INNERVATION OF THE TONGUE NERVE SUPPLY OF TONGUE
- Slides: 35
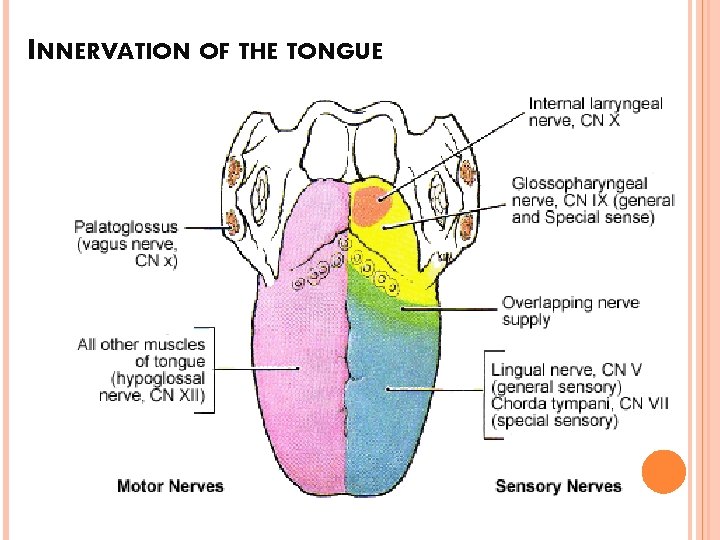
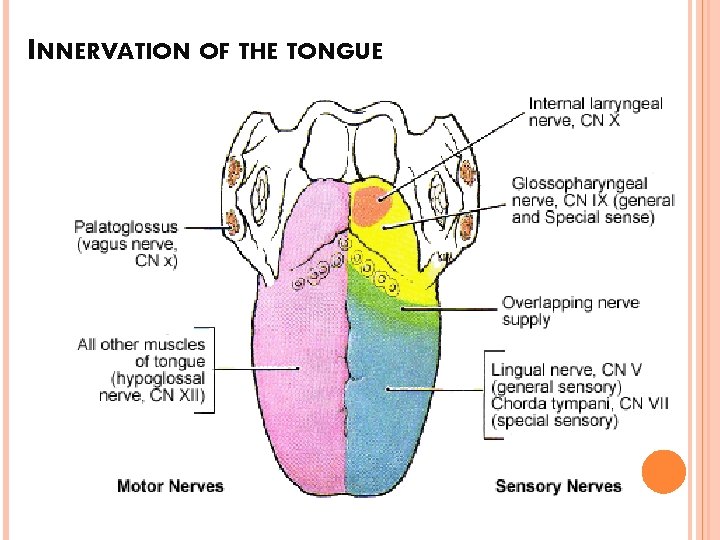
INNERVATION OF THE TONGUE
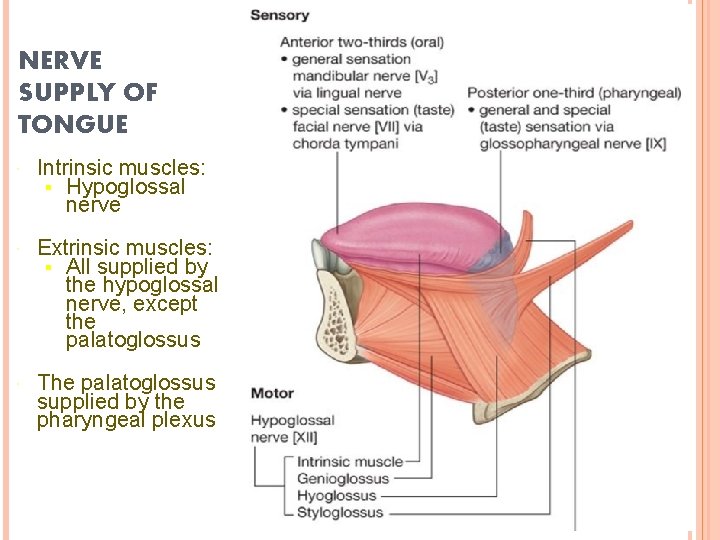
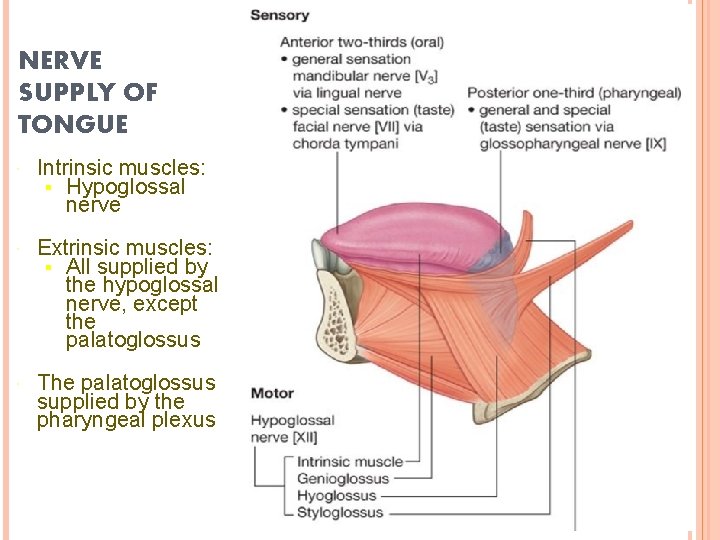
NERVE SUPPLY OF TONGUE Intrinsic muscles: § Hypoglossal nerve Extrinsic muscles: § All supplied by the hypoglossal nerve, except the palatoglossus The palatoglossus supplied by the pharyngeal plexus
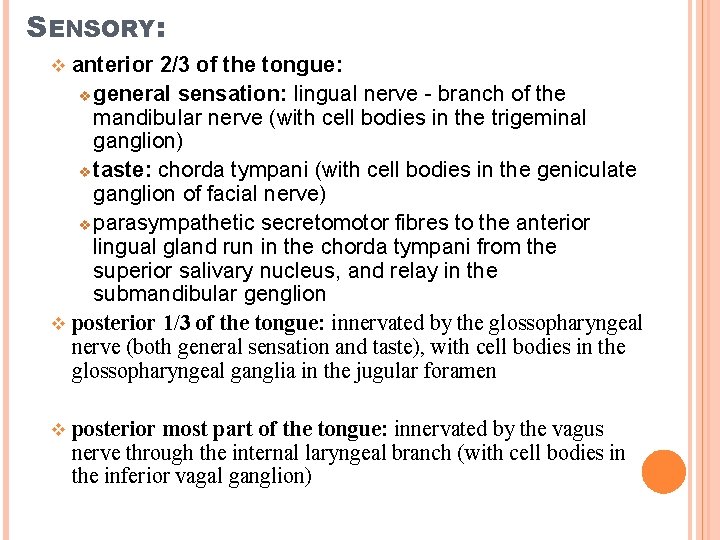
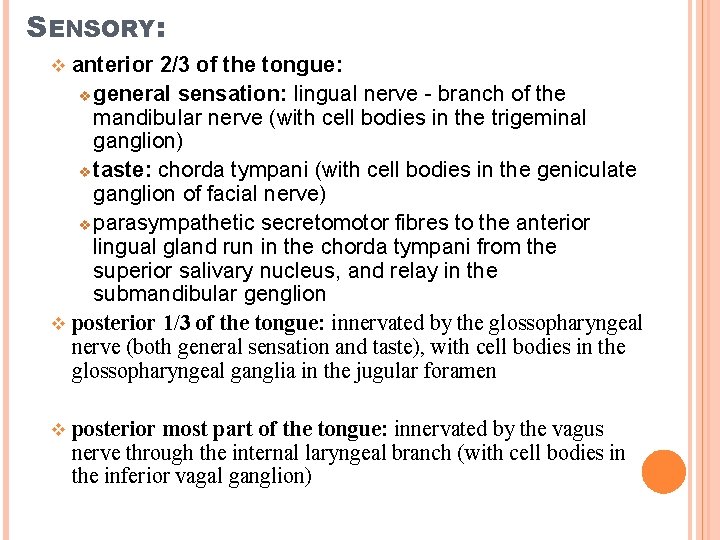
SENSORY: anterior 2/3 of the tongue: v general sensation: lingual nerve - branch of the mandibular nerve (with cell bodies in the trigeminal ganglion) v taste: chorda tympani (with cell bodies in the geniculate ganglion of facial nerve) v parasympathetic secretomotor fibres to the anterior lingual gland run in the chorda tympani from the superior salivary nucleus, and relay in the submandibular genglion v posterior 1/3 of the tongue: innervated by the glossopharyngeal nerve (both general sensation