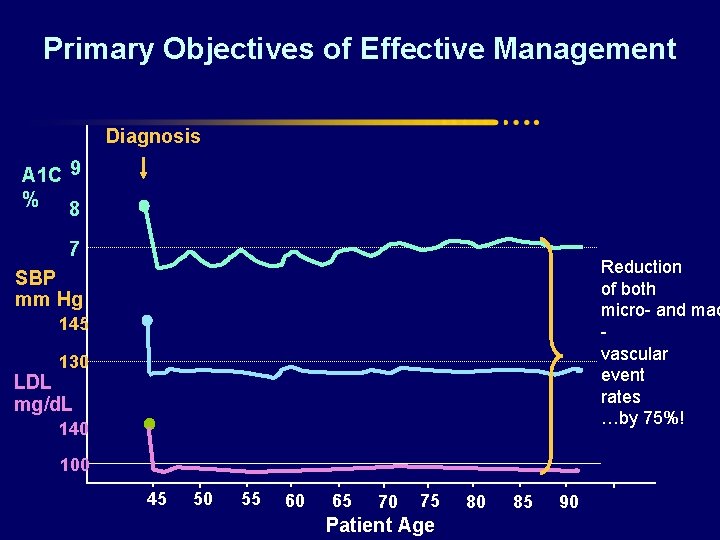
Primary Objectives of Effective Management Diagnosis A 1 C 9 % 8 7 Reduction of both micro- and mac vascular event rates …by 75%! SBP mm Hg 145 130 LDL mg/d. L 140 100 45 50 55 60 65 70 75 Patient Age 80 85 90
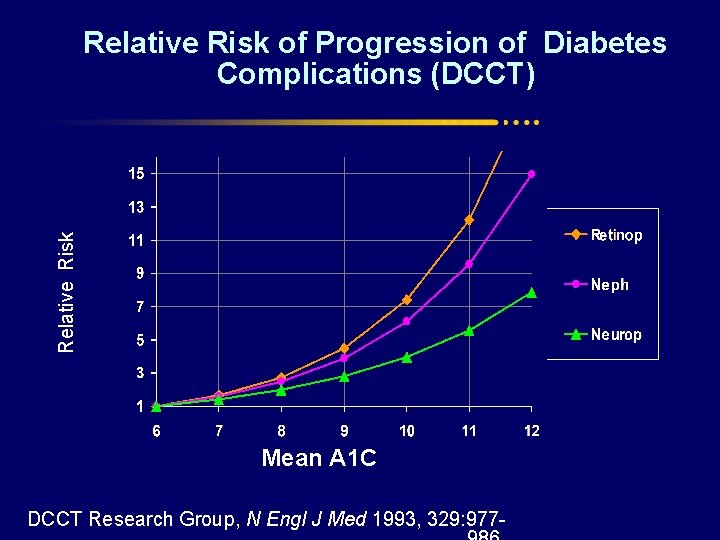
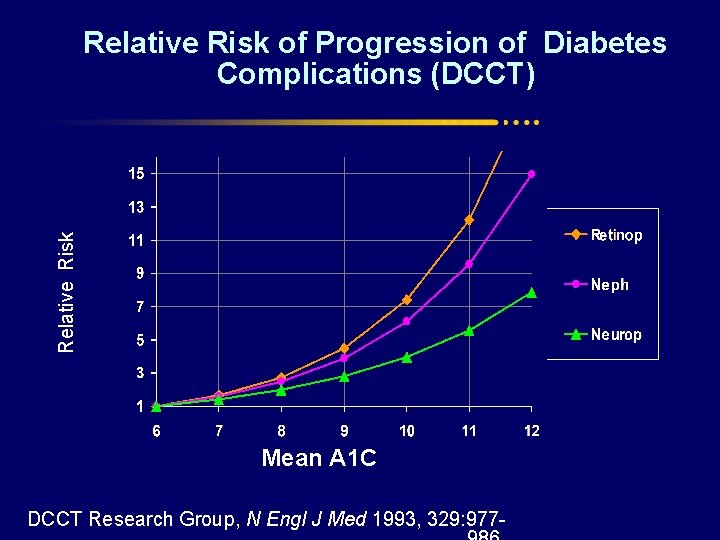
Relative Risk of Progression of Diabetes Complications (DCCT) Mean A 1 C DCCT Research Group, N Engl J Med 1993, 329: 977 -
Control your Diabetes well 7 Life is better under Seven < Hb. A 1 c
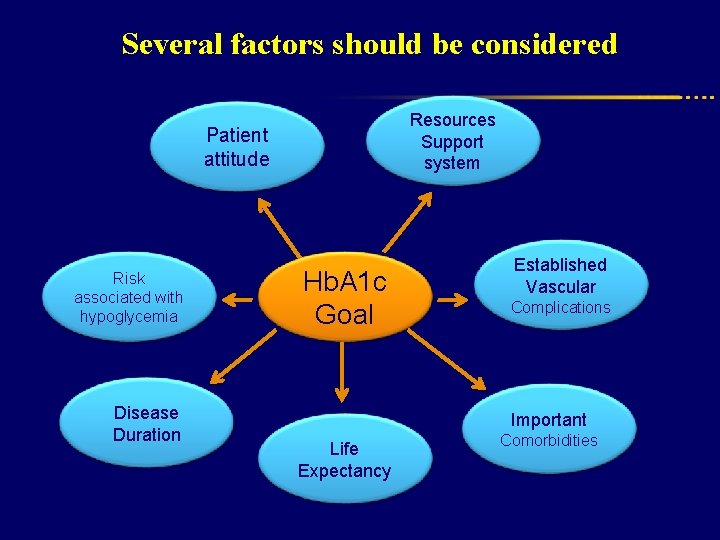
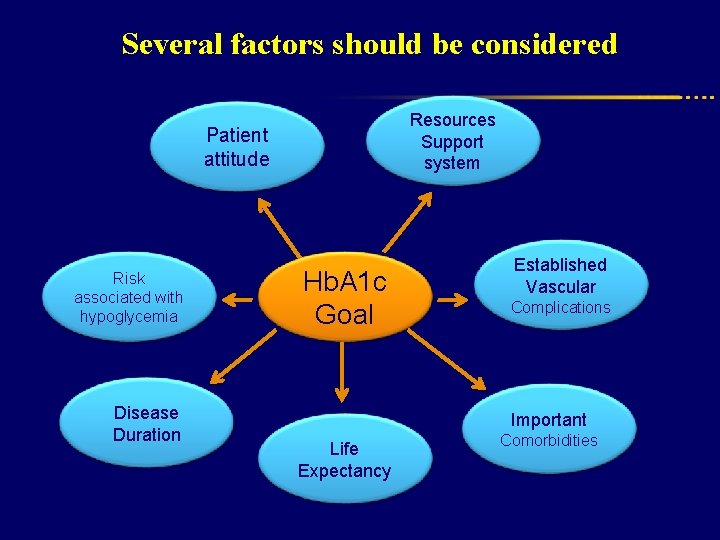
Several factors should be considered Resources Support system Patient attitude Risk associated with hypoglycemia Disease Duration Hb. A 1 c Goal Established Vascular Complications Important Life Expectancy Comorbidities
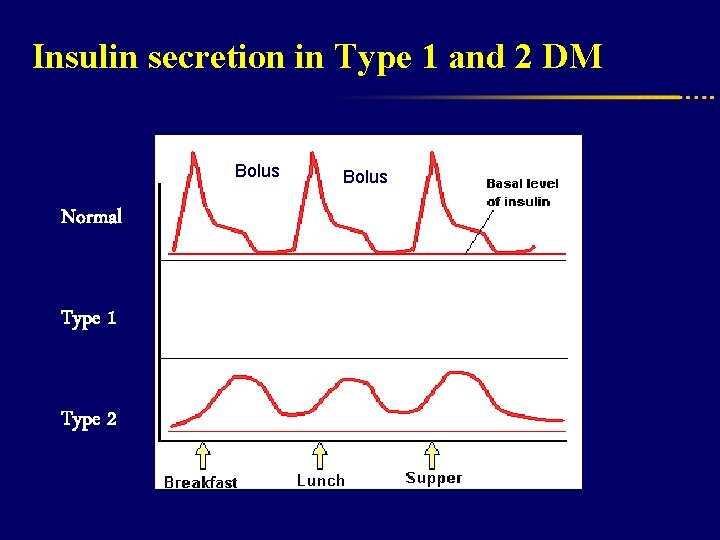
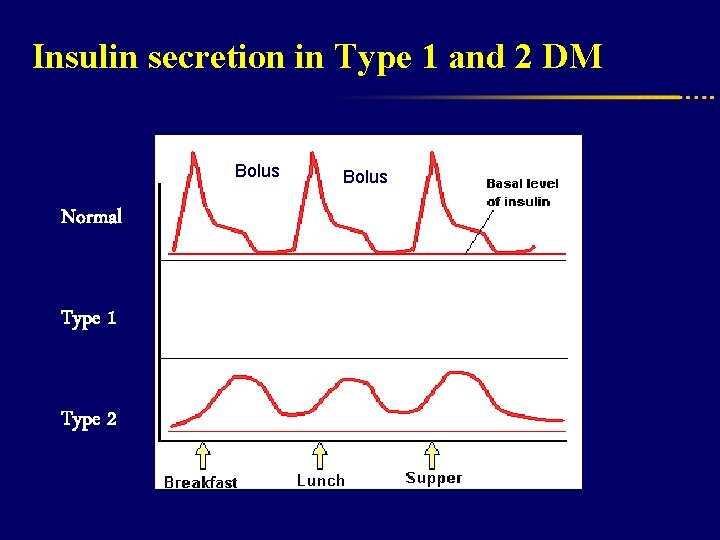
Insulin secretion in Type 1 and 2 DM Prandial Bolus Normal Type 1 Type 2 Bolus
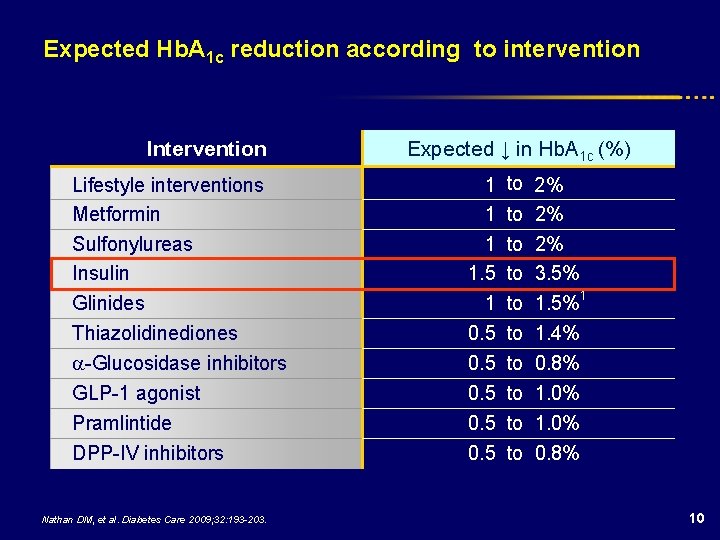
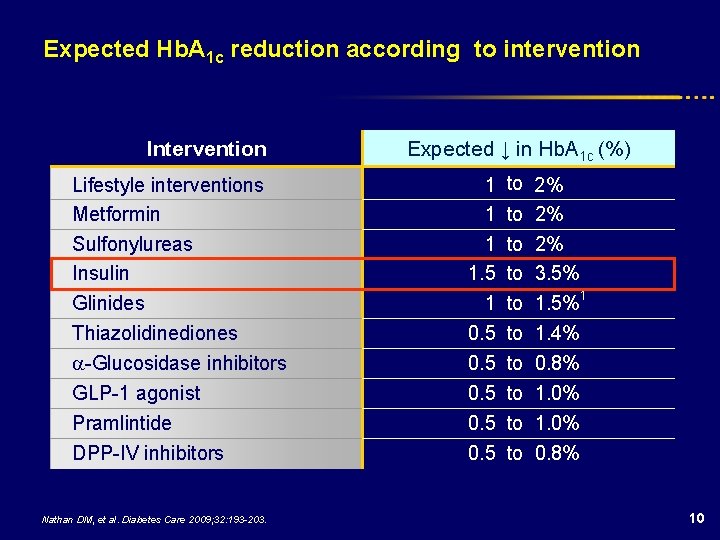
Expected Hb. A 1 c reduction according to intervention Intervention Lifestyle interventions Metformin Sulfonylureas Insulin Glinides Thiazolidinediones -Glucosidase inhibitors GLP-1 agonist Pramlintide DPP-IV inhibitors Nathan DM, et al. Diabetes Care 2009; 32: 193 -203. Expected ↓ in Hb. A 1 c (%) 1 to 1. 5 to 1 to 0. 5 to 2% 2% 2% 3. 5% 1. 5%1 1. 4% 0. 8% 1. 0% 0. 8% 10
INSULIN The most powerful agent we have to control glucose
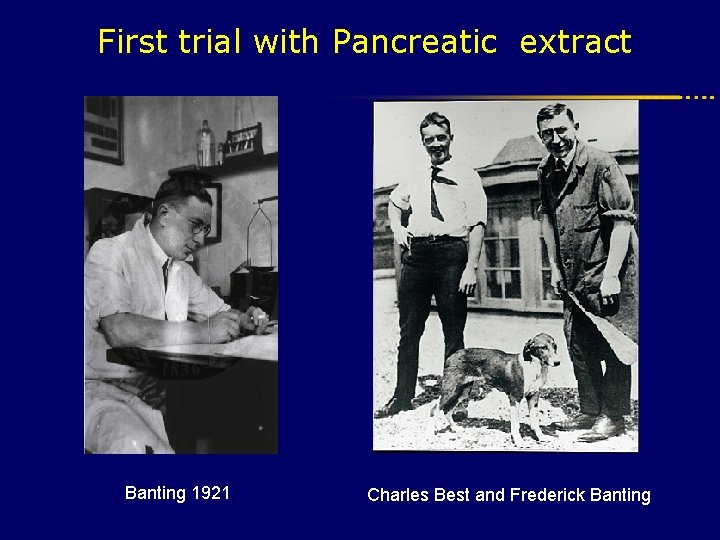
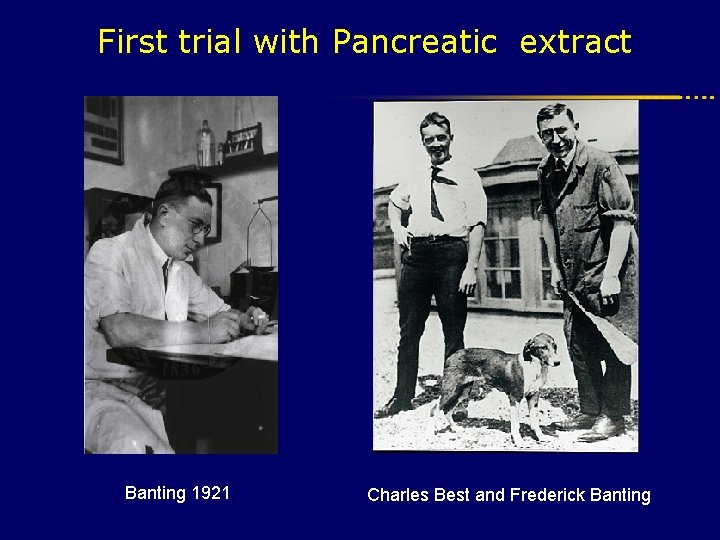
First trial with Pancreatic extract Banting 1921 Charles Best and Frederick Banting
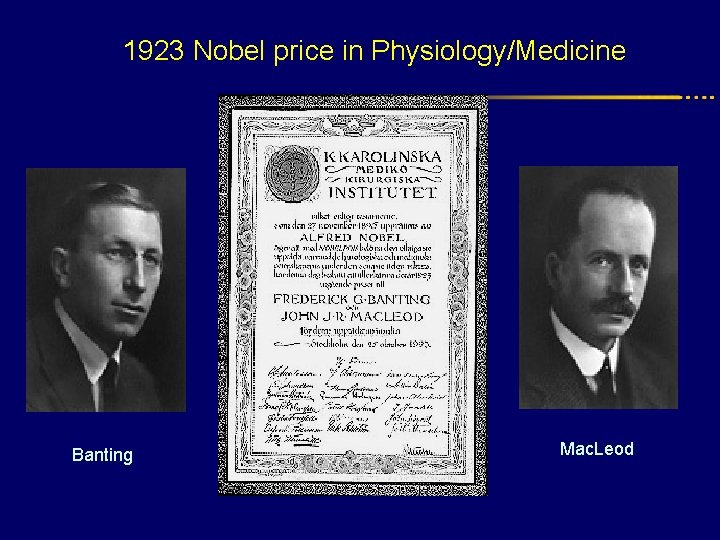
1923 Nobel price in Physiology/Medicine Banting Mac. Leod
Banting, s wedding day
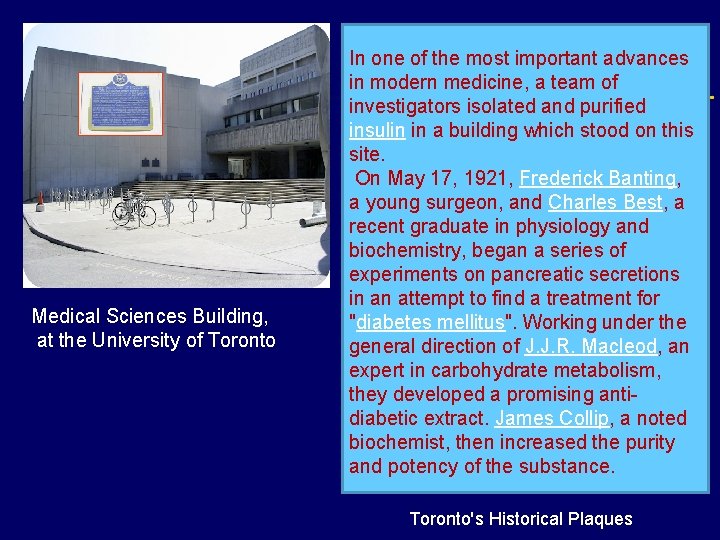
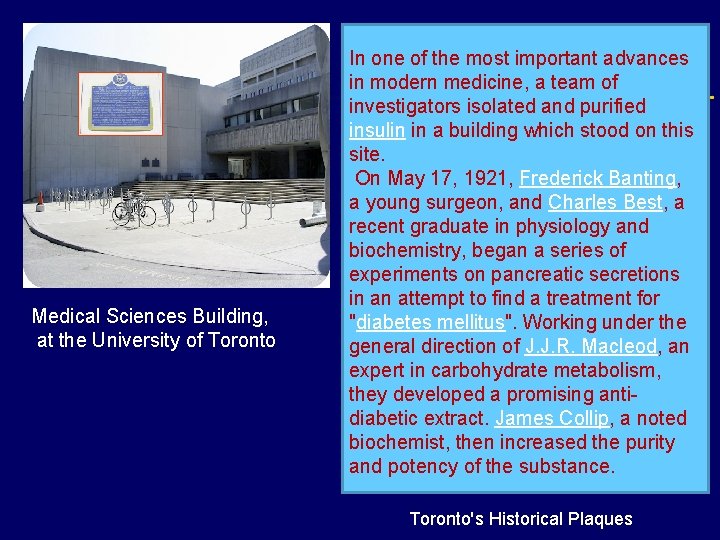
Medical Sciences Building, at the University of Toronto In one of the most important advances in modern medicine, a team of investigators isolated and purified insulin in a building which stood on this site. On May 17, 1921, Frederick Banting, a young surgeon, and Charles Best, a recent graduate in physiology and biochemistry, began a series of experiments on pancreatic secretions in an attempt to find a treatment for "diabetes mellitus". Working under the general direction of J. J. R. Macleod, an expert in carbohydrate metabolism, they developed a promising antidiabetic extract. James Collip, a noted biochemist, then increased the purity and potency of the substance. Toronto's Historical Plaques
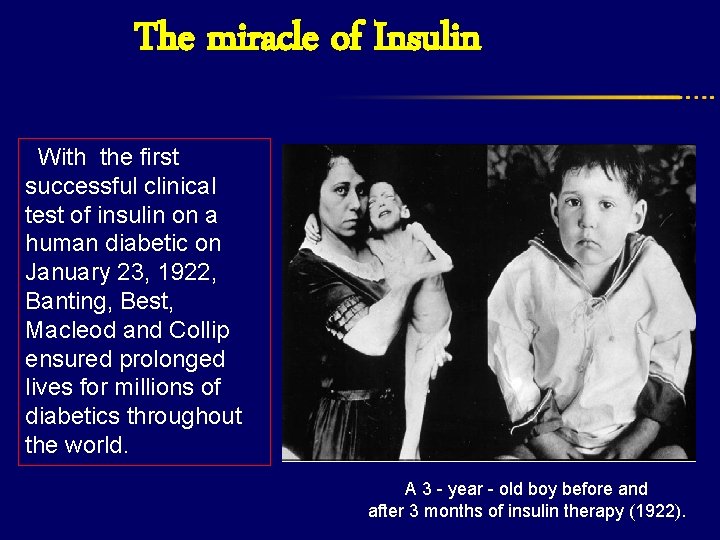
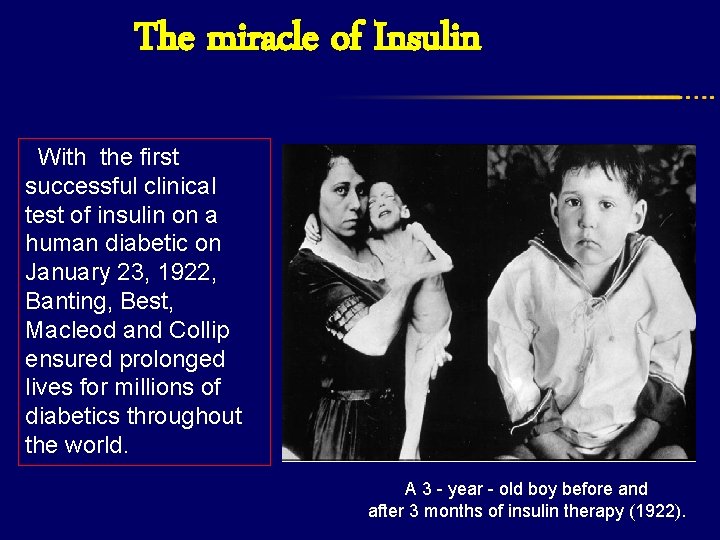
The miracle of Insulin With the first successful clinical test of insulin on a human diabetic on January 23, 1922, Banting, Best, Macleod and Collip ensured prolonged lives for millions of diabetics throughout the world. A 3 - year - old boy before and after 3 months of insulin therapy (1922).
