Instrumentation for the Dental Hygienist DENTALELLE TUTORING Instrument











- Slides: 65
Instrumentation for the Dental Hygienist DENTALELLE TUTORING
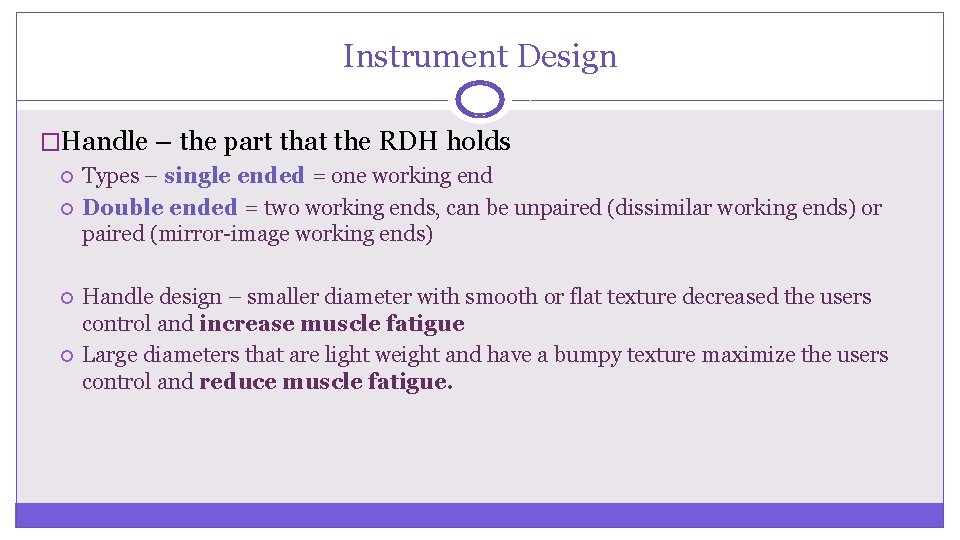
Instrument Design �Handle – the part that the RDH holds Types – single ended = one working end Double ended = two working ends, can be unpaired (dissimilar working ends) or paired (mirror-image working ends) Handle design – smaller diameter with smooth or flat texture decreased the users control and increase muscle fatigue Large diameters that are light weight and have a bumpy texture maximize the users control and reduce muscle fatigue.
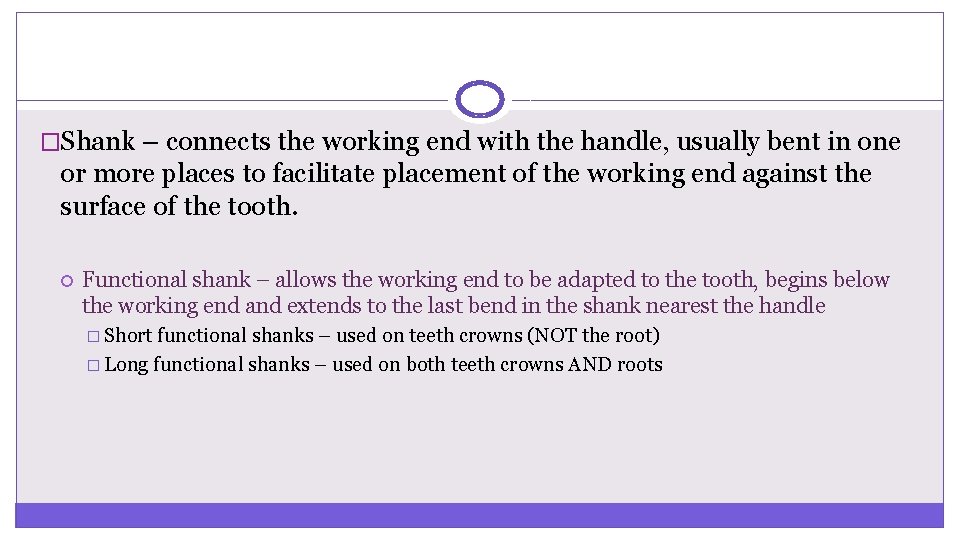
�Shank – connects the working end with the handle, usually bent in one or more places to facilitate placement of the working end against the surface of the tooth. Functional shank – allows the working end to be adapted to the tooth, begins below the working end and extends to the last bend in the shank nearest the handle � Short functional shanks – used on teeth crowns (NOT the root) � Long functional shanks – used on both teeth crowns AND roots
�Lower (terminal shank) – bent portion of the functional shank nearest to the working end �Simple shank – bent in one plane (from to back) used mainly on anterior teeth (also called straight shank) �Complex shank – bent in two planes (front to back and side to side) to facilitate instrumentation of posterior teeth; necessary to reach areas around the crown and onto root surface (also called angled shank or curved shank) �Extended lower shank – 3 mm longer than a standard lower shank; provides additional leverage, acting like a fulcrum, and is ideal when using advanced levering techniques or for working in deep pockets
Working end �Working end – part that contacts the tooth or soft tissue to perform the work of the instrument; begins where the instrument shank ends; an instrument may have one or two working ends. Function of the working end – assessment and/or debridement Parts of the working end – face, back, lateral surfaces, toe, tip…a cutting edge is formed by the union of a lateral surface and face of the working end Application of the working end – the tooth surface or areas of the mouth on which an instrument can be used: � Anterior – one single-ended instrument can be used to perform procedures on the facial, lingual, mesial, and distal surfaces of anterior teeth � Posterior – one double ended instrument can be used on the facial, lingual, mesial, and distal of posterior teeth � Universal – one double ended instrument can be used on both anterior and posterior teeth � Area-specific – only to specific areas of the mouth
Design Characteristics � A double ended instrument will have two design numbers If the design name and number are stamped along the length of the handle each working end is identified by the number closest to it. If the design name and number are stamped across the handle, the first number identifies the working end at the top of the handle, and the second number identifies the working end a he bottom. � Instrument identification – the unique design name and number that identify each instrument Design name – original design that identifies the individual responsible (Gracey 11) Design number – with the working end, when combined with the design name provides the exact identification of the working end (Gracey 11) � Instrument balance – a balanced instrument has working ends that are aligned with the long axis of the handle Balance ensures that finger pressure applied against the handle is transferred to the working end, which results in pressure against the tooth IF not balanced this increases stress on the muscles of the hand arm
Hand Activated Instruments
Classifications �Periodontal probes, explorers, sickle scalers, periodontal files, universal curets, area-specific curets, hoes, or chisels �Design characteristics include: Design of the cutting edges, back, lateral surfaces, and shank Cross section of the working end Relationship of the face to the lower shank �When selecting an instrument for a specific task, one of the most important considerations is the classification of the working end
Use of Hand Activated Instruments �Probe – pocket depths, CAL, attached gingiva, recession, lesions, evaluation of gingival tissue, bleeding, pus �Furcation Probe – Nabers Probe – furcation involvement �Explorer – detecting calculus, tooth surface irregularities, margins and restorations �Sickle scaler – removal of medium to large calculus deposits, supragingival use �Periodontal file – used to crush large calculus deposits, prepare burnished calculus for removal, NOT to be used on cementum �Universal curet – debridement of crown and root surfaces, removing light to medium calculus, supra and subgingival �Area-specific curet – debridement of crown and root surfaces, removal of light supra and subgingival calculus,
Dental Mirror �The working end has a reflecting (mirrored) surface �Uses Indirect vision – the mirrors reflecting surface provides a view of the tooth surface or intraoral structure that cannot be seen directly Retraction – using the mirror to hold the clients cheek or tongue back Indirect illumination – reflecting light from the mirrored surface into a dark area of the mouth Transillumination – reflecting light from the mirrored surface through anterior teeth �Types: Front surface – reflecting surface is on the front of the glass, produces a clear mirror image Concave – the reflecting surface is on the front surface of the mirror lens; produced a magnified but slightly distorted image Plane – the reflecting surface is on the back surface of the mirror lens; this type of surface is less easily scratched than a front surface mirror but produces a double or ‘ghost’ image

Probe �Used to evaluate the health of the periodontal tissue �Calibrations Certain millimeters may be indicted on the probe or each may be (1 -2 -3 -5 -7), or (1 -2 -3 -4 -5 -6) Color coded are marked in bands, each band being several millimeters (3 -5 mm) �Types: Calibrated probe – slender shape, blunt working end, millimeters, Furcation probe – Nabers probe – curved, blunt-tipped instrument used to detect and access bone loss in the furcation areas