and taste), with cell bodies in the glossopharyngeal ganglia in the jugular foramen v v posterior most part of the tongue: innervated by the vagus nerve through the internal laryngeal branch (with cell bodies in the inferior vagal ganglion)
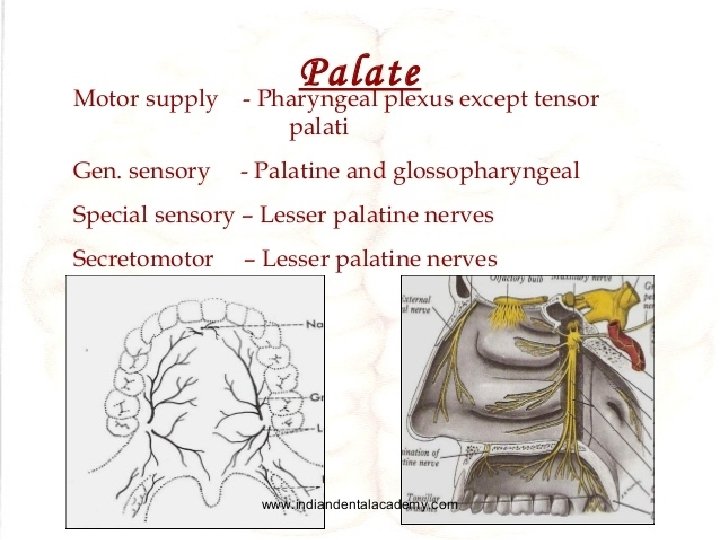
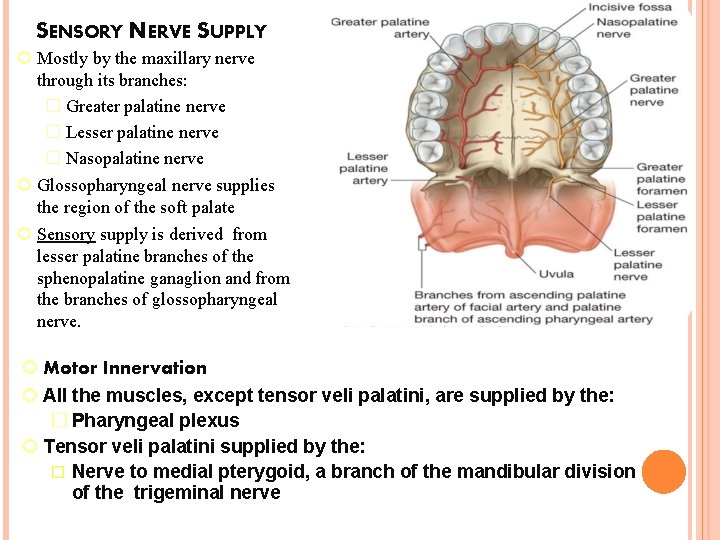
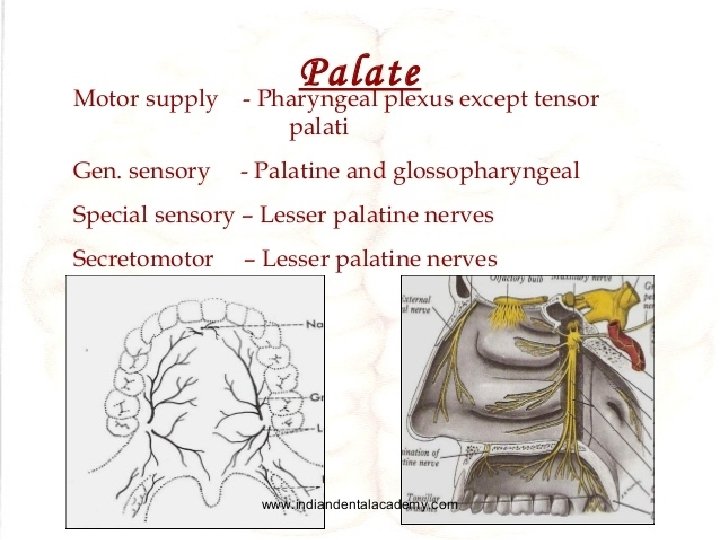
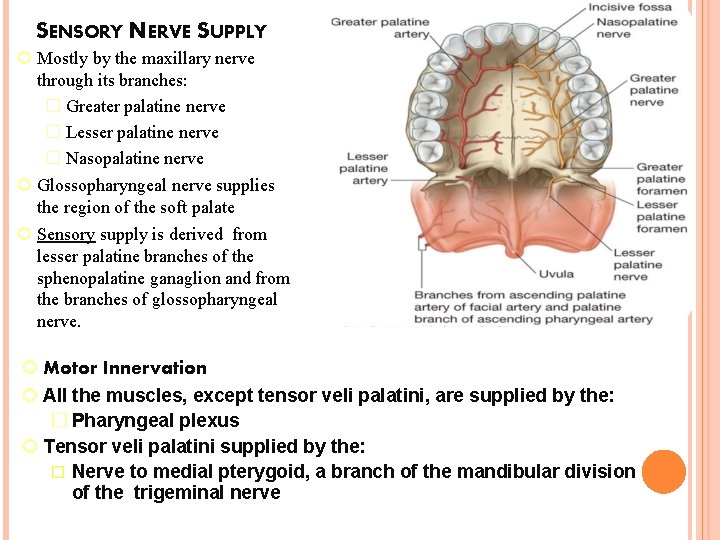
SENSORY NERVE SUPPLY Mostly by the maxillary nerve through its branches: � Greater palatine nerve � Lesser palatine nerve � Nasopalatine nerve Glossopharyngeal nerve supplies the region of the soft palate Sensory supply is derived from lesser palatine branches of the sphenopalatine ganaglion and from the branches of glossopharyngeal nerve. Motor Innervation All the muscles, except tensor veli palatini, are supplied by the: � Pharyngeal plexus Tensor veli palatini supplied by the: � Nerve to medial pterygoid, a branch of the mandibular division of the trigeminal nerve
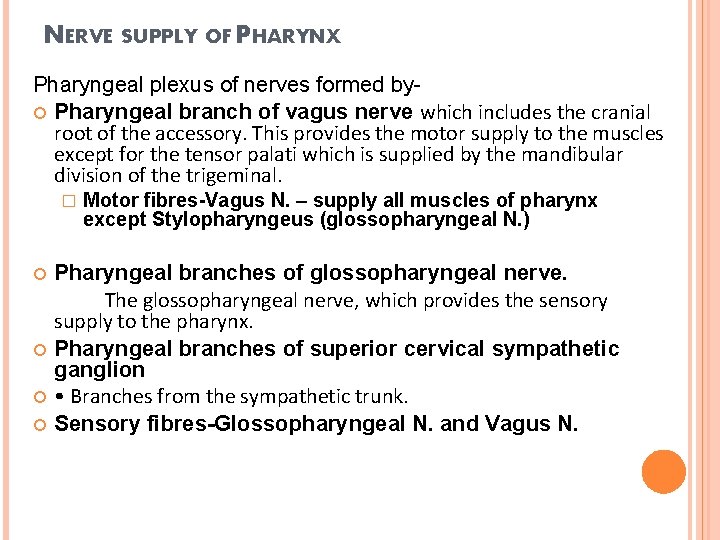