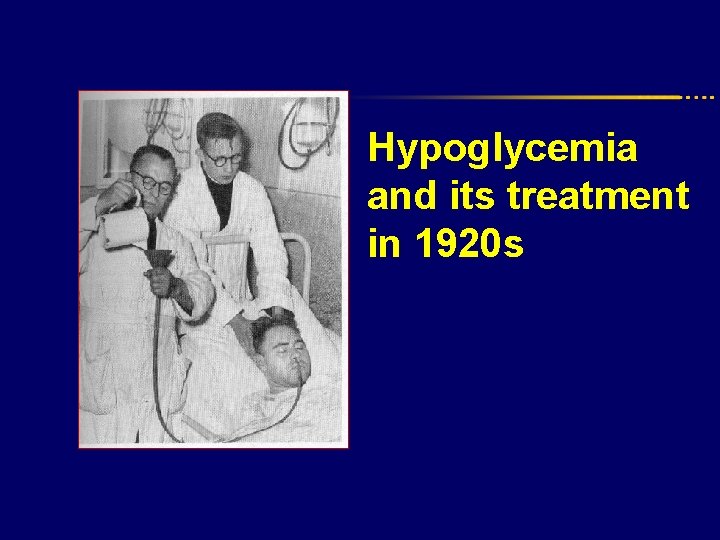
Hypoglycemia and its treatment in 1920 s
Characteristics of first commercial insulin l 1 U/ml l Acidic l Bovine origin l Impure l Only short acting Academia Request : Longer acting insulin
Longer acting insulin l 1930: Insulin plus adrenalin l 1934: Zinc insulin crystallisation l 1936: Protraction with Protamin Academia Requirement: Purity
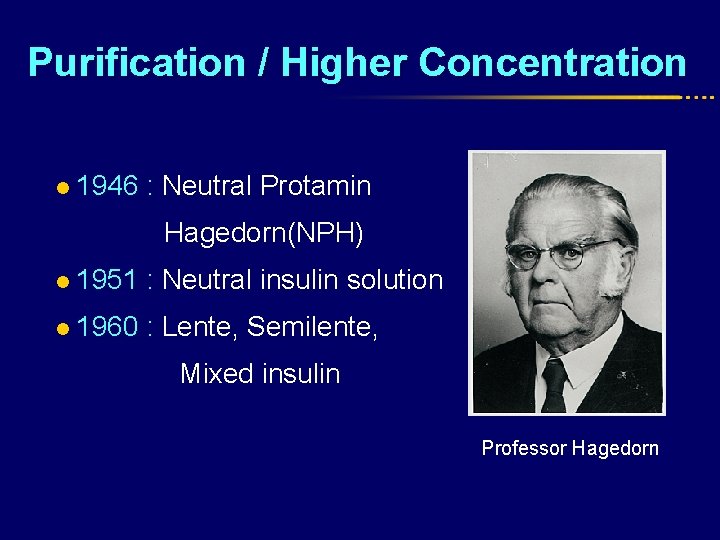
Purification / Higher Concentration l 1946 : Neutral Protamin Hagedorn(NPH) l 1951 : Neutral insulin solution l 1960 : Lente, Semilente, Mixed insulin Professor Hagedorn
NPH : Is the most important discovery for diabetes treatment since the discovery of insulin” P Joslin 1947
Gene technology– 1986 Transfer and cloning of the insulin gen 1990 Human insulin (Short- and long-acting and Mixed insulin )
- Academia Requirement : Simple Administration
1926 : The first pens

Diabetes care today
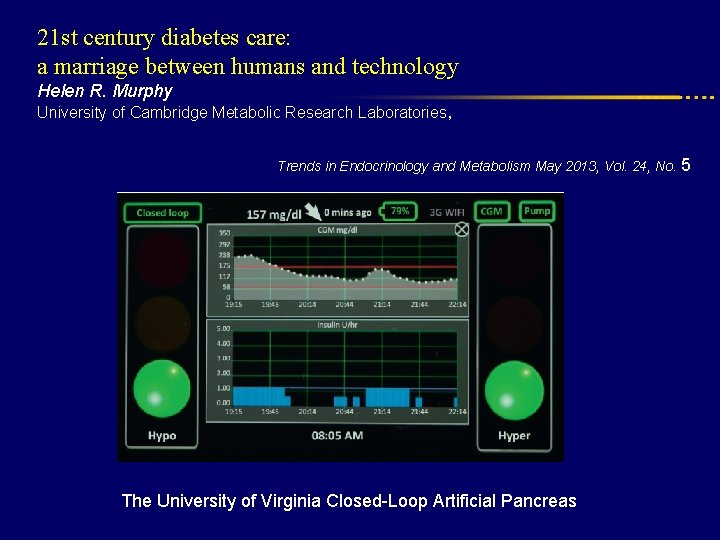
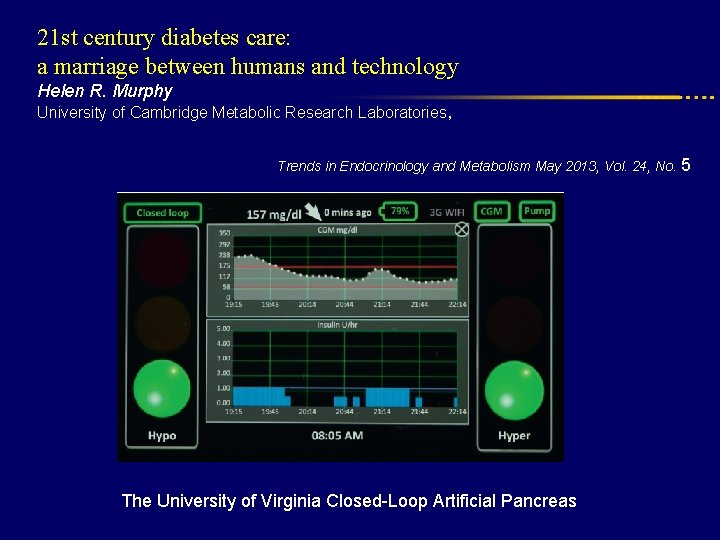
21 st century diabetes care: a marriage between humans and technology Helen R. Murphy University of Cambridge Metabolic Research Laboratories, Trends in Endocrinology and Metabolism May 2013, Vol. 24, No. 5 The University of Virginia Closed-Loop Artificial Pancreas
Types of Insulin Ø More than 20 types of insulin Ø Different time of onset and duration of action. Ø Among the criteria considered in choosing insulin are: ○ How soon it starts working (onset) ○ When it works the hardest (peak time) ○ How long it lasts in the body (duration)
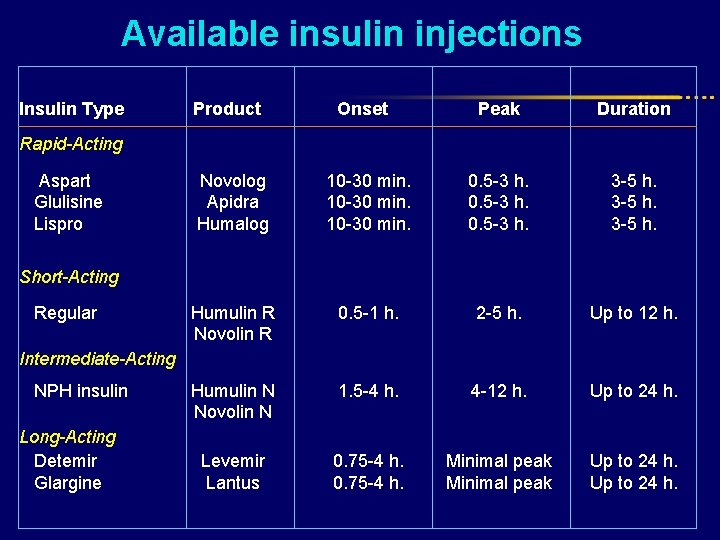
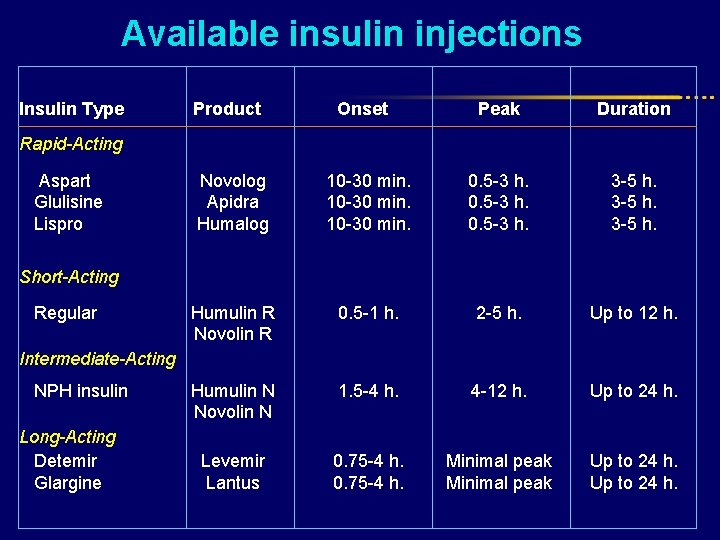
Available insulin injections Insulin Type Product Onset Peak Duration Novolog Apidra Humalog 10 -30 min. 0. 5 -3 h. 3 -5 h. Humulin R Novolin R 0. 5 -1 h. 2 -5 h. Up to 12 h. Humulin N Novolin N 1. 5 -4 h. 4 -12 h. Up to 24 h. Levemir Lantus 0. 75 -4 h. Minimal peak Up to 24 h. Rapid-Acting Aspart Glulisine Lispro Short-Acting Regular Intermediate-Acting NPH insulin Long-Acting Detemir Glargine
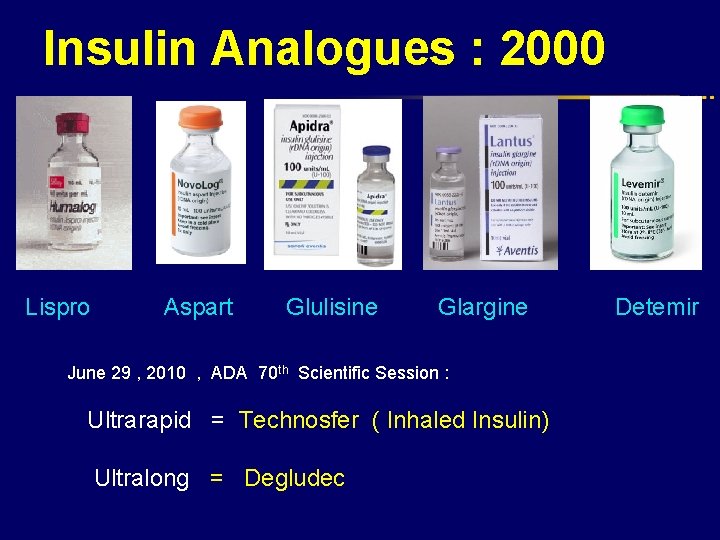
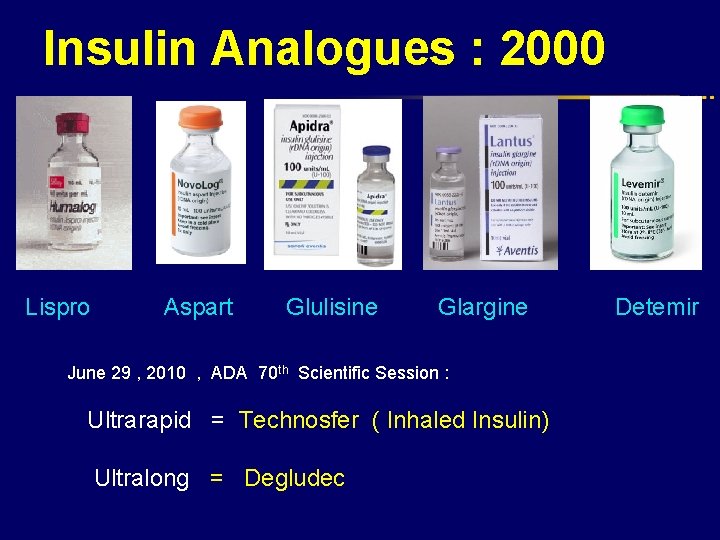
Insulin Analogues : 2000 Lispro Aspart Glulisine Glargine Detemir June 29 , 2010 , ADA 70 th Scientific Session : Ultrarapid = Technosfer ( Inhaled Insulin) Ultralong = Degludec
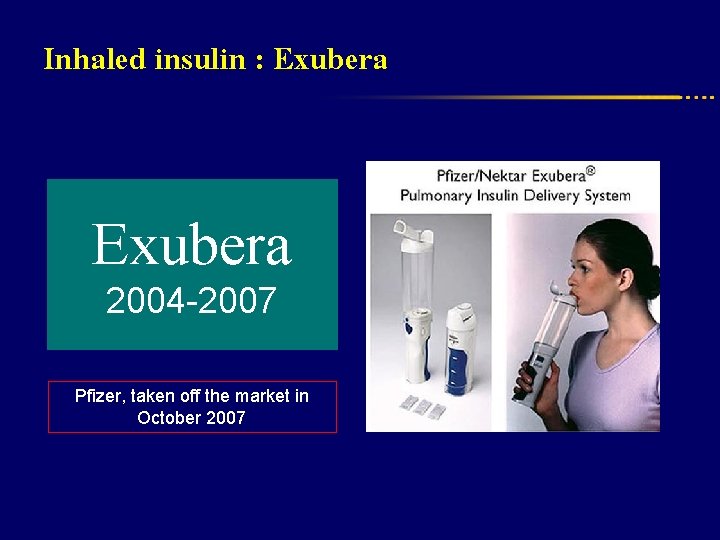
Inhaled insulin : Exubera 2004 -2007 Pfizer, taken off the market in October 2007
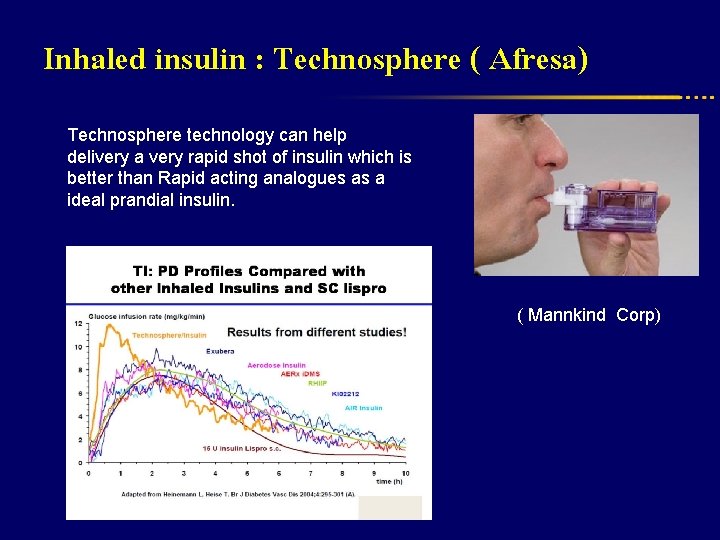
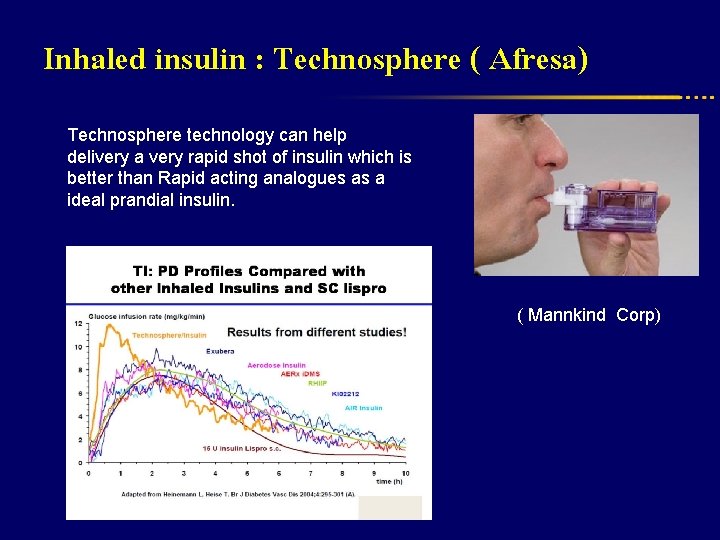
