Initial Nursing Assessment for Spiritual Religious Needs Tedford
- Slides: 18
Initial Nursing Assessment for Spiritual / Religious Needs Tedford J. Taylor, MDiv, BCCC Director of Pastoral Care & Training ttaylor@rwjuhh. edu DO NOT DUPLICATE WITHOUT AUTHOR’S PERMISSION © 2012
Why A Spiritual Assessment? Faith is already a factor affecting the lives and healthcare choices of many of our patients. Most patients and their families already use faith-based / religious practices (like prayer, diet, ritual, etc. ) to complement treatment modalities. Healthcare practitioners need to assess how faith impacts individual treatment choices. A spiritual assessment is less about WHAT a person believes and more about HOW their faith / belief system functions as a source of support.
Joint Commission Guidelines for Spiritual Assessments n n n Spiritual assessments are required by the Joint Commission. A spiritual assessment should, at a minimum, determine the patient’s religious beliefs (if any), as well as any values or practices important to the patient. The main goal of a spiritual assessment should be to identify the patient’s needs, hopes, resources, and possible outcomes regarding their spirituality. Joint Commission: “The Source”, February 2005, Vol. 3, Iss. 2
Other Benefits of A Spiritual Assessment Acknowledging spirituality can positively affect the clinician-patient relationship. Addressing spiritual concerns with your patient and their family can provide comfort and increase trust-building. In itself the assessment becomes a therapeutic intervention.
Important Considerations n Respect the privacy of patients with regard to their unique spirituality. n Do not impose your own beliefs and practices on others.
The FACT Initial Spiritual Assessment Tool n n n The FACT Tool is a hybrid of history and assessment. A Spiritual History collects information on spirituality and religious practice that may help them cope with their present health crisis. A Spiritual Assessment involves an informed judgment concerning treatment options – including referral to a chaplain for a more in-depth assessment.
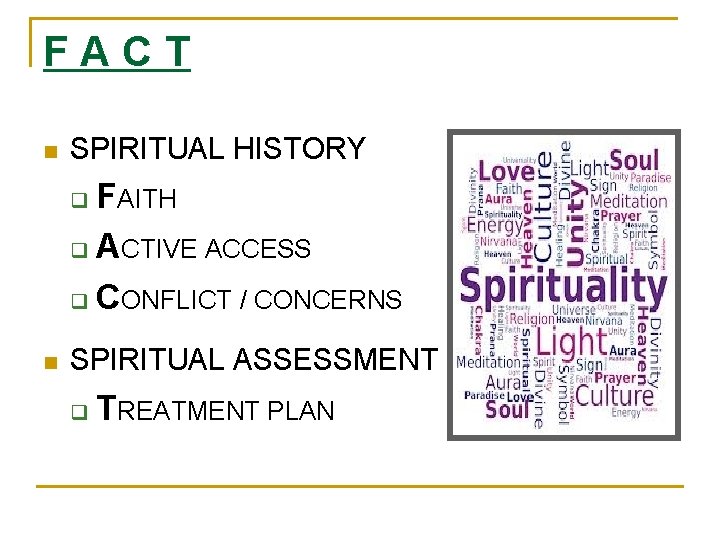
FACT n SPIRITUAL HISTORY FAITH q ACTIVE ACCESS q CONFLICT / CONCERNS q n SPIRITUAL ASSESSMENT q TREATMENT PLAN
Nursing Intake Spiritual Assessment Questions n The following questions are part of a new spiritual assessment process. n Positive answers trigger instant referrals for followup pastoral care, such as: q q q Communion requests Communication with the patient’s religious congregation Consultation on issues of religious / cultural sensitivity In-depth spiritual assessment by a chaplain General emotional or spiritual support by a chaplain
Faith n Can you confirm your religious affiliation that I have recorded from your admission documents? (Check patient's ID band for religious affiliation). I see you are (religious affiliation). Is this correct? q Contact admissions office to update / correct this information.
Faith n If patient is Catholic, would he/she like to receive communion? q q SCRIPT: “Eucharistic Ministry volunteers are available daily to distribute communion to Catholic patients and their families. ” Generates an automatic referral to pastoral care.
Active Access n Do you participate in a religious congregation? q q SCRIPT: “Our pastoral care team will help you contact them. I’ll let the team know of this request. ” Generates an automatic referral to pastoral care.
Active Access Pastoral care is offered to all patients. Would you like me to expedite a visit from one of the pastoral care team members? n q q Call chaplain on duty (*072) if there is an emergent need for pastoral support. “Yes” generates an automatic referral to pastoral care.
Conflict / Concerns n What cultural, spiritual, or religious practices / values are important for us to know? q SCRIPT: “I’ll work with my colleagues to make sure we work with you on these concerns. ” q Free-text assessed needs. q Consult with Pastoral Care as appropriate.
Conflict / Concerns Do any of your religious practices conflict with or affect how we will need to treat you while you are here? (Example: diet, medication, visitors, privacy, rituals. ) n q SCRIPT: “I’ll work with my colleagues to make sure we work with you on these concerns. ” q Free-text assessed needs. q Update plan of care as appropriate. q Dietary or Pastoral Care Departments are automatically referred.
Conflict / Concerns n Do you have any particular concerns or fears about your stay in the hospital? q q q Address those fears / concerns that you are able to. SCRIPT: “Our chaplains are also here to help address many of these concerns. Would you like me to expedite a visit from one of the chaplains? ” Generates an automatic referral to pastoral care.
Treatment Plan Does the patient appear to be coping well and have adequate social / emotional / spiritual support? n q q q Free-text assessed needs. Call chaplain on duty (*072) if there is an emergent need for pastoral support. Non-emergent needs (“no” answers) generate an automatic referral to pastoral care.
Final Thoughts n If questioned on the role of pastoral care and chaplains refer the patient / family to facility guides. Or, contact pastoral care for assistance.
Final Thoughts n Referrals to pastoral care generated by the FACT assessment will be completed in 24 hours. A chaplain will visit to further assess ongoing issues and pastoral care needs. n Urgent pastoral care needs (emergency sacraments, family crises, death / dying issues) should be referred to the chaplain on duty for immediate response.