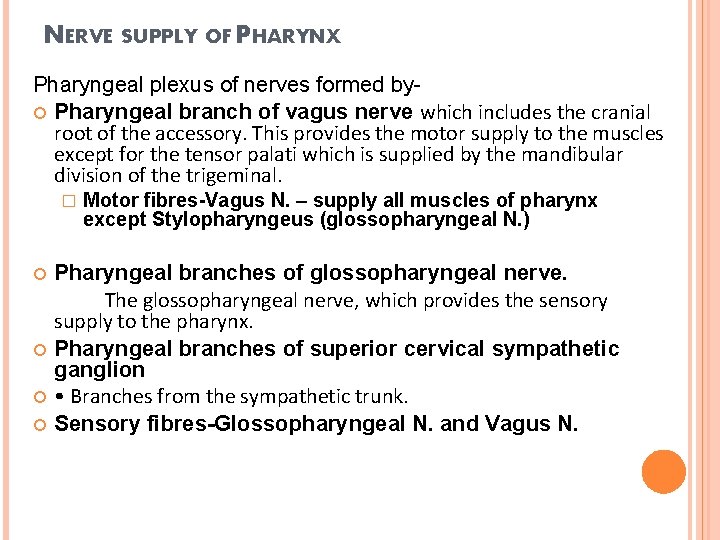
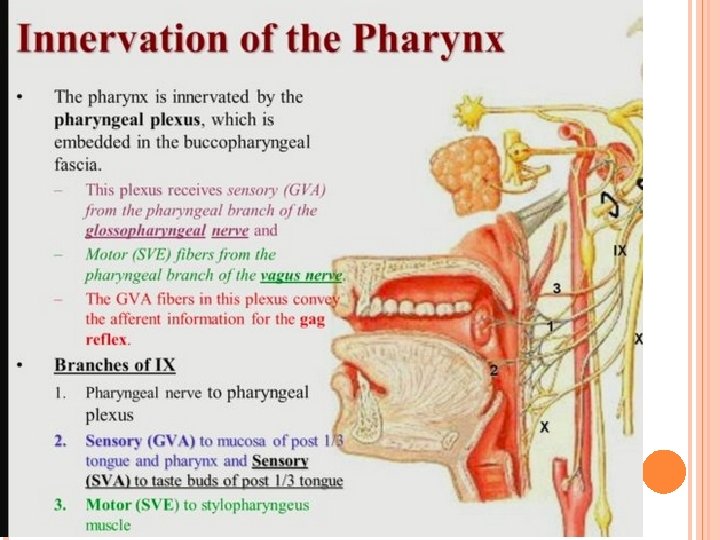
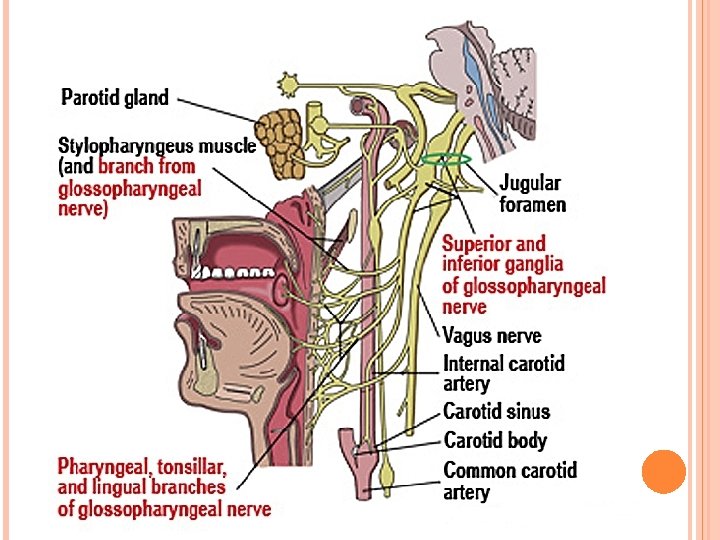
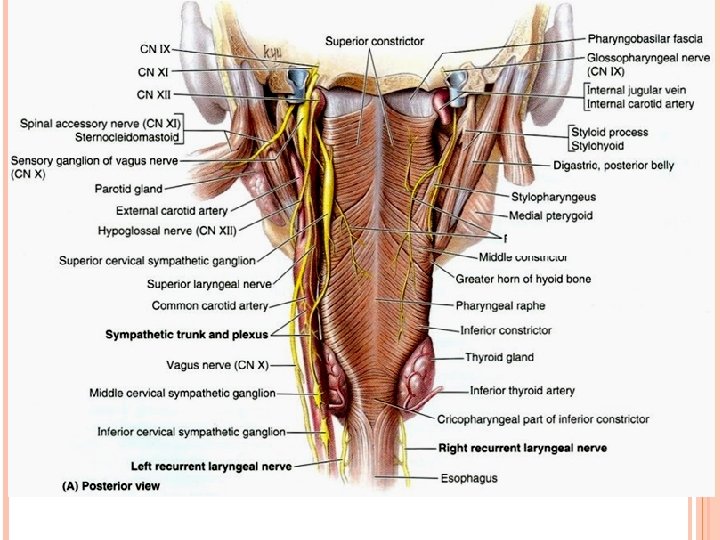
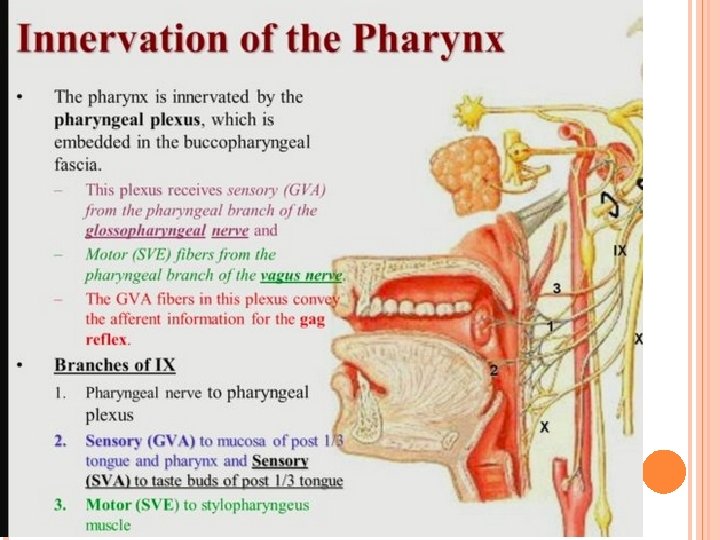
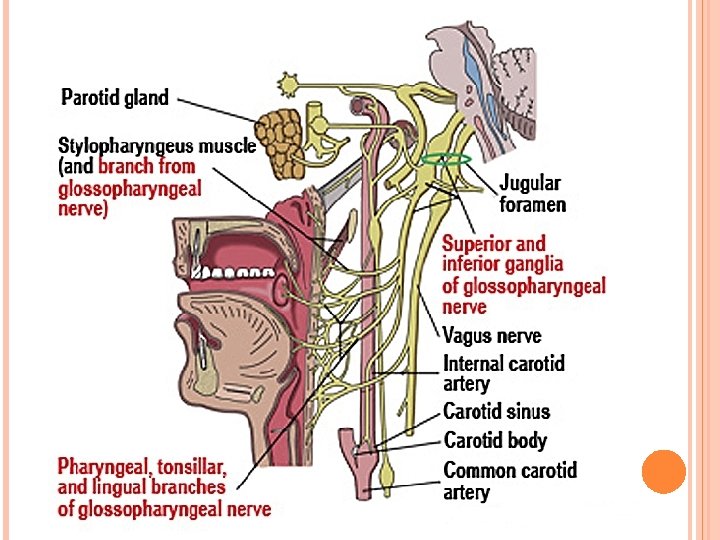
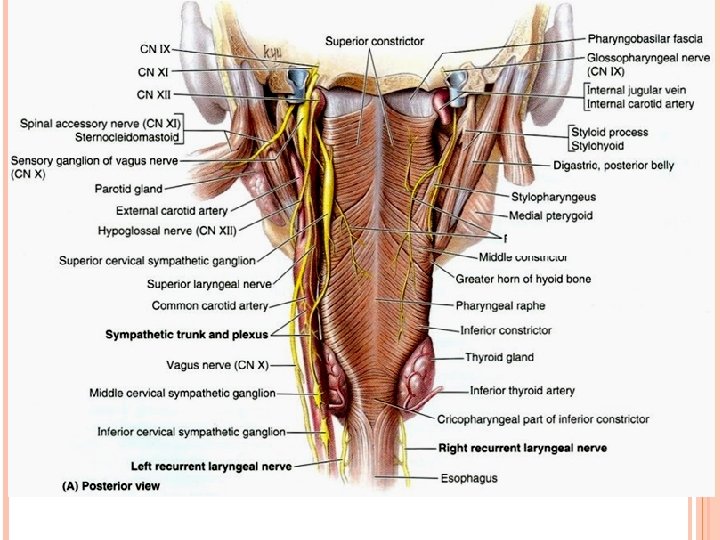
NERVE SUPPLY OF PHARYNX Pharyngeal plexus of nerves formed by Pharyngeal branch of vagus nerve which includes the cranial root of the accessory. This provides the motor supply to the muscles except for the tensor palati which is supplied by the mandibular division of the trigeminal. � Motor fibres-Vagus N. – supply all muscles of pharynx except Stylopharyngeus (glossopharyngeal N. ) Pharyngeal branches of glossopharyngeal nerve. The glossopharyngeal nerve, which provides the sensory supply to the pharynx. Pharyngeal branches of superior cervical sympathetic ganglion • Branches from the sympathetic trunk. Sensory fibres-Glossopharyngeal N. and Vagus N.
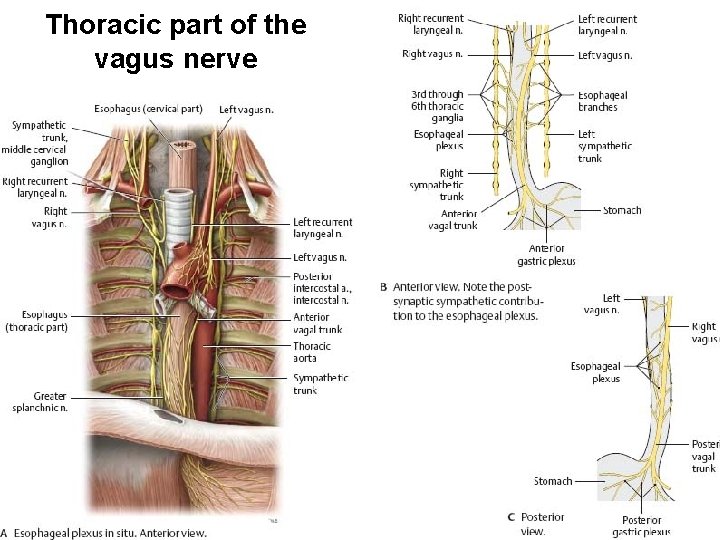
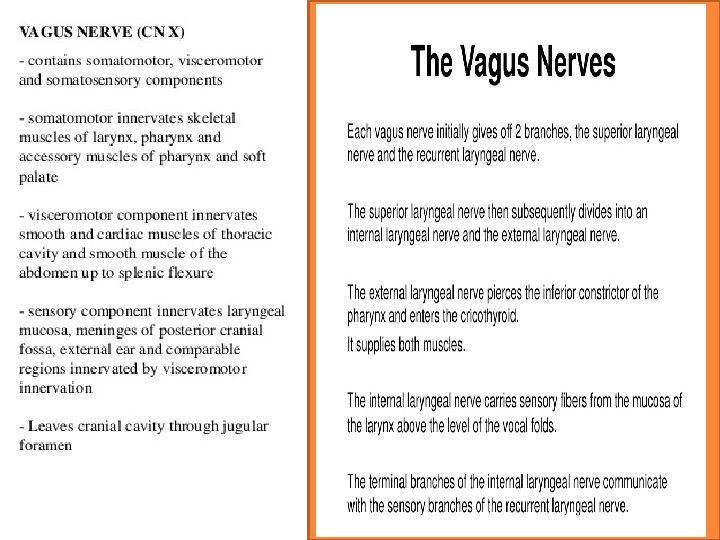
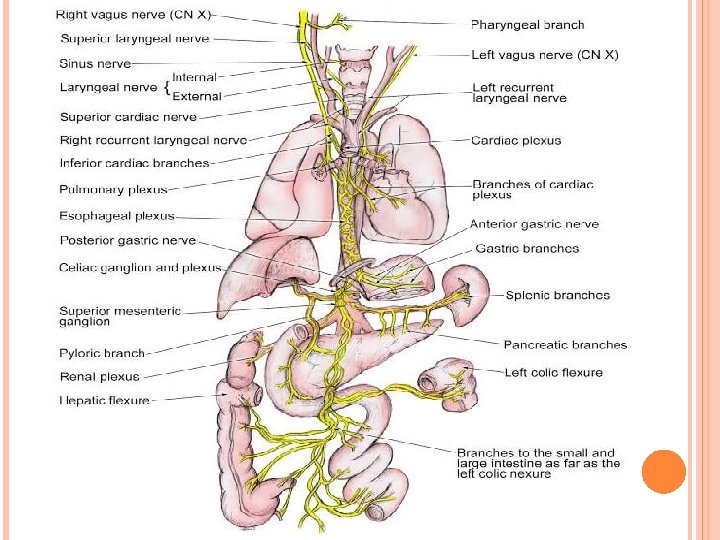