Explorer � Assessment with a fine, flexible, wire-like working end � Types: Shepard hook – unpaired with short, highly curved shank and sharp point. Supra gingival only so not recommended for sub gingival calculus detection Straight explorer – unpaired with short lower shank and sharp point, not recommended for subgingival calculus detection Curved explorer – unpaired with curved shank and sharp point, examining normal sulci or shallow pockets Orban explorer – unpaired with straight lower shank, used in deep pockets with only slight tissue displacement, explorer tip is bent at 90 degrees to the terminal shank, subgingival calculus in anterior teeth or facial/lingual of posterior teeth Pigtail explorer – paired universal explorer with short broadly curved lower shank, detects calculus in normal sulci or shallow pockets 11/12 type explorer – paired universal with extended lower shank and tip bent at 90 degrees to terminal shank, adapts to most areas of the mouth – even deep or shallow pockets � Provides the best tactile information to the clinicians fingers, used to locate calculus, irregularities, defecting margins, etc. Design – the working end is 1 -2 mm in length and referred to as the tip, the SIDE of the tip is used to detect calculus Circular in cross section, the explorer may have paired or unpaired working ends
Periodontal File �Calculus removal used to prepare calculus deposits before removal with another instrument �Uses Preparation of burnished calculus Crushing of larger calculus deposits Smoothing an over extended or rough amalgam restoration �Design Cutting edges – multiple cutting edges at a 90 -105 degree angle to the lower shank Working end – thin with large circumference at base Area-specific – each working end is designed for use on single surface. Files with simple shanks work best on anterior teeth, complex shanks work best on posterior teeth � Limitations Only for enamel surfaces or outer surface of calculus deposits Do not adapt well to curved tooth surfaces
Universal Curet � One of the most frequently used debridement instrument � Supra gingivally and sub gingivally � Design Two cutting edges that have a rounded toe Back – rounded back is ideal for subgingival use Cross-section – semi-circular; lateral surfaces meet at the face at 70 -80 degrees Face – perpendicular to the lower shank so the cutting edges are level with each other; the cutting edge require the lower shank be tilted slightly toward the tooth surface to establish correct angulation Universal use – one double ended instrument can be applied to the tooth in anterior and posterior regions of the mouth � Limitations The toe is wider and may be more difficult to adapt beneath contact areas of anterior teeth The level cutting edges require the lower shank be tilted slightly towards the tooth for correct angulation � Uses Debridement of crown and roots Removal of small to medium sized calculus deposits
Area-Specific Curets � Debridement with one cutting edge; a set of curets is needed to perform procedures throughout the mouth � The curet is used supragingivally and subgingivally; especially for root surface debridement within periodontal pockets � Designs include area specific curets with miniature working ends, extended shanks, and flexible and rigid shanks � Design Cutting edge – one working cutting edge per working end; only the lower, longer cutting edge is used Back - rounded back, ideal for subgingival use Cross section – semi-circular, the lateral surfaces meet the instrument face at an internal angle between 70 -80 degrees Face – tilted at 60 -70 degree angle in relation to the lower shank, making one cutting edge (the working cutting edge) lower than the other; this tilted relationship makes the working cutting edge “self angulated” Area-specific – each working end is limited to use only on certain teeth and surfaces � Limitation The toe is wider than a pointed tip and is more difficult to adapt to anterior crowns Needing to exchange instruments more often � Uses Debridement of crown and root surfaces Removal of small deposits
Hand Instruments for Root Debridement

Characteristics �Treating clients with periodontal disease means needing longer shanks and miniature working ends for root concavities and furcation areas �Designs include area-specific curets with miniature working ends, extended shanks, flexible and rigid, and diamond coated working ends. �Instruments that are Diamond Coated Diamond coated instruments can be used to be remove light residual calculus Used with light and even pressure against the root surface �Modified Graceys – Gracey curets with extended shanks, miniature Gracey curets, and micro Gracey curets Design features include extended lower shank length, thinner working ends, and working ends that are shorter in length than in a standard Gracey.
Ergonomics
Operator Positioning �First, it is imperative that the hygienist is seated properly and the stool is correctly adjusted. �From an ergonomic standpoint, the operator stool is the most important chair in the treatment room. Its adjustment can profoundly impact posture and musculoskeletal health. �Positioning in the operatory should always begin with adjusting the operator stool first, then the patient. Ideally, the stool should be used by only one operator to prevent repeated adjustments. �Keep in mind that a stool is only ergonomic if it adjusts to fit your body size and shape.
Sitting � The sequence for adjusting a traditional operator stool is as follows: � Adjust the backrest height so the most convex portion (the lumbar support) nestles in your low-back curve. On most dental stools, there is no recognizable lumbar support. On these stools, adjust the backrest to a height where the shape fits most snugly against the curves of your back. � Move the backrest away from your back, which enables you to sit all the way back on the seat pan. � Check for appropriate size of the stool by placing three finger-widths behind your knee. � If the closest finger touches the seat, the seat pan is too deep, and you should select a stool with a shorter seat. � If your stool has a tilting mechanism, tilt the seat very slightly forward, only five to 15 degrees. � Adjust the height with your feet flat on the floor until your thighs slope slightly downward. Your weight should be evenly distributed in a tripod pattern: through each foot on the floor and through your buttocks. If, at the highest adjustment, your thighs are still parallel to the floor, you may need to order a tall cylinder from the manufacturer. � If the stool has armrests, adjust them one at a time to a height where the shoulder is not visibly elevated when compared with the opposite shoulder, yet the arm is fully supported.