Inhaled insulin : Technosphere ( Afresa) Technosphere technology can help delivery a very rapid shot of insulin which is better than Rapid acting analogues as a ideal prandial insulin. ( Mannkind Corp)
Conventional Insulins l REGULAR : Traditional Bolus insulin since 1921 l NPH : Traditional Basal insulin replacement since 1950 l Several well known limitations : * Absorption Variation : unfavorable plasma profiles * Duration of acton * Peak effect * Fasting hyperglycemia * Nocturnal hypoglycemia
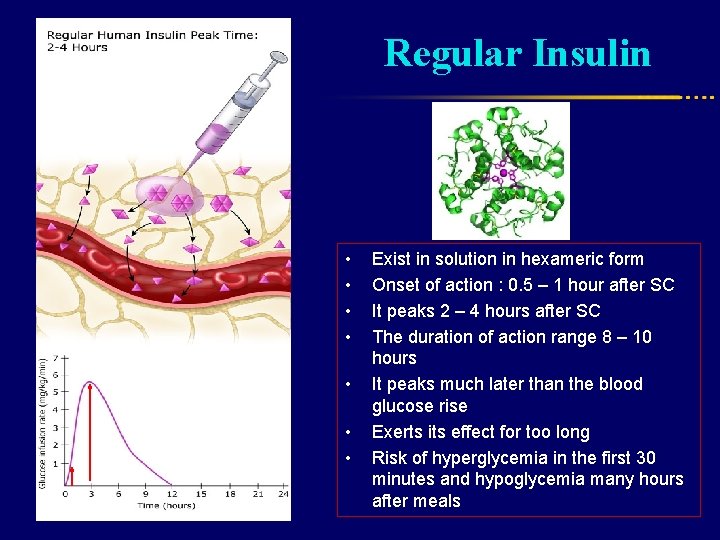
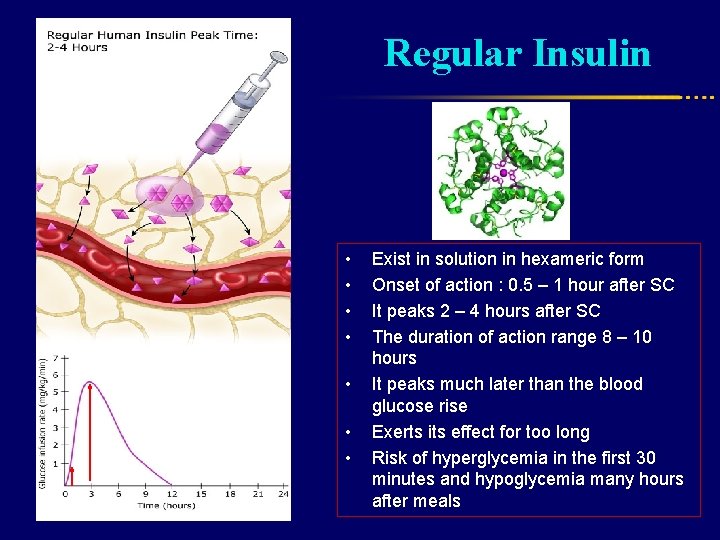
Regular Insulin • • Exist in solution in hexameric form Onset of action : 0. 5 – 1 hour after SC It peaks 2 – 4 hours after SC The duration of action range 8 – 10 hours It peaks much later than the blood glucose rise Exerts its effect for too long Risk of hyperglycemia in the first 30 minutes and hypoglycemia many hours after meals
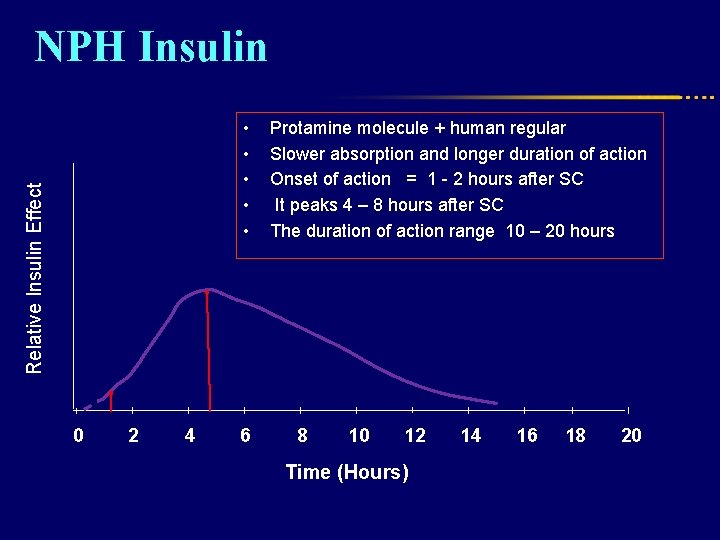
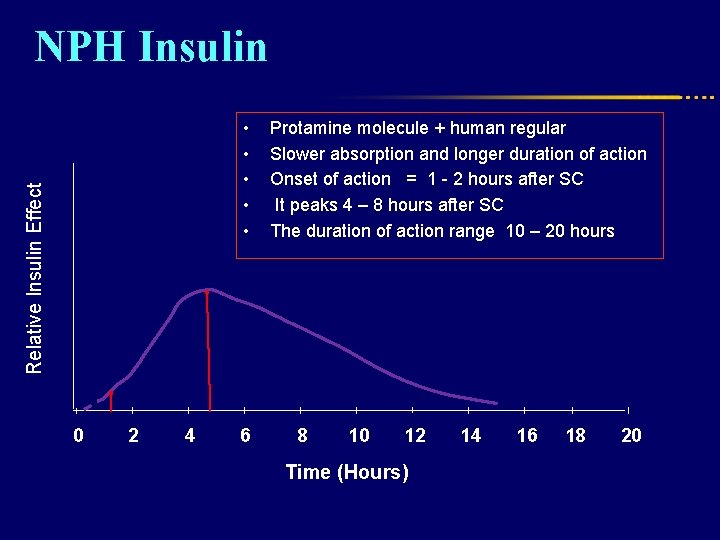
NPH Insulin Relative Insulin Effect • • • 0 2 4 6 Protamine molecule + human regular Slower absorption and longer duration of action Onset of action = 1 - 2 hours after SC It peaks 4 – 8 hours after SC The duration of action range 10 – 20 hours 8 10 12 Time (Hours) 14 16 18 20
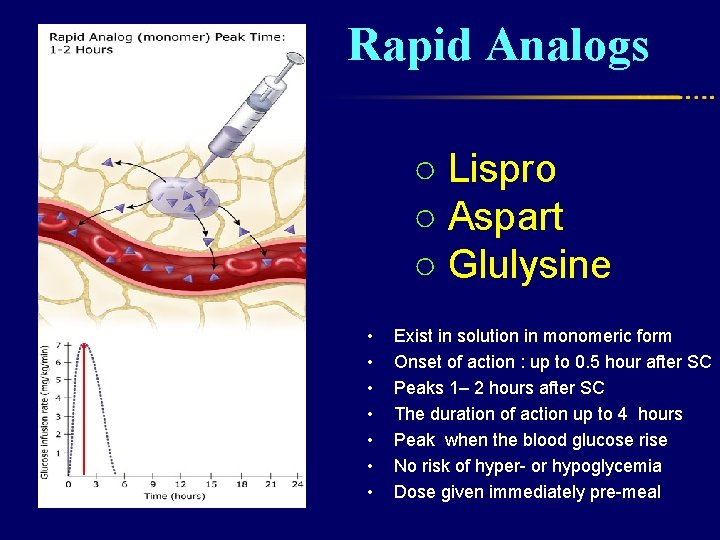
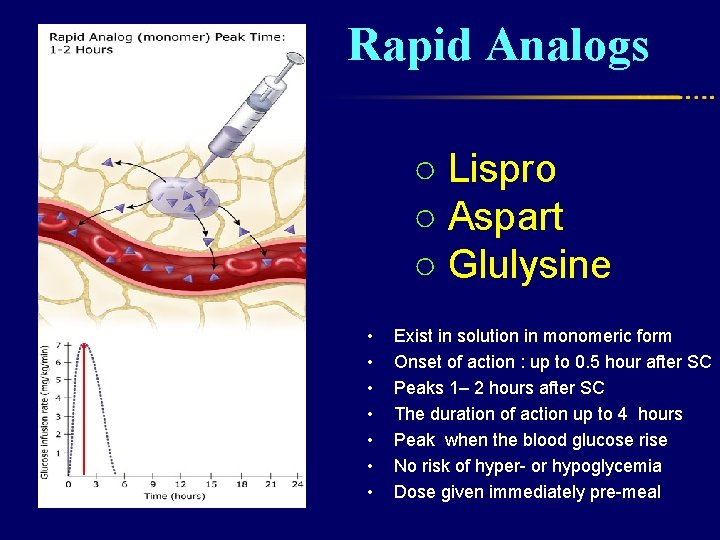
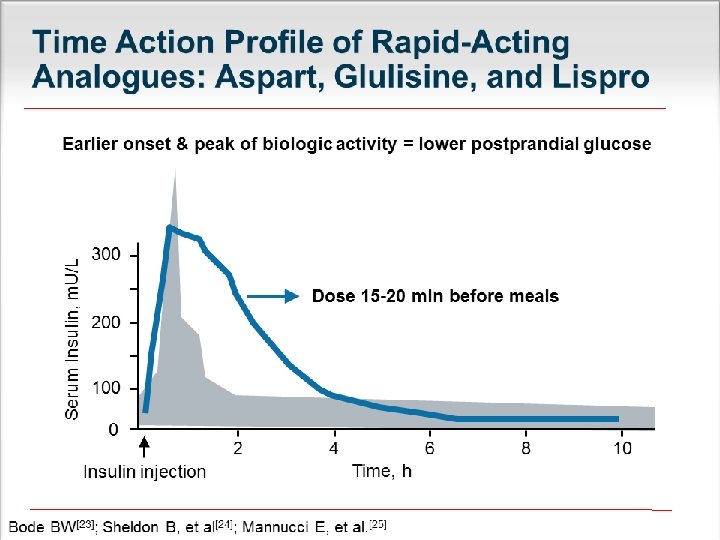
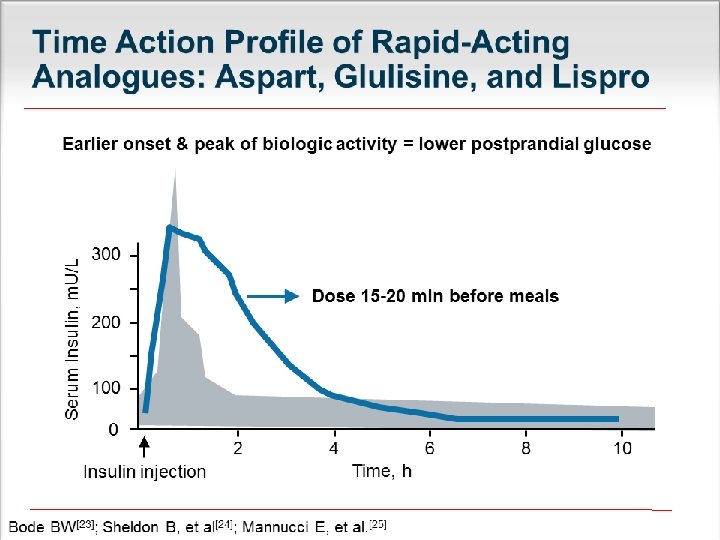
Rapid Analogs ○ Lispro ○ Aspart ○ Glulysine • • Exist in solution in monomeric form Onset of action : up to 0. 5 hour after SC Peaks 1– 2 hours after SC The duration of action up to 4 hours Peak when the blood glucose rise No risk of hyper- or hypoglycemia Dose given immediately pre-meal
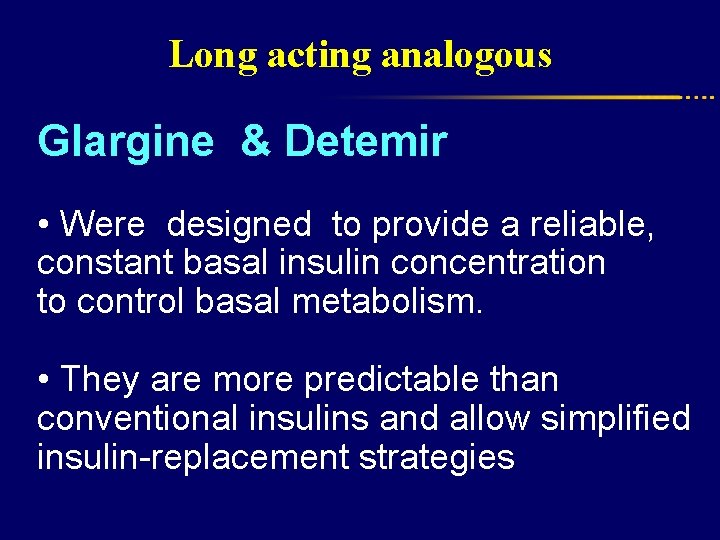
Long acting analogous Glargine & Detemir • Were designed to provide a reliable, constant basal insulin concentration to control basal metabolism. • They are more predictable than conventional insulins and allow simplified insulin-replacement strategies
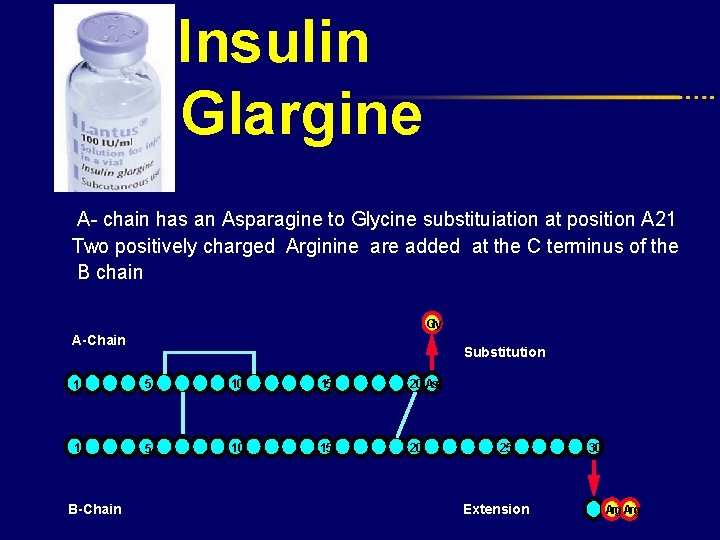
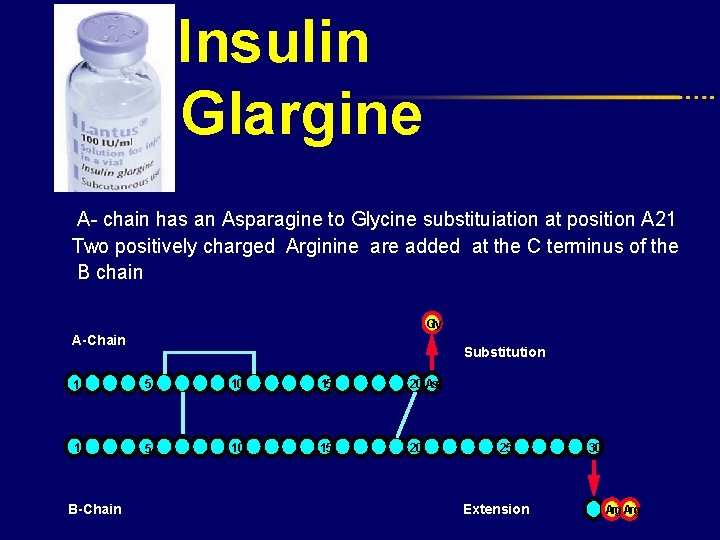
Insulin Glargine A- chain has an Asparagine to Glycine substituiation at position A 21 Two positively charged Arginine are added at the C terminus of the B chain Gly A-Chain Substitution 1 5 10 15 20 Asn 1 5 10 15 20 B-Chain 25 Extension 30 Arg
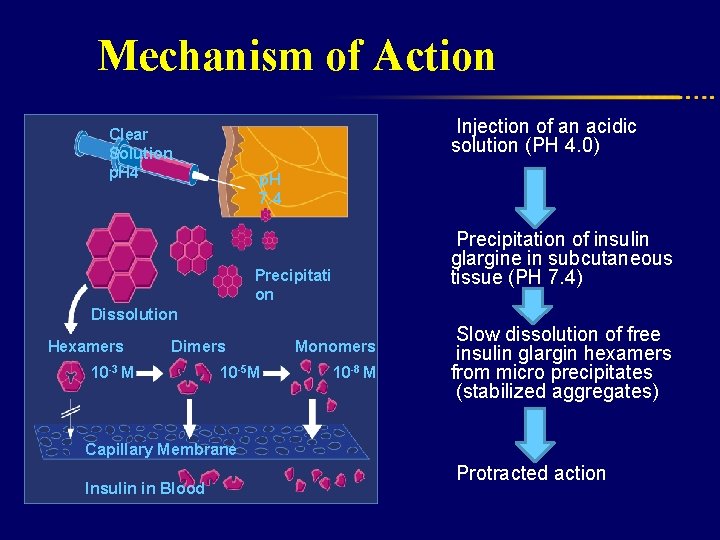
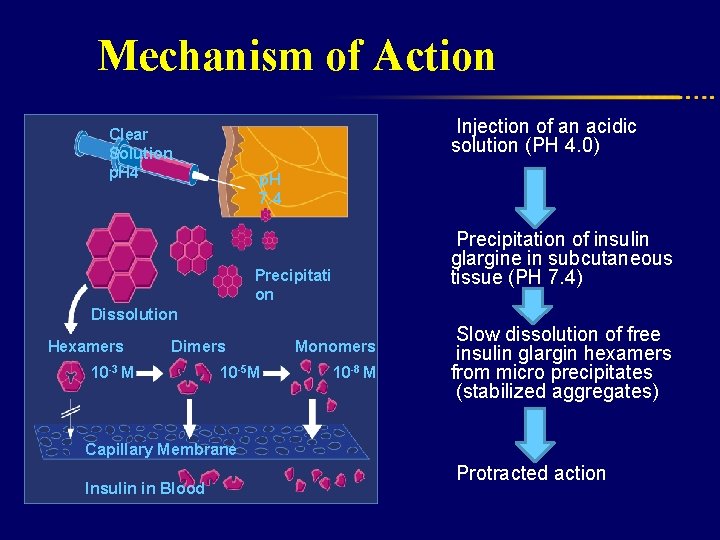