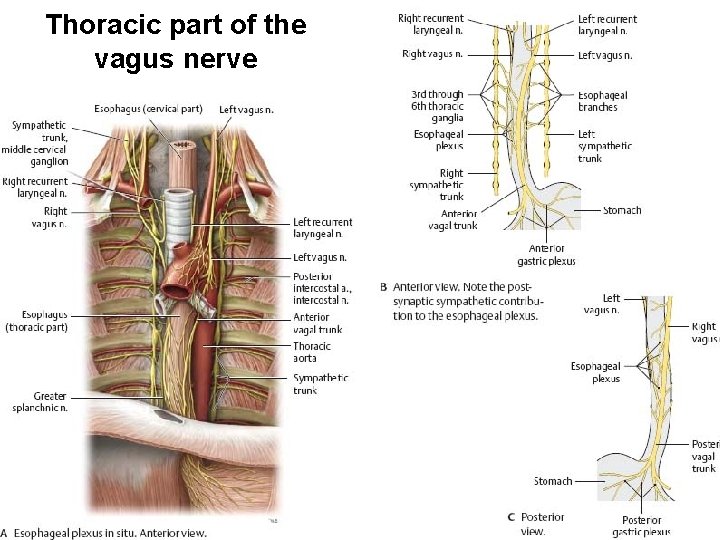
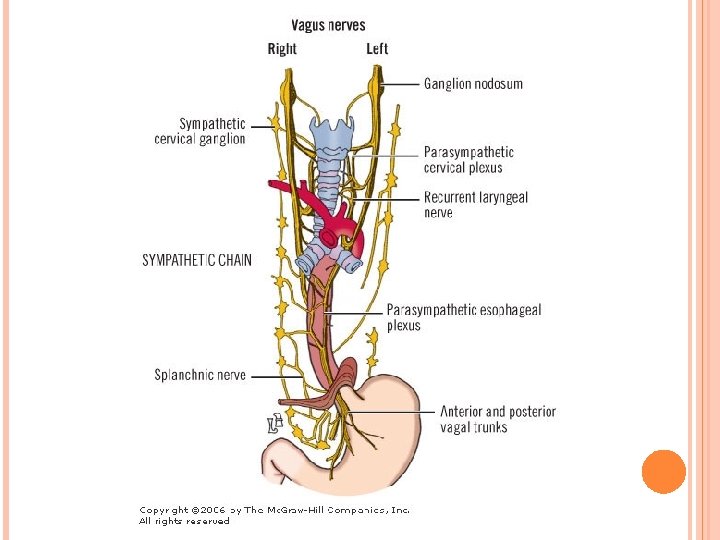
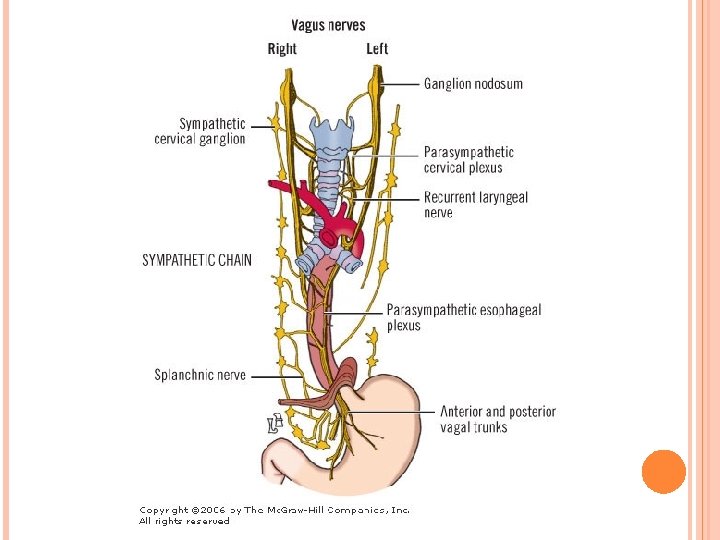
Thoracic part of the vagus nerve
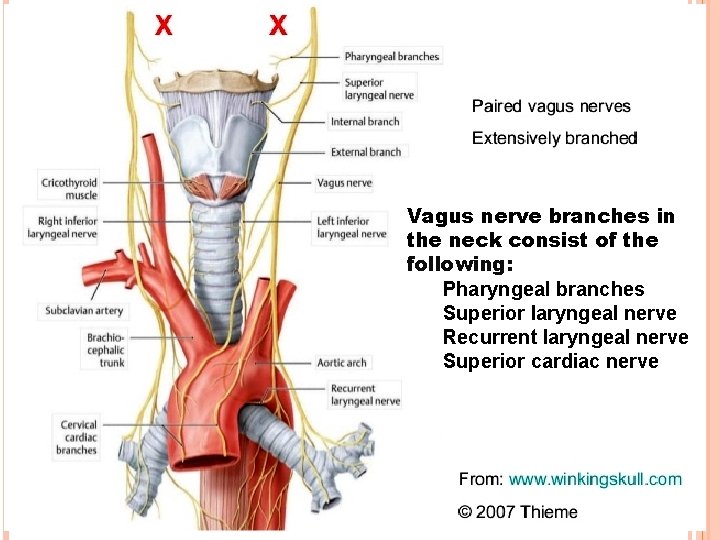
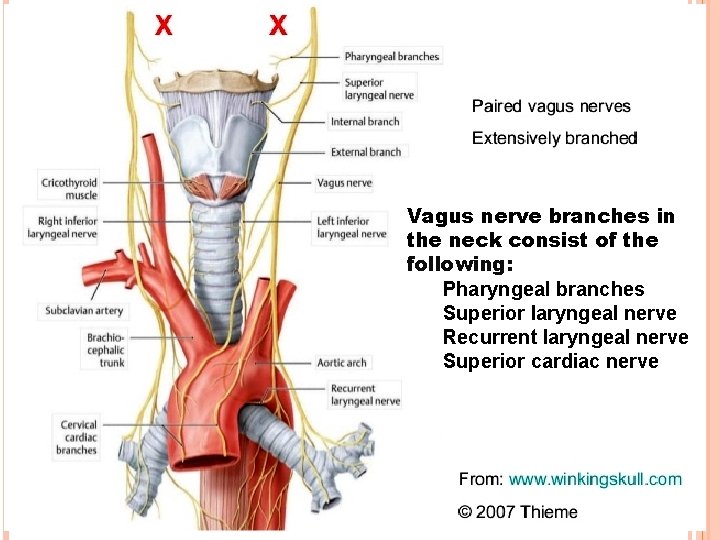
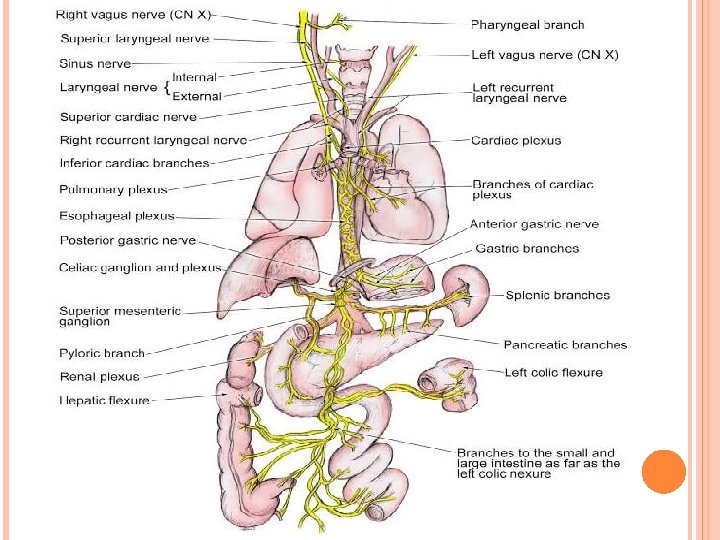
Vagus nerve branches in the neck consist of the following: Pharyngeal branches Superior laryngeal nerve Recurrent laryngeal nerve Superior cardiac nerve
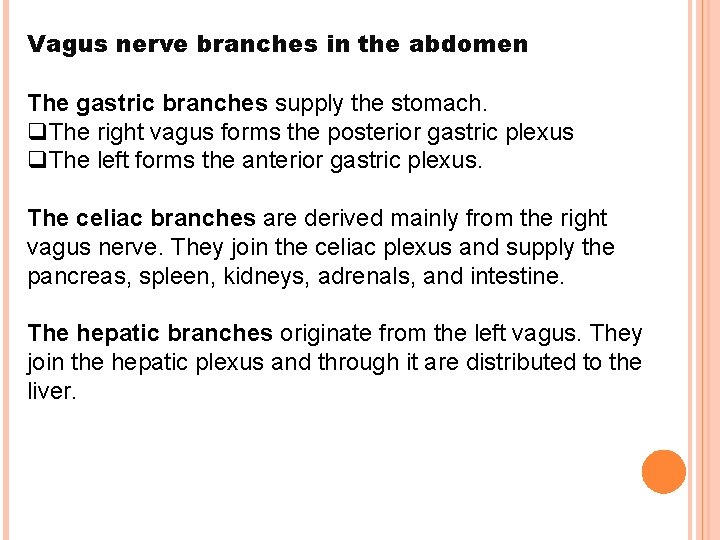
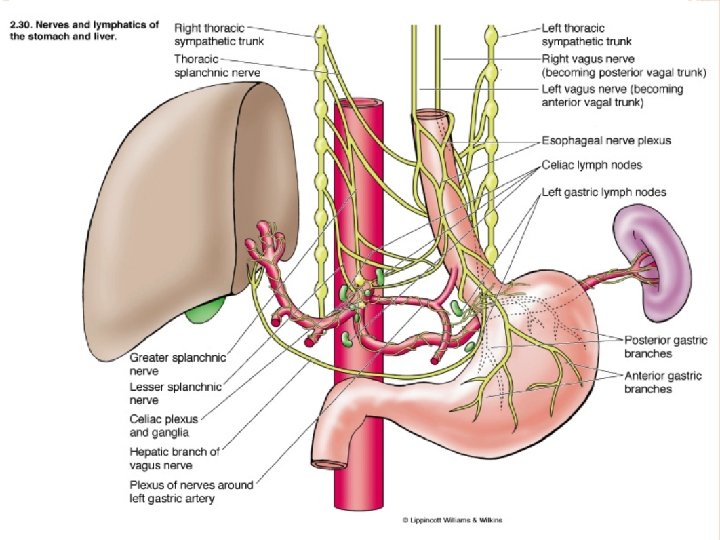
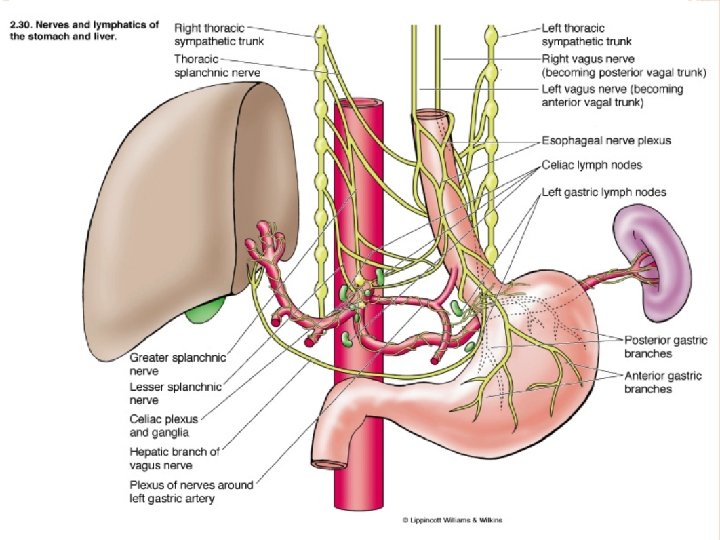
Vagus nerve branches in the abdomen The gastric branches supply the stomach. q. The right vagus forms the posterior gastric plexus q. The left forms the anterior gastric plexus. The celiac branches are derived mainly from the right vagus nerve. They join the celiac plexus and supply the pancreas, spleen, kidneys, adrenals, and intestine. The hepatic branches originate from the left vagus. They join the hepatic plexus and through it are distributed to the liver.
