Inner Ear Disorders Children Lecture 15 Selected Causes
- Slides: 38
Inner Ear Disorders. Children Lecture 15
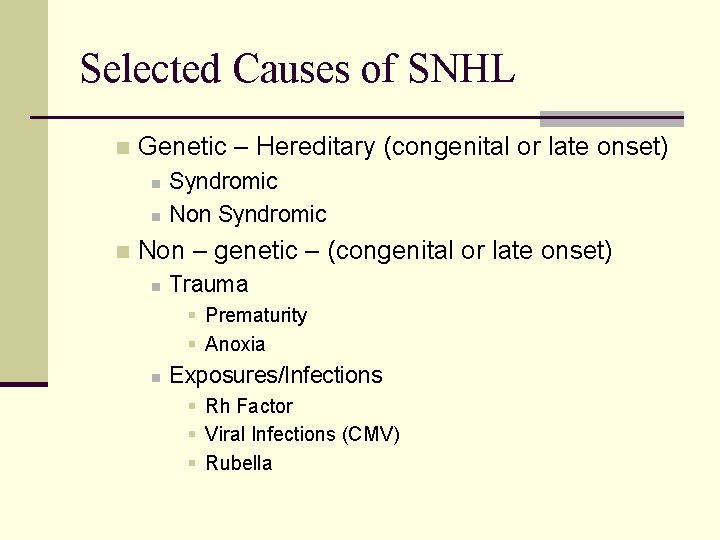
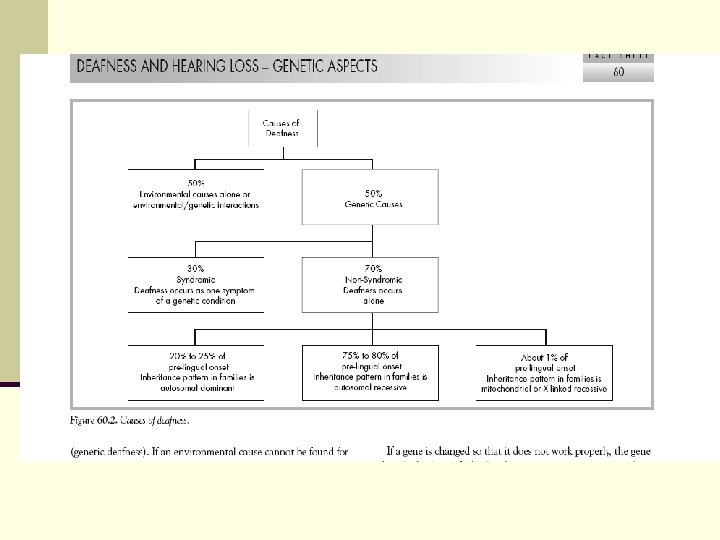
Selected Causes of SNHL n Genetic – Hereditary (congenital or late onset) n n n Syndromic Non – genetic – (congenital or late onset) n Trauma § Prematurity § Anoxia n Exposures/Infections § Rh Factor § Viral Infections (CMV) § Rubella
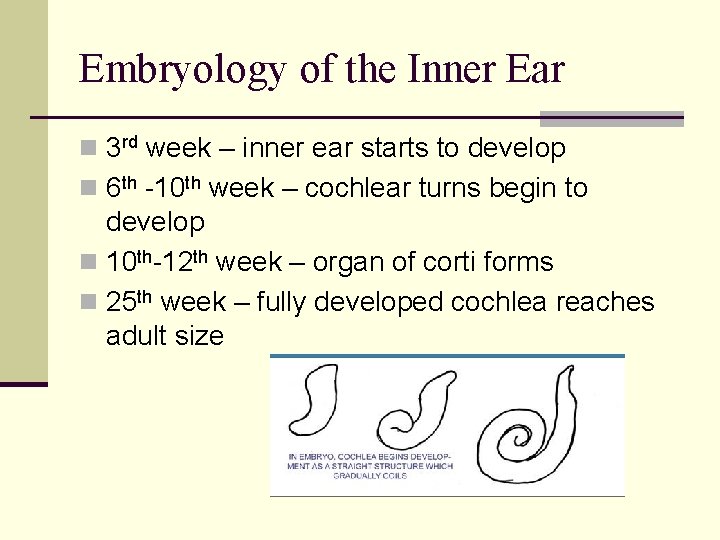
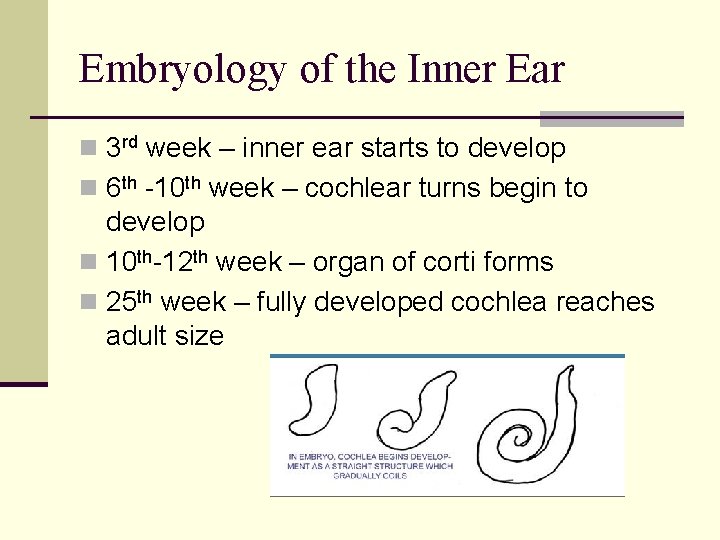
Embryology of the Inner Ear n 3 rd week – inner ear starts to develop n 6 th -10 th week – cochlear turns begin to develop n 10 th-12 th week – organ of corti forms n 25 th week – fully developed cochlea reaches adult size
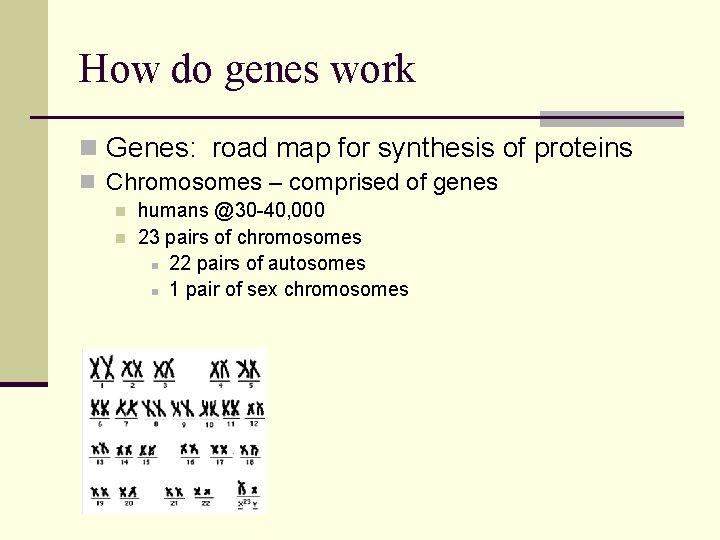
How do genes work n Genes: road map for synthesis of proteins n Chromosomes – comprised of genes n n humans @30 -40, 000 23 pairs of chromosomes n 22 pairs of autosomes n 1 pair of sex chromosomes
Hereditary Patterns n One chromosome from each parent is inherited Male XY - Female XX Gene: basic physical and functional unit of heredity comprised of DNA act as instructions to make proteins n DNA is made up of 4 chemical letters.