Mechanism of Action Injection of an acidic solution (PH 4. 0) Clear Solution p. H 4 p. H 7. 4 Precipitation of insulin glargine in subcutaneous tissue (PH 7. 4) Precipitati on Dissolution Hexamers Dimers 10 -3 M 10 -5 M Capillary Membrane Insulin in Blood Monomers 10 -8 M Slow dissolution of free insulin glargin hexamers from micro precipitates (stabilized aggregates) Protracted action
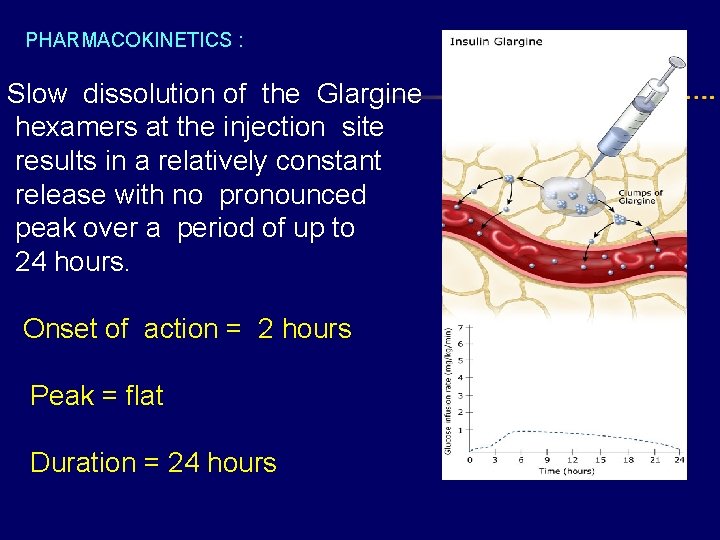
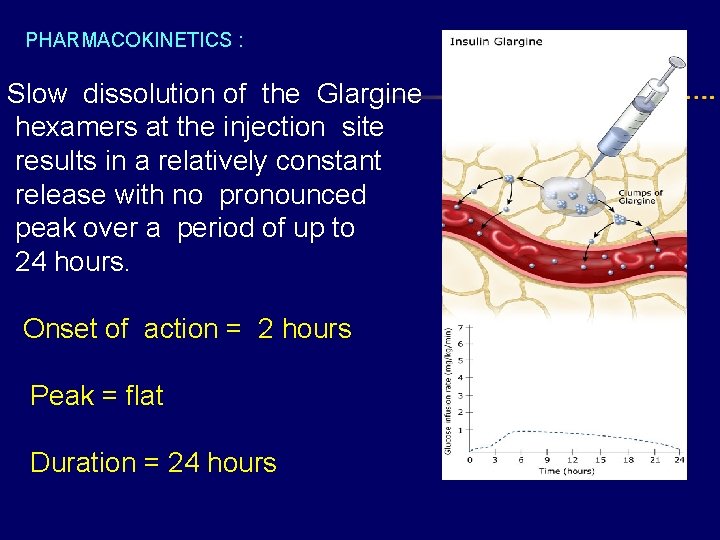
PHARMACOKINETICS : Slow dissolution of the Glargine hexamers at the injection site results in a relatively constant release with no pronounced peak over a period of up to 24 hours. Onset of action = 2 hours Peak = flat Duration = 24 hours
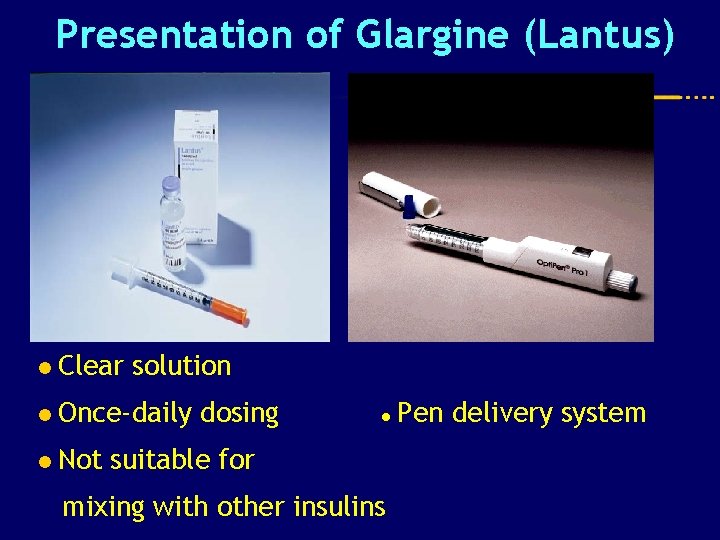
Presentation of Glargine (Lantus) l Clear solution l Once-daily l Not dosing ● suitable for mixing with other insulins Pen delivery system
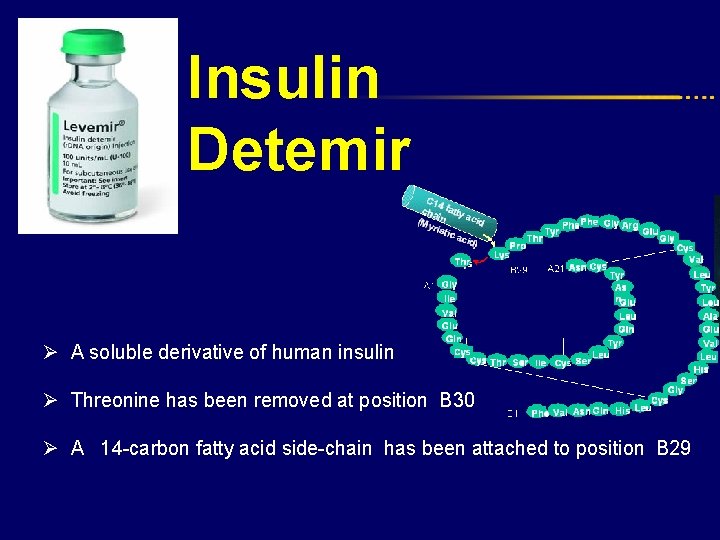
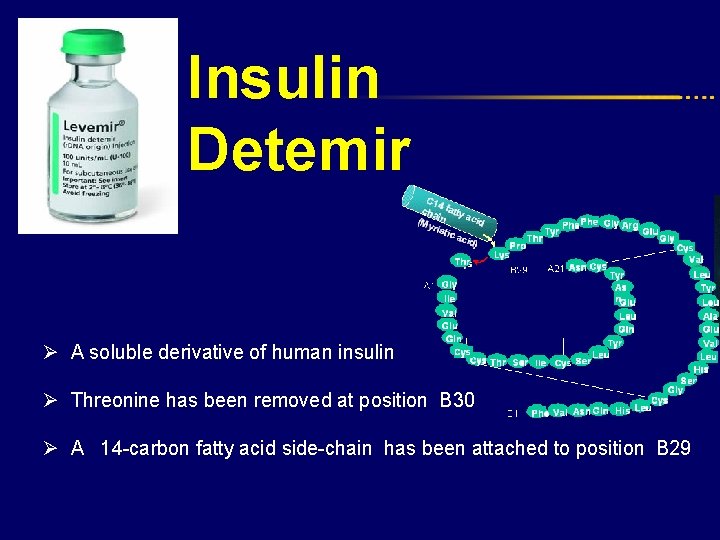
Insulin Detemir Ø A soluble derivative of human insulin Ø Threonine has been removed at position B 30 Ø A 14 -carbon fatty acid side-chain has been attached to position B 29
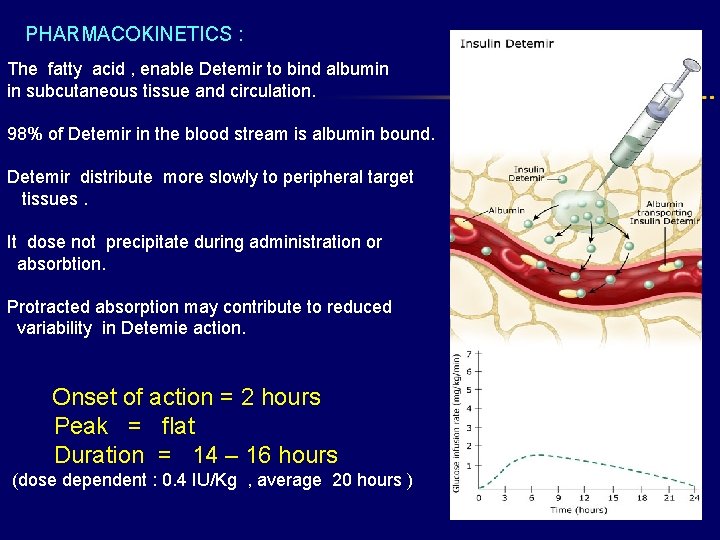
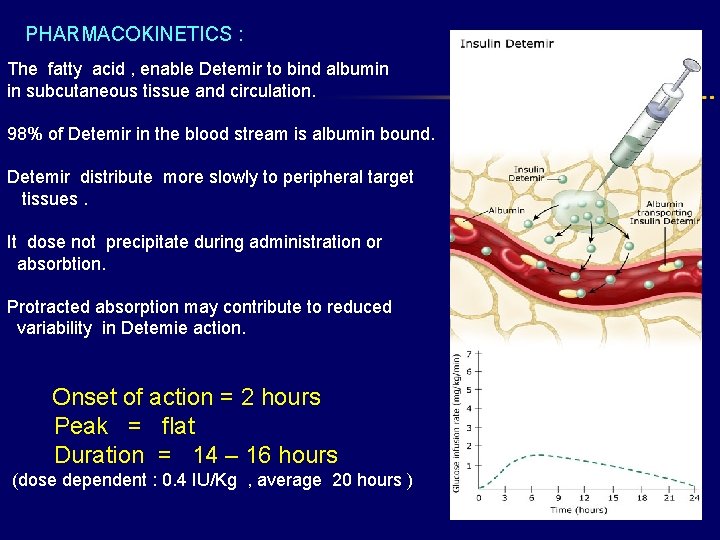
PHARMACOKINETICS : The fatty acid , enable Detemir to bind albumin in subcutaneous tissue and circulation. 98% of Detemir in the blood stream is albumin bound. Detemir distribute more slowly to peripheral target tissues. It dose not precipitate during administration or absorbtion. Protracted absorption may contribute to reduced variability in Detemie action. Onset of action = 2 hours Peak = flat Duration = 14 – 16 hours (dose dependent : 0. 4 IU/Kg , average 20 hours )
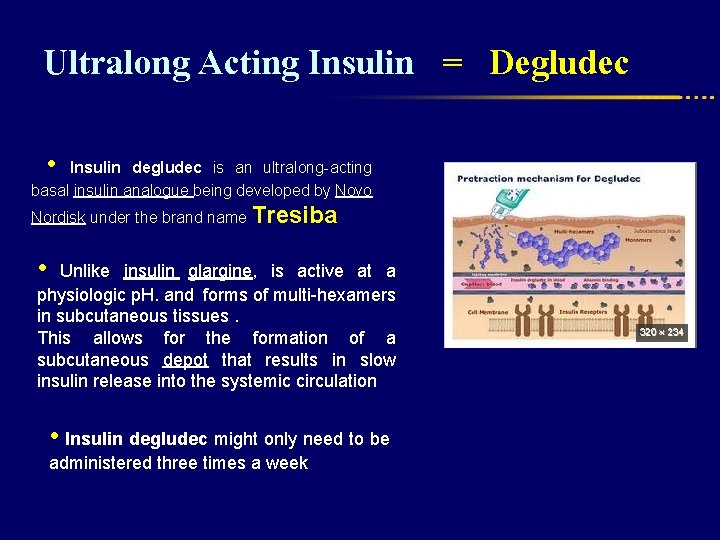
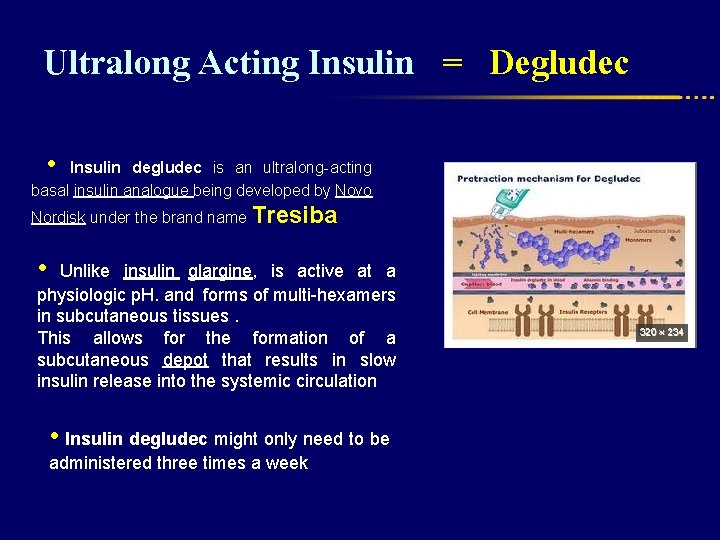
Ultralong Acting Insulin = Degludec • Insulin degludec is an ultralong-acting basal insulin analogue being developed by Novo Nordisk under the brand name Tresiba • Unlike insulin glargine, is active at a physiologic p. H. and forms of multi-hexamers in subcutaneous tissues. This allows for the formation of a subcutaneous depot that results in slow insulin release into the systemic circulation • Insulin degludec might only need to be administered three times a week
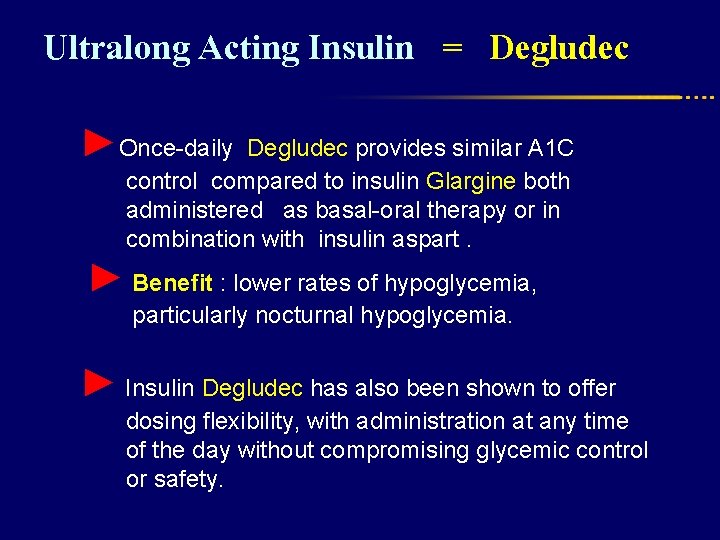
Ultralong Acting Insulin = Degludec ►Once-daily Degludec provides similar A 1 C control compared to insulin Glargine both administered as basal-oral therapy or in combination with insulin aspart. ► Benefit : lower rates of hypoglycemia, particularly nocturnal hypoglycemia. ► Insulin Degludec has also been shown to offer dosing flexibility, with administration at any time of the day without compromising glycemic control or safety.