Stools �Saddle stools are becoming increasing popular among dental hygienists, since they are very easy to move around the head of the patient, facilitate proper posture at the 9 o’clock position (see Figure 2), and are ideal for confined operatory spaces. �Because of its shape, it places the pelvis in a neutral position, so the spinal curves can more easily balance and also minimizes the need for backrest support. �addle stools are especially beneficial for shorter operators. By opening the hip angle, they allow lower positioning of the patient, and a more relaxed arm and shoulder posture. �Saddle stool height should be adjusted so the thighs slope downward at about a 45 -degree angle.
Client Positioning � Since the hygienist moves frequently around the head of the patient during treatment, they will ask the patient to rotate the head or tilt the chin during treatment to attain a line of sight that is perpendicular to the tooth surface. � Ideally, the patient should be positioned supine for treating the upper arch and semi-supine for the lower arch. However, in the real world, time constraints and practicality usually prevent the hygienist from such luxuries. � Therefore, it is recommended that the chair back be positioned so it is elevated 10 to 15 degrees from the floor (use the control of the patient chair to set this angle) and left in that position throughout the treatment. Proper orientation of the occlusal plane can then be achieved using a contoured dental neck cushion for treating the upper and lower arches. Ensure that the positioning aid is not too large, or it will be counterproductive, forcing the patient’s head forward. Many “dog-bone” pillows I have seen in operatories cause such positioning. � After reclining the chair, ask the patient to scoot to the end of the headrest. This is especially important if using a flat headrest — reaching or leaning over the “dead” headrest space can lead to a myriad of musculoskeletal dysfunctions. Often, this is not done in deference to the patient’s comfort — their spinal curves may not align properly with the patient chair support when scooted up all the way to the end of a headrest. This is easily resolved with dental ergonomic cushions that support the patient’s neck, low back, and knees.

Continued � When treating the upper arch, adjust the headrest so the occlusal plane of the upper jaw is about 15 to 20 degrees backward in relation to the vertical plane. You can check for proper positioning from the side, using an instrument handle to visualize the angle of the occlusal plane (see Figures 1 a, b). This angle is most easily attained with double-articulating headrests — by angling the headrest upward into the patient’s occiput. On flat headrests, use a contoured dental pillow with the large end under the patient’s neck, to angle the head back and chin higher. Then, adjust the height of the patient chair so forearms are parallel to the floor or sloping 10 degrees upward. 17 Whether using flat or double-articulating headrests, contoured memory foam cervical support cushions will make the patient much more tolerant to reclining. � In the 8 to 9 o’clock position, the hygienist can treat the upper posterior and anterior surfaces facing toward the hygienist, remembering to ask the patient to rotate their head to preserve their own best working posture. For example, ask the patient to turn their head slightly away when treating the upper right facial surfaces, and for the anterior facials, ask the patient to turn their head toward you. Sidesitting in the 8 to 9 o’clock position is one of the most damaging positions the hygienist can assume, and should be eliminated or minimized to avoid injury. This can lead to pain and musculoskeletal disorders in the hips, back, shoulders, neck, and arms. Always try to face the patient directly during treatment. A saddle stool can help greatly with gaining close proximity in the 8 to 9 o’clock position. � A majority of the upper arch should be treated from the 11 to 1 o’clock positions, using direct or indirect vision. Mirrors should be used whenever direct viewing of the oral cavity requires leaving neutral posture. One study revealed that more pain-free dental professionals use a mirror than those who did not use a mirror. 18 Frequent positioning at the 10 o’clock position without a mirror tends to encourage more arm abduction and neck/shoulder problems. 19 The hygienist must remember to reposition the delivery system when moving around the head of the patient. Hand pieces and instruments should be at about elbow level. Finger fulcrums are important to increase stability and to reduce compression in the carpal tunnel.
Positioning � As the hygienist moves around the patient, the overhead light must be repositioned to prevent shadowing. The light should parallel the hygienist’s line of sight to within 15 degrees. Thus, the light will be placed slightly behind and to one side of their head. To avoid repeated upward reaching for the light, the hygienist should consider a lightweight head-mounted light, which will parallel even more closely with the operator’s line of sight to prevent shadowing. Dr. Lance Rucker, professor and chairman of operative dentistry in the Department of Oral Health Sciences at the University of British Columbia has done valuable research in this area. For the upper arch, a mirror may be used to reflect light onto the surface. � When treating the lower arch, adjust the headrest so the occlusal plane of the lower arch is about 30 degrees elevated from the horizontal plane. On a double-articulating headrest, angle the headrest slightly forward, so the patient’s chin tilts downward. On flat headrests, reverse the position of a contoured dental cushion, so the large end is behind the head. It may be necessary to slightly lower the height of the patient chair so forearms are parallel to the floor or sloping 10 degrees upward. � Some hygienists may find that the chair does not adjust low enough to allow proper, relaxed arm posture. In this case, a saddle stool may be used to raise the hygienist to a higher seated position, since this places them between standing and sitting. � The hygienist should watch their wrists as they move to different quadrants to ensure a safe, neutral wrist posture. If the wrist is excessively flexed, a different clock position should be explored to enable a straight wrist posture. � With tight patient schedules, emergencies, and productivity goals to consider, it is easy to overlook proper patient positioning. However, taking the time to position the patient, hygienist, and equipment properly can not only have positive ramifications for the operator’s posture, comfort, and career longevity — it can also lead to better treatment and increased productivity.