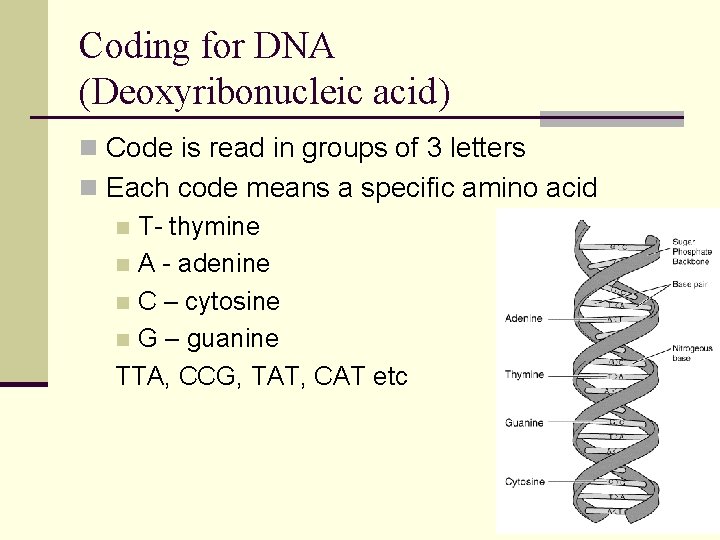
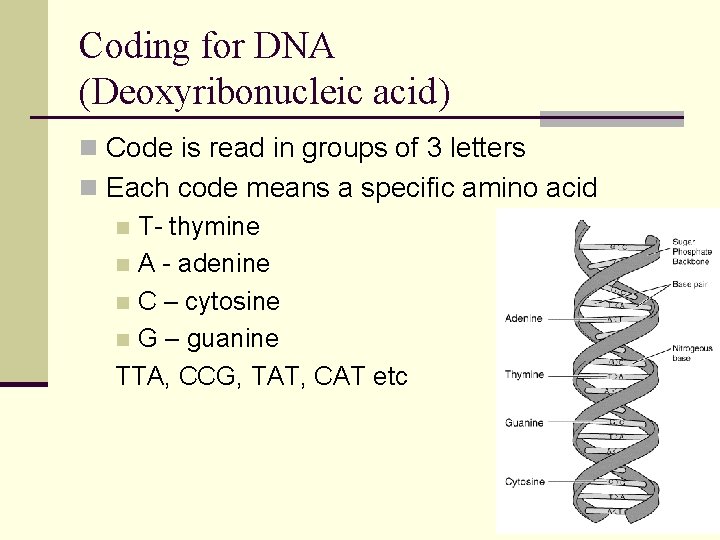
Coding for DNA (Deoxyribonucleic acid) n Code is read in groups of 3 letters n Each code means a specific amino acid n T- thymine n A - adenine n C – cytosine n G – guanine TTA, CCG, TAT, CAT etc
Patterns of genetic codes n Wildtype – common code/typical pattern n Mutation - triplet codes can be changed by substitution deletion insertion n Outcomes: beneficial (rare) n neutral (common) n deleterious (rare) n
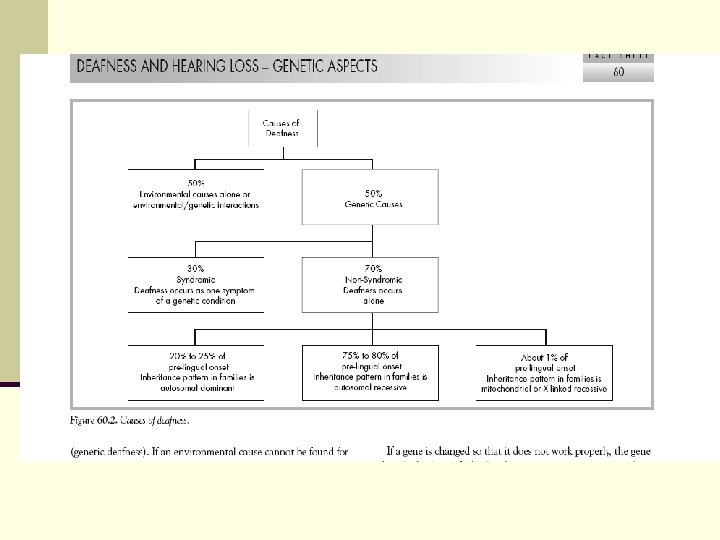
Pre-natal Causes of HL: n Autosomal Dominant: n one gene required from parent for HL to be inherited n Autosomal Recessive: n both parents are carriers for HL, but have normal hearing n X-linked: n recessive alleles are carried on the X chromosome, so HL occurs more in males than females n Mitochondrial : gene passed from mother