Ultralong Acting Insulin = Degludec l Insulin Degludec has an onset of action of 30 -90 minutes (similar to insulin Glargine and insulin Detemir). l There is no peak in activity, due to the slow release into systemic circulation. l The duration of action of insulin degludec is reported as being longer than 24 hours l Novo Nordisk hopes to begin marketing the insulin analog in 2013
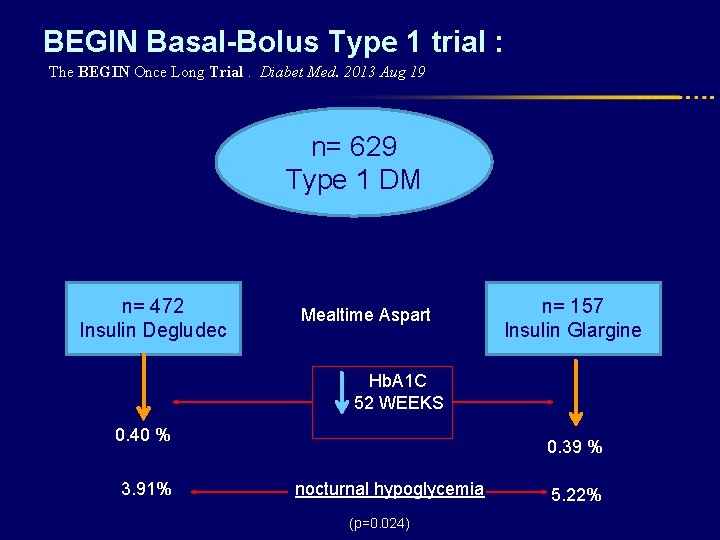
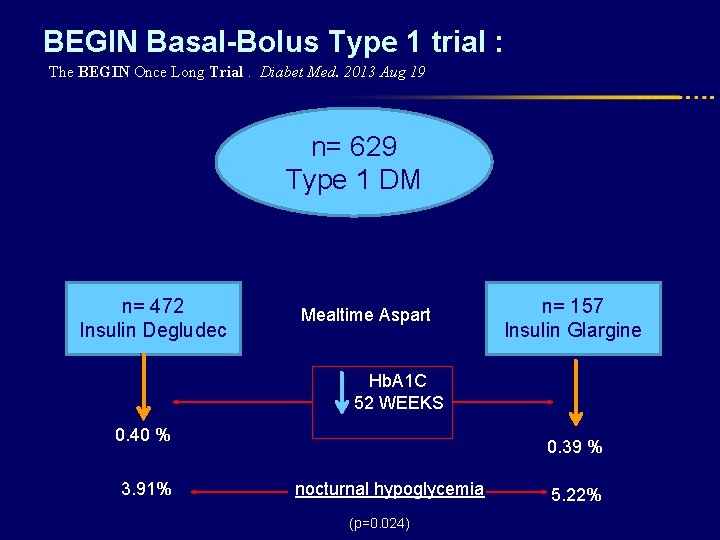
BEGIN Basal-Bolus Type 1 trial : The BEGIN Once Long Trial. Diabet Med. 2013 Aug 19 n= 629 Type 1 DM n= 472 Insulin Degludec Mealtime Aspart n= 157 Insulin Glargine Hb. A 1 C 52 WEEKS 0. 40 % 3. 91% 0. 39 % nocturnal hypoglycemia (p=0. 024) 5. 22%

Insulin treatment regimens
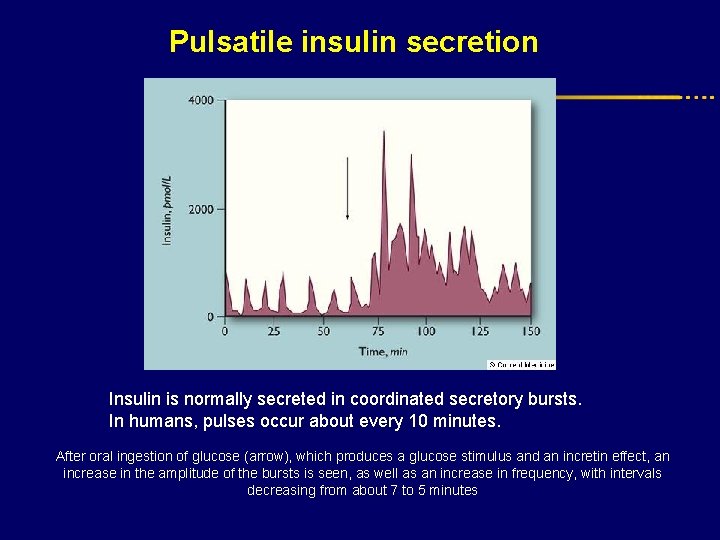
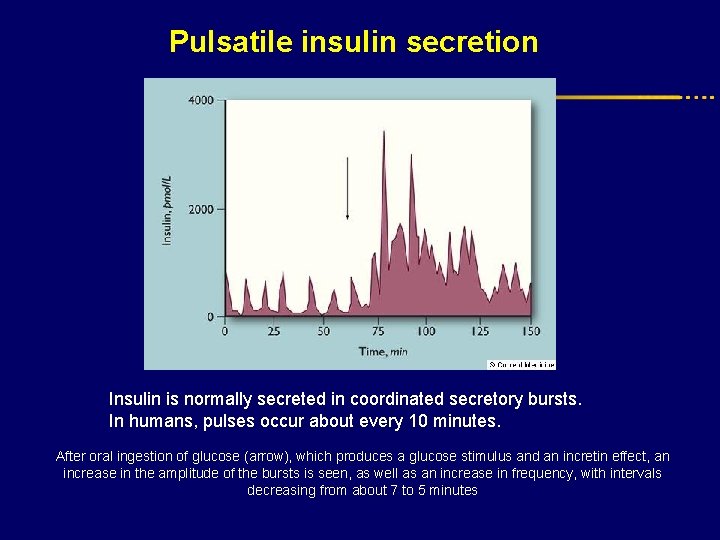
Pulsatile insulin secretion Insulin is normally secreted in coordinated secretory bursts. In humans, pulses occur about every 10 minutes. After oral ingestion of glucose (arrow), which produces a glucose stimulus and an incretin effect, an increase in the amplitude of the bursts is seen, as well as an increase in frequency, with intervals decreasing from about 7 to 5 minutes
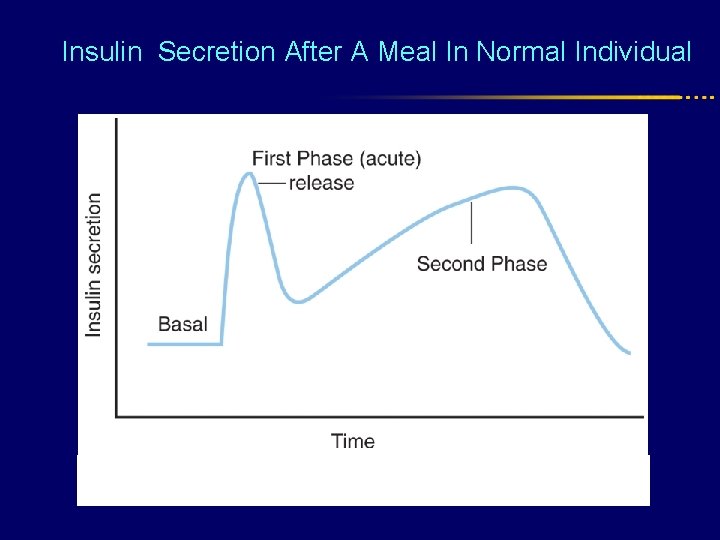
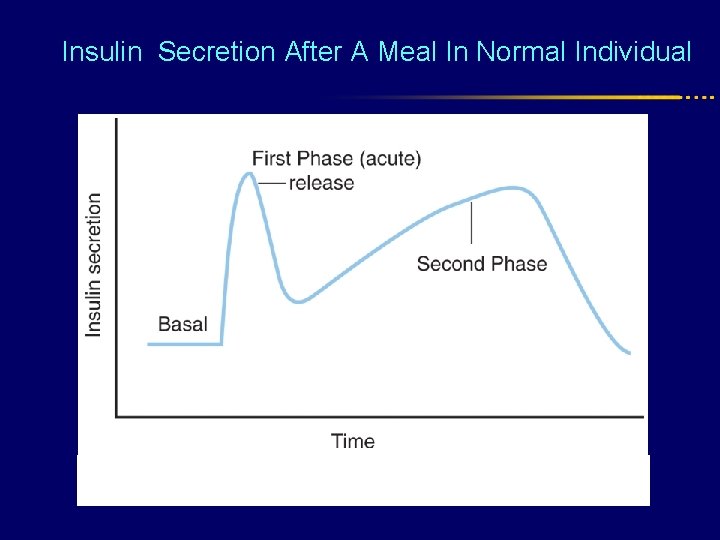
Insulin Secretion After A Meal In Normal Individual
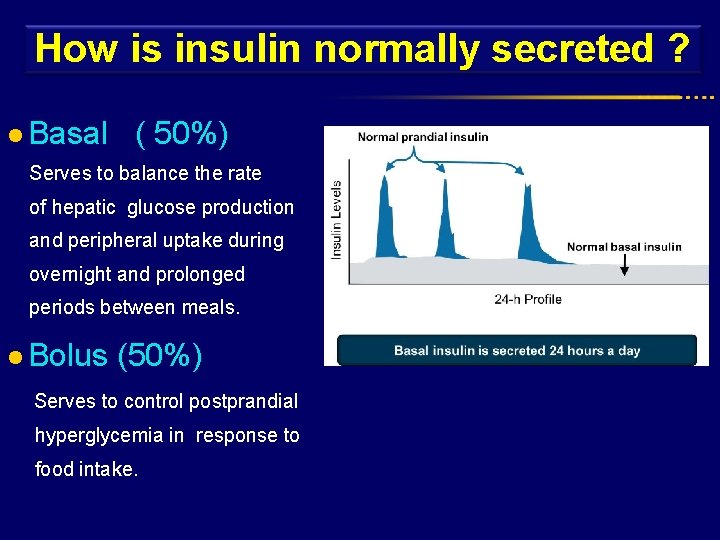
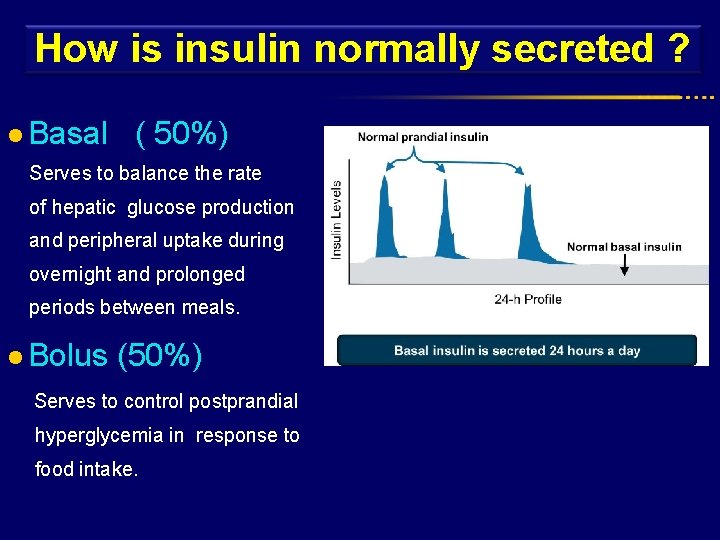
How is insulin normally secreted ? l Basal ( 50%) Serves to balance the rate of hepatic glucose production and peripheral uptake during overnight and prolonged periods between meals. l Bolus (50%) Serves to control postprandial hyperglycemia in response to food intake. Basal
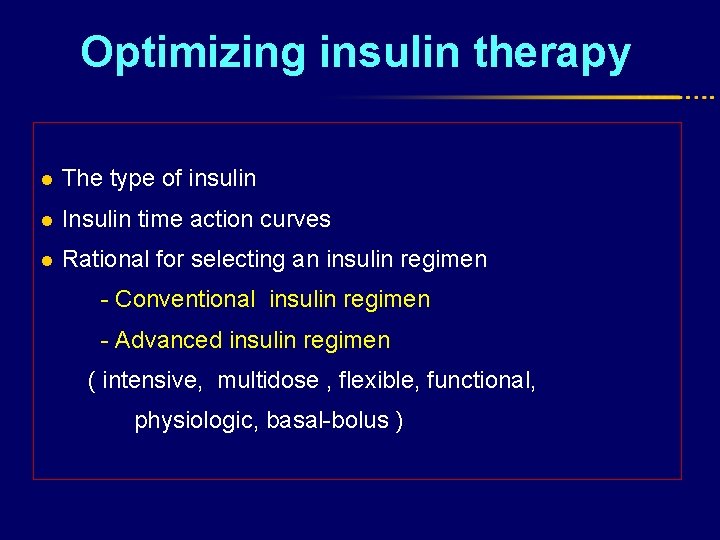
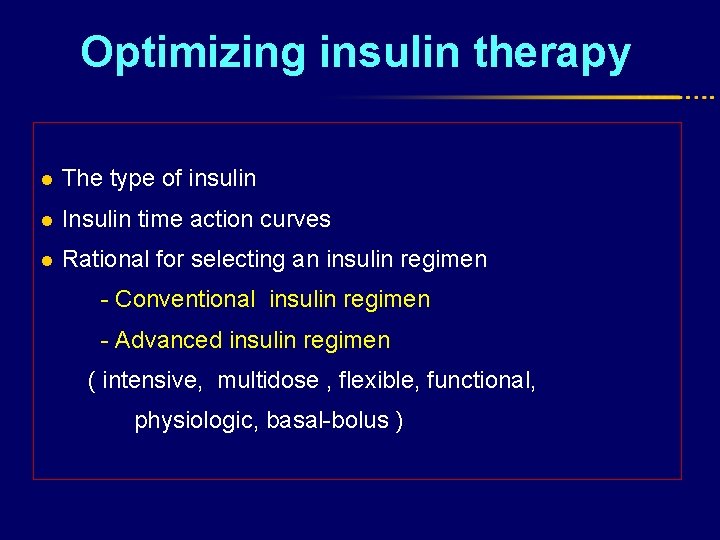
Optimizing insulin therapy l The type of insulin l Insulin time action curves l Rational for selecting an insulin regimen - Conventional insulin regimen - Advanced insulin regimen ( intensive, multidose , flexible, functional, physiologic, basal-bolus )
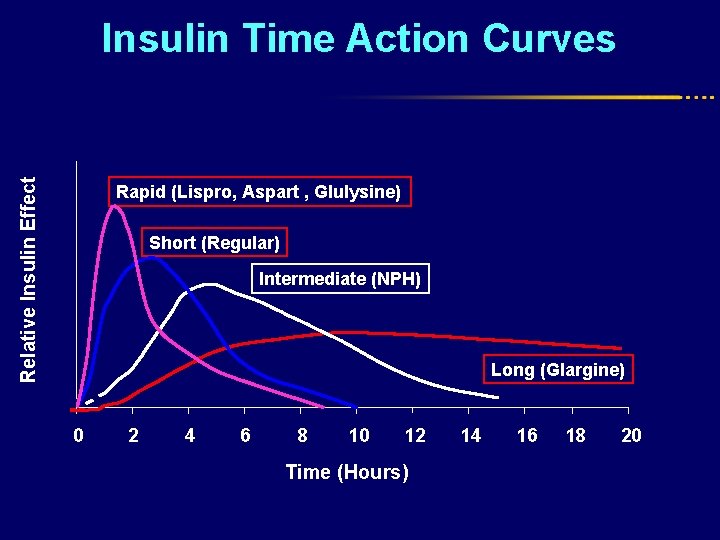
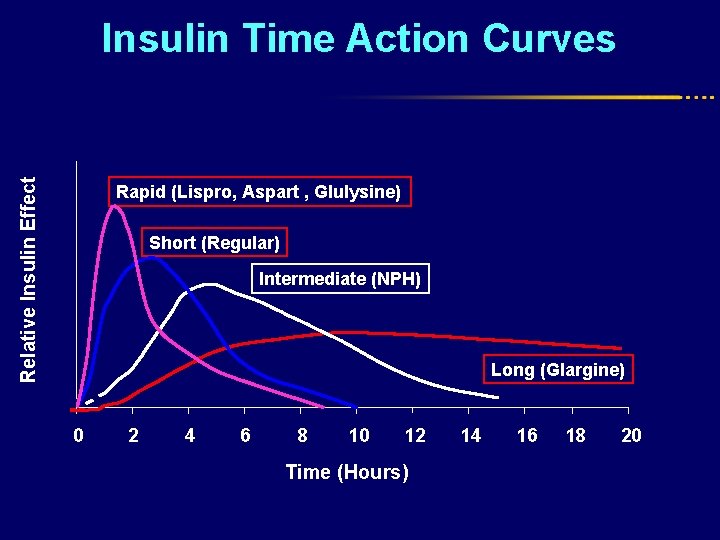
Relative Insulin Effect Insulin Time Action Curves Rapid (Lispro, Aspart , Glulysine) Short (Regular) Intermediate (NPH) Long (Glargine) 0 2 4 6 8 10 12 Time (Hours) 14 16 18 20
Single insulin dose Is rarely able to achieve normoglycemia, Least effective regimen and rarely suitable - Occasionally in newly diagnosed T 1 DM - Diabetic patients with ESRD on dialysis
Once Daily Insulin Regimen (for patients with type 2 diabetes on oral agents) For people with type 2 diabetes, in whom basal insulin replacement is not as critical, once or twice daily regimens can still work satisfactorily with reasonable glycemic control achieved. • NPH, Glargine , or Detemir are most often given at bedtime. • For patient who eat large amounts of carbohydrates at dinner, an insulin mixture, regular and NPH or a prexmixed insulin, can be given prior to dinner.