Grasps
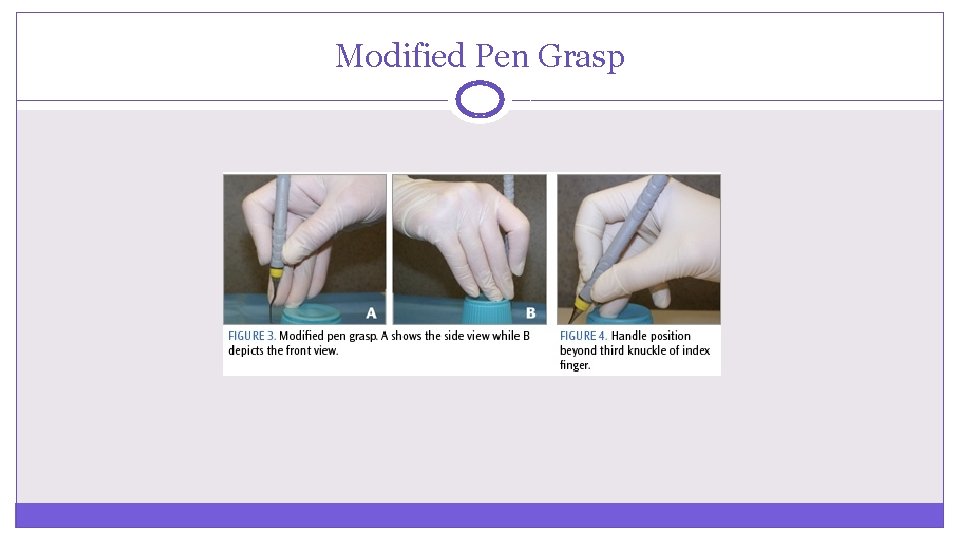
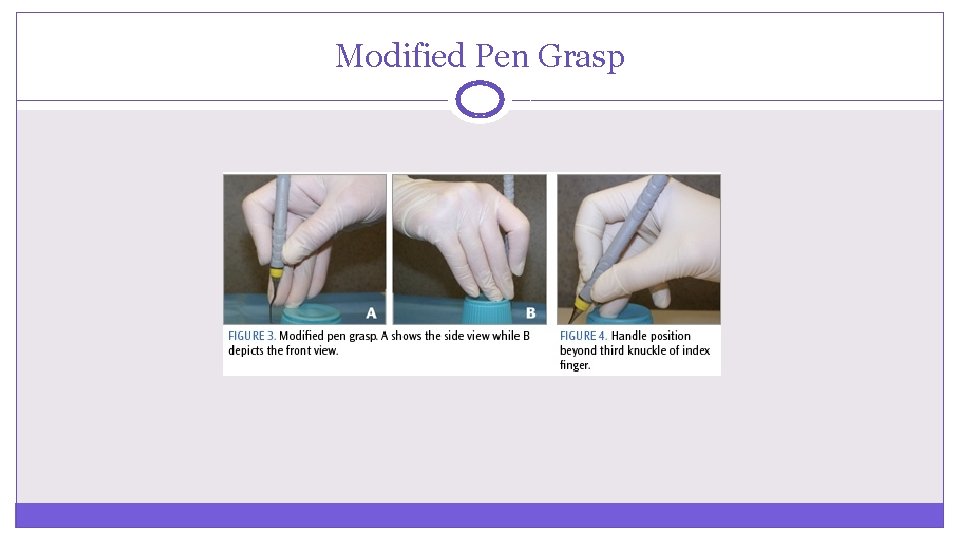
Modified Pen Grasp � The modified pen grasp is a variation of the pen grasp. Whereas a pen grasp varies from person to person, the modified pen grasp requires all clinicians to hold the instrument in a similar manner. The advantages of the modified pen grasp are better control of the instrument, prevention of finger fatigue, and an increase in tactile sensitivity. � Clinicians should notice placement of the thumb, index, and middle fingers as well as the relationship of the instrument handle to the second and third knuckles of the index finger. Maintaining a neutral position with the modified pen grasp requires modification based on wrist and forearm positioning. � In a modified pen grasp, the instrument is held in the dominant hand with the pads of the index finger and thumb opposite each other on the handle closest to the working end. The thumb and index finger are not touching, thereby creating a tripod effect with the middle finger that is placed along the shank of the instrument. This tripod effect balances the instrument in the clinician’s hand to provide stability and control. By keeping the index finger and thumb separated, the clinician can roll the instrument between these digits with ease and control. � The thumb is slightly curved in a c-shape, whereas the index finger is straight from the fingertip to the second knuckle. The index finger bends at the second knuckle, and the instrument handle rests somewhere between the second and third knuckle. If the index finger bends at the first knuckle, it may result in loss of wrist motion and strength for scaling.
Continued � When the clinician has difficulty maintaining a neutral wrist position, the handle of the instrument should be moved back toward the V in the hand or forward slightly in front of the second knuckle of the index finger. This range in positioning will produce a greater amount of flexibility for the operator to maintain a neutral position. The side pad near the fingernail of the middle finger is against the shank and serves to guide the instrument. The middle finger may bend at the second knuckle or can remain straight. � If the pad of the middle finger is placed on the shank, it results in ineffective pressure against the instrument and pulls the instrument too far forward of the second knuckle on the index finger, making it difficult to apply lateral pressure of the cutting edge against the root or tooth surface. The middle and ring finger should always remain in contact somewhere along the length of either finger. This contact ensures proper wrist motion and limits the amount of finger motion to activate the instrument
Modified Pen Grasp
Fulcrum � The fulcrum or finger rest serves as a stabilizing point for the instrument, prevents injury to the patient and operator, and enables the hand instrument to move as a single unit. The pad, specifically the lateral (outer) tip of the ring finger of the dominant hand, serves as the fulcrum finger. When activating the instrument, the clinician exerts downward pressure on the fulcrum finger and slightly squeezes the instrument with the index finger and thumb to increase stability and control during scaling while not causing patient discomfort. A flat finger fulcrum where the clinician uses the middle of the pad can hinder the maneuverability or pivot of the fulcrum finger, thereby limiting the ability to adapt, angle, and activate the instrument properly. General guidelines for an appropriate intraoral fulcrum include the placement of the ring finger on solid tooth surface in the same arch and close to the work area. � However, intraoral fulcrums can sometimes prevent the wrist and hand from maintaining a neutral position. In those situations, the clinician should adapt to an extraoral fulcrum so the hand, in particular the palm, can be slanted downward toward the pinkie finger. Extraoral fulcrums can help the clinician establish the correct instrument to tooth angulation while maintaining neutral positioning of the joints. 3 � The extraoral fulcrum shown in is ideal in the maxillary posterior region, where instrument angulation may be challenging. When using an extraoral fulcrum on the maxillary right facial quadrant (left facial for the left-handed clinician), the clinician places the back of the hand against the patient’s chin, with the nail side of the middle and ring fingers gently pressing against the face. The clinician’s palm is facing up.
Continued �Instrumentation on the left maxillary facial quadrant (right facial for the left- handed operator) requires a modified palm-down approach. This time, the pads of the middle and ring fingers are placed against the chin while light pressure is exerted against the face. Additionally, an extraoral fulcrum below the commissure of the lip can be used when seated at the 12: 00 position and instrumenting the mandibular anterior teeth. �The instrument grasp is one of several ergonomic components to consider when practicing dental hygiene. A poor grasp is most likely the cause of instrument problems. Good posture is the key to longevity in the practice of dental hygiene. Paying attention to head, neck, back, shoulder, and elbow positioning is critically important. It is never too late to revisit and learn new ergonomic principles that can lead to a long and successful career in dental hygiene.