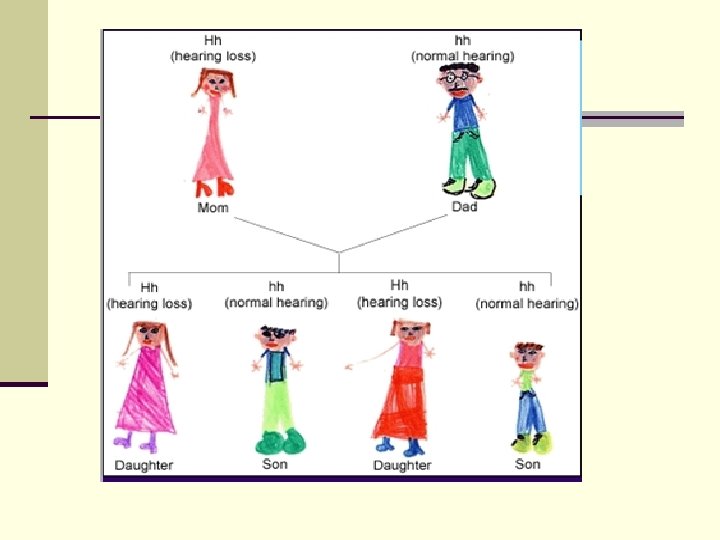
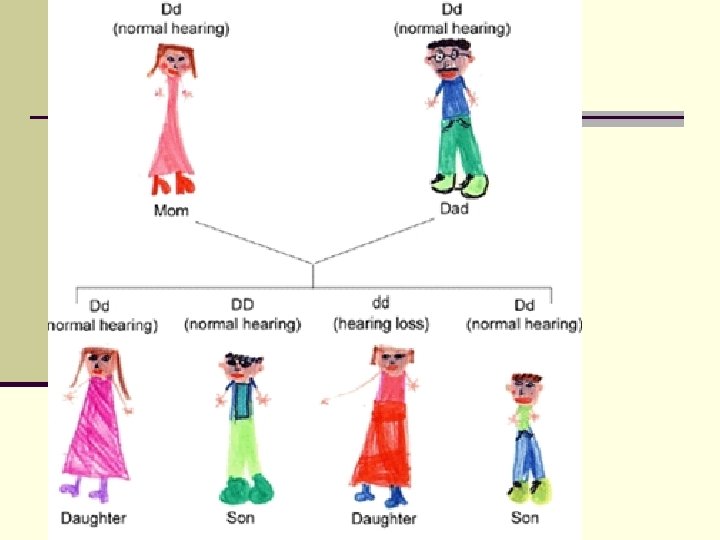
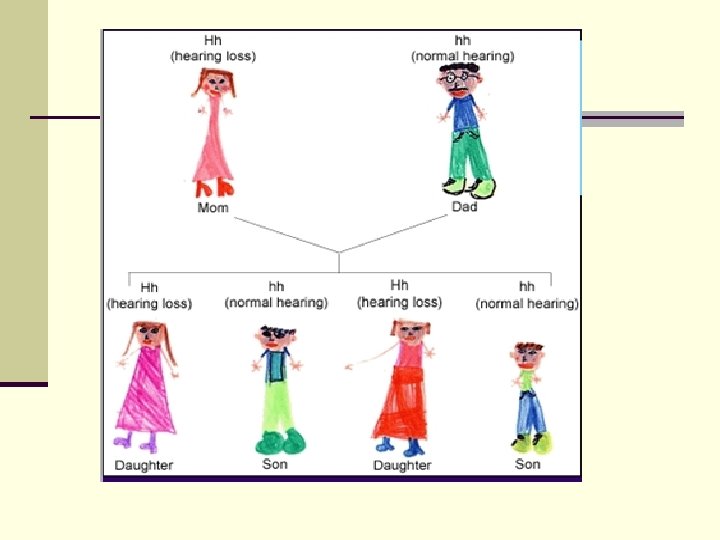
Autosomal Dominant n Mutations occur on an autosome (1 -22) n Child needs to inherit one copy of dominant trait to have disorder. n 50% chance of an affected parent passing gene onto children n Sometimes appears to “skip” generations
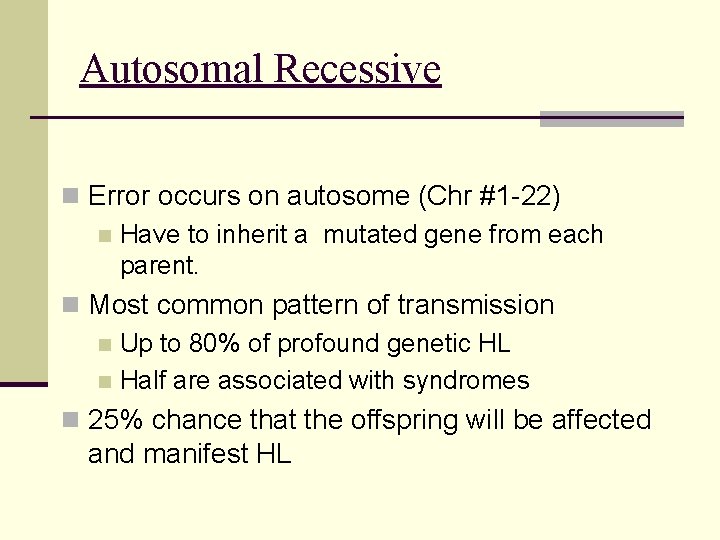
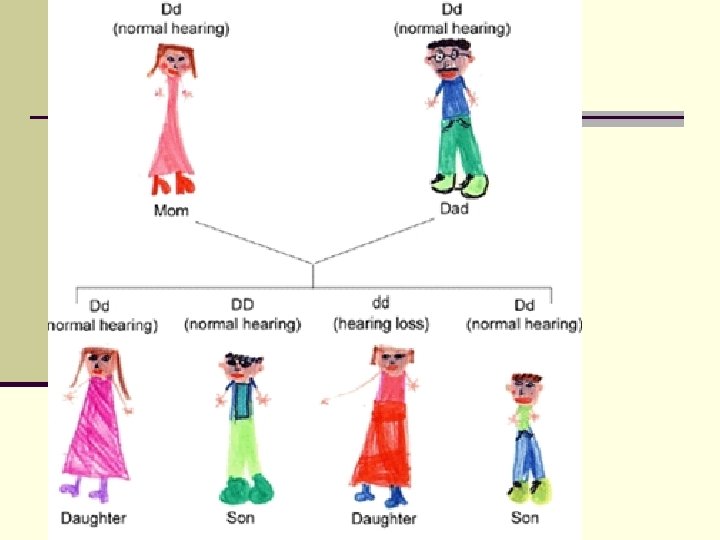
Autosomal Recessive n Error occurs on autosome (Chr #1 -22) n Have to inherit a mutated gene from each parent. n Most common pattern of transmission n Up to 80% of profound genetic HL n Half are associated with syndromes n 25% chance that the offspring will be affected and manifest HL
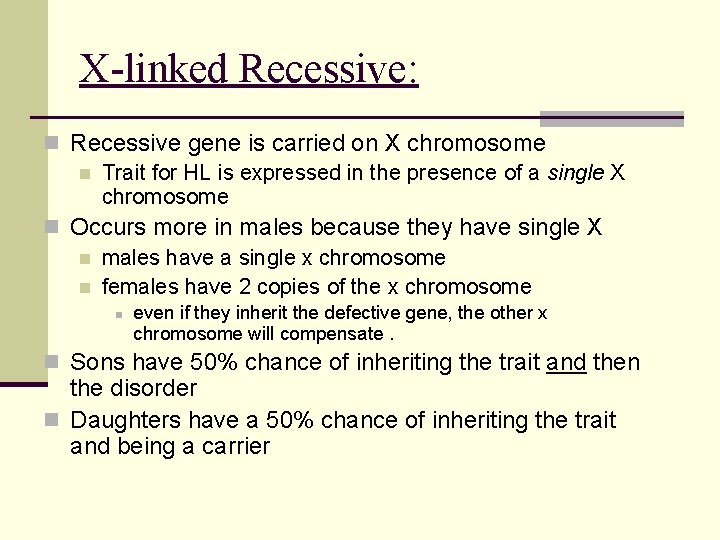
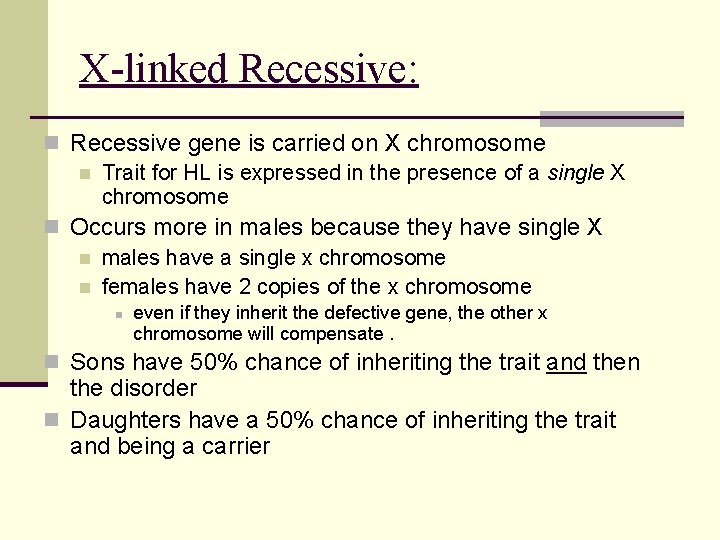
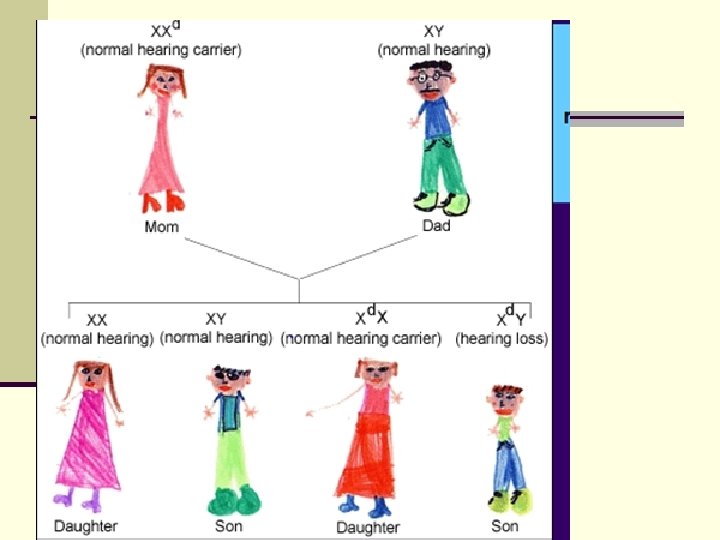
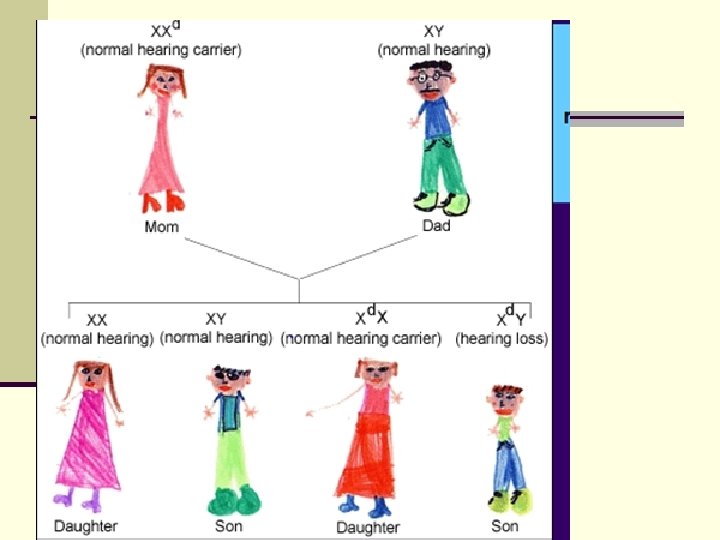
X-linked Recessive: n Recessive gene is carried on X chromosome n Trait for HL is expressed in the presence of a single X chromosome n Occurs more in males because they have single X n males have a single x chromosome n females have 2 copies of the x chromosome n even if they inherit the defective gene, the other x chromosome will compensate. n Sons have 50% chance of inheriting the trait and then the disorder n Daughters have a 50% chance of inheriting the trait and being a carrier
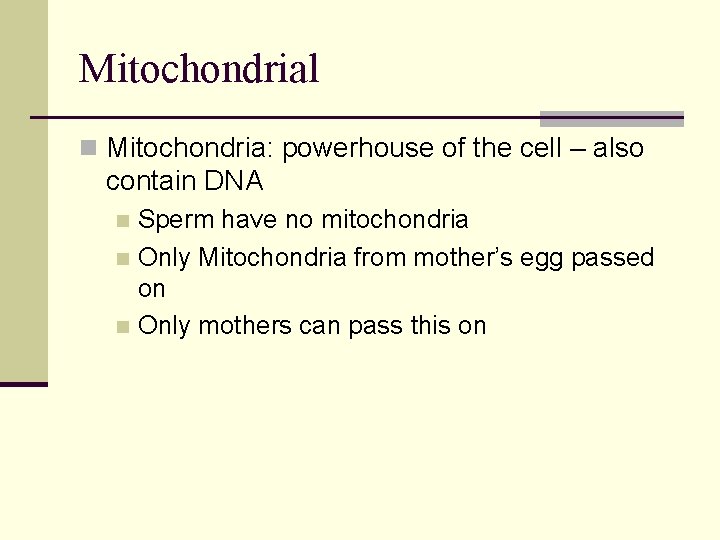
Mitochondrial n Mitochondria: powerhouse of the cell – also contain DNA Sperm have no mitochondria n Only Mitochondria from mother’s egg passed on n Only mothers can pass this on n