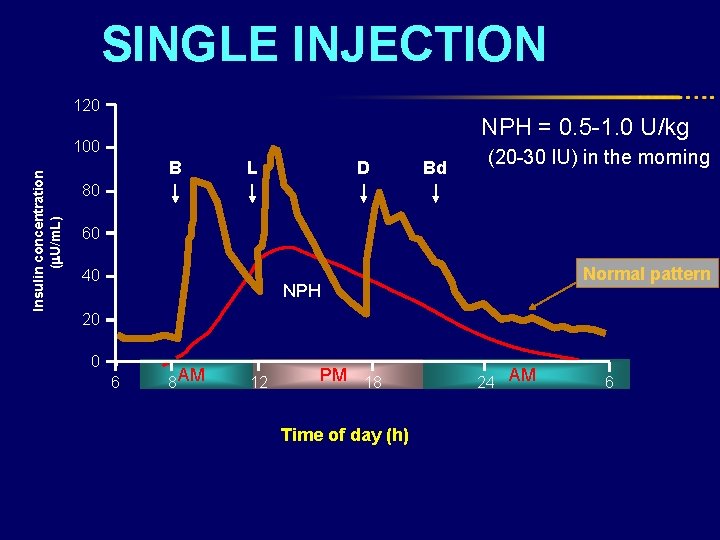
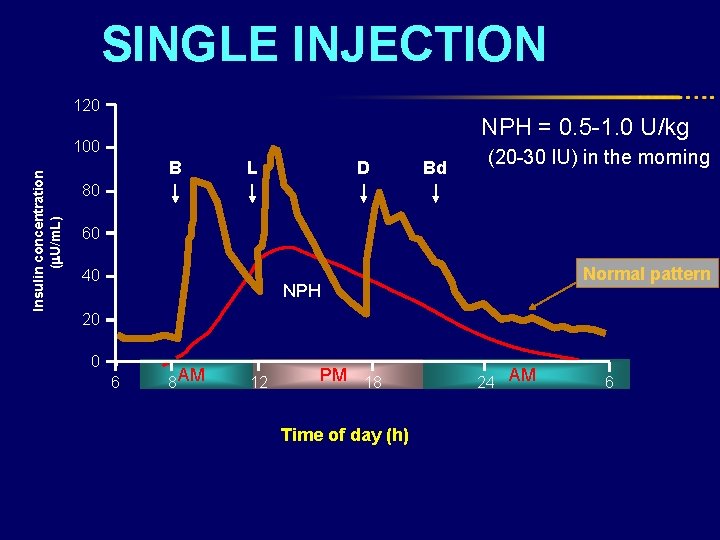
SINGLE INJECTION 120 Insulin concentration ( U/m. L) 100 B L D Bd NPH = 0. 5 -1. 0 U/kg (20 -30 IU) in the morning 80 60 40 Normal pattern NPH 20 0 6 AM 8 12 PM 18 Time of day (h) AM 24 6
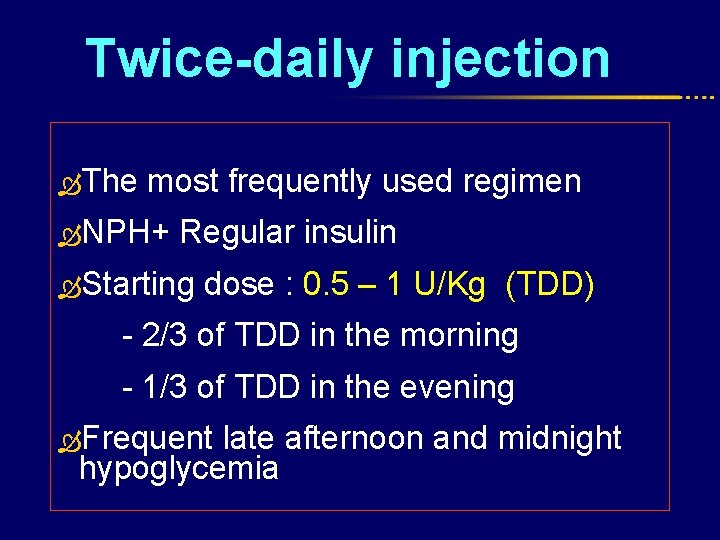
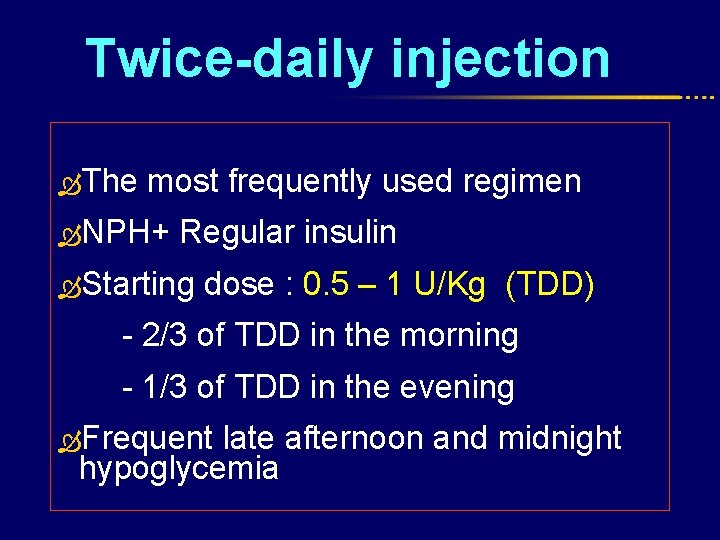
Twice-daily injection The most frequently used regimen NPH+ Regular insulin Starting dose : 0. 5 – 1 U/Kg (TDD) - 2/3 of TDD in the morning - 1/3 of TDD in the evening Frequent late afternoon and midnight hypoglycemia
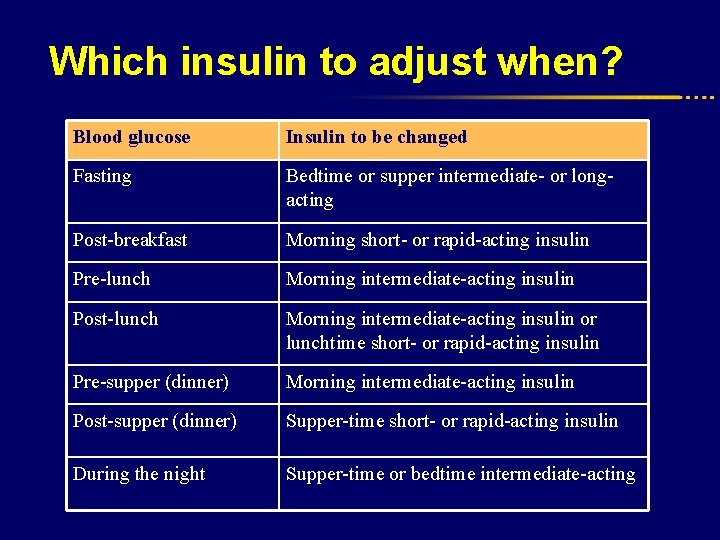
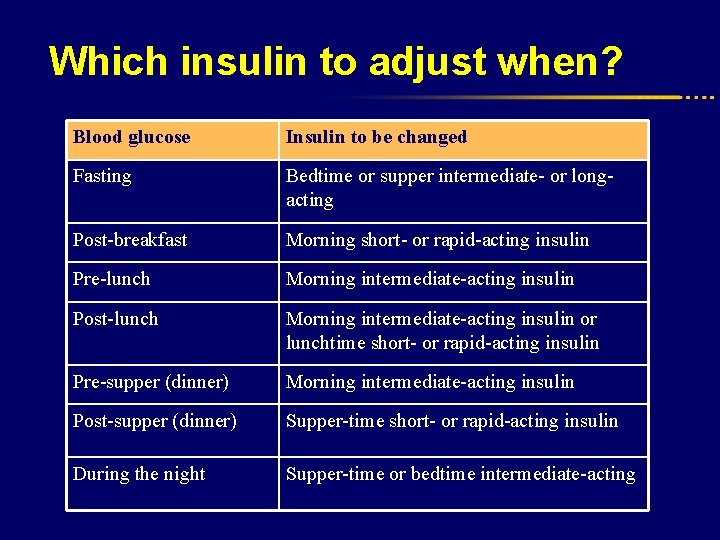
Which insulin to adjust when? Blood glucose Insulin to be changed Fasting Bedtime or supper intermediate- or longacting Post-breakfast Morning short- or rapid-acting insulin Pre-lunch Morning intermediate-acting insulin Post-lunch Morning intermediate-acting insulin or lunchtime short- or rapid-acting insulin Pre-supper (dinner) Morning intermediate-acting insulin Post-supper (dinner) Supper-time short- or rapid-acting insulin During the night Supper-time or bedtime intermediate-acting
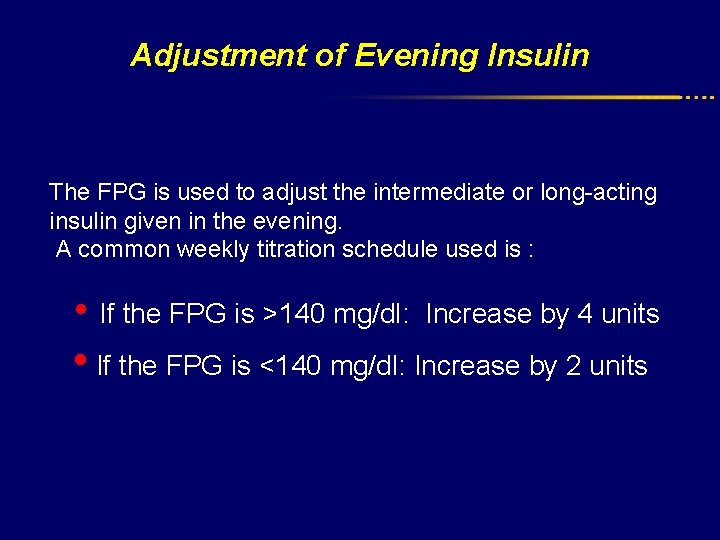
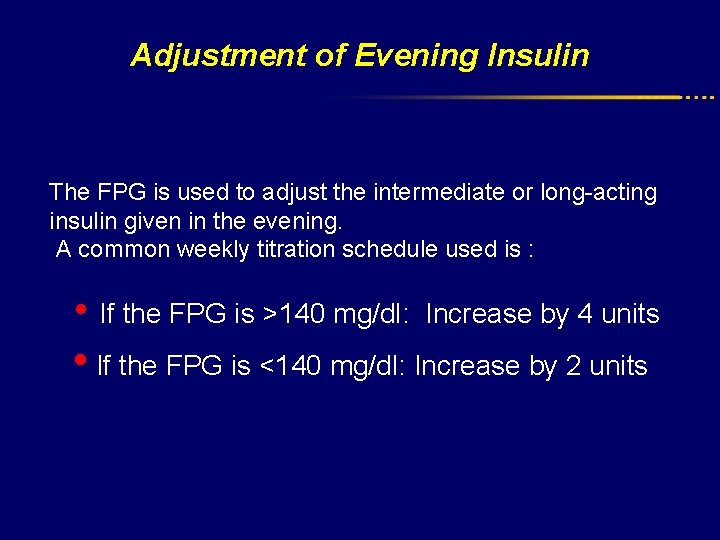
Adjustment of Evening Insulin The FPG is used to adjust the intermediate or long-acting insulin given in the evening. A common weekly titration schedule used is : • If the FPG is >140 mg/dl: Increase by 4 units • If the FPG is <140 mg/dl: Increase by 2 units
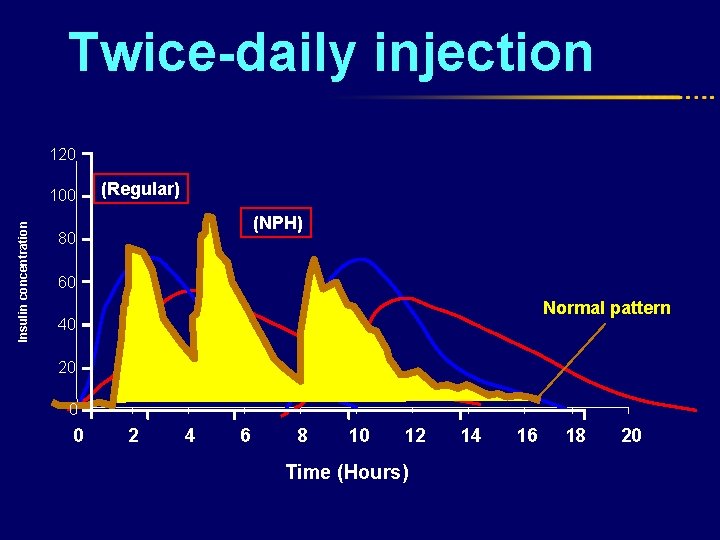
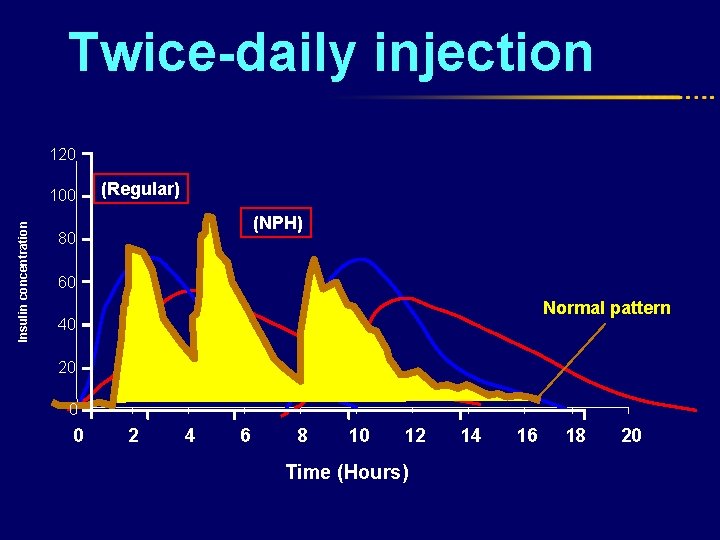
Twice-daily injection 120 Insulin concentration 100 (Regular) (NPH) 80 60 Normal pattern 40 20 0 0 2 4 6 8 10 12 Time (Hours) 14 16 18 20
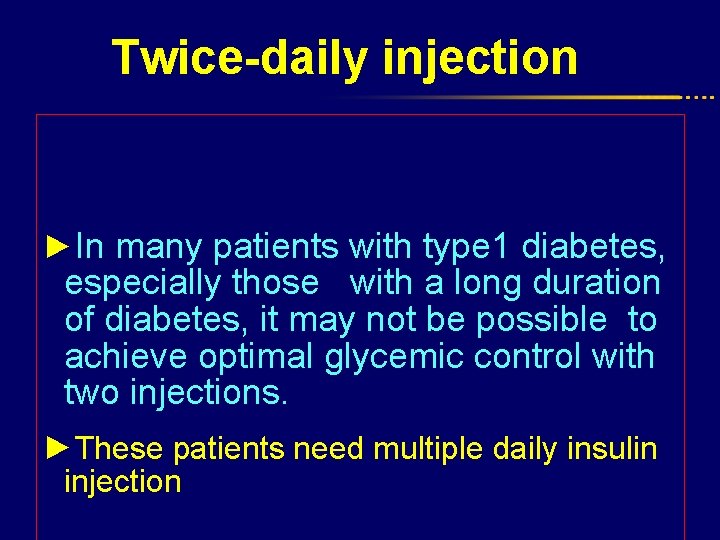
Twice-daily injection ►In many patients with type 1 diabetes, especially those with a long duration of diabetes, it may not be possible to achieve optimal glycemic control with two injections. ►These patients need multiple daily insulin injection
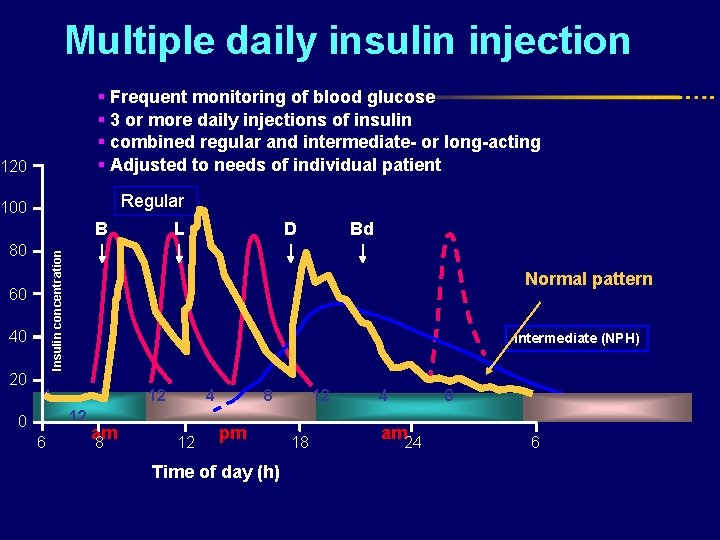
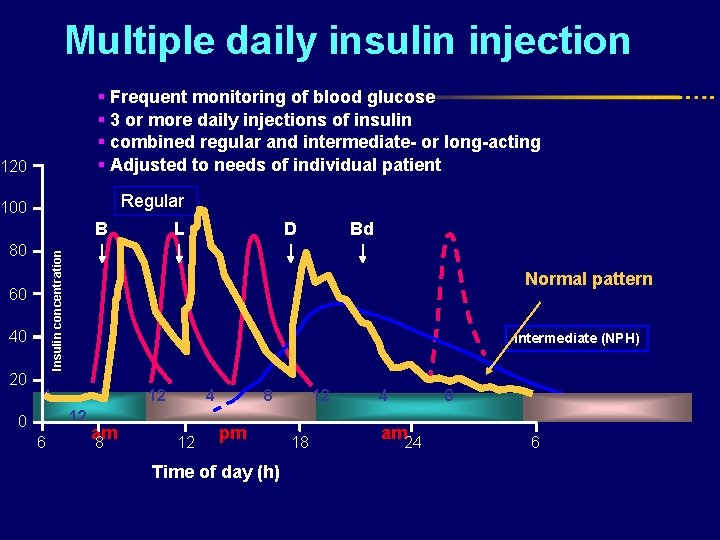