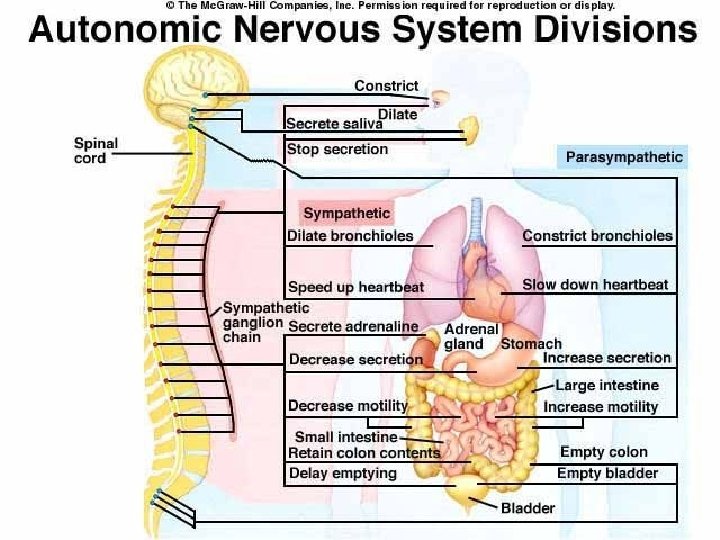
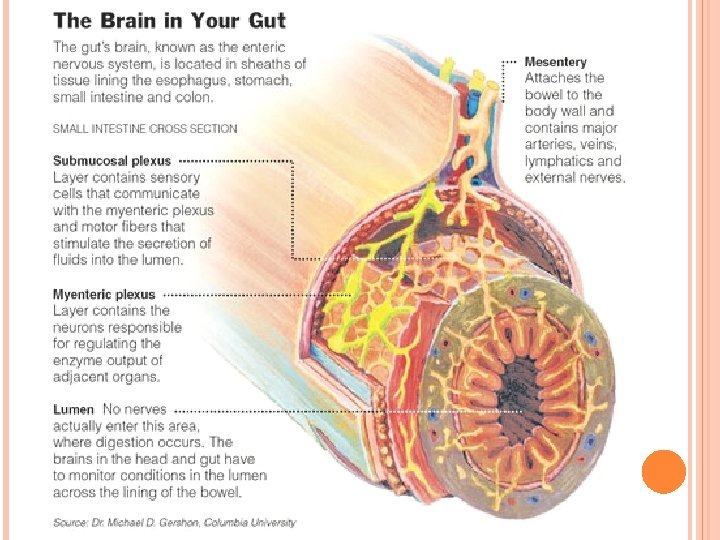
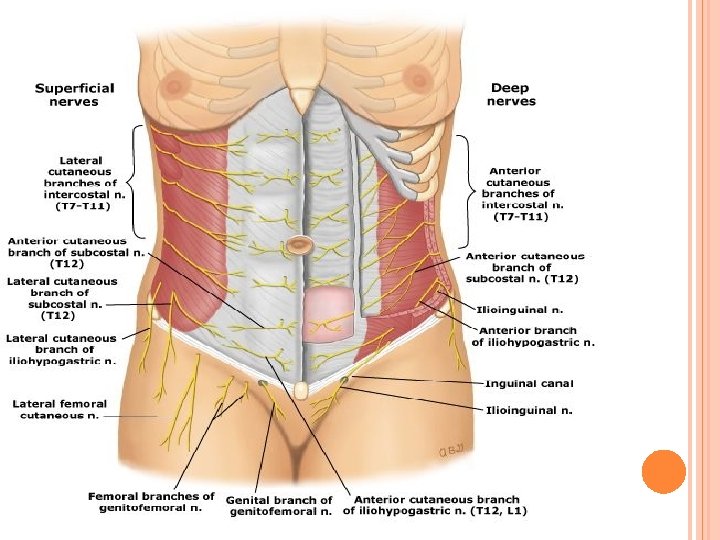
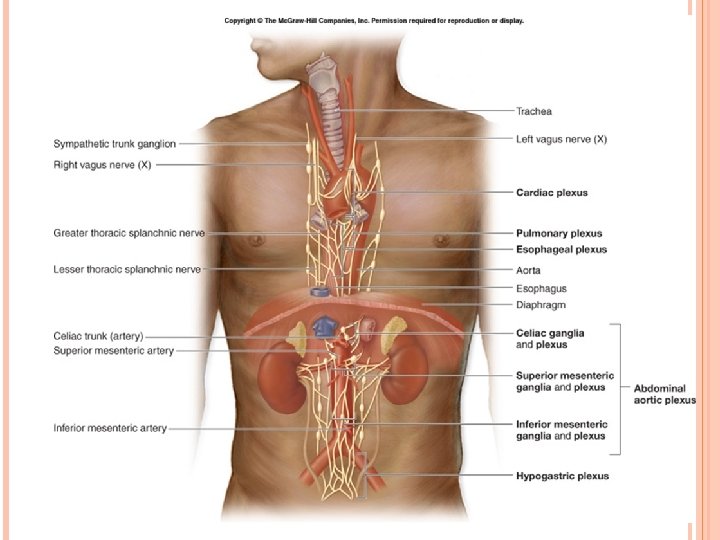
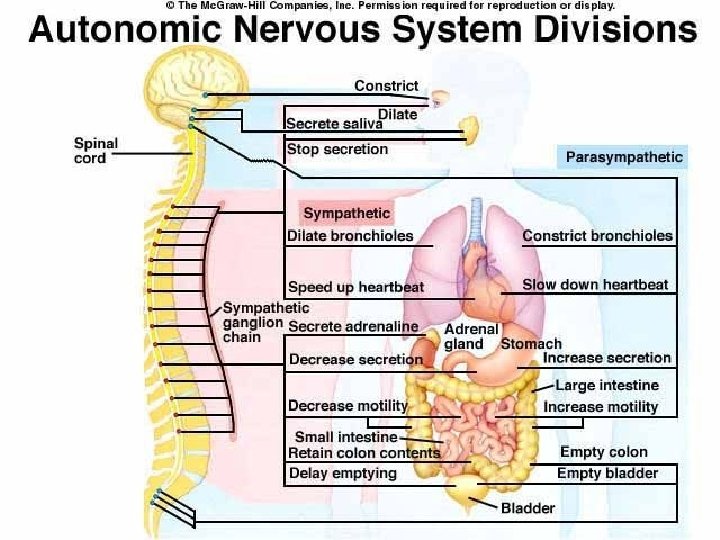
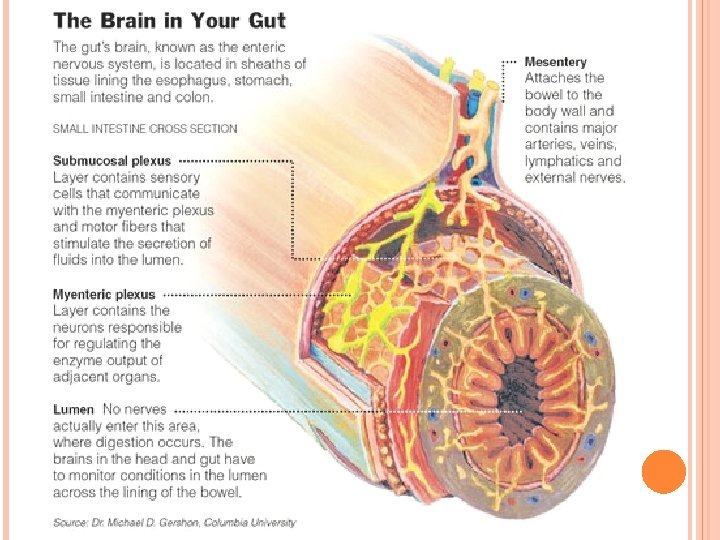
The abdominal viscera are innervated by the autonomic nervous system. The parasympathetic innervation is delivered by the vagus primarily, with help from the pelvic splanchnic nerves. The sympathetic innervation comes primarily from the thoracic splanchnic nerves, greater, lesser, and least, with help from the upper lumbar splanchnic nerves. Generally, parasympathetic innervation results in digestion, by stimulating peristalsis in the gut and secretion by associated glands. Sympathetic innervation, on the other hand, decreases blood flow to the abdominal viscera and inhibits digestion. Blood flow is diverted to the trunk and limbs, to aid the body in "fight or flight".