Syndromic vs Non-syndromic HL n NON-SYNDROMIC: Cases of hereditary HL & no associated abnormalities n SYNDROMIC: Hereditary HL also assoc w/ other abnormalities i. e. n n n n external ear, skull, facial deformities, cleft palate, optic disorders, changes in eye, hair and skin pigmentation, thyroid disease, disorders of the heart, musculoskeletal anomalies, mental retardation, difficulty with balance
CHARGE Syndrome n C= Coloboma of the eye n Etiology: AD n H= Heart defects n CHL – Common n A= Atresia of nasopharynx n R= retardation of growth or development n G= Genital and/or unrinary problems n E = Ear abnormalities and deafness n SNHL – 90% malformed cochlea
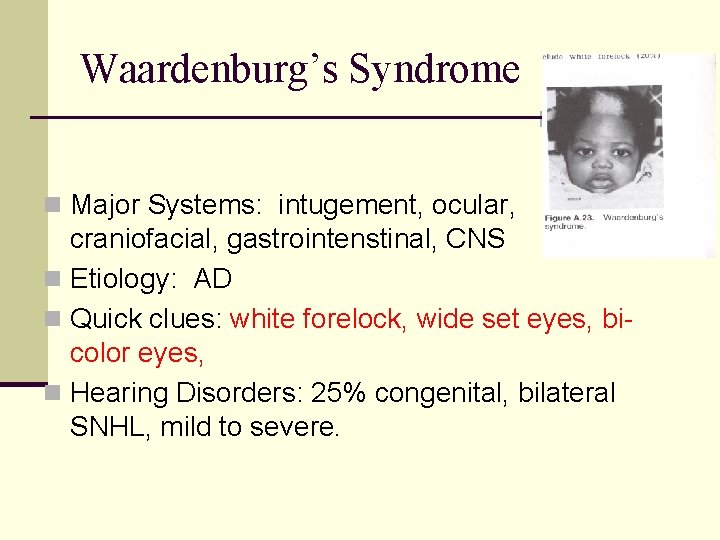
Waardenburg’s Syndrome n Major Systems: intugement, ocular, craniofacial, gastrointenstinal, CNS n Etiology: AD n Quick clues: white forelock, wide set eyes, bicolor eyes, n Hearing Disorders: 25% congenital, bilateral SNHL, mild to severe.