Multiple daily insulin injection § Frequent monitoring of blood glucose § 3 or more daily injections of insulin § combined regular and intermediate- or long-acting § Adjusted to needs of individual patient 120 Regular 100 B 60 40 20 D Bd Insulin concentration 80 L Normal pattern Intermediate (NPH) 4 8 12 0 6 am 8 12 4 12 8 pm Time of day (h) 12 18 4 8 am 24 6
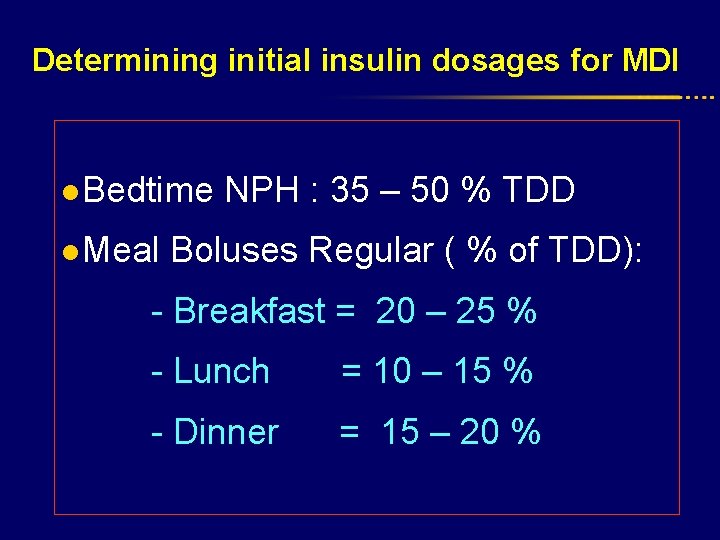
Determining initial insulin dosages for MDI l Bedtime NPH : 35 – 50 % TDD l Meal Boluses Regular ( % of TDD): - Breakfast = 20 – 25 % - Lunch = 10 – 15 % - Dinner = 15 – 20 %
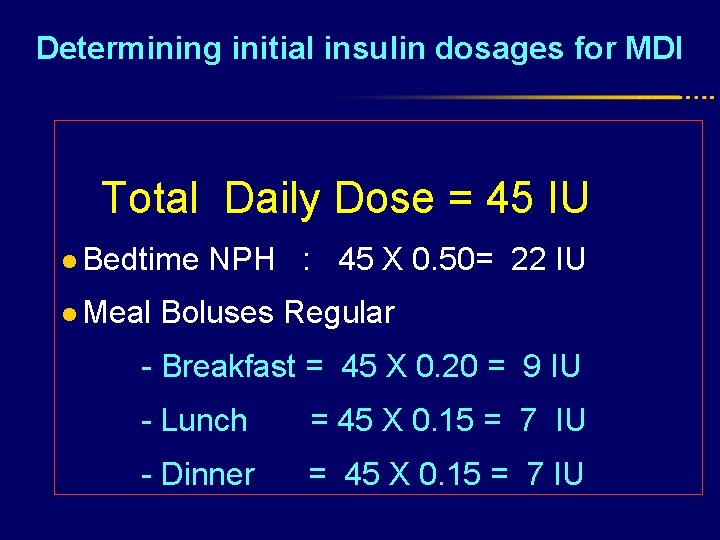
Determining initial insulin dosages for MDI Total Daily Dose = 45 IU l Bedtime NPH : 45 X 0. 50= 22 IU l Meal Boluses Regular - Breakfast = 45 X 0. 20 = 9 IU - Lunch = 45 X 0. 15 = 7 IU - Dinner = 45 X 0. 15 = 7 IU
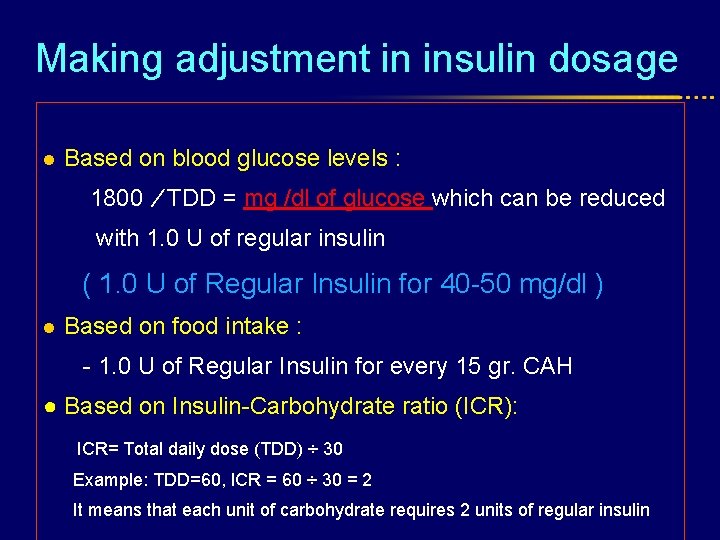
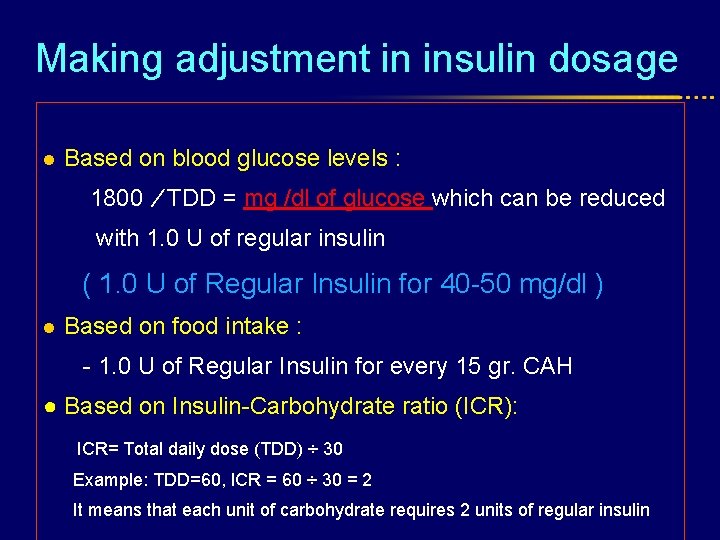
Making adjustment in insulin dosage l Based on blood glucose levels : 1800 ⁄ TDD = mg /dl of glucose which can be reduced with 1. 0 U of regular insulin ( 1. 0 U of Regular Insulin for 40 -50 mg/dl ) l Based on food intake : - 1. 0 U of Regular Insulin for every 15 gr. CAH ● Based on Insulin-Carbohydrate ratio (ICR): ICR= Total daily dose (TDD) ÷ 30 Example: TDD=60, ICR = 60 ÷ 30 = 2 It means that each unit of carbohydrate requires 2 units of regular insulin
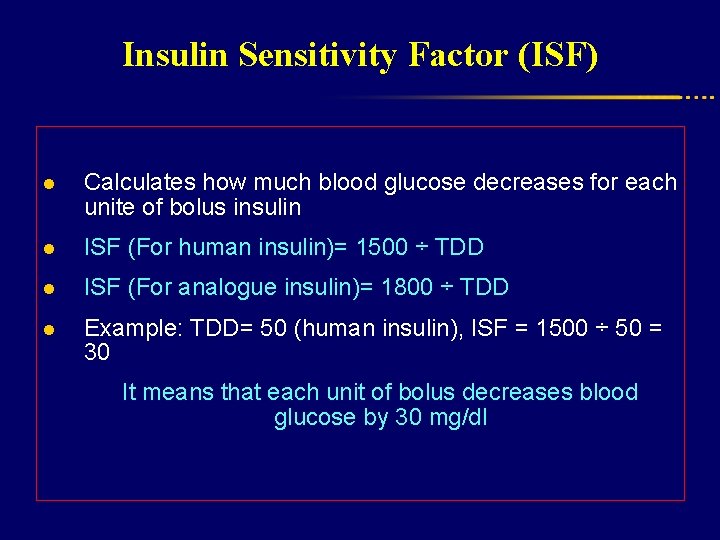
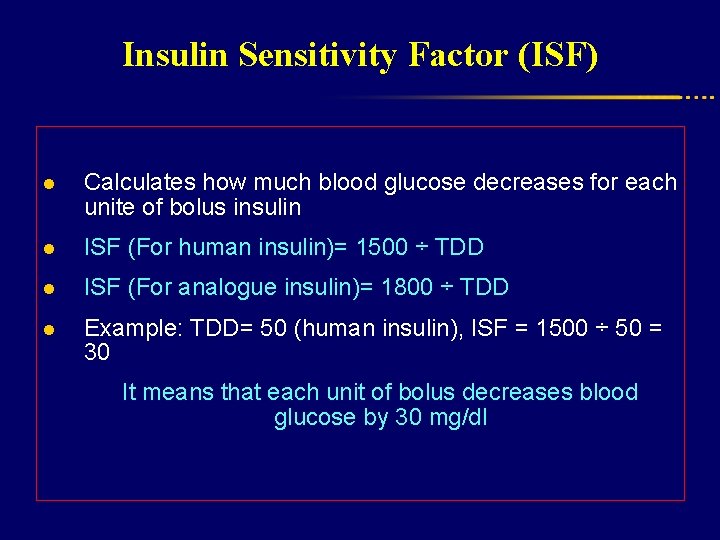
Insulin Sensitivity Factor (ISF) l Calculates how much blood glucose decreases for each unite of bolus insulin l ISF (For human insulin)= 1500 ÷ TDD l ISF (For analogue insulin)= 1800 ÷ TDD l Example: TDD= 50 (human insulin), ISF = 1500 ÷ 50 = 30 It means that each unit of bolus decreases blood glucose by 30 mg/dl
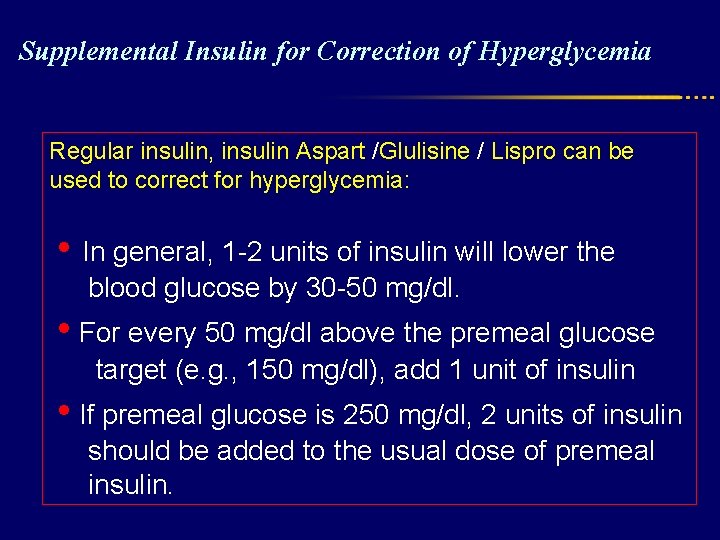
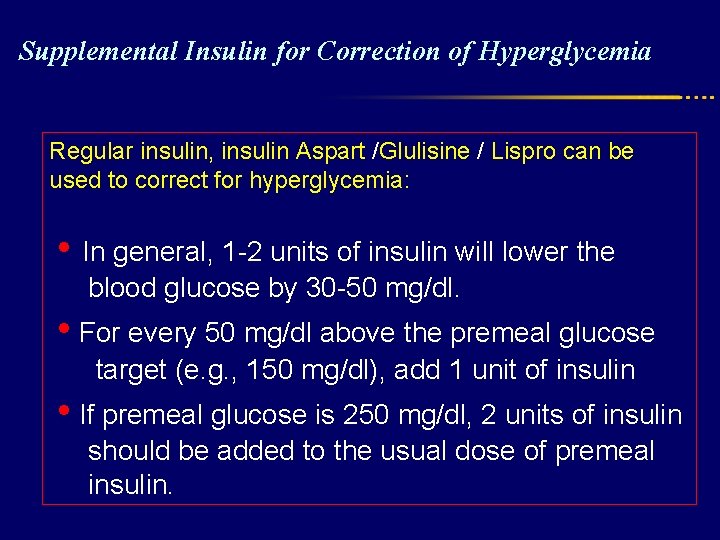
Supplemental Insulin for Correction of Hyperglycemia Regular insulin, insulin Aspart /Glulisine / Lispro can be used to correct for hyperglycemia: • In general, 1 -2 units of insulin will lower the blood glucose by 30 -50 mg/dl. • For every 50 mg/dl above the premeal glucose target (e. g. , 150 mg/dl), add 1 unit of insulin • If premeal glucose is 250 mg/dl, 2 units of insulin should be added to the usual dose of premeal insulin.