Fulcrum
Grasp Pressure � The upper extremity musculoskeletal disorders most frequently experienced by dental hygienists are often caused by repetitive strain and cumulative trauma from high pinch forces of the grasp used in periodontal instrumentation. Inexperienced clinicians tend to exert consistently heavy pressure as they learn to control the instrument, but this can become a debilitating habit. In order to prevent injury, clinicians must be cognizant of the pressure used in their grasp. � Grasp pressure on the instrument handle changes according to the task at hand. Insertion, placement, and assessment strokes call for light pressure in order to maximize tactile sensitivity as the instrument tip or blade travels across the tooth or root surface. Surface vibrations transmitted to sensory nerves of the fingertips are heightened when an even, delicate pressure is used. This same light pressure is implemented to confirm the soft tissue attachment—whether probing, exploring, or preparing for a working stroke with a bladed instrument. � Working strokes require an increase in grasp pressure that should vary in intensity based on a deposit's bulk, degree of mineralization, and tenacity. The pressure exerted from the three grasp points— index finger, middle finger, and thumb—should also vary, as opposed to the even application used in a light-pressured assessment grasp. A working stroke requires force to be directed laterally toward the surface being instrumented. Once the placement stroke is made (light pressure) and soft tissue attachment confirmed, lateral pressure is applied prior to and during activation, then released at completion. The process is repeated for subsequent strokes: light pressure for placement, firm lateral pressure for the working stroke, followed by release.
Fulcrum Pressure and Stabilization �The type of fulcrum used, which provides a stabilizing point for the instrument, changes based on what area is being instrumented and the type of stroke needed. A fulcrum may be an intraoral finger rest or an extraoral hand rest, requiring light, moderate, or firm pressure. For example, extraoral fulcrums are preferred for the maxillary posterior region to facilitate proper angulation of the instrument and to help the operator maintain a neutral wrist position. �In terms of pressure, probing calls for light-pressured fulcrums whereas calculus removal requires firm pressure on the fulcrum—whether extraoral or intraoral.
Lateral Pressure and Burnishing � The goal of nonsurgical periodontal therapy is to produce a clean, hard root surface free of contaminants. � Partially scaled, burnished deposits create a microscopic biofilm niche that sustains infection in the soft tissue overlying the root. Burnishing occurs readily when instruments are dull, but even sharp instruments can burnish calculus on a root surface when insufficient lateral pressure is applied to the blade. When inadequate lateral pressure is used, small increments of deposit are shaved from its outermost surface, leaving the base layer of the calculus intact— smooth and burnished rather than cleanly removed. This may be one of the most common errors in periodontal therapy. � Returning maintenance patients who present with bleeding points invariably have burnished calculus on these surfaces, as evidenced by endoscopic studies.

Instrumentation � Grasp pressure and lateral pressure integrate in dynamic fluctuation during activation. The lateral pressure used to engage the blade against the deposit is regulated by the grasp and originates from the digits facing the surface to be treated, ie, the thumb, middle finger, index finger, combination of thumb and index finger, or index finger and middle finger, depending on the tooth surface being treated. Using this model prevents the three-point "death grip" grasp that contributes to musculoskeletal injury. � In order to maintain the correct adaptation, angulation, and pressure needed for a precisely controlled working stroke, while also protecting musculoskeletal health, clinicians must determine the appropriate body, arm, and wrist position; fulcrum; and grasp for the task at hand. To accomplish this, clinicians must first visualize the instrument's position against the tooth surface to determine which digits will provide the vector of force necessary for a good working stroke. This should then determine the position and fulcrum used.
Balancing Pressures � The relationship between the pressure used in the grasp and the fulcrum is often overlooked. A light-pressured grasp should be supported with a light-pressured fulcrum or hand rest. A moderate grasp with lateral pressure for biofilm debridement calls for a moderately- secure fulcrum pressure to stabilize the working stroke. Mineralized deposit removal requires strong lateral pressure for activation, and an equally strong fulcrum pressure. � Adequate lateral pressure must be used with calculus removal strokes, which need to be supported by equivalent pressure into the fulcrum—whether an intraoral finger rest or extraoral hand rest is used. 8 In other words, the lateral force directed into the tooth surface by the blade prior to activation must equal the force exerted by the fulcrum finger on a tooth or by the hand against the patient's extraoral soft tissue. Clinicians may be reluctant to apply firm extraoral hand rest pressure against the face of a patient. Without sufficient fulcrum force, however, the extraoral hand rest will lack the stability needed to control a working stroke for calculus removal. A wellcontrolled instrument is preferred to an unstable one that is slipping off the tooth surface. Stroke control on mineralized deposits is facilitated by lateral pressure that equals fulcrum pressure. The failure to balance these pressures will result in loss of stroke control. � Incorporating pressure dynamics into instrumentation helps clinicians improve instrumentation control and therapy outcomes, while also reducing the risk of injury. The correct application of force in both grasp and fulcrums takes careful consideration, but the extra time spent yields significant benefits for both clinicians and patients.

Strokes � Placement stroke – position the working end at the base of the sulcus or apical to calculus � Root debridement work strokes – 60 -70 degrees Light to moderate lateral pressure Lighter strokes of moderate length � Calculus removal – Angulation 70 -80 degrees Lateral pressure – firm to moderate Powerful and short strokes � Assessment strokes – used to evaluate the tooth surface or health of the tissue Used with probes, explorers, curets Angulation – 50 -70 degrees Lateral pressure – in contact with tooth surface; light pressure Character – fluid strokes of moderate length Number – many strokes used to cover the root surface

Stroke Direction �Multidirectional A combination of vertical, oblique, and horizontal strokes �Horizontal Perpendicular to the long axis of the tooth, used at the line angles of posterior teeth, furcations, and within narrow pockets �Oblique Diagonal to the long axis of the tooth, used mostly on facial and lingual surfaces �Vertical Parallel to the long axis of the tooth; used on facial, lingual, and proximal surfaces of anterior teeth and on the mesial and distal surfaces of posterior teeth
Stroke Characteristics �Length – short, powerful stroke for calculus removal; longer, lighter strokes for root debridement �Overlap – strokes could overlap to ensure complete removal; long ridges of calculus are treated in sections �Large calculus deposits should be removed in sections with a series of short, firm strokes Should NEVER be removed in layers because removing the outermost layer will leave a burnished surface

Calculus Removal � Adapting the cutting edge – If working subgingivally, close the face of the working end toward the tooth, and slide the working end to the junctional epithelium; use a light grasp while positioning the working end Adapt the toe-third of the cutting edge to the tooth surface Establish the instrument face-to-tooth surface angulation of 70 -80 degrees Fine-tune the grasp and the wrist position Stabilize the grasp, and apply lateral pressure Press down the ring finger against the finger rest Apply pressure against the instrument handle with the index finger and the thumb Activate a pulling stroke away from the JE Use hand-forearm activation for strength and control Activate pulling strokes in a coronal direction Use vertical and oblique strokes in most areas but horizontal strokes if needed Use short and powerful strokes for calculus removal and lighter strokes for root surface debridement Use overlapping strokes to ensure complete coverage
Probing Techniques
Probing �Probing is the act of walking the tip of a probe along the junctional epithelium within the sulcus or pocket for the purpose of assessing the health status of the periodontal tissues. Careful probing technique is essential if the information obtained with a periodontal probe is to be accurate. �THE WALKING STROKE is the movement of a calibrated probe around the perimeter of the base of a sulcus or pocket. Walking strokes are used to cover the entire circumference of the sulcus or pocket base. It is essential to evaluate the entire “length” of the pocket base because the junctional epithelium is not necessarily at a uniform level around the tooth. In fact, differences in the depths of two neighboring areas along the pocket base are common.
The Walking Stroke � Production of the Walking Stroke � 1. Walking strokes are a series of bobbing strokes that are made within the sulcus or pocket. The stroke begins when the probe is inserted into the sulcus while keeping the probe tip against the tooth surface. � 2. The probe is inserted until the tip encounters the resistance of the junctional epithelium that forms the base of the sulcus. The junctional epithelium feels soft and resilient when touched by the probe. � 3. Create the walking stroke by moving the probe up and down, in short bobbing strokes and forward in 1 -mm increments. With each down stroke, the probe returns to touch the junctional epithelium. � 4. The probe is not removed from the sulcus with each upward stroke. Repeatedly removing and reinserting the probe can traumatize the tissue at the gingival margin. � 5. The pressure exerted with the probe tip against the junctional epithelium should be between 10 and 20 grams. A sensitive scale that measures weight in grams can be used to standardize your probing pressure. � 6. Either wrist or digital (finger) activation may be used with the probe because only light pressure is used when probing.
Adaptation � ADAPTATION The side of the probe tip should be kept in contact with the tooth surface. The probe tip is defined as 1 to 2 mm of the side of the probe. � PARALLELISM The probe is positioned as parallel as possible to the tooth surface. The probe must be parallel in the mesiodistal dimension and faciolingual dimension. � Correct Adaptation. The probe tip is kept in contact with the tooth surface. � Incorrect Adaptation. The probe tip should not be held away from the tooth. � Probe Parallel to Long Axis. This probe is correctly positioned parallel to the long axis of the tooth. � Probe Not Parallel to Long Axis. This probe is incorrectly positioned in relation to the long axis of the tooth.

Interproximal Technique �When two adjacent teeth are in contact, a special technique is used to probe the area directly beneath the contact area. A two-step technique is used: �Step 1: Position the probe with the tip in contact with the proximal surface. While maintaining the tip in contact with the tooth surface, walk it between the teeth until it touches the contact area. The area beneath the contact area cannot be probed directly because the probe will not fit between the contact areas of the adjacent teeth. �Step 2: Slant the probe slightly so that the tip reaches under the contact area. The tip of the probe extends under the contact area while the upper portion touches the contact area. With the probe in this position, gently press downward to touch the junctional epithelium.
Charting Probing Depths � Probing depth measurements are recorded on a periodontal chart and become a permanent part of the patient chart. � 1. Six Sites Per Tooth. Probing depth measurements are recorded for 6 specific sites on each tooth: (1) distofacial, (2) facial, (3) mesiofacial, (4) distolingual, (5) lingual, and (6) mesiolingual � 2. One Reading Per Site. Only one reading per site is recorded. If the probing depths vary within a site, the deepest reading obtained in that site is recorded. For example, if the probing depths in the facial site were to range from 2 to 6 mm, only the 6 mm reading would be entered on the chart for that site. � 3. Full Millimeter Measurements. Probing depths are recorded to the nearest full millimeter. Round measurements to the next higher whole number; for example, a reading of 3. 5 mm is recorded as 4 mm, and a 5. 5 mm reading is recorded as 6 mm.
Technique �Stroke Technique. It is common for the depth of the pocket base to vary considerably from one spot to the next. What would happen if only one or two probing strokes were made on the facial surface of the tooth? �Record the Deepest Reading Per Site.

Positioning �The technique used for probing is different from that used with other periodontal instruments. For example, it is not necessary to use different clock positions when probing the anterior surfaces toward and away from your non dominant hand. �The diagrams on this page show the recommended clinician clock positions and a suggested sequence for probing the maxilla and mandible. This sequence is a logical one to follow as you probe the dentition and record the probing measurements on a periodontal chart.
Remember… � 1. Insert probe at the distofacial or distolingual line angle. � 2. Position the probe as parallel as possible to the long axis of the tooth surface being probed. � 3. Adapt the tip of the probe to the tooth surface as you activate short up-and-down strokes within the sulcus or pocket. Touch the junctional epithelium with each down stroke. � 4. Assess the area beneath the contact area by tilting the probe and extending the tip beneath the contact area. Press down gently to touch the junctional epithelium. � 5. Walk the probe around the entire circumference of the junctional epithelium using strokes that are about 1 mm apart. � 6. Use light stroke pressure, between 10 and 20 grams. � 7. Record 6 measurements per tooth (the deepest measurement in each of the 6 sites is recorded).
CAL � Another measurement of the extent of the periodontal support that is often reported, but is occasionally misinterpreted is the clinical attachment level (CAL). This is the measurement of the position of the soft tissue in relation to the cemento-enamel junction (CEJ) that is a fixed point that does not change throughout life, albeit at times it is hard to visualize (e. g. in case of abfraction lesions or chemical root erosions). � Two measurements are used to calculate the CAL: the probing depth and the distance from the gingival margin to the CEJ. � Where it gets confusing is that the gingival margin may be in one of three places: � 1. The CEJ may be coronal to the gingival margin. This is known as recession and is very simple to measure. � 2. The CEJ may be at the same level as the gingival margin. � 3. Occasionally, the gingival margin extends significantly over the CEJ making an accurate measurement quite difficult � Taken together, the probing depth plus the distance from the gingival margin to the CEJ comprises the clinical attachment level
P. S. R � CODE 0: • Color-coded reference mark is completely visible in the deepest sulcus or pocket of the sextant. � • No calculus or defective margins on restorations are present. � • Gingival tissues are healthy with no bleeding evident on gentle probing. � CODE 1: • Color-coded reference mark is completely visible in the deepest sulcus or pocket of the sextant. � • No calculus or defective margins on restorations are present. � • Bleeding IS present on probing. � CODE 2: • Color-coded reference mark is completely visible in the deepest sulcus or pocket of the sextant. � • Supragingival or subgingival calculus and/or defective margins are detected. � CODE 3: • Color-coded reference mark is partially visible in the deepest sulcus or pocket in the sextant. � • This code indicates a probing depth between 3. 5 and 5. 5 mm.
Codes Continued � CODE 4: • Color-coded reference mark is not visible in the deepest sulcus or pocket in the sextant. � • This code indicates a probing depth of greater than 5. 5 mm. � CODE *: The * symbol is added to the code of a sextant exhibiting any of the following abnormalities: furcation involvement, mobility, mucogingival problems, or recession extending into the colored area of the probe. Pictured here is an example of a sextant that has teeth with furcation involvement; therefore, the symbol should be recorded next to the sextant code. � CODE * Example: Recession This sextant exhibits gingival recession and mucogingival problems and therefore should include the * symbol next to the sextant code. � CODE * Example: Mucogingival Problems This sextant exhibits mucogingival problems and calculus and therefore should include the * symbol next to the sextant code.
Documenting P. S. R �Code Further Clinical Documentation �Code 0, 1, or 2 in all sextants No further documentation needed �Code 3 in one sextant Comprehensive periodontal assessment of sextant with 3 code �Code 3 in two or more sextants Comprehensive periodontal assessment of entire mouth �Code 4 in one or more sextants Comprehensive periodontal assessment of entire mouth
Furcation Probes �A furcation probe is a type of periodontal probe used to evaluate the bone support in the furcation areas of bifurcated and trifurcated teeth. � 1. Furcation probes have curved, blunt-tipped working-ends that allow easy access to the furcation areas. 2. Examples of furcation probes are the Nabers 1 N and 2 N. �Furcation Probes. Probe A has black bands from 3 to 6 mm and from 9 to 12 mm. Furcation probes with millimeter markings often are used in research studies. �The correct working-end of the probe has been selected if the lower (terminal) shank is positioned parallel to the tooth surface being examined. The incorrect working-end has been selected if the lower shank is perpendicular to the long axis of the tooth surface being examined.
Furcation Classes �Class I The concavity—just above the furcation entrance—on the root trunk can be felt with the probe tip; however, the furcation probe cannot enter the furcation area. �Class II The probe is able to partially enter the furcation—extending approximately one third of the width of the tooth— but it is not able to pass completely through the furcation. �Class III In mandibular molars, the probe passes completely through the furcation between the mesial and distal roots. �In maxillary molars, the probe passes between the mesiobuccal and distobuccal roots and touches the palatal root. �Class IV Same as a class III furcation involvement except that the entrance to the furcation is visible clinically owing to tissue recession.
Goals of Debridement �Periodontal health �Decreased pocket depths �Healthier host environment for maintenance of periodontal health �Removal of plaque biofilms and calculus �Eliminates bleeding �Increases effectiveness of client self care �Prevents recurrence of disease through supportive periodontal therapy
Endpoint of Instrumentation �The goal is to render the root surface and pocket space acceptable to tissue so that healing occurs �Tissue healing happens slowly, you need to wait at least 1 month to really determine the health of the tissue This is why a clients re-evaluation appointment is done 4 -6 weeks afterwards Probing, CAL, and bleeding should be looked at again Any areas not responsive to treatment will need to be deplaqued and calculus removed

Sharpening
Principles of Sharpening �Choose a stone appropriate for the instrument that needs to be sharpened. �Use a sterilized stone if you are sharpening during patient treatment. �Use the proper angle between the stone and the blade of the instrument. �Maintain a firm grasp of both the stone and the instrument keeping the entire surface of the blade even with the stone to produce a proper cutting edge. �Use up and down strokes finishing with a down stroke toward the cutting edge. �The angle between the face of the blade and the lateral surface of any curet is 70 -80 degrees for the most effective calculus removal.
Sharpening of Hand Instruments � � � � � Sharpening Universal Curets: • Lay the lateral surface of the curet on the stone at a 90 degree angle. • Open the angle by rotating the instrument 10 -20 degrees, laterally. The angle between the stone and the face of the blade is now 100 -110 degrees and perpendicular to the floor. • Start at the shank of the cutting edge and work toward the toe, using a consistent light pressure in an up and down motion and maintaining the correct angle, a metal sludge should appear on the face of the blade. • Test sharpness on a plastick. Once that end is sharp, the opposite can be sharpened the same way. Sharpening Gracey Curets: • Unlike a universal curet which has a straight cutting edge, Gracey curets are curved when viewed above the face of the blade. • Use the same technique as above with a few modifications. • Hold the face of the blade parallel to the floor; the Gracey curet has an offset blade. • The same angles apply, as above, now turn the instrument from shank to toe as you sharpen with up and down strokes, as not to flatten the blade and to keep the original rounded curvature of the blade. Sharpening Sickles: • Some sickles have entirely flat later surfaces the angle between the face of the blade and the stone will automatically be 100 -110 degrees. • Sharpen with short up-down stokes using a consistent light pressure keeping the stone in contact with the blade. • Look for the sludge check the sharpness.
Manual Sharpening � Instruments should be sharpened at the first sign of dullness. A sharpening work station incorporated into the dental hygiene treatment room allows clinicians to react quickly when instruments become dull. Several sets of sterile stones and test rods should be available so sharpening can be conducted quickly prior to seating patients and during treatment when an instrument may become noticeably dull. � Manual sharpening is an effective method for preserving instrument shape and contour. Stone selection should be based on the dullness of the instrument. Fine to medium stones are necessary for routine sharpening and a coarse stone is best for extremely dull cutting edges. A two-sided abrasive surface (medium on one side and fine on the other) is an efficient option. While some stones must be treated with water or oil, many do not require lubrication. � The stationary instrument/moving stone technique relies on the clock face for instrument positioning. While the instrument is held in the nondominant hand with the face of the blade parallel to the floor, the stone is held in the dominant hand initially placed at the 12 o'clock position and then moved to 1 o'clock or 11 o'clock to activate the sharpening stroke. By looking down onto the face of the instrument blade, the dental hygienist can visually see the contour of the cutting edge and closely follow it with the stone.
Automatic Devices � A variety of automated devices are available to sharpen instruments. When evaluating these products, consider the following: � 1. Does it sharpen the lateral sides of the blade or the face? Removing metal from the lateral side of the working end maintains the overall strength of the instrument, which, in turn, prolongs its service life. 1 � 2. Can instruments with curved blades be moved in a pendulum-like motion across the stone to maintain the curvature? Maintaining the original shape of the instrument is just as important as having a sharp cutting edge. � 3. Are the instructions easy to understand? The directions must be followed carefully to avoid altering the design of scaling instruments.
Continued �A honing machine is one example of an automated sharpening device. It can be a bench-type or smaller battery-operated piece of equipment that follows the principles of instrument preservation. �Specially designed honing disks are mounted on top of the machine, and rotate up to 7, 000 rpm. These devices will remove metal from either the face or lateral sides of the blade as the clinician controls the pressure. If the metal is being removed from the lateral sides of the cutting edge, the dental hygienist must be able to maintain the pendulum-like motion from heel to toe to preserve the gentle curve of the Gracey cutting edge or the flame-shaped cutting edge of some sickles. In addition, clinicians must be confident in instrument positioning and application of pressure.
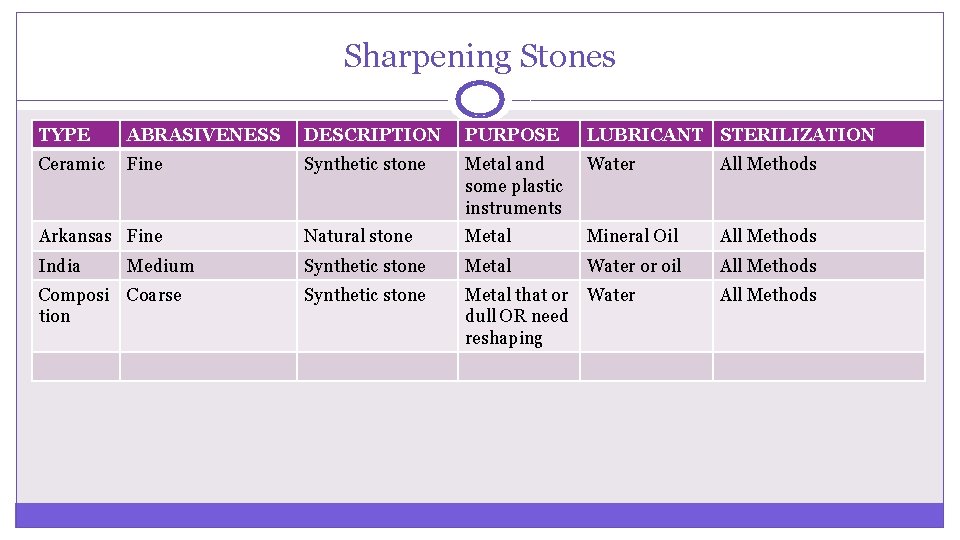
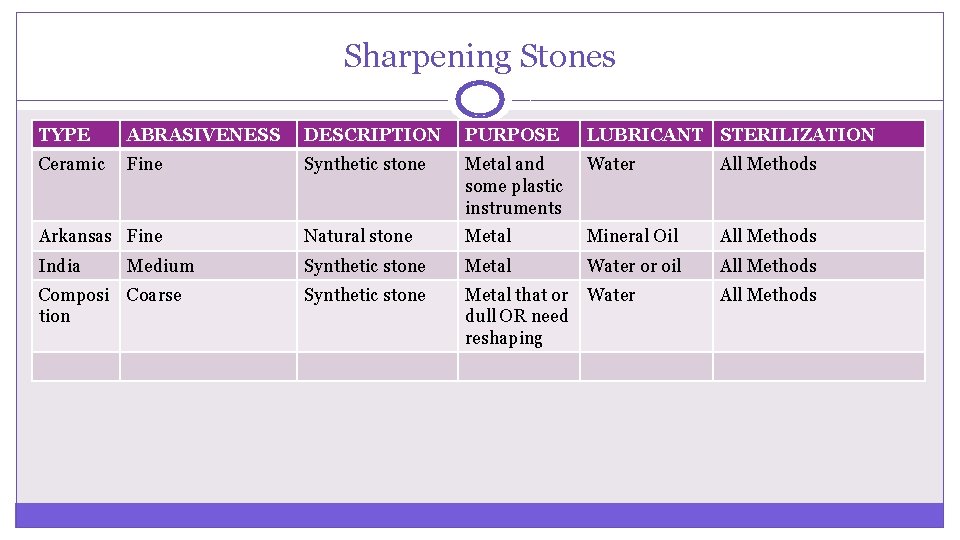
Sharpening Stones TYPE ABRASIVENESS DESCRIPTION PURPOSE LUBRICANT STERILIZATION Ceramic Fine Synthetic stone Metal and some plastic instruments Water All Methods Arkansas Fine Natural stone Metal Mineral Oil All Methods India Medium Synthetic stone Metal Water or oil All Methods Composi tion Coarse Synthetic stone Metal that or Water dull OR need reshaping All Methods
 Cdha membership
Cdha membership Campus portal keiser university
Campus portal keiser university Dental hygienist advancement opportunities
Dental hygienist advancement opportunities Dentalelle
Dentalelle Dentalelle
Dentalelle Active instruments examples
Active instruments examples Straight chisel dental use
Straight chisel dental use Dycal applicator function
Dycal applicator function The three specific parts of hand instruments are the
The three specific parts of hand instruments are the Part of a dental instrument that the operator grasps.
Part of a dental instrument that the operator grasps. Tutoring
Tutoring Chinese tutoring
Chinese tutoring Tutoring definicja
Tutoring definicja Wise ant tutoring
Wise ant tutoring Media hopper replay
Media hopper replay Tutoring
Tutoring Cdli tutoring
Cdli tutoring Small group tutoring
Small group tutoring Uri advising by major
Uri advising by major Connective tutoring
Connective tutoring Bcc tutoring
Bcc tutoring Scholarly tutoring
Scholarly tutoring The tutoring cycle
The tutoring cycle Ksu ccse fye
Ksu ccse fye Small group tutoring
Small group tutoring Msi tutoring ucsc
Msi tutoring ucsc Rpi alac tutoring
Rpi alac tutoring Msu smarty cats
Msu smarty cats Tutoring čechy
Tutoring čechy Accuplacer tutoring
Accuplacer tutoring Stanford vptl tutoring
Stanford vptl tutoring Tutoring shawlands
Tutoring shawlands Tutoring cycle
Tutoring cycle Big bang theory math
Big bang theory math Mutuo insegnamento pedagogia
Mutuo insegnamento pedagogia Uri aec tutoring
Uri aec tutoring Istituto leonardo da vinci parigi
Istituto leonardo da vinci parigi Uci antplanner
Uci antplanner Tutoring
Tutoring Tutoring
Tutoring Kindergarten tutoring
Kindergarten tutoring Aspire tutoring
Aspire tutoring Wise tutoring
Wise tutoring Tryck formel
Tryck formel Presentera för publik crossboss
Presentera för publik crossboss Rådet för byggkompetens
Rådet för byggkompetens Vad är densitet
Vad är densitet Kung som dog 1611
Kung som dog 1611 Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Tack för att ni har lyssnat
Tack för att ni har lyssnat Smärtskolan kunskap för livet
Smärtskolan kunskap för livet Referatmarkeringar
Referatmarkeringar Epiteltyper
Epiteltyper Trög för kemist
Trög för kemist Karttecken brunn
Karttecken brunn Uppställning multiplikation
Uppställning multiplikation Delegerande ledarstil
Delegerande ledarstil Blomman för dagen drog
Blomman för dagen drog Elektronik för barn
Elektronik för barn Underlag för särskild löneskatt på pensionskostnader
Underlag för särskild löneskatt på pensionskostnader Borra hål för knoppar
Borra hål för knoppar Bris för vuxna
Bris för vuxna Mat för unga idrottare
Mat för unga idrottare Ledarskapsteorier
Ledarskapsteorier Teckenspråk minoritetsspråk argument
Teckenspråk minoritetsspråk argument Humanitr
Humanitr