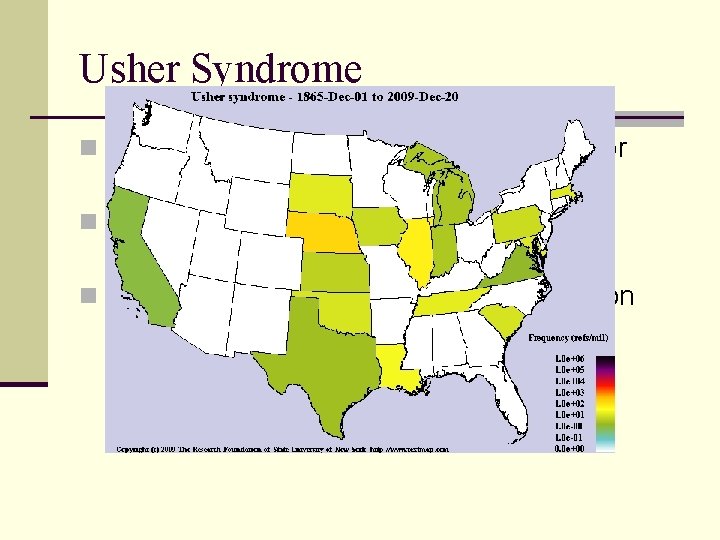
Usher Syndrome (Retinitis Pigmentosa) n Major Systems: Auditory, vestibular, ocular, CNS n Etiology: AR n Quick clues: No external physical clues Association between HL and visual impairment, clumsy gait n Hearing Disorders: Profound, bilateral SNHL n Speech Disorders: Associated with HL
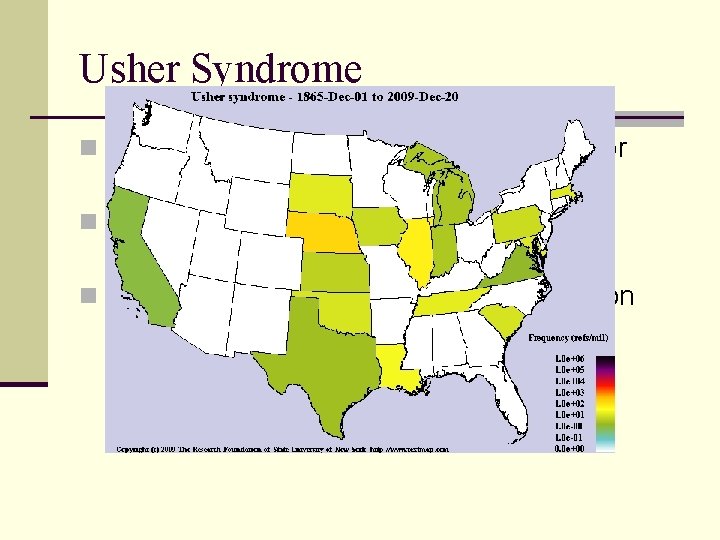
Usher Syndrome n Type I: Profound SNHL, early onset, poor vestibular function n Type II: Severe SNHL, good vestibular function, late onset n Type III : Progressive, variable expression and onset
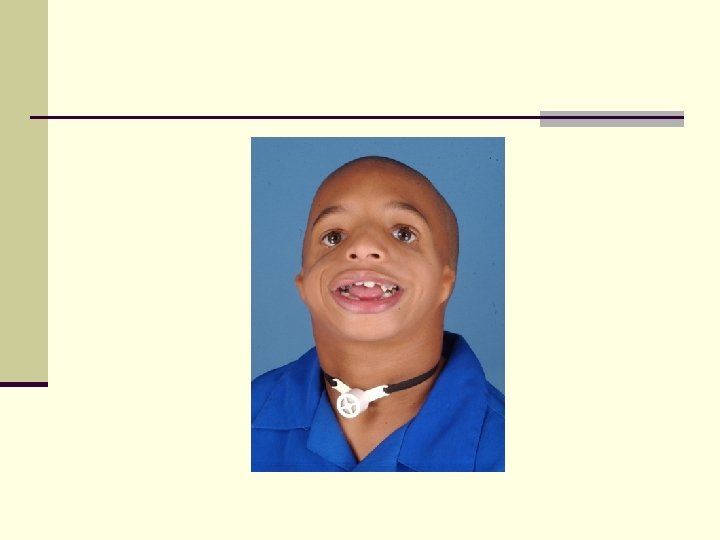
Treacher Collins n Major Systems: Craniofacial, respiratory n Etiology: AD n Quick Clues: Slanting eyes, small jaw, malformed ears, n Hearing Disorders: CHL, mild to moderate n Feeding: sometimes cleft palate, small jaw effects breathing and feeding issues n S/L – crowding in oral cavity, normal IQ, expressive/receptive delays assoc w hearing loss
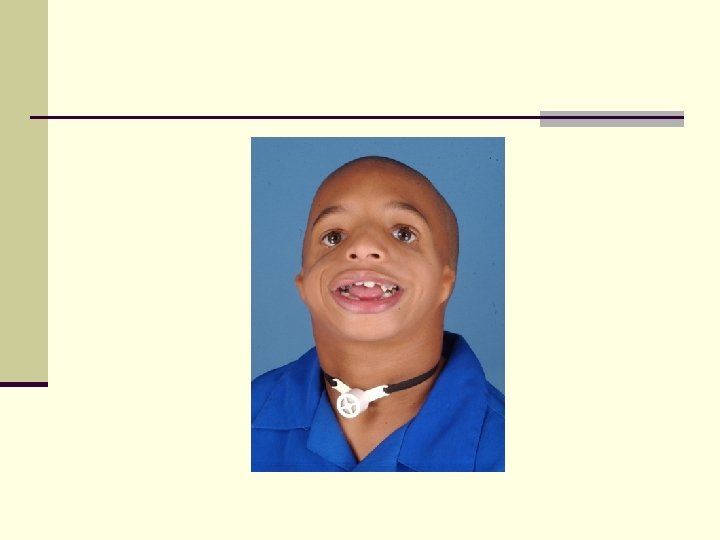
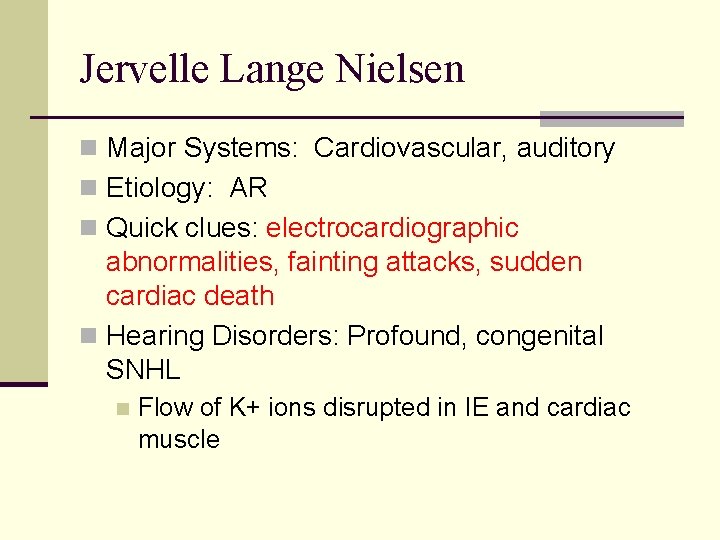
Jervelle Lange Nielsen n Major Systems: Cardiovascular, auditory n Etiology: AR n Quick clues: electrocardiographic abnormalities, fainting attacks, sudden cardiac death n Hearing Disorders: Profound, congenital SNHL n Flow of K+ ions disrupted in IE and cardiac muscle
Genetic: Late onset SNHL in children (Non-syndromic) n Connexin 26 protein found on GJB 2 gene n n n Nonsyndromic, genetic cause of late onset HL Most common (50% of Recessive genetic HL ) Mutation on GJB 2 protein n Screening tests are available n Connexin 30 n n Non-syndromic cause of late onset HL Less common
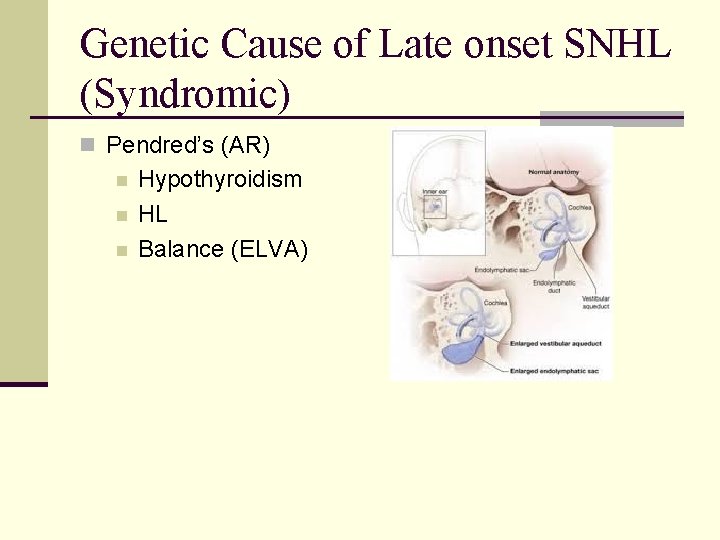
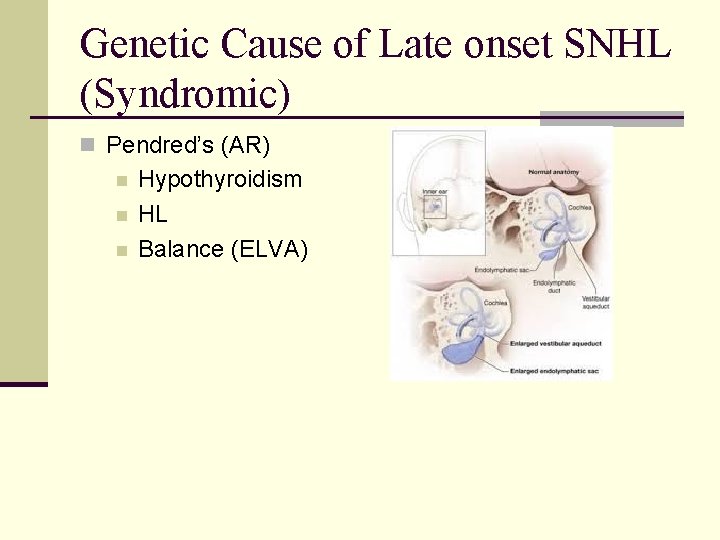
Genetic Cause of Late onset SNHL (Syndromic) n Pendred’s (AR) n n n Hypothyroidism HL Balance (ELVA)
Enlarged Vestibular Aqueduct Syndrome n Genetic origin n Usually a later onset SNHL n Vestibular aqueduct – last IE structure to develop fully n Sudden or fluctuating SNHL, progressive n Aggravated by additional trauma to head n Dxd with a CT scan and history
Non – genetic causes Childhood HL
Prematurity 5% of children born before 32 weeks present with HL by age of 5 n Auditory system not fully developed if premature n n n VLBW Aminoglycosides NIHL Oxygen supply
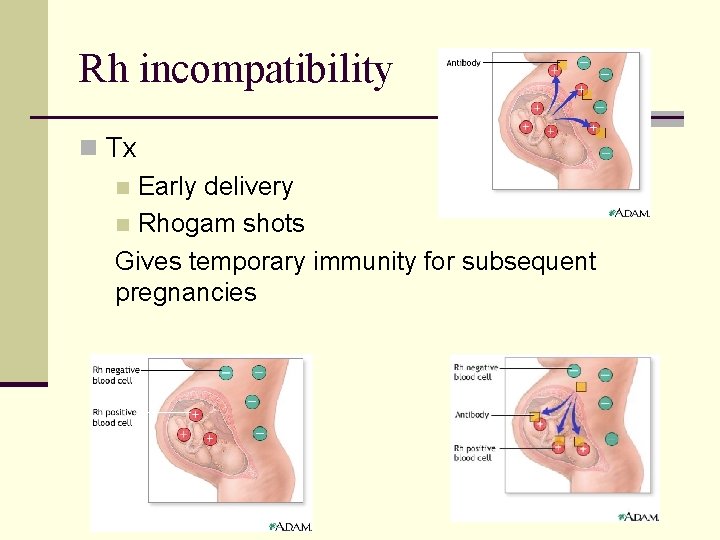
Prenatal causes of HL: Rh Factor n Most people are Rh+ n If mother is Rh- and partner is Rh+ n Protein in “Rh” blood molecule is absent (negative) in the mother, but present (positive) in the fetus. n When Rh negative blood is exposed to Rh positive blood, the Rh negative person begins producing antibodies to fight off invading blood n n An Rh- mother will develop antibodies to protect herself against the harmful effects of Rh + blood cells of the fetus. Her antibodies destroy the Rh + blood cells of the fetus which can no longer carry oxygen to the cochlea
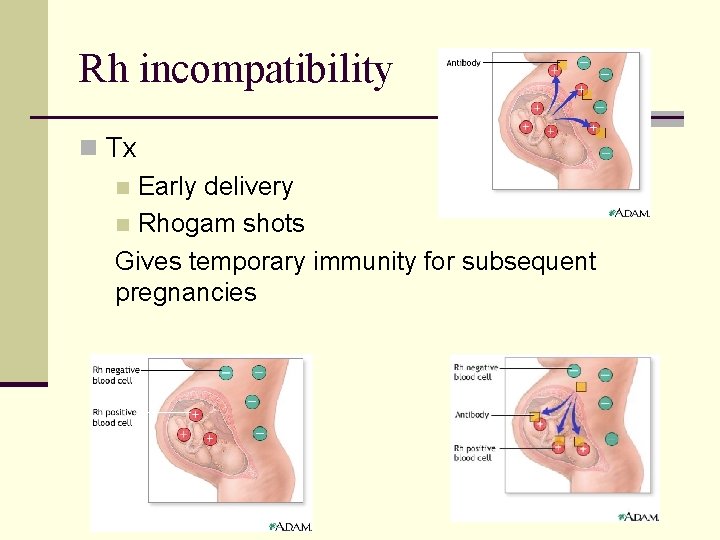
Rh incompatibility n Tx Early delivery n Rhogam shots Gives temporary immunity for subsequent pregnancies n
Cytomegalovirus (CMV) si-to-MEGuh-lo-vi-rus Viral Infection – herpes group Transmission prenatally, perinatally or postnatally CMV spreads from person to person by direct contact. CMV infection is usually harmless, it can cause severe disease in persons with weakened immune systems n Considered major cause of unknown etiology for SNHL n Asymptomatic or Symptomatic CMV n 31% of infants infected with CMV manifest HL (Johnson et al, 1986) n n