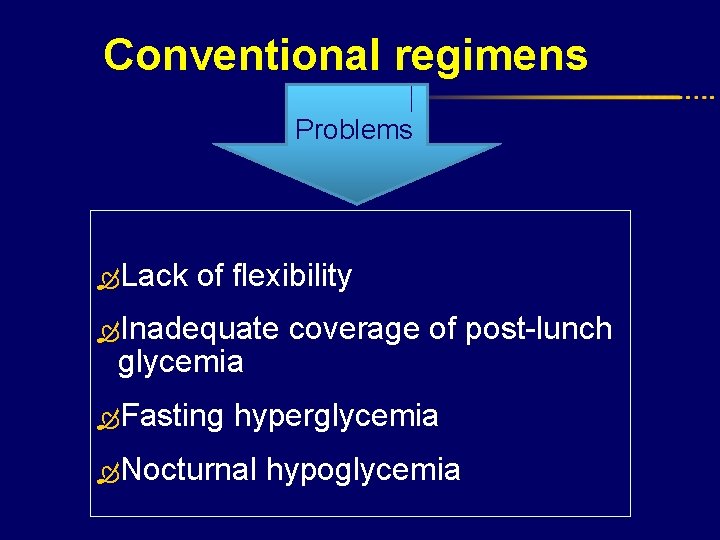
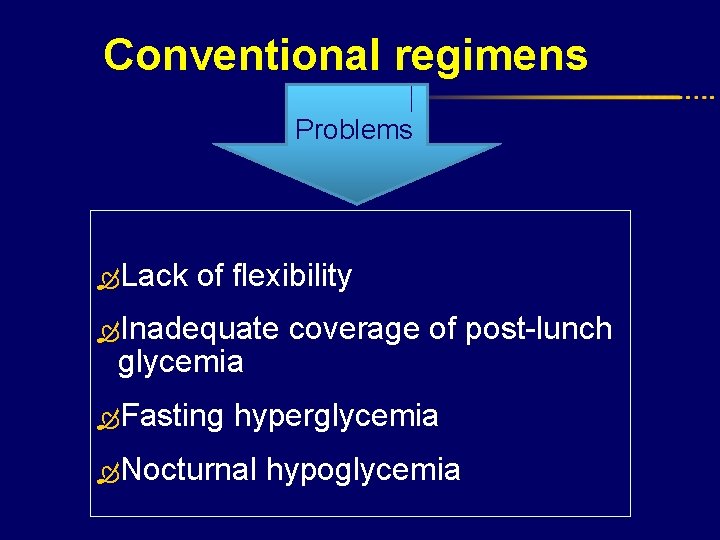
Conventional regimens Problems Lack of flexibility Inadequate coverage of post-lunch glycemia Fasting hyperglycemia Nocturnal hypoglycemia
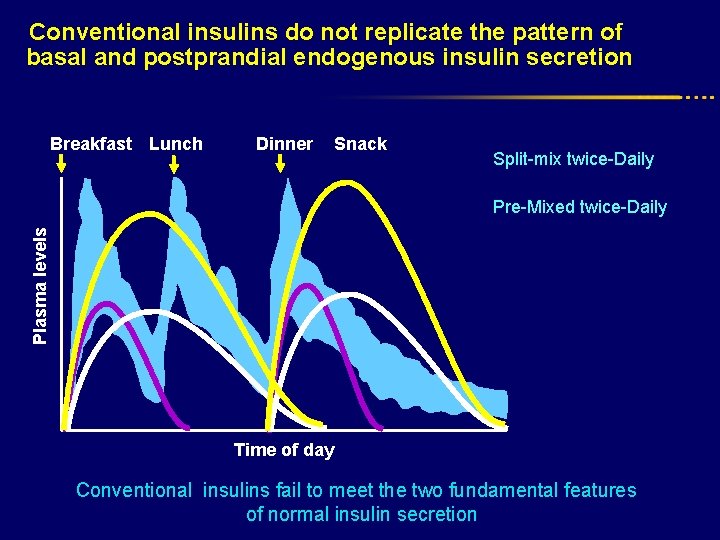
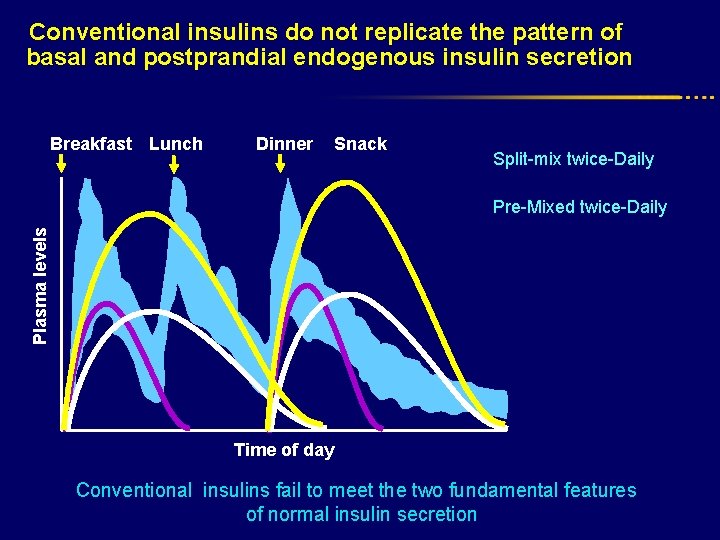
Conventional insulins do not replicate the pattern of basal and postprandial endogenous insulin secretion Breakfast Lunch Dinner Snack Split-mix twice-Daily Plasma levels Pre-Mixed twice-Daily Time of day Conventional insulins fail to meet the two fundamental features of normal insulin secretion
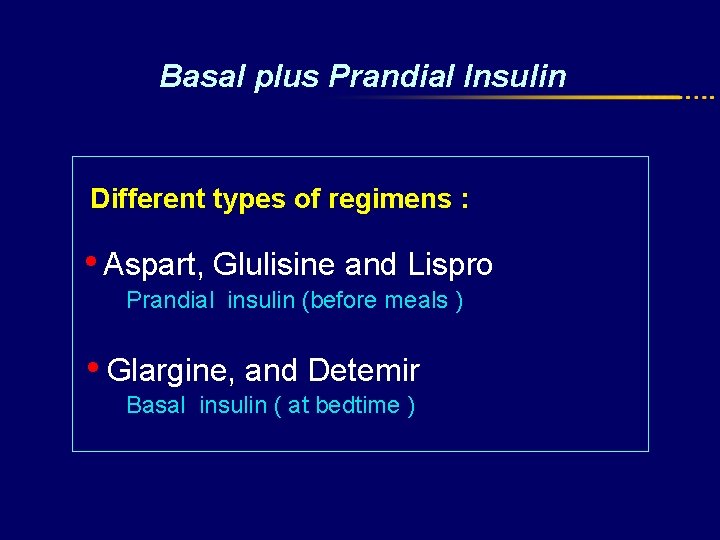
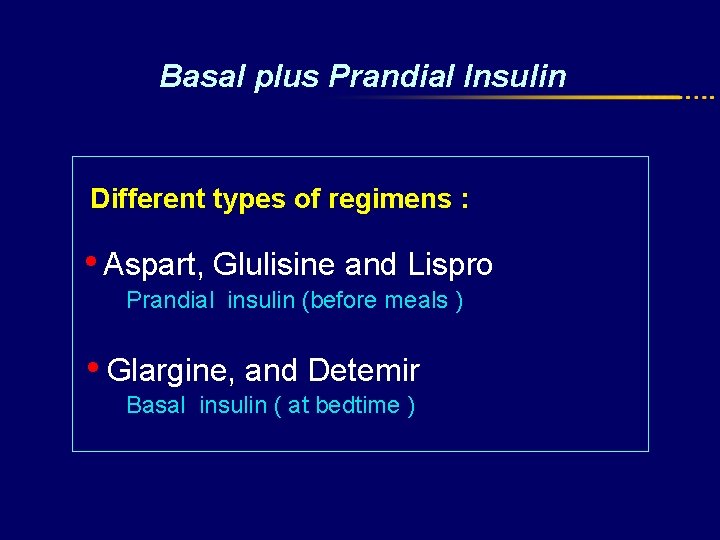
Basal plus Prandial Insulin Different types of regimens : • Aspart, Glulisine and Lispro Prandial insulin (before meals ) • Glargine, and Detemir Basal insulin ( at bedtime )
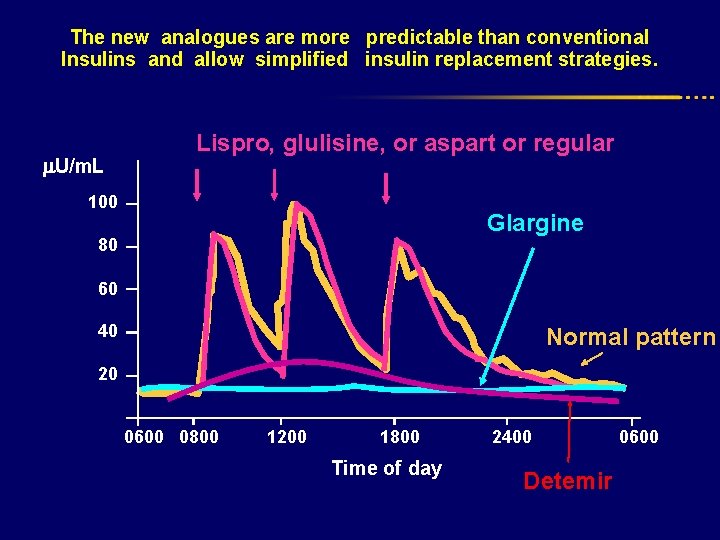
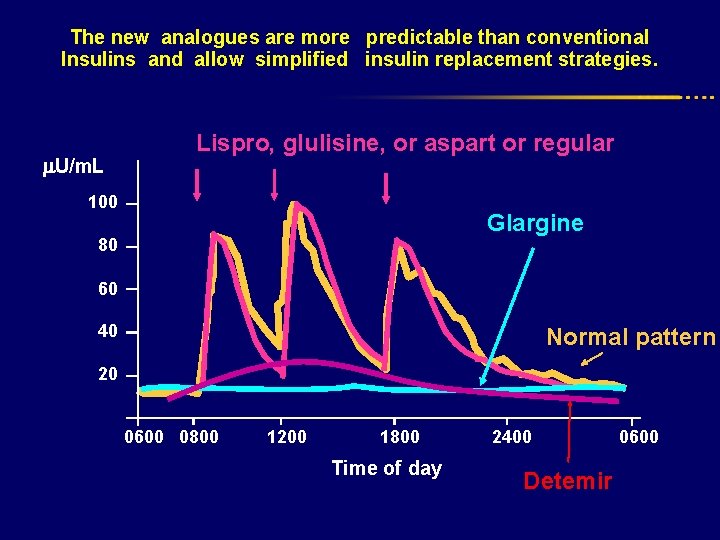
The new analogues are more predictable than conventional Insulins and allow simplified insulin replacement strategies. U/m. L Lispro, glulisine, or aspart or regular 100 Glargine 80 60 40 Normal pattern 20 0600 0800 1200 1800 Time of day 2400 Detemir 0600
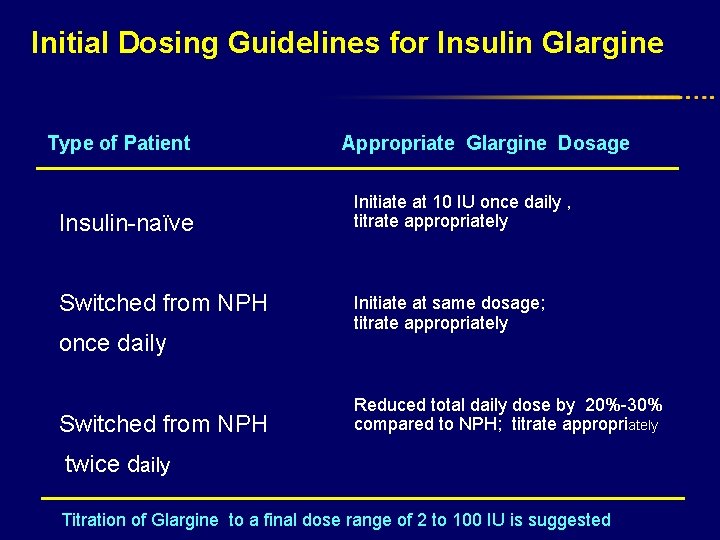
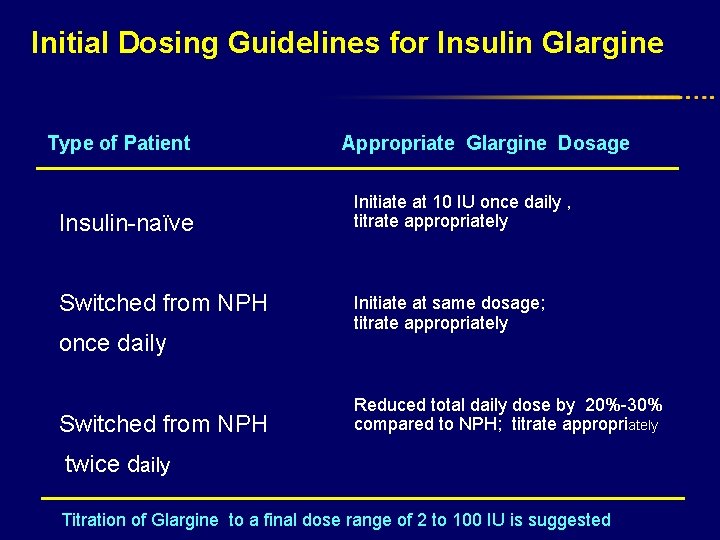
Initial Dosing Guidelines for Insulin Glargine Type of Patient Insulin-naïve Switched from NPH once daily Switched from NPH Appropriate Glargine Dosage Initiate at 10 IU once daily , titrate appropriately Initiate at same dosage; titrate appropriately Reduced total daily dose by 20%-30% compared to NPH; titrate appropriately twice daily Titration of Glargine to a final dose range of 2 to 100 IU is suggested
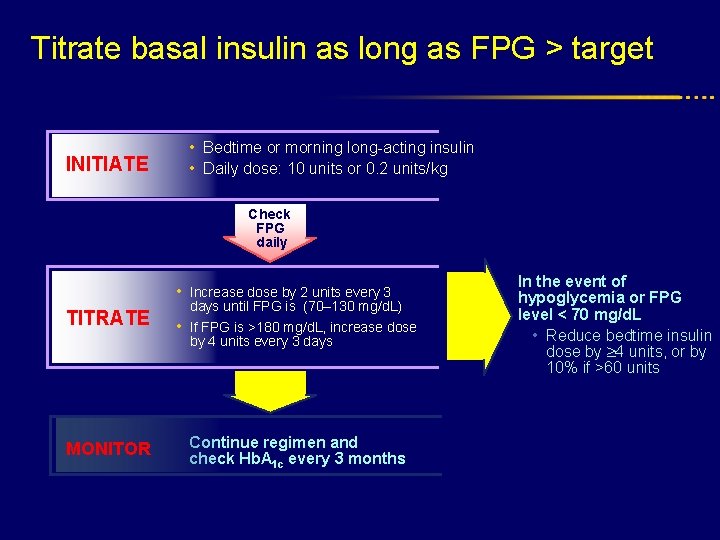
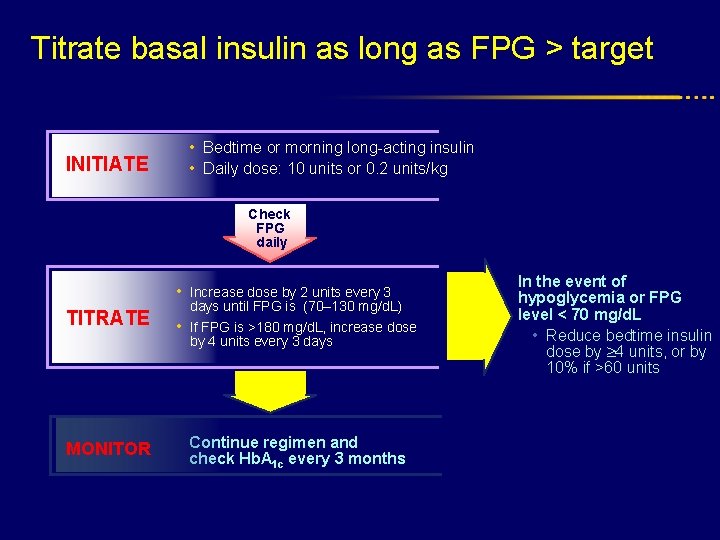
Titrate basal insulin as long as FPG > target INITIATE • Bedtime or morning long-acting insulin • Daily dose: 10 units or 0. 2 units/kg Check FPG daily • Increase dose by 2 units every 3 TITRATE days until FPG is (70– 130 mg/d. L) • If FPG is >180 mg/d. L, increase dose by 4 units every 3 days MONITOR Continue regimen and check Hb. A 1 c every 3 months In the event of hypoglycemia or FPG level < 70 mg/d. L • Reduce bedtime insulin dose by 4 units, or by 10% if >60 units
Adjustments for Exercise improves insulin sensitivity : • For morning exercise : Reduce pre-breakfast insulin (~25%) • For early-afternoon exercise : Reduce the pre-lunch insulin • For evening exercise Reduce pre-dinner insulin
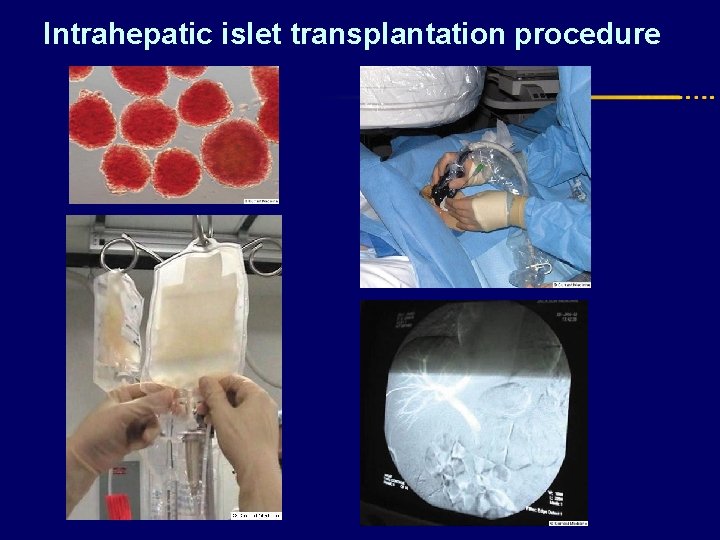
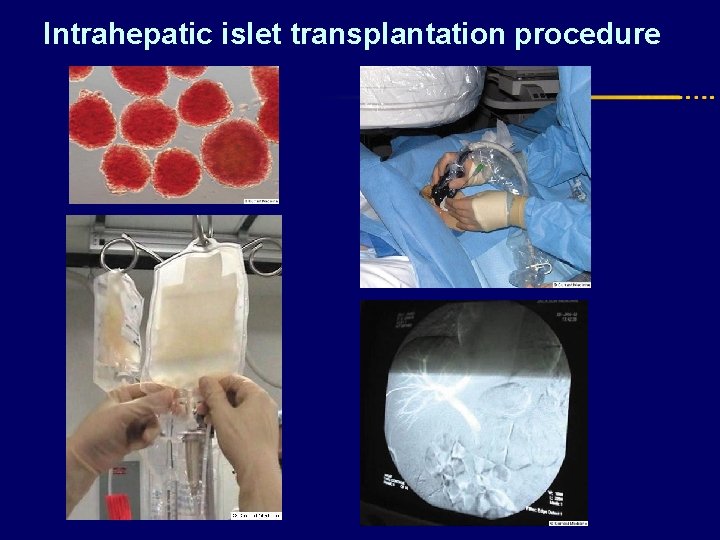
Intrahepatic islet transplantation procedure