THE SYMPATHETIC NERVOUS SYSTEM The central part of the sympathetic system is located in the lateral horns of the spinal cord between the level of C 7 and Th 1 -L 3 in the intermediolateral nucleus. � It give rise to fibres innervating the smooth muscles of the viscera and the sensory organs (eyes), and the glands. Vasomotor, pilomotor and respiration centres are also located here. The peripheral part of the sympathetic system is formed by two symmetrical right and left sympathetic trunks stretching on either side of the spinal from the base of the skull to the coccyx where the caudal ends of both trunks meet to form a single common ganglion
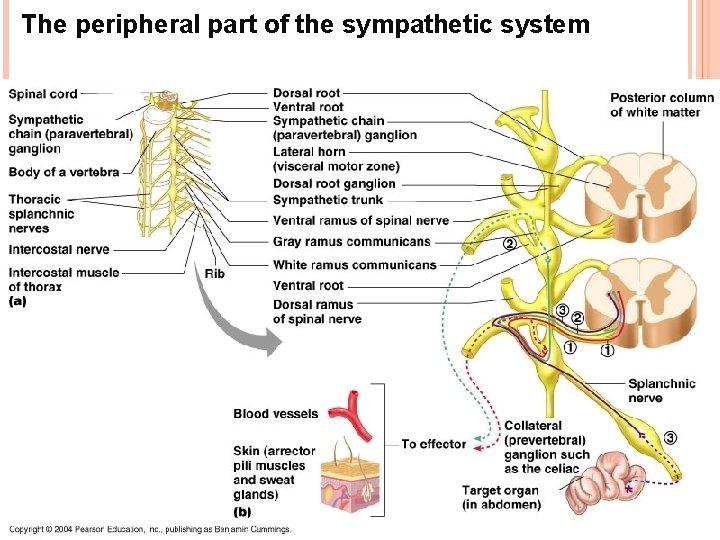
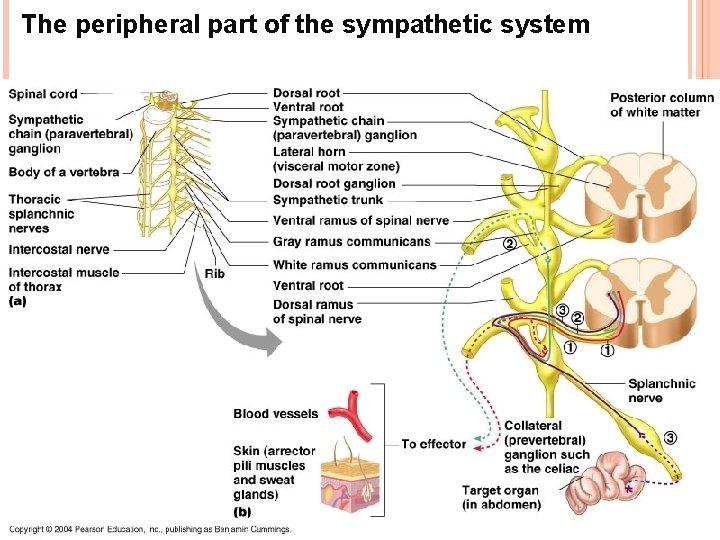
The peripheral part of the sympathetic system
Each sympathetic trunk is composed of a series of nerve ganglia of the first order connected by longitudinal interganglionic branches that consist of nerve fibres. The processes of cells located in the lateral horns of the thoracolumbar part of the spinal cord emerge from it through the anterior roots and pass in the white communicating branches to the sympathetic trunk. From the white communicating branches the processes of the cells join by means of synapsis with the cells of the sympathetic trunk ganglia or pass through the ganglia without interruption and reach one of intermediate ganglia. This is the preganglionic pathway. From the ganglia of the sympathetic trunk or from the intermediate ganglia arise non-medullated fibres of the postganglionic pathways and pass to the blood vessels and viscera.
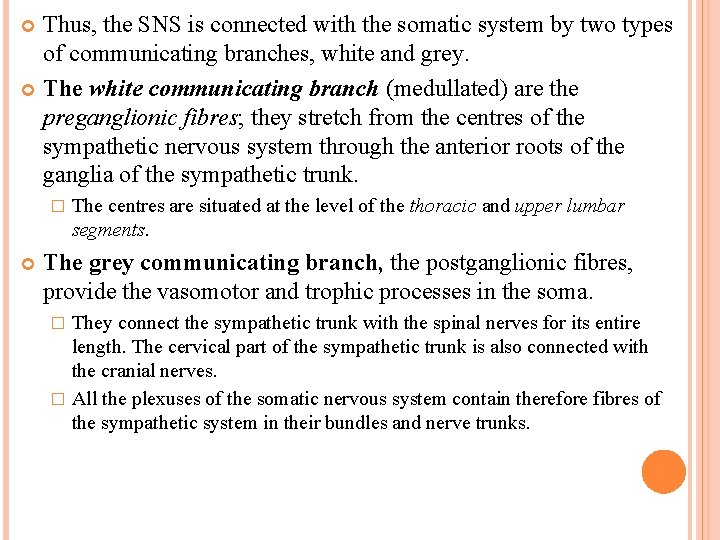
Thus, the SNS is connected with the somatic system by two types of communicating branches, white and grey. The white communicating branch (medullated) are the preganglionic fibres; they stretch from the centres of the sympathetic nervous system through the anterior roots of the ganglia of the sympathetic trunk. � The centres are situated at the level of the thoracic and upper lumbar segments. The grey communicating branch, the postganglionic fibres, provide the vasomotor and trophic processes in the soma. They connect the sympathetic trunk with the spinal nerves for its entire length. The cervical part of the sympathetic trunk is also connected with the cranial nerves. � All the plexuses of the somatic nervous system contain therefore fibres of the sympathetic system in their bundles and nerve trunks. �
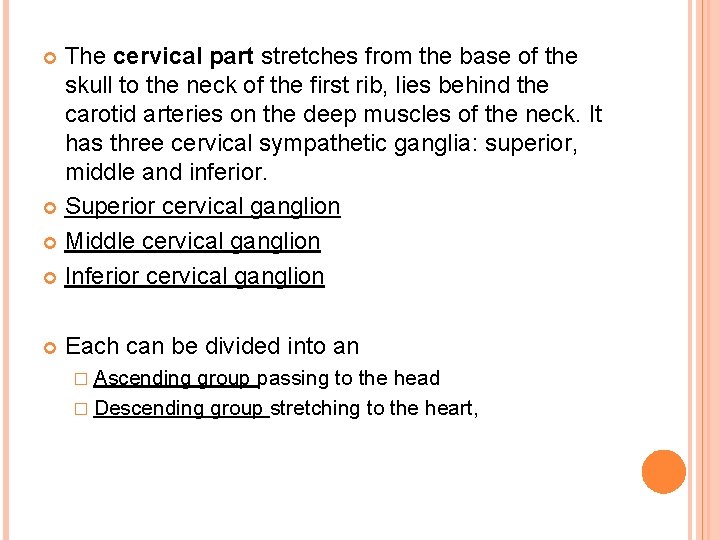
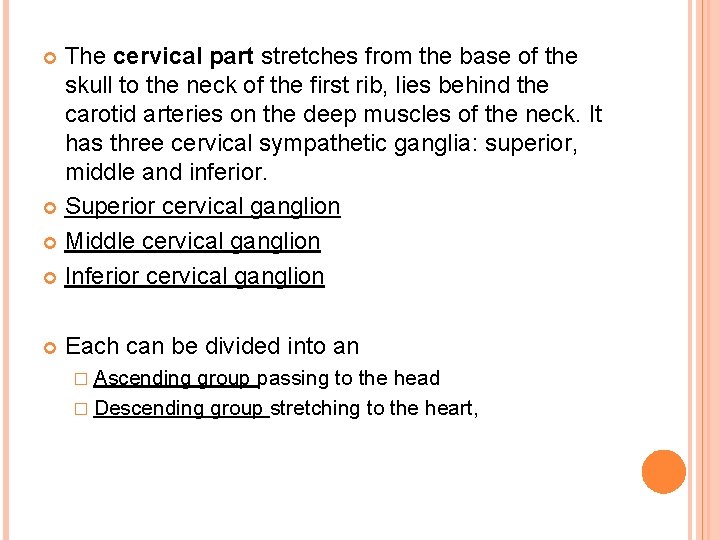
The cervical part stretches from the base of the skull to the neck of the first rib, lies behind the carotid arteries on the deep muscles of the neck. It has three cervical sympathetic ganglia: superior, middle and inferior. Superior cervical ganglion Middle cervical ganglion Inferior cervical ganglion Each can be divided into an � Ascending group passing to the head � Descending group stretching to the heart,
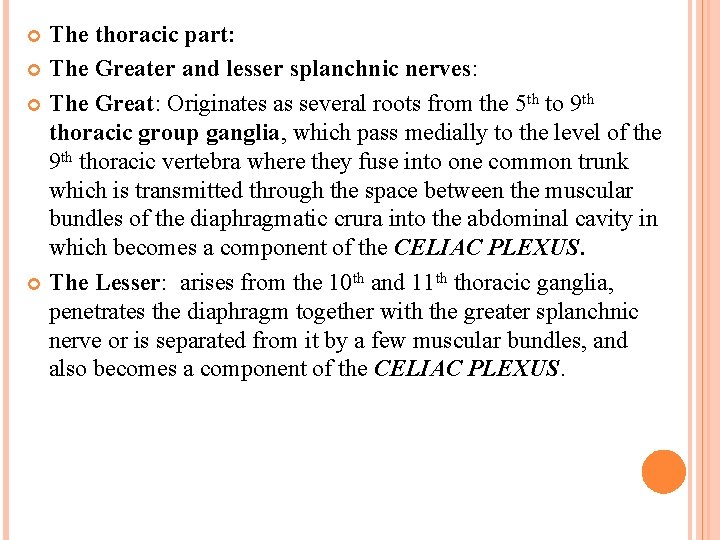
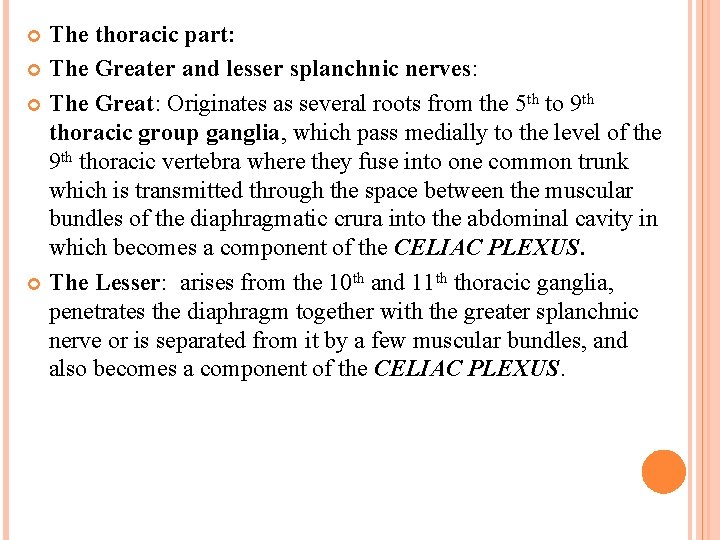
The thoracic part: The Greater and lesser splanchnic nerves: The Great: Originates as several roots from the 5 th to 9 th thoracic group ganglia, which pass medially to the level of the 9 th thoracic vertebra where they fuse into one common trunk which is transmitted through the space between the muscular bundles of the diaphragmatic crura into the abdominal cavity in which becomes a component of the CELIAC PLEXUS. The Lesser: arises from the 10 th and 11 th thoracic ganglia, penetrates the diaphragm together with the greater splanchnic nerve or is separated from it by a few muscular bundles, and also becomes a component of the CELIAC PLEXUS.
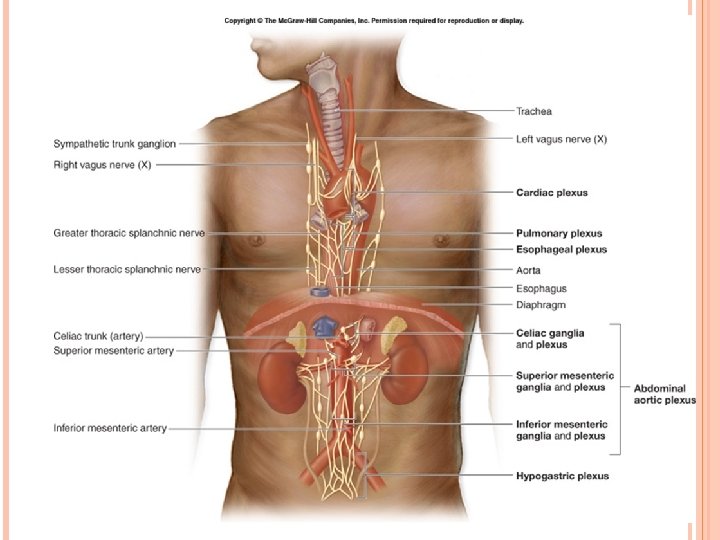
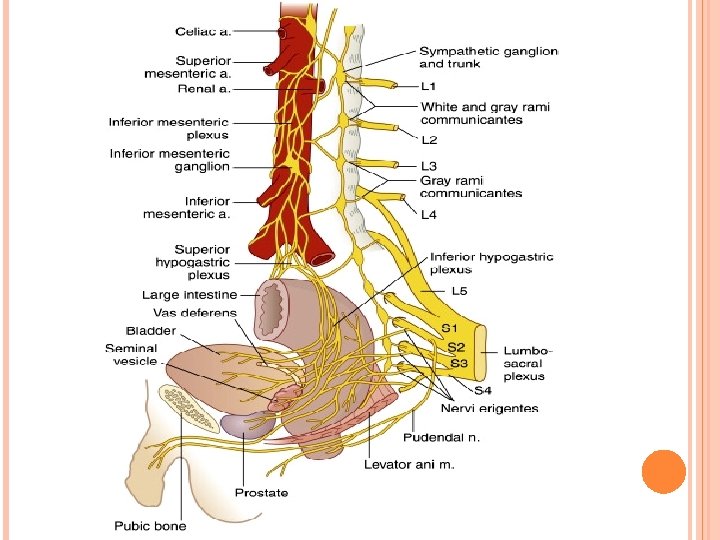
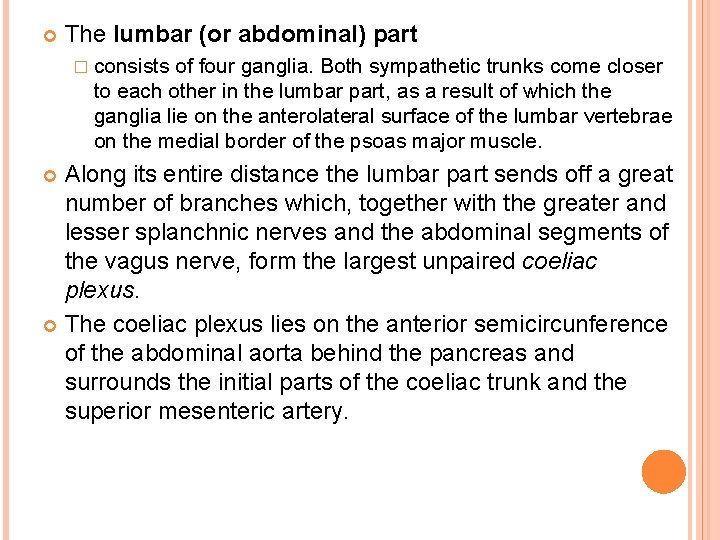
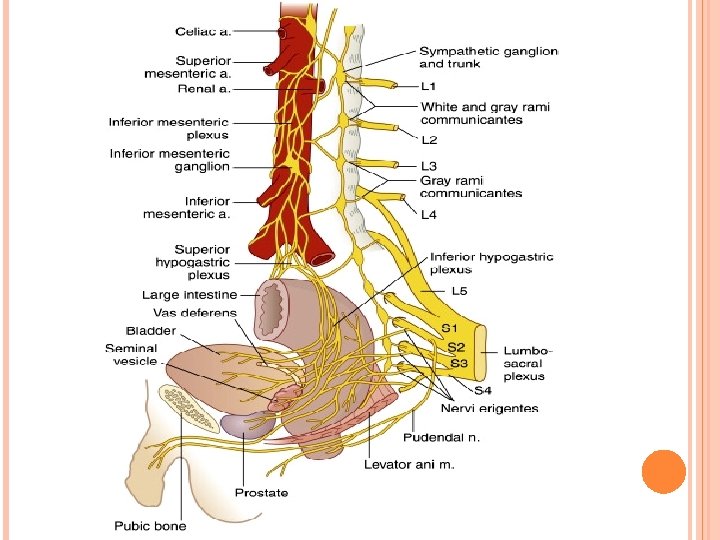
The lumbar (or abdominal) part � consists of four ganglia. Both sympathetic trunks come closer to each other in the lumbar part, as a result of which the ganglia lie on the anterolateral surface of the lumbar vertebrae on the medial border of the psoas major muscle. Along its entire distance the lumbar part sends off a great number of branches which, together with the greater and lesser splanchnic nerves and the abdominal segments of the vagus nerve, form the largest unpaired coeliac plexus. The coeliac plexus lies on the anterior semicircunference of the abdominal aorta behind the pancreas and surrounds the initial parts of the coeliac trunk and the superior mesenteric artery.
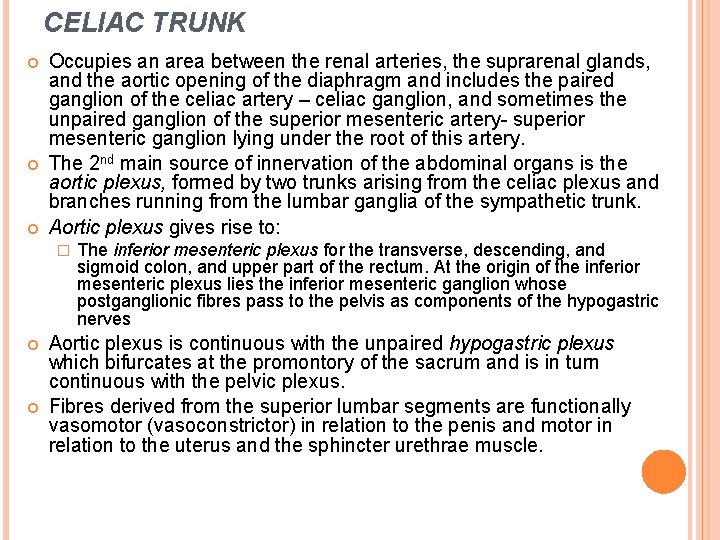
CELIAC TRUNK Occupies an area between the renal arteries, the suprarenal glands, and the aortic opening of the diaphragm and includes the paired ganglion of the celiac artery – celiac ganglion, and sometimes the unpaired ganglion of the superior mesenteric artery- superior mesenteric ganglion lying under the root of this artery. The 2 nd main source of innervation of the abdominal organs is the aortic plexus, formed by two trunks arising from the celiac plexus and branches running from the lumbar ganglia of the sympathetic trunk. Aortic plexus gives rise to: � The inferior mesenteric plexus for the transverse, descending, and sigmoid colon, and upper part of the rectum. At the origin of the inferior mesenteric plexus lies the inferior mesenteric ganglion whose postganglionic fibres pass to the pelvis as components of the hypogastric nerves Aortic plexus is continuous with the unpaired hypogastric plexus which bifurcates at the promontory of the sacrum and is in turn continuous with the pelvic plexus. Fibres derived from the superior lumbar segments are functionally vasomotor (vasoconstrictor) in relation to the penis and motor in relation to the uterus and the sphincter urethrae muscle.
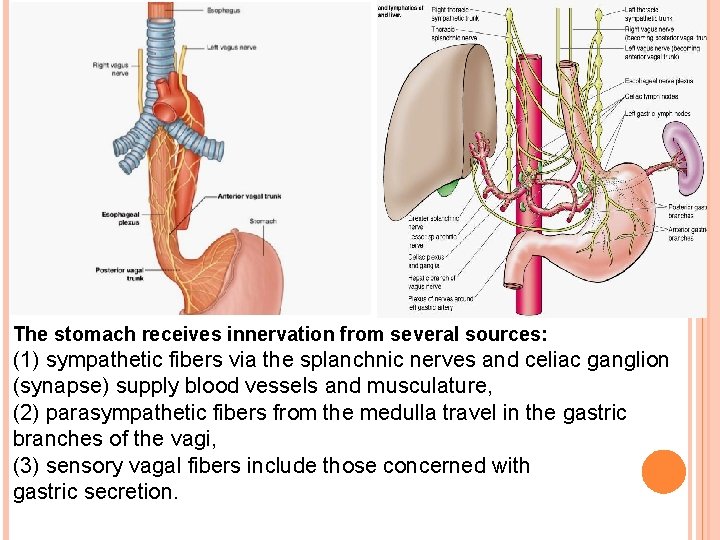
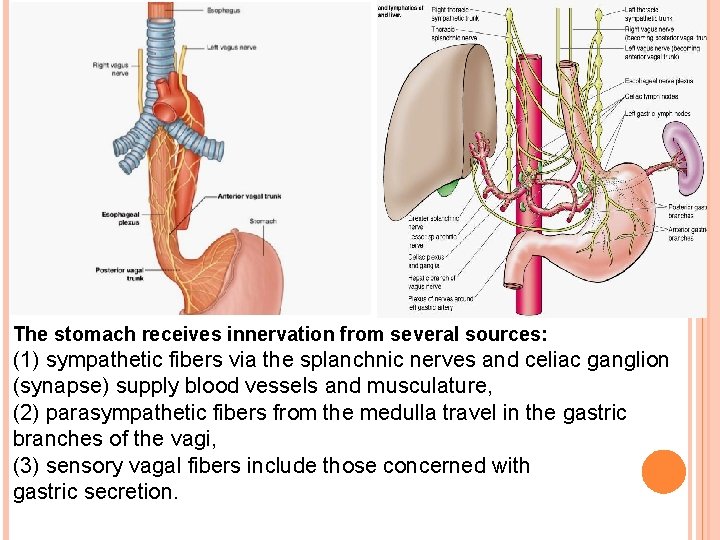
The stomach receives innervation from several sources: (1) sympathetic fibers via the splanchnic nerves and celiac ganglion (synapse) supply blood vessels and musculature, (2) parasympathetic fibers from the medulla travel in the gastric branches of the vagi, (3) sensory vagal fibers include those concerned with gastric secretion.
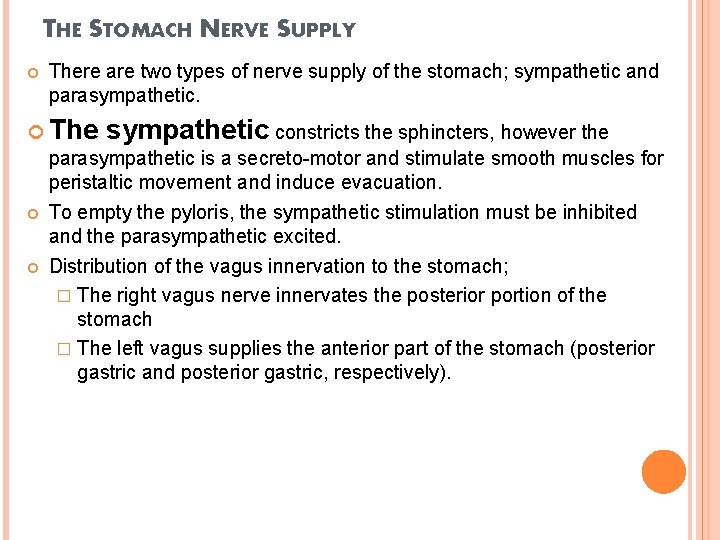
THE STOMACH NERVE SUPPLY There are two types of nerve supply of the stomach; sympathetic and parasympathetic. The sympathetic constricts the sphincters, however the parasympathetic is a secreto-motor and stimulate smooth muscles for peristaltic movement and induce evacuation. To empty the pyloris, the sympathetic stimulation must be inhibited and the parasympathetic excited. Distribution of the vagus innervation to the stomach; � The right vagus nerve innervates the posterior portion of the stomach � The left vagus supplies the anterior part of the stomach (posterior gastric and posterior gastric, respectively).
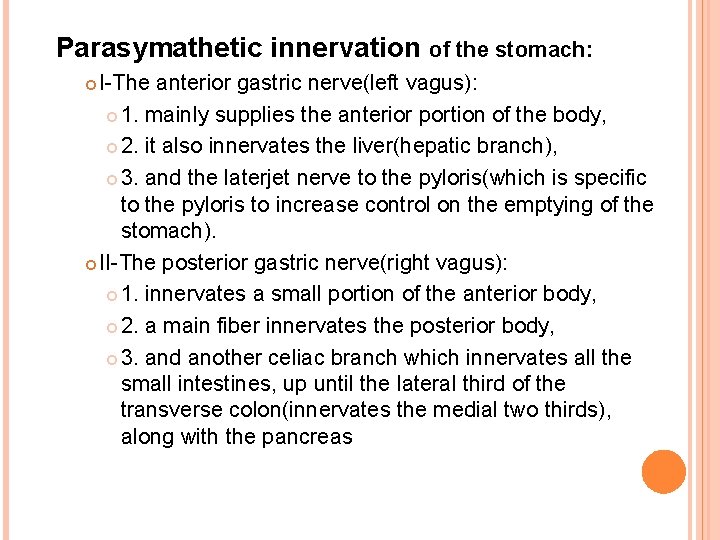
Parasymathetic innervation of the stomach: I-The anterior gastric nerve(left vagus): 1. mainly supplies the anterior portion of the body, 2. it also innervates the liver(hepatic branch), 3. and the laterjet nerve to the pyloris(which is specific to the pyloris to increase control on the emptying of the stomach). II-The posterior gastric nerve(right vagus): 1. innervates a small portion of the anterior body, 2. a main fiber innervates the posterior body, 3. and another celiac branch which innervates all the small intestines, up until the lateral third of the transverse colon(innervates the medial two thirds), along with the pancreas
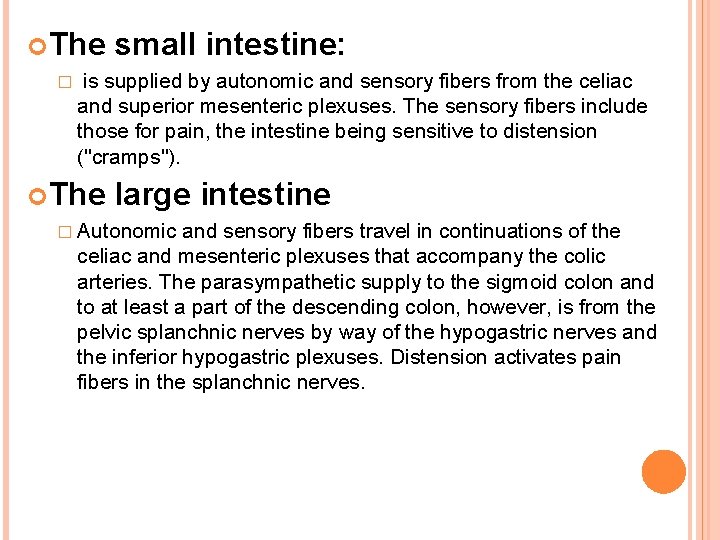
The � small intestine: is supplied by autonomic and sensory fibers from the celiac and superior mesenteric plexuses. The sensory fibers include those for pain, the intestine being sensitive to distension ("cramps"). The large intestine � Autonomic and sensory fibers travel in continuations of the celiac and mesenteric plexuses that accompany the colic arteries. The parasympathetic supply to the sigmoid colon and to at least a part of the descending colon, however, is from the pelvic splanchnic nerves by way of the hypogastric nerves and the inferior hypogastric plexuses. Distension activates pain fibers in the splanchnic nerves.