Who is at risk for CMV? n Babies born to women who have a first-time CMV infection during pregnancy n Pregnant women who work with infants and children n Persons with weakened immune systems, including cancer patients on chemotherapy, organ transplant recipients, and persons with HIV infection
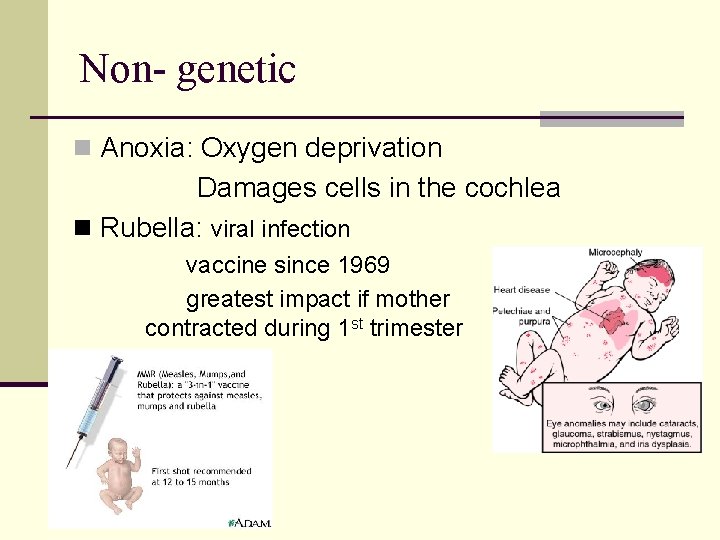
Non- genetic n Anoxia: Oxygen deprivation Damages cells in the cochlea n Rubella: viral infection vaccine since 1969 greatest impact if mother contracted during 1 st trimester
Meningitis n Infection of the fluid around the spinal cord n Causes inflammation of the meninges n Viral – more common n Bacterial – rare n Outcome n Viral: less severe n Bacterial: n n 1/10 – fatal 1/7 severe handicap
Meningitis n Bacteria and viruses that infect the skin, urinary system, gastrointestinal or respiratory tract can spread through the bloodstream to the meninges n Spread by direct contact with the discharges from the nose or throat of an infected person n Not easily spread – not airborne n 10 -25% of population is a carrier at any one time n Bacteria do not live outside the body
Possible outcomes from bacterial meningitis n SNHL n Paralysis n MR n Seizures n Coma/Death
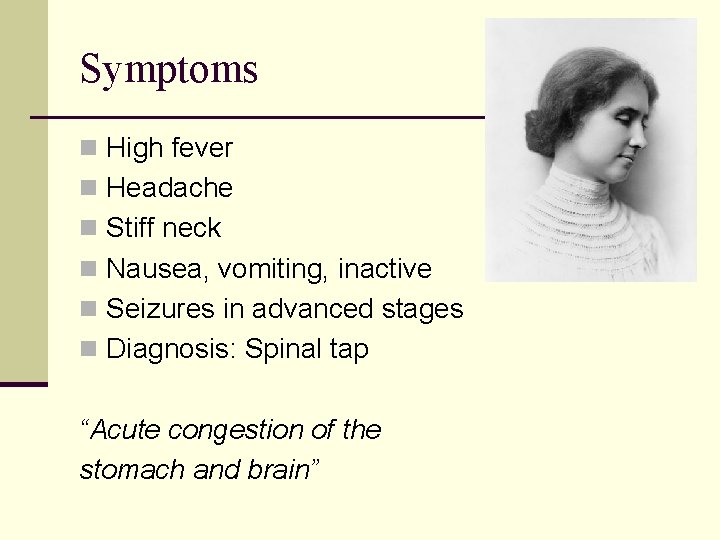
Symptoms n High fever n Headache n Stiff neck n Nausea, vomiting, inactive n Seizures in advanced stages n Diagnosis: Spinal tap “Acute congestion of the stomach and